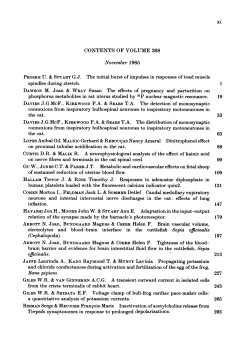
Iatrogenic Paresthesia in the Third Division of the Trigeminal Nerve:
A P P L I E D R E S E A R C H Iatrogenic Paresthesia in the Third Division of the Trigeminal Nerve: 12 Years of Clinical Experience • René Caissie, DMD, MSc • Jacques Goulet, DMD, FRCD(C) • • Michel Fortin, DMD, PhD, FRCD(C) • • Domenic Morielli, BSc, DDS • • A b s t r a c t Background: Iatrogenic paresthesia in the third division of the trigeminal nerve remains a complex clinical problem with major medicolegal implications. However, most lawsuits can be prevented through better planning of procedures and by obtaining informed consent. The purpose of this article is to present the authors’ clinical experience over the past 12 years, to review the principles of prevention and management of trigeminal paresthesia and to highlight the resulting medicolegal implications. Methods: The files of all 165 patients referred to the oral and maxillofacial surgery department for evaluation of iatrogenic paresthesia in the third division of the trigeminal nerve were reviewed. The characteristics of the subgroup of patients who had taken an attending dentist to court were compared with those of the other patients. Results: Surgical extraction of impacted molars was the main cause of paresthesia in 109 (66%) of the 165 subjects. The alveolar nerve was affected in 89 (54%) subjects, the lingual nerve in 67 (41%) subjects, and both nerves were affected in 9 (5%) subjects. There were more female than male patients (ratio 2.2:1). Lawsuits were initiated in 33 (20%) of the cases; patients who initiated lawsuits were younger, were more likely to have experienced anesthesia and were more likely to need microsurgery (all p < 0.001). Poor surgical planning and lack of informed consent were the most common errors on the part of the dentists. Conclusions: An accurate evaluation of surgical indications and risk, good surgical technique, preoperative informed consent and sufficient postoperative follow-up should help to reduce the frequency of neurosensory deficits after dental treatment and attendant lawsuits. MeSH key words: molar, third/surgery; postoperative complications; sensation; trigeminal nerve/injuries © J Can Dent Assoc 2005; 71(3):185–90 This article has been peer reviewed. C hanges in feeling in the orofacial region may interfere with speaking, chewing and social interactions.1 Even apparently minor changes can significantly affect a patient’s quality of life.2 Trauma to a peripheral nerve may result in a deficiency ranging from total loss of sensation (anesthesia) to a mild decrease in feeling (mild hypoesthesia). These sensory deficits may be either temporary or permanent. Some patients may also experience dysesthesia, which is characterized by abnormally painful sensations. Such pain may be caused by a Journal of the Canadian Dental Association neuroma located at the site of the trauma, changes in the autonomic nervous system (sympathetically mediated pain) or alterations in the central nervous system (central neuropathic pain). Allodynia is a type of dysesthesia characterized by a painful response to normally nonpainful stimuli, such as light touching or shaving. Hyperalgesia is an exaggeration of the pain response to stimuli, whereas hyperpathia is an exaggerated response to pain that persists even after the stimulus has been removed.3 The pathophysiology of these neuropathies is complex, and treatment March 2005, Vol. 71, No. 3 185 Caissie, Goulet, Fortin, Morielli Table 1 Causes of paresthesia in the third division of the trigeminal nerve Nerve affected; no. (and %) of patients Cause of injury Exodontics Injection Osteotomy Implant Endodontics Accident Parodontics Alveolar nerve (n = 89) Lingual nerve (n = 67) Both (n = 9) Total (n = 165) 52 (78) 14 (21) 0 1 (1) 0 0 0 7 (78) 0 2 (22) 0 0 0 0 109 (66) 19 (12) 17 (10) 9 (5) 5 (3) 4 (2) 2 (1) Total (n = 165) p value 50 (56) 5 (6) 15 (17) 8 (9) 5 (6) 4 (4) 2 (2) Table 2 Factors influencing probability of lawsuits No. (and %) of patients Factor Lawsuit (n = 33) Mean age (years) Sex ratio (F/M) Anesthesia Dysesthesia Microsurgery required Lingual nerve affected 32.8 21/12 (1.75) 9 (27) 5 (15) 17 (52) 14 (42) No lawsuit (n = 132) 36.1 93/39 (2.38) 9 (7) 31 (23) 16 (12) 62 (47) results are often disappointing.4 The presence of anesthesia, dysesthesia or spontaneous pain also indicates poor prospects for recovery without surgical intervention. Overall, 