Bowel preparation before colonoscopy: get it right fi rst time
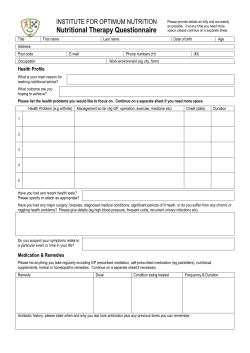
Bowel preparation before colonoscopy: get it right first time Content supplied by the authors and the publication funded by Ferring Pharmaceuticals This is an Affinity publishing service provided by BMJ Group Dec 2012 Satellite_December_OFC.indd 1 29/10/12 7:05 PM BOWEL PREPARATION BEFORE COLONOSCOPY: GET IT RIGHT FIRST TIME Ferring Pharmaceuticals was involved in the outline development and medicolegal approval of this supplement and provided financial support for its publication. The views expressed in this publication are not those of the publisher or Ferring Pharmaceuticals. Full editorial control of the article rested with the authors. Full prescribing information is available on page 8. Paper Bowel preparation before colonoscopy: get it right first time P Bhandari, A Agrawal, C Lim, S Manjunath, S Murphy, B Rembacken, J Robb 1 The BMJ Group provided copy editing and production, but had no involvement in selection or peer review of the content other than to check it for relevance and usefulness to the medical community. When citing an article from this Satellite, please use the following citation format: [Author]. [Title]. In: [Satellite title]. London: BMJ Group [year]: [page numbers]. TO FIND OUT MORE ABOUT SATELLITES, PLEASE CONTACT: Joy Clarke Senior Sales Manager BMJ Group BMA House, Tavistock Square London WC1H 9JR Tel: +44 (0) 20 7383 6055 Email: [email protected] Website: group.bmj.com Disclaimer: Satellites are published by the BMJ Publishing Group Ltd (“BMJ Group”), a wholly owned subsidiary of the British Medical Association (“BMA”). Satellites are intended for medical professionals and are provided to them without warranty, express or implied. Statements within are the responsibility of the authors and sponsors and not authors’ institutions, the BMJ Group or the BMA unless otherwise determined by law. Acceptance of advertising or sponsorship does not imply endorsement. To the fullest extent permitted by law the BMJ Group shall not be liable for any loss, injury or damage resulting from the use of Satellites or any information or material contained therein, whether based on contract, tort or otherwise. Readers are advised to verify information from Satellites they choose to rely upon. Copyright © 2012 BMJ Publishing Group Ltd. All rights reserved. No part of the publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means including electronic, mechanical, by photocopying, recording or otherwise without prior permission. J460Sat21 Dec 2012 Bowel preparation before colonoscopy Bowel preparation before colonoscopy: get it right first time Pradeep Bhandari,1 Anurag Agrawal,2 Chee Lim,3 Srikantaiah Manjunath,4 Seamus Murphy,5 Bjorn Rembacken,6 Jane Robb7 ABSTRACT Detection of anomalies during colonoscopy is contingent on an effective prior bowel cleanse. Indeed, inadequate bowel cleansing can result in missed lesions, thereby hampering the identification of colon cancer, or the need for a repeat procedure which is both costly and inconvenient. Despite its importance, the quality of bowel preparation in clinical practice is suboptimal. Understanding the rationale for the bowel cleanse and the implications of a poor preparation will help motivate patients to comply with the cleansing requirements. Furthermore, patients should undergo a thorough clinical pre-assessment before the bowel preparation is prescribed and physicians should select the bowel preparation according to the specific needs of each patient rather than follow a ‘one prep for all’ policy. Introduction The use of diagnostic and therapeutic colonic investigation procedures has increased significantly over the past decade and several advances in techniques and equipment have also been made.1 Colonoscopy now plays a central role in the investigation and surveillance of several bowel conditions, such as inflammatory bowel disease and colonic polyps, and is fundamental to national bowel cancer screening 1 Queen Alexandra Hospital, Portsmouth, UK Doncaster Royal Infirmary, Doncaster, UK 3 Good Hope Hospital, Birmingham, UK 4 Manor Hospital, Walsall, West Midlands, UK 5 Southern Trust, Northern Ireland, Ireland 6 Leeds Teaching Hospitals Trust, Leeds, UK 7 Newham University Hospital, London, UK 2 Correspondence to Professor P Bhandari, Solent Centre for Digestive Diseases, Queen Alexandra Hospital, Portsmouth PO63LY, UK; [email protected] Prescribing information can be found at the end of this Satellite programmes. Colonoscopy has the potential to prevent future colon cancers by detecting and eradicating dysplastic colonic lesions, such as adenomas. Technological advances, including magnifying endoscopes, electronic imaging and confocal imaging, can identify subtle precancerous lesions but this requires a meticulously clean mucosa devoid of