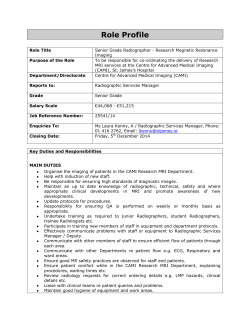
ESMRN-book-online
1 Organised by: Sponsored by: Design: Hakan Pettersson Nuno Canto Moreira Welcome to ESMRN 2015 Warm welcome to Porto, for the 13th biennial Congress of ESMRN! As in previous editions, we hope for our Congress to be a preferred meeting point for all those working in Neuropediatrics including Imaging, Clinics, Genetics, Metabolism and basic Science. We chose Porto this time. This is a city of outstanding scenic beauty, traditions and surrounding landscape - that include the Douro and Port wine region - but also known for the warmth of its people and longstanding tradition in Neuroscience. By combining a high-quality faculty with our special southern-european atmosphere, we hope to set the stage for a great event! on behalf of ESMRN, yours truly Nuno Canto Moreira (President) ESMRN 2015 3 Contents Welcome3 Contents4 Fundação de Serralves 5 About ESMRN 6 Precongress - 13th MAY 8 Day 1 - 14th MAY 10 Day 2 - 15th MAY 12 Day 3 - 16th MAY 14 Free lectures 16 Posters36 Photo legends 55 ESMRN 2015 4 Fundação de Serralves The Serralves Foundation is recognized as one of the main Portuguese cultural institutions and the most relevant of Northern Portugal. Its entire landscape and architectural heritage have been classified as a National Monument in 2012 and are composed by the Museum of Contemporary Art, the House and the Serralves Park. The museum and auditorium (designed by Alvaro Siza) meet the remarkable landscape and architectural ensemble of the art-deco House and the Park, this with 18 acres that include exquisite gardens designed by Jacques Gréber in the 1930’s. ESMRN 2015 5 About ESMRN ESMRN is a small unique Society, which currently holds no list of active members or paying memberships! Founded in 1989 by G. Bydder, D. Christmann, J. Haddad and E. Martin, ESMRN was planned as a forum to gather pediatric neurologists, neuropediatricians, neonatologists, neuroscientists, physicists and (neuro-) radiologists, that use Magnetic Resonance as common denominator. From conventional imaging to advanced MR techniques, ESMRN is committed to better understand the pathophysiological background of neurological disorders in neonates, infants and children. Every other year ESMRN offers a scientific meeting of high standard, usually in the hometown of the president. Here, invited speakers and proffered lectures familiarize the audience with state-of-the-art information, helping to build the strong reputation for quality ESMRN maintains in the Scientific Community. The Society has also been active in teaching activities, with a particular focus on the European Courses on Pediatric Neuroradiology - ECPNR, that are organized jointly with the European Society of Neuroradiology and the European Society of Paediatric Radiology. ESMRN 2015 6 ESMRN Board 13th ESMRN Congress President Nuno Canto Moreira, Uppsala Scientific Committee Organizing Committee Andrea Rossi, Genova Charles Raybaud, Toronto Daniela Prayer, Vienna Ernst Martin, Zürich Gabriel Otterman, Uppsala Ingeborg Krägeloh-Mann, Tübingen Jaap Valk, Amsterdam Jeroen Vermeulen, Maastricht Jim Barkovich, San Francisco Jürgen Hennig, Freiburg Linda De Vries, Utrecht Marjo S. van der Knaap, Amsterdam Nuno Canto Moreira, Uppsala Thierry Huisman, Baltimore Zoltan Patay, Memphis João Xavier, Porto Nuno Canto Moreira, Uppsala João Teixeira, Porto Claudia Pereira, Porto Alexandra Lopes, Porto Teresa Temudo, Porto Vice-President Daniela Prayer, Vienna Secretary Ernst Martin, Zürich Honorary member Jaap Valk, Amsterdam Council members Jim Barkovich, San Francisco Linda De Vries, Utrecht Jürgen Hennig, Freiburg Ingeborg Krägeloh-Mann, Tübingen Charles Raybaud, Toronto Andrea Rossi, Genova Marjo S. van der Knaap, Amsterdam Jeroen Vermeulen, Maastricht ESMRN 2015 7 Precongress - 13th MAY 08.30 - Opening of reception desk and registration 1) Neuroimaging: The tools 09.15 - 10.00 Pediatric neuroimaging: From the past to the future Thierry Huisman (Baltimore) 10.00 - 10.20 fMRI - accuracy, reliability, validity and limitations Daniela Seixas (Porto) 10.20 - 10.40 DWI and experimental design: State of the art Rita Nunes (Lisbon) 10.40 - 11.00 Basics of brain connectivity and graph theory analysis Hugo Ferreira (Lisbon) Coffee break 11.30 - 11.50 MR spectroscopy in pediatric CNS disorders - where are we as users? Carla Conceição (Lisbon) 11.50 - 12.10 New insights by post-mortem brain MRI Christian Mitter (Vienna) 12.10 - 12.30 PET in Neuropediatrics Nuno Canto Moreira (Uppsala) 12.30 - 13.00 Wrap-up and discussion Lunch ESMRN 2015 8 2) Some hot (and re-heated) topics 14.00 - 14.30 Hydrocephalus Charles Raybaud (Toronto) 14.30 - 15.00 Dandy-Walker spectrum Jim Barkovich (San Francisco) 15.00 - 15.30 The fetus and the neonate at equivalent age. How do they differ? Nadine Girard (Marseille) Coffee break 16.00 - 16.25 Movement disorders in autism and Rett syndrome Teresa Themudo (Porto) 16.30 - 16.55 Imaging of autism - does it exist? Alexandre Andrade (Lisboa) 17.00 - 17.25 Hypothermia in neonatal hypoxic ischemic injury Jeroen Vermeulen (Maastricht) 17.30 - 17.55 How much at rest is the resting brain? Sonia Gonçalves (Coimbra) 19.00 - Welcome reception at BH FOZ, Avenida do Brasil 498. ESMRN 2015 9 Day 1 - 14th MAY 08.00 - Opening of reception desk and registration 08.30 - 09.00 Opening remarks Pediatric SNC tumors 09.00 - 09.30 Pediatric brain tumors: The molecular biology revolution and its imaging implications Zoltan Patay (Memphis) 09.30 - 10.00 Challenges and opportunities of consortium-based imaging research in pediatric brain tumors Monika Warmuth-Metz (Würzburg) 10.00 - 10.30 Quantitative imaging opportunities and challenges in pediatric brain tumors. The DIPG experience. Zoltan Patay (Memphis) 10.30 - 11.00 PET in pediatric tumors - beyond FDG Torsten Danfors (Uppsala) Coffee break 11.30 - 12.00 Free lectures (Brain tumors) see pages 17 - 19 12.10 - 13.00 Free lectures (Epilepsy / Malformations) see pages 20 - 24 Lunch ESMRN 2015 10 Epilepsy / malformations 14.00 - 14.45 New concepts in cortical development and brain malformations Jim Barkovich (San Francisco) 14.45 - 15.30 Unilateral Hemispheric Malformations: PMG, FCD, HME Renzo Guerrini (Florence) 15.30 - 16.00 Tubulinopathies and brain malformations Nadia Bahi-Buisson (Paris) 16.00 - 16.30 New concepts of brain dysplasias Jim Barkovich (San Francisco) Coffee break 17.00 - 17.30 Embryology of spinal dysraphisms: Challenging myths and misbeliefs 17.30 - 18.00 Spinal dysraphisms: Basic nomenclature, advanced concepts, and Andrea Rossi (Genova) challenging cases 18.00 - 18.30 Wrap up and discussion Martin Catala (Paris) The panel ESMRN 2015 11 Day 2 - 15th MAY Neurodevelopment and Plasticity 08.30 - 09.00 Developmental anatomy Charles Raybaud (Toronto) 09.00 - 09.30 Imaging of prenatal brain development Andràs Jakab (Vienna) 09.30 - 10.00 Imaging of brain development in neonates and infants Serena Counsell (London) Coffee break 10.30 - 11.00 Imaging of brain development - toddlers and up Marko Wilke (Tübingen) 11.00 - 11.30 Brain adaptation to school attendance A. Castro Caldas (Lisbon) 11.40 - 12.40 Free lectures (Neonatal / Fetal) see pages 25 - 30 Poster presentation / Lunch Roles of the small-brain 14.00 - 14.30 Cerebellar disorders in children: Clinical features Eugen Boltshauser (Zürich) 14.30 - 15.00 Late fetal / premature cerebellum / the challenges Gregor Kasprian (Vienna) Andrea Poretti (Baltimore) 15.00 - 15.30 Cerebellar connectivity Serena Counsell (London) ESMRN 2015 12 Coffee break 16.00 - 16.20 Cerebellar atrophy in children: a neuroimaging pattern-recognition approach Eugen Bolsthauser (Zürich) 16.20 - 16.40 Cerebellar involvement in neurocutaneous disorders Andrea Poretti (Baltimore) 16.40 - 17.00 Chiari I.: a malformation? Chen Wang (Stockholm) 17.10 - 18.00 Free lectures (Genetics / Advances / Miscellaneous) see pages 31 - 35 20.00 - Congress dinner at Taylor´s Wine cellar, Rua do Choupelo #250 - Vila Nova de Gaia. ESMRN 2015 13 Day 3 - 16th MAY Inborn errors of metabolism 08.30 - 08.55 MR parameters in hypomyelination in view of starting treatment Nicole Wolf (Amsterdam) trials 08.55 - 09.20 MR parameters in metachromatic leukodystrophy and the role in Samuel Groeschel (Tübingen) treatment trials 09.20 - 09.45 Patterns of MR diffusion restriction in neonatal metabolic disorders Susan Blaser (Toronto) 09.45 - 10.10 MRS in diagnosis and monitoring of treatment in metabolic disorders Steffi Dreha (Göttingen) 10.10 - 10.35 Conceptualizing MRI phenotypic variation in metabolic white matter disorders Marjo van der Knaap (Amsterdam) Coffee break ESMRN 2015 14 Abusive head trauma 11.00 - 11.25 AHT - clinical dilemmas and controversies Gabriel Otterman (Uppsala) 11.25 - 11.50 AHT - neuroimaging controversies and the evidence base Allison Kemp (Cardiff) 11.50 - 12.15 Spine and neck lesions in AHT Tim Jaspan (Nottingham) 12.15 - 12.45 Research agenda on AHT - where do we go from here? Alison Kemp (Cardiff) The panel 12.45 - 13.00 Prize awards and final remarks The end. See you again at the next ESMRN ! ESMRN 2015 15 Free lectures Day 1 - 14th MAY 11.30 - 12.00 Brain tumors pages 17 - 19 Moderators: Zoltan Patay & Vilma Velickaite Day 1 - 14th MAY 12.00 - 13.00 Epilepsy / Malformations pages 20 - 24 Moderators: Renzo Guerrini & Nadine Girard Day 2 - 15th MAY 11.40 - 13.00 Neonatal / Fetal pages 25 - 30 Moderators: Jeroen Vermeulen & Gregor Kasprian Day 2 - 15th MAY 17.10 - 18.00 Genetics / Advances / Miscellaneous pages 31 - 35 Moderators: Nicole Wolf & Susan Blaser ESMRN 2015 16 Diagnostic and prognostic value of 18F-DOPA PET and 1H-MR Spectroscopy in pediatric supratentorial infiltrative gliomas: a comparative study. Giovanni Morana 1, Arnoldo Piccardo 2, Matteo Puntoni 3, Paolo Nozza 4, Armando Cama 5, Maria Luisa Garrè 6, Andrea Rossi 1. 1 Neuroradiology Unit, Istituto G. Gaslini, Genova, Italy. 2 Nuclear Medicine Unit, Ospedali Galliera, Genova, Italy. 3 Clinican Trial Unit, Scientific Directorate, Ospedali Galliera, Genova, Italy. 4 Pathology Unit, Istituto G. Gaslini, Genova, Italy. 5 Neurosurgery Unit, Istituto G. Gaslini, Genova, Italy. 6 Neuro-oncology Unit, Istituto G. Gaslini, Genova, Italy. Introduction: 1H-MR Spectroscopy (MRS) and 18F-dihydroxyphenylalanine (DOPA) PET are non-invasive imaging techniques able to assess metabolic features of brain tumors. The aim of this study was to compare diagnostic and prognostic information gathered by 18F-DOPA PET and 1H-MRS in children with supratentorial infiltrative gliomas or non-neoplastic brain lesions suspected to be gliomas. Methods: We retrospectively analyzed 27 pediatric patients with supratentorial infiltrative brain lesions on conventional MRI (21 gliomas and 6 non-neoplastic lesions) who underwent 18F-DOPA PET and 1H-MRS within 2 weeks of each other. 