Sexual Function/Infertility Efficacy of Coenzyme Q10 on Semen Parameters, Sperm
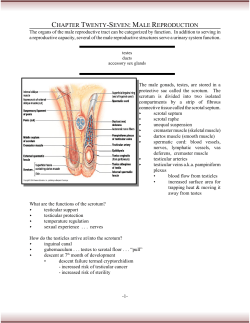
Sexual Function/Infertility Efficacy of Coenzyme Q10 on Semen Parameters, Sperm Function and Reproductive Hormones in Infertile Men Mohammad Reza Safarinejad* From the Urology and Nephrology Research Center, Shahid Beheshti University (MC), Tehran, Iran Purpose: We determined the efficacy of coenzyme Q10 supplementation on semen parameters, sperm function and reproductive hormone profiles in infertile men. Materials and Methods: A total of 212 infertile men with idiopathic oligoasthenoteratospermia were randomly assigned to receive 300 mg coenzyme Q10 (Kaneka, Osaka, Japan) orally daily (106 in group 1) or a similar placebo regimen (106 in group 2) during a 26-week period, followed by a 30-week treatment-free phase. Two semen analyses, acrosome reaction test, immunobead test for antisperm antibody, and determination of resting levels of luteinizing hormone, follicle-stimulating hormone, prolactin, testosterone and inhibin B were done in all participants. Blood and seminal plasma total coenzyme Q10 was also assessed. Results: Significant improvement in sperm density and motility was evident with coenzyme Q10 therapy (each p ⫽ 0.01). Using the Kruger classification sperm morphology evaluation revealed an increase in the percent of normal forms in the coenzyme Q10 group (p ⫽ 0.07). A positive correlation was found between treatment duration with coenzyme Q10 and sperm count (r ⫽ 0.46, p ⫽ 0.03) as well as with sperm motility (r ⫽ 0.45, p ⫽ 0.04) and sperm morphology (r ⫽ 0.34, p ⫽ 0.04). The coenzyme Q10 group had a significant decrease in serum folliclestimulating hormone and luteinizing hormone at the 26-week treatment phase (each p ⫽ 0.03). By the end of the treatment phase the mean ⫾ SD acrosome reaction had increased from 14% ⫾ 8% and 15% ⫾ 8% to 31% ⫾ 11% and 16% ⫾ 10% in the coenzyme Q10 and placebo groups, respectively (p ⫽ 0.01). Conclusions: Coenzyme Q10 supplementation resulted in a statistically significant improvement in certain semen parameters. However, further studies are needed to draw a final conclusion and evaluate the effect of coenzyme Q10 supplementation on the pregnancy rate. Abbreviations and Acronyms CoQ10 ⫽ coenzyme Q10 FSH ⫽ follicle-stimulating hormone LH ⫽ luteinizing hormone PRL ⫽ prolactin RCT ⫽ randomized, controlled trial TEAE ⫽ treatment emergent adverse event Submitted for publication November 5, 2008. Study received approval from the Urology and Nephrology Research Center human ethics committee. * Correspondence: P. O. Box 19395-1849, Tehran, Iran (telephone: 0098 21 22454499; FAX: 0098 21 22456845; e-mail: [email protected]). Key Words: testis; spermatozoa; infertility, male; coenzyme Q10; dietary supplements WORLDWIDE approximately 1 of 10 couples is infertile, which is due to male factors in approximately half.1,2 Because the etiology and pathogenesis are still not fully understood, a significant proportion of male infertility is considered idiopathic and is usually accompanied by oligoasthenoterato- spermia. Recently worldwide concerns have been raised about the impact of industrialization on public health. Indeed, during the last decades there has been evidence of decreasing sperm quality because of the use of chemicals and repeat exposure to hazardous compounds at work.3 The distress and 0022-5347/09/1821-0237/0 THE JOURNAL OF UROLOGY® Copyright © 2009 by AMERICAN UROLOGICAL ASSOCIATION Vol. 182, 237-248, July 2009 Printed in U.S.A. DOI:10.1016/j.juro.2009.02.121 www.jurology.com 237 238 COENZYME Q10 AND SEMEN PARAMETERS personal devastation experienced by couples with infertility has been documented since the beginning of recorded time in cultures throughout the world. The social and psychological consequences of involuntary childlessness in developing countries are more severe. Common scenarios include unstable marriages, divorce, polygamy and ostracism of the women.4 Modern medicine has made several advances in the diagnosis, treatment and prevention of infertility. However, most infertile men with idiopathic oligoasthenoteratospermia have remained untreated. Treatment for idiopathic male infertility is empirical. For whatever reason the possible role of these treatments on idiopathic oligoasthenoteratospermia has failed to gain wider acceptance. It is known that excess reactive oxygen species impairs sperm cell function and has a negative role in male fertility. CoQ10 or ubiquinone, an isoprenylated benzoquinone that transports electrons from complexes I and II to complex III in the mitochondrial respiratory chain, is essential for the stability of complex III.5 In addition, CoQ10 is an antioxidant, an energy promoting agent, a membrane stabilizer and a regulator of mitochondrial permeability transition pores.6 In sperm cells most CoQ10 is concentrated in the mitochondria of the mid piece and energy dependent processes in the sperm cell depend on the availability of CoQ10.7 CoQ10 in seminal fluid shows a direct correlation with semen parameters.8 CoQ10 has 2 forms, that is reduced (ubiquinol) and oxidized (ubiquinone) forms. A strong correlation among sperm count, motility