Collagen induction therapy for the treatment of upper lip wrinkles
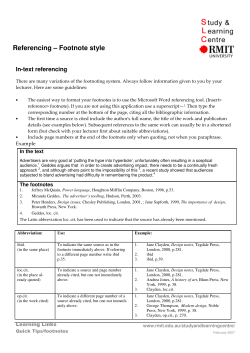
Journal of Dermatological Treatment. 2012; 23: 144–152 ORIGINAL ARTICLE J Dermatolog Treat Downloaded from informahealthcare.com by IBI Circulation - Ashley Publications Ltd on 03/29/12 For personal use only. Collagen induction therapy for the treatment of upper lip wrinkles GABRIELLA FABBROCINI1, VALERIO DE VITA1, FRANCESCO PASTORE1, MARIA CARMELA ANNUNZIATA1, SARA CACCIAPUOTI1, AMBRA MONFRECOLA1, NORMA CAMELI2 & ANTONELLA TOSTI3 1 Department of Dermatology and Venereology, University of Naples Federico II, Naples, Italy, 2San Gallicano Dermatological Institute, Rome, Italy and 3Department of Dermatology and Cutaneous Surgery, Miller School of Medicine, University of Miami, Miami, FL, USA Abstract Upper lip wrinkles are very common and impair the quality of life of many people due to their perceived unsightly appearance. Several options are available today for their treatment. A new therapeutic option, called collagen induction therapy (CIT), seems to be effective and safe for the treatment of upper lip wrinkles. The aim of this study is to demonstrate the efficacy and safety of CIT in the treatment of upper lip wrinkles. Ten female subjects, aged 50–65 years old, with upper lip wrinkles were enrolled. Each patient was treated with a specific tool in two sessions. Using a digital camera, photographs were taken of all the patients to evaluate the depth of the wrinkles and a silicon-print technique was used to obtain a microrelief impression of the wrinkles. Data of the cutaneous casts were analyzed by computerized image analysis. Analysis of the patients’ photographs, supported by the sign test, and of the degree of irregularity of the surface microrelief, supported by Fast Fourier Transform and by wrinkle image processing, showed that, after only two sessions, the wrinkles’ severity grade in most patients was greatly reduced. The present study confirms CIT as an effective and safe technique to improve upper lip wrinkles. Key words: collagen induction therapy, skin needling, upper lip wrinkles Introduction Upper lip wrinkles are very common and impair the quality of life of many people due to their perceived unsightly appearance. Wrinkles are modifications of the skin associated with cutaneous aging and develop preferentially on sun-exposed skin. Increased fragility, decreased dermal thickness and vascularity, a reduced number of dermal fibroblasts and their ability to synthesize, and a decreased response to growth factors are the most specific aspects of aged skin. Histological examination of intrinsically aged skin reveals atrophy of the dermal extracellular matrix (ECM), with reduced levels of collagen and elastin (1). Nowadays, wrinkles have a greater social impact. Upper lip wrinkles can be the most frustrating and unsightly of all wrinkles, in particular because for women the perioral area has always been considered a very sensual part of the face. The treatment for these wrinkles varies with the degree of severity. Several therapeutic options are available today: topical medications, chemical peels, dermabrasion, muscle-relaxing injections, laser resurfacing, cosmetic filler injections, and, most recently, collagen induction therapy (CIT). CIT is an effective (2–6) method of treating wrinkles and other dermatological lesions, such as post-acne and other scars. It consists of puncturing the skin multiple times with small needles to induce collagen growth. This technique has been used since 1995, when Orentreich and Orentreich2 described ‘subcision’ as a way of building up connective tissue beneath retracted scars and wrinkles. Fernandes simultaneously and independently used a similar technique Correspondence: Gabriella Fabbrocini, Department of Dermatology and Venereology, University of Naples Federico II, Via Sergio Pansini n. 5, 80133 Naples, Italy. E-mail: [email protected] (Received 29 September 2010; accepted 13 November 2010) ISSN 0954-6634 print/ISSN 1471-1753 online ! 2012 Informa Healthcare USA on behalf of Informa UK Ltd. DOI: 10.3109/09546634.2010.544709 Collagen induction therapy for treatment of upper lip wrinkles to treat the upper lip by sticking a 15-gauge needle into the skin and then tunnelling under the wrinkles in various directions, parallel to the skin surface (7). 