T Spring 2009 A Quarterly Informational Publication for EMS Providers
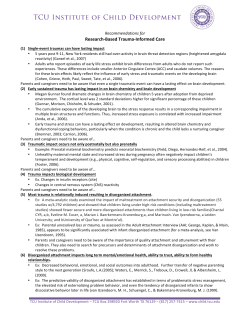
Spring 2009 A Quarterly Informational Publication for EMS Providers What’s Inside: PAGE 3 EMS SERVICE SPOTLIGHT Rothschild Fire and EMS 4 E M S C O O R D I N AT O R U P D AT E S 6 F E AT U R E S T O R Y Spirit Medical Transportation Services Marks 15th Anniversary 7 N C R TA C U P D AT E S What is the RTAC’s Role in Reviewing EMS Trauma Care 8 Trauma Care Through a Lifetime 9 T R A U M A E D U C AT I O N Alcohol and Trauma 9 Safety is Not by Accident 10 F O R Y O U R I N F O R M AT I O N Everyone Goes Home 11 P O S T - T E S T FOR C O N T I N U I N G E D U C AT I O N 12 U P C O M I N G E V E N T S From the Director’s Chair Trauma in the Pregnant Patient This knowledge should be tempered by the fact rauma is the leading that pregnant women may appear stable but have cause of death in Twomen injuries that place the fetus at risk. With any of child bearing age and the leading cause of death during pregnancy. Common causes of trauma deaths in this patient population include MVA (55%), falls (22%), assaults (22%), and burns (7%). Pregnancy is divided into three trimesters; each trimester is three months, with a normal pregnancy lasting nine months, from conception to delivery. It is important to know how far along the patient is in her pregnancy as this determines the risks and types of injuries, exam findings, and patient management decisions. There are significant physiologic changes that occur in women during pregnancy. Late in the second trimester, baseline blood pressure typically drops by 5 to 15 mmHG. This is accompanied by a 10 - 15 percent increase in heart rate and an increase in maternal blood volume. The combination of relatively low blood pressures with tachycardia often misleads the EMS provider to assume the patient is in shock when in fact these can be normal vital signs late in pregnancy. maternal injury resulting in significant blood loss, blood flow is shunted away from the fetus in an effort to compensate for the maternal blood loss. More than one million women are victims of domestic violence in the U.S. every year; 10 - 30 percent of these women are pregnant and in the first four to five months of their pregnancy. Common injuries include blunt trauma to the head, neck, breasts and abdomen as well as penetrating injuries from gunshot and knife wounds. Injuries from falls are more common in the second and third trimester due in large part to the change in the mother’s center of gravity of her body as the uterus enlarges to accommodate the growing fetus. Initial management of the pregnant trauma patient is no different than any other trauma patient. After evaluating and correcting any problems with airway, breathing, and circulation, the patient should be fully exposed and the secondary exam should be performed, preferably by a female EMS provider. If the patient is of child bearing age, ask if she is pregnant, and if so, how far along she is in her pregnancy. As a general rule, women that are more than 24 weeks into their pregnancy are considered to have a fetus that Continued on page 2. C O N TA C T I N F O R M AT I O N V ital Connections is a shared effort of Saint Joseph’s Hospital and Saint Joseph’s Children’s Hospital in Marshfield and Saint Clare’s Hospital in Weston. This quarterly publication serves to provide readers with information on current EMS topics and issues. It is our combined hope to continue to bring you an informative newsletter that will reflect expertise, knowledge, technology and EMS information from both facilities. As always, we invite your comments and/or suggestions for improvement. You can contact us via the various resources listed below. If you have questions, concerns or ideas/information for articles in future publications, or if you would like to be added to our mailing list, please contact either Sandy or Don via the contact information provided below. Please include your name, mailing address, phone number, e-mail address (if applicable), service affiliation, and level of provider. Sandy R. Johnson, RN, NREMT-P EMS Coordinator Saint Joseph’s Hospital 611 Saint Joseph Avenue Marshfield, WI 54449-1898 From the Director’s Chair Trauma in the Pregnant Patient (continued) could survive a premature delivery if necessary, due to maternal injuries. This is critical information to relay to the emergency department so that an obstetrician can be involved early in the care of the pregnant trauma patient. The uterus is protected by the pelvis during the first 12 weeks of pregnancy. As the uterus continues to grow to accommodate the enlarging fetus, it becomes an abdominal organ and is susceptible to blunt trauma from falls and MVA and penetrating injuries. Attempt to palpate the uterus. Is the uterus tender, rigid, are there contractions? Document these findings. All pregnant trauma patients should be placed on high flow oxygen; this will benefit both the mother and the fetus. Pregnant patients beyond 20 weeks gestation that are placed supine can experience a drop in blood pressure from the weight of the uterus and fetus collapsing the mother’s large vessels 14th Annual Spirit Medical Transportation Services Conference 2009 What’s Hot and What’s Not in Trauma OFFICE: 715.393.2945 [email protected] FAX: 715.393.2905 2 With knowledge of the types of injuries during different stages of pregnancy and specific pre-hospital management unique to pregnant trauma patients, the EMS provider can provide optimal care for both mom and the baby. Steven H. Mickel, MD Medical Director, Spirit Medical Transportation Service, Marshfield Base Save the Date! Thursday, August 13 and Friday, August 14 Ramada Inn Stevens Point, Wisconsin For additional information, please contact: Audrey Schmeeckle, conference coordinator, at [email protected] OFFICE: 715.387.7995 [email protected] FAX: 715.389.4030 stjosephsmarshfield.org/ems Don Kimlicka, NREMT-P, CCEMT-P EMS Coordinator Saint Clare’s Hospital 3400 Ministry Parkway Weston, WI 54476-5220 that return blood from the lower half of the body to the heart. For this reason, pregnant patients in their late second or third trimester should always be transported on cots in the left lateral decubitus position. If the patient has been immobilized, the spine board should be tilted at least 15 degrees to the left. Both these measures will improve circulation and blood pressure. Contracted Partner of Spirit Medical Transportation Services Spring 2009 E M S S E R V I C E S P O T L I G H T Rothschild Fire and EMS Leah