2015 BCN Referral and Clinical Review Program - e
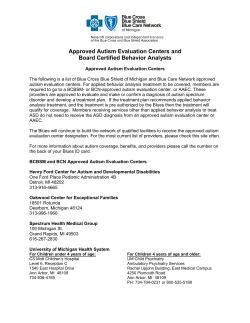
Changes from previous publication are identified by a Blue Dot and explained on page 10 of this document. 2015 BCN Referral / Clinical Review Program Guidelines related to plan notification, clinical review and referral requirements for members with all BCN HMOSM, BCN AdvantageSM HMO-POS and BCN AdvantageSM HMO products For more complete information about plan notification, clinical review and referral requirements, refer to the BCN Provider Manual. BCN Care Management Hours: Monday through Thursday 8:30 a.m. to 12 noon and 1 p.m. to 5 p.m. Friday 9:30 a.m. to 12 noon and 1 p.m. to 5 p.m. Telephone: 1-800-392-2512 BCN Behavioral Health Hours: Monday through Friday 8 a.m. to 5 p.m. Telephone – BCN: 1-800-482-5982 Telephone – BCN Advantage: 1-800-431-1059 OUT-OF-STATE SERVICES: Clinical review and referral requirements for out-of-state services may vary from those outlined in this document. For information on requirements for out-of-state services, contact BCN Care Management at 1-800-392-2512. For all services, noncontracted providers and providers who are not part of the designated network associated with the member's plan must obtain clinical review from BCN Care Management. Section 1: Plan notification and clinical review requirements Plan notification alerts BCN to a scheduled service and is used for claims processing purposes. BCN does not perform clinical reviews on services that require plan notification only. Plan notification must be submitted prior to services being rendered. Benefit / clinical review is conducted for benefit determination or the application of medical necessity criteria or both. Benefit / clinical review requests must be submitted at least 14 days prior to services being rendered. Note: This list is not all-inclusive. See also the notes at the end of Section 1. In addition, authorization of a service by BCN Care Management based on the clinical information provided does not guarantee payment. When the claim for the service is submitted, it may be subject to edits including, but not limited to, diagnosis, frequency and dose. The outcome of those edits may override the initial authorization. Service Requirements Adagen® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Aldurazyme® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Aralast NP § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Arthroscopy, knee Benefit / clinical review is required for all members. Must complete the appropriate knee arthroscopy questionnaire. Autism treatment: applied behavior analysis Contact BCN Behavioral Health for benefit / clinical review. Evaluation at a Blues-approved autism evaluation center is required, with BCN notified prior to the evaluation. Does not apply to members with BCN Advantage products. For additional information, see Autism services. Autism treatment: PT-OT-ST services See entry for physical / occupational / speech therapy in this section. Bariatric surgery Benefit / clinical review is required for all members. Benlysta® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Berinert® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Biofeedback for urinary incontinence and chronic constipation Benefit / clinical review is required for all members. Bone anchored hearing aid Benefit / clinical review is required for all members. Boniva § Prior authorization / clinical review is required for all members. Botox® § Prior authorization / clinical review is required for all members. Breast biopsy, excisional Benefit / clinical review is required for all members. Must complete the breast biopsy (excisional) questionnaire. Cardiac rehabilitation Benefit / clinical review is required for all members. Cerezyme § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Chiropractic services Plan notification is required for all members, including those whose coverage allows self-referrals. CinryzeTM § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Cognitive therapy Benefit / clinical review is required for all members. Colonoscopy – virtual Benefit / clinical review is required for all members. Coronary computed tomographyangiography (CCTA) Effective Feb. 3, 2014: Benefit / clinical review is required for all members. Must complete the CCTA questionnaire. Cosmetic surgery Benefit / clinical review is required for all members. Dental services Benefit / clinical review is required for all members. ® ® Page 1 of 11 Revised July 1, 2015 Changes from previous publication are identified by a Blue Dot and explained on page 10 of this document. 