and ubiquinol-10 content in seminal fluid has been reported.9 In a recent study exogenous administration of CoQ10 was effective for improving sperm kinetic features in patients with idiopathic asthenozoospermia.10 To our knowledge, while a previous RCT exists of the role of CoQ10 supplementation in semen parameters, this is the first study to look at sperm function and the hormone profile in infertile men with idiopathic oligoasthenoteratospermia. Diagnosis of a fertile female partner was based on history, physical examination, baseline body temperature, luteal phase progesterone, normal hematological and biochemical investigations, normal sexual hormones, absent sperm immobilizing antibodies in serum and a normal hysterosalpingogram. Cervical cultures for Ureaplasma, Mycoplasma, Chlamydia and bacterial vaginosis were also done as needed. Female partners with abnormal findings on hysterosalpingography underwent laparoscopy. Trial requirements were explained to participants. We explained that determining the effect of any intervention to treat male factor infertility requires at least a 6-month period, that is 2 spermatogenesis cycles. Study Inclusion Criteria Patients were included in the study after fulfilling certain criteria, including unwilling childlessness at least 24 months in duration with a female partner, no known medical condition that could account for infertility, total testicular volume 12 ml or greater on ultrasound and a normal fertile female partner according to investigations. All patients were required to have ceased all medical therapy at least 12 weeks before study initiation. Only patients seeking medical attention for the disease were included in this study. Study Exclusion Criteria Exclusion criteria were azoospermia or severe oligospermia (sperm count less than 5 million per ml); a history of epididymo-orchitis, prostatitis, genital trauma, testicular torsion, inguinal or genital surgery, urinary tract infection or previous hormonal therapy; another genital disease (cryptorchidism, current genital inflammation or varicocele); severe general or central nervous system disease and endocrinopathy; use of cytotoxic drugs, immunosuppressants, anticonvulsives, androgens or antiandrogens; and a recent history of sexually transmitted disease. Patients were also excluded from analysis if they had psychological or physiological abnormalities that would impair sexual performance or the ability to provide semen samples; drug, alcohol or substance abuse; hepatobiliary disease; significant renal insufficiency; Y chromosome microdeletions or karyotype abnormalities; occupational and environmental exposures to potential reproductive toxins; a body mass index of 30 kg/m2 or greater; participation in another investigational study; and unlikely availability for followup. Evaluations MATERIALS AND METHODS A total of 268 infertile males between 21 and 42 years old with idiopathic oligoasthenoteratospermia were enrolled in the study from February 2005 to October 2006. All men presenting for infertility treatment had had a minimum of 2 years of unprotected intercourse. Male infertility was diagnosed if 1 or more standard semen parameters were below the cutoff levels accepted by WHO (sperm density less than 20 ⫻ 106/ml, sperm motility less than 50%, normal morphology less than 30% and/or semen volume less than 2 ml) based on at least 2 semen analyses performed 3 months apart to eliminate accidental and possible adverse effects of various factors on spermatogenesis. After providing a complete medical and reproductive history exploring all aspects that may be related to fertility patients underwent physical examination, urinalysis, and serum chemical and hematological laboratory tests. All patients were asked to complete a face-to-face questionnaire, including occupational history and lifestyle. The presence of varicocele was determined by Doppler ultrasonography of the scrotum with the Valsalva maneuver. Testicular volume was measured using the formula of Behre et al11 with a volume of less than 12 ml considered small. Serum hormonal evaluation, including FSH, LH, inhibin B, PRL and testosterone, were performed in each patient. Additional safety evaluations, including measurement of serum aspartate aminotransferase, alanine ami- COENZYME Q10 AND SEMEN PARAMETERS notransferase, lactic dehydrogenase, creatine kinase, alkaline phosphatase and glucose, were also determined at baseline and at each followup point. Genetic testing included karyotype analysis and Y chromosome microdeletion analysis in patients with a sperm count of less than 10 ⫻ 106/ml. Also, blood and seminal plasma specimens in each participant were analyzed for the CoQ10 concentration. All patients underwent at least 2 baseline semen analyses. When values differed by more than 20%, a third test was done. All semen samples were obtained in a sterile wide mouth and metal-free plastic container after 3 days of recommended sexual abstinence. In addition, every participant completed a form about sperm collection information. Samples were delivered to the fertility laboratory within 1 hour after production. All procedures and interpretations used were in accordance with established 