1 H-MRS data (Choline/ N-acetylaspartate, Choline/Creatine ratios, and presence of lactate) and 18F-DOPA uptake parameters (Lesion/Normal tissue and Lesion/Striatum ratios) were compared and correlated with histology, WHO tumor grade, and patient’s outcome. Results: 1H-MRS and 18F-DOPA PET data were positively correlated. Sensitivity, specificity, and accuracy in distinguishing gliomas from non-neoplastic lesions were 95%, 83%, and 93% for 1H-MRS and 76%, 83%, and 78% for 18F-DOPA PET, respectively. No statistically significant differences were found between the two techniques (p>0.05). Significant differences regarding 18F-DOPA uptake and 1H-MRS ratios were found between low- and high-grade gliomas (p≤0.001 and p≤0.04, respectively). On multivariate analysis, 18F-DOPA uptake independently correlated with progression-free survival (p≤0.05) and overall survival (p=0.04), whereas 1H-MRS did not show significant association with outcome. Conclusions: 1H-MRS and 18F-DOPA PET provide useful complementary information for evaluating pediatric brain lesion metabolism. 1H-MRS represents the method of first choice in differentiating brain gliomas from non-neoplastic lesions. 18F-DOPA uptake better discriminates low- from high-grade gliomas and is an independent predictor of outcome. Free lecture - Brain tumors - Thursday 11.30 - 11.40 ESMRN 2015 17 Use of DWI and T2 weighted images in predicting tumour grade. Trivedi Chintan Rajendra 1, Sitoh Yih Yian 1, Tang Phua Hwee 2. 1 National Neuroscience Institute, Singapore. 2 KK Women and Children Hospital, Singapore. Introduction: It is desirable for an accurate preoperative imaging method to assign tumour grade. High grade neoplasms may be very cellular and densely packed reducing free motion of molecules. This produces a high signal on DWI and a relatively hypointense signal onT2 images. We aim to use T2 and DWI images to predict tumour grade. Methods: We retrospectively reviewed MRI images of children with histopathologically proven brain tumours performed in National Neuroscience Institute from 1999 to 2005. Regions of Interest (ROI) were drawn manually in the region of tumour and uninvolved cortex on DWI and T2. In heterogeneous tumours, the areas with most hyperintense DWI signal were selected, avoiding areas of haemorrhage or calcification. Results: A total of 38 scans with adequately measurable tumour region were reviewed. There were 22 high grade (WHO II and above) and 16 (WHO grade I) tumours. Average DWI tumour to normal cortex ratio in high grade tumours was 1.4 (range of 0.9 to 1.8) while in low grade tumours the average value was 0.9 (range of 0.6 to 1.3). Average T2 tumour to normal cortex ratio was 1.3 (range of 0.9 to 1.6) in high grade tumours and 1.9 (range of 1 to 2.9) in low grade tumours. Tumours with hyperintense DWI signal were hypointense on T2 thus ruling out a T2 shine through effect. Conclusion: Using 0.9 cut off value for DWI ratio allows 100% sensitivity, 43% specificity for detecting high grade tumours with positive and negative predictive values of 71% and 100%. Free lecture - Brain tumors - Thursday 11.40 - 11.50 ESMRN 2015 18 ETANTR (Embryonal tumors with abundant neuropil and true rosettes): our neuroimaging experience at CHOP. Karuna Shekdar 1, Mariarita Santi-Vicini 2, Erin Schwartz 1. 1 Dept. of Radiology. The Children’s Hospital of Philadelphia (CHOP). 2 Dept. of Pathology. The Children’s Hospital of Philadelphia (CHOP). Introduction: Embryonal tumor with abundant neuropil and true rosettes (ETANTR) is a recently identified variant of primitive neuroectodermal tumor, with fewer than 50 cases reported in the literature to date. ETANTRs have microscopic features of neuroblastoma and ependymoblastoma. Methods: We describe a series of 6 cases with pathologically proven diagnosis of ETANTR. All these cases had MR imaging of the brain with contrast. 3 cases had an initial head CT study. In addition all cases had MR imaging of the entire spine with contrast. Tissue diagnosis was obtained from either surgical resection or biopsy. Results: We will describe 6 cases of ETANTR at this presentation. Our series of 6 cases of ETANTR had 4 located in the posterior fossa and 2 were supra-tentorial in location. We will illustrate the MR imaging findings of the neuro axis of these cases. Discussion: ETANTR is a newly described, highly malignant CNS embryonal neoplasm that typically occurs in young children. Clinically ETANTRs have shown high malignant potential and poor clinical outcome despite aggressive treatment. By reporting these cases of ETANTR, we want to share our experience and welcome a discussion and experience of other pediatric neuro-radiologists of this rare entity of pediatric posterior fossa neoplasms. Free lecture - Brain tumors - Thursday 11.50 - 12.00 ESMRN 2015 19 Clinical presentation and MRI correlation in a pediatric population - a CHLO Epilepsy Surgery Group Engel Ia outcome series. Vera Cruz e Silva 1,2, Ana Rita Pinto 1, Clara Romero 1,3, Nuno Canas 1, Pedro Cabral 1,4, José Carlos Ferreira 1,4. 1 Epilepsy Surgery Group, Centro Hospitalar de Lisboa Ocidental (CHLO). 2 Neuroimaging Department, Hospital Egas Moniz (CHLO). 3 Neurosurgery Department, Hospital Egas Moniz (CHLO). 4 Neuropediatrics Department, Hospital S. Francisco Xavier (CHLO). Introduction: Refractory epilepsies are syndromes in which therapies with two or more antiepileptic drugs do not result in control of crisis. Etiopathology includes malformations of cortical development, such as focal cortical dysplasia (FCD), tuberous sclerosis complex (TSC), hippocampal sclerosis (MTS) or low-grade tumours. Presurgical evaluation combines ictal semiology, electroencephalographic (EEG) and Magnetic Resonance Imaging (MRI) studies, pointing towards an epileptogenic lesion. Methods: Retrospective analyses of patients submitted to surgery for refractory epilepsy from 2009 to 2014 (6 years) was performed. Inclusion criteria included Engel Ia outcome (1-year minimum of follow-up), type of surgical procedure (lesionectomy or amigdalo-hippocampectomy), available pre-operative MRI, video-EEG recording and histopathology diagnosis. We evaluated clinical presentations and MRI findings, regarding the exact localization of the lesions (gyri and functional areas) and compared obtained data to previously published descriptions. Results and Discussion: A total of 26 patients with Engel Ia outcome were depicted, from which 14 lesionectomies and 4 amigdalo-hippocampectomies were selected (n=18). Histopathology diagnosis included MTS (n=4), FDC class I (n=2) and IIb (n=2), TSC (n=3), DNET (n=3), ganglioglioma (n=1) and cavernoma (n=1). An ulegyria focus was diagnosed in 1 patient, whose histopathology showed non-specific cortical disorganization, and another with encephalomalacia focus due to neonatal ischemic insult. All of the patients with MTS showed less informative clinical findings at early-onset. Clinical presentation was highly similar to published data in more than half of patients, while others presented semiologic features described in more than one location, independently of the etiology, reinforcing the importance of combining different diagnostic techniques. Free lecture - Epilepsy / Malformations - Thursday 12.10 - 12.20 ESMRN 2015 20 Does 3T imaging improve lesion identification in children with focal intractable epilepsy? Felice D’Arco, Elysa Widjaja Diagnostic Imaging, The Hospital for Sick Children, Toronto, Ontario, Canada. Background and aims: 3T MRI provides higher resolution imaging and may improve the detection of subtle lesions such as focal cortical dysplasia (FCD) in children with focal intractable epilepsy. The aim of the study was to assess lesion identification in patients with focal intractable epilepsy, comparing 3T versus 1.5T MRI. Methods: Children with focal intractable epilepsy who have undergone epilepsy surgery for the period 2001 to 2013 were included in study. MRI was done on 3T for the period 2008-2013 (post 2008) and on 1.5T for the period 2001-2007 (pre 2008). We assessed the imaging findings and the histopathology of these patients. Results: Of the 182 children included, 89 had surgery pre 2008 and 93 post 2008. Pre 2008, 65/89 (73.0%) lesions were identified and post 2008, 93/102 (91.2%) lesions were identified. The histopathological findings pre 2008 included 39 malformations of cortical development (MCD), 7 mesial temporal sclerosis (MTS), 13 tumors, and 37 others. The histopathological findings post 2008 included 41 MCD, 17 tumors, 7 MTS and 28 others. Pre 2008, 10/14 (71.4%) FCD I and 6/9 (66.7%) FCD II were detected on MRI. Post 2008, 14/16 FCD I (87.5%) and 14/17 (82.3%) FCD II were identified on MRI. Conclusion: Our preliminary findings indicate that 3T improves lesion detection, in particular FCD in children with focal intractable epilepsy. Free lecture - Epilepsy / Malformations - Thursday 12.20 - 12.30 ESMRN 2015 21 Investigating incomplete hippocampal inversion of the pediatric epilepsy patients with normal brain MRI findings. Mehtap Beker-Acay 1, Resit Koken 2, Ebru Unlu 1, Emre Kacar 1, Cinar Balcik 1. 1 Afyon Kocatepe University Faculty of Medicine, Department of Radiology. 2 Afyon Kocatepe University Faculty of Medicine, Department of Pediatrics. Introduction: There are manifold studies evaluating the relationship between epilepsy and hippocampus. It has been speculated that incomplete hippocampal inversion (IHI) which is the fail of the folding of hippocampal structures around the hippocampal sulcus into the temporal lobe can be related to epilepsy. Our study was conducted to analyze the frequency of incomplete inversion of the hippocampus in pediatric age group with epilepsy and the control group without epilepsy that has no abnormal findings on brain magnetic resonance (MR) imaging. Methods: From 2012 to 2015, 1700 brain MR examinations of the patients between 0-16 ages were selected from the hospital archives retrospectively. Out of them, patients with obvious abnormal findings and whom had not coronal sequences on MR imaging were excluded. Finally 118 patients were enrolled in the study; 68 of these had epilepsy and 50 of them were normal for control group. The coronal sequences were analysed in order to investigate IHI. Results: Incomplete inversion of the hippocampus was found in 15/68 of the epilepsy group and 5/50 of the control group. The collateral sulcus was vertically oriented in all subjects with a deviating hippocampal shape. 8 of them were left sided, 5 were right sided, 2 were bilateral in epilepsy group and in the control group all of them were left sided. There was no significant difference between the groups (p: 0.086). Conclusion/Discussion: Future investigation by developing large scale studies will likely lead to explain whether IHI is an aetiological factor in epilepsy or not. Free lecture - Epilepsy / Malformations - Thursday 12.30 - 12.40 ESMRN 2015 22 Delayed rotation of the cerebellar vermis: an important pitfall in early second trimester MR imaging studies. Pinto J 1, Paladini D 2, Severino M 2, Morana G 2, Pais R 1, Rossi A 2. 