Toboyek, CCEMT, Paramedic, Spirit MTS Weston Base Glen Engebretson, EMT, Driver-Spirit MTS, Assistant Chief, Rothschild Fire Dept T he Rothschild Fire/EMS Department is located off of Grand Avenue in the Village of Rothschild. The service covers approximately 27 square miles within the Village of Rothschild and provides mutual aide to surrounding departments when requested. The fire department was organized in the early 1900s and started with about 15 men. The equipment consisted of a cart on wheels and a hose. In 1944, first aid was instituted in the fire department and was the standard until the first EMT class. A few members of the Rothschild Fire Department attended the first class that was held in Wausau. Some of the state EMT license numbers below #20 were held by members of the department. EMT #1282 is still currently with the department. Currently, the department has 36 members, of which 29 are EMT-Basic or EMT-IV Tech. They have several fire apparatus as well as two ambulances, and are expecting delivery of a new Med-Tech ambulance in March as well as a new Pierce fire engine sometime this summer. The service went IV-Technician in 2005. Prior to that, they provided Basic EMS. The service transports patients to Saint Clare's Hospital and Aspirus Wausau Hospital. Their medical director is Michael Curtis, MD, from Saint Clare's Hospital. Rothschild EMS was the first ambulance service to bring a patient to Saint Clare's Hospital on the day it first opened on October 4, 2005. The members of the Rothschild Fire/EMS Department are paid on-call with the exception of Monday through Friday, from 8 a.m. – 4 p.m. During these hours, there is a crew at the station consisting of two EMTs (one of which is IV-Technician). Members of the department participate in many community-based events/fundraisers, including the Annual Semi-pull Fundraiser at Cedar Creek, Badger State Games and Annual MDA Motorcycle Ride Fundraiser. They also host an open house annually at their station. For more information on Rothschild Fire & EMS, please call 359.3660 or email [email protected]. SAINT JOSEPH’S HOSPITAL EMS Appreciation Event May 19, 2009 6 p.m. Dinner • 7 – 9 p.m. Guest Speaker Mother Francis Streitel Conference Center – Saint Joseph’s Hospital Marshfield, Wisconsin “I Believe … Lessons I’ve Learned in 30 Years of EMS” Dwight Polk is the paramedic program director at the University of Maryland Baltimore County (UMBC) in Baltimore, Maryland, and is a familiar face at conferences around the country. Along with being a full time educator, he is a volunteer paramedic and co-author of Jones & Bartlett’s Prehospital Behavioral Emergencies and Crisis Response. Additionally, he has written for JEMS magazine, publishing several articles on mental illness. Dwight has a master’s degree in occupational social work and is a crisis counselor for the Grassroots Crisis Center in Columbia, Maryland. He is also a mental health professional on the Baltimore City Fire Department and Maryland Department of Natural Resources Critical Incident Stress Management (CISM) teams. Dwight shares with you some of his experiences and the lessons he has learned (often the hard way) after 30 year of experience in EMS. This humorous and thought-provoking presentation will have you nodding your head and saying, “Yep, I’ve seen that…” Saint Joseph’s Hospital salutes our local and area EMS providers for their expertise and excellent care given to our patients, 24 hours a day, seven days a week. Join Us For An Evening of Celebration! Look for your invitation in the mail! 3 E M S I s your EMS service prepared to handle the impact of a pandemic disease outbreak? We hear this word “pandemic” frequently in the news, we read about it in magazines and listen to experts debate about the effect of a pandemic on society. According to the World Health Organization (WHO), a pandemic can start when three conditions have been met: 1. The emergence of a disease new to a population. 2. Infectious agents infect humans, causing serious illness. 3. Infectious agents spread easily and are easily sustained among humans. An epidemic is a contagious disease that spreads rapidly and extensively among many individuals in an area. In contrast, a pandemic is an epidemic that is spread over an especially wide geographic area, for instance a continent, or even worldwide, and comes from the Latin word, pandemies meaning “of all the people.” This is the very reason that pandemics can be so deadly and disruptive to society. There are numerous accounts of epidemics and pandemics throughout history caused by various infectious agents: typhus, smallpox, cholera, typhoid fever and pandemic flu, just to name a few. Seasonal flu should not be confused with pandemic flu. Seasonal flu is a respiratory illness that most people have some immunity to, either through exposure or vaccination. Seasonal flu may infect large numbers of people, but is only generally lifethreatening to the very old and the very young and has an overall low mortality rate. The first pandemic flu, recorded in 1510, traveled from Africa, and spread across Europe. Flu pandemics have happened before, including three during the 1900s. The “Spanish Flu” was first identified in March 1918, in U.S. troops training at Camp Funston, Kansas. By October 1918, it had spread to become a worldwide pandemic on all continents, and eventually infected 2.5 - 5 percent of the human population. In six months, some 50 million were dead; some estimates put the total number of those killed worldwide at over twice that 4 number, which included 675,000 in the U.S. The second pandemic, the 1957-58 “Asian Flu,” caused about 70,000 deaths in the U.S., and was first identified in China in 1957. The third pandemic to hit the U.S. was the “Hong Kong Flu” in 1968-69. This virus was detected in Hong Kong in early 1968 and spread to the U.S. later that year, causing about 34,000 deaths. Because flu viruses are always changing, scientists are positive that another flu pandemic will happen, although they cannot say for sure when it will happen. Nor can they tell how severe a pandemic will be, as it depends on the exact strain of the virus and how much can be done to prevent the spread of the disease. In February 2004, avian influenza virus was detected in birds in Vietnam, increasing fears of the emergence of new variant strains or types of the virus. It is feared that if the avian influenza virus combines with a human influenza virus, (in a bird or a human), the new subtype created could be both highly contagious and highly lethal to humans. By