25% of patients with iatrogenic paresthesia suffer permanent effects.5 The risk of iatrogenic paresthesia of the third division of the trigeminal nerve depends on the procedure performed, the technique used and the surgeon’s experience. Iatrogenic paresthesia remains a complex clinical problem with major medicolegal implications. The purpose of this article is to present the authors’ clinical experience over the past 12 years, to review the principles of prevention and management of trigeminal paresthesia and to highlight the resulting medicolegal implications. Methods The files of all patients referred to the authors’ oral and maxillofacial surgery department between 1990 and 2001 for evaluation of iatrogenic paresthesia in the third division of the trigeminal nerve were reviewed. All patients had been seen and treated by the same surgeon. The data extracted from the files included age, sex, description of the trauma, lesion location, initial diagnosis, need for microsurgery and type of surgery performed. The sample was divided into 2 subgroups according to whether the patient had initiated a lawsuit against the dentist who had performed the surgery. These subgroups were compared by the Student t-test to determine whether any of the independent variables were associated with initiation of lawsuits. 186 March 2005, Vol. 71, No. 3 35.4 114/51 (2.2) 18 (11) 36 (22) 33 (20) 76 (46) < 0.001 0.46 < 0.001 0.35 < 0.001 0.68 Results The cohort consisted of 165 patients. The most common cause of paresthesia in the third division of the trigeminal nerve was extraction of impacted third molars (109 patients), followed by trauma due to injection (19 patients) (Table 1). In 135 patients, the lesion was located at the level of a single nerve, the lower alveolar nerve in 82 (61%) of these patients and the lingual nerve in 53 (39%). Twenty-one patients had bilateral pain in the lower alveolar or the lingual nerve, and 9 patients had pain in both of these nerves on the same side. One hundred and fourteen (69%) of the subjects were female (ratio of women to men 2.2:1). During the initial evaluation, most patients presented with hypoesthesia (103 [62%]) or anesthesia (17 [10%]). Dysesthesia was seen in 36 (22%) of the cases, and the proportion of female subjects was significantly higher in this subgroup (p = 0.007). Thirty-three patients (20%) underwent microsurgery for ablation of a neuroma, reanastomosis or neural decompression. Legal proceedings were initiated by 33 (20%) of the 165 patients. Patients who initiated lawsuits were younger, were more likely to have experienced anesthesia and were more likely to have needed microsurgery (Table 2). The average amount granted in the legal proceedings was $17,956, which was 42% of the average amount requested, $43,047 (Table 3). The highest amount awarded was $35,347 and the lowest $5,167. Most disputes were settled amicably or out of court. In general, higher amounts were granted to patients who had recourse to a lawyer’s services. Journal of the Canadian Dental Association Iatrogenic Paresthesia in the Third Division of the Trigeminal Nerve Table 3 Settlements for lawsuits Average amount ($) Lawsuit No. Requested Awarded Amicable settlement without legal proceedings or lawyer Amicable settlement without legal proceedings but with lawyer Legal action and unfavourable judgement to the patient Legal action and favourable judgement to the patient Legal action, settled out of court Legal action, not settled Denial of responsibility with lawyer, without any action taken Discontinuation of suit before court case Preventive notice without any action taken Overall 6 8 2 1 6 5 3 1 1 33 19,478 40,437 60,868 39,000 59,878 138,689 30,031 38,000 NA 17,956 12,838 19,997 28,733 0 17,062 NA NA NA NA 43,047 NA = not applicable Table 4 Indications and contraindications for extraction of lower third molars Indications Prevention and treatment of infection Prevention and treatment of dental and periodontal pathology Prevention and treatment of cysts and odotongenic tumours Orthodontic considerations (facilitate alignment, prevent relapse) Contraindications Advanced age (> 30 years) Very young age (< 12 years) Imminent damage to adjacent structures Possibility that tooth might erupt or serve as an abutment Orthodontic considerations (tooth needed as an anchor or for the alignment of teeth) Patient refusal to accept risks associated with extraction Discussion The