10 Things ICUs Must Do Better Organ Donation: An Update
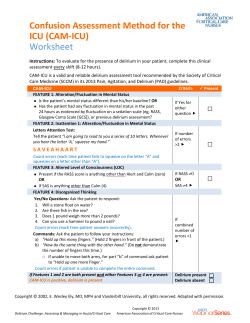
“Keeping you in touch with our collective critical care team” 10 Things ICUs Must Do Better Recently, in his plenary address at the Society of Critical Care Medicine Conference, R. Phillip Dellinger (MD) reflected on the “10 Things ICUs Must Do Better”, based on 35 years of Critical Care experience. (Medpage Today, http://www.medpagetoday.com/MeetingCov erage/SCCM/49606) While not necessarily evidence-based topics, all of them represent plain ol’ common sense! They are worth taking a look at: 1. Add a bigger dose of compassion 2. Employ 2-way communication with patients and their families 3. Remain vigilant about good Sepsis care, which has brought about dramatic improvements in mortality (despite recent trials eschewing protocolized-based treatments): “we should not rest on our laurels” 4. Recognize the importance of Post-ICU Syndrome (e.g., PTSD, depression, cognitive and physical challenges), and implement strategies to reduce the impact, such as, using fewer restraints, promote sleep, ambulate early and carefully consider medication choices for agitation and delirium. 5. Improve/recognize the more urgent need for pre-ICU Care 6. Align research and healthcare changes 7. Do more physical exams (“lay hands”!) and model this behaviour for fellows and residents. 8. Standardize and streamline multidisciplinary ICU rounds 9. Focus on Patient Safety, to decrease lengths of stay and improve patient experiences (e.g., improved hand washing rates, decreased pressure ulcers, minimize delirium rates, etc) 10. Employ electronic medical record documentation Page 1 Organ Donation: An Update As you are all aware, CDHA is a national leader in terms of Organ Donation. We have an active team, made up of an extremely passionate and dedicated group of individuals. The medical director for Organ Donation is Dr. Stephen Beed (Critical Care & Anaesthesia) and the manager is the Health Services Manager for 5.2 MSNICU (currently in transition), where all potential donors are admitted for assessment and workup. The four Organ Donor Coordinators are: Tami Murphy, Jane Franklin, Mark Bonin and Janet Ballem. They work on a rotating call schedule and can be reached 24/7 for any question and/or assessment of potential donors. In addition to donation after neurological declaration of brain death (NDD), at CDHA, we are now practicing donation after cardiac death (DCD). There are strict criteria for both, in addition to protocols for care of the potential organ donor patient. The table below lists the organ donation statistics for chart audits from January 1, 2014 through December 31, 2014*: Referrals to Critical Care Organ Donation (CCOD) 43 Actual Donors 12 NDD, 5 DCD (17 Total) Family Declines 11 Missed Referrals 10 * Chart audits on all death charts (433 charts) in Critical Care and Emergency Department at QEII, VG, Dartmouth General and IWK. Thank you to everyone for your continued vigilance and hard work; donation is often the only bright spot for families during a tragic time in their lives. One donor can benefit more than 75 people and save up to 8 lives – cantransplant.ca Critical Care Quality News ● March 2015 ● Issue 3 Delirium & Pressure Ulcers Many dedicated people are working hard to make patient DELIRIUM IN THE ICU: safety a top priority. Current a. In August 2014 data collection about the number of CAM-ICU positive (i.e., initiatives of the QA group Delirious patients) began. Some important findings have emerged: (through various working groups) i. 66% of our patients are mechanically ventilated (which is a major risk include DELIRIUM PREVENTION (in factor for the development of delirium); conjunction with the Mobility ii. There has been great uptake with daily CAM-ICU data collection by Project) and PRESSURE ULCER Charge Nurses & Staff Nurses! THANK YOU AND KEEP UP THE GREAT WORK! PREVENTION. b. What next? i. We are aiming to discuss delirium EVERY DAY ON ROUNDS! ii. We are aiming to INCLUDE pain, agitation and sleep assessments daily also! iii. We will be moving forward with a Practice Grant looking at the Sleep Promoting Environment in ICU: PLEASE VOLUNTEER TO HELP! iv. THERE WILL BE A PRACTICE COUNCIL EDUCATION EVENT APRIL 1, including a presentation on Delirium & Medications - don’t forget to register and attend! (Information regarding event can be found on Page 4) PRESSURE ULCER PREVENTION: a. Pressure ulcers are neither glamorous nor sexy (see image above), but they are important risks to patient safety and wellbeing, and have also been identified by Accreditation Canada and provincial bodies as a priority area of focus in Critical Care. b. In order to improve pressure ulcer prevention, we need to ramp up AWARENESS OF THE