November 2007, numerous confirmed cases of the avian flu strain had been identified across Europe; however, by the end of October, only 59 people had died as a result, which is atypical of previous influenza pandemics. To date, avian flu cannot be categorized as a pandemic, because the virus cannot yet cause sustained and efficient human-to-human transmission. Cases so far are recognized to have been only transmitted directly from bird to human. Taking a look at our history can give us the advantage of planning for our future. Other than the obvious human suffering and loss of life that is inevitable in a pandemic, we need to consider the other life-altering effects that a pandemic will have on society. Communities may need to take public measures to prevent the spread of the virus. These measures could include closing schools and business, and placing limits on travel and large gatherings. Businesses should plan for up to 40 percent of their workforce being absent due to sickness or having to care for family members. Hospitals and other health care centers may be overwhelmed with patients. There may not be enough supplies and medications on-hand. Health care workers may be absent due to illness or the need to care for family members. C O O R D I N A T O R There may be a need for quarantines or selfisolation of infected persons—who will care for them? There is real concern that public services such as electricity, water, food and gasoline could be disrupted due to the shortage of healthy workers. Ethical dilemmas and issues regarding civil liberties will flourish. What can EMS do to prepare for pandemics? Know that the Wisconsin Health Department and public health officials throughout the U.S. are focusing efforts on ways to detect the virus early and prevent the spread of the disease, which will help to limit the number of those exposed. Proper planning strategies for a flu pandemic are mandatory to achieve the greatest good for the greatest number of patients. EMS leaders will have to plan and make adjustments in their system to maintain service to the community because EMS is a critical element that must remain in operation. Without sufficient planning and established protocols in place prior to any events, EMS systems may fail their communities in their time of greatest need. To that end, the Department of Health and Human Services (HHS) and the Centers for Disease Control and Prevention (CDC) have developed a checklist to help EMS assess and improve its preparedness for responding to pandemic influenza. EMS will be involved in the care and transport of acutely ill patients with known or suspected pandemic influenza to emergency departments. This checklist identifies key areas for pandemic influenza planning. EMS can use this tool to self-assess and identify strengths and weaknesses of current planning. The list is comprehensive, but not all-inclusive, and each EMS organization will have unique and unanticipated concerns that will also need to be addressed. Collaboration among EMS, hospital, public health and public safety personnel are encouraged during all phases of preparedness planning. This checklist can be found at hhs.gov/pandemicflu/plan/sup3.html#app2 Additional information regarding pandemic flu in general can be found at pandemicflu.gov Spring 2009 U P D A T E S Pandemic flu preparedness is also taking place at the state level, according to Dana Sechler, paramedic program coordinator, Bureau of Local Health Support and EMS. Sechler states, “The Wisconsin Department of Health Services, Division of Public Health has identified coordination with EMS as a high priority in planning for an influenza pandemic. The goal is to improve preparedness for responding to pandemic influenza by involving EMS, to establish protocols for triaging patients and to ensure that EMS staff is protected in a pandemic. Since EMS organizations will be involved in the transport of acutely ill patients with known or suspected pandemic influenza to emergency departments or alternate care sites, it is essential that EMS organizations be involved in pandemic influenza planning efforts.” Sechler continues, “In addition, the EMS section has begun the process of identifying how EMS organizations can assist in aiding the public health sector, should an influenza pandemic occur. The EMS office staff recently approved two pilot projects which allowed EMTs and paramedics to receive training and education, and work in partnership with their local county health department in administering flu vaccinations. The data from the pilot is still being collated, but the preliminary results appear to be quite positive.” For more information about the pilot projects, or pandemic-related information for EMS providers, please contact any of the following individuals: • Brian Litza, EMS Section Chief, at [email protected] • Dana Sechler, Paramedic Program Coordinator, at [email protected] • Paul Wittkamp, Communications Coordinator, at [email protected] Do not be caught off-guard when pandemic flu hits. Take the time to collaborate with key resources within your community now, in order to get your pandemic protocols/procedures in place. Once your plan is in place, consider conducting a tabletop exercise to test the strength and effectiveness of your efforts. Learn from the past, plan for the future. Sandy R. Johnson, RN, NREMT-P EMS Coordinator, Saint Joseph’s Hospital, Marshfield Sources: CDC.gov, Wikipedia, WI Department of Health and Family Services. S afety is an important component of our lives every day. The best safety measure is to avoid a situation before it happens. This can be accomplished through many methods, including preventive measures or preplanning. In emergency services, safety is strongly emphasized, from before the call until the return to your facility. Just as in our personal lives, safety begins with prevention and preplanning. An important area that has recently come to our attention is the use of red lights and siren (RLS). The question is, “Does running RLS truly make a difference?” Research reveals that RLS was originally added as a way to get the patient to the hospital quicker. This was before the day of trained EMTs who provided life saving or stabilizing measures. With our ability to bring significant care measures to patients, is it prudent to run emergently with red lights flashing and the siren blaring? The State of Wisconsin EMS Advisory Board recently adopted a position on this topic. The recommendation is that the use of RLS should be avoided as often as possible and reserved for