2015 BCN Referral and Clinical Review Program For all services, noncontracted providers and providers who are not part of the designated network associated with the member's plan must obtain clinical review from BCN Care Management. Section 1: Plan notification and clinical review requirements Plan notification alerts BCN to a scheduled service and is used for claims processing purposes. BCN does not perform clinical reviews on services that require plan notification only. Plan notification must be submitted prior to services being rendered. Benefit / clinical review is conducted for benefit determination or the application of medical necessity criteria or both. Benefit / clinical review requests must be submitted at least 14 days prior to services being rendered. Note: This list is not all-inclusive. See also the notes at the end of Section 1. In addition, authorization of a service by BCN Care Management based on the clinical information provided does not guarantee payment. When the claim for the service is submitted, it may be subject to edits including, but not limited to, diagnosis, frequency and dose. The outcome of those edits may override the initial authorization. Service Requirements Developmental delay treatment Benefit / clinical review is required for all members. Diagnostic and therapeutic tests A global referral is required for HMO members in the East and Southeast regions; for all other members, including HMO members in the Mid, West and Upper Peninsula regions, no plan notification or benefit / clinical review is required. No plan notification or benefit / clinical review is required for members with BCN Advantage HMO-POS. Note: For University of Michigan Premier Care, Premier Care 65 and GradCare members, and for members with Blue Cross® Metro Detroit HMO, Blue Cross® Partnered, BCN AdvantageSM HMO ConnectedCare and BCN AdvantageSM HMO MyChoice Wellness coverage, see exceptions to the general rule in Section 2: Referral requirements. DME, medical supplies – diabetic supplies only (includes diabetic shoes / inserts) Benefit / clinical review is required for all members. Must contact J & B Medical Supply to review all requests for diabetic and insulin pump supplies and diabetic shoes / inserts (1-888-896-6233). DME, medical supplies, P&O – nondiabetic Benefit / clinical review is required for all members. Must contact Northwood to review all requests for nondiabetic DME, medical supplies and prosthetics / orthotics (1-800-667-8496). Elaprase® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Elective termination of pregnancy Benefit / clinical review is required for all members. Electrocardiographic rhythm recording and storage devices, long-term, continuous (such as the Zio® Patch and LifeStar ACT) Benefit / clinical review is required for all members. Electroconvulsive therapy Benefit / clinical review is required for all members. Elelyso Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. TM § Endometrial ablation (in office only) Benefit / clinical review is required for all members. Must complete the endometrial ablation questionnaire. Experimental and investigational Benefit / clinical review is required for all members. Eylea § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Fabrazyme® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Firazyr® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Flolan® § Prior authorization / clinical review is required for all members. Fusilev® (levoleucovorin) § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Glassia § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Home health care Benefit / clinical review is required for UAW Retiree Medical Benefits Trust members. For all other members, no plan notification or benefit / clinical review is required. Home TPN and enteral feedings Benefit / clinical review is required for all members. H.P. Acthar Gel § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Hyperbaric oxygen therapy Benefit / clinical review is required for all members. Ilaris® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Immune globulin therapy (IV / SQ) § Prior authorization / clinical review is required for all members. Infertility procedures Benefit / clinical review is required for all members. ® ® Page 2 of 11 Revised July 1, 2015 Changes from previous publication are identified by a Blue Dot and explained on page 10 of this document. 2015 BCN Referral and Clinical Review Program For all services, noncontracted providers and providers who are not part of the designated network associated with the member's plan must obtain clinical review from BCN Care Management. Section 1: Plan notification and clinical review requirements Plan notification alerts BCN to a scheduled service and is used for claims processing purposes. BCN does not perform clinical reviews on services that require plan notification only. Plan notification must be submitted prior to services being rendered. Benefit / clinical review is conducted for benefit determination or the application of medical necessity criteria or both. Benefit / clinical review requests must be submitted at least 14 days prior to services being rendered. Note: This list is not all-inclusive. See also the notes at the end of Section 1. In addition, authorization of a service by BCN Care Management based on the clinical information provided does not guarantee payment. When the claim for the service is submitted, it may be subject to edits including, but not limited to, diagnosis, frequency and dose. The outcome of those edits may override the initial authorization. Service Requirements Inpatient admissions Benefit / clinical review is required for all members. This includes for long-term acute care, inpatient rehabilitation and skilled nursing care. Providers should notify BCN of all emergency admissions within 1 business day. Intensive outpatient therapy (mental health / substance abuse) Benefit / clinical review is required for all