Trifecta for the Fussy Breastfeeding Infant: Clinical Care in the Infant
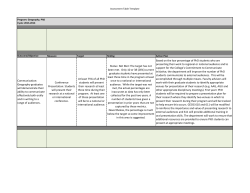
Integrated behavioral health in pediatrics: From practicalities of practice to policy change March 23, 2015 Maya Bunik, MD, MSPH Ayelet Talmi, PhD Christopher Stille, MD, MPH Cody Belzley Maya Bunik, MD, MSPH Associate Professor, Pediatrics Ayelet Talmi, PhD Associate Professor, Psychiatry and Pediatrics GETTING STARTED, PRACTICAL APPLICATIONS, DISSEMINATION, & SYSTEMS ISSUES Maya Bunik, MD, MSPH Ayelet Talmi, PhD No financial disclosures or conflicts 3 PROJECT CLIMB: CONSULTATION LIAISON IN MENTAL HEALTH AND BEHAVIOR INTEGRATING BEHAVIORAL HEALTH INTO PEDIATRIC PRIMARY CARE 4 CLIMB…how we started • Partnership of Psychiatry and Pediatrics • Initial Health Foundation funding Started with: • Developmental screening (>85% rates) • Added pregnancy-related depression screening • Built foundation of collaboration and comanagement of two disciplines • Planned for sustainability with funds from ASQ & Dept of Peds making it whole 5 Generously Funded By: with special thanks to Children’s Hospital Colorado Foundation and Kathy Crawley and Jennie Dawe • American Academy of Child and • • • • • • Adolescent Psychiatry Access Initiative Grant Rose Community Foundation: Access to Mental Health Services CLIMB to Community The Colorado Health Foundation Pediatric Resident Education Caring for Colorado Walton Family Foundation CLIMB to Community Liberty Mutual Denver Post Season to Share Administration: Maya Bunik, MD, MSPH Kelly Galloway, RN Ayelet Talmi, PhD Our Team Pediatric Residents and Trainees: Psychologists: Melissa Buchholz, PsyD Emily Muther, PhD Kate Margolis, PhD Aurora Mental Health Clinician: Cathy Danuser, LPC Psychiatrists: Leigh Anne Bakel, MD Scott Canna, MD Jacinta Cooper, MD Michael DiMaria, MD Thomas Flass, MD Adam Green, MD Danna Gunderson, MD Kasey Henderson, MD Ashley Jones, MD Sita Kedia, MD Gina Knapshaefer, MD Courtney Lyle, MD Catherine MacColl, MD Jennifer McGuire, MD Michelle Mills, MD Amy Nash, MD Rupa Narra, MD Nicole Schlesinger, MD Teri Schreiner, MD Heather Wade, MD And many more… Kim Kelsay, MD Celeste St. John-Larkin, MD Postdoctoral Fellows: Shannon Beckman, PhD, Steven Behling, PhD, Anna Breuer, PsyD, Melissa Buchholz, PsyD, Bridget Burnett, PsyD, Dena Dunn, PsyD, Kendra Dunn, PsyD, Emily Fazio, PhD, Barbara Gueldner, PhD, Rachel Herbst, PhD, Jason Herndon, PhD, Jennifer Lovell, PhD, Kate Margolis, PhD, Dailyn Martinez, PhD, Christine McDunn, PhD, Brigitte McClellan, PsyD, Brenda Nour, PhD, Sarah Patz, PhD, Psychology Interns: Megan Allen, MA, Caitlin Conroy, MA, Tamie DeHay, MA, Barbara Meg Picard, PsyD, Shawna Roberts, PsyD, Kriston Schellinger, PhD, Casey Wolfington, Gueldner, MA, Patrece Hairston, PsyM, Erin PsyD Hambrick, MA, Idalia Massa, MA, Jessican Psychology Trainees: Dena Miller, MA, Keri Linas, MA, Emma Peterson, MA, Jessica Technow, MA, Crosby Troha, MA Research Interns: Hamid Hadi, Traci Lien, MD, Iman Mohamed, Cody Murphy, BA, Molly Nowles, BA, Shagun Pawar, BA, Nick Pesavento, Clare Rudman, Danica Taylor, BA, Jen Trout, BA, Zeke Volkert, MD, Tyler Weigang, MPH Malmberg, MA, Alexis Quinoy, MA, Ryan Roemer, MA, Justin Ross, MA, Cristina Scatigno, MA, Tess Simpson, MA, Michelle Spader, MA, Bethany Tavegia, MA, Crosby Troha, MA, Brennan Young, MA, Jay Willoughby, MA CHC Faculty Mandy Allison, MD Edwin Asturias, MD Steve Berman, MD Karen Call, MD Mandy Dempsy, MD Gretchen Domek, MD Karen Dodd, PNP Brandi Freedman, MD David Fox, MD Annie Gallagher, MD Sita Kedia, MD Allison Kempe, MD Lindsey Lane, MD Maureen Lennsen, PNP Tai Lockspieser, MD Dan Nicklas, MD Steve Poole, MD Bart Schmidt, MD Chris Stille, MD Christina Suh, MD Meghan Trietz, MD Shale Wong, MD CHC Staff Liz Gonzales Nicole Vallejo-Cruz CLIMB Research Team Ryan Asherin, BA Mandi Millar, BA Iman Mohamed Marianne Wamboldt, MD & Bob Brayden, MD (original PIs) Brian Stafford, MD, MPH (co-PI) Child Health Clinic • Children’s Hospital Colorado • Large Urban Primary Care Teaching Clinic • Low income= >90% Medicaid/SCHIP • 29,000 visits per year • 60% of visits for zero to 3 years • 56% Hispanic, 40% Spanish Primary Language • Pod based clinic design • Dissemination to community based clinics Page 8 Program and Services • Developmental Screening Initiative (Child) • Pregnancy related depression (PRD) screening (Caregiver, • • • • • • • • Child, Family) Healthy Steps for Young Children & MIECHV (Child, Caregiver, Family) Baby & Me at the CHC (Child, Caregiver, Family) Case-based consultation (Child, Caregiver, Family) Care coordination, triage, and referral (Child, Caregiver, Family) Psychopharmacology consultations (Child) Counseling and brief therapy services (Child, Caregiver, Family) CLIMB to Community pilot (Child, Caregiver, Family) Training