faecal residue (figure 1).2 3 Effective bowel preparation may be particularly important for right-sided cancers, which can be challenging to detect, and for flat colonic lesions, where the features may be subtle and easily missed.4–7 Inadequate prior cleansing can result in a colonoscopy being aborted or pathological lesions being missed.1–3 Repeating a colonoscopy generates unnecessary additional workload and cost. Furthermore, repeating the investigation— and therefore the bowel preparation—puts patients at unnecessary risk. The uncertainty and delay in diagnosis can also be extremely stressful for patients. Despite its importance, the quality of bowel preparation prior to colonoscopy is currently suboptimal. In a recent analysis of 12 787 colonoscopies at a hospital-based endoscopy unit, bowel preparation was inadequate in 24% of cases.8 Remarkably, only 17% of patients with an inadequate preparation underwent repeat endoscopy within the following 3 years. Of the 198 adenomas identified during this study, 42% were found only on repeat colonoscopy, 27% of which were advanced. It was, however, unclear whether radiological alternatives were considered in patients where colonoscopy was suboptimal. The retrospective nature of this study associated with the possibility of selection bias would suggest that this study was susceptible to a type II error. Regardless, these data add to the growing body of evidence suggesting that poor bowel preparation is common and leads to missed pathology, and this situation clearly needs to be redressed. The objectives of this report are to raise awareness of the importance of good bowel preparation before colonoscopy, and identify strategies to improve the standard of bowel cleansing practices. Bhandari P, Agrawal A, Lim C, et al. Satellites 2012;21:1–8 1 Bowel preparation before colonoscopy Figure 1 Adequate bowel preparation is essential before colonoscopy. The preparation is excellent in the top two images, allowing optimal visualization of a polyp in the top right image (arrow). In contrast, the bottom two images show inadequate bowel preparation, with semisolid or solid debris that obscures the complete view of the mucosa in spite of extensive flushing and suction. Reproduced with permission from CCMJ. Atreja A, Nepal S, Lashner BA. Making the most of currently available bowel preparations for colonoscopy. Cleve Clin J Med 2010;77:317–326. Reprinted with permission. Copyright © 2010 Cleveland Clinic Foundation. All rights reserved. Issues and challenges in ensuring a good bowel preparation When considering how to improve the quality of bowel preparation before colonoscopy, it is prudent first to review the current clinical situation and potential reasons for inadequate bowel preparation. Understanding and adherence Patients do not always adhere fully to the bowel preparation requirements, typically due to tolerability issues with the product and/or the regimen. In general, there may be insufficient appreciation among patients, but also among physicians, of the importance of an effective bowel preparation and of the implications of a poor preparation. The information and support provided to patients may not be sufficient, and there may not be any follow-up from clinicians or nurses to check that a patient has complied with the preparation instructions. Inpatients may be particularly vulnerable to poor bowel cleansing as they are often sedentary and can have other medical conditions that may have an impact on the success of bowel preparation.1 There may also 2 Bhandari P, Agrawal A, Lim C, et al. Satellites 2012;21:1–8 be unintentional alterations in the timing of bowel preparation administration with difficult access to toilet facilities and adequate fluid intake due to the busy nature of the inpatient wards, which can affect the outcome of the bowel preparation. Pre-assessment and prescribing Clinicians want a choice of which bowel cleansing agent to use, and desire a product that provides a clean mucosa with no residue, is well tolerated and requires no monitoring or screening. Conversely, the focus of patients is on tolerability. They want a palatable product with good taste and few side effects (eg, pain, cramps, nausea). They want the regimen to have a manageable fluid intake, allowing a choice of fluids, tolerable dietary restriction, with limited impact on their activities of daily living and productivity. The available agents differ in their mechanism of action, and therefore in their administration and effect (table 1). No single agent is ideal in all clinical scenarios.9 10 However, there are notable differences among the products in tolerability and patient acceptability.12 Bowel preparation before colonoscopy Table 1 Bowel preparation products available in the UK, by active ingredient(s)9–11 Active ingredient(s) Products Mechanism of action Comments Polyethylene