Carisoprodol: an underrecognized drug of abuse in north India
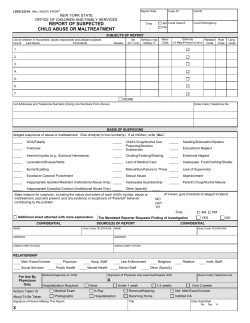
Available online at www.sciencedirect.com General Hospital Psychiatry xx (2012) xxx – xxx Carisoprodol: an underrecognized drug of abuse in north India☆,☆☆ Naresh Nebhinani, M.D., D.N.B. a,⁎, Munish Aggarwal, M.D. b , Surendra Kumar Mattoo, M.D. b , Debasish Basu, M.D., D.N.B., M.A.M.S. b a b Department of Psychiatry, Postgraduate Institute Medical Science, Rohtak, Haryana, 124001, India Department of Psychiatry, Postgraduate Institute of Medical Education & Research, Chandigarh, 160012, India Received 7 June 2012; accepted 29 July 2012 Abstract Background: There is limited literature on clinical profile of subjects abusing carisoprodol. Methods: Our series of 34 subjects shows that a typical subject was an unmarried, unemployed, urban resident from a nuclear family set up; was a substance abuser before being introduced to carisoprodol by another substance abuser; initiated the use to get a better “kick” and after regular use reported craving and withdrawal symptoms. Results: The effect of carisoprodol was dose dependent: a majority reported a feeling of general wellbeing on consuming up to three tablets; a hypomanic state with 4–10 tablets and confusion, disorientation and drowsiness with N10 tablets at a time. Conclusion: Thus being an underrecognized drug of abuse, carisoprodol is in need of wider awareness and regulatory measures to prevent its emergence as a greater menace in the future. © 2012 Elsevier Inc. All rights reserved. Keywords: Carisoprodol; Meprobamate; Abuse; Dependence 1. Introduction Carisoprodol or N-isopropylmeprobamate (brand names Carisoma and Soma) is a centrally acting muscle relaxant indicated in acute painful musculoskeletal conditions [1]. It was developed and promoted as a congener of meprobamate emphasizing better muscle relaxing properties, lower risk of overdose, and less potential for abuse [2]. Initially it was thought to be devoid of abuse potential [2]. However, later experience has established that it is associated with both abuse and impairment (i.e., increased risk of automobile accidents) [3]. It is usually prescribed for administration three times daily and at night in dosage formulations of 250 and 350 mg [4]. The onset of action is rapid (about 30 minutes) and the effects last about 2–6 hours. Metabolized in the liver via the cytochrome P450 oxidase isozyme CYP2C19, and excreted ☆ Funding: None. Conflict of interest: None to declare. ⁎ Corresponding author. Tel.: +91 8059434515; fax: +91 01262 211162. E-mail address: [email protected] (N. Nebhinani). ☆☆ 0163-8343/$ – see front matter © 2012 Elsevier Inc. All rights reserved. http://dx.doi.org/10.1016/j.genhosppsych.2012.07.011 by the kidneys, it has a half-life of about 8 hours. The abuse potential can be attributed to a considerable proportion being metabolized to meprobamate, a known drug of abuse and dependence [5]. Tachycardia, involuntary movements, hand tremor, and horizontal gaze nystagmus may be specific carisoprodol intoxication effects [6]. Serotonergic and GABAergic systems are implicated for some of the symptoms and signs of carisoprodol intoxications [7]. This may have implications for the clinical evaluation and treatment of such intoxications [8]. Recreational users of carisoprodol seek its muscle relaxing, anxiolytic, and sedating effects. Also, because of its potentiating effects on narcotics, it is often abused in conjunction with opioid drugs. Additionally, it is used as sexual performance enhancer and to prevent withdrawal among opioid addicted users [9–11]. It is believed that carisoprodol has gained reputation among drug abusers as an agent whose use begins as benign substitute for “harder” drugs and then escalates gradually for its own psychic effects. The “carry-over” phenomenon of dissemination of information from one addict to another makes the abuse of carisoprodol self-sustained. This is said to explain the 2 N. Nebhinani et al. / General Hospital Psychiatry xx (2012) xxx–xxx spreading popularity of carisoprodol