145 treatments within the last 8 weeks before the start of the study, and lack of cooperation. Procedure Objective J Dermatolog Treat Downloaded from informahealthcare.com by IBI Circulation - Ashley Publications Ltd on 03/29/12 For personal use only. In order to confirm the effectiveness and safety of CIT for the treatment of upper lip wrinkles, we performed this procedure to treat a group of 10 female subjects affected with different grades of upper lip wrinkles. Patients and methods Patients This study was conducted between 1 September 2008 and 29 May 2009 at the University of Naples “Federico II”, Department of Systematic Pathology, Division of Clinical Dermatology, in accordance with the ethical guidelines of the 1975 Declaration of Helsinki. In total, 10 female subjects, 50–65 years old (mean age 59), with upper lip wrinkles were enrolled and gave their informed consent. The study was approved by the ethical committee. Inclusion and exclusion criteria Inclusion criteria were as follows: voluntary participation, age between 50 and 65 years, an agreement not to undergo other local skin rejuvenation treatments during the study, and providing written informed consent (with the option to withdraw from the study at any time without a negative impact on their further treatment at our Division of Dermatology). Exclusion criteria were as follows: history of keloid scarring, immunosuppression, diabetes, neuromuscular disease, collagen vascular disease, bleeding disorder, anticoagulant therapy, corticosteroid therapy, presence of skin cancers, warts, solar keratoses and any skin infection, any local skin rejuvenation Before the treatment (Baseline, T0) the severity of lesions in each patient was scored by an experienced dermatologist involved in the study. Upper lip wrinkle severity was evaluated using the Wrinkle Severity Rating Scale (WSRS). The WSRS was chosen as the best published and validated method of rating the upper lip wrinkles. The WSRS is a 5-point grading scale that describes the severity of the upper lip folds, with the right end (5) indicating maximum severity and the left end (1) indicating minimum severity (Table I). It has been shown to be a valid instrument with good intraobserver and interobserver agreement (8–10). Wrinkles were faithfully captured using a photographic digital camera (Canon Power Shot G10): a photograph of upper lip area was taken of each patient by another dermatologist not involved in the study. In order to obtain an objective quantitative imageanalysis assessment, all pictures were taken under the same conditions, maintaining a constant level of illumination and distance. The patients were required to maintain a steady position with respect to the digital camera. An ophthalmic examination table was used to fix the patient’s head to avoid any vertical and horizontal displacement. The photographs were recorded and filed in a single database. In addition, to achieve reliable evidence, we performed for each patient an upper lip cutaneous cast, using a silicon-print technique. We mixed the silicon rubber material with a catalyst in a ratio of about 1 drop of catalyst/ml paste for 15–20 seconds on a clean tray and we finally smeared it over the skin area Patients always lay supine while the replicas were taken to prevent any postural difference from affecting the gravity-related relaxation of skin and muscles (Figure 1). After polymerization, the resin Table I. Wrinkle Severity Rating Scale (WSRS). Score Description 1 Absent: no visible fold; continuous skin line 2 Mild: shallow but visible fold with a slight indentation; minor facial feature. Implant expected to produce a slight improvement in appearance 3 Moderate: moderately deep folds; clear facial feature visible at normal appearance but not when stretched. Excellent correction expected from injectable implant 4 Severe: very long and deep folds; prominent facial feature; less than 2-mm visible fold when stretched. Significant improvement expected from injectable implant 5 Extreme: extremely deep and long folds detrimental to facial appearance; 2- to 4-mm visible V-shaped fold when stretched. Unlikely to have satisfactory correction with injectable implant alone J Dermatolog Treat Downloaded from informahealthcare.com by IBI Circulation - Ashley Publications Ltd on 03/29/12 For personal use only. 146 G. Fabbrocini et al. Figure 1. Skin replica procedure in a 56-year-old woman taken at baseline. Figure 2. Skin needling procedure in a 61-year-old woman during the first treatment. print was removed from the skin, numbered and archived and analyzed using image-analysis software (Image-Pro"; Media Cybernetics, Bethesda, MD, USA). The use of skin replica analysis in conjunction with photographic digital technology provided an instrument to evaluate the changes in the skin during the study. Several studies (11,12) have confirmed the value of optical profilometry as an