members. Jevtana® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Kadcyla® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Kalbitor® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. KrystexxaTM § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Kyprolis® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Laboratory services, genetic tests Benefit / clinical review is required for all members. Must send requests to JVHL at 1-800-445-4979. Lucentis® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Lumizyme® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. MakenaTM § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Maternity: up to 48 hours following routine delivery / 96 hours following C-section Plan notification is required for all members, including those whose coverage allows self-referrals. Mental health therapy Benefit / clinical review is required for all members through BCN Behavioral Health. MRI of breast Benefit / clinical review is required for all members. Myozyme § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Naglazyme® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Neuropsychological / psychological testing for bariatric surgery Plan notification is required for all members. Nplate® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Orthognathic surgery Benefit / clinical review is required for all members. Pain management with epidural or facet joint injections Benefit / clinical review is required for all members. Must complete the appropriate pain management questionnaire. Partial hospitalization (mental health / substance abuse) Benefit / clinical review is required for all members. Physical / occupational / speech therapy autism treatment The provider is responsible for verifying whether each member has autism benefits and, if so, how they are managed and what the clinical review requirements are. In general, benefit / clinical review is not required for members whose autism benefits are managed separate from their medical benefits. It may be required for members whose autism benefits are managed as part of their medical benefits. When clinical review is required, those requests are handled by BCN Care Management. Refer to the e-referral Autism page for additional information. Physical / occupational / speech therapy unrelated to autism treatment Benefit / clinical review is required for all members. Contact Landmark Healthcare and see additional information on Outpatient PT-OT-ST Management Program. ® Page 3 of 11 Revised July 1, 2015 Changes from previous publication are identified by a Blue Dot and explained on page 10 of this document. 2015 BCN Referral and Clinical Review Program For all services, noncontracted providers and providers who are not part of the designated network associated with the member's plan must obtain clinical review from BCN Care Management. Section 1: Plan notification and clinical review requirements Plan notification alerts BCN to a scheduled service and is used for claims processing purposes. BCN does not perform clinical reviews on services that require plan notification only. Plan notification must be submitted prior to services being rendered. Benefit / clinical review is conducted for benefit determination or the application of medical necessity criteria or both. Benefit / clinical review requests must be submitted at least 14 days prior to services being rendered. Note: This list is not all-inclusive. See also the notes at the end of Section 1. In addition, authorization of a service by BCN Care Management based on the clinical information provided does not guarantee payment. When the claim for the service is submitted, it may be subject to edits including, but not limited to, diagnosis, frequency and dose. The outcome of those edits may override the initial authorization. Service Requirements ® Prolastin § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. ProliaTM § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Proton beam therapy Benefit / clinical review is required for all members. Provenge § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Pulmonary rehabilitation Benefit / clinical review is required for all members. Radiology high-tech procedures All BCN-participating freestanding diagnostic facilities, outpatient hospital settings, ambulatory surgery centers and physician’s offices that provide MRI, CT, nuclear medicine and nuclear cardiology are required to call 1-855-774-1317 or to visit www.carecorenational.com (starting July 6, 2015, visit www.evicore.com) for clinical review. Refer to BCN's e-referral Radiology Management Program Web page for additional information. Reclast® See zoledronic acid. ® Remodulin § Prior authorization / clinical review is required for all members. Sleep studies Benefit / clinical review is required for all members. Must complete a questionnaire for the Sleep Management Program. In addition, effective Aug. 5, 2013, a nondiagnostic home sleep test is required for adult members with symptoms of obstructive sleep apnea without certain other comorbid conditions prior to consideration for coverage of a sleep study in the outpatient facility or clinic. Soliris® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Specialist office visits and treatment A global referral is required for HMO members in the East and Southeast regions; for all other members, including HMO members in the