and it getting established as an addictive substance by itself [12]. In India carisoprodol was not considered a problem drug till recently. In 1999, the Ministry of Social Justice and Empowerment, Government of India (MSJE, GOI) and the United Nations International Drug Control Program, Regional Office for South Asia (UNIDCP, ROSA) started a large scale national survey for the extent, pattern and magnitude of substance abuse in India. The National Household Survey (NHS), a major component of this survey reported the following nationwide current prevalence profile: Alcohol was the commonest substance (21.4%), followed by cannabis (3%) and opioids (0.7%). Drug Abuse Monitoring Survey (DAMS) component of this survey, obtained from consecutive new patients/treatment seekers contacting various treatment facilities, again revealed alcohol as the commonest substance (43.9%), followed by opioids (26%) and cannabis (11.6%). Possibly because it was not listed in any of the survey forms that were to be filled by the data collectors, carisoprodol abuse was not reported by this survey [13]. However, all over the world in the past 2 decades, concern among the medical professionals about the abuse of carisoprodol has increased steadily [9–12,14–24]. Most of this literature consists of case reports of single or few cases with abuse or dependence [9,10,12,14–20]; in the last decade, a few reviews have been added [11,21,22]. Sikdar et al. [12] mentioned dose-related variable effects, i.e., 1–3 tablets (each tablet of 350 mg), general relaxation and drowsiness; 4–10 tablets, hypomania and N10 tablets, acute organic brain syndrome-like state. Resultantly it is schedule IV controlled substance in several European countries [25,26] and since January 2012 in the US, too; but in India, carisoprodol is still freely available in the drug stores. This is mainly because it is not listed in Narcotic Drug Psychotropic Substance Act [27], as under this act, it is illegal for a person to produce/manufacture/cultivate, possess, sell, purchase, transport, store and consume the listed narcotic drug or psychotropic substance. Data about therapeutic, toxic and withdrawal effects of carisoprodol intake in Indian setting are limited. The present research aimed to study the sociodemographic and clinical profile of subjects abusing carisoprodol. 2. Methodology The study was conducted at the Drug De-addiction and Treatment Centre (DDTC) of a multispecialty tertiary-care teaching hospital providing services to a major area of north India. Most patients came by family or self-referral, and some were referred from other hospitals or other departments of our Institute. The study was approved by the institutional research ethics committee. Patients reporting carisoprodol use were recruited consecutively from the patients who attended the DDTC between May 2010 and December 2011 (20 months). The data intake were done by N.N. Diagnosis of substance dependence was made by a consultant psychiatrist as per ICD-10 [28]. A written informed consent was obtained from the patients taken up for the study. The inclusion criteria were patients who were using carisoprodol and gave informed consent for participation in the study; thus, those not using carisoprodol or not consenting were excluded from the study. An open-ended clinical interview was conducted to obtain the data on demographics and substance use, including carisoprodol. 2.1. Measures Demographic form: it was used to record sex, age, mean years of education, occupation, marital status, religion, family and locality. Clinical Form: specially developed for the study, it was used to collect information regarding ages of initiating any substance and carisoprodol, durations of carisoprodol use and dependence, onset and duration of carisoprodol action, dose and frequency of carisoprodol intake, source and reason of initiating carisoprodol, and carisoprodol related craving, tolerance, withdrawal, intoxication, harmful use etc. 2.2. Data analysis The data were analyzed using SPSS version 14.0 for Windows (Chicago, IL, USA). Descriptive data were analyzed by percentage, mean, and standard deviation. 