objective technique that can reproducibly measure changes in skin topography with minimal variability or potential for bias. Before the first session of treatment began (T1), digital photographs were obtained of each patient’s upper lip area and a database was compiled. During the first session, each patient was prepared in a manner similar to a surgical procedure: facial skin was disinfected, then an anaesthetic cream (EMLA) was topically applied. At 90 minutes after the lidocaine-prilocaine cream application, each patient was treated with a tool that consists of a 12-cm plastic handle connected to a cylinder, like a small paintroller, measuring 20 mm in diameter and 20 mm in length. On the surface of the cylinder are 24 circular arrays of four needles each (total 96 needles); needle length is 1.5 mm with a diameter of 0.25 mm. Needles and disks are firmly bound together with a special medically approved adhesive. Among all the medical tools for skin needling, this type is studied for huge photoaging. Our patients are aged from 50 to 65 years old and, according to other studies on skin needling, this is the right tool to use, since skin thickness on the upper lip varies with age. The special tool was rolled over the areas affected by wrinkles. Rolling consisted of moving at least four to six times in four directions: horizontally, vertically and diagonally right and left (Figure 2). As expected, after the treatment, the skin bled for a short time but soon stopped (Figure 3). Adverse events and their severities were recorded. The second session of treatment (T2) was conducted, identically to the first one, 8 weeks later. Before this second intervention, new digital photographs were obtained for each patient using identical patient positioning, lighting, and camera settings, which were filed in the database and compared to the previous one taken before the first treatment. To estimate the improvement of wrinkles and the efficacy of CIT, each patient was also examined and, according to severity lesions, a new score was given using the WSRS. Furthermore, all patients were rated as improved or better on the Global Aesthetic Improvement Scale (GAIS) (Table II). The last check-up was conducted 30 weeks after the second treatment (T3): patients’ photographs were taken and compared to the photographs taken before Figure 3. Bleeding after skin needling in a 61-year-old woman during the first treatment. Collagen induction therapy for treatment of upper lip wrinkles J Dermatolog Treat Downloaded from informahealthcare.com by IBI Circulation - Ashley Publications Ltd on 03/29/12 For personal use only. Table II. Global Aesthetic Improvement Scale (GAIS). Score Rating Description 4 Very much improved Optimal cosmetic result 3 Much improved Marked improvement in appearance from baseline, but not completely optimal 2 Improved Improvement in appearance from initial condition 1 No change Appearance same as baseline 0 Worse Appearance worse than baseline the first treatment. Each patient was conferred a new WSRS score and GAIS rating. We assessed the great improvement induced by CIT on upper lip wrinkles after two session of skin needling. Moreover, during the last check-up we made other cutaneous casts that were compared with the ones made before beginning the first treatment and assessed the degree of irregularity in these casts by a computerized image analysis (13). Statistical analysis The digital photographic data were analyzed using a test for non-parametric data (sign test for paired data). The null (H0) is that the median of the difference is zero (P+ = P!) and the alternative hypotheses (HA) is that the median of the differences is negative (P+ < P!), a = 0.05. The result is given by computing the binomial probability. Computerized image analysis of skin cast Acquisition of images. The acquisition of skin casts was carried out using a stereomicroscope connected to an analogue video camera. Evaluation of surface’s microrelief. The morphometric study of the skin surface allows an evaluation of the surface’s irregularity in order to determine the possible variation caused by treatment. Determining the microrelief’s irregularity degree was made by the study of Fourier spectrum (FFT = Fast Fourier Transform) on images of skin casts. In detail, using a special software, on skin texture images, the average values of grey obtained along the x-axis and y-axis were evaluated; the estimated indexes, ISIwx and ISIwy (Irregular Skin Index of wx-axis and wy-axis), are the integrals of areas bounded by the curves resulting from the distribution of pixels along the x- and y-axes. 147 Wrinkles’ images processing. Image processing was carried out by a method of computerized image analysis. Skin casts were shot with a light incident at 45" which created shadows at the ridges (= negative image of wrinkles). The shadows were converted into a greyscale, whose intensity was directly proportional to the intensity of the shadows and to the depth of the wrinkles. Once the image was displayed on the screen and the area to be studied was identified for each patient, the definition pixel by pixel of series of lines (scanning), that pass through this area perpendicularly, was started. Thus, the average intensity of grey for each pixel in the intercepted area was obtained. Meticulous care was obviously taken in executing and orienting skin casts, in order to always obtain well reproducible scans (uncertainty level < 13). The uncertainty was calculated in accordance with EN45001 rules. Five skin profilometric criteria were chosen in order to evaluate the results of this study: RA measured average roughness, which is the arithmetic mean in absolute value of all variation of the mean; RT, which is the maximum depth of the wrinkles in the considered area; RZ, measured the average depth of the wrinkles; Rmax, which is the maximum height of the filtered profile; Rmin, which is the minimum height of the filtered profile. Results All the participants completed the study. Within a few minutes from the treatment, mild oedema, erythema and swelling could be appreciated; 48–72 hours after they had disappeared. No other side effect was observed. At 8 weeks after the first session of CIT all patients had smoother upper lip skin, a slight reduction in lesion severity and a minimal aesthetic improvement. At 32 weeks after the second session of CIT the improvement of upper lip wrinkles was evident: the photographic comparison highlighted that, independently of lesion grading, in each group of patients the relative depth of wrinkles was significantly reduced (Figures 4A and B). In fact, the sign test for paired data (p < 0.05) highlights that the median of the differences is negative, showing that the reduction in severity grade of upper lip wrinkles, before and after CIT, should be considered significant. When WSRS scores at T0 were compared to 30 weeks posttreatment assessment scores, each post-treatment WSRS score was significantly lower than the baseline WSRS score. A 1 to 3 point improvement occurred in all treated patients. More precisely, the mean WSRS score at 30 weeks post-treatment was approximately 2.3 times lower than the mean WSRS score at T0 (1.41 vs 3.24). Similar changes were observed in 148 G. Fabbrocini et al. J Dermatolog Treat Downloaded from informahealthcare.com by IBI Circulation - Ashley Publications Ltd on 03/29/12 For personal use only. A. B. Figure 4. (A) Upper lip wrinkles in a 61-year-old woman before the first treatment; (B) upper lip wrinkles in a 61-year-old woman 30 weeks after the second treatment. Bubbles are follicular pores. GAIS scores, which were significantly lower at 30 weeks. According to the GAIS score at 30 weeks after the second treatment, one patient was very much improved, four patients were much improved, four patients were improved and one patient had no change. A. In view of the small sample of patients considered, the results of the computerized image analysis of skin casts were not subjected to inferential statistical analysis but expressed in percentages and they are only indicative of the trend of considered parameters. The results with regard to evaluation of surface microreliefs (Figures 5A and B) showed, after treatment, a reduction in the degree of irregularity of skin texture with respect to the basal corresponding to 33% for both axes considered (x-axis and y-axis) (Figures 6A and B). The results with regard to wrinkle profilometric evaluation showed an important reduction of RA and RT parameters with respect to the basal corresponding to 35.44% for RA (from an average at T0 equal to 14.15% and at 30 weeks post-treatment equal to 9.14%) (Figure 7) and to 30.51% for RT (from an average at T0 equal to 91.27% and at 30 weeks post-treatment equal to 63.42%) (Figure 8). In addition, it was estimated there was a clinically relevant increase in the Rmin parameter with respect to the basal corresponding to 25.31% (from an average at T0 equal to 136.7% and at 30 weeks posttreatment equal to 171.3%) (Figure 9). With regard to the Rz and Rmax parameters, the profilometric evaluation did not show important variations with respect to the baseline. At the end of the study no patients complained of side effects, such as hypo- or hyperpigmentation and