1 Centro Hospitalar Universitario de Coimbra, Coimbra, Portugal. 2 Istituto Giannina Gaslini, Genoa, Italy. Introduction: Posterior fossa cystic malformations are a frequently discussed topic in fetal neurology, and pose a significant challenge when fetal MRI is performed. Upward rotation of a hypoplastic cerebellar vermis, cystic expansion of the fourth ventricle, and enlarged posterior cranial fossa comprise the classical Dandy-Walker malformation (DWM). Knowledge of physiological variations in cerebellar vermis development is crucial for a correct interpretation of findings. We aim to describe two cases in which delayed rotation of the cerebellar vermis simulated a DWM on early second trimester MRI scans. Case description: Two pregnant women with suspected posterior fossa anomaly on ultrasounds underwent fetal MRI at gestational ages 21 weeks (case 1) and 19 weeks (case 2), respectively. In both cases, upward rotation of an apparently hypoplastic vermis was noted; on midsagittal images, the ponto-tegmental angle was 28° and 43°, respectively. The posterior fossa appeared to be mildly enlarged, while all other findings were within normal range. Follow-up MRI at 28 gestational weeks (case 1) and 1 year postnatally (case 2) showed completely normalized findings. Both children had normal psychomotor development and neurological examinations at age 1 year. Discussion and conclusion: Incomplete cerebellar vermis rotation can be a physiological finding on early second trimester MRI studies, and can simulate DWM or other forms of cerebellar hypoplasia. Embryologically, delayed permeabilization of the Blake’s pouch could account for delayed vermian rotation. Follow-up MRI at later gestational ages is crucial in order not to overreport this condition and to avoid the potential risk of unnecessary pregnancy interruption. Free lecture - Epilepsy / Malformations - Thursday 12.40 - 12.50 ESMRN 2015 23 Dynamic analysis of the interaction between physiological and epileptic resting state networks. Vânia Tavares 1, Hugo Ferreira 1, Alberto Leal 2. 1 Institute of Biophysics and Biomedical Engineering, Faculty of Sciences, University of Lisbon, Portugal. 2 Department of Clinical Neurophysiology, Centro Hospitalar Psiquiátrico de Lisboa, Lisbon, Portugal. Introduction: Simultaneous functional magnetic resonance imaging (fMRI) and electroencephalography (EEG) allows both the analysis of physiological resting state networks’ (RSNs) dynamics and their relation with scalp epileptic activity. In this study we propose a dynamic analysis of RSNs with the main objective of exploring functional connectivity (FC) between physiological and epileptic RSNs and characterizing the relationship between FC and scalp epileptic activity. These advances promise to improve knowledge on the impact of epilepsy in brain physiology. Methods: fMRI/EEG data of four children who underwent epilepsy surgery were analysed. Three types of RSNs were selected for each patient using fMRI data: the epileptic RSN (RSNepi), a RSN that is spatially “neighbor” of the RSNepi (RSNnhb) and the defaultmode network as a reference (RSNref). The FC between the RSNs was studied using a sliding temporal window. The relation between the FC and the scalp epileptic activity was explored. Results and Discussion: A stronger FC between the RSNepi and RSNnhb in comparison with the one between the RSNnhb and RSNref was observed. We found a positive relationship of RSNepi FC with the other RSNs and the scalp epileptic activity. This suggests that the RSNepi has an associated pathologic signature regarding its synchrony with others RSNs. Conclusion: A distinct temporal dynamics was observed for epileptic RSN activity when compared with the dynamics of the remaining physiological RSNs. Free lecture - Epilepsy / Malformations - Thursday 12.50 - 13.00 ESMRN 2015 24 Genetic assessment and genotype-specific clinical course and therapeutic response in patients with neuronal migration disorders. Ute Hehr 1,2, Tanja Roedl 1, Sophie Schirmer 1, Max Langez 3, Tobias Geis 4, Gerhard Schuierer 5, Saskia M. Herbst 1,2. 1 Center for Human Genetics, 2 Department of Human Genetics, 3 Department of Neurosurgery, University Hospital, 4 Department of Pediatrics, University Hospital, 5 Division of Neuroradiology, University Hospital. Regensburg, Germany. Introduction: Neuronal migration disorders are an important cause of early and profound developmental delay, cognitive impairment and difficult to treat seizures. They are classified based on specific structural abnormalities observed in cerebral imaging. Methods: (1) Individual genetic testing algorithm based on clinical information only (n=810) or with additional in-house reevaluation of cMR imaging (n=141) of independent patients with the assigned diagnosis of periventricular nodular heterotopia (PVNH), subcortical band heterotopia (SBH), classic lissencephaly (CL), or polymicrogyria (PMG)/cobblestone lissencephaly (CSL) including linkage analysis for suitable families, CNV analysis, Sanger sequencing and more recently massive parallel panel or exome sequencing. (2) Retrospective assessment of the long-term course and genotype-specific response to antiepileptic and supportive therapies for patients with classic lissencephaly (n=28) or PVNH (n=34) using a standardized questionnaire. Results: Causal mutations were identified in 20,9% of our overall cohort. In-house reevaluation of cMR imaging significantly increased the mutation detection rate to 31.9%. Our preliminary data suggest a genotype-specific response to antiepileptic medication. In LIS1-associated CL valproate and lamotrigine were rated most successful in reducing the number of seizures. For FLNA-associated PNVH lamotrigine was the preferred antiepileptic medication. Discussion: Genome wide genetic testing strategies will further improve the number of genes and genetic alterations identified in neuronal migration disorders, but continue to require their critical interpretation in the context of clinical findings and cerebral imaging. The assessment of larger cohorts may ultimately contribute to develop first genotype-specific treatment recommendations to substantially reduce seizure frequency and overall quality of life as important outcome parameters. Free lecture - Neonatal / Fetal - Friday 11.40 - 11.50 ESMRN 2015 25 Radial vulnerability of white matter segments in preterm infants evaluated with conventional MRI. Ivica Kostović 1, Mirna Kostović-Srzentić 2, Vesna Benjak 3, Nataša Jovanov-Milošević 1, Milan Radoš 1. 1 Croatian Institute for Brain Research, University of Zagreb School of Medicine, Zagreb, Croatia. 2 Department of Health Psychology, University of Applied Health Sciences, Zagreb, Croatia. 3 Department of Pediatrics, Clinical Hospital Center Zagreb, University of Zagreb School of Medicine, Zagreb, Croatia. Introduction: Perinatal white matter lesions have diverse clinical presentation from motor and sensory impairments to disturbance of behavior and cognition. Despite considerable development of neuroimaging techniques it is still difficult to predict clinical outcome for different lesions. Methods: We performed conventional MRI on three groups of children (4 control, 11 normotypic and 19 preterm with lesions) who were examined at the term equivalent age and after the first year of life. Results: Our study indicate that there is developmentally related vulnerability of white matter along radial axis (from ventricle to pia) during perinatal period. We found that borders between different white matter segments (I-V according to Von Monakow) are visible on conventional MRI but after perinatal lesions these borders could be lost at birth and enhanced during subsequent development. For example, perinatal lesions of centrum semiovale lead to loss of border between centrum semiovale and subplate remnant at birth but show enhanced delineation of subplate remnant from centrum semiovale on later MR exam. We interpret the phenomenon of radial vulnerability as a consequence of different developmental schedule for different groups of axonal fibers. Accordingly, lesion of centrum semiovale affect predominantly long associative fibers in centrum semiovale but do not affect short U-fibers which develop later in adjacent subplate remnant. Conclusion: We propose that MRI signal abnormalities and changes at the borders between different white matter segments may be related to lesion of different classes of axonal pathways and have prognostic value for predicting the likely outcome of prenatal and perinatal lesions. Free lecture - Neonatal / Fetal - Friday 11.50 - 12.00 ESMRN 2015 26 An exploration of task-based fMRI in neonates using echo-shifting. Giulio Ferrazzi 1,3, Rita G. Nunes 1,2, Andreia Gaspar 1,2, Tomoki Arichi 1, Emer Hughes 1, Anthony Price 1, Joseph Hajnal 1,3. 1 Centre for the Developing Brain, King’s College London, London, United Kingdom. 2 Instituto de Biofísica e Engenharia Biomédica, Universidade de Lisboa, Lisbon, Portugal. 3 Division of Imaging and Sciences and Biomedical Engineering, King’s College London, London, United Kingdom. Introduction: Achieving optimal BOLD-to-noise contrast in neonatal fMRI is challenging because of the much longer T2* compared to the adult brain. Conventional optimisation approaches would suggest matching the echo time (TE) and T2*. However, using long TEs with conventional EPI decreases the achievable temporal resolution. We applied echo-shifting to improve BOLD-to-noise contrast while maintaining efficient data sampling. The method was tested in neonatal subjects using a passive sensori-motor task. Methods: echo-shifted EPI (es-EPI) is a modification of the standard 2D EPI sequence which enables a TE longer than the time between consecutive excitations. This is done by immediately crushing the signal excited from each slice and only refocusing it during the following readout. 3 infants and 1 preterm baby were scanned using es-EPI with TR/TE of 2545/75 ms, 2mm isotropic resolution. As reference, dual-echo single shot EPI data with TEs of 25 and 75 ms were acquired (identical TR and resolution). Activation was assessed by fitting to the General Linear Model. Results: 1 subject produced useful data with both sequences, whereas the others moved significantly. For this subject, the signal over the activation region was extracted and its variation converted into percent signal change. Standard deviation for es-EPI data, first and second dual-echoes were 1.03%, 0.4% and 0.72% respectively. Discussion/Conclusion: It was possible to elongate TE using es-EPI to match the longer T2* of developing brain, without sacrificing sampling rate and obtain promising activation results. Free lecture - Neonatal / Fetal - Friday 12.00 - 12.10 ESMRN 2015 27 Can cerebral ultrasound findings during therapeutic hypothermia for neonatal hypoxic-ischemic encephalopathy predict significant changes in MRI? Joana Barreira 1, Carolina Santos 2, André M. Graça 3. 