3. Result Between May 2010 and December 2011 a total 3202 patients were registered in the DDTC and out of them 34 patients (nearly 1%) were using carisoprodol. All carisoprodol using patients were male with mean age of 27 years and formal education of 12 years. Majority were single (67%), from urban (70%), nuclear family (58%) and unemployed and Sikh by religion (55% each) (Table 1). As mentioned in Table 2, most of the patients started using any substance at age 18 years, took nearly 5 years to start carisoprodol (23.5 years) and reported to us after another 5 years (including 3.6 years of using carisoprodol in a dependent pattern). Majority were also using opioids (88%; mainly heroin and dextropropoxyphene), and nearly half were using one or another form of tobacco (55.9%); while alcohol (17.6%), cannabis (17.6%) and sedatives (8.8%) remained less common substances. Most of the patients were introduced to carisoprodol by friends or co-addicts (88.2%). Majority (70%) were using up to 10 tablets in a day (3500 mg) in two to three divided doses. Majority were taking carisoprodol to get better ‘kick’ (58%) or to combat withdrawal of mainly opioids (32%) or just out N. Nebhinani et al. / General Hospital Psychiatry xx (2012) xxx–xxx Table 1 Sociodemographic profile Variable Frequency/mean (S.D.) Age (y) Education (y) Marital status Single Married Occupational status Working Not working Religion Hindu Sikh Family type Nuclear Extended/joint Locality Urban Rural 27 (5.9) 12.38 (2.32) 23 (67.6) 11 (32.4) 15 (44.1) 19 (55.9) 15 (44.1) 19 (55.9) 20 (58.8) 14 (41.2) 24 (70.6) 10 (29.4) of curiosity (8.8%). Majority reported craving (97%) and tolerance (85%) for carisoprodol. Most of the subjects reported dose-dependent effects of carisoprodol. Consumption of one to three tablets produced a feeling of general wellbeing and feeling energetic, while consumption of 4–10 tablets produced a hypomanic state 3 characterized by overcheerfulness, psychomotor excitement, increased socialization and self-confidence. Higher one-time dose (N10 tablets) produced an acute organic brain syndrome-like state with confusion, disorientation, and partial amnesia for the events during such intake. Increased energy and pleasurable effects at all doses and escalating with dose increase were reported by 5 subjects (14.7%). Acute confusional state at relatively lower doses (seven to eight tablets) was reported by four subjects (11.8%). More than two thirds of subjects (70%) reported one or another form of withdrawal symptoms; the commonest being restlessness (35%), followed by weakness/reduced energy (23%), aches and pains (20.5%), irritability (20%), reduced sleep (17.6%), lack of pleasure (11.7%), drowsiness (5.8%), watery stools (5.8%) and reduced appetite (2.9%). Half of the subjects reported harmful use of carisoprodol (50%), though only minority (11.8%) had shifted to carisoprodol as the preferred substance. Also, less than half reported history of intoxication (41%) with the commonest manifestations being in the form of gait disturbance (35%), followed by tremors (32%), speech impairment (26%), impaired consciousness (26%), impaired vision (11.7%) and nystagmus (8.8%). Most of subjects (91%) knew other persons in the community who were using carisoprodol. 4. Discussion Table 2 Carisoprodol related details Variable Frequency/ Mean (SD) Age of initiating any substance (years) Age of initiating carisoprodol (years) Duration of carisoprodol use (years) Duration of carisoprodol dependence (years) Onset of carisoprodol action (minutes) Duration of action of carisoprodol (hours) Dose of carisoprodol (daily) Up to 5 tabs 6–10 tabs N10 tabs Frequency of carisoprodol N4 times/day 2–3 times/day Once daily Once a week Introduced by Friends/co-addicts Local chemist Reason for initiation To combat the withdrawal To get better kick Curiosity Craving-present Tolerance-present Withdrawal symptoms, present Intoxication, present Impaired control, present Harmful use, present Shift to carisoprodol as the preferred substance