Document 11553
4/1/14 Denise L. Wunderler, DO, FAOASM Primary Care Sports Medicine Physician Department of Orthopedic Surgery Fort Knox, Kentucky AOASM Annual Conference 2014, Tampa ¨ ¨ ¨ ¨ ¨ ¨ ¨ Gain an understanding of how to successfully prepare for an international sports medicine trip Review vaccines and traveler’s diarrhea Discuss performance considerations regarding altitude and jet lag Can be challenging Usually great preparation leads to a smooth, successful trip But you can’t anticipate everything Goal: be as prepared as you can be 1 4/1/14 ¨ With whom are you traveling? ¡ ¡ Athletes, coaches, other staff, family members Make contact with them early to open the lines of communication for questions or concerns ú Allows better planning for everyone ú Be aware of any allergies or known medical problems ú standard vaccines should be UTD, including tetanus ú Gives them time to obtain needed vaccines for a specific country ú obtain complete list of ALL meds (Rx, OTC, herbs, “natural remedies”, vitamins, supplements; daily/PRN) ú determine if an athlete is taking a banned substance ú need for a therapeutic use exemption (TUE)? For athletes with a documented medical condition who need a prohibited substance/prohibited method At least 30 days before the competition ú Old/new injuries, any taping that is needed ¨ ¨ I made a chart with the Team Delegation’s names, meds, allergies, other Where are you going? ¡ Local vs. international ú http://www.cdc.gov/travel (specific country) ú what is allowed in the country/through customs Some prescription meds are illegal in other countries- need to check with the embassy or consulate for that country; must have a letter from your doctor stating the med and that it was prescribed for you I would not recommend carrying any narcotics Letter for epi pens in my luggage 2 4/1/14 ú what can be brought on the plane in carry-on bag ú small stock of Ibuprofen, Acetaminophen, Tums, Pepto- Bismol, Immodium, throat lozenges ú tablets in original containers or marked clearly with the name and dose ú Depending on the destination, specific vaccinations will be needed- check CDC website ¡ ¡ Packed supplies will be different if it is international How much are you going to bring ú the more you bring, the more you carry ú If you need an item, how difficult will it be to obtain i.e. Moist heat packs for shoulder/back- it took our Peruvian delegate 2 days to locate them for us in Lima i.e. Meds- if purchased overseas, they may not be made according to US standards, may be ineffective, contain contaminants, or may be in unsafe drug combinations ¡ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ Encourage them to bring healthy snacks from home cdc.gov who.int Routine vaccinations need to be up-to-date (MMR, DPT, polio, etc) Hepatitis A Typhoid Fever Hepatitis B Yellow Fever Malaria Rabies 3 4/1/14 ¨ Transmission: viral contaminated food/ water, illegal drugs, intimate relations nausea, anorexia, fever, malaise, abdominal pain, dark urine, clay-colored stools, jaundice, joint pain Tx: supportive ¨ Hepatitis A vaccine (inactivated/killed) or IG ¨ ¨ ¡ ¡ ¡ ¨ ¨ ¨ ¨ begin 2-4 weeks (ideally) prior to travel; there is some protection no matter when it is given for immediate, temporary protection, immune globulin can be given for long-term protection, 2 vaccine doses are required 6 months apart Transmission: Contaminated food/water insidious onset, F/C, constipation, abdominal pain, HA, rose-colored macular rash on abdomen and chest (“rose spots”), malaise, myalgia Salmonella typhi bacteria Tx: fluoroquinolone (cipro); Injectable thirdgeneration cephalosporins; Azithromycin 4 4/1/14 ¨ Inactivated (killed)- IM (Typhim Vi) ¡ ¡ ¨ one shot at least 2 weeks before travel booster q 2 yrs if at risk live, attenuated (weakened)- PO (Vivotif) ¡ ¡ ¡ 4 doses- one capsule QOD for a week (day 1, day 3, day 5, day 7) final dose should be given at least 1 week before travel; given 1 hr before a meal with lukewarm/cold beverage booster q 5 yrs if at risk ¨ Transmission: blood/ body fluid, IV drug use, intimate relations Fever, fatigue, loss of appetite, N/V, abdominal pain, dark urine, claycolored stools, joint pain, jaundice Tx: supportive if acute ¨ Vaccine (Hep B surface Ag): ¨ ¨ ¡ ¡ 3 doses: time 0, 1 month, 6 months May last at least 20 years 5 4/1/14 ¨ ¨ ¨ ¨ Transmission: Flavivirus infected Mosquito Most have no illness or mild illness- sudden onset of F/C, severe HA, back pain, general body aches, N/V, fatigue, weakness Tx: supportive, close observation Live, attenuated virus vaccine ¡ ¡ ¨ ¨ ¨ single dose protects against disease for 10 years or more booster dose q 10 years if continued risk Transmission: Plasmodium (parasite) infected mosquito high fevers, chills, diaphoresis, HA, N/V, malaise/myalgias Tx: depends on disease severity, species of parasite, part of the world in which the infection was acquired 6 4/1/14 ¨ ¨ NO vaccine available Doxycycline 100 mg PO daily for prevention ¡ ¡ ¡ ¨ ¨ ¨ ¨ ¨ ¨ Begin 1-2 days prior to exposure Discontinue 4 weeks after exposure Side effects include diarrhea, nausea, dyspepsia, HA, photosensitivity insect repellent with 30-50% DEET long pants/sleeves and hats to prevent insect bites remain indoors in a screened or air-conditioned area during peak biting period (dusk and dawn) Transmission: saliva from the bite of an infected animal (or brain/nervous system tissue) Dogs in developing countries General weakness, fever, HA, itching at the bite site, eventually cerebral dysfunction, delirium ¡ Almost always fatal once symptoms begin ¨ Tetanus shot (if not received in last 10 years) Tx: supportive ¨ Do not touch/feed animals (including dogs, cats) ¨ Pre-exposure: ¨ Post-exposure prophylaxis if never immunized: ¨ ¡ ¡ pets that look healthy may have rabies, other diseases Inactivated/killed viral vaccine- IM wound cleansing (greatly reduces likelihood of rabies) with soap/water/virucidal agent (ie. povidine-iodine) ¡ vaccine on days 0, 3, 7, 14 + HRIG (human rabies immune globulin) local infusion at wound site + additional amount IM at site distant from the vaccine ¡ ¨ Post-exposure prophylaxis if previously immunized: ¡ wound cleansing + vaccine on days 0 and 3 7 4/1/14 ¨ ¨ Are you the only medical staff for your team? Physician duties ¡ ¡ BE PROACTIVE and stay in the loop of communication with the team Do your best to keep everyone healthy ú if they had a hint of a symptom (GI, blister, URI, etc), they knew to tell me immediately ¨ ATC duties ¡ ¡ ¨ ¨ This lists prohibited substances/methods that can enhance athletic performance updated annually ¡ ¨ ¨ ¨ ¨ ¨ ¨ ¨ separated by substances that are prohibited at all times, in competition, and in particular sports) Full list at http://list.wada-ama.org/ ALL TIMES: Anabolic steroids, growth factors, blood products, gene doping are prohibited Danazol- anabolic steroid for endometriosis, fibrocystic breast disease, hereditary angioedema All beta-2 agonists ¡ ¨ Taping, ice, everything else I refreshed basic taping with an ATC before traveling except inhaled salbutamol (albuterol) max 1600 mcg over 24 hrs, inhaled formoterol max 54 mcg over 24 hrs, or inhaled salmeterol (long-acting beta agonist) when used in accordance with manufacturer’s regimen Clomiphene- for ovulation induction Insulins Masking agents: acetazolamide (Diamox), probenecid (for gout) 8 4/1/14 ¨ ¨ IN COMPETITION: Stimulants ¡ ¡ methylphenidate (Concerta, Ritalin) Pseudoephedrine (PSE) (Sudafed)- for nasal congestion, when [urine] is >150mcg/mL ú WADA advises athletes to stop taking PSE 24 hours before the in-competition period ¡ ¨ ¨ ¨ ¨ ¨ Narcotics- Fentanyl, hydromorphone (Dilaudid), oxycodone (in Percocet, OxyContin) Marijuana All glucocorticosteroids (prednisone)- PO, IV, IM, PR IN COMPETITION IN CERTAIN SPORTS: Alcohol ([blood alcohol] of 0.10g/L) ¡ ¨ ¨ ¨ ¡ ¨ archery and shooting (both also prohibited out-ofcompetition), automobile, billiards, darts, golf, skiing/ snowboarding- ski jumping, freestyle aerials/halfpipe and snowboard halfpipe/big air MONITORING PROGRAM: substances not on prohibited