Mid, West and Upper Peninsula regions, no plan notification or benefit / clinical review is required. No plan notification or benefit / clinical review is required for members with BCN Advantage HMO-POS. ® Note: For University of Michigan Premier Care, Premier Care 65 and GradCare members, and for members with Blue Cross Metro Detroit HMO, Blue Cross Partnered, BCN Advantage HMO ConnectedCare and BCN Advantage HMO MyChoice Wellness coverage, see exceptions to the general rule in Section 2: Referral requirements. Spine Care Referral Program Benefit / clinical review is required for all members for the initial visit to a spine care specialist and for office visits / procedures. This includes members with coverage through products that would typically allow for self-referral within a designated provider network. See additional information on the Spine Care Referral Program. StelaraTM § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Substance abuse therapy Benefit / clinical review is required for all members through BCN Behavioral Health. Surgery, lumbar spine Benefit / clinical review is required for all members. Must complete the appropriate lumbar spine surgery questionnaire. Surgical procedures, routine A global referral is required for HMO members in the East and Southeast regions; for all other members, including HMO members in the Mid, West and Upper Peninsula regions, no plan notification or benefit / clinical review is required. No plan notification or benefit / clinical review is required for members with BCN Advantage HMO-POS. Note: For University of Michigan Premier Care, Premier Care 65 and GradCare members, and for members with Blue Cross Metro Detroit HMO, Blue Cross Partnered, BCN Advantage HMO ConnectedCare and BCN Advantage HMO MyChoice Wellness coverage, see exceptions to the general rule in Section 2: Referral requirements. TMJ treatment Benefit / clinical review is required for all members. Transcatheter aortic valve implantation (TAVI) and replacement (TAVR) Benefit / clinical review is required for all members effective July 1, 2013. Page 4 of 11 Revised July 1, 2015 Changes from previous publication are identified by a Blue Dot and explained on page 10 of this document. 2015 BCN Referral and Clinical Review Program For all services, noncontracted providers and providers who are not part of the designated network associated with the member's plan must obtain clinical review from BCN Care Management. Section 1: Plan notification and clinical review requirements Plan notification alerts BCN to a scheduled service and is used for claims processing purposes. BCN does not perform clinical reviews on services that require plan notification only. Plan notification must be submitted prior to services being rendered. Benefit / clinical review is conducted for benefit determination or the application of medical necessity criteria or both. Benefit / clinical review requests must be submitted at least 14 days prior to services being rendered. Note: This list is not all-inclusive. See also the notes at the end of Section 1. In addition, authorization of a service by BCN Care Management based on the clinical information provided does not guarantee payment. When the claim for the service is submitted, it may be subject to edits including, but not limited to, diagnosis, frequency and dose. The outcome of those edits may override the initial authorization. Service Requirements Transcranial magnetic stimulation (TMS) for psychiatric or neurological disorders Benefit / clinical review is required for all members effective Oct. 1, 2013. Transgender surgery Benefit / clinical review is required for all members. Transplants Benefit / clinical review is required for all members, for solid organ and bone marrow evaluations and harvesting (except kidney / skin / cornea): • HMO members should be directed to a Blue Distinction® Center+ for Transplants if one is available for the type of transplant the member needs. If one is not available, a Blue Distinction® Center for Transplants facility may be used. This is effective May 1, 2015. • BCN Advantage members must have their transplants performed in a CMS-approved facility that is contracted with BCN. When a Blue Distinction Center for Transplants is available, BCN Advantage members should be referred there. Unclassified procedures Benefit / clinical review is required for all members. (Also called "not otherwise classified (NOC)," "unlisted" and "unspecified.") Varicose veins, treatment Benefit / clinical review is required for all members. Must complete the varicose vein treatment questionnaire. Ventricular assistive devices, percutaneous Benefit / clinical review is required for all members. Vpriv § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Woman’s Choice services See Woman's Choice Referral and Clinical Review Guidelines. XgevaTM § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Xiaflex® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Yervoy® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Zemaira® § Prior authorization / clinical review is required for all members except those with BCN Advantage coverage. Zoledronic acid (Reclast® or Zometa® ) § Prior authorization / clinical review is required for all members. Must complete the zoledronic acid questionnaire. Zometa® See zoledronic acid. ® § See the footnote on page 9. Note: BCN 65 members: BCN Care Management must be notified before a member’s Medicare days are exhausted. Infusion is not routinely covered by Medicare. All care should be coordinated by the primary care physician. Note: BCN as secondary carrier: BCN does not require clinical review when it is the secondary payer. However, the claim will be denied when the service is not a BCN covered benefit and the member has not followed the requirements of the primary carrier. Page 5 of 11 Revised July 1, 2015 Changes from previous publication are identified by a Blue Dot and explained on page 10 of this document. 