unstable medical conditions. At that point, it’s reasonable to believe that their use will lead to a clinically relevant time saver, to delivery, to definitive care. Furthermore, patient care goals are outlined: • Identify patients for whom using RLS can potentially reduce morbidity and mortality. • Eliminate unnecessary use of RLS to improve patient comfort, reduce anxiety and enhance safety. The position also outlines a suggested procedure list: • RLS transport does not necessitate exceeding posted speed limits. • Road type, traffic and weather conditions must always be considered when using RLS • When approaching an intersection, the unit should come to a complete stop, regardless of traffic control devices present on the unit or when the unit has an apparent right of way. • When using RLS: - Never pass in a no-passing zone unless a vehicle is well over on the shoulder and comes to a complete stop. - Come to a complete stop 100 feet in front or behind a school bus with flashing lights activated. - Never force the right of way or assume you have the right of way. - Never tailgate another vehicle even if they have not moved to the right or come to a stop. • Specific medical or trauma conditions are outlined primarily with unstable cardiac, respiratory, trauma or neurological patients. • Transports where reducing time to definitive care is clinically indicated, consider all options before using RLS. • Critical care or inter-facility transports should not automatically indicate RLS use. • When there is a conflict of use between an on-board physician or nurse, attempt to resolve the issue or utilize Medical Control. • RLS should be avoided in DNR patients, inter-facility transports to a lower level facility, transport of human organs, blood or transplant teams, and unsalvageable patients. This position was drafted from a position statement released by the National Association of Emergency Medical Services Physicians (NAEMSP) back in November 1993, and can be found at: naemsp.org/documents/ UseWarnLightsSirens.pdf The Wisconsin EMS Association also released a position statement on emergency driving, which includes use of RLS which can be found at: wemsa.com/docs/ Emergency%20Vehicle%20Operations.pdf As you can see, this is an area of great concern. Now would be the perfect time for your service members to sit down with your medical director and consider developing a policy. Please contact me or Dr. Michael Curtis if you need more information or assistance. Don Kimlicka, NREMT-P, CCEMT-P EMS Coordinator, Saint Clare’s Hospital, Weston 5 Spirit Medical Transp th Marks 15 Anniversa Spirit N611SJH taking off from Saint Joseph’s Hospital. I n November 1993, Ministry Health Care launched Spirit Medical Transportation Services to provide ground and air medical transport services to the people of central and northern Wisconsin. Last year marked the 15th anniversary of its founding and a long history of service to the region. Spirit Medical Transportation Services’ mission is to provide comprehensive, regionally-integrated ground and air transportation for adult, pediatric, neonatal, and high-risk obstetrical critical care patients from referral institutions and scenes of injury. Spirit Medical Transportation Services was started in Marshfield at Saint Joseph’s Hospital, and as the service has grown, it has evolved into a comprehensive Ministry service with ground bases in Weston, Woodruff and Rhinelander. Providing interfacility transportation for patients requiring advanced life support (ALS) or critical care management to or from tertiary hospitals is of particular importance, and is one of the primary reasons Spirit services is are needed. Spirit Medical Transportation Services was also designed to support, supplement, and assist local and regional ambulances and other emergency services that play the initial key role in any emergency medical transport. Nurses and paramedics staff the helicopter and each of the ground ambulance bases. Transport nurses have several years of critical care and emergency department experience. Our paramedics are welltrained in critical care and advanced skills and also have several years in emergency medical services. On average, the Spirit helicopter flies over 600 missions a year, while the ground 6 Ground units based in Marshfield at Sa Key Facts About Spirit Medical Transportation Services: transport teams average over 2,900 calls. The combined team provides the most comprehensive medical transport service in the region. High-risk newborns that need specialized care and treatment are often transferred to Saint Joseph's Hospital Level III NICU. For these transports, the Spirit Medical Transportation Service crew is joined by a neonatal transport nurse and respiratory therapist. This team has advanced training in the stabilization and care of critically ill neonatal patients during transport. This team effort of more than 100 employees i *comprised of Medical Control Physicians, nurses paramedics, EMTs, pilots, ambulance drivers, communication specialists, support staff and mecha * Top transport types are cardiac, medical and trau * Covers a 35-county radius. * Average flight run is 1.25 hours. can travel between 130 - 160 mph * Helicopter under normal flight conditions, with an average speed of 145 mph. Looking back over the 15-year history of the program, Saint Joseph’s Hospital Executive Vice President Terri Richards noted, “Our program has grown to continue to meet the needs of our communities with a highly skilled team that pays special attention to safety. The Spirit crews demonstrate every day our commitment to quality and the highest level of patient care.” The 15th anniversary will be celebrated with a variety of events and activities across the region. As the anniversary year comes to a close, the program will take ownership of the new American Eurocopter EC145 helicopter, one of the most advanced airships in service for medical transportation today. Mock Farm accident scene working with the Pittsville Fire Department. Sp Spring 2009 portation Services ary N C R TA C U P D A T E What is the RTAC’s Role in Reviewing EMS Trauma Care? Michael Fraley, BS, NREMT-P, NCRTAC Coordinator O ccasionally I get calls or emails asking me if the RTAC should review a particular pre-hospital call. My response is usually, “What does your service normally do to review calls?” int Joseph’s Hospital. Spirit crew loading a patient for transport. is s, nics. uma. Weston ground unit outside Saint Clare’s Hospital. Captain Nils Strickland Night time shot after snow fall