reported incidence of paresthesia after extraction of impacted third molars varies between 0.2%6 and 22%7 for the lingual nerve and between 0.4%8 and 7%9 for the lower alveolar nerve. These variations can be explained by differences in procedures and technique, in particular with regard to clinical evaluation and diagnostic criteria, as well as differences in the surgeon’s experience. The risk of paresthesia depends on the clinical situation. It may be almost nonexistent under the best conditions (young patient, incompletely formed roots, mandibular canal not in close proximity) but could exceed 50% in other circumstances (elderly patient, unfavourable position of the tooth, proximity of the mandibular canal). A good clinical evaluation can be used to inform the patient about the potential risks of surgery. Written informed consent, after the patient has received a complete description of these risks, must be obtained in all cases of nontherapeutic surgical removal of the molars (i.e., preventive treatment). Consent is also strongly recommended in cases of therapeutic surgical extraction (treatment of pathology) for semi-impacted or impacted third molars. Journal of the Canadian Dental Association Among patients with iatrogenic paresthesia in the third division of the trigeminal nerve, 75% regain normal sensitivity without further treatment.5 In most cases, complete recovery occurs 6 to 8 weeks after the trauma, although it may take up to 24 months. If paresthesia is not completely resolved within about 2 months, the probability of a permanent deficit increases significantly; it is unlikely that complete resolution will occur if the deficit is still present after 9 months.10 The prognosis of spontaneous recovery is better for the lower alveolar nerve than for the lingual nerve.8 In the preoperative evaluation for nontherapeutic extraction of impacted third molars, the surgeon must decide whether the risks of surgery exceed the expected benefits. This study and the authors’ clinical experience have shown that, too often, the risk of surgery had been poorly evaluated and, in certain cases, the treatment is not even indicated. The surgeon must be familiar with the indications for removal of impacted third molars (Table 4). He or she must also be familiar with the radiologic signs indicating the proximity of the lower alveolar nerve. The presence of a radiolucent band at the apex of the third molar, loss of continuity of the upper or lower bony cortex in the lower alveolar canal and shrinking or deviation of this canal are all reliable signs indicating closer proximity of the lower alveolar nerve to the root of the wisdom tooth (Figs. 1 to 3).11 Management Perioperative Precautions If the patient feels a sensation like an electric shock when the needle is inserted, the needle should be withdrawn by a few millimetres before the solution is administered. If the position of the extracted tooth allows the lower alveolar nerve to be seen at the bottom of the alveolus, many surgeons prefer to place a piece of absorbable gelatin in the alveolus (e.g., Gelfoam, Pharmacia & Upjohn Co, Kalamazoo, Mich.) before closing. However, the March 2005, Vol. 71, No. 3 187 Caissie, Goulet, Fortin, Morielli Figure 1: A 34-year-old patient who underwent extraction of tooth 48. Anesthesia in the area of the lip and chin was noted upon initial examination. Neural decompression with debridement revealed that the nerve had been partially cut, and there was intense scarring at the affected site. Legal proceedings were initiated against the dentist. Note the presence of a radiolucent band at the apex of the third molar. Figure 2: A 32-year-old patient who underwent extraction of tooth 38. After the surgery, the patient presented with severe dysfunctional hypoesthesia as well as hyperalgesic neuralgia and eventually launched a lawsuit. Note the classic signs of very close proximity between the lower alveolar nerve and the apex of the third molar, i.e., loss of continuity of the bony cortex of the lower alveolar canal, as well as its shrinking and deviation at the apex. Figure 3: A 32-year-old patient who was evaluated for hypoesthesia of the lip and chin and the vestibular mucosa after extraction of tooth 38. There is major deviation of the lower alveolar canal, indicating close proximity between the canal and the tooth. Figure 4: Mapping of the affected area can delimit the scope of the problem and can be used to follow its development. Figure 5: A swab may be used to evaluate the patient’s sensations in the affected area. Only the point of the swab should come into contact with the subject’s tissues, so as to obtain a reliable reading. Figure 6: A soft hairbrush can be used to assess the patient’s ability to detect direction of movement. 