list, but which WADA wishes to monitor in order to detect patterns of misuse in sport In competition only ¡ ¨ air sports (aeronautic), archery, automobile, karate, motorcycling, powerboating Beta-blockers ¡ ¨ (NOT PROHIBITED: caffeine, nicotine, phenylephrine, synephrine) Stimulants: caffeine, nicotine, phenylephrine, pseudoephedrine <150mcg/mL, synephrine Narcotics: Hydrocodone (in Vicodin), tramadol NOTE: Intramuscular PRP was removed from the prohibited list *To inquire about a certain ingredient by sport, look at http://www.globaldro.com/ 9 4/1/14 ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ Meet the Head Physician of the event (which could be you), other local event medical staff Protocol to contact emergency staff AED location Ambulance access to facility Training room facilities local hospital locations Bring contact information of people in case of problems (trusted physicians, NGB staff) Be familiar with the World Anti-Doping Code ¡ ¨ ¨ ¨ ¡ ¨ I kept a full printed copy in my binder M-5 declaration of medications of each athlete (before match) M-10 injury report form (after match) Random doping controls occurred team physician is present for this When preparing for travel, prepare for the most common problems ¡ ¡ ¡ *food/water contamination-leading cause of illness in travelers Altitude Jet lag 10 4/1/14 ¨ ¨ ¨ ¨ ¨ ¨ ¨ GI meds- Loperamide, Tums, Pepto-Bismol, ABX, Antiemetics, MVI, Docusate ABX- Cipro, Clinda, Amox, Augmentin, Vigamox gtts Electrolyte-replacement powder, MVI Cough suppressants, throat lozenges Pain relievers- Acetaminophen, Ibuprofen, Aspirin, topicals Urgent: Epi pens, Albuterol HFA Allergies- Loratidine ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ Traveler’s Diarrhea (Gastroenteritis) Jet lag Altitude “Boil it, cook it, peel it, or forget it” Can occur anywhere, however it mostly occurs in developing countries ¡ ¨ ¨ Miconazole intravaginal Topicals: Bacitracin, Clotrimazole, Hydrocortisone IVF Injectables Lac tray, wound/blister supplies Glucometer, BP cuff, stethoscope, pen light/ headlamp, thermometer, otoscope Pregnancy tests, UA, hemoccult tests Flow meter, pulse ox Taping supplies, ice bags, Shark SAM splints, joint braces highest risk areas: Central and South America, Mexico, Africa, Middle East, South Asia Almost 50% of Americans visiting developing countries main sources of infection: Food and water contaminated with fecal matter 11 4/1/14 ¨ Prevalence of specific organisms varies with travel destination ¡ Most common causes: ú E.Coli, Campylobacter, Salmonella, Shigella- mainly bacterial abroad ú viral gastroenteritis in US ¡ Less common causes: ú protozoal parasites ú if diarrhea lasts >2 weeks OR if no response to ABX- Giardia Iamblia, Entamoeba histolytica, Cyclospora cayetanensisseen in returning travelers ¡ ¨ Classic definition: ¡ ¨ ¨ ¨ ¨ Rarely life-threatening ¡ ¨ 3 or more unformed stools in 24 hours with at least 1 of the following symptoms: Fever, N/V, abdominal cramps, tenesmus (urge to pass stool), bloody stools Milder forms can present with less than 3 stools Can also have bloating, general fatigue Most occur within the first 2 weeks of travel and last 4 days without treatment ¡ ¨ norovirus on cruise ships 1 in 5 travelers is bedridden for a day > 1/3 must alter their activities Those more susceptible: immunocompromised, those with lowered gastric acidity (taking histamine H2 blockers or proton pump inhibitors), younger age and adventurous travelers; luxury resorts or cruise ships “Food poisoning” is part of the differential dx of TD: gastroenteritis from preformed toxins (Staph aureus, Bacillus cereus) has a short incubation time (1-6 hours) and symptoms usually resolve within 24 hours ¡ Distinguish from TD by perioral numbness, flushing and warmth ¡ 12 4/1/14 ¨ Prevention: A fluoroquinolone can be used for a maximum of 3 weeks in a “critical” competition ¡ Bismuth subsalicylate (Pepto-Bismol) ¡ ú ideally two 262 mg tables QID (with meals and in evening) ú Even though it has a 60% rate of protection, it is