Marshfield base. Spirit crew member working with a pediatric patient. pirit crew members rushing a patient into the Emergency Department. A well-publicized, tragic event is not the best time to start a Process Improvement (PI) program. A better option is having a PI plan already in place and reviewing calls based on set inclusion criteria, not just because it seems like a particular call should be under the spotlight. Doing this tends to put the participants in a defensive “What did we do wrong?” mindset rather than viewing it as “How can we improve our system?” The RTAC’s PI Committee may provide a forum for doing case reviews, but more importantly, we’ve already provided several tools to individual services to build a PI program. An example of a simple PI program is reviewing all trauma calls using the NCRTAC Trauma and Triage Guidelines to determine if a trauma patient was properly identified as critical or not, and if they were transported to an appropriate level trauma center. From there, you can look at scene times, whether or not ALS or helicopters should have been used, and documentation of important data such as mechanism of injury, a primary survey and initial vital signs, including GCS. The NCRTAC also has a sample PI form available for selective spinal immobilization cases. Others can be developed at your request. A service could also set up criteria to do a more thorough review of a call if it met certain inclusion criteria, such as a trauma death, pediatric patients, etc. Inclusion of your medical director is important. He or she may not be able to review all cases but should be consulted for questionable runs. Services should also have a system to review calls referred back to them by the Trauma Program Manager at the receiving trauma center. All hospitals should be including EMS care as part of their PI processes, and you should be part of the feedback loop. Contact your hospital’s Trauma Program Manager to ask how you can be included. 7 Trauma Care Through a Lifetime Mary Jo Casey, BSN, RN, Trauma Program Manager, and Amy Schmidt, BSN, RN, Pediatric Trauma Program Coordinator The call goes out: car versus deer, vehicular rollover, four occupants. As you respond to the scene, your thoughts are racing as you anticipate what you will discover. Throughout Wisconsin, there are more than 100 hospitals. For trauma care, most are selfdesignated or state designated Level III or IV Trauma Centers. Nine hospitals in Wisconsin are American College of Surgeons (ACS) Verified Level I or II Adult Trauma Centers, providing the highest level of trauma care. Only three hospitals in Wisconsin are Pediatric ACS Verified Trauma Centers— they include Saint Joseph’s Hospital in Marshfield, Children’s Hospital of Wisconsin in Milwaukee, and University of Wisconsin Hospital and Clinics in Madison. Saint Joseph’s Hospital is distinguished in our region as the only ACS Verified Adult and Pediatric Level II Trauma Center. You arrive at the car and find a family— dad, mom, son, and daughter. Dad and son—are un-responsive, the daughter has a deformity to her upper arm and facial bruising, and mom has no apparent injuries. The call is placed for ALS air and ground transport. Ground arrives and transports the daughter and mom to the local Level III Trauma Center. Your assessment reveals both father and son are severely injured and are transported from the scene to Saint Joseph’s Hospital, an ACS Verified Adult and Pediatric Level II Trauma Center. Once there, both adult and pediatric trauma activations are called. You hand off care, your run report is completed, yet the patients’ and family’s stories are just beginning. Decisions made in the field can impact life. The physician’s admission note reads: “Prior to transport, the patient developed signs of respiratory distress with absent breath sounds noted on the right. Needle decompression was performed with improvement in breathing.” 8 Transport decisions made in the field may determine how a family responds and copes. Physical separation of family members creates stress during an already stressful time. If one family must be taken to different hospitals, communication with each hospital about the location of other family members is needed. Thinking beyond the Emergency Department to the long-term needs of the patient and family can positively affect the outcomes for everyone concerned. The father and son are airlifted to Saint Joseph’s Hospital and admitted to the Intensive Care Unit and Pediatric Intensive Care Unit, respectively. Mom alternates between her husband and son’s bedside, only leaving to sleep at the nearby Ronald McDonald House, a facility unique for a rural community. The separation from her daughter is difficult, but mom will be okay. Her husband and son need her more. Her daughter is being cared for by relatives since her discharge from the hospital. Patient care requires more than physicians and nurses. It is a multi-disciplinary team working in unison to provide skilled care and decision-making for successful patient outcomes. Hospital staff provided mom with a journal to keep track of her loved-ones’ progress. One of mom’s journal entries reads: “Today has been hard. Ron was in Physical and Occupational Therapy for what seemed like hours today… Benji’s recovery has been more difficult. He is quiet, only laughing when the Child Life Specialists come to see him. They help distract him from the pain of his injuries.” Trauma patients might require rehabilitation to re-learn and adapt skills within the limits of their injury in order to regain independence and to return to their communities. The days continue and stretch into weeks. Dad has made enough progress to be admitted to the inpatient rehabilitation center. The son, with his severe traumatic brain injury, has a prolonged hospital stay. With intensive pediatric rehabilitation, the son is discharged home with home health and follow-up appointments. Trauma Center staff thinks beyond the Emergency Department, beyond in-patient care, to rehabilitation and integration back into the community. Saint Joseph’s Hospital’s Rehabilitation Unit is accredited by the Commission on Accreditation of Rehabilitation Facilities (CARF) in three areas: adult rehabilitation, child/adolescent rehabilitation, and as a stroke specialty program. Mom’s final journal entry: “I give thanks to everyone who has touched our family and provided the care we needed to go home. Their knowledge and skills saved our family. I give thanks for providing a place for us to be together. I give thanks for life.” Trauma