Knowledge of other person taking carisoprodol Carisoprodol current use, present 18.85 (5.7) 23.55 (4.9) 5.13 (5.33) [median-2.75] 3.69 (4.5) [median-1.5] 14.44 (7.09) 3.70 (2.22) 10 (29.4) 14 (41.2) 10 (29.4) 5 (14.7) 22 (64.7) 5 (14.7) 2 (5.9) 30 (88.2) 4 (11.8) 11 (32.4) 20 (58.8) 3 (8.8) 33 (97.1) 29 (85.3) 24 (70.6) 14 (41.2) 24 (70.6) 17 (50) 4 (11.8) 31 (91.2) 32 (94.1) A typical study subject was a young male, single, school educated and from an urban nuclear family. Majority were introduced to carisoprodol by friend/co-addicts. They initiated carisoprodol to get a better “high” from their preexisting opioid and tobacco use. However, later they experienced the distinct reinforcing effect of carisoprodol and gradually became also dependent on it. Carisoprodol has been reported to have tolerance and antagonist-precipitated withdrawal, suggesting it may have an addiction potential similar to benzodiazepine or barbiturate compounds [29]. Similar to earlier case reports/series [9,14,19] we also found frequent withdrawal symptoms and toxic effects with carisoprodol. While one study reported seizures in one-forth of sample [20], none of our subjects reported seizure, respiratory depression and coma. Similarly, none of our subjects reported withdrawal delirium as reported by one earlier study at discontinuing a high dose of 10.5 g [23]. Similar to an earlier study [30], majority of our patients (88%) were also abusing opioids in addition to carisoprodol. Due to lack of facilities, we did not analyze drug and metabolites in body fluids [20,31], which would have confirmed the use of carisoprodol and other substances. In comparison to the earlier study from our centre [12], the present study was a prospective one, covered a 20 month period (vs. postal contact with 15 years period patient pool) and a larger sample size (34 vs. 16), reported a higher mean age (27 vs. 24 years) and education (12.3 vs. 10 years), a 4 N. Nebhinani et al. / General Hospital Psychiatry xx (2012) xxx–xxx higher age of initiating substance abuse (18.8 vs. 17 years), a longer period for shifting from initial drug abuse to carisoprodol intake (4.5 vs. 3.5 years), and a longer period of carisoprodol intake (61 vs. 33 months). Also in comparison to our previous study [12] the most common initiator to carisoprodol intake was co-addicts (vs. local chemist), and the most common reason for initiating carisoprodol was for better “kick” (vs. to combat aches). Dose-dependent effect (general wellbeing→ hypomania→confusional state) and craving, tolerance, toxic and withdrawal (physical and psychological) effects were common to our two studies [12]. The results of the present study must be seen within its limitations. The sample size was small, and it was conducted at a single site; hence, the results can't be generalized to other primary care and community settings. The information collected by patients' self-reports raises the possibility of individual patients over-/under-reporting; however, selfreports of substance users are said to be fairly acceptable [32]. Most of the available literature on carisoprodol users is based on those who were co-using other substances. Hence, the future research on carisoprodol should investigate the specific clinical manifestations of carisoprodol as a standalone drug. It would also be important to study the genetic variability of the CYP2C19 liver enzyme and neurobiological basis of any specific carisoprodol effects. The reporting by many of our subjects of other persons in community using carisoprodol is indicative of the actual community prevalence being much higher compared to the much smaller “tip of the iceberg” seen in the clinics. This makes carisoprodol an underrecognized drug of abuse and reflects a need for increasing awareness and regulatory measures. References [1] Harveys C. Hypnotics and sedatives. In: Gilman AG, Goodman LS, Rall TW, Murad F, editors. Goodman and Gilman's the pharmacological basis of therapeutics. New York: Macmillan; 1985, pp. 364–5. [2] Berger F, Kletzkin M, Ludwig B, Margolin S. The history, chemistry, and