glycol (PEGs)/macrogols • Klean-Prep • Moviprep Non-absorbable isosmotic solutions that Diluted in large volumes of water (up pass through the bowel without absorption to 4 l), unpalatable taste; leaves leading to reduced fluid and electrolyte increased watery residue10 flux Phosphate • Fleet phospho-soda Hyperosmotic and draws large volumes of water into the colon Diluted in approx 250 ml water; use has decreased due to issues with renal insufficiency9 Sodium picosulfate with magnesium citrate • CitraFleet • Picolax* Two ingredients have synergistic effects. Picosulfate stimulates peristalsis; magnesium citrate has an osmotic effect Requires 300 ml water for dilution; leaves the least amount of watery residue9 10; patients can drink fluid of their choice Klean Prep® and Moviprep® are registered trademarks of the Norgine® group of companies. CitraFleet® and Fleet Phospho-soda® are registered trademarks of Laboratorios Casen-Fleet SLU. *Brand name Picoprep is used in some countries outside the UK. Pre-assessment of patients may not be as rigorous as it should be and bowel preparation regimens are sometimes provided to patients without the correct prescribing and dispensing policies being followed. Furthermore, despite there being a selection from which to choose, hospitals may blanket prescribe one product for all patients. There may be several barriers to overcome when trying to use a product that is not included in the hospital bowel preparation protocol. Guidance on the use of bowel preparation products In 2009, the National Patient Safety Agency (NPSA) issued an alert in response to reported safety incidents following the use of oral bowel cleansing preparations.13 The alert called for a clinical risk assessment to be made for all patients prior to bowel cleansing. It also stated that bowel preparation should be authorised at the same time as the procedure, that an explanation on the safe use of the product be provided to the patient/carer and that an authorised clinical professional should supply the medicine and written information to each patient. The NPSA alert triggered many changes in bowel preparation practices. Clinics stopped posting bowel preparations directly to patients and instigated new departmental guidelines and organisational changes to ensure patients were pre-assessed in the clinic before undergoing bowel cleansing. A greater emphasis was placed on the use of blood tests to assess estimated glomerular filtration rate and baseline sodium and potassium levels, and some local protocols restricted the choice of bowel cleansing products in an attempt to simplify the pre-assessment process. The British Society of Gastroenterology working party guidelines were subsequently developed to provide greater detail on how to assess risk in patients prior to bowel preparation.9 10 The guidelines were developed by a multidisciplinary team representing key medical societies, including the Renal Association, the British Society of Gastroenterology, the Royal College of Radiologists and the Royal College of Surgeons. Contrary to the NPSA, the consensus guidelines do not demand that all patients are pre-assessed in clinic, but agree that screening for risk factors is important. The guidelines list absolute and relative contraindications to the use of oral bowel cleansing agents and recommendations on the choice and administration of agents (table 2). They also provide a useful checklist for pre-assessing patients, which can be adapted at a local level (figure 2). Evidence to guide the paediatric use of bowel cleansing products is scant. A Cochrane review by Gordon et al found only seven randomised controlled trials in this population.12 Of these, four used sodium phosphate, which is no longer considered suitable for use in children, and two evaluated Picolax versus polyethylene glycol (PEG) or bisacodyl.14 15 In this population, Picolax was as effective as PEG but had better tolerability and patient acceptance. For example, a nasogastric Bhandari P, Agrawal A, Lim C, et al. Satellites 2012;21:1–8 3 Bowel preparation before colonoscopy Table 2 Key recommendations from the consensus guideline on the prescription and administration of bowel cleansing products9 10 Absolute contraindications to the use of bowel cleansing agents • GI obstruction or perforation, ileus or gastric retention • Severe acute inflammatory bowel disease or toxic megacolon • Reduced levels of consciousness • Hypersensitivity to any product ingredients • Inability to swallow without aspiration (nasogastric tube may be used) • Ileostomy Relative contraindications to the use of bowel cleansing agents • CKD • Haemodialysis patients • Peritoneal dialysis patients • Renal transplant patients • Congestive cardiac failure • Liver cirrhosis and/or ascites • Patients taking renin–angiotensin blockers, diuretics, NSAIDs or medications known to induce the