2015 BCN Referral and Clinical Review Program Section 2: Referral requirements GENERAL RULE. When members need specialty care, their primary care physician must submit a global referral to BCN for a contracted provider. A global referral allows the specialist to perform necessary services to diagnose and treat a member in the office, with the exception of services that require benefit / clinical review. Specialists may not refer patients to other specialists. If the specialist determines services are needed outside those specified by a global referral, including further diagnosis or treatment in an alternate treatment setting (either outpatient or inpatient), the specialist is responsible for submitting all required plan notifications or clinical review requests to BCN. EXCEPTIONS TO THE GENERAL RULE. The following are exceptions to the requirement for a global referral. • Global referrals cannot be used for chiropractic services or for physical, occupational or speech therapy; see Section 1 for those requirements. • BCN’s referral requirements vary based on the region assigned to the medical care group the member’s primary care physician is associated with. (See the Blue Care Network Provider Consultant Regions map at the end of this document.) For BCN HMO members not assigned to a U-M primary care physician and living in the Mid, West or Upper Peninsula region, no global referral is required as long as the specialist is located in one of those regions. For BCN HMO members not assigned to a U-M primary care physician and living in the East or Southeast region, a referral is required. • For University of Michigan Premier Care, Premier Care 65 and GradCare members assigned to a non-U-M primary care physician and referred to any specialist (U-M or non-U-M), a referral is required. This guideline applies regardless of where the member lives or where the practitioners are located. • For BCN Advantage HMO-POS members in any region, no global referral is required as long as the specialist is part of the BCN Advantage HMO-POS network. • For Blue Cross Partnered, BCN Advantage HMO ConnectedCare and BCN Advantage MyChoice Wellness members, services rendered by providers outside of the network designated for each of those products require clinical review. • Blue Cross Metro Detroit HMO members must choose their primary care physician from within the Blue Cross Metro Detroit HMO provider network. That physician coordinates services within the Blue Cross Metro Detroit HMO provider network. Standard referral and clinical review requirements apply. • Members who have coverage through Blue Elect Plus Self-Referral OptionSM may choose to self-refer to any provider within or outside of the statewide BCN HMO network provider without need for a referral, but clinical review requirements do apply for certain services and some services are covered only if rendered by an in-network provider. Providers should go to web-DENIS to get full information on the requirements for each service. • For members who have coverage through self-funded or other products that allow members to refer themselves directly to a specialist within a designated provider network, no referral is required from the primary care physician in order to access specialist services within that network. However, benefit/clinical review requirements apply. Providers should always check Section 1 of this document for benefit/clinical review requirements. • Some services do not require a referral as long as the service is performed by a contracted provider. The table below provides a list of services that do not require a referral for ANY member. Note: This list is not all-inclusive. Note: When a referral does not need to be submitted to BCN, the primary care physician can "refer" the member to the specialist using any method that can be documented by both the primary care physician and the specialist -- for example, a written request, fax or prescription, or telephone notes. Office / outpatient / ancillary services Ambulance - emergent Referral is not required for any member. Anesthesia Referral is not required for any member. Bone density studies Referral is not required for any member. Cardiac stress tests Referral is not required for any member. Chemotherapy / radiation Referral is not required for any member. Diagnostic and therapeutic tests See Section 1. Echocardiograms Referral is not required for any member. EKGs Referral is not required for any member. Emergency room services Referral is not required for any member. Fetal non-stress tests Referral is not required for any member. Hearing aid services (with hearing aid rider) Referral is not required for any