pharmacology of carisoprodol. Ann N Y Acad Sci 1959;86:90–07. [3] Fraser HF. Evaluation of carisoprodol and phenyramidol for addictiveness. Bull Narc 1961;13:3–7. [4] Zacny JP, Paice JA, Coalson DW. Characterizing the subjective and psychomotor effects of carisoprodol in healthy volunteers. Pharmacol Biochem Behav 2011;100:138–43. [5] Olsen H, Koppang E, Alvan G, Mørland J. Carisoprodol elimination in humans. Ther Drug Monit 1995;16:337–40. [6] Bramness JG, Skurtveit S, Mørland J. Impairment due to intake of carisoprodol. Drug Alcohol Depend 2004;74:311–8. [7] Gonzalez LA, Gatch MA, Taylor CM, Bell-Horner CL, Forster MJ, Dillon GH. Carisoprodol-mediated modulation of GABAA receptors: in vitro and in vivo studies. J Pharmacol & Exp Ther 2009;329: 827–37. [8] Bramness JG, Mørland J, Sørlid HK, Rudberg N, Jacobsen D. Carisoprodol intoxications and serotonergic features. Clin Toxicol (Phila) 2005;43:39–45. [9] Reeves RR, Carter OS. Use of carisoprodol by substance abusers to modify the effects of illicit drugs. South Med J 1999;92:441. [10] Reeves RR, Carter O, Pinkofsky HB, Struve FA, Bennett DM. Carisoprodol (Soma): abuse potential and physician awareness. J Addict Dis 1999;18:51–6. [11] Reeves RR, Liberto V. Abuse of combinations of carisoprodol and tramadol. South Med J 2001;94:512–4. [12] Sikdar S, Basu D, Malhotra AK, Varma VK, Mattoo SK. Carisoprodol abuse: a report from India. Acta Psychiatr Scand 1993;88:302–3. [13] Pal HR, Kumar A. Epidemiology of substance use. In: Lal R, editor. Substance use disorder: Manual for Physicians. 1st ed. New Delhi: National Drug Dependence Centre, All India Institute of Medical Science; 2005, pp. 9–14. [14] Mose RM, Chua L. Carisoprodol dependence: a case report. Am J Drug Alcohol Abuse 1978;5:527–30. [15] Luehr JG, Meyerle KA, Larson EW. Mail-order (veterinary) drug dependence. JAMA 1990;263:657. [16] Elder NC. Abuse of skeletal muscle relaxants. Am Fam Physician 1991;44:1223–6. [17] Wyller TB, Korsmo G, Gadeholt G. Dependence on carisoprodol (Somadril)? A prospective withdrawal study among prisoners. Tidsskr Nor Laegeforen 1991;111:193–5. [18] Rust GS, Hatch R, Gums JG. Carisoprodol as a drug of abuse. Arch Fam Med 1993;2:429–32. [19] Reeves RR, Pinkofsky HB, Carter OS. Carisoprodol: a drug of continuing abuse. J Am Osteopath Assoc 1997;97:723–4. [20] Bailey DN, Briggs JR. Carisoprodol: an unrecognized drug of abuse. Am J Clin Pathol 2002;117:396–400. [21] Reeves RR, Parker JD. Somatic dysfunction during carisoprodol cessation: evidence for a carisoprodol withdrawal syndrome. J Am Osteopath Assoc 2003;103:75–80. [22] Logan BK, Case GA, Gordon AM. Carisoprodol, meprobamate, and driving impairment. J Forensic Sci 2000;45:619–23. [23] Ni K, Cary M, Zarkowski P. Carisoprodol withdrawal induced delirium: a case study. Neuropsychiatr Dis Treat 2007;3:679–82. [24] Rohatgi G, Rissmiller DJ, Gorman JM. Treatment of carisoprodol dependence: a case report. J Psychiatr Pract 2005;11:347–52. [25] Reeves RR, Burke RS. Is it time for carisoprodol to become a controlled substance at the federal level? South Med J 2008;101: 127–8. [26] Reeves RR, Burke RS. Carisoprodol: abuse potential and withdrawal syndrome. Curr Drug Abuse Rev 2010;3:33–8. [27] Government of India, Ministry of Law and Justice. Narcotic Drugs and Psychotropic Substances Act, 1985. New Delhi: Controller of Publications; 1985. [28] World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders — clinical descriptions and diagnostic guidelines. Geneva: WHO; 1992. [29] Gatch MB, Nguyen JD, Carbonaro T, Forster MJ. Carisoprodol tolerance and precipitated withdrawal. Drug Alcohol Depend 2012; 123:29–34. [30] Bramness JG, Furu K, Engeland A, Skurtveit S. Carisoprodol use and abuse in Norway. A pharmacoepidemiological study. Br J Clin Pharmacology 2007;64:210–8. [31] Backer RC, Zumwalt R, Mcfeeley P, Veasev S, Wohlenberg N. Carisoprodol concentrations from different anatomical sites: three overdose cases. J Anal Toxicol 1990;14:332–4. [32] Darke S. Self-report among injecting drug users: a review. Drug Alcohol Depend 1998;51:253–63.
© Copyright 2026