syndrome of inappropriate ADH secretion Choice of oral bowel cleansing product • Magnesium salt preparations are relatively contraindicated in patients with stages 4 and 5 CKD. • Sodium picosulfate preparations should be used with caution in patients at risk or, or suffering from, hypovolaemia, including those patients taking high-dose diuretics, those with congestive cardiac failure and advanced cirrhosis, and those with CKD. • The use of sodium phosphate preparations is strongly discouraged in patients with CKD, pre-existing electrolyte disturbances, congestive cardiac failure, cirrhosis or with a history of hypertension. • The use of oral sodium phosphate preparations in otherwise healthy patients is currently acceptable in cases where sodium picosulfate, magnesium salts and polyethylene glycols are contraindicated or have proven ineffective or intolerable. Administration of oral bowel cleansing agents • The appropriate doses of oral bowel cleansing preparations should not be exceeded. • The period of bowel cleansing should not normally exceed 24 h. • Hypovolaemia must be corrected prior to administration of oral bowel cleansing preparations. • Hypovolaemia must be prevented during administration of oral bowel cleansing preparations. • If no recent measurement of kidney function is available (within 3 months), renal function should be measured (using an eGFR from serum creatinine concentration) for certain patients. • Regular medications: W Regular oral medications should not be taken 1 h before or after administration of bowel cleansing preparations. W Patients taking the oral contraceptive pill should take alternative precautions during the week following taking the bowel preparation. W Patients in whom reduced absorption of regular medications may prove catastrophic (eg, patients taking immunosuppressives post-transplant) may require hospital admission to allow intravenous administration. W Patients with diabetes mellitus receiving treatment with insulin will require specific advice and guidance for management of diabetes while on reduced oral intake. ADH, antidiuretic hormone; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; GI, gastrointestinal; NSAIDs, non-steroidal anti-inflammatory drugs. tube was needed in 75% of children given PEG but in only 2.5% of children given Picolax.15 Research into maximising the success of bowel preparation continues. For example, recent studies have explored differences in the success of bowel preparation before morning and afternoon procedures, and the impact of the time delay between the last dose of the bowel cleanse product and colonoscopy.16–20 4 Bhandari P, Agrawal A, Lim C, et al. Satellites 2012;21:1–8 Studies have also investigated patient treatment preference and determinants of compliance with bowel cleansing.20–22 Recommendations to improve the standard of bowel cleansing Several steps can be taken to ensure good quality bowel preparation prior to colonoscopy. Bowel preparation before colonoscopy Figure 2 Oral bowel cleansing agent prescription checklist, according to the Consensus guidelines for the safe prescription and adminstration of oral bowel clensing agents. See reference 10, appendix 5. Supplementary data published online. Improve the level of patient education It is imperative to explain to patients the importance of a good bowel preparation and to motivate them to adhere to the process. They should be made aware that following the bowel cleanse instructions precisely is fundamental to the success of the colonoscopy. Furthermore, if the bowel preparation is not carried out correctly, the investigator may miss lesions, which could have a significant negative impact on their future health, and patients are likely to have to undergo the bowel cleanse and the colonoscopy for a second time. This education should be extended to ward staff to help improve the quality of bowel cleansing for inpatients. Patients should be given comprehensive, highly illustrated, written information about the bowel cleanse.3 This should be provided at the pre-procedure clinic appointment. The educational material must describe clearly how and when to take the doses of the laxatives, how patients can determine whether the bowel preparation is complete, the foods and drinks to avoid and the fluids to take. It should also detail the need to maintain adequate hydration when taking the preparation. Finally, it is also important to emphasise that following the instructions ‘to the letter’ reduces but does not completely eliminate the possibility of an unclean bowel. Further study data are needed to define the dietary recommendations that should be given to patients. Clinical experience shows that following a low residue diet for 1–2 days prior to the colonoscopy is useful. However, controversy remains over whether patients need to restrict their intake to only clear fluids for 