1992 WHO criteria. Morphology was established according to the Kruger parameters. Normal values were considered to be volume 2.0 ml or greater, sperm density 20 ⫻ 106/ml or greater and motility 50% or greater with forward progression. Semen volume was measured in a 15 ml conical tube. Sperm density and percent motility were assessed in a Makler counting chamber using the Hamilton-Thorn automated system (Hamilton-Thorn Research, Beverly, Massachusetts). Percent motile sperm was calculated using WHO criteria, including grade A sperm—rapidly progressive with a velocity of 25 m per second or greater at 37C and B grade sperm—slow/sluggish progressive with a velocity of 5 m per second or greater but less than 25 m per second.12 Using the Kruger strict criteria males with greater than 14% normal forms were considered normal. A total of 100 consecutive sperm were scored in each of 2 selected areas of a single slide. For strict morphology when the absolute percent of normal sperm from the 2 areas of the slide differed by more than 5%, an additional 100 sperm were scored from a third area. Samples were assessed at least twice for volume, sperm density, progressive and total motility, and the percent normal forms. All semen analyses were performed by the author (MRS) and the same laboratory technicians. The total motile sperm count was determined by the formula, (semen volume ⫻ sperm density ⫻ motility percent)/100. Strict quality control measures were enforced throughout the entire study. Quality control and proficiency criteria were set for less than 15% variation to certify the technician trained to do semen analysis in the study. In every patient the immunobead test for antisperm antibody binding was also performed. As a sperm function test, the acrosome reaction assay was done. 239 sured using immunochemiluminometric assay with an intra-assay and interassay coefficient of variation of 3.2% and 6.7%, respectively. The normal FSH range is 1.4 to 18.1 IU/l. Serum inhibin B was determined by enzymelinked immunosorbent assay using kit reagents and inhibin B standard (Oxford Bio-Innovation, Oxon, United Kingdom). Assay sensitivity was 4 pg/ml and between assay variation was 15%. Blood and seminal plasma samples were analyzed for total CoQ10 using high performance liquid chromatography with an electrochemical detector using methodology adapted from that of Tang et al.13 Between and within run coefficients of variation for total CoQ10 measurement were approximately 3.3%. The normal reference range for the total concentration of the reduced and oxidized forms of CoQ10 in the blood plasma of healthy individuals is 0.4 to 2.0 g/ml. There was strict quality control. Precision of the method was measured by coefficients of variation. The mean coefficient of variation for CoQ10 measurement in blood and seminal plasma was 2.1% for within day determinations and 2.8% for day-to-day determinations. Antibodies bound to the surface of sperm were detected with the immunobead binding test. Antisperm antibody assay was performed using specific beads that bind separately to IgG and IgA. Antisperm antibody assay was considered positive when there were more than 20% sperm bound immunobeads, according to 1992 WHO recommendations.14 Acrosome Reaction Assay Sperm from 1 sample was incubated at 37C in a 5% CO2/air environment for 6 hours with a 5 mmol/l solution of calcium ionophore A 23187. Samples were then fixed in Carnoy’s fixative and stained using the triple stain technique of Garde et al.15 Subsequently we determined the percent of sperm showing vesiculation and membrane disruption in the acrosomal region. The test was considered positive when the acrosomal reaction occurred in 30% or more of the sperm and negative when it occurred in less than 30%.16 All patients who met study inclusion and exclusion criteria provided informed consent before entering the study, which was done in accordance with International Conference on Harmonisation-Good Clinical Practice guidelines and the principles of the Declaration of Helsinki. The human ethics committee at the Urology and Nephrology Research Center approved the study protocol. No remuneration was offered. Of the 268 screened patients 212 met inclusion/exclusion criteria and consented to proceed with the study protocol. Laboratory Methods Study Design Serum testosterone and PRL were assayed using commercial radioimmunoassay kits. These commercial kits had been previously used with an interassay and intra-assay variation of less than 10%. The reference range for testosterone and PRL is 10 to 35 nmol/l and 92 to 697 pmol/l, respectively. LH was measured by immunochemiluminometric assay, in which intra-assay and interassay coefficients of variation were 3.4% and 3.8%, respectively. The normal LH range is 1.5 to 9.3 IU/l. FSH was also mea- The study consisted of a 4-week screening phase, a 26week treatment phase and a 30-week treatment-free period (fig. 1). At the beginning of the study qualifying patients were randomized to treatment with CoQ10 or placebo. Each eligible patient received a randomization number, which was determined by a computer generated schedule. Thereafter a randomization table was generated by the