1 Department of Neuroradiology - Hospital de Egas Moniz - CHLO. 2 Department of Neuroimaging - Hospital de Santa Maria CHLN. 3 Neonatal Intensive Care Unit - Department of Pedaitrics - Hospital de Santa Maria - CHLN. Introduction: Neonatal hypoxic-ischemic encephalopathy is an important cause of central palsy due mainly to central gray matter lesions. MRI is the gold standard to evaluate those lesions and to predict outcome. We aim to evaluate the ability of early cUS to predict MRI changes on the second week of life. Methods: We reviewed cUS and MRI images from all patients treated with hypothermia at our NICU. cUS were classified according to a local classification system (unpublished) comparing echogenicity of the basal ganglia-thalami with the choroid plexus (0 - lower; 1 - similar; 2 - higher-focal; 3 - higher-diffuse) and the visualization of the internal capsule (0 - not visible; 1 - equivocal; 2 - unequivocal). MRI was classified according to Rutherford (Lancet Neurol 2010). Patients were then reclassified as having lesions that predict an adverse outcome or not, according to Biarge (Early Hum Dev 2010). Results: 44 patients were studied. cUS has shown good specificity (77%) and negative predictive value (70%), but lower sensibility (29%) and positive predictive value (36%) for predicting adverse findings on MRI. McNemar test showed a strong association between cUS and MRI when comparing non-severe vs. severe findings (p=0.629). Full classifications were also compared using McNemar-Bowker test, showing a significant association (p=0.113). Conclusions: US was found to be a good tool for predicting a normal MRI,but the same did not occur for findings associated with an adverse outcome. During hypothermia it is important to use a multimodal approach to outcome prediction, but MRI after completing treatment remains essential to predict outcome. Free lecture - Neonatal / Fetal - Friday 12.10 - 12.20 ESMRN 2015 28 Motion insensitive fetal fMRI combining localized excitation with Echo Volumar imaging. Rita G. Nunes 1,2, Giulio Ferrazzi 1, Andreia Gaspar 1,2, Anthony Price 1, Matthew Fox 1, Christina Malamateniou 1, Mary Rutherford 1, Joseph Hajnal 1,3. 1 Centre for the Developing Brain, King’s College London, London, United Kingdom. 2 Instituto de Biofísica e Engenharia Biomédica, Universidade de Lisboa, Lisbon, Portugal. 3 Division of Imaging and Sciences and Biomedical Engineering, King’s College London, London, United Kingdom. Introduction: Initial fetal fMRI studies used standard multi-slice 2D Echo Planar Imaging (EPI) requiring careful post-processing to correct for fetal motion. To improve robustness to motion, we propose combining Echo Volumar Imaging (EVI), allowing acquisition of a whole fMRI volume following each RF excitation, with selective excitation of the fetal brain. This is a suitable environment for EVI since field inhomogeneities are much less pronounced than in the adult as air-tissue interfaces are absent. Also, T2* values measured across the fetal brain are much longer than in the adult. Methods: An existing multi-echo EPI sequence was modified to achieve EVI. Selective excitation was performed using a Pencil Beam (PB), exciting a cylindrical column along the foot-head (FH) axis. Extra phase encode gradients were added on the anterior-posterior (AP) axis. The approach was tested on 3 adult volunteers with selective excitation of the ventricular region, and 1 fetus (gestational age of 30+4 weeks, assessed as normal). For all localised acquisitions, the FOV was 200×100×100 mm3, with an excited PB diameter of 70 mm. Results: Acquisitions were successful in all cases. Combining EVI with localized excitation, the whole fetal brain could be imaged within approximately 150 ms attaining a 5.0 mm isotropic resolution. Discussion/Conclusion: After further optimizing the sequence to reduce acoustic noise, resting state fMRI data will be acquired on a group of fetuses and the recovered brain networks compared to those estimated using multi-slice 2D-EPI. Free lecture - Neonatal / Fetal - Friday 12.20 - 12.30 ESMRN 2015 29 Correlation of fetal MRI with postmortem imaging and neuropathology in subjects with thanatophoric dysplasia. C Mitter 1, G Gruber 2, U Nemec 1, P Brugger 2, G Kasprian 1, D Prayer 1. 1 Department of Biomedical Imaging and Image-guided Therapy, Medical University of Vienna, Vienna, Austria. 2 Centre for Anatomy and Cell Biology, Department of Systematic Anatomy, Medical University of Vienna, Vienna, Austria. Introduction: Thanatophoric dysplasia (TD), a perinatal lethal form of chondrodysplastic dwarfism includes both skeletal and cerebral abnormalities, including enlargement and abnormal sulcation of the temporal lobes, which both can be diagnosed before 24 gestational weeks (GW) by fetal MRI. We aimed to investigate the potential of several postmortem examination methods in the confirmation and refinement of the fetal MRI diagnosis of TD. Methods: We included 6 subjects between GW 17 and 23 in which fetal MRI at 1,5T or 3T lead to a diagnosis of TD. Postmortem imaging included postmortem MRI at 3T in 2 cases, postmortem CT in 2 cases and postmortem X-ray in 3 cases. In addition the postmortem MRI of a 14GW-old subject was included, from which fetal MRI was not available. In 3/6 cases autopsy was performed. Results: In addition to the well known skeletal findings like short long bones, micromelia and narrow thorax, fetal MRI revealed in 5/6 subjects temporal lobe enlargement with abnormal sulcation, which was confirmed in 2/6 with postmortem MRI as well as in 1/6 additionally at autopsy. Temporal lobe abnormalities could be seen even in the 14GW old subject. In 1/6 subject fetal MRI revealed normal temporal lobe anatomy which was confirmed by histological analysis. Conclusion: Although TD can be reliably diagnosed using fetal MRI as early as GW 17, postmortem examination in case of fetal demise has the potential to both confirm intrauterine findings and reveal additional pathologies that currently can’t be sufficiently assessed by fetal MRI. Free lecture - Neonatal / Fetal - Friday 12.30 - 12.40 ESMRN 2015 30 Effectiveness of melatonin in pediatric neuro - head and neck MRI scans. EJE Heida 1,2, RJ Lunsing 2, OF Brouwer 2, LC Meiners 1. Departments of Radiology 1 and Pediatric Neurology 2, University Medical Centre Groningen. Aim: To assess whether pediatric Neuro-Head and Neck (NHN) MRI scans made with melatonin were diagnostic or contributing to diagnosis, whether effectiveness could be enhanced by BLADE and whether successful scans could be contributed to melatonin. Methods: 72 NHN MRI scans were made from January 2013-October 2014 in children (10 months - 5 years) using 3 to 10 mg melatonin. All scans were retrospectively assessed as diagnostic, contributing to diagnostic trajectory or failed. Number of MRI scans with sleeping/still children was calculated by counting number of scans with no movement in any sequence. Number of successful T1, T2 and FLAIR combined with BLADE was assessed. Actual effectiveness of melatonin was studied by comparing MRI scans in two matched groups (n=19) of swaddled children with and without melatonin. Results: 12/72 scans were diagnostic and 45/72 contributed. 4/72 scans failed. No scans In 11/72. 17/57 diagnostic/contributing scans showed no movement in any sequence. In 27/57 diagnostic/contributing cases one or more BLADE series were used, as replacement or as addition to the protocol. In 18/27 cases, contribution of BLADE scans alone was definite (n =15) or dubious (n=3). In both groups of swaddled children, MRI scans of all cases were diagnostic or contributing. Conclusions: This study suggests that MRI scans made with melatonin in young children are successful in contributing to the diagnosis in the majority of cases. However, it cannot be stated that this is due to the effect of melatonin. The BLADE sequence may be a valuable addition to the neuropediatric scan protocol. Free lecture - Genetics / Advances / Miscellaneous - Friday 17.10 - 17.20 ESMRN 2015 31 Longitudinal MRI volumetry of gray matter reveals a remarkable uniformity of disease progression in CLN2 neuronal ceroid lipofuscinosis. Löbel U 1, Nickel M 2, Sedlacik J 1, Lezius S 3, Fiehler J 1, Nestrasil I 4, Kohlschütter A 2, Schulz A 2. 1 Dept of Diagnostic and Interventional Neuroradiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany. 2 Dept of Pediatrics, University Medical Center Hamburg-Eppendorf, Hamburg, Germany. 3 Dept of Medical Biometry and Epidemiology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany. 4 Dept of Pediatrics, University of Minnesota, Minneapolis, USA. Introduction: Brain atrophy due to neuronal loss is a striking feature of patients with late-infantile neuronal ceroid lipofuscinosis (CLN2), one of the most common degenerative brain disorders in childhood. Tools for quantitative description of disease progression are urgently needed for the evaluation of experimental therapeutic trials. Using MRI volumetry of gray matter (GM), white matter (WM) and lateral ventricles (LV), the aim of our study was to identify suitable MRI correlates of clinical disease progression. Methods: Twenty-one 3D T1-weighted magnetization-prepared rapid gradient-echo data sets of eight patients (5f, 3m; mean age, 6.9±2.5 years) with genetically confirmed CLN2 were performed on a 1.5T MR scanner. Segmentation of brain volumes was done using Freesurfer image analysis suite. Clinical severity was assessed by a disease-specific scoring system. Results: Volumes of supratentorial cortical GM (Median=318.1;SD=101.4; r=-0.93;p<0.01), basal ganglia/thalami (Median= 107.4;SD=26.7; r=-0.90;p<0.01), cerebellar GM (Median= 56.2;SD=16.7; r=-0.80;p<0.01) and cerebellar WM (Median=15.2;SD=4.6; r=-0.88;p<0.01) significantly decreased with age while LV increased (Median=38.0;SD=18.2; r=0.54;p=0.01). Notably, supratentorial cortical GM showed a very uniform decline across the patient cohort. Brain volumes correlated significantly with clinical scoring for supratentorial cortical GM (r=0.89;p<0.01), basal ganglia/thalami (r=-0.71;p<0.01), cerebellar GM (r=-0.60;p<0.01), cerebellar WM (r=-0.56;p<0.01) and LV (r=-0.55;p=0.01). Discussion/Conclusion: Patients with CLN2 showed a homogeneous decline of GM and WM volumes and an increase of LV with age. The decline in supratentorial GM volume was very homogenous across the patient cohort. Therefore, cross-sectional MRI volumetry of supratentorial GM seems to be a suitable marker to quantitatively assess disease progression in CLN2 in experimental therapeutical trials. Free lecture - Genetics / Advances / Miscellaneous - Friday 17.20 - 17.30 ESMRN 2015 32 Brain iron quantification by irreversible/reversible/effective transverse relaxation (R2/R2’/R2*) and quantitative susceptibility mapping (QSM) in healthy controls and mitochondrial membrane protein-associated neurodegeneration (MPAN) under iron-chelating therapy. Sedlacik J 1, Löbel U 1, Schweser F 2,3, Nickel M 4, Deistung A 5, Fiehler J 1, Schulz A 4, Reichenbach JR 5, Kohlschütter A 4. 