scars. Discussion CIT efficacy depends on its capacity to induce and, then, strongly stimulate the neo-collagen genesis process and the wound-healing process but, actually, the B. Figure 5. (A) Skin replicas in a 61-year-old woman taken at baseline. The replica taken after the needling has numerous holes. Holes can be considered a consequence of the presence of some bubbles. Bubbles are artefacts of technique, due to a casual variation of density, in some points, of the silicon mixture. They are outlined in red-coloured circles to distinguish them from the black-coloured circles which denote follicular pores. (B) Surface microreliefs in a 61-year-old woman 30 weeks after the second treatment. Collagen induction therapy for treatment of upper lip wrinkles 149 Surface microrelief (X-axis) A. 2000 Grey level (average) 1600 1648.1 1699.4 1407.8 1596.8 1400 1200 1102.9 1000 798 800 600 400 200 0 Before treatment Average Grey level (average) 2000 1800 1600 1400 1200 1000 800 600 400 200 0 After treatment Average + 1/2 dev. st Average – 1/2 dev. st Surface microrelief (Y-axis) B. 1645.3 1696.6 1402.2 1594 1097.6 793 Before treatment Average After treatment Average + 1/2 dev. st Average –1/2 dev. st Figure 6. (A) Degree of irregularity of skin texture with respect to the basal – x-axis; (B) degree of irregularity of skin texture with respect to the basal – y-axis. real mechanism of action responsible for its effects is unclear. The wound-healing process is a complex series of events that begins at the moment of injury in order to restore cellular structures and tissue layers. The classic model of wound healing is divided into three sequential, yet overlapping, phases: 1. inflammatory phase; 2. proliferative phase; 3. remodelling phase. The inflammation phase (phase 1) starts soon RA (average roughness) Grey levels (average) J Dermatolog Treat Downloaded from informahealthcare.com by IBI Circulation - Ashley Publications Ltd on 03/29/12 For personal use only. 1800 20 19 18 17 16 15 14 13 12 11 10 9 8 7 6 5 4 3 2 1 0 17.786 14.153 10.521 10.933 9.137 7.341 Before treatment Average Figure 7. RA parameter with respect to the basal. Average + 1/2 dev. st After treatment Average – 1/2 dev. st 150 G. Fabbrocini et al. Gray levels (average) 120 110 100 90 80 70 60 50 40 107.943 91.272 78.122 74.601 63.421 48.720 30 20 10 0 After treatment Before treatment Average Average + 1/2 dev. st Average –1/2 dev. st Figure 8. RT parameter with respect to the basal. after the injury: platelets, once activated, release chemotactic factors, which cause an invasion of other platelets, neutrophils and fibroblasts. During the proliferative phase (phase 2), neutrophils are replaced by monocytes that change into macrophages and release several growth factors including platelet-derived growth factor (PDGF), fibroblast growth factor (FGF), transforming growth factor (TGF-a) and transforming growth factor (TGF-b), which stimulate the migration and proliferation of fibroblasts. They start producing all the components to re-establish the basement membrane with laminin and collagen, especially collagen type III. At 48 hours after CIT, the fibroblasts begin to proliferate and release growth factors to promote collagen deposition by the fibroblasts. New blood vessels are also created. Finally, the remodelling phase (phase 3) starts and continues for several months: collagen type III is laid down in the upper dermis, just below the basal layer of the epidermis, and is gradually replaced by collagen type I; the matrix metalloproteinases (MMPs 1-2-3) are essential for the conversion process. Recently, a hypothesis based on evidence for electric fields in wound healing has been proposed to explain the CIT mechanism of action. The body has its own bioelectric system and the existence of ionic currents exiting injured tissue has been known for some time (it was first demonstrated by Matteucci in 1830). Dubois-Reymond, founder of the science of bioelectricity, was the first to experimentally demonstrate, in 1843, the existence of wound currents. He measured approximately 1 mA of current from a wound in human skin. Other more recent studies have confirmed this finding. Transepithelial potential between 25 and 50 mV (inside positive) have been recorded in human skin, maintained by a skin battery, Rmin (minimum height) Gray levels (average) J Dermatolog Treat Downloaded from informahealthcare.com by IBI Circulation - Ashley Publications Ltd on 03/29/12 For personal use only. Rt (maximun roghness) 200 180 160 140 120 100 80 60 40 20 0 171.300 188.400 154.200 136.700 152.800 120.600 Before treatment Average Figure 9. Rmin