24 h before the procedure. Enhance pre-assessment Clinics should develop a written protocol for pre-assessment of patients undergoing bowel cleansing. The likely effect of the bowel preparation and the required fluid intake on concomitant medications and on pre-existing conditions should be evaluated carefully. In addition to screening for safety reasons, physicians should also enquire about a patient’s bowel habits. Chronic constipation has been associated with poor bowel preparation2 and is best identified before a bowel preparation is selected. In patients who have previously undergone colonoscopy, enquiring about past experiences of bowel preparations can prove useful for identifying the most appropriate product to prescribe and, if necessary, a different bowel cleaning agent Bhandari P, Agrawal A, Lim C, et al. Satellites 2012;21:1–8 5 Bowel preparation before colonoscopy may be more appropriate for the subsequent procedure. For example, a patient may report previous tolerability issues with a product that may affect the likelihood of their adherence to a repeat use of that medication. Select the most appropriate bowel cleansing product for the individual The choice of bowel cleansing product should be based on the needs of the individual patient, and should take into consideration the varying mechanisms of action of the products, precautions for use and tolerability profiles. Physicians should not simply use one product for all patients. The ideal would be to identify which products are best for each patient subtype (eg, the immobile, children, inpatients, patients with learning difficulties, patients with chronic constipation, patients with a previous failed preparation). However, there is insufficient evidence to guide this differentiation presently. Until further clinical trial data answer this question, hospitals should develop a local protocol based on the advice given in the consensus guidelines (see table 2 and figure 2). While the use of bowel preparations requires caution in patients with severe chronic kidney disease, congestive heart disease and other medical conditions, blanket prescribing of one product for all patients should not be accepted. The patients at risk are small in number and are easily identified, particularly with the improved pre-assessment process. Re-evaluate the approach in repeat colonoscopy In patients with failed colonoscopies, it is important to check normal bowel habits to identify chronic constipation. It is also useful to review any issues the patient had with the bowel cleansing product or process. In patients who have followed all of the bowel cleansing guidelines but the effect was unsatisfactory, a different approach may be needed—for example, in terms of the products used, the timing of the procedure or perhaps involving supervision of compliance in a hospital setting. Conclusions Colonoscopy is a powerful tool in the fight against colorectal cancer but relies heavily on effective prior cleansing of the bowel. The implications of poor bowel preparation practices are serious, with high miss rates of early and advanced lesions. Repeating colonoscopy generates significant additional workload and cost to healthcare services, and unnecessary stress, risk and inconvenience to the patient. 6 Bhandari P, Agrawal A, Lim C, et al. Satellites 2012;21:1–8 Bowel preparation is a demanding process. Patients have to follow a restricted diet and take a laxative that produces large volume diarrhoea, often with associated nausea and bloating. In some cases, the laxative may taste unpleasant and there may be significant amounts of fluid to consume. The process is disruptive to their normal routines and requires time off from work in addition to the inconvenience of the colonoscopy itself.3 It is not surprising that patients do not always follow the bowel preparation instructions fully. To motivate patients to comply with the directions, physicians should help patients to understand the rationale for the bowel cleansing process and the likely outcome if the preparation is poor. Prescription of bowel preparations should be individualised, rather than follow a ‘one prep for all’ policy, and should follow a thorough clinical pre-assessment. Although none of the available products shows a significantly superiority in terms of efficacy, differences exist in tolerability and patient acceptance, and these may be key to ensuring patient compliance. When considering the issues of cost, it should be remembered that the cost of repeat colonoscopy is a far greater issue than that of the bowel preparation product. In summary, much can be done to improve the quality of bowel preparation practices; to get it right first time. Indeed, achieving a high quality bowel preparation is in the best interests of both the hospital and the patient as neither wishes to repeat a colonoscopy unnecessarily. Effective