method of random permuted blocks. Individuals who were geographically and operationally independent of 240 COENZYME Q10 AND SEMEN PARAMETERS Figure 1. Study design the study investigator performed the study randomization. The clinician prescriber and patients were blinded to the treatment condition. To maintain and guarantee blinding CoQ10 and placebo were identical in appearance. Participant data collected during this trial were kept confidential and locked in a secure office area. Randomization codes were opened only after all patients had completed the whole study protocol. Patients were randomized to group 1—106 who received 300 mg CoQ10 once daily and group 2—106 who received matching placebo for 26 weeks. The existing literature suggests that 200 mg CoQ10 daily for 12 weeks are sufficient to restore the plasma CoQ10 concentration.17 Compliance was assessed by comparing the number of pills ingested with the number of days between dispensing visits. Followup points were weeks 4, 8, 12, 16, 20, 26, 32, 40, 46, 52 and 56. At each followup visit 2 semen samples were collected within a 1 to 2-week period. Measurement of blood and seminal plasma CoQ10, determination of serum testosterone, prolactin, inhibin B, LH and FSH, and additional safety evaluations were done at each followup visit. The study protocol also included monthly contact to deliver study medications and evaluate compliance and TEAEs. Safety and Tolerability Assessment Safety and tolerability were evaluated based on spontaneously reported adverse effects and physical examination during each patient visit. TEAEs were defined as unfavorable medical events, such as subjective symptoms, objective symptoms or unfavorable abnormal clinical data, that the volunteers commented on after receiving the prescribed material regardless of whether they appeared to be related to the test material. The Medical Dictionary for Regulatory Activities, version 5.0 was used to determine severity and the relationship to study drug assessed TEAEs. When there was an adverse event, the patient was treated as required. Statistical Analysis The investigator was responsible for accurate and complete data collection. Data are presented as the mean ⫾ SD unless otherwise stated. Analysis was performed according to per protocol analysis. The primary efficacy end point was the change in semen parameters from baseline to week 26. The null hypothesis was that CoQ10 and placebo did not differ on all primary efficacy variables. To reject the null hypothesis a 2-tailed significance of 0.05 was required. A sample size of 200 patients, that is 100 per group, was calculated to provide greater than 90% power to detect a significant treatment effect in each primary efficacy variable at ␣ ⫽ 0.05. ANCOVA was used to evaluate the primary efficacy end points. In addition, the change from baseline in efficacy measures was assessed using ANCOVA models with terms for the baseline value of the efficacy variable and the treatment group. All patients who received at least 1 dose of study medication and who had posttreatment data available were evaluated for safety. The unpaired t test was used to compare laboratory variables between the CoQ10 and placebo groups. Correlations were assessed by Spearman’s rank correlation test with p ⬍0.05 considered statistically significant. Statistical analysis was performed using SPSS® Base, version 10.0 and SigmaStat®. RESULTS Patient Characterization Table 1 lists baseline characteristics of the study patients. Those who received CoQ10 supplement and those who received placebo were similar in baseline characteristics. Compliance was greater than 90% in all patients. A total of 212 patients were recruited but only 194 (91.5%) completed the whole study, including 98 of 106 in the CoQ10 group and 96 of 106 in the placebo group (fig. 2). A total of 18 patients (8.5%) did not complete the study because of withdrawal of consent in 5 (2 in the CoQ10 group and 3 in the placebo group), loss to followup in 6 (3 per group) and missing data in 7 (3 in the CoQ10 group and 4 in the placebo group). The dropout rate was not significantly different between the 2 groups (p ⫽ 0.08). COENZYME Q10 AND SEMEN PARAMETERS Table 1. Baseline patient demographics, serum hormones and semen parameters Characteristics Age Body mass index (kg/m2) Serum hormones: Testosterone (nmol/l) LH (IU/l) FSH (IU/l) PRL (pmol/l) Inhibin B (ng/l) Plasma CoQ10: Blood (g/ml) Semen (ng/ml) % Acrosome reaction % Immunobead binding test: IgG IgA Semen parameters: Ejaculate vol (ml) Total sperm/ejaculate (⫻106) Sperm density (⫻106/ml) % Motility % Normal strict morphology Mean ⫾ SD CoQ10* 28 ⫾ 26.6 ⫾ 15.8 12.1 16.7 374 86 9 2.7 ⫾ 5.4 ⫾ 2.6 ⫾ 4.1 ⫾ 120 ⫾ 24 1.1 ⫾ 0.6 37.6 ⫾ 10.2 34 ⫾ 8 4.12 ⫾ 10.62 3.27 ⫾ 8.32 2.7 46.6 20.2 22.2 7.2 ⫾ 1.3 ⫾ 12.6 ⫾ 4.6 ⫾ 2.4 ⫾ 2.6 Mean ⫾ SD Placebo* 28 ⫾ 10 26.4 ⫾ 2.4 15.6 12.4 16.6 361 87 ⫾ 4.8 ⫾ 2.4 ⫾ 4.1 ⫾ 123 ⫾ 26 1.1 ⫾ 0.4 38.2 ⫾ 11.6 35 ⫾ 8 4.14 ⫾ 11.12 3.29 ⫾ 8.32 2.8 47.2 20.4 22.3 7.3 ⫾ 1.4 ⫾ 12.2 ⫾ 4.4 ⫾ 2.6 ⫾ 2.7 * Total of 106 patients per group (each p not significant). Testicular Volume and Semen Parameters At the end of week 56 testicular volume in the CoQ10 group did not differ significantly from that in the placebo group (23.6 ⫾ 2.8 and 22.9 ⫾ 2.8 ml, respectively, p ⫽ 0.07). Table 2 shows posttreatment and 56-week followup period semen parameters. 