parameter with respect to the basal. Average + 1/2 dev. st After treatment Average –1/2 dev. st J Dermatolog Treat Downloaded from informahealthcare.com by IBI Circulation - Ashley Publications Ltd on 03/29/12 For personal use only. Collagen induction therapy for treatment of upper lip wrinkles presumably generated by inward transport of sodium through the membrane Na+/K+ ATPase pump in intact human skin, where current flow is limited by very high-resistance stratum corneum. When a wound disturbs the epidermal integrity, there is a net flow of current through the low-resistance wound pathway with the resultant generation of a lateral electric field within or beneath the adjacent epidermis. The ‘current of injury’, generated between the skin and inner tissues, will continue until the skin defect is repaired. Numerous studies (14) have shown that there is a ‘current of injury’ when amphibian skin is wounded, and have provided other compelling evidence for a role of endogenous electric fields in wound healing in the newt. When wound electric fields are nullified, pharmacologically or electrically, the rate of wound re-epithelialization is significantly reduced. There is significant scientific literature to support the notion that endogenous electric fields form immediately upon wounding of skin and play a role in the wound-healing process (15). Different simulation modalities are used as a basic treatment regimen in wound healing, such as direct current (DC) and alternate current (AC). Direct current, sometimes referred to as galvanic current, is continuous and unidirectional in flow (from cathode to anode): its passage through tissue produces electro-thermal, electro-chemical and electrophysical effects that can be avoided by minimizing the amplitude and the treatment time. Alternate current is defined as a current that changes the direction of flow with reference to the zero baseline at least once every second. One of the mechanisms by which the electric fields may participate in wound healing is the galvanotaxis, which consists in directing cell migration and, as such, enhancing wound healing. Many cell types have been noted to exhibit this response, and specifically keratinocytes and endothelial cells. The mechanism by which cells respond to an electric field with directional migration is the subject of ongoing investigations. Electric field-induced lateral electrophoresis and redistribution of protein within the plasma membrane is one proposed mechanism. Other possible targets include membrane channel and resultant changes in ion fluxes, changes in the organization of the actine cytoskeleton, and in the distribution of adhesive structures, such as integrins, or local activation of protein kinases. The role of electric fields is probably involved in the changes induced in the skin by CIT. When during CIT micro-needles penetrate the skin, cells react to this intrusion with a current (that the authors define as ‘demarcation current’) that is additionally increased by the needles’ own electrical potential. The membrane of a living cell has been shown to have a resting 151 electrical potential of –70 mV. The electrical potential depends greatly on the transport mechanisms. If a single acupuncture needle comes close to a cell, the inner electrical potential quickly increases to – 100 mV. Cell membranes react to the local change with an electrical potential that creates increased cell activity and a release of potassium ions, proteins and growth factors (16). According to this new hypothesis based on bioelectricity, CIT triggers a cascade of growth factors that stimulate directly the maturation phase of wound healing, so the penetration of micro-needles into the skin do not create a wound in the classic sense; they cause fine wounds and the wound-healing process is cut short, as the body is somehow ‘fooled’ into believing that an injury has occurred. Conclusion This study confirms CIT as a simple, effective and safe technique to improve upper lip wrinkles, according to the results of previous studies (2,4,7), some of them conducted on a greater number of patients. The results of computerized image analysis of skin casts, reflecting a smoothening of the skin surface in individuals treated with CIT, were consistent with clinical data showing greater improvement in fine wrinkling and roughness after collagen induction therapy. As CIT does not have severe and/or long-lasting side effects, patient compliance is good. The neo-collagen genesis process starts from about day 5 after wounding and continues slowly over a long time period; the formation of new collagen reaches its peak at