1 Dept of Diagnostic and Interventional Neuroradiology, Univ Medical Center Hamburg-Eppendorf, Hamburg, Germany, 2 Buffalo Neuroimaging Analysis Center, Dept of Neurology, State Univ of New York, Buffalo, NY, USA, 3 Buffalo Clinical and Translational Research Center (CTRC), Molecular and Translational Imaging Center, State Univ of New York, Buffalo, NY, USA, 4 Clinic for Degenerative Brain Diseases, Dept of Pediatrics, Univ Medical Center Hamburg-Eppendorf, Hamburg, Germany, 5 Medical Physics Group, Institute of Diagnostic and Interventional Radiology, Univ Hospital Jena, Friedrich Schiller Univ, Jena, Germany. Introduction: MRI methods for iron quantification differ in sensitivity. R2 is sensitive to dispersed ferritin molecules, whereas R2’ and R2* are sensitive to ferritin or hemosiderin accumulation within cells and QSM being sensitive to the bulk magnetic susceptibility. To quantify iron content on the basis of MRI, calibration curves of healthy controls over the range of normal iron content are commonly used. However, in case of heavy iron overload, e.g., in MPAN, the extrapolated calibration curves between the different MRI methods diverge which gives valuable information about the iron deposits. Methods: Brain iron content was estimated for 66 healthy controls (18-84 years) based on the study of Hallgren and Sourander 1958. A 13-year-old girl (clinical symptoms: bilateral optic nerve atrophy, mild cognitive decline, gait abnormalities) diagnosed with MPAN received iron-chelating therapy monitored by MRI over 2 years. MRI sequences encompassed 2D multi-echo turbo-spin-echo (R2), multi-echo gradient-echo (R2*) and 3D dual-echo gradient-echo (QSM). R2’ was calculated by R2’=R2*-R2. R2/R2’/R2*-iron calibration curves for healthy controls were determined. QSM-iron calibration of Langkammer et al. 2012 was used. Results: In our patient, iron content (IC) [mg/100g] was highly increased in the globus pallidus (baseline/8/16/24months): IC(R2)=43.4/43.9/48.6/42.6; IC(R2’)=77.1/77.6/72.4/71.9; IC(R2*)=69.1/69.7/66.5/64.9; IC(QSM)=53.0/48.5/47.4/46.3. Discussion/Conclusion: Calibration curves for the healthy control groups agreed with literature. The higher IC(R2’) and IC(R2*) compared to IC(R2) and IC(QSM) in the MPAN patient suggests accumulated iron deposits within cells, which may be a reason why only a small decrease in iron content was observed. This is in contrast to reports on Pantothenate Kinase-Associated Neurodegeneration. Free lecture - Genetics / Advances / Miscellaneous - Friday 17.30 - 17.40 ESMRN 2015 33 H-MRS in glutaric aciduria type 1 (GA1): Impact of biochemical phenotype and age on cerebral accumulation of neurotoxic metabolites. 1 Inga Harting 1, Nikolas Boy 2, Jana Heringer 2, Angelika Seitz 1, Martin Bendszus 1, Petra J.W. Pouwels 3, Stefan Kölker 2. 1 Department of Neuroradiology, University of Heidelberg Medical Center. 2 Department of General Pediatrics, Division of Inherited Metabolic Disease, University Children’s Hospital, Heidelberg, Germany. 3 Department of Physics and Medical Technology, VU University Medical Center, Amsterdam, Netherlands. Introduction: In GA1 the neurotoxic metabolites glutaric acid (GA) and 3-hydroxyglutaric acid (3-OH-GA) accumulate within the brain. Biochemical monitoring of their intracerebral accumulation is as yet not possible due to limited efflux across the blood-brain-barrier. We investigated brain metabolites in GA1 using 1H-MRS with focus on detecting GA and 3-OH-GA. Methods: Short echo time 1H-MRS was performed in 13 treated metabolically stable patients. 21 white matter and 16 basal ganglia spectra from 12 patients were included. Subgroups based on age, biochemical phenotype and/or associated MRI changes were compared with controls. Results: GA was elevated in white matter of patients. 3-OH-GA was elevated in white matter of older patients with associated MR signal changes, which was structurally characterized by decreased tCr and elevated Cho. Metabolite changes differed with biochemical phenotype and disease duration: Low excretors with up to 30% residual enzyme activity had only mildly, non-significantly elevated GA and mildly subnormal tNAA. High excretors with complete lack of enzyme activity had significantly increased GA, tNAA was mildly subnormal in younger and decreased in older high excretors. Conclusion: 1H-MRS can detect GA and 3-OH-GA and might therefore finally allow biochemical followup monitoring of intracerebrally accumulating neurotoxic metabolites in GA1. A high excreting phenotype appears to be a risk factor for cerebral GA accumulation and progressive neuroaxonal compromise despite a similar clinical course in younger high and low excreting patients, which might have consequences for the long-term outcome. Free lecture - Genetics / Advances / Miscellaneous - Friday 17.40 - 17.50 ESMRN 2015 34 Acute non-neoplastic spinal cord lesions in children: An MRI approach to differential diagnosis - five years experience at a Pediatric Center. Carolina Figueira 1, Joana Pinto 1, Mónica Vasconcelos 2, Teresa Garcia 1, Rui Pedro Pais 1. 1 Serviço de Imagem Médica - Neurorradiologia. 2 Neuropediatria, Centro de Desenvolvimento da Criança Hospital Pediátrico - Centro Hospitalar e Universitário de Coimbra, Portugal. Introduction: Spinal cord lesions are rare in children and the clinical picture can be very similar, so differentiating among them remains crucial to their approach. The most common etiologies are: demyelinating and inflammatory diseases, infectious, vascular, neoplastic or paraneoplastic disorders. Magnetic resonance imaging (MRI) is the most sensitive imaging modality in the diagnosis and follow-up of these lesions. Methods: A retrospective analysis was performed, with review of clinical and imagiological data of pediatric patients with acute spinal cord lesions, during the years of 2010 to 2014. In our review we did not considered the cases of spinal cord neoplasms. Results: A total of 19 patients were reviewed, 10 males and 9 females, with ages between 1 to 16 years at diagnosis. Twelve patients were considered to have a vascular etiology (7 were iatrogenic in the context of scoliosis surgery), three an infectious disorder, and four with possible demyelinating lesions. The images were carefully reviewed and, we obtained a T2 hyperintense signal located at the anterior cord in vascular lesions, and more diffuse and multifocal pattern in infectious or demyelinating disorders. Discussion/Conclusion: The location, degree of cord expansion, enhancement pattern, and single versus multiple lesions help to differentiate spinal cord lesions, however, these changes can sometimes be difficult to distinguish, so the clinical and laboratory context is also central to the diagnosis. Radiological, clinical and laboratorial findings of acute myelopathies are reviewed, as are how these findings can be used to distinguish between vascular, demyelinating, infectious, and inflammatory etiologies. Free lecture - Genetics / Advances / Miscellaneous - Friday 17.50 - 18.00 ESMRN 2015 35 Posters Poster discussion will take place 15th May, between 12.40 and 13.50. Presenters are asked to be available near their posters during that time. ESMRN 2015 36 Concurrence among abnormal MRI scans, pathological EEG and intellectual disability in autism spectrum disorder. F. Piras 1, C. Masala 4, M. Carta 1, D. Serra 1, G. Bitti 3, M.T. Peltz 3, R. Fadda 2, G. Doneddu 1. 1 Center for Pervasive Developmental Disorders, AOB, Cagliari, Italy. 2 Department of Pedagogy, Psychology and Philosophy, University of Cagliari, Italy. 3 Department of Diagnostic Imaging, AOB, Cagliari, Italy. 4 Department of Biomedical Sciences, Section of Physiology, University of Cagliari, Monserrato (CA), Italy. Introduction: Abnormal MRI scans and pathological EEG are frequent in Autism Spectrum Disorders (ASD), especially with Intellectual Disability (ID). However, little is still known about the concurrence between ID, pathological EEG and abnormal MRI scans in ASD. Our study aimed to evaluate abnormal MRI scans, pathological EEG and their relation with ID in individuals with non-syndromic ASD. Methods: MRI scans and EEG investigations were studied in 100 children and adolescents. Based on recommended clinical screenings, we excluded patients with infectious, metabolic or genetic diseases, or any other neurological symptoms. Mean chronological age was (2-24 years old). EEG investigations were recorded according to 10-20 system during sleep and MRI scans were acquired with a 1.5-Tesla Signa GE. Results: 68% of individuals had ID, while 32% had typical intellectual development. Moreover, 45% of individuals showed pathological EEG and 46% had abnormal MRI scans. The most frequent MRI abnormalities were cortical dysplasia/atrophy (37%), bilateral periventricular leukomalacia (32.6%), cystic formations (13%), distended optic nerve sheaths (6.5%), vascular malformations (6.5%) and basal ganglia malformation (4.3%). Furthermore, 56.5% individuals had pathological EEG coupled with abnormal MRI scans and 22.2% exhibited pathological EEG, abnormal MRI scans and severe ID. Conclusion/discussion: In line with two previous studies (1,2), our results indicate a considerable percentage of patients with EEG abnormalities, ID and abnormal MRI scans. References: 1) Stanfield A. et al., 2008. 2) Ünal Ö. et al., 2009. Poster # 1 ESMRN 2015 37 Functional connectivity of the language network in left temporal lobe epilepsy. Widmann C 1, Nenning KH 2, Langs G 2, Prayer D 1, Kasprian G 1. 1 Division of Neuro- and Musculoskeletal Radiology, Department of Biomedical Imaging and Image-guided Therapy, Medical University of Vienna, Austria. 