241 The most improved posttreatment semen analysis was used for data analysis. Statistically significant differences were found between the groups in 26-week sperm count and motility values (p ⫽ 0.01). However, a significant difference was not found in sperm morphology (p ⫽ 0.07). At the end of 56-week treatment-free phase all 3 semen parameters (count, motility and morphology) in the CoQ10 group were higher than those in the placebo group but this did not attain statistical significance (each p ⫽ 0.07). The mean percent change in semen parameters from baseline at the 8, 16 and 26-week treatment phases were different from each other in the CoQ10 group (fig. 3). A positive correlation was found between treatment duration with CoQ10 and sperm count (r ⫽ 0.46, p ⫽ 0.03) as well as mean sperm motility (r ⫽ 0.45, p ⫽ 0.04) and sperm morphology (r ⫽ 0.34, p ⫽ 0.04). At the 26-week treatment phase the increment from baseline in sperm density was 21.5% in the CoQ10 group and 1.3% in the placebo group (p ⫽ 0.01, table 3). The percent change from baseline in sperm motility was 30.7% and 2% in the CoQ10 and placebo groups, respectively (p ⫽ 0.01). Participants treated with CoQ10 and placebo had a 33.3% and 6.8% increase in strict morphology, respectively (p ⫽ 0.01). Figure 4 shows the percent change from baseline in semen parameters at various study points. By the end of the treatment phase the percent of acrosome reaction had increased from 34 ⫾ 8 and 35 ⫾ 8 to 41 ⫾ 11 and 36 ⫾ 10 in the CoQ10 and Figure 2. Participant flow diagram 242 COENZYME Q10 AND SEMEN PARAMETERS Table 2. Semen parameters, reproductive hormones and CoQ10 at various assessment points 26 Wks* Mean ⫾ SD CoQ10 Parameters Total sperm count (⫻106) Sperm density (⫻106/ml) Ejaculate vol (ml) % Sperm motility % Normal strict morphology Serum hormones: Testosterone (nmol/l) LH (IU/l) FSH (IU/l) PRL (pmol/l) Inhibin B (ng/l) Plasma CoQ10: Blood (g/ml) Seminal (ng/ml) % Acrosome reaction % Immunobead binding test: IgG IgA p Value vs Baseline 56 Wks* Mean ⫾ SD Placebo p Value vs Baseline Mean ⫾ SD CoQ10 p Value vs 26 Wks Mean ⫾ SD Placebo p Value vs 26 Wks/CoQ10 56 Wks 57.6 26.4 2.7 27.6 9.6 ⫾ 14.4 ⫾ 4.4 ⫾ 1.4 ⫾ 2.2 ⫾ 2.4 0.01 0.01 0.1 0.01 0.07 47.8 20.8 2.7 23.1 7.8 ⫾ 11.2 ⫾ 4.3 ⫾ 1.7 ⫾ 2.1 ⫾ 2.1 0.1 0.1 0.1 0.08 0.1 51.7 22.8 2.7 24.2 8.2 ⫾ 12.4 ⫾ 3.8 ⫾ 1.3 ⫾ 2.1 ⫾ 2.1 0.07 0.07 0.1 0.07 0.08 47.8 21.2 2.8 22.8 7.4 ⫾ 11.6 ⫾ 3.8 ⫾ 1.2 ⫾ 2.2 ⫾ 1.8 0.1/0.07 0.1/0.08 0.1/0.1 0.1/0.07 0.1/0.07 18.6 8.8 10.7 368 105 ⫾ 5.6 ⫾ 2.6 ⫾ 4.1 ⫾ 118 ⫾ 28 0.07 0.03 0.03 0.1 0.03 15.8 12.6 16.8 365 88 ⫾ 4.6 ⫾ 2.4 ⫾ 4.2 ⫾ 121 ⫾ 25 0.1 0.1 0.1 0.1 0.1 16.4 10.1 14.4 376 94 ⫾ 5.1 ⫾ 2.3 ⫾ 3.8 ⫾ 120 ⫾ 22 0.08 0.08 0.08 0.1 0.08 15.7 12.4 16.6 362 87 ⫾ 4.4 ⫾ 2.2 ⫾ 4.4 ⫾ 118 ⫾ 20 0.1/0.08 0.1/0.08 0.1/0.08 0.1/0.08 0.1/0.08 2.04 ⫾ 0.8 88.4 ⫾ 12.6 41 ⫾ 11 0.01 0.01 0.01 1.1 ⫾ 0.5 38.4 ⫾ 11.2 36 ⫾ 10 0.1 0.1 0.1 1.1 ⫾ 0.4 37.8 ⫾ 11.2 38 ⫾ 11 0.01 0.01 0.01 1.1 ⫾ 0.4 37.9 ⫾ 11.6 35 ⫾ 12 0.1/0.1 0.1/0.1 0.1/0.08 4.18 ⫾ 10.58 3.24 ⫾ 8.72 0.1 0.1 4.13 ⫾ 12.1 3.44 ⫾ 8.76 0.1 0.001 4.14 ⫾ 11.12 3.41 ⫾ 9.12 0.1 0.1 4.11 ⫾ 10.44 3.48 ⫾ 8.76 0.1/0.1 0.1/0.1 * Total of 106 patients per group. placebo groups, respectively (p ⫽ 0.01). The acrosome reaction had a significant positive correlation with sperm density (r ⫽ 0.48, p ⫽ 0.03), mean sperm motility (r ⫽ 0.49, p ⫽ 0.03) and sperm morphology (r ⫽ 0.42, p ⫽ 0.03, table 3). Serum Hormones Mean serum LH, FSH, PRL, inhibin B and testosterone were not significantly different between the groups at baseline (each p ⫽ 0.1, table 1). When comparing the CoQ10 supplemented group with the placebo group, the CoQ10 group had a significant decrease in serum FSH and LH at the 26-week treatment phase (each p ⫽ 0.03, table 2). At the end of the 56-week treatment-free phase serum FSH and LH in the CoQ10 group were lower than those in the placebo group but the difference was not statistically significant (p ⫽ 0.08). At baseline mean serum inhibin B was at the lower limit of normal reference range. By the end of the 26-week treatment period serum inhibin B had significantly increased in the CoQ10 group compared with that in the placebo group (p ⫽ 0.03, table 2). A positive correlation existed between serum inhibin B and sperm density (r ⫽ 0.42, p ⫽ 0.02). The mean change from baseline in serum LH, FSH, testosterone and inhibin B was different in the group treated with CoQ10 at 4, 8, 12, 16 and 26 weeks of treatment (fig. 5). Changes in serum testosterone and inhibin B were 17.7% and 22.1% in the CoQ10 group, and 1.3% and 1.1% in the placebo group (p ⫽ 0.02 and 0.01, respectively). The most striking changes in serum hormones occurred in FSH. Serum FSH decreased by 35.9% in the CoQ10 group and it increased by 1.2% in the placebo group (p ⫽ 0.01, table 3). Table 3 and figure 6 show detailed explanations about changes from baseline in serum hormones. Semen volume and binding of antisperm antibody of the IgG and IgA types were not influenced by either treatment (table 2). Blood and Semen CoQ10 Oral supplementation with 300 mg CoQ10 