and education (Providers/Health Professionals) Formal didactics Precepting trainees Collaborative care 10 12 Clinician Identified Problem by Consultation Type (%) * Mothers of patients birth to 4 months were screened for pregnancy-related depression CLIMB Initiatives • Pregnancy-related depression • Ages and Stages Developmental • • • • Screening Healthy Steps for Young Children Program Baby and Me Group visits Second Hand Smoke and Motivational Interviewing Trifecta for Breastfeeding Management 14 Pregnancy-Related Depression • Formal screening at well-child visits from birth to four months using Edinburgh Postnatal Depression Scale (Cox et al., 1987) • Primary care services Training for providers Psychoeducation Support to mothers Referral Electronic medical record • System changes Capacity building • (Caregiver, Child, Family) PRD data • 89% of mothers seen for well child visits < 4 • • • months of age get screened 10% of mothers scored ≥10 on at least one visit. 60 % by CLIMB provider only, 4% (21/508)social worker (SW), 11 % Those mothers who score high have more clinic visits as part of their treatment compared to those that do not (means 2.6 (1.1 sd), median 3.0 and 2.3 (1.1 sd), median 2.0, respectively 16 17 Developmental Screening and Closing the Referral Loop Talmi A, Bunik M Pediatrics 2014 18 ASQ and EI Findings • Developmental screening and referral is necessary but not sufficient. • Success of developmental screening process depends on enhancing referral completion. • An intervention providing phone follow-up and assistance with referral yielded higher rates of referral and greater provider knowledge of referral outcomes. Talmi A, Bunik M Pediatrics 2014 Healthy Steps for Young Children (www.healthysteps.org) • Provide enhanced developmental services in • • • • • pediatric primary care settings; Focus on developing a close relationship between the clinician and the family in order to address the physical, socioemotional, and cognitive development of babies and young children; Currently used in 18 residency training programs nationally MIECHV funding to expand our program and develop new sites across Colorado Baby & Me at the CHC (Child, Caregiver, Family) Content analysis of well-child visits, Healthy Steps vs. control (Buchholz & Talmi, 2012) 17% Breast Feeding 70% * 11% Postpartum depression 48%** 6% How parent is feeling 75%** 3% Child Care 23% * 56% Home Safety Temperament 90% * 0% 28% * Promoting healthy eating Healthy Steps 28%** 28% Sleep Daytime/Nighttime routines Control 6% 63%** 0% 35%** 3% Importance of Play 33%** 3% Social Skills 38% * 8% Language Development 35% * 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% * ≤ 0.03 **≤ 0.01 Baby & Me at the CHC (Child, Caregiver, Family) 23 24 25 Bunik M et al. Pediatrics July 2013 26 Methods: MI Intervention The pediatric provider offers a MI session to help make a plan for cessation or reduction. If yes, trained provider meets family for 20 minute session. CLIMB providers are primary counselors for the intervention. If no, reasons for refusal are solicited. 27 Results: Survey for Satisfaction • At the 1 week surveys, 81% (n=25/31) • • • reported MI definitely worth their time. 81% (n=25/31) felt MI educator understood their situation very or fairly well. 77% (n=24/31) found the quality of the MI program excellent or good. 70% reported that most or almost all of the of the participants needs were met (n=21/30) 28 Summary of SHS Findings • The 'ONE Step' Quality Improvement intervention was associated with a higher quit rate (14%) compared to Colorado 2008 state data for low SES population (5%). • Most parent/caregivers reported reductions in smoking behaviors • Addition of MI looks promising but need to talk to families ‘treat it as an MI emergency’ Bunik M et al. Pediatrics July 2013 29 Breastfeeding Management Evaluation earlier is better and support from an infant mental health specialist is crucial It’s Complicated • • • • • • • • Pregnancy-related depression Paternal depression Sleep expectations/deprivation Sibling adjustment Financial stress Other family stressors Transition to parenthood Previous fertility or loss issues Bunik M J Hum Lact 2014 31 What We Do: The Trifecta Model 1. Comprehensive functional breastfeeding assessment and intervention: • Physical exam • Medical history • Psychosocial history • Pre-post feeding weights • Assess latch • Evaluate milk transfer • Observe infant regulation • Post hospitalization feeding plan • Evaluate baby growth and milk supply 2. Psychosocial assessment and support: • Evaluate family adjustment • Assess pregnancy-related depression/Administer EPDS • Acknowledge and support partner’s involvement in feeding routines • Discuss sibling adjustment • Self-care: • “Baby out of the building” • Enjoyable activities • Help with childcare Community Intervention Family Baby Intervention Breastfeeding Dyad 3. Follow-up recommendations, future planning, and referrals: • Communication with medical home • Discuss return to work • Pumping • Childcare • Planning feeding and sleep routines • Community referrals if needed: • Fussy Baby Network • Mental health referral • Occupational therapy Lactation Consultant + Pediatrician + Psychologist Bunik, Dunn, Talmi, & Watkins, 2012. Do not distribute without permission. 