Sudden Infant Death Syndrome Betty Connal, RN, MS SIDS Mid-Atlantic
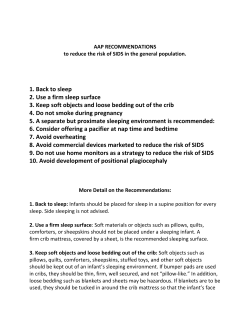
Sudden Infant Death Syndrome Betty Connal, RN, MS SIDS Mid-Atlantic 2700 S. Quincy St. Suite 220 Arlington Va 22206 703-933-9100 [email protected] www.sidsma.org Definition The sudden death of an infant under 1 year of age, which remains unexplained after Thorough case investigation Complete autopsy Death scene investigation Review of the clinical history Alexandra Facts About SIDS SIDS is the leading cause of post neonatal infant death (AAP, 2000). About 4500 infants in the US die of sudden infant death annually, ½ SIDS ½ “other” 8% of all infant deaths are now due to SIDS. Virginia had 90 SIDS and 13 undetermined sudden infant deaths in 2005, increased from 79 SIDS in 2004 Other deaths due to suffocation or strangulation, infection, anything not expected Maryland had 64 SIDS deaths in 2004, DC had 9 Facts About SIDS No one can tell in advance which babies will die – SIDS cannot be predicted SIDS babies do not appear severely ill Some appear to have mild URI before death, but infections are not found on autopsy SIDS cannot be prevented Facts About SIDS 91% of SIDS deaths occur before 6 months of age Peak is between 2-4 months of age African American infants are nearly 2 ½ times more likely to die of SIDS than white infants. Gene has been identified in black baby boys. Brenna Facts About SIDS Almost always occurs when the infant is asleep SIDS is not Caused by immunization Contagious The result of neglect or abuse Which Babies Are at Greatest Risk? Infants who sleep in the prone position Premature infants and/or low birth weight infants (under 1000 grams) Infants who had prenatal nicotine exposure Infants with prenatal illicit drug exposure Brycen Which Babies Are at Greatest Risk? Infants who sleep on soft bedding Male infants African Americans and Native Americans Infants of mothers with late/no prenatal care Overheated infants Infant of young mothers (under age 20) SIDS Statistics 80 70 60 50 40 30 20 10 0 1.4 1.2 1 0.8 0.6 0.4 0.2 0 1992 1993 1994 1995 1996 1997 % Babies Sleeping on Stomach SIDS rate per 1000 live births Chloe SIDS vs. Suffocation Triple Risk Model Highest risk for SIDS Vulnerable Infant Critical period of development Exogenous Stressors Christian Some Theories… Researchers have identified that serotonin receptors of the brain are abnormal in SIDS babies Abnormal response to hypoxia, putting an infant at risk for sudden death during sleep This area of the brain regulates respiration, temperature, blood pressure, heart rate Some Theories Why does the prone position carry such a high risk for SIDS? Babies sleeping on their stomachs have lower blood pressure, higher heart rate and body temperature This leads us to believe that there is some degree of vasomotor instability in the prone position Arousal may be diminished in the prone position Colin More Theories Babies in a risky environment (soft bedding) may be rebreathing CO2 Babies who have their heads covered with blankets, may have a 300% rise in their thermal resistance, causing a lethal rise in brain temperature Some babies may die from cardiac arrhythmias – long QT Syndrome Recommendation from European Union that all babies have EKG at about one month. Cost effective and could save about 250 European babies’ lives per year Nicotine Exposure Nicotine is used in 12.5% of all pregnancies in the US (DHHS, 2004). Nicotine is a neuroteratogen Causing cell damage/deficits in cell number May shut off the fetal response to hypoxia before the adult mechanisms can take over Babies may have a blunted response to hypoxia Exposure to passive smokers also increases the risk in a dose-dependent manner (Flemming, et. al, 2000) Kylie African American Infant Mortality A gap in knowledge about SIDS and SIDS risk reduction among African American mothers 2/3 of the mothers reported they were not aware of sleep position recommendations before their baby died Rate of SIDS is 3X higher in African American infants than white infants Data is from Chicago Infant Mortality study – unpublished as of 7/2001 CPSC Findings Only 31% of African American parents surveyed put babies on their Backs to Sleep 80% of all parents put babies on their Backs to Sleep Ethan CPSC Data Some 900 deaths a year attributed to SIDS may be soft bedding deaths In 30% of these deaths, the infants nose and mouth were covered in soft bedding 23 soft bedding deaths in Virginia in 2003 Diagnosis subjective ☺ A change in retail practices began in the spring of 2000 