member. Holter monitor Referral is not required for any member. Home health care See Section 1. Home infusion Referral is not required for any member. Immunizations Referral is not required for any member. Laboratory services, general Referral is not required for any member. Neuropsychological / psychological testing for other than bariatric surgery Referral is not required for any member. Observation stays Referral is not required for any member. Note: Surgical procedures rendered during an observation stay require a separate outpatient referral, plan notification or benefit/ clinical review. For the benefit/clinical review requirements pertaining to other procedures rendered during observation, see Section 1. Page 6 of 11 Revised July 1, 2015 Changes from previous publication are identified by a Blue Dot and explained on page 10 of this document. 2015 BCN Referral and Clinical Review Program Section 2: Referral requirements GENERAL RULE. When members need specialty care, their primary care physician must submit a global referral to BCN for a contracted provider. A global referral allows the specialist to perform necessary services to diagnose and treat a member in the office, with the exception of services that require benefit / clinical review. Specialists may not refer patients to other specialists. If the specialist determines services are needed outside those specified by a global referral, including further diagnosis or treatment in an alternate treatment setting (either outpatient or inpatient), the specialist is responsible for submitting all required plan notifications or clinical review requests to BCN. EXCEPTIONS TO THE GENERAL RULE. The following are exceptions to the requirement for a global referral. • Global referrals cannot be used for chiropractic services or for physical, occupational or speech therapy; see Section 1 for those requirements. • BCN’s referral requirements vary based on the region assigned to the medical care group the member’s primary care physician is associated with. (See the Blue Care Network Provider Consultant Regions map at the end of this document.) For BCN HMO members not assigned to a U-M primary care physician and living in the Mid, West or Upper Peninsula region, no global referral is required as long as the specialist is located in one of those regions. For BCN HMO members not assigned to a U-M primary care physician and living in the East or Southeast region, a referral is required. • For University of Michigan Premier Care, Premier Care 65 and GradCare members assigned to a non-U-M primary care physician and referred to any specialist (U-M or non-U-M), a referral is required. This guideline applies regardless of where the member lives or where the practitioners are located. • For BCN Advantage HMO-POS members in any region, no global referral is required as long as the specialist is part of the BCN Advantage HMO-POS network. • For Blue Cross Partnered, BCN Advantage HMO ConnectedCare and BCN Advantage MyChoice Wellness members, services rendered by providers outside of the network designated for each of those products require clinical review. • Blue Cross Metro Detroit HMO members must choose their primary care physician from within the Blue Cross Metro Detroit HMO provider network. That physician coordinates services within the Blue Cross Metro Detroit HMO provider network. Standard referral and clinical review requirements apply. • Members who have coverage through Blue Elect Plus Self-Referral Option may choose to self-refer to any provider within or outside of the statewide BCN HMO network provider without need for a referral, but clinical review requirements do apply for certain services and some services are covered only if rendered by an in-network provider. Providers should go to web-DENIS to get full information on the requirements for each service. • For members who have coverage through self-funded or other products that allow members to refer themselves directly to a specialist within a designated provider network, no referral is required from the primary care physician in order to access specialist services within that network. However, benefit/clinical review requirements apply. Providers should always check Section 1 of this document for benefit/clinical review requirements. • Some services do not require a referral as long as the service is performed by a contracted provider. The table below provides a list of services that do not require a referral for ANY member. Note: This list is not all-inclusive. Note: When a referral does not need to be submitted to BCN, the primary care physician can "refer" the member to the specialist using any method that can be documented by both the primary care physician and the specialist -- for example, a written request, fax or prescription, or telephone notes. Office / outpatient / ancillary services Pacemaker adjustments Referral is not required for any member. Pediatric Choice services See BCN Requirements for Pediatric Choice Program. Radiology - routine (procedure codes other than those identified as high-tech) Referral is not required for any member. Also see Section 1. Specialist office visits and treatment See Section 1. Sterilization procedures (with appropriate benefit) Referral is not required for any member. Surgical procedures, routine See Section 