daily increased blood and seminal plasma CoQ10. At the end of the 26-week treatment period the percent increase in blood plasma and seminal plasma CoQ10 was 85.5% and 135.1% in the CoQ10 group, and 0% and 0.5% in the placebo group, respectively (each p ⫽ 0.001, table 3). Changes in blood plasma CoQ10 showed significant positive correlations with the changes in seminal plasma CoQ10 (r ⫽ 0.62, p ⫽ 0.02). Total blood plasma CoQ10 reached a maximum in 2 weeks, after which it remained stable for 4 weeks. By 2 weeks after withdrawal plasma CoQ10 had decreased to the baseline level. The pattern of the change in seminal plasma CoQ10 was somewhat different than the pattern observed in blood plasma. Seminal plasma CoQ10 reached a plateau by week 8. By the end of followup at week 56 the blood and seminal plasma CoQ10 concentrations were not significantly different from baseline. There were strong and significant correlations between seminal plasma CoQ10 and sperm count (r ⫽ 0.77, p ⫽ 0.01), sperm motility (r ⫽ 0.76, p ⫽ 0.01) and sperm morphology (r ⫽ 0.54, p ⫽ 0.02). COENZYME Q10 AND SEMEN PARAMETERS 243 Figure 3. Mean sperm density, total sperm count, sperm with normal morphology and sperm motility during treatment and followup. Single asterisk indicates number of patients analyzed in CoQ10 group. Double asterisks indicate number of patients analyzed in placebo group. Safety and Adverse Events No side effects were observed due to the oral administration of CoQ10 in any participants. CoQ10 re- sulted in no clinically significant changes in vital signs, urinalyses, serum chemical values or hematological values. There were no serious adverse Table 3. Change in measured variables from baseline during study period 26-Wk Treatment Parameters Total sperm count Sperm density Ejaculate vol Sperm motility Strict morphology Serum hormones: Testosterone LH FSH PRL Inhibin B Plasma CoQ10: Blood Seminal Acrosome reaction Immunobead binding test: IgG IgA % CoQ10 56-Wk Recovery % Placebo p Value % CoQ10 % Placebo p Value 21.5 30.7 0 24.3 33.3 1.3 2 ⫺3.6 3.6 6.8 0.01 0.01 0.08 0.01 0.01 10.9 12.9 0 9 13.9 1.3 2.9 0 2.2 1.4 0.03 0.03 — 0.04 0.03 17.7 ⫺27.3 ⫺35.9 ⫺1.6 22.1 1.3 1.6 1.2 1.1 1.1 0.02 0.01 0.01 0.1 0.01 3.8 ⫺16.5 ⫺13.8 0.5 9.3 0.6 0 0 0.3 0 0.07 0.02 0.03 0.1 0.03 85.5 135.1 20.6 0 0.5 0.3 0.001 0.001 0.01 0 0.5 11.8 0 ⫺0.8 0 — 0.1 0.03 1.5 ⫺0.9 0.2 4.6 0.1 0.07 0.5 4.3 ⫺0.7 5.8 0.1 0.1 244 COENZYME Q10 AND SEMEN PARAMETERS Figure 4. Percent change from baseline in total sperm count, and sperm density, motility and morphology during whole study period events and no study withdrawals due to adverse events. DISCUSSION We examined the efficacy of CoQ10 for improving semen parameters, sperm function and reproductive hormone profiles by performing a RCT. Controlled studies are mandatory for assessing any clinical intervention for idiopathic oligoasthenoteratospermia. This study demonstrated that daily administration of 300 mg CoQ10 for 26 weeks or approximately 2 human spermatogenesis cycles significantly improved semen parameters and sperm function testing, and altered reproductive hormones. However, the beneficial effects in terms of semen parameters were modest. Mean strict Kruger morphology values did not differ significantly from values in the placebo group (9.6 ⫾ 2.4 and 9.6 ⫾ 2.4, respectively, p ⫽ 0.07). Although a statistically significant improvement in density or motility was achieved in the CoQ10 group, there was no difference in the pregnancy rate during the study period between the 2 groups. The reasons for this apparent discrepancy lie in the posttreatment semen parameters. Sperm motility was 27.6 ⫾ 2.2 per ml in the CoQ10 group and 23.1 ⫾ 2.1 per ml in the placebo group, which may not be clinically relevant. The 2 values are far from the recommended normal value for sperm motility (motility 50% or greater with forward progression). In addition, at the 26-week treatment phase mean total sperm count in the CoQ10 group was less than 60 million. However, semen analysis is far from a perfect assessment of male reproductive potential and the fact that some infertile men had semen analyses exceeding WHO criteria COENZYME Q10 AND SEMEN PARAMETERS 245 Figure 5. Mean serum LH, FSH, testosterone and inhibin B during treatment and followup. Single asterisk indicates number of patients analyzed in CoQ10 group. Double asterisks indicate number of patients analyzed in placebo group. added to the difficulty. To our knowledge whether a longer treatment trial or higher doses might have resulted in better findings has yet to be identified. There are a few noteworthy implications of our study results. 1) CoQ10 supplementation may have a potential clinical application in infertile men. 2) Patients with idiopathic oligoasthenospermia may consume a diet that is inadequate in CoQ10. 