Centers and Emergency Medical Services provide ongoing excellence for patients and communities which they serve. This commitment is shown through education and training. Saint Joseph’s Hospital offers educational classes for EMS, including Pre-hospital Trauma Life Support, Pediatric Education for Pre-hospital Professionals, Spirit Medical Transportation Services Conference, and outreach visits to EMS. Other offerings include Advanced Trauma Life Support and Advanced Trauma Care for Nurses, Trauma Nurse Core Curriculum, Emergency Nursing Pediatric Course and Outreach education, including Rural Trauma Team Development Course and outreach to hospitals. Together; EMS, Ministry Health Care, hospitals, regional and state trauma advisory councils are all part of a trauma system. It’s a system devoted to meeting the needs of the injured patient, from injury prevention through rehabilitation. Spring 2009 T R A U M A E D U C A T I O N Alcohol and Trauma Amy Schmidt, RN, BSN, Injury Prevention/Outreach & Pediatric Trauma Program Coordinator, Saint Joseph’s Hospital Trauma Services It’s midnight and the hospital trauma pager goes off. The activation reads: Level I adult trauma, bay 2, ETA 15 minutes. Nurses responding to the activation look to the board for the patient information, including if alcohol was involved. Not only will alcohol mask the pain from traumatic injuries, it can also delay the identification of injury during the exam. A cervical collar needs to remain in place until the patient is sober, and the intoxicated patient cannot be discharged. Hospital admission for observation is guaranteed. vehicle collisions—consider a potentially intoxicated hypothermic patient. Other sources of alcohol-related trauma are snowmobile collisions, fires and burns, falls, drownings, tree stand falls, suicides, aggravated assaults, and any other source of injury you can imagine. T The respiratory system is also compromised—alcohol can disrupt ventilatory effort, leading to possible interventions. Plus, the gag reflex is depressed, increasing the risk of gastric aspiration. Add sedating medications, and you have a potentially serious situation. How often are trauma patients admitted to the hospital with positive blood alcohol levels? Based on the Saint Joseph’s Hospital Trauma Registry, in 2008, 22.31 percent of adults greater than age 18 had positive blood alcohol levels. he presence of alcohol in a trauma patient is posted not for curiosity, but as a factor in the physical assessment. EMS is the first line of patient care. Information that assists in guiding the trauma resuscitation includes history, interventions, and mechanism of injury. Early suspicion of alcohol use will also assist in guiding the initial assessment, and will impact the patient’s hospital stay. What can alcohol do? It can mask injuries. Belligerence and noncompliance may be attributed to alcohol, yet these are also signs of a head injury. A change in mental status cannot solely be attributed to alcohol, nor can one say there is no cerebral injury in the presence of alcohol. This necessitates a head CT. Alcohol can adversely affect early physiological responses to injury. For example, the immunosuppressive consequences of alcohol lead to antibiotic use. The impaired cardiovascular response to acute blood loss may lead to more invasive monitoring. Acute alcohol ingestion reduces the electrical threshold (ventricular arrhythmias) and promotes electro-mechanical dissociation (Moore, 2005). Alcohol is involved in more than just motor So what can EMS do? First, consider the presence or suspicion of alcohol as part of the assessment or the mechanism of injury. This is vital information for trauma physicians caring for the patient. Second, make a difference in your community, before the call comes. Consider becoming a voice for injury prevention. Become an agent for change. You may just save a life. Reference: Moore, E. E. (2005) Alcohol and Trauma: The Perfect Storm. The Journal of Trauma Injury, Infection, and Critical Care, 59(3), 53-57. Safety is Not by Accident Deb Martin, RN, MSN, CCRN, CMTE, Flight Nurse, Spirit MTS “…Spirit currently lifting, three souls on board, 1 hour 20 on fuel, enroute to ________ with a heading of ________. Estimated time en route __________...” T his daily verbiage is “normal” in our dispatch center, and is mirrored 24/7 in many communication centers both regionally and across the country. It’s difficult to remember when air medical transport was not an option for rapid transfer of the critically ill or injured. In fact, availability is such that our geographic region is privy to the response of no less than eight different flight programs. While advantageous if needed for multiple/mass response, it also emphasizes the need for vigilant safety practices. Spirit Medical Transportation Services does not take safety for granted, and is proud that thousands of patients have been safely transported since its inception in November 1993. However, we can never assume that safety will “happen on its own.” The recent unacceptable increase in the national air medical accident rate has grasped attention of media, the air medical transport industry, EMS, fire, and law enforcement, governmental agencies, and the public. Numerous meetings and discussions have been held, with inclusion of industry leaders, the FAA, and NTSB. Subsequently, the need for improved technology and reduction in “human error” factors has been identified as initial approaches to decrease known risk. More stringent weather and operational requirements are being integrated by many vendors. Other improvements include advancements in safety-related equipment expected to become standard on newer helicopters. These include but are not limited to: state-of-the-art helicopter terrain Continued on page 12. 