SCOPE OF THE PROBLEM – toward that end, pressure ulcer screening (3x/month) began in August 2014. c. WHAT ARE THE NEXT STEPS? i. We will be continuing to collect ICU pressure ulcer data at least 3 times per month ii. Continue ongoing education through various methods, and participate in local and national prevalence studies iii. Continuing with the mobility project iv. We will be getting pressure-redistributing chair cushions for use with high-risk patients Family Survey’s PRESSURE ULCERS IN CRITICAL CARE – 3A/5.2 Between August 2014 & February 2015, screening was completed on 51 days! A total of 420 ICU patients were assessed. The most common location for ulcers is the coccyx (59%), followed by heels (25%). Number of Pressure Ulcers known to be ICU Acquired - 11 Number of Pressure Ulcers Possibly ICU Acquired - 9 ICU Acquired Pressure Ulcers are present in between 2.6% and 4.8% of the patients assessed. The CDHA Pressure Ulcer Prevention Committee would like to hear from staff to be able to develop effective improvement strategies. They want to hear from Critical Care: - What are the current barriers for your team in preventing or treating pressure ulcers? - What are the current enablers that allow you to effectively prevent, or care for existing ulcers? Please email [email protected] to contribute to our response. There will also be postings on the units to capture people’s thoughts. What do families tell us? Overall, families tell us how satisfied they are with the clinical expertise and care provided in our units. As a family we were very pleased with the professional service provided. Above this, one thing was very evident, the staff showed a very caring attitude that we appreciated. Thank You. A top priority repeatedly identified is communication. Families need information in an understandable manner that is open, honest, and consistent across professions. Please encourage family feedback! There are family surveys available in the main Waiting Rooms on both 3A & 5.2. Please encourage families to complete the surveys. They can place them in the locked box, or they can mail them back to us. Page 2 Critical Care Quality News● 2014 ● Volume 1, Issue 1 Critical Care Quality News ● March 2015 ● Issue 3 Organizational Health Grants Competition! Congratulations to our Teams on 3A & 5.2 for submitting successful applications to the Organizational Health Grants competition! More information about participating will be circulated & posted on the units. The 3A submission was entitled I.C.U….Do U.C. ME?, the goal is to build inter-disciplinary team capacity, cohesiveness and resilience. They will plan an event at OnTree Fun and Adventure Park in Windsor, NS where they will learn to push their boundaries by trying a new activity, laughing and sharing new challenges as they get to know each other better along the way. OnTree Fun and Adventure Park offers fun for people of all ages and abilities with 13 different exciting course events, 350 foot zip lines, a bike on a wire, tarzan ropes, spider webs, and a 50 foot base jump! The 5.2 submission was entitled Do you want to run away and Join the Circus?. From their submission: “there are many different people of various professional educations and support services who come together every day to provide holistic care to the sickest of the sick in the 5.2 Intensive Care Unit. The toll on the team can be physically and mentally exhausting. We would like to provide a chance to these hard-working men and women to laugh, participate in group activities and interact outside the workplace. The setting would allow an environment free from work roles, hierarchy and job descriptions”. They will plan a team event hosted by Atlantic Cirque, in Dartmouth. It will be designed to involve people of varying physical abilities, using circus apparatus, acrobatics, trampoline, human pyramids, and juggling. Try to get some rest. I’ll be in every few minutes to ensure you don’t. Sleep Promotion in the ICU: Fact or Fallacy? Nurses from 3A & 5.2 received a Nursing Practice Grant to examine the sleep promoting environment in the ICUs. In February, a survey was done to better understand barriers and to inform an initial plan for improvement. Thanks to all who participated in the survey! Everyone that completed the survey had an opportunity to put their name in a draw for 2 tickets to a taping of This Hour Has 22 Minutes. Congratulations to our winners! From the 3A ballot envelope: Clinton Lewis From the 5.2 ballot envelope: Chris White Critical Care Research! Critical Care research coordinator Lisa Julien works closely with professors Dr. Richard Hall and Dr. Robert Green to conduct a wide range of studies (industry and grant funded) involving patients admitted to the Intensive Care Units at the