impractical for athletes ú Not for those taking anti-coagulants or other salicylates ú Interferes with doxycycline absorption (malaria prophylaxis) ú Side effects include: black stool, black tongue, constipation, tinnitus ¡ Lactobacillus may protect up to 47%; more studies needed ¡ wash hands often with soap/water, esp before eating ú Antibacterial hand wipes/alcohol-based hand sanitizer (at least 60% alcohol) ¡ ¡ ¡ ¡ ¡ Only use bottled water with an unbroken seal, boiled water (best way to purify water), or carbonated beverages in cans/ bottles avoid tap water, fountain drinks, and ice cubes use bottled water for teeth brushing Inspect hotel kitchens and inquire re: the source of fruits and vegetables and the water in which they are washed and prepared confirm that water in a hotel setting is filtered, boiled, or bottled no food from street vendors Eat only fully cooked food ¡ eat hot foods when they are hot; cold foods when they are cold ¡ no room temp sauces ¡ ¡ ú microbes can multiply in foods that are allowed to cool or warm to room temp ¡ ¡ ¡ ¡ ¡ ¡ avoid raw/undercooked meat, fish, or shellfish Do not eat reheated, cooked food avoid leafy salads, unpeeled fruit/vegies in developing countries avoid dairy, unless it is pasteurized boiled/baked/peeled foods are the safest Boiling water is the best way to purify water 13 4/1/14 ¨ Treatment: ¡ ¡ ¡ ¡ ¨ Loperamide (Imodium) ¡ ¡ ¡ ¡ ¨ ¡ 500 mg BID x 1-3 days drug of choice (for most parts of the world) where invasive organisms like Campylobacter and Shigella are common Azithromycin ¡ ¡ ¡ ¨ two 2mg tablets after 1st loose stool, then 1 tab after each subsequent loose stool; max 8 mg in 24 hours x 2days limits symptoms to one day Can be started after the 1st episode of diarrhea if symptoms resolve within 24 hours, no further tx Ciprofloxacin ¡ ¨ Boiled soups/bouillon/broth and electrolytereplacement solutions (have salt which was depleted during diarrhea episodes) Hydration Complex carbohydrates- bananas, rice, bread, potatoes Empiric tx with ABX and loperamide in areas with quinolone-resistant Campylobacter (i.e. Thailand) and for children and pregnant women 1 gram x1 dose OR 500 mg x 1-3 days 10mg/kg daily x 3 days Rifaximin (newer ABX) ¡ ¡ ¡ can be used where noninvasive E.Coli is the main pathogen (i.e. Mexico) decreases symptoms x 1 day 200 mg PO TID x 3 days 14 4/1/14 ¨ Athletes face many challenges at altitude that can effect performance: ¡ ¡ ¡ ¡ ¡ ¡ ¨ ¨ Therefore, acclimatization, proper sleep, sun protection, hydration, good nutrition, and appropriate training are important to help minimize these challenges Acclimatize to help prevent altitude illness: ¡ ¡ ¡ ¡ ¡ ¡ ¡ ¨ avoid flying into high altitude cities if going to higher altitude destination (above 8000 ft) consider sleeping one night at a lower altitude increase altitude gradually Hydrate limit activity initially avoid alcohol high carbohydrate diet can improve oxygenation and exercise performance There is no ideal preventative med for athletes traveling to altitude ¡ ¨ Lower oxygen saturation in the air increased radiation (sun) compromised immune system increased fatigue Malnutrition and dehydration overtraining Ibuprofen (600 mg TID, 6 hours before ascent) can help Recommended: athlete arrives early and resides x 2 weeks at the competition altitude 15 4/1/14 ¨ ¨ ¨ At altitude, lack of hydration (due to plasma volume drop à lower COà lower maximal aerobic power) and iron (due to strong demand on erythropoiesis at altitude) may negatively impact performance Recommended that athletes are screened for serum ferritin levels 8-10 weeks prior to going to altitude, allowing time for supplementation; recommend increased dietary iron intake through various foods Rapid ascent above 2500 m (8200 ft) to a more hypobaric, hypoxic environment is the main cause of altitude illness ¨ AMS HACE HAPE ¨ AMS ¨ ¨ ¡ ¡ HA, dizziness, insomnia, anorexia, nausea, dyspnea, fatigue Tx: Descent*, O2, Gamow bag, Diamox, Dexamethasone, Acetaminophen, Ibuprofen, Aspirin, Zofran 16 4/1/14 ¨ HACE ¡ ¡ ¡ ¡ ¨ HAPE ¡ ¡ ¡ ¨ Medical emergency! same symptoms as AMS + confusion and ataxia and altered level of consciousnes Can result in a coma and possibly death due to brain herniation Tx: immediate descent, O2, Dexamethasone, Gamow bag Medical emergency! dyspnea, tachypnea, moist cough (pink frothy sputum), poor exercise tolerance, low-grade fever Tx: descent*, rest, keep warm, O2*, Gamow bag, CPAP mask or helmet, rehydration, Sildenafil, Tadalafil, Nifedipine, Diamox, Albuterol/salmeterol inhaler Athletes traveling to altitude for training/ competition are at risk for poor sleep quality as a result of both jet lag and the altitude itself 17 4/1/14 ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ Considered to be a significant source of disturbance to athletes, especially when traveling from west to east Goal is to increase adaptation and minimize decrease in performance Sleep deprivation exacerbates the magnitude and duration of jet lag sleep when you can hydrate before and during the trip avoid alcohol 1 day of adjustment needed for each time zone crossed* Travel Management Program (Samuels) – Preflight, inflight, postflight components Preflight: ¡ ¡ ¡ ¡ ¡ ¨ Within 7 days of travel Getting a solid night sleep at least the night before the flight Decrease volume and intensity of training adjust training to the destination time zone a few days before departure evening flight for eastward travel and layovers for travel across 10 or more time zones to help with adapting Inflight ¡ ¡ ¡ ¡ ¡ ¡ ¡ adjust watches to destination time zone comfortable environment (pillows, etc) to facilitate sleep and rest minimize distractions (electronics) eyeshades/earplugs to aid rest noise-canceling listening devices to help relaxation sleep and eat meals on the destination schedule (athletes to bring meals if possible) hydration is a priority 18 4/1/14 ¨ Postflight: ¡ ¡ ¡ ¡ ¡ ¨ Any special considerations re: the injured athlete and returning home by air? ¡ ¡ ¡ ¨ ¨ ¨ 2-4 days after arrival Modification of behavior, not necessarily meds scheduled light therapy, light avoidance, melatonin napping and caffeine (improve alertness, minimize fatigue) ? sedatives if insomnia for 1-2 days or not responding to melatonin Athlete with a pneumothorax may not be able to fly A cast needs to be bivalved Special seating- ie. if GI issues- obtain an aisle seat near a bathroom; if lower extremity injury, obtain an aisle seat Traveling in sports medicine can be challenging However, the key to a successful trip is great preparation and being proactive with the care of your team And remember, always strive to be a positive ambassador- You are representing our country! 19 4/1/14 ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ ¨ www.cdc.gov www.fivb.org http://list.wada-ama.org www.globaldro.com www.cdc.gov www.who.int Epocrates Yates, J. Traveler’s Diarrhea. Am Fam Physician. 2005. 71(11):2095-2100. Harrison, L. New Rifamycin Formulation Curtails Traveler's Diarrhea. http://www.medscape.com/viewarticle/812427.2013. Lipman GS, et al. Ibuprofen prevents altitude illness: A randomized controlled trial for prevention of altitude illness with nonsteroidal anti-inflammatories. Annals of Emergency Medicine. 2012. 59(6): 484–490. Samuels, C. H. Jet Lag and Travel Fatigue: A Comprehensive Management Plan for Sport Medicine Physicians and High-Performance Support Teams. Clin J Sport Med. 2012. 22(3): 268-273. Pipe, A.L. International Travel and the Elite Athlete. Clin J Sport Med. 2011. 21 (1): 62-66. Koehle, M.S., et al. Canadian Academy of Sport and Exercise Medicine Position Statement: Athletes at High Altitude. Clin J Sport Med. 2014. 24 (2): 120-127. Koch, et al. A Successful Therapy of High Altitude Pulmonary Edema With a CPAP Helmet on Lenin Peak (Case Report). Clin J Sports Med. January 2009; 19 (1): 72-73. Michael Savino, D.O. Lori Boyajian-O’Neil, D.O. David Dyck, D.O. Bill Feldner, D.O. Andy Gregory, M.D. Zenos Vangelos, D.O. USA Volleyball AOASM 20
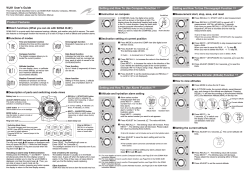
© Copyright 2026