about 12 weeks after treatment. So, in accordance with the literature, CIT complete results can be appreciated only after 30 weeks from the last session of treatment and they are permanent. CIT has several advantages in respect to conventional ablative methods. The most important one is that the epidermis remains intact because it is not removed or otherwise damaged, eliminating most of the risks and negative side effects of chemical peeling or laser resurfacing. In comparison with traditional ablative procedures, CIT has lower risks as side effects and is a less invasive method. In particular, the advantage of the needles over poration of the skin with a 15 blade is that the needling procedure is less invasive because the epidermis is intact and the needles penetrate through epidermis to explicate its effects on collagen induction neo-synthesis. An added benefit is also the short healing phase that follows after each treatment, and when the result is not sufficient, the treatment can be repeated (17) according to the single patient response in order to enhance clinical results. Finally, with respect to fillers, J Dermatolog Treat Downloaded from informahealthcare.com by IBI Circulation - Ashley Publications Ltd on 03/29/12 For personal use only. 152 G. Fabbrocini et al. which are temporary infiltration for the upper lips, needling stimulates permanent production of collagen and can antagonize the chrono / photoaging. Needling is an important tool for the anti-aging strategy and it can be combined with other anti-aging techniques such as filler, radio frequency and lasers. Needling stimulates permanent production of collagen and it can antagonize chrono- and photoaging over time. The procedure may be repeated according to the single patient response in order to enhance clinical results. Neo-collagen synthesis is a non-stop process, requiring an almost 2-month wash-out interval. All this evidence configures CIT as a very interesting therapeutic approach for skin rejuvenation. Further in-depth research and additional experimentation are necessary in order to obtain a best definition of the ideal number of treatment sessions and the time required between them. Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper. References 1. Braverman IM, Fonferko E. Studies in cutaneous aging: I. The elastic fiber network. J Invest Dermatol. 1982;78: 434–443. 2. Orentreich DS, Orentreich N. Subcutaneous incisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatol Surg. 1995;21:543–549. 3. Fabbrocini G, Fardella N, Monfrecola A, Proietti I, Innocenzi D. Acne scarring treatment using skin needling. Clin Exp Dermatol. 2009;34:874–879. 4. Fabbrocini G, Fardella N, De Vita V, De Padova MP, Monfrecola G, Tosti A. Periorbital wrinkles treatment using Collagen Induction Therapy. Surg Cosmet Dermatol. 2009;1 (3):106–111. 5. Fabbrocini G, Fardella N, Monfrecola A. Needling. In: Acne Scars. Tosti A, De Padova MP, Beer KR (Eds.). London: Informa Healthcare; 2009. p. 57–66. 6. Fabbrocini G, Fardella N, Panariello L, De Vita V, Sepulveres R, D’Agostino E, et al. Combined use of skin needling and platelet rich plasma in acne scarring treatment. Cosmet Dermatol. 2011;24:177–183. 7. Fernandes D. Minimally invasive percutaneous collagen induction. Oral Maxillofac Surg Clin North Am. 2005;17:51–63. 8. Day DJ, Littler CM, Swift RW, Gottlieb S. The Wrinkle Severity Rating Scale: A validation study. Am J Clin Dermatol. 2004;5(1):49–52. 9. Lemperle G, Holmes RE, Cohen SR, Lemperle SM. A classification of facial wrinkles. Plast Reconstr Surg. 2001;108(6):1735–1750. 10. Gormley DE, Wortzman MS. Objective evaluation of methods used to treat cutaneous wrinkles. Clin Dermatol. 1988;6(3):15–23. 11. Rachel JD, Jamora JJ. Skin rejuvenation regimens: A profilometry and histopathologic study. Arch Facial Plast Surg. 2003;5:145–149. 12. Creidi P, Vienne MP, Ochonisky S, Lauze C, Turlier V, Lagarde JM, et al. Profilometric evaluation of photodamage after topical retinaldehyde and retinoic acid treatment. J Am Acad Dermatol. 1998;39:960–965. 13. Grove GL, Grove MJ, Leyden JJ. Optical profilometry: An objective method for quantification of facial wrinkles. J Am Acad Dermatol. 1989;21:631–637. 14. Robinson KR. The response of cell to electrical fields: A review. J Cell Biol. 1985;101:2023–2027. 15. Ojingwa JC, Isseroff RR. Electrical stimulation of wound healing. J Invest Dermatol. 2003;121(1):1–12. 16. Jaffe L. Control of development by steady ionic currents. Fed Proc. 1981;40:125–127. 17. Fernandes D, Signorini M. Combating photoaging with percutaneous collagen induction. Clin Dermatol. 2008;26:192–199.
© Copyright 2026