1. Map the affected area by pencil outline on a drawing or a photograph of the patient (Fig. 4). 2. Determine the sensations felt by the patient when a cotton swab is lightly applied to the affected area (Fig. 5). 3. Determine the ability of the patient to detect the direction of a sweeping motion (in an area of about 1 cm), applied with a resin applicator or the tip of a rolled-up tissue (Fig. 6). Figure 7: The flat tip of a 27-gauge needle is used to evaluate the patient’s perception of painful stimuli. effectiveness of this measure, which aims to minimize fibrosis and thus prevent paresthesia, has not been established. Clinical Evaluation Patients with postoperative paresthesia must be treated promptly and should be seen as soon as possible for clinical evaluation. The clinical evaluation should comprise the following elements: 188 March 2005, Vol. 71, No. 3 4. Describe the patient’s sensations when a 27-gauge hard needle is applied in the affected region with sufficient pressure to indent the skin without penetrating it (Fig. 7). The presence of dysesthesia or spontaneous pain must be noted. Each test must be conducted at 3 sites: the lower lip, the lip–chin fold and the chin. Any patient with paresthesia should receive corticosteroids to minimize the inflammatory response.12 Empiric treatment with prednisone (50 mg once daily) for 7 days is often used in the authors’ oral surgery department. This medication must be started as soon as possible, ideally the day after surgery. Journal of the Canadian Dental Association Iatrogenic Paresthesia in the Third Division of the Trigeminal Nerve Seven-day antibiotic treatment with penicillin, the gold standard for patients without penicillin allergy, or clindamycin is commonly prescribed to prevent infection, which would slow the healing process and decrease the likelihood of full recovery of the nerve. Clinical evaluation should be repeated once a month to assess the presence or absence of functional recovery. Referring the Patient Some patients must be referred to an oral and maxillofacial surgeon. Microsurgery may be indicated in the following cases: confirmed transection of a nerve; total anesthesia of the affected area 2 months after the trauma; lack of protective reflexes (on biting or burning of the tongue or lower lip) 2 months after trauma, with little or no improvement; or dysesthesia.13 Microsurgery involves general anesthesia, a period of convalescence and a few weeks off work. The surgeon dissects the affected nerve and, if the damage is extensive, joins the proximal and distal portions. This surgery should ideally be done within 4 months after the trauma to prevent atrophy of the distal part of the nerve.14 Therefore, if it is felt that the patient’s condition might be improved through surgery (on the basis of the criteria listed above), he or she should be referred immediately to allow the surgeon to make his or her own assessment and measure the lack of functional recovery over a period of 2 months before intervening. Although considerable functional improvement is seen in many patients after surgery,13,15 regaining normal sensation is not possible. Just under half of patients experience no improvement, and all patients who undergo surgery will have some permanent sensory deficit. In cases of dysesthesia, a more medical approach is required, since surgery is rarely useful in these cases, especially for patients with sympathetically mediated pain or central neuropathic pain.16 Conclusions Most cases of iatrogenic paresthesia can be prevented. However, when this problem occurs, follow-up must be initiated quickly, since the first few months may determine the degree of nerve healing. If there is a high risk of nerve trauma, the patient should be referred preoperatively to an oral and maxillofacial surgeon. Most patients recover normal sensation without treatment. However, permanent deficits are often poorly tolerated, as indicated by the high proportion of lawsuits in such cases. More than half of lawsuits are associated with lack of preoperative informed consent.17 In-depth knowledge of anatomy and surgical