QEII Health Sciences Centre. With as many as six studies going on at any one time, they are testing new medications for treating severe sepsis and hospital acquired pneumonia, new approaches to preventing blood clots, and new ways of assessing and treating injuries to the kidneys, lungs, brain and other organs. The QEII/Capital Health organization is one of the top-recruiting sites in the Canadian Critical Care Trials Group. Involving more than 40 hospitals across Canada, this is one of the most active and successful critical care research groups in the world. Page 3 Current studies we are recruiting into are: 1) Industry: A randomized, double-blind, placebo controlled, phase 3 study to assess the safety and efficacy of ART 123 in subjects with severe sepsis and coagulopathy 2) Grant: Early Determination of Neurological Prognosis in ICU patients with Severe Traumatic Brain Injury: TBI -Prognosis Multicenter Prospective Study 3) Grant: Re-Evaluating the Inhibition of Stress Erosions: Gastrointestinal Bleeding Prophylaxis In ICU (REVISE): A Feasibility Pilot Trial 4) Grant: Bacteremia Antibiotic Length Actually Needed for Clinical Effectiveness: (BALANCE)-Pilot 5) (Non-Funded): Effect of inflammation on the bloodspinal barrier. A sub-study of the CAMPER Study. 6) (Industry):A Phase 3 Randomized Double-blind Study Comparing TR-701-FA and Linezolid in Ventilated Gram-positive Nosocomial Pneumonia Critical Care Quality News ● March 2015 ● Issue 3 Upcoming Events: Critical Care Nursing Practice Council Educational Event! Wednesday April 1st @ 0800-1200 Weather Watch Room, Dickson Bldg Presenters: -Dr. Meghan Mackenzie & Clinical Pharmacists – Delirium & Medications -Dr. Rob Green – Resuscitation before Intubation: Lessons Learned -Dr. Babar Haroon – Patient Safety through Team Communication -Carol Meade-Corkum – ECG Rhythm Interpretation To register please email [email protected] Blood and Beyond 2015: Issues in Trauma, Bleeding, Coagulation and More! April 18th & 19th 2015 The Prince George Hotel, Halifax, NS Presented by Perioperative Blood Management Services, Department of Anesthesia, Dalhousie To learn more and/or to register visit http://nsanesthesia.ca/s/blood-and-beyond CANN: Neurology at a Glance May 4th 2015 0900-1530 Royal Bank Theatre, Halifax Infirmary “All Healthcare professionals & Students are invited to join us for a day of Neuroscience Learning”. Register by April 24th 2015, email CANN-NS Councillor Joan Pacione at [email protected] COMING SOON! Daily Rounds Tool As we know, one of the key’s to patient safety is team communication. In ICU, BEDSIDE ROUNDS represents the main opportunity dedicated to interdisciplinary team communication. We are going to be starting to use a Daily Rounds Tool, to help us ensure key components are being addressed. This Daily Rounds Tool is a simple electronic survey on the ICU portable computers that can be completed by any team member, and can be passed back and forth between team members during rounds. It is meant to support, not impede, our teamwork! Any feedback, as this is implemented, should be passed along to Sarah McMullen or Karen Webb-Anderson so that we can ensure it is as efficient and user-friendly as possible. Medication Safety Huddles Medication Safety Huddles are being re-introduced on both 3A & 5.2. They will be held each Thursday at 1415 and co-lead by the Clinical Pharmacist & Charge Nurse. Topics to consider: What are your concerns about medication safety? What strategies can be put in place to prevent errors / near misses? What is new in our critical care pharmacy world? "Alone we can do so little, together we can do so much." ~Helen Keller~ Critical Care Grand Rounds @noon Rm 378 Bethune: Tues March 31st – Dr. Marion Cornish Tues April 7th – Dr. Emily Rowsell Tues May 5th – Critical Care Research Group Tues June 2nd – Dr. Tobias Witter *specific topics TBA/All teams welcome to attend!! Changes to our Critical Care Family Welcomes! & Thank Yous! We have had a new addition to our ICU family. WELCOME! 5.2 New Staff: Brent De Young With the coming of new staff we have seen some amazing members of our family leave. A BIG thank you for your dedication and hard work! You will be missed!! 3A RETIREMENTS: Debbie Labrech 5.2 RETIREMENTS: Katy MacAulay & Eleanor Tinkham Page 4 Our Critical Care Quality Team would like to thank Dawnelda Murray for her commitment to our Team's success. We wish her all the best as moves into her new role in 3 IMCU and we look forward to future opportunities to collaborate! Produced by Department of Critical Care 1276 South Park St Rm 377 Bethune Bldg Halifax, Nova Scotia B3H 2Y9 Phone: (902) 473-3486 Fax: (902) 473-3610 Email: kristen.griffiths@cdha. nshealth.ca Critical Care Quality News ● March 2015 ● Issue 3
© Copyright 2026