Child Care Providers About 18% of SIDS babies die while being cared for by a child care provider Statistically, only 9% of SIDS should occur in child care Half die in the first week of child care (Moon, 2000) Lily Why do so many babies die in child care? Many of these infants are sleeping prone Some of these infants are not used to sleeping on their stomachs Child care providers don’t know about back sleeping or don’t believe it works Parental request Inexperienced Prone Sleeping Recent studies suggest that infants unaccustomed to prone sleeping are at a greatly increased risk (up to 20 X) for SIDS when they are placed prone or roll to prone position during sleep (Mitchell, 1999)(Moon, 2000) Side sleeping may pose a risk, as the position is unstable; the infant may role to prone Hannah A Little History In the early 1990’s researchers identified the prone sleep position as a risk factor for SIDS In 1992 the American Academy of Pediatrics (AAP) recommended that infants sleep on their back or side In 1996, the AAP modified their earlier statement on sleep position and recommended back sleeping for all healthy infants In 2005, AAP made new recommendations to prevent SIDS Modifiable Behaviors That Reduce the Risk of SIDS Back sleeping – infants who sleep on their backs are 3 times less likely to die from SIDS than those who sleep on their stomachs They are also less likely to overheat, rebreathe CO2 and have more arousals during sleep Advise parents not to smoke around their baby Five A’s of Smoking Cessation The evidence-based intervention for providers to help their pregnant smokers quit is based on the following five steps (the "5 As"): 1. ASK – 1 minute: Ask patient about smoking status. I have NEVER smoked, or have smoked LESS THAN 100 cigarettes in my lifetime. I stopped smoking BEFORE I found out I was pregnant, and I am not smoking now. I stopped smoking AFTER I found out I was pregnant, and I am not smoking now. I smoke some now, but I cut down on the number of cigarettes I smoke SINCE I found out I was pregnant. I smoke regularly now, about the same as BEFORE I found out I was pregnant. 2. ADVISE – 1 minute Provide clear, strong advice to quit with personalized messages about the impact of smoking on mother and fetus Five A’s 3. ASSESS – 1 minute Assess the willingness of the patient to make a quit attempt within the next 30 days 4. ASSIST – 3 minutes + Suggest and encourage the use of problem-solving methods and skills for cessation. Provide social support as part of the treatment. Arrange social support in the smoker’s environment. Provide pregnancy-specific, self-help smoking cessation materials. 5. ARRANGE – 1 minute + Periodically assess smoking status and, if she is a continuing smoker, encourage cessation. Modifiable Behaviors That Reduce the Risk of SIDS Eliminate soft bedding and blankets from cribs Consider using a blanket sleeper or sleepsack as an alternative to blankets If using a blanket, use a thin one and tuck it around the mattress so it reaches only as far as the baby’s chest No stuffed animals or pillows in cribs HALO Sleepsack Modifiable Behaviors That Reduce the Risk of SIDS Remove bumper pads from cribs Avoid over bundling babies Make sure pregnant women receive good prenatal care Advise caretakers that babies should sleep on their backs Joseph Safe Sleeping Environment What About Aspiration? 52% of all parents surveyed by the CPSC feared babies would choke in vomit if placed on their backs Babies are NOT more likely to choke while sleeping on their backs! What About Aspiration? According to the AAP “there is NO evidence of an increase in aspiration or increased complaints of vomiting since the incidence of supine sleeping has increase dramatically” (AAP, 2000). There is also some “direct and indirect evidence that infants who vomit are at greater risk of choking if they are sleeping face down” (AAP, 2000). Plagiocephaly a.k.a Flat Heads Sleep position and SIDS There are concerns about head asymmetries in babies who sleep on their backs Encourage parents to give baby SUPERVISED tummy time when awake Babies only need to be on their backs for naptime and night-time sleep Lucas Bed Sharing Deaths from suffocation have increased as SIDS deaths decreased Bed sharing is NOT protective against SIDS The AAP discourages bed sharing 20% increase in infant deaths when bedsharing especially if father or sibling in bed Bed sharing confers a higher risk of SIDS when Parents smoke and bed share. Co-sleeping means baby in same room as parents, not same bed. Co-sleeping is safest for baby NO SMOKING! Or drinking, or drugs Bed Sharing There are also hazards in adult beds and some risk of overlay deaths in certain situations: People using drugs or alcohol while bed sharing If the baby slips under the covers, under pillows, becomes trapped between the mattress and bed frame, is rolled on, or becomes overheated Bedsharing TJ AAP Guidelines 2005 Infants should be put to sleep on their backs every time Use a firm crib mattress and a snug fitting crib sheet Keep soft objects and loose bedding out of the crib. No pillows, quilts, comforters, sheepskins or stuffed toys. AAP 2005 Do not smoke during pregnancy and avoid exposing babies to second hand smoke Offer the baby a pacifier at nap time and bedtime. Do not reinsert the pacifier once the baby falls asleep. Pacifier use should begin once breast feeding is well established, and it needs to be consistent Infants should be lightly clothed for sleep. Bedroom temperature should be comfortable for a lightly clothed adult. AAP 2005 Avoid commercial devices marketed to reduce the risk of SIDS, like wedges and positioners. None has been shown to be safe or effective. Parents should not share their bed with the baby during sleep Home monitors do not reduce the risk of SIDS. Positioning Device Do not use. Unnecessary and may be harmful. AAP 2005 Avoid positional plagiocephaly (flat heads) by encouraging “tummy time” Babies should not spend excessive time in car seat carriers and bouncers. SIDS in Your Practice? Provide parents with names and numbers of support groups in the area Have someone review the autopsy with the parents – if they desire Don’t be afraid to say the baby’s name Expect these parents to need extra support upon birth of subsequent children Considerations for Subsequent Children Expanded newborn screening Virginia tests for 29 disorders as of March 2006 Testing for long QT syndrome No smoking and safe sleep Monitors for preemies with apnea or for parents’ peace of mind Hayley Expanded Newborn Screening Virginia tests for 29 disorders Pediatrix screening 55 disorders for $49.50 45 disorders for $24.50 1-866-463-6436 Mayo medical laboratories 35 disorders for $50 1-800-533-1710 ask for supplemental newborn screen, MML test # 82594 NewScreenTM 55 disorders for $98.50 1-800-747-3319 Baylor medical center over 30 disorders for $25 1-800-422-9567 Reduce The Risk Back is best—in baby’s own crib Advise pregnant women not to smoke Learn Five A’s Method Advise parents to avoid second hand smoke exposure around baby Remove soft bedding from crib Avoid overheating baby Give baby supervised tummy time when awake Kylie’s Playground Step 1: Baby is placed on back to sleep when in open crib or one week prior to going home. Step 2: Do not bundle baby while asleep or keep the room too warm The best temperature is 65-71 degrees. Do not put loose bedding, bumper pads or stuffed toys in the crib. Step 3: Baby can be on tummy for playtime while always being watched. Step 4: Parents need to tell all caregivers that baby sleeps on back only. Step 5: Home should be smoke free. Questions? SIDS Mid-Atlantic 703-933-9100 Websites www.sidsma.org WWW.AAP.org WWW.firstcandle.Org WWW.cjsids.com www.asip1.org www.sidsresources.org www.marchofdimes.com New Logo for Brisan References American Academy of Pediatrics Task Force on Infant Sleep Position and Sudden Infant Death Syndrome. (2000). Changing concepts of sudden infant death syndrome: implications for infant sleeping environment and sleep position. [on-line]. Pediatrics, 105, (3), 650-656. Hudson Mohawk SIDS Affiliate. (1998). Reducing the risk of SIDS: what public health nurses need to know. Kemp, J. S. & Thach, B. T. (1995). Quantifying the potential of infant bedding to limit CO2 dispersal and factors affecting rebreathing in bedding. American Physiological Society, 740-745. Lockridge, T., Taqino, L. T., Knight, A., (1999). Back to Sleep:Is there room in that crib for both AAP recommendations and developmentally supportive care? Neonatal Network, 18 (5), 29-31. References Moon, R., (2000). Answering medical questions about SIDS. Presented at the National SIDS Alliance Conference, Salt Lake City, Utah. Willinger, M., Ko, C. W., Hoffman, H. J., Kessler, R. C., Corwin, M. J. (2000) Factors Associated with caregivers’ choice of infant sleep position, 1994-1998. JAMA, 283 (16), 2135-2142. Zeskind, P. S., (2000). Maternal cigarette-use during pregnancy disrupts rhythmic activity in fetal autonomic regulation. Presented at the National SIDS Alliance Conference, Salt Lake City, Utah
© Copyright 2026