32 Dissemination: CLIMB to Community • CLIMB to Community intends to implement and evaluate the sustainability of integrated behavioral health services in community-based pediatric primary care practices serving publicly insured children by disseminating the Project CLIMB model. • Expansion of integrated behavioral health services will improve the health outcomes for publicly insured children ages 0-18 through increased access to behavioral health services. 33 34 35 Systems Isssues • Maternal Infant Early Childhood Home • • • • Visitation (MIECHV) federal funding State Innovations Model (SIM) - $65M Office of Early Childhood Regional Care Collaboratives Behavioral Health Organizations 36 Questions? “I've learned that people will forget what you said, people will forget what you did, but people will never forget how you made them feel.” Maya Angelou 37 INTEGRATED BEHAVIORAL HEALTH: A FINAL PIECE OF THE MEDICAL HOME PUZZLE Christopher Stille, MD, MPH Department of Pediatrics, UC Denver SOM/Children’s Hospital Colorado, March 23, 2015 April 1, 2015 The Medical Home: definitions • US MCHB definition: A Medical Home provides care which is: • Accessible • Family-Centered • Continuous • Comprehensive • Coordinated • Compassionate • Culturally Effective • Robert Frost definition: “Home is the place where when you go there, they have to take you in.” • My definition: The medical place where the buck stops. Why focus on behavioral health services? | | We see this, many times, every day 4 year old boy for a 20 minute well child checkup Previously healthy, few minor medical problems Screen with PEDS: “behavioral problems” Lives with mother (teen) and grandmother, father incarcerated Described as "a handful", "hard to manage" and "difficult" since he started to walk. Referred for EI and behavioral therapy in past After 30 minutes of rambling history, they finally admit their primary concern: he has injured two kittens that live in the house and expresses no remorse over this practice. The family is concerned for safety (his and theirs) | | Why does integrated care matter so much? • Accessible • Family-Centered • Continuous • Comprehensive • Coordinated • Compassionate • Culturally Effective | | Current challenges • Challenges unique to behavioral health that are addressed by integrated care: Insurance “carveouts” Stigma Tradition of confidentiality Lack of continuity Interplay of physical and behavioral health • Lack of awareness of the medical home as a source of mental health care (and other services) • • • • • • • • • • • • Accessible Family-Centered Continuous Comprehensive Coordinated Compassionate Culturally Effective Typical Medical Care System | | Well-functioning Medical Home High Thinking about MH services in the context of a patientcentered medical home: Continuum of Needs Crisis and emergency services Intervene with specialty mental health services Intervene with resources of the practice Low Watchful waiting Child Mental Health: Opportunities for prevention | | But I’m just a primary care provider…? • I see LOTS of behavioral health issues • I think I am reasonably smart and caring • I can’t do diagnostic interviews • I can’t do therapy • I can prescribe meds, but only so far… | | For the primary care team: take a “Common Factors” approach • Tending to the alliance you build with families is a treatment in itself, and facilitates the impact of other treatment you provide • Clarifying concrete concerns and making it clear that you are working toward addressing those concerns is also therapeutic • A relatively small repertoire of brief advice may help many families while waiting for more definitive diagnosis and treatment From Wissow et al. Adm Policy Ment Health. Jul 2008;35(4):305-318 | | Step 2: Make use of your integrated behavioral health colleagues… • After screening and identifying concerns, and clarifying needs with patients and families, you are best prepared to inform your behavioral health colleagues so they can get a head start • Later, you can best support what they do in followup visits with the family | | What About A Virtual Team? • Consult liaison model • PCP as point of contact • Phone consult with 30 minutes • Single visit psychiatric consult within 2 weeks • Care coordination for “hard cases” • Funding secured to bring modified program statewide • Open