9 H E L P F U L W E B R E S O U R C E S F I O R Y O U R N F O R M A T I O N T Everyone Goes Home Wisconsin Department of Health Services, Emergency Medical Services – The majority of questions pertinent to ambulance operations and points of contact in Wis. can be found at this site. dhs.Wisconsin.gov/ems Scott Owen, Deputy Fire Chief, Marshfield Fire & Rescue Department he following is a list of useful e-mail addresses with current application to Emergency Medical Service operations: North Central Regional Trauma Advisory Council – Excellent site to follow the Trauma Advisory Council progress. ncrtac-wi.org Wisconsin Trauma Care System – Includes information about the Wisconsin Trauma System for health care providers, legislators and the public. Trauma brochures, Power-Point presentations, and a White Paper are available for download. wisconsintraumacare.org Wisconsin Department of Transportation – Find Ambulance inspection forms. Trans 309 and other news. dot.wisconsin.gov/statepatrol/inspection/ambulance.htm National Association of Emergency Medical Technicians – Resource site for all EMS levels. Includes links for PHTLS and the AMLS programs. naemt.org National Registry of EMTs – Questions and answers to National Registry issues, as well as exam dates and various criteria for students. nremt.org/about/nremt_news.asp Federal Emergency Management Administration – Source for disaster preparedness and management, current and historical national news. fema.gov American Ambulance Association – Highlights current issues pertaining to ambulances and hospital interaction. the-aaa.org Paramedic Systems of Wisconsin – Provides continuing education for administrators of Advanced Life Support (ALS) ambulance services to share information and work together for the betterment of Emergency Medical Services in Wisconsin. psow.org Wisconsin EMS Association – Represents and supports the views and interests of our membership in Wisconsin communities by promoting education, sharing information and facilitating legislative action. wemsa.com American Heart Association – Main page for all links to the heart association, including guidelines regarding the 2006 changes. americanheart.org National Highway Traffic and Safety Administration (NHTSA) – Resources regarding federal rules for EMS and other traffic programs. EMS is listed under “traffic safety.” nhtsa.dot.gov/portal/site/nhtsa/menuitem 10 T he fire service is filled with myths, both large and small. Often times, we act in unsafe ways because “it’s the way we’ve always done it.” Unsafe myths permeate our business, our tradition, and our culture, passed on from one generation to the next. These myths gain acceptance within our culture because they glamorize what we do. New firefighter students are taught correct and safe ways to operate at fires and emergencies, but often, when they join a department, they’re “reeducated” as to the ways “real firefighters do it.” Of course, they want to fit in and they strive to emulate the perfect picture of fire service strength that the myths perpetuate. And so the cycle continues. Take a minute and think back to when you first started in the fire service. Were you ever told by the other firefighters that wearing your chin strap is dangerous, or that you don’t need to wear seatbelts because they will only slow you down? How about the one about “save your air for when you really need it,” and “don’t put the training fire out, let it burn a little.” Perhaps you heard “real firefighters don’t need all their PPE—your coat and helmet is good enough.” These are just a few items to get you thinking about the way we have done business for many, many years. In no way do I want to take anything away from this great job or its traditions, but I do want to remove the tradition of death and dying in the fire service. We will continue to have an uphill battle if bad information keeps getting passed along from one generation to the next. In 2004, the National Fallen Firefighters Foundation (NFFF) held the first annual Firefighter Life Safety Summit in Tampa, Florida, to address the need for change within fire and emergency services. As a result of this meeting, 16 Life Safety Initiatives were produced to ensure that Everyone Goes Home at the end of the day. It also gave the fire service a blueprint for making changes to reduce the number of preventable firefighter line of duty deaths (LODD). Firefighters must have the courage to face a multitude of risks in order to save lives and protect their communities. Their courage allows them to willingly risk their own lives so that others can be saved. However, a different type of courage is required to stay safe in potentially dangerous situations by avoiding needless risks and tragic consequences. I urge everyone to take a personal inventory of their knowledge and experience base. Are you passing along the bad information and myths? Are you buying into unsafe practices because it makes the job more glamorous, or because “that’s the way it’s always been done?” Are you one of those fire chiefs or line officers that make up the excuses for your crews because of their inadequate skills? We don’t need to make this job more difficult than it already is. By continuing the cycle of safety abuse, we’re helping to ensure that the number Continued on the next page. Spring 2009 Everyone Goes Home of our line-of-duty deaths and injuries also continues. On the face of it, the Life Safety Initiatives are fairly basic. Promoting their value to the fire service should be like selling baseball pitchers on the importance of the curveball and the changeup. But it’s not as easy as that. Few firefighters take issue with the individual Life Safety Initiatives, in concept. While the process of implementing specifics within the Initiatives should yield healthy discussions, the conceptual framework is not P O S T - T E S T (continued) only sound, but practically inarguable. What makes the task of reducing line-of-duty deaths and injuries so challenging is that certain negative behaviors, attitudes, and systems are engrained in many fire department cultures. Our success in reducing deaths and injuries on the job is directly related to our ability to change behaviors and attitudes—to change culture. I encourage all emergency responders, whether fire or EMS, to take the time and visit the Everyone Goes Home Web site at F O R C everyonegoeshome.com and attend one of these firefighter life safety presentations. This program is a must-see for all who care, share, and have a feeling for the safety of all firefighters. For more information, or to inquire about scheduling a training presentation, please contact me at [email protected] or at the Marshfield Fire & Rescue Department at 715.486.2094. Be safe and ensure Everyone Goes Home at the end of the day. O N T I N U I N G E D U C A T I O N The following questions were taken from the various articles in this edition of Vital Connections. Continuing Education Hours (1.5 hours) will be awarded for completing the following post-test. 1. Common injuries in pregnant patients include blunt trauma to the head, neck, breasts and abdomen as well as penetrating injuries from gunshot wounds and knife wounds. True or False 2. Pregnant patients in their late second or third trimester should always be transported on cots in the ____ _______ _________ position. 