oral bowel cleansing products are available, and guidance exists to direct the safe and effective use of these products. What is now needed is to improve awareness of the importance of optimal bowel cleansing to maximise the protective capabilities of colonoscopy. Key points ▪ Effective bowel cleansing prior to colonoscopy is essential. ▪ Poor cleansing can result in pathological lesions being missed, or the colonoscopy may need to be repeated. ▪ The standard of bowel cleansing practices in the UK should be improved. ▪ Recommended steps to improve bowel cleansing include: – Improving the level of education given to patients – Enhancing pre-assessment – Selecting the most appropriate bowel cleansing product for the individual patient. Bowel preparation before colonoscopy Competing interests All authors received an honorarium related to attending the advisory board meeting and development of this paper. Dr Chee Lim has declared associations with the following companies/organisations: Ferring Pharamceuticals Ltd. Full details of the relationship are held with the publisher. Funding This satellite was sponsored by Ferring Pharmaceuticals and is based on discussions at a Ferring sponsored advisory board meeting held on 1 June 2012. Writing support was provided by Lyndsey Wood, Freelance Medical Writer. All costs related to development of the Satellite were provided by Ferring Pharmaceuticals. Ferring Pharmaceuticals was involved in the outline development and medicolegal approval of this supplement and provided financial support for its publication. The views expressed in this publication are not those of the publisher or Ferring Pharmaceuticals. For further details on the discussion at this advisory board meeting, please contact Medical Information, Ferring Pharmaceuticals Ltd. Tel: 0208 5804100. Email: [email protected] 8. Lebwohl B, Kastrinos F, Glick M, et al. The impact of suboptimal preparation on adenoma miss rates and the factors associated with 9. early repeat colonoscopy. Gastrointest Endosc 2011;73:1207–14. Connor A, Tolan D, Hughes S, et al. Consensus guideline for the prescription and administration of oral bowel cleansing agents. 2009. http://www.rcr.ac.uk (accessed 28 Jun 2012). 10. Connor A, Tolan D, Hughes S, et al. Consensus guidelines for the safe prescription and administration of oral bowel cleansing agents. Gut 2012;61:1525–32. 11. British National Formulary. London: BMJ Publishing Group Ltd, RCPCH Publications Ltd and the Royal Pharmaceutical Society of Great Britain, No 63, March 2012. 12. Gordon M, Harper V, Thomas A, et al. Bowel preparation for paediatric colonoscopy: a systematic review. Abstract Presented at the British Society of Paediatric Gastroenterology Hepatology and Nutrition (BSPGHAN) Annual Meeting; Nottingham, January 2012. www.bspghan. org.uk (accessed 28 Jun 2012). 13. National Patient Safety Agency. Rapid Response Alert. Reducing risk of harm from oral bowel cleansing solutions. http://www.npsa.nhs.uk/ nrls/alerts-and-directives/rapidrr/reducing-risk-of-harm-from-oral-bowelcleansing-solutions (accessed 25 Jun 2012). 14. Gremse DA, Sacks AI, Raines S. Comparison of oral sodium phosphate to polyethylene glycol-based solution for bowel preparation for colonoscopy in children. J Pediatric Gastroenterol Nutrition 1996;23:586–90. References 1. Hendry PO, Jenkins JT, Diament RH. The impact of poor bowel preparation on colonoscopy: a prospective single centre study of 10571 colonoscopies. Colorectal Dis 2007;9:745–8. 2. Froehlich F, Wietlisbach V, Gonvers JJ, et al. Impact of colonic cleansing on quality and diagnostic yield of colonoscopy: the European Panel of Appropriateness of Gastrointestinal Endoscopy European multicenter study. Gastrointest Endosc 2005;61:378–84. 3. Spiegel BMR, Talley J, Shekelle P, et al. Development and validation of a novel patient educational booklet to enhance colonoscopy preparation. Am J Gastroenterol 2011;106:875–83. 4. Hetzel JT, Huang CS, Coukos JA, et al. Variation in the detection of serrated polyps in an average risk colorectal cancer screening cohort. Am J Gastroenterol 2010;105:2656–64. 5. Kahi CJ, Hewett DG, Norton DL, et al. Prevalence and variable detection of proximal colon serrated polyps during screening colonoscopy. Clin Gastroenterol Hepatol 2011;9:42–6. 6. Brenner H, Chang-Claude J, Seiler CM, et al. Interval cancers after negative colonoscopy: population-based case-control study. Gut 2012;61:1576–82. 7. Singh H, Nugent A, Demers AA, et al. The reduction in colorectal cancer mortality after colonoscopy varies by site of the cancer. Gastroenterology 2010;139:1128–37. 15. Turner D, Benchimol EI, Dunn H, et al. Pico-Salax versus polyethylene glycol for bowel cleanout before colonoscopy in children: a randomized controlled trial. Endoscopy 2009;41:1038–45. 