3) The usefulness of CoQ10 supplementation for achieving pregnancy in infertile couples should be evaluated in further prospective studies. CoQ10 therapy was able to influence semen parameters, probably by modifying the balance between oxygen radicals and antioxidant defense. To establish this point it is important to assess oxidative stress and antioxidant levels in seminal plasma at baseline and after therapy. We did not do this, which is one of the study limitations. Indexes of healthier seminiferous tubules are higher inhibin B and lower FSH.18 Higher serum FSH implies poorer spermatogenesis. Inhibin B levels correlate with testis size and reflect Sertoli’s cell function. There is negative feedback between FSH and inhibin B. Improvement in seminiferous tubules function is associated with improvement in seminiferous tubules function indexes. After CoQ10 supplementation serum FSH decreased by 35.9% and serum inhibin B increased by 22.1% from baseline. These values were statistically significant compared with those in the placebo group. This denotes that CoQ10 supplementation may have a direct effect on the seminiferous tubule level. In addition, we observed modest changes in serum testosterone in the CoQ10 group. At the end of 26 weeks of treatment with CoQ10 supplementation serum testosterone increased 17.7% from baseline. However, mean ⫾ SD serum testosterone at the end of 26-week treatment phase did not differ significantly from that in the placebo group. In the current study sperm count and motility were also improved after CoQ10 supplementation. These results support the hypothesis that systemic CoQ10 supplementation causes more efficacious spermatogenesis by the seminiferous tubules, and the recovery of sperm count and morphology. The decrease in gonadotropins was associated with improved spermatogenesis and increased serum inhibin B. The plasma CoQ10 concentration is altered in pituitary diseases, such as acromegaly or secondary hypothyroidism.19 In addition, 246 COENZYME Q10 AND SEMEN PARAMETERS Figure 6. Percent changes from baseline in serum testosterone, LH, FSH and inhibin B during whole study period cholesterol and ubiquinone have a common biosynthetic pathway.19 Therefore, the role of CoQ10 in the pituitary-gonadal axis requires further clarification. Mancini et al assayed the CoQ10 content in seminal plasma and seminal fluid in 77 patients with normal or pathological findings on standard semen analysis.20 They noted a significant correlation among sperm count, motility and the CoQ10 content in seminal fluid. Seminal plasma CoQ10 was low in patients with asthenospermia. In addition, sperm cells, which are characterized by low motility and abnormal morphology, have low levels of CoQ10.21 Therefore, infertile men with idiopathic oligoasthenoteratospermia might benefit from CoQ10 supplementation. In a RCT Balercia et al evaluated the effectiveness of 200 mg CoQ10 per day for improving semen quality in 60 men with idiopathic infertility.10 They found a weak linear relationship between seminal plasma or intracellu- lar CoQ10 and semen kinetic parameters. The study was flawed due to small sample size (30 men per group). Moreover, many studies of semen analysis in men from various geographic regions have revealed surprisingly different results at different locations. This may be due to environmental factors, such as the type of food consumed and where it is grown. These effects may adversely affect the male endocrine and reproduction systems. However, while published data are imperfect, they suggest that certain medications may be beneficial to male reproductive capacity, including trace elements. In a double-blind, placebo controlled study 200 g selenium orally daily for 26 weeks significantly improved all semen parameters.22 Recently Kumar et al searched PubMed®/MEDLINE® using the key words male infertility, treatment, therapy, oligospermia, asthenospermia, teratospermia androgens, testosterone, gonadotropins, FSH, LH, GnRH, LH-RH, mesterolone, clomifene, testolactone, tamoxifen, anastrozole, aro- COENZYME Q10 AND SEMEN PARAMETERS matase inhibitor, antiestrogens, antioxidant, lycopene, ␣ tocopherol, vitamin E, glutathione (L-␥-glutamyl-Lcysteinylglycine), carnitine, CoQ10 and coenzyme Q10 in various combinations.23 They concluded that drug therapy for idiopathic male infertility is at best empirical. There is no clear benefit of using any medication in these patients. Therefore, the approved and effective treatment for idiopathic oligoasthenoteratospermia has yet to be identified. In the current study sperm density in patients had a narrow range of 10 to 30 ⫻ 106/ml. The reason is that 86.8% of the participants had oligospermia, defined as sperm density less than 20 ⫻ 106/ml. In addition, we excluded patients with azoospermia or severe oligospermia, defined as a sperm count of less than 5 million per ml. Sperm morphology was assessed using Kruger’s strict criteria. The Kruger evaluation was done because of the possibility of performing in vitro fertilization in any of these couples in the future after CoQ10 treatment. The association between sperm morphology as recorded by strict criteria and the in vitro fertilization rates has been well documented.24 Our study had the benefits of a placebo controlled, randomized study design, patients with idiopathic oligoasthenoteratospermia, sperm function test data and serum reproductive hormone profile analysis. It 247 also had another important limitation. It is not clear whether improved semen parameters translate directly to improved fertility. We did not address