An audit of sedation and richmond agitation
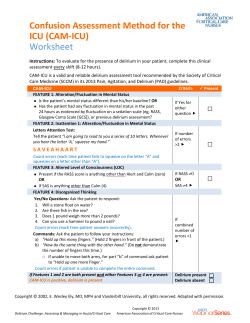
An audit of sedation and richmond agitation-sedation scale scores in intensive care Dr Christopher McGovern CT2 ICM & Anaesthetics, Dr Brian Digby Consultant ICMand Anaesthetics Royal Alexandra Hospital, Paisley Introduction 1 The RASS (Richmond Agitation-Sedation Scale) is used to assess the level of sedation of a patient using response to physical or verbal stimuli, eye opening and the presence and severity of agitation. At present we have no formal protocol or guideline to help nursing staff adjust sedative drug doses. It is becoming increasingly apparent that excessive sedation can lead to harm, making this an ideal topic for 2 quality improvement . Before intervention we wished to ascertain data on our current sedation practice. Methods We conducted a retrospective audit of ten ventilatedpatients in our mixed surgical and medical adult intensive care unit from August to December 2014.We included patients that were ventilated for seventy two hours or more and an Apache II diagnosis of seps is or respiratory infection on the national ICU database. We looked at time spent at ahigh RASS Scores (≥+1), ideal (0 or -1), or low (≤-2) as recorded by nursing staff. We also looked at the dose of sedative drugs used and documentation of sedation breaks and delirium. Results We found a large variation in RASS scores for each patient, with 0 to 54% (mean 27%) of time spent at an ideal RASS. Overall, patients spent 6% of the time at RASS ≥+1, 27% at 0 or -1 and 67% at ≤-1. The most common sedative agent used was propofol, with patients receiving between 6.3 and 37.6 mcg/kg/min (mean 15.9).Opiate drugs used included morphine (3 patients receiving 30 to 170mcg/kg/hr, mean 87.1) and alfentanil (8 patients receiving 6.2 to 53.8 mcg/kg/hour, mean 16.7). Other sedative drugs used included diazepam, midazolam, ketamine, clonidine, quetiapine and dexmedetomidine. Sedation breaks or a plan regarding adjustment of sedation were documented in 61 of 70 ward rounds, with corresponding evidence of this being carried out on the observation chart on 56 occasions.Delirium was documentedat some point in 7 of 10 of our patients, with the first documentation varying from day 2 to day 5 (mean 3.3).On 36 of 70 ward rounds, CAM-ICU or delirium was not be commented, usually due to the patient’s conscious level being insufficient to permit a full assessment. Conclusions Overall our patients spent 27% of their time ventilated at an ideal RASS of 0 or -1. We hope to use this data to implement education of nursing staff and introduce goal directed sedation guidelines in our intensive care 3 unit .With improved education and targeted sedation scores we would hope to also see an increase in time spent at an ideal RASS, reduction in delirium and more opportunity to assess patients for delirium. References 1. 2. 3. The Richmond agitation-sedation scale, validity and reliability in adult intensive care unit patients. Am J RespirCrit Care Med. 2002;166:1338-1344 Riker RR et al. Adverse events associated with sedatives, analgesics and other drugs that provide patient comfort in the intensive care unit. Pharmacotherapy. 2005;25:8S-18S DeGrado JR et al. Evaluation of a local ICU sedation guideline on goal directed administratio n of sedatives and analgesics. J Pain Res. 2011;4:127-134 Funding None Declaration of interest None declared
© Copyright 2026