16. Siddiqui AA, Yang K, Spechler SJ, et al. Duration of the interval between the completion of bowel preparation and the start of colonoscopy predicts bowel-preparation quality. Gastrointest Endoscopy 2009;69:700–6. 17. Cohen LB. Split dosing of bowel preparations for colonoscopy: an analysis of its efficacy, safety and tolerability. Gastrointest Endosc 2010;72:406–12. 18. Unger RZ, Amstutz SP, Seo DH, et al. Willingness to undergo split-dose bowel preparation for colonoscopy and compliance with split-dose instructions. Dig Dis Sci 2010;55:2030–4. 19. Seo EH, Kim TO, Park MJ, et al. Optimal preparation-to-colonoscopy interval in split-dose PEG bowel preparation determines satisfactory bowel preparation quality: an observational prospective study. Gastrointest Endoscopy 2012;75:583–90. 20. Van Dongen M. Enhancing bowel preparation for colonoscopy: an integrative review. Gastroenterol Nursing 2012;35:36–44. 21. Lebwohl B, Wang TC, Neugut AI. Socioeconomic and other predictors of colonoscopy preparation quality. Dig Dis Sci 2010;55:2014–20. 22. Rosenfeld G, Krygier D, Enns RA, et al. The impact of patient education on the quality of inpatient bowel preparation for colonoscopy. Can J Gastroenterology 2010;24:543–6. Bhandari P, Agrawal A, Lim C, et al. Satellites 2012;21:1–8 7 Bowel preparation before colonoscopy Prescribing information: Picolax Please consult the full summary of product characteristics before prescribing Name of product: Picolax. Composition: Active ingredients: sodium picosulfate and magnesium citrate. Each sachet contains 10 mg sodium picosulfate, 3.5 mg light magnesium oxide and 12 g anhydrous citric acid. Indication: To clean the bowel prior to x-ray examination, endoscopy or surgery. Dosage: To be reconstituted in water. Please consult the full summary of product characteristics for information about reconstitution and fluid intake. Adults (including the elderly): First sachet to be taken at 8 am on the day before the procedure, second sachet 6–8 h later. Children: 1–2 years: ¼ sachet morning and afternoon. 2–4 years: ½ sachet morning and afternoon. 4–9 years: 1 sachet morning, ½ sachet afternoon. 9 years and above: adult dose. Contraindications: Hypersensitivity to any of the ingredients, congestive cardiac failure, gastric retention, gastrointestinal ulceration, toxic colitis, toxic megacolon, ileus, nausea and vomiting, acute surgical abdominal conditions such as acute appendicitis and gastrointestinal obstruction or perforation. In patients with severely reduced renal function, accumulation of magnesium in plasma may occur; another preparation should be used in such cases. Special warnings and precautions: Take care in patients with recent gastrointestinal surgery, renal impairment, heart disease and inflammatory bowel disease. Use with caution in patients on drugs that might affect water and/or electrolyte balance. Picolax may modify the absorption of regularly prescribed oral medication. An inadequate oral intake of 8 Bhandari P, Agrawal A, Lim C, et al. Satellites 2012;21:1–8 water and electrolytes could create clinically significant deficiencies, particularly in less fit patients; the elderly, debilitated individuals and patients at risk of hypokalaemia may need particular attention. Prompt corrective action should be taken to restore fluid/electrolyte balance in patients with signs or symptoms of hyponatraemia. The period of bowel cleansing should not exceed 24 h because longer preparation may increase the risk of water and electrolyte imbalance. Side effects: Please consult the full summary of product characteristics for further information about side effects. Very rare: anaphylactoid reaction; hypersensitivity; hyponatraemia; epilepsy; grand mal convulsion; convulsions; confusion; headache; vomiting; diarrhoea; abdominal pain; nausea; proctalgia; rash; urticaria; pruritis; purpura; drug interaction. Nature and contents of container: Carton containing two sachets. Marketing authorisation number: 03194/0014. Marketing authorisation holder: Ferring Pharmaceuticals Ltd, Drayton Hall, Church Road, West Drayton, UB7 7PS, UK. Legal category: P. Basic NHS price: £33.90 for 10×2 sachets. Date of preparation of prescribing information: August 2012. Picolax is a registered trademark. Adverse events should be reported. Reporting forms and information can be found at http://www.mhra.gov.uk/ yellowcard. Adverse events should also be reported to Ferring Pharmaceuticals. A patient information leaflet on Picolax is available from Ferring—which can be adapted, for example, to add hospital information or local branding. BMJ Group BMA House, Tavistock Square, London WC1H 9JR. Tel. +44 (0)20 7383 6055. Fax. +44 (0)20 7383 6668 © 2012 All rights of reproduction of this material are reserved in all countries in the world. Published by the BMJ Publishing Group Ltd, typeset by Techset and printed in UK. affinity.bmj.com Satellite_December_OBC.indd 1 29/10/12 9:16 PM
© Copyright 2026