1. Urgent care Referral is not required for any member. Woman's Choice services See Woman's Choice Referral and Clinical Review Guidelines. VENDOR CONTACT INFORMATION Vendor name Services Contact information eviCore healthcare Reviews requests for select high-tech radiology procedures. www.evicore.com 1-855-774-1317 J&B Medical Supply Reviews all requests for outpatient diabetic and insulin pump supplies 1-888-896-6233 JVHL Provides statewide network and third-party administration for outpatient laboratory services 1-800-445-4979 Landmark Healthcare Provides care management for members receiving physical, occupational and speech therapy services in office and outpatient settings, including outpatient hospital settings LMhealthcare.com Northwood Reviews all requests for outpatient nondiabetic DME, medical supplies and P&O 1-800-667-8496 Page 7 of 11 Revised July 1, 2015 Changes from previous publication are identified by a Blue Dot and explained on page 10 of this document. 2015 BCN Referral and Clinical Review Program SEC. 3: For services not involving medications covered under the medical benefit Procedures That Require Clinical Review Procedure codes* (Note: This list is not all inclusive.) Note: ALL procedures with "not otherwise classified (NOC)," "unclassified," "unlisted" or "unspecified" codes require clinical review. 00170 19340 2120821210 29870 4084240845 58260 6447964480 74160 ¶ 9086790869 97116 S0199 0295T0298T 19342 21215 2987329877 41800 58275 6448364484 74170 ¶ 90901 97124 S2083 0318T 19350 21230 2987929883 4180541806 58291 6449064495 7417674178 ¶ 90911 97140 S2202 1192011922 19355 21235 2988529887 4182041823 58353 6790067909 7418174183 ¶ 9250792508 97150 S9472S9473 1578015783 19357 21240 30400 4182541828 58356 6971069718 74263 9252192524 97530 1578615789 19361 2124221249 30410 41830 5854158544 70328 7557175574 9379793798 9753297533 1579215793 19364 21255 30420 41850 58550 70336 77003 9578295783 97535 1581915830 1936619371 21270 30430 41870 5855258554 70450 ¶ 7705877059 9580095801 97537 1583215839 19380 21280 30435 41872 58563 70460 ¶ 77520 9580595811 97542 15847 19396 21282 30450 41874 5984059841 70470 ¶ 7752277523 96105 9754597546 1587615879 21010 2129521296 30620 42120 5985059852 7048670488 ¶ 77525 9700197004 97750 17340 21050 21480 3166031661 4364443645 5985559857 7055170553 ¶ 7820178202 ¶ 97010 97755 17360 21060 21485 3336133369 4377043775 6228162282 71250 ¶ 7820578206 ¶ 97012 99183 17380 21070 21490 3399033993 4384243848 62287 71260 ¶ 7821578216 ¶ 97014 A4575 19101 21116 2149321494 3646836471 4388643888 6231062311 71270 ¶ 7822678227 ¶ 97016 C1300 19120 2112021127 22533 3647536476 44130 6231862319 7213172133 ¶ 7845178454 ¶ 97018 G0289 1912519126 2114121147 22558 3647836479 55970 63005 7214172142 ¶ 78466 ¶ 97022 G0398G0400 19300 2115021151 22612 37718 55980 63012 7214672149 ¶ 7846878469 ¶ 97024 G0422G0424 19316 2115421155 22630 37722 56805 63017 7215672158 ¶ 7847278473 ¶ 97026 L8039 19318 2115921160 2733227333 3776537766 57335 63030 7219272194 ¶ 78481 ¶ 97028 L8600 1932419325 21188 27425 37780 58150 63042 7321873223 ¶ 78483 ¶ 9703297036 L8692 19328 2119321199 29800 37785 58152 63047 7371873723 ¶ 78494 ¶ 97110 Q4100 19330 21206 29804 40840 58180 63056 74150 ¶ 78496 ¶ 9711297113 S0190S0191 *CPT codes, descriptions and two-digit numeric modifiers only are copyright 2014 American Medical Association. All rights reserved. ¶ Effective July 1, 2014, clinical review requests for these procedures must be reviewed by eviCore healthcare (formerly CareCore National). Refer to BCN's e-referral Radiology Management Program Web page for information on the eviCore review process. Note: Additional details are provided about the services represented by these codes in the tables found earlier in this document. Page 8 of 11 Revised July 1, 2015 Changes from previous publication are identified by a Blue Dot and explained on page 10 of this document. 2015 BCN Referral and Clinical Review Program SEC. 4: For services involving medications covered under the medical benefit Procedures That Require Clinical Review § Procedure codes (Note: This list is not all inclusive.) Note: ALL procedures with "not otherwise classified (NOC)," "unclassified," "unlisted" or "unspecified" codes require clinical review. C9269C9270 J0220J0221 J0638 J1290 J1559 J1725 J2504 J3285 J3590 J9999 C9272C9273 J0256J0257 J0641 J1300 J1561 J1740 J2507 J3357 J9043 Q2040 J0178 J0490 J0775 J1325 J1566 J1743J1744 J2778 J3385 J9047 Q2042Q2044 J0180 J0585J0588 J0800 J1458J1459 J1568J1569 J1786 J2796 J3489 J9228 J0215 J0597J0598 J0897 J1557 J1572 J1931 J3060 J3490 J9354 § For medications covered under the medical benefit that require prior authorization / clinical review, providers are encouraged to submit requests using the e-referral system by including the necessary information in the e-referral Comments section. The requests may also be called in to BCN Care Management at 1-800-392-2512 or submitted using the Medical Benefit Drug Request Form. This form can be accessed on the e-referral Forms Web page. In addition, see Clinical Information for Drugs Covered under the Medical Benefit That Require Medical Necessity Review, which shows the clinical information and criteria for each drug. Note: Additional details are provided about the services represented by these codes in the tables found earlier in this document. Page 9 of 11 Revised July 1, 2015 Changes from previous publication are identified by a Blue Dot and explained on page 10 of this document. 