2Computational Image Analysis and Radiology Lab, Department of Biomedical Imaging and Image-guided Therapy, Medical University of Vienna, Austria. Introduction: Atypical language representations are frequently seen in left hemispheric temporal lobe epilepsy (lTLE) patients. fMRI based language connectome analysis offers a novel approach to study neuronal networks, linked to language function. The aim of this study was to identify alterations of these networks and characterize the language connectome (LC) in a cohort of lTLE patients. Methods: The functional LC was calculated on the basis of preoperatively acquired functional MRI data (3 Tesla, TE=35ms, TR=3000ms, slice thickness: 4mm, 32 slices, 96x96 matrix, 2.4x2.4x4mm, 100 dynamics, verb generation task, FreeSurfer, FSL). The language connectome of 8 patients with non lesional lTLE (median age 35) and 12 lTLE patients with hippocampal sclerosis (HS) (median age 42) were compared to a reference LC based on 13 healthy controls (median age 38). Variations in the functional connectome analysis were quantified using the network-based statistics (NBS) approach. Results: The language connectome of non lesional lTLE patients and HS patients showed a significantly increased interhemispheric connectivity (p<0.001), compared to healthy controls. While a stronger connectivity in the default mode network was found in controls, both - non lesional lTLE and HS patients showed an increased node degree in the Broca region. Conclusion/Discussion: Task-based NBS analysis reveals widespread alterations in the language connectome of lTLE patients. The recruitment of interhemispheric connections may be linked to structural alterations of the temporal lobe and/ or seizure activity. These observations refine existing theories of language reorganization in TLE. Poster # 2 ESMRN 2015 38 Dual pathology in epilepsy - clinical challenges due to pathological diversity - an illustrated review. Tiago Gil Oliveira 1,2, José Manuel Amorim 1, João Paulo Soares-Fernandes 1. 1 Hospital de Braga, Division of Neuroradiology, Braga, Portugal. 2 Life and Health Sciences Research Institute (ICVS), School of Health Sciences, University of Minho, Braga, Portugal. Introduction: A major challenge in the management of epilepsy in clinical cases with potential indication for surgical ablation is the presence of dual pathology. Methods: A revision of the clinical MRI records of our institution was performed. A selection of representative cases of dual brain pathology in a pediatric population with clinical evidence of seizures is presented. Results: We present 5 patients with a combination of at least two pathological findings identified on imaging studies that could be either responsible for the potential epileptic foci or relevant for management and treatment. Patient#1 presents hypoplastic corpus callosum, nodular subependymal heterotopia and an ectopic neurohypophysis. In Patient#2, a cavernous malformation in the cingulate gyrus and a focal cortical dysplasia were found. Patient#3, a neonatal Sturge-Weber syndrome case, presented bilateral pial angiomas and accelerated myelination. Patient#4 demonstrated bilateral mesial temporal lobe sclerosis. In Patient#5 mesial temporal lobe sclerosis was associated with anterior temporal lobe gliosis. Conclusion/Discussion: In this revision we highlight the role of a thorough imaging evaluation in patients with refractory epilepsy. We further discuss the challenges of defining if one or more lesions are responsible for the presentation of seizures, or their consequence. The identification and detailed characterization of the imaging findings in epilepsy are fundamental for the proper management of each patient. Poster # 3 ESMRN 2015 39 Fetal brain abnormalities associated with congenital heart disease: report of two cases. Valentina Ribeiro 1, José Eduardo Alves 1, João Teixeira 1, Maria Céu Rodrigues 2. 1 Service of Neuroradiology, Centro Hospitalar do Porto, Portugal. 2 Prenatal Diagnosis Center, Centro Hospitalar do Porto, Portugal. Brain and heart development occur simultaneously in the human fetus. Fetuses with congenital heart disease (CHD) have a high incidence of structural prenatal central nervous system abnormalities (CNS), both malformative and acquired. Objective and methods: We report fetal brain and neck MRI abnormalities of two fetuses with isolated congenital heart disease at ecochardiography at Centro Materno Infantil do Porto, who underwent MRI ranged 20-24 weeks gestation. Results: Fetus 1 had a truncus arteriosus and MRI showed corpus callosum agenesis, cerebellar hypoplasia and germinolytic cysts. Fetus 2 presented with coarction of the aorta and MRI revealed a cervical cystic hygroma and brain left ventricular dilatation. In both cases, extensive investigation excluded genetic defects and malformative syndromes. Discussion: Our cases are in line with the literature that both malformations and acquired brain abnormalities are already present prior to birth in fetuses with CHD. Abnormalities in utero cerebral blood flow are associated with abnormal brain development in newborns with CHD, although further studies with fetal MRI are necessary to confirm this suggestion. Our case also show that there is a relationship between cystic hygroma and CHD and NT (nuchal translucency) measurement in the first trimester is potentially useful for screening for fetal major CHD. Poster # 4 ESMRN 2015 40 Fatal acenocoumarol-related in utero subdural hemorrhage. Mariana Diogo 1, Carla Conceição 1, Nisa Félix 2, Cláudia Rijo 2. 1 Department of Neuroradiology, Centro Hospitalar de Lisboa Central, Lisbon, Portugal, 2 Gynecology and Obstetrics Department, Maternidade Alfredo da Costa, Lisbon, Portugal. Introduction: Subdural hematoma (SDH) is a frequent finding in newborns, but antenatal SDH is exceptional. Risk factors include trauma and other maternal or fetal conditions: coagulopathies, infections and iatrogenic effect of drugs, namely vitamin K antagonists; they cross placental barrier and exposure in the second or third trimesters is associated with central nervous system (CNS) malformations or hemorrhagic complications. We present a rare case of extensive, acenocoumarol-associated SDH occurring in the third trimester, emphasizing the importance of anticoagulation as a cause of antenatal intracranial bleeding and the major role played by fetal magnetic resonance imaging (MRI) in its diagnosis. Case Description: A 24-year-old woman under anti-coagulation for prosthetic mitral valve became pregnant. Due to maternal high thromboembolic risk, it was decided to maintain treatment with acenocoumarol throughout the gestation, with bi-weekly ultrasound (US) evaluations. Routine US at 35 weeks of gestation was suggestive of enlarged extra-cerebral space and fetal MRI performed the following day revealed an extensive SDH involving both hemispheric convexities and the tentorium, with significant mass effect. The fetus died 2 days later and autopsy confirmed the imaging diagnosis. Conclusion/Discussion: Anticoagulant-associated fetal hemorrhage is a rare but severe event. There is no alternative regimen that can effectively replace vitamin K antagonists in women with mechanical heart valves. Although US studies are valuable for regular monitoring, MRI offers a more detailed assessment of fetal CNS and provides a better characterization of both hemorrhagic and malformative pathology. Poster # 5 ESMRN 2015 41 Fetal and postnatal MRI of aicardi syndrome. Mariana Diogo 1, Carla Conceição 1, Amets Irañeta 2, Eulália Calado 3. 1 Department of Neuroradiology, Centro Hospitalar de Lisboa Central, Lisboa, Portugal. 2 Department of Neurosurgery, Centro Hospitalar de Lisboa Central, Lisboa, Portugal. 3 Department of Neuropediatrics, Centro Hospitalar de Lisboa Central, Lisboa, Portugal. Introduction: Aicardi syndrome (AS) is classically defined by a triad of corpus callosum agenesis, chorioretinal “lacunae” and infantile spasms. In recent years and with the advent of MRI, further imaging findings have been described: cortical polymicrogyria, periventricular heterotopia, choroid plexus anomalies, intracranial cysts and gross asymmetry of the hemispheres, that probably represents a specific malformation complex and is highly suggestive of AS. The purpose of this exhibit is to describe a case of AS detected in fetal MRI and confirmed in postnatal clinical assessment and imaging studies. Case Description: A pregnant woman was referred to our neuroradiology department for an avascular inter-hemispheric cyst detected in prenatal ultrasound. Fetal MRI was performed at 35 weeks of gestation, and depicted several intracranial anomalies, including agenesis of the corpus callosum with associated inter-hemispheric, multiseptated cyst, a space occupying lesion of the III ventricle, subependymal heterotopias and thickening and irregularity of the frontal cortex. After birth the newborn developed partial seizures and a brain MRI was performed, corroborating the prenatal findings and better depicting the cortical malformation (compatible with polymicrogyria). Diagnosis of Aicardi syndrome was later confirmed by ophthalmologic findings. Conclusion/Discussion: We present a case of Aicardi syndrome with pre and postnatal MRI. Prenatal images were quite elucidative, but since it is a clinical-imagiological entity, definitive diagnosis wasn’t possible until postnatal evaluation. Imaging findings in these patients are paramount for the diagnosis as callosal agenesis is a mandatory feature. Poster # 6 ESMRN 2015 42 Altered brain development in second trimester fetuses with Tetralogy of Fallot in fetal MRI. Christoph Schellen 1, Ernst Schwartz 2, Gerlinde M. Gruber 3, Michael Weber 4, Peter C. Brugger 3, Georg Langs 2, Prayer Daniela 1, Gregor Kasprian 1. 1 Division of Neuroradiology and Musculoskeletal Radiology, Department of Radiology, Medical University of Vienna, Austria. 2 Computational Image Analysis and Radiology Lab, Department of Radiology, Medical University of Vienna, Austria. 3 Center for Anatomy and Cell Biology, Department of Systematic Anatomy, Integrative Morphology Group, Medical University of Vienna, Austria. 4 Department of Biomedical Imaging and Image-guided Therapy, Medical University of Vienna, Austria. Introduction: Abnormal brain growth has previously been described in fetuses with congenital heart disease (CHD). However, little is known about the precise timing of altered brain development and its occurrence in specific CHD subgroups. This in utero MRI study aimed to identify early (median, 25 gestational weeks [GW]) changes in fetal total brain (TBV), gray matter (GMV), and subcortical brain (SBV) volumes in Tetralogy of Fallot (TOF) cases. Methods: Fetal MRI (1.5 Tesla) was performed in 24 fetuses with TOF and 24 age-matched controls (20-34 GW). TBV, GMV, SBV, and intracranial cavity (ICV), cerebellar (CBV), ventricular (VV), and external cerebrospinal fluid (eCSFV) volumes were quantified by manual segmentation (ITK-SNAP) of T2-weighted coronal sequences. Mixed model analyses of variance (ANOVA) and t-tests were performed to compare cases and controls. Results: TBV was significantly lower (p<0.001) in early (<25 GW) and late TOF cases. Both GMV (p=0.003) and SBV (p=0.001) were reduced. GMV to SBV ratios declined in fetuses with TOF (p=0.026). VV was increased (p=0.0048). eCSFV was enlarged in relation to head size (p<0.001). ICV (p= 0.314) and CBV (p= 0.074) were not significantly reduced. Conclusion/Discussion: Fetuses with TOF have reduced gray and white matter volumes and enlarged CSF spaces at 25 GW and earlier. Previously, fetuses with right-sided obstructive lesions were assumed to be less affected by altered cerebral perfusion than fetuses with left ventricular dysfunction. However, the changes in the brains of fetuses with TOF presented in this study indicate a severe impact of TOF on early antenatal brain development Poster # 7 ESMRN 2015 43 Diffuse benign villous hyperplasia - prenatal MRI diagnosis and postnatal follow up. Mariana Diogo 1, Carla Conceição 1, Amets Irañeta 2, Alvaro Cohen 3. 