principles is also imperative. It is often easy to treat slight hypoesthesia, but treatment becomes complex in cases of sympathetically mediated pain or central neuropathic pain. If a large area has been affected, it is impossible to regain normal sensation regardless of the therapeutic measures Journal of the Canadian Dental Association undertaken. The well-informed general dentist should be able to perform an initial assessment and then refer the patient to a maxillofacial surgeon at the appropriate time to maximize the chances of functional recovery of the affected nerve. C Acknowledgements: The authors would like to thank the Fonds d’assurance responsabilité of the Quebec Order of Dentists, as well as Pauline O’Brien and Valérie Savoie-Rosay for their contributions in writing this article. Dr. Caissie is a doctoral student in experimental medicine at Laval University’s faculty of medicine in the Experimental Organogenesis Laboratory (LOEX), Quebec City, Quebec, and a second-year resident in the oral and maxillofacial program, Hôpital de l’Enfant-Jésus, Quebec City. Dr. Goulet is an oral and maxillofacial surgeon at the Hôpital Hôtel-Dieu de St-Jérôme, St-Jérôme, Quebec. Dr. Fortin is an oral and maxillofacial surgeon at the Hôpital Enfant-Jésus de Québec, Lévis, Quebec. He is also a Fellow in surgical oncology and reconstructive surgery from the Jackson Memorial Hospital, University of Miami. Dr. Morielli is an oral and maxillofacial surgeon at the Hôpital de l’Enfant-Jésus and a clinical professor at Laval University’s faculty of dentistry, Quebec City, Quebec. Correspondence to: Dr. Jacques Goulet, 208–200, rue Durand, StJérôme, QC J7Z 7E2. E-mail: [email protected]. The authors have no declared financial interests in any company manufacturing the types of products mentioned in this article. References 1. Ziccardi VB, Assael LA. Mechanisms of trigeminal nerve injuries. Atlas Oral Maxillofac Surg Clin North Am 2001; 9(2):1–11. 2. Sandstedt P, Sorensen S. Neurosensory disturbances of the trigeminal nerve: a long-term follow-up of traumatic injuries. J Oral Maxillofac Surg 1995; 53(5):498–505. 3. LaBanc JP. Classification of nerve injuries. Oral Maxillofac Clin North Am 1992; 4(2):285–96. 4. Cooper BY, Sessle BJ. Anatomy, physiology, and pathophysiology of trigeminal system paresthesias and dysesthesias. Oral Maxillofac Clin North Am 1992; 4(2):297–322. 5. Zuniga JR, LaBanc JP. Advances in microsurgical nerve repair. J Oral Maxillofac Surg 1993; 51(suppl 1):62–8. 6. van Gool AV, Ten Bosch JJ, Boering G. Clinical consequences of complaints and complications after removal of the mandibular third molar. Int J Oral Surg 1977; 6(1):29–37. 7. Von Arx DP, Simpson MT. The effect of dexamethasone on neurapraxia following third molar surgery. Br J Oral Maxillofac Surg 1989; 27(6):477–80. 8. Alling CC 3rd. Dysesthesia of the lingual and inferior alveolar nerves following third molar surgery. J Oral Maxillofac Surg 1986; 44(6):454–7. 9. Middlehurst RJ, Barker GR, Rood JP. Postoperative morbidity with mandibular third molar surgery: a comparison of two techniques. J Oral Maxillofac Surg 1988; 46(6):474–6. 10. Robinson PP. Observations on the recovery of sensation following inferior alveolar nerve injuries. Br J Oral Maxillofac Surg 1988; 26(3):177–89. March 2005, Vol. 71, No. 3 189 Caissie, Goulet, Fortin, Morielli 11. Tammisalo T, Happonen RP, Tammisalo EH. Stereographic assessment of mandibular canal in relation to the roots of impacted lower third molar using multiprojection narrow beam radiography. Int J Oral Maxillofac Surg 1992; 21(2):85–9. 12. Gregg JM. Nonsurgical management of traumatic trigeminal neuralgias and sensory neuropathies. Oral Maxillofac Clin North Am 1992; 4(2):375–92. 13. Pogrel MA. The results of microneurosurgery of the inferior and lingual nerve. J Oral Maxillofac Surg 2002; 60(5):485–9. 14. Ruggiero S.Terminal nerve injury and repair. N Y State Dent J 1996; 62(8):36–40. 15. Gregg JM. Studies of traumatic neuralgia in the maxillofacial region: symptom complexes and response to microsurgery. J Oral Maxillofac Surg 1990; 48(2):135–40. 16. Gregg JM. Studies of traumatic neuralgias in the maxillofacial region: surgical pathology and neural mechanisms. J Oral Maxillofac Surg 1990; 48(3):228–37. 17. Lydiatt DD. Litigation and the lingual nerve. J Oral Maxillofac Surg 2003; 61(2):197–200. 190 March 2005, Vol. 71, No. 3 Journal of the Canadian Dental Association
© Copyright 2026