2015 BCN Referral and Clinical Review Program Blue Dot Changes to the 2015 BCN Referral and Clinical Review Program Service or Topic Change Description Radiology management CareCore National is renamed eviCore healthcare. Starting July 6, 2015, to submit online requests for clinical review for high-tech radiology procedures, providers should visit www.evicore.com. Until that date, providers should visit www.carecorenational.com. Drugs covered under the medical benefit that require prior authorization / clinical review Effective July 1, 2015, services associated with the drugs listed below require prior authorization / clinical review for all members except those with BCN Advantage coverage. Transplants The requirements for transplants are clarified: • Adagen • Firzyr • Kadcyla • Lumizyme • Naglazyme • Aldurazyme • Jevtana • Kyprolis • Myozyme • Xiaflex • Yervoy • HMO members should be directed to a Blue Distinction Center+ for Transplants if one is available for the type of transplant the member needs. If one is not available, a Blue Distinction Center for Transplants facility may be used. This is effective May 1, 2015. • BCN Advantage members must have their transplants performed in a CMS-approved facility that is contracted with BCN. When a Blue Distinction Center for Transplants is available, BCN Advantage members should be referred there. Drugs covered under the medical benefit that require prior authorization / clinical review Effective April 1, 2015, services associated with the drugs listed below require prior authorization / clinical review for all members except those with BCN Advantage coverage. • Aralast NP • Elaprase • Fabrazyme • Ilaris • Soliris • Cerezyme • Elelyso • Glassia • Prolastin • Vpriv • Zemaira For services associated with procedure code J9999, all requests require prior authorization / clinical review for all members, effective April 1, 2015. The list of procedure codes that require clinical review is now divided into two lists: one for services not involving drugs covered under the medical benefit (titled "Sec. 3") and the other for services involving drugs covered under the medical benefit (titled "Sec. 4"). BCN Advantage HMO ConnectedCare References to BCN Advantage HMO Local are removed. Information about BCN Advantage HMO ConnectedCare is added. This product is effective Jan. 1, 2015, and has its own designated provider network. For BCN Advantage HMO ConnectedCare members, services rendered by providers outside of the network designated for that product require clinical review. Blue Cross Metro Detroit HMO Information about to the Blue Cross Metro Detroit HMO product is added. The Blue Cross Metro Detroit HMO product, which is effective Jan. 1, 2015, has its own designated provider network. Standard referral and clinical review requirements apply. Blue Elect Plus SelfReferral Option The information about Blue Elect Plus Self-Referral Option requirements is clarified. Members who have coverage through Blue Elect Plus Self-Referral Option may choose to self-refer to any provider within or outside of the statewide BCN HMO network provider without need for a referral, but clinical review requirements do apply for certain services and some services are covered only if rendered by an in-network provider. Providers should go to web-DENIS to get full information on the requirements for each service. Radiology high-tech procedures The requirements for high-tech radiology procedures are clarifed. All BCN-participating freestanding diagnostic facilities, outpatient hospital settings, ambulatory surgery centers and physician’s offices that provide MRI, CT, nuclear medicine and nuclear cardiology are required to call 1-855-774-1317 or to visit www.carecorenational.com (starting July 6, 2015, visit www.evicore.com) for clinical review. Refer to BCN's e-referral Radiology Management Program Web page for additional information. Page 10 of 11 Revised July 1, 2015 Blue Cross Blue Shield of Michigan and Blue Care Network bcbsm.com Provider Consultant Regions Keweenaw Houghton Ontonagon Baraga Gogebic Luce Marquette Alger Iron Dickinson Chippewa Schoolcraft Mackinac Delta Menominee Upper Peninsula Emmet Cheboygan Presque Isle Charlevoix Antrim West region Otsego Montmorency Alpena Crawford Oscoda Alcona East region Leelanau Provider consultant regional toll-free numbers: Upper Peninsula 1-866-497-7647 West Michigan 1-800-968-2583 East Michigan 1-800-527-1906 Mid region Grand Traverse Benzie Kalkaska Southeast region Manistee Mason Wexford Missaukee Roscommon Osceola Lake Clare Iosco Ogemaw Arenac Gladwin Huron Oceana Newaygo Mecosta Isabella Mid Michigan 1-877-258-0168 Allegan Southeast 1-866-299-4667 Van Buren Berrien Cass Ionia Eaton Barry Kalamazoo Clinton Calhoun St. Joseph Branch Sanilac Saginaw Gratiot Muskegon Kent Bay Tuscola Montcalm Ottawa Midland Shiawassee Ingham Jackson Hillsdale Genesee Livingston Oakland Washtenaw Lenawee Lapeer St. Clair Macomb Wayne Monroe Here’s how to find more comprehensive contact information: 1 Log in at bcbsm.com/provider. 2 Click on web-DENIS. Updated June 2014 3 Click either BCBSM Contact Us or BCN Contact Us. R011579
© Copyright 2026