Adolescent Sports Medicine Update - University of Missouri
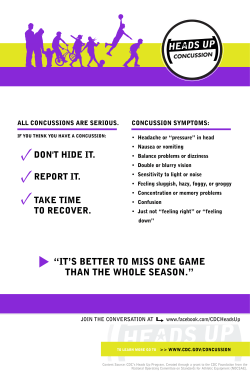
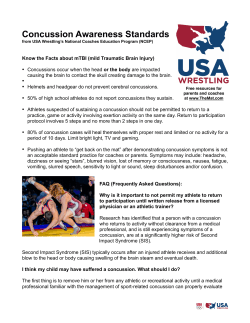
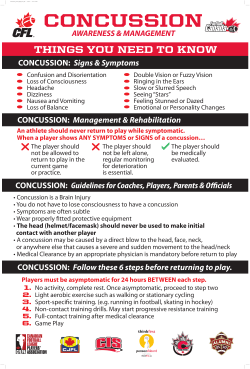
05/18/2015 Adolescent Sports Medicine Update Objectives X Understand unique diagnostic and management considerations of concussions in adolescents. X Review diagnosis and management of adolescent specific musculoskeletal conditions. X Discuss answers to common questions parents ask about exercise and sports participation in adolescents. AARON GRAY, MD DEPARTMENTS OF FAMILY MEDICINE & ORTHOPAEDICS UNIVERSITY OF MISSOURI. Concussions 1 05/18/2015 Missouri State Law X 3. A youth athlete who is suspected of sustaining a concussion or brain injury in a practice or game shall be removed from competition at that time and for no less than twenty-four hours. X 4. A youth athlete who has been removed from play shall not return to competition until the athlete is evaluated by a licensed health care provider trained in the evaluation and management of concussions as defined in the guidelines developed under subsection 1 of this section and receives written clearance to return to competition from that health care provider Features of Concussion XDirect blow to head or elsewhere on the body with an “impulsive force transmitted to the head” XRapid onset of short lived impairment of neurologic function that resolves spontaneously 3rd International Conference on Concussion in Sport (Zurich, 2008) McCrory, et al 2009 Clin J Sport Med 2009; 19:185-200 Definition X “a complex pathophysiological process affecting the brain, induced by traumatic biomechanical forces” 3rd International Conference on Concussion in Sport (Zurich, 2008) McCrory, et al 2009 Clin J Sport Med 2009; 19:185-200 Definition XMay result in neuropathologic changes, but the acute clinical symptoms largely reflect a functional disturbance rather than a structural injury XMay or may not include loss of consciousness XNo abnormality is seen on standard structural neuroimaging 3rd International Conference on Concussion in Sport (Zurich, 2008) McCrory, et al 2009 Clin J Sport Med 2009; 19:185-200 2 05/18/2015 Epidemiology X Epidemiology Estimated 207,000 emergency room visits per year for sports related traumatic brain injury (TBI). X Children X X Football age 5-18 account for 65% of these visits. X Girls’ Centers for Disease Control MMWR. 2007; 56;733-7 X High School Sports Concussions 1.6-3.8 million estimated sports related TBIs occur each year 40.5% soccer 21.5% X Boys’ soccer 15.4% X Girls’ basketball 9.5% X Many do not seek care or are not treated by a physician Langlois J. J Head Trauma Rehab 2006. Epidemiology X High School X X Estimated 136,000 concussions per academic year 544 concussions recorded in online surveillance system during 2008-2009 X 57% involved in football X 84% resolution of symptoms in 1 week X 94% experienced headache X 24% had amnesia X 4.6% lost consciousness Meehan et al AJSM, published online Aug. 17, 2010 Gessel et al. J Athl Train, 2007 Pathophysiology of Concussion X Concussion results in a temporary neuronal dysfunction not cell death X Complex neurometabolic cascade occurs immediately and abnormalities are found for at least 7 days after a concussion occurs Giza and Hovda J of Athl Training, 2001. 3 05/18/2015 Pathophysiology of Concussion X Immediate release of glutamate which binds to NMDA receptor X Neuronal efflux of K+ and influx of Ca2+ X Increased Na+-K+ pump activity which increases demand of ATP Pathophysiology of Concussion X X X Giza and Hovda J of Athl Training, 2001. Biochemical Response to Concussive Blow Giza and Hovda in Neurologic Athletic and Spine Injuries 2000 Increased glucose metabolism and decreased cerebral blood flow lead to energy mismatch Decreased cerebral blood flow up to 50% is a likely mechanism for increased vulnerability to another concussion After initial metabolic state the brain goes in to hypometabolism, glycolysis, and increased lactate accumulation Giza and Hovda J of Athl Training, 2001. Cerebral Blood Flow Response to Concussive Blow X 12 children ages 11-15 with sports related concussion X Significant reduction in cerebral blood flow compared to controls X Only 27% improved to control levels at 14 days X 64% took greater than 30 days to return to control levels Maugans, et al. Pediatrics, 2012. 4 05/18/2015 Concussion Management X Three aspects of management X Starts exam with the pre-participation physical X Sideline X Return assessment to play decisions On Field & Sideline Evaluation Symptoms may be delayed X Exercise high suspicion because athletes often will deny symptoms X Diagnosis X Concussion should be suspected in the presence of any one or more of the following: X Symptoms X Physical (headache, etc.) signs (unsteadiness, etc.) X Impaired brain function (e.g. confusion) X Abnormal behavior 5 05/18/2015 Concussion Symptoms Concussion should be suspected in the presence of any one or more of the following: X Feeling “in a fog” X Difficulty concentrating X Difficulty remembering X “Pressure in head” Feeling slowed down Dizziness X Blurred vision Amnesia X Headache X Sensitivity to noise or light X X X X Neck pain X Nausea or vomiting Loss of consciousness X Seizure or convulsion X Concussion Symptoms X Balance Problems X Fatigue or low energy Percentage of Players with Concussion Reporting Moderate to Severe Symptoms at Time of Injury X Headache 85% X Dizziness/balance difficulties 77% X “Slowed Down” 69% X Decreased Concentration 60% X Sensitivity to Noise or Light 60% X Fatigue 55% X Memory Problems 45% X Confusion X Drowsiness X More emotional X Irritability X Sadness X Nervous or anxious Now that a Concussion is Suspected… X Remove from practice/game X Take the helmet or other required equipment X Monitor for deterioration X X Seizures X Impaired consciousness X Focal neurologic signs X Vomiting or worsening of headache X Increasing confusion or slurring of speech If these occur get athlete to ER ASAP! Guskiewicz, McCrea, et al. JAMA 2003; 290:2549-255 6 05/18/2015 Does a Suspected Concussion Need a Head CT? Recurrent Concussions X In a prospective cohort study of 4251 player seasons, 6.3% NCAA football players had a concussion X X 6.5% of these players had a repeat concussion the same season Players reporting a