to all (MassHealth and private payers) And It Has Caught On…. National Network of Child Psychiatry Access Programs (NNCPAP.org) NNCPAP.org Alaska Massachusetts Vermont Arkansas Michigan Virginia California Minnesota Washington Colorado Missouri Washington, D.C. Connecticut Nebraska Wisconsin Delaware New Hampshire Wyoming Florida New Jersey Georgia New York Illinois North Carolina Iowa Ohio Louisiana Oregon Maine Pennsylvania Maryland Texas CPAP vs. integrated care • CPAP more accessible especially at a distance • Few of the benefits of integrated care but much better than the “status quo” • Bridge to an integrated care model • Complements integrated care • Psychiatry available by phone if not available in person • Coordination of psychiatry and psychology essential • This is not telehealth… but telehealth is being explored as a way to improve it in some states | | And then, the State Innovation Model: There is a LOT going on in Colorado. | | Colorado SIM grant: brand new • Goal: 80% of people statewide have access to integrated behavioral health • Practice transformation • Payment reform • Measurement • Challenge: aligning adult and child interests • Pilot of a model like this ongoing in 8 practices using the CLIMB model | | The policy argument • Triple Aim (or just money): • Moving from episodic payment to whole person care • Any divides hurt this • Mental illness begins in childhood • Early treatment saves money and improves outcomes • Children are not little adults • Need different systems • Need better measures • Need different payment April 1, 2015 Presentation Title 56 Useful links AAP Mental Health Task Force http://www2.aap.org/commpeds/dochs/mentalhealth/mh1a. html National Network of Child Psychiatry Access Programs http://nncpap.org or http://web.jhu.edu/pedmentalhealth/nncpap.html Center for Mental Health Services in Pediatric Primary Care http://web.jhu.edu/pedmentalhealth/ My email: [email protected] | | Policy Change to Support Integrated Behavioral Health in Pediatrics Cody Belzley Vice President, Health & Strategic Initiatives Colorado Children’s Campaign Nonprofit, nonpartisan advocacy organization committed to realizing every chance for every child in Colorado. Grounding Data Childhood Adversity and Developmental Delays Children with Developmental Delays 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 1 or 2 Source: Barth, et al. 3 4 5 Number of Risk Factors 6 7 Grounding Data Many children who are identified as having a developmental delay never receive intervention services Initial Screenings Further Evaluation Services Source: PolicyLab, The Children’s Hospital of Philadelphia Understanding Your Policy Audience • Most elected officials are not health policy experts. • Most elected officials are juggling very full agendas. • Medicaid Directors have a huge job and limited capacity Framing The Policy Discussion • Children are Not Small Adults • Whole Family Care Essential • Focus on Prevention • Focus on Community Settings • Appropriate Evaluation Policy Opportunities Access and Delivery Models • Meet families where they are – reduce stigma • Primary care doctors offices • Child care settings & schools • Infrastructure for screening, referral & case management • Standardized tools & protocol for screening • Unified data collection • Resources for families in crisis • Statewide crisis support line Policy Opportunities Financing • Paying for preventive services and non-medical supports • Screening, referral, follow-up • Case management, transportation, food • Family care, not individual patient care • Multi-generational care from same provider • Appropriate metrics for evaluating and paying for care • Process metrics, if not outcome metrics Policy Opportunities Workforce • Addressing shortages in rural & underserved communities • Recruiting and retaining providers in underserved places • Telehealth and innovative models to serving remote communities • Professional development and training • Supporting continued training opportunities and career ladders for medical and education professionals • Team-based approaches • Scope of practice Policy Strategies • Educate and Engage Policy Makers – Start with the basics – Find personal connections to the issue • Build Champions – Invest time and resources in cultivating a few well-positioned champions • Form Partnerships & Nurture Coalitions – Look for existing networks to leverage – Build new groups only when necessary or at critical junctures Policy Strategies • Capitalize on Opportunities – Be opportunistic over the short term – Find places to build a pediatric mental health component into existing work • Create New Movements – Be intentional and proactive over the long-term – Build a multi-year agenda More Info? Cody Belzley (303) 620-4560, [email protected]
© Copyright 2026