this issue. None of the patients reported pregnancy during the study period. A more effective outcome parameter would probably be the pregnancy rate since that is the ultimate end point of therapy. The etiology of male factor infertility is frequently multifactorial. Semen has a unique biochemical composition and its biological function has never been fully explained. CONCLUSIONS This study indicates that oral supplementation with CoQ10 significantly improves semen parameters compared with that of placebo. Although this observation may not be clinically relevant, we propose that because of its antioxidant effects and safety profile, CoQ10 should be considered a good candidate for treatment in infertile men with idiopathic oligoasthenoteratospermia. A longer term study with different treatment regimens is needed to draw a final conclusion. ACKNOWLEDGMENTS Shiva Safarinejad assisted with the manuscript. REFERENCES 1. De Kretser DM and Baker HW: Infertility in men: recent advances and continuing controversies. J Clin Endocrinol Metab 1999; 84: 3443. 2. Safarinejad MR: Infertility among couples in a population-based study in Iran: prevalence and associated risk factors. Int J Androl 2008; 31: 303. 3. Carlsen E, Giwercman A, Keiding N and Skakkebaek NE: Evidence for decreasing quality of semen during the past 50 years. BMJ 1992; 305: 609. 4. Vayena E, Rowe PJ and Peterson HB: Assisted reproductive technology in developing countries: why should we care? Fertil Steril 2002; 78: 13. 5. Santos-Ocaña C, Do TQ, Padilla S, Navas P and Clarke CF: Uptake of exogenous coenzyme Q and transport to mitochondria is required for bc 1 complex stability in yeast coQ mutants. J Biol Chem 2002; 277: 10973. 6. Turunen M, Olsson J and Dallner G: Metabolism and function of coenzyme Q. Biochim Biophys Acta 2004; 1660: 171. 7. Lewin A and Lavon H: The effect of coenzyme Q10 on sperm motility and function. Mol Aspects Med, suppl., 1997; 18: S213. 8. Mancini A, Milardi D, Conte G, Festa R, De Marinis L and Littarru GP: Seminal antioxidants in humans: preoperative and postoperative evalua- tion of coenzyme Q10 in varicocele patients. Hormon Metab Res 2005; 37: 428. coenzyme Q10 in human plasma. Clin Chem 2001; 47: 256. 9. Alleva R, Scararmucci A, Mantero F, Bompadre S, Leoni L and Littarru GP: The protective role of ubiquinol-10 against formation of lipid hydroperoxides in human seminal fluid. Mol Aspects Med, suppl., 1997; 18: S221. 14. WHO Laboratory Manual for the Examination of Human Semen and Sperm-Cervical Mucus Interaction, 3rd ed. London: Press Syndicate of University of Cambridge 1992; pp 8 –50. 10. Balercia G, Buldreghini E, Vignini A, Tiano L, Paggi F, Amoroso S et al: Coenzyme Q(10) treatment in infertile men with idiopathic asthenozoospermia: a placebo-controlled, double-blind randomized trial. Fertil Steril 2008; Epub ahead of print. 11. Behre HM, Nashan D and NieSchlag E: Objective measurement of testicular volume by ultrasonography: evaluation of technique and comparison with orchidometer estimate. Int J Androl 1989; 12: 395. 12. Gyllenborg J, Skakkebaek NE, Nielsen NC, Keiding N and Giwercman A: Secular and seasonal changes in semen quality among young Danish men: a statistical analysis of semen samples from 1927 donor candidates during 1977–1995. Int J Androl 1999; 22: 28. 13. Tang PH, Miles MV, DeGrauw A, Hershey A and Pesce A: HPLC analysis of reduced and oxidised 15. Garde JJ, Ortiz N, Garcia A and Gallego L: Use of triple-stain technique to detect viability and acrosome reaction in deer spermatozoa. Arch Androl 1997; 39: 1. 16. Aitken RJ and Clarkson JS: Cellular basis of defective sperm function and its association with the genesis of reactive oxygen species by human spermatozoa. J Reprod Fertil 1987; 81: 459. 17. Watts GF, Playford DA, Croft KD, Ward NC, Mori TA and Burke V: Coenzyme Q(10) improves endothelial dysfunction of the brachial artery in type II diabetes mellitus. Diabetologia 2002; 45: 420. 18. Coughlin MT, Bellinger MF and Lee PA: Age at unilateral orchiopexy: effect on hormone levels and sperm count in adulthood. J Urol 1999; 162: 986. 19. Mancini A, Bianchi A, Fusco A, Sacco E, Leone E, Tilaro L et al: Coenzyme Q10 evaluation in pituitary-adrenal axis disease: preliminary data. Biofactors 2005; 25: 197. 248 COENZYME Q10 AND SEMEN PARAMETERS 20. Mancini A, De Marinis L, Oradei A, Hallgass ME, Conte G, Pozza D et al: Coenzyme Q10 concentrations in normal and pathological human seminal fluid. J Androl 1994; 15: 591. 21. Balercia G, Arnaldi G, Fazioli F, Serresi M, Alleva R, Mancini A et al: Coenzyme Q10 levels in idio- pathic and varicocele-associated asthenozoospermia. Andrologia 2002; 34: 107. 22. Safarinejad MR and Safarinejad S: Efficacy of selenium and/or N-acetyl-cysteine for improving semen parameters in infertile men: a doubleblind, placebo controlled, randomized study. J Urol 2009; 181: 741. 23. Kumar R, Gautam G and Gupta NP: Drug therapy for idiopathic male infertility: rationale versus evidence. J Urol 2006; 176: 1307. 24. Esterhuizen AD, Franken DR, Lourens JG, Van Zyl C, Müller II and Van Rooyen LH: Chromatin packaging as an indicator of human sperm dysfunction. J Assist Reprod Genet 2000; 17: 508.
© Copyright 2026