1 Neuroradiology Department, 2 Neurosurgery department, 3 Gynecology and Obstetrics Department, Centro Hospitalar de Lisboa Central, Lisbon, Portugal. Introduction: Diffuse benign villous hyperplasia (DVH) is a rare congenital condition characterized by bilateral enlargement of the choroid plexus and increased ventricular size. MRI is the imaging modality of choice in establishing the diagnosis. We present a case of DVH diagnosed by fetal MRI (fMRI) and compare it to postnatal brain MRI findings. To our knowledge, no other cases have been diagnosed in utero using this imaging modality. Case Description/Results: A primiparous mother had an ultrasound at 21 weeks’ gestation, which showed asymmetrical enlargement of the lateral ventricles. Brain fMRI was performed at 23 weeks’ gestation (and again at 27w), showing moderate lateral ventricle dilatation with enlarged choroid plexus, occupying both atria and occipital horns. Biparietal and fronto-occipital diameters were above P90. Given the findings, DVH was considered the most probable diagnosis and parents decided to carry pregnancy to term. After birth (at 39 weeks) physical and neurological examination was normal, apart from cephalic perimeter (CP) above 95th percentile. Postanatal brain MRIs were performed at 5 weeks and 9 months and corroborated the prenatal findings. No other abnormalities were noted. Ventricular size remained stable, with no need for shunting. Conclusion/Discussion: Enlarged lateral ventricles are a common reason of referral for fMRI. This case depicts a rare entity, diagnoses by fMRI and illustrating the crucial role of this imaging modality in prenatal CNS evaluation. DVH is a benign entity demanding differential diagnosis with more ominous disorders, like CP tumors. Poster # 8 ESMRN 2015 44 Is fetal vermian lobulation quantifiable? Dovjak G 1, Brugger PC 2, Gruber G 2, Schwartz E 3, Bettelheim D 4, Prayer D 1, Kasprian G 1. 1 Division of Neuro- and Musculoskeletal Radiology, Department of Biomedical Imaging and Image-guided Therapy, Medical University of Vienna, Austria. 2 Center for Anatomy and Cell Biology, Department of Systematic Anatomy, Integrative Morphology Group, Medical University of Vienna, Austria. 3Computational Image Analysis and Radiology Lab, Department of Biomedical Imaging and Image-guided Therapy, Medical University of Vienna, Austria. 4Department of Obstetrics and Gynecology, Medical University of Vienna, Austria. Introduction: This MRI study aims to quantitatively assess normal vermian development in human fetal brains in vivo. Furthermore the accuracy of fetal MRI based vermian visualization is determined by comparing in vivo with post-mortem segmentation results. Methods: 29 fetuses (18-30 gestational weeks - GW, mean 25.55GW) were scanned prenatally (1.5 Tesla, T2-TSE, resolution 0.7/0.7/4.4mm before 24GW and 0.9/0.9/4.4mm after 24GW) and 7 fetuses (16-30GW, mean 21.9GW, 3 Tesla, CISS sequence, resolution: 0.33/0.33/0.33mm) scanned within 24 hours post-mortem were selected for postprocessing. A T2-weighted midline sagittal slice was identified and 2D vermian segmentation was performed using ITK snap. Results: 7 of the 9 Vermian lobules could be discriminated prenatally and post-mortem. The mean proportional percentage of each vermian lobule was (in vivo vs. post mortem): 6.88% vs. 6.82% (Lingula), 10.13% vs. 11.42% (Centrum), 27.67% vs. 29.87% (Culmen), 21.9% vs. 21.42% (Declive+ Folium+ Tuber), 13.84% vs. 15.24% (Pyramis), 15.8% vs. 10.88% (Uvula), 3.78% vs. 4.35% (Nodule) across all gestational ages (18-30GW). The standard deviation ranged between 1.08-3.97 (in vivo) and 1.94%-3.31% (post mortem) per lobule. 3D models of post-mortem cerebellar hemispheres were generated. Conclusion/Discussion: Different vermian segments can be reliably visualized between 18 and 30GW by fetal MRI. Proportions of the vermian lobules correlate between post-mortem and in vivo measurements and remain stable during this observational period. In future, comparative analysis will help to further classify cases of hindbrain malformations at prenatal stages. Poster # 9 ESMRN 2015 45 Brain Magnetic Resonance Imaging findings after in utero toxic exposure. José Manuel Amorim, Tiago Gil Oliveira, Jaime Rocha, João Soares Fernandes. Serviço de Imagiologia - Departamento de Neurorradiologia, Hospital de Braga. Introduction: Central Nervous System (CNS) malformations are mainly caused by genetic defects. However, when pregestational and/or gestational toxic exposure occurs, a teratogenic etiology should be considered. Methods: We reviewed our institution’s neuroimaging archive and collected a series of 5 illustrative cases of children who suffered in utero exposure to alcohol (cases 1 and 2), alcohol and valproate (case 3), cocaine and opiates (case 4) and isotretinoin (case 5). Brain and spine MRI findings are described. Results: Polysubstance abuse was present in 2 of the 5 cases. In the cases related to in utero alcohol exposure only, imaging findings ranged from brain abnormalities (including midline malformations and simplified gyral pattern) to craniocervical junction (CCJ) malformations and spine segmentation or fusion disorders. In valproate and alcohol consumption we found brain midline malformations, CCJ malformations and diastematomyelia. In cocaine and opiate abuse, callosal hypogenesis and subependymal hemorrhages were found. The use of retinoic acid was associated with cerebellar malformations, short corpus callosum and brain volume loss. Conclusion: A wide range of CNS malformations are associated with in utero toxic exposure. The recognition of characteristic imaging abnormalities plays an important role in the diagnosis and/or confirmation of suspected drug-induced CNS malformations. This has important medicolegal implications and also clinical significance to avoid unsuccessful and misleading genetic testing. Poster # 10 ESMRN 2015 46 A pauci-simptomatic presentation of Leukoencephalopathy with Vanishing White Matter. Vera Cruz e Silva 1, Marcelo Mendonça 2, Gonçalo Matias 3, Marjo Van der Knaap 4, Joana Graça 1. 1 Neuroradiology Department, Hospital Egas Moniz (CHLO), Lisboa. 2 Neurology Department, Hospital Egas Moniz (CHLO), Lisboa. 3 Neurology Department, Hospital Geral das Forças Armadas, Lisboa. 4 VU University Medical Center, Amsterdam. Introduction: Leukoencephalopathy with Vanishing White Matter (LVWM) is an autosomal recessive hereditary disease and one of the more prevalent leukoencephalopathies in children. It presents mostly with long term onset and clinical presentation usually includes cerebellar ataxia and progressive neurological deterioration. Beyond the pediatric phenotype, some pauci-symptomatic presentations have been reported in older patients. Case description: We present a case of a 15-year-old male with normal psycho-motor development presenting a generalized seizure after being hit in the face by a ball. Three months later, in a similar context, describes a 3-minute episode of isolated sudden conscious loss. Neurological examination depicted only hyperactive deep tendon reflexes. Electroencephalogram showed diffuse slowing, predominant in the frontal lobes, without paroxysmal activity. MRI presented extensive bilateral and symmetric hyperintensity on T2-weigthed images of white matter associated with cystic degeneration, without basal ganglia or thalamic abnormalities, nor increased signal after gadolinium. The diagnosis of LVWM was considered and confirmed by genetic test: 2 pathogenic compound heterozygous mutations in the gene EIF2B5. A 3-year follow-up showed no clinical or imaging deterioration. Discussion: The pediatric phenotype of LVWM is well known and usually points towards the diagnosis, which is afterwards confirmed by MRI studies. However, in cases with mild or unsuspicious clinical presentation such an advanced imaging presentation is usually rare and surprising. We suggest this entity to be considered among the differential diagnosis of young onset leukodistrophies, even in the absence of typical clinical findings. Poster # 11 ESMRN 2015 47 The role of MRI in the diagnosis of Wolfram syndrome - a review about three cases. Mariana C. Diogo, Carla Conceição, Catarina Perry Câmara. Neuroradiology Department, Hospital Dona Estefânia, CHLC, Lisbon, Portugal. Introduction: Wolfram syndrome (WFS) is a neurodegenerative genetic disorder, also known by the acronym DIDMOAD, describing its main features: diabetes insipidus (DI), diabetes mellitus (DM), optic atrophy, and deafness. Although genetic studies offer the definite diagnosis, magnetic resonance imaging (MRI) plays a preponderant role in showing an array of suggestive findings. Methods: We reviewed 3 cases of genetically confirmed WFS, imaged and diagnosed in our center, in which MRI played a preponderant role in the diagnosis. Major findings in this syndrome are discussed, with special focus on the imaging aspects. Results: Three cases of WFS in non-related adolescent girls are described. A summary of each clinical presentation, as well as imaging findings, are presented. Age of first symptoms’ onset varied from 18 months to 11 years of age, with several years until diagnosis. MRI findings included: absence of the neurohpophysis physiological signal, thinning of the optic nerves and chiasm, and atrophy and signal anomalies of the cerebral cortex, brain stem, and cerebellum. Using these 3 cases as a starting point we review the classic and atypical imaging findings and their correlation with the clinical presentation in WFS. Conclusion/Discussion: Diagnosis of WFS is not always straightforward, as symptoms can develop over a long period of time and concern different medical specialties. Neuroradiolgists should be aware of findings typical of WFS and suggest the possibility of this diagnosis in the association of loss of neurohypophysis high signal and optic atrophy in patients performing MRI for deafness or visual alterations. Poster # 12 ESMRN 2015 48 Acute necrotizing encephalitis of children (ANEC). Ibrahim Shoukry Cairo University. Tarek Farid National Research center Cairo. Background: Acute necrotizing encephalitis is a catastrophic disease presenting as encephalopathy and complicated by motor and cognitive disability. Liver affection is a common association. MRI is diagnostic showing always bilateral thalamic involvement in addition to brain stem and tegmentum in some cases. This work aims at analyzing outcome of this condition in relation to neuron-imaging. Methods: This study comprises 3 boys and 2 girls, aged between 10 and 22 months. They presented with fever and disturbed sensorium. MRI, EEG, CSF analysis, liver and coagulation profile were done. Results: Seizures were present in three cases two focal and one generalized. Hypotonia and sluggish tendon reflexes were evident in four cases. Bulbar manifestations were present in two, one case had asymmetrical facial palsy and one had ophthalmoplagia. MRI showed bilateral symmetrical thalamic necrosis in all cases. Subcortical white matter lesions in parasagital and parietal areas were present in four cases and brain stem signals in two. Elevated transaminase and hypoprothrombinemia were found in all cases. CSF showed increased Protein in four cases. EEG showed hypoactivity and featureless background in two cases. One case recovered completely after hydrocortisone. Two cases with brain stem and white matter lesion developed psychomotor retardation and were assigned on intervention program. The two cases showing hemorrhagic necrosis in thalami died in ICU. Conclusion: Despite thalamic necrosis in all ANEC cases, those with hemorrhagic necrosis have the worst prognosis. Brain stem and white matter lesions are associated with neurological dysfunction and intellectual retardation. Poster # 13 ESMRN 2015 49 Isolated bulbo-medullary atrophy/hypoplasia - anoxic-ischemic or malformative origin? A cause for severe central hypoventilation in a neonate. Carolina Figueira, Joana Pinto, Teresa Garcia, Rui Pedro Pais. Serviço de Imagem Médica - Neurorradiologia, Hospital Pediátrico - Centro Hospitalar e Universitário de Coimbra, Portugal. Introduction: Systemic hypotension and other conditions of reduced perfusion in the fetus with early or late onset in gestation, may result in symmetrical longitudinal columns of infarction in the midbrain, pons and medulla oblongata. Isolated malformations involving the brainstem and bulbo-medullary junction are extremely rare and usually are associated with cerebellar disorders. Magnetic Resonance Imaging (MRI) is helpful, although diagnosis during life can be quite a challenge. Case Report: A thirty-two weeks premature male newborn with monitorized pregnancy, revealed intrauterine growth delay, polyhydramnios and alterations in the doppler ultrasound. An urgent cesarean was performed with required intubation and aggressive mechanical ventilatory support. The MRI performed at the 39th day of life revealed segmental bulbo-medullary atrophy/hypoplasia with 1 mm in the antero-posterior axis. No abnormalities were found in the cerebellum and in the cranial nerves VI, VII, VIII, IX and X. During hospitalization within intensive care unit the patient showed severe clinical deterioration and died at the fifth month and fourteenth day of life. Anatomopathological autopsy was performed. Conclusion/Discussion: In our case, the hypothesis of a severe anoxic-ischemic injury during fetal life was considered rather than a malformation. This cases rarely appear in the literature and, to our knowledge, there is no published case report with similar MRI findings. Poster # 14 ESMRN 2015 50 Clinical and MRI multicentric prospective study for diagnosis of leptomeningeal angiomata and Sturge-Weber syndrome in neonates with upper facial port-wine stain. Chateil JF, Dutkiewicz AS, Havez-Enjolras M, Ezzedine K, Léauté-Labrèze C, Bessou P. University hospital Pellegrin, Departments of Pediatric Radiology and Dermatology, Bordeaux, France. Introduction: congenital facial port-wine stain (PWS) located in the V1 territory is at risk for leptomeningeal angiomata (LMA), leading to Sturge Weber syndrome. The authors compared patterns of PWS and MRI. Methods: clinical data and MRI were prospectively collected in 71 infants. Face photographs were analysed, PWS were classified into 6 distinct patterns. MRI with at least T1, T2 and post-contrast sequences were blindly evaluated by 2 radiologists, to search for LMA or indirect signs: white matter signal asymmetry, ventricular and choroid plexus size, pericerebral spaces, atrophy, calcification. A composite MRI score evaluated the probability for LMA, and compared to PWS patterns and neurological signs, at least after 6 months. Results: 71 patients were enrolled, 66 were finally included. PWS involving midline, scalp, nose, temporal areas were associated with an increased risk of LMA, several at-risk patterns were recognized. Mean age of MRI was the first 4 months of life. 11 patients presented LMA, with significant composite score; there was one false negative with early MRI. Most sensitive signs were white-matter signal asymmetry on T2, asymmetry of size hemispheres and choroid plexus, visibility of the LMA after injection. Diffusion imaging can contribute to diagnosis; SWI is promising but has not been carried out systematically in our series. Conclusion: LMA is not always present at birth. Recognition of indirect MRI signs is crucial. The protocol that can be proposed for babies with at-risk PWS patterns should include: Sagittal T1, axial T1 IR, axial T2, diffusion, SWI, T1 after contrast. Poster # 15 ESMRN 2015 51 Central nervous system imaging in childhood LCH : Preliminary findings. Luciana Porto 1, Stefan Schöning 2, Elke Hattingen 1, Jan Sörensen 2, Thomas Lehrnbecher 2. 1 Neuroradiology Department. 2 Hospital for Children and Adolescents. Johann Wolfgang Goethe University Frankfurt/Main, Germany. Objective: Langerhans cell histiocytosis (LCH) is a systemic disease with variable impact on the central nervous system (CNS). The aim of this study was to evaluate the cerebral MR imaging abnormalities in children with LCH. Material and Methods: Two experienced neuroradiologists retrospectively reviewed 31 cranial MR examinations available out of 94 children and adolescents with LCH. The incidence of typical cerebral pathologies of LCH was rated regarding their signal intensity on T2-w images and on contrast-enhanced T1-w images. Results: The most common MR changes were osseous (55%), followed respectively by pineal enlargement (45%), pituitary stalk mass (32%) and signal changes of dentate nucleus (32%). Occasionally, hyperintensity in hippocampus, parenchymal and meningeal enhancement, as well as white matter hyperintensity also occurred. The inter-rater agreement was 69-100%. The lowest agreement was found for the pineal region and the dentate nucleus. Conclusion: The most common sites of manifestation in LCH after the bone were the pineal gland and the hypothalamic-pituitary system. We showed that neurodegeneration can begin at early age and that the CNS may be affected not only as primary site, but also as secondary degeneration with the involvement of the cerebellum and the white matter. It is important to increase the sensitivity of the radiologist staff to specific MRI changes related to LCH, especially for the pineal region and the dentate nucleus. Poster # 16 ESMRN 2015 52 Methionine-PET in the initial work-up of suspected brain tumours: is there an added value? V. Velickaite, T. Danfors, N. Canto-Moreira. Uppsala University Hospital, Sweden. Introduction: The uptake of C11-Methionine in PET (MET-PET) reflects protein synthesis. The normal brain has a low uptake, so the method helps in the workup of suspected tumours, mostly to evaluate tumour size and, indirectly, both cell and vessel proliferation. Its value is known in the adult population, but few data exist in the special group of pediatric brain tumours. Methods: We reviewed brain MET-PET examinations performed since 2004 on patients younger than 18 years, for evaluation after MRI of a new suspected tumour (n=31). Preoperative PET and MRI were compared regarding matching of lesion size/location, suspected diagnosis and potential added value for patient management. The surgical results (WHO grading) were compared 1) to maximum MET uptake (“hotspot”), and 2) to the type of match between MRI (FLAIR and T1-contrast) and PET. Results: Comparing to the suspected MRI diagnosis, PET did not add relevant clinical information in 19 (61%) patients, was less performing in 3 (10%), and added significant information in 9 (29%). In 3 of these, PET changed the proposed treatment. Amongst the patients that had surgery (n=18) there was no correlation between WHO grade and maximum MET uptake. A correlation (<. 05) existed between the pattern of PET/ FLAIR match and WHO grade, but not concerning T1-contrast. Conclusion: MET-PET is useful in the initial workup of pediatric tumours, but does not correlate with WHO grade. Should be interpreted jointly with MRI studies. Poster # 17 ESMRN 2015 53 A case report based discussion concerning extra-axial tumors in pediatric age - can we suggest a gliosarcoma diagnosis? Luísa Sampaio, Irene Bernardes, José Fonseca. Neuroradiology Department, Centro Hospitalar de São João, Porto, Portugal. Introduction: Extra-axial tumors in pediatric age are rare and often have the burden of a tricky differential diagnosis. In spite of this, they are almost always forgotten when discussing pediatric tumors. We intent to discuss them, based on a clinical case and focusing on three differential diagnosis. Case description: An 8 year-old boy presented to the emergency department with headaches during for the last 2 months, without neurologic deficits. CT scan showed a volumous extra-axial left temporo-parietal occupying-space lesion, mildly heterogeneous (vascularized with necrotic-cystic areas) that enhanced avidly on postcontrast images (except in the necrotic-cystic areas); bone algorithm depicts thinning of the overlying calvaria. Brain MR confirmed the extra-axial location of the tumor, showing well defined boundaries. For its heterogeneous morphology contributed an antero-medial necrotic area with hemorrhagic residues and vascular flow voids. The postcontrast enhancement was intense and homogenous outside the mentioned heterogeneous areas. This lesion was surrounded by moderate vasogenic edema. No “dural tail sign” was identified. He was submitted to surgery and the pathologic examination diagnosed gliosarcoma. Conclusion/discussion: We believe that the main differential diagnosis to consider were anaplastic hemangiopericytoma, atypical meningioma and gliosarcoma. We believe that atypical meningioma was the less likely, because of the thinning of the overlying bone, that most frequently shows hyperostosis. Regarding the other two diagnosis, the imaging differential is virtually unachievable. Both can display necrotic areas, vascular voids and thinning of the nearby calvaria. Also, they may or may not have an associated “dural tail sign”. Poster # 18 ESMRN 2015 54 Photo legends 1. Port wine cellar 2. Typical Rabelo boat, used to carry barrels down the Douro river 3. FC Porto: the city’s mascot! 4. Panorama view of Porto, taken from Gaia. 5. Our own Hospital S. Antonio... a long time back! 6. D. Maria bridge, year 1876 7. Ana Clara sliding down, year 2009 8. Winter storm at Felgueiras Lighthouse, year 2010 ESMRN 2015 55
© Copyright 2026