Randy Poelman , Johan van der Meer , Coretta van Leer
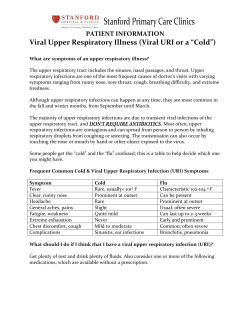
POINT-OF-IMPACT TESTING IN THE EMERGENCY DEPARTMENT: DIAGNOSTICS FOR RESPIRATORY VIRAL INFECTIONS Randy Poster ID: S35 1 Poelman , 1Department Johan van der 2 Meer , Coretta van 1 Leer-Buter , Annelies 1 Riezebos-Brilman , Alex 1 Friedrich and Bert 1 Niesters of Medical Microbiology, Division of Clinical Virology; 2Emergency Department, The University of Groningen, University Medical Center Groningen, the Netherlands Background Objective Methods Molecular diagnostics for infectious diseases is increasingly important in a clinical setting for both disease management and infection control. New highly sensitive and specific tests become readily available due to the shifting trend from single to multiplex testing, as well as from centralized to decentralized Point-Of-Impact Testing (POIT). With a critical window of opportunity for innovations within a hospital setting, we aimed to assess the value of POIT for respiratory viral diagnostics at the emergency department, by implementing an adequate diagnostic policy. This will affect the laboratory hands-on time and the total turnaround time which is related to adequate therapy, infection control measures and cost redundancy. For the improved hospital broad diagnostic policy, the emergency department (ED), the department of medical microbiology and several clinical wards were actively involved. The BioFire respiratory panel (bioMerieux) was implemented and we extended our service from 08h to 22h, 7 days a week during the respiratory season from early December 2014 to early April 2015. We created a hospital broad model to represent the cost-effectiveness and measured the (clinical) benefits and costs for a two months period. Improved diagnostic policy The AID stewardship model Active involvement of the multi disciplinary stakeholders improved open discussion and has shown to be important for creating hospital-broad awareness and support. Improved diagnostic policy involves not only an Antimicrobial Stewardship Program (ASP), but also an Infection prevention Stewardship Program (ISP) and a Diagnostic Stewardship Program (DSP). Besides, since the sensitivity of commercial assays approach the quality of Laboratory Developed Tests, we introduced the €hr concept (comparable with kWh), to represent the value of POIT in patient care. Patients with a suspected respiratory viral infection appearing at the emergency department during the respiratory season: The improved clinical outcome resulted in: Less unnecessary isolations Less nosocomial infections Sample collection in early triage and dispatch to lab Mean turnaround time from 19 hours to 1 hour No incremental costs Fig 1b Figure 1a Multi stakeholder platform, including the ASP, ISP and DSP, with effective diagnostics as a solid base. Figure 1b Optimal diagnostic policy includes: quality, time and cost, merged in the €hr concept. A that improved the patient outcome. Besides, it helps to keep control of antibiotic resistance. Figure 2 Routing as intended in the improved diagnostic policy Fig 1a The total turnaround time decreased significantly to a mean of 3 hours, which contributed to: Improved (preliminary) diagnosis More adequate therapy € 175,000* € 40,000* I Furthermore, cohorting of patients leads to a huge improved bed management. A slight increase of costs at the division of clinical virology due to: Extended service € 10,000 Increased number of tests performed € 40,000* D * Preliminary calculations Performing the random access commercial test Mean turnaround time from 17 hours to 2 hours Laboratory hands-on time: from 5 hours to 5 minutes Financial benefit per patient tested: €135 * 33h = 4,455 €hr Figure 3 hospital broad benefits exceeded incremental costs for POIT diagnostics Conclusions Our co-creative approach resulted in a new hospital broad policy, which includes an optimal implementation of POIT for the detection of respiratory viral infections. This policy increases the value of molecular diagnostic testing for respiratory viruses with respect to patient safety, therapy, and infection control, which is reflected by applying the AID stewardship model and by combining time and cost in the €hr concept. Hospital broad financial benefits in only the first two months were estimated to be at least €160,000, which makes the implementation of POIT in the respiratory season to be very cost-effective. Contact: medicalmicrobiology.eu
© Copyright 2026