3. The initial management of the pregnant trauma patient is no different than any other trauma patient. True or False 4. List the three conditions that must be met before a pandemic can be declared: 1._____________________________________________ _______________________________________________ 2._____________________________________________ _______________________________________________ 3._____________________________________________ _______________________________________________ 5. Proper planning strategies for a flu pandemic are mandatory to achieve the greatest good for the greatest number of patients. True or False 6. The use of “Red Lights and Sirens” should be avoided as often as possible and reserved for unstable medical conditions when it is reasonable to believe that the use of them will lead to a clinically relevant time saver, to delivery, to definitive care. True or False 7. Spirit Medical Transportation Services: a. Covers a 35-county radius b. Is a team effort of more than 100 employees, comprised of: nurses, paramedics, pilots, ambulance drivers, communications specialists, support staff and mechanics. c. Average flight run is 1.25 hours d. The helicopter can travel between 130 -160 mph under normal flight conditions. e. All of the above. 8. What affects can alcohol have on the Trauma patient? a. Alcohol can mask injuries and the pain from injuries. b. Belligerence and non-compliance may be attributed to alcohol, but may also be a sign of head injury. c. Alcohol can compromise ventilatory effort. d. Alcohol depresses the gag reflex increasing the risk of aspiration. e. All of the above. 9. List some of the safety-related equipment expected to become standard on newer helicopters: _______________________________________________ _______________________________________________ _______________________________________________ 10. Ongoing education, including landing zone training, specialized patient care topics, and safety concerns are paramount, and may also influence optimal patient outcomes. Spirit MTS remains committed to providing specialized training/classes as requested by regional agencies, hospitals and organizations. True or False (Please print legibly) Name: ______________________________________ Address:__________________________________________________ City: ___________________________________________________________ State: ________ ZIP: __________________ Please return this completed post-test by May 25, 2009, to: Don Kimlicka, EMS Coordinator, Saint Clare’s Hospital, 3460 Ministry Parkway, Weston, WI 54476-5220 A certificate will be sent to you. 11 U P C O M I N G E V E N T S May 17 – 23 National EMS Week May 19 Saint Clare’s Hospital EMS Appreciation Event, 6 – 9 p.m., Saint Clare’s Hospital Conference Center, Weston, Wis. For more information, contact Don Kimlicka at [email protected] Saint Joseph’s Hospital EMS Appreciation Event, featuring Dwight Polk, presenting, “I Believe … Lessons I’ve Learned in 30 Years of EMS,” Saint Joseph’s Hospital - Mother Streitel Conference Center, Marshfield, Wis. For more information, contact Sandy Johnson at [email protected] August 13 & 14 14th Annual Spirit Medical Transportation Services Conference – “What’s Hot and What’s Not in Trauma,” Ramada Inn, Stevens Point, Wis. For more information, contact Audrey Schmeeckle at [email protected] *Accreditation Statement: Marshfield Clinic is accredited by the Wisconsin Medical Society to provide continuing medical education for physicians. Safety is Not by Accident awareness and avoidance warning systems, satellite tracking, in-flight weather radar, and Night Vision Goggle capability, all of which will be included in delivery of Spirit’s new EC-145 later this year. Additionally, various “human factors” have been identified as the major contributor to air medical crashes. Regionally, there are many things we can do to minimize risk: Recognize that responsibility for air medical safety includes not only flight program staff, but also agencies that request these services. For scene response, this includes EMS, fire, and law enforcement, while regional hospitals fulfill a vital communications role during interfacility transport. Regardless of scenario, clear, concise and updated information/radio traffic is paramount to operational safety. Pre-planning and practice “drills” should be vital components of all supporting agencies, in order to effectively plan for those “what ifs” and “atypical” situations. If more than one helicopter is being requested, it is vitally important to share that information ASAP with all services responding—to enhance communication and safe operations for everyone, both in the air and on the ground. Always have a “Plan B” (for potential ground transport need). As frequently experienced here in the Midwest, “Mother Nature” routinely influences whether (continued) conditions are safe for flight. While we understand the frustration that a “weather no-go” may cause for those at a hectic scene or in a busy ED, conditions have been deemed as unacceptable for safe flight at that particular time. That said, due to geographic location, there may be rare instances when one program may be able to perform a transport while another can not. While it is recognized that “helicopter shopping” may occur, this practice can be dangerous if all information is not readily shared upfront. Therefore, it is crucial that if another program has already turned down a transport, that this information is shared prominently if calling another service. Additionally, ongoing education, including landing zone training, specialized patient care topics, and safety concerns, are paramount, and may also influence optimal patient outcomes. Spirit MTS remains committed to providing specialized training/classes as requested by regional agencies, hospitals, and organizations. For more information, please contact Spirit MTS at 715.387.7110 with your request, and the appropriate crew representative will contact you. Combined with the efforts of our regional providers, we look forward to further serving our shared patients in a safety-enhanced environment. Non-profit Organization U.S. POSTAGE PAID Wausau, WI Permit No. 611 Vital Connections is an EMS publication of Saint Joseph’s Hospital & Saint Clare’s Hospital. Please send comments to: Sandy Johnson, EMS Coordinator Saint Joseph’s Hospital 611 Saint Joseph Avenue Marshfield, WI 54449-1898 OR Don Kimlicka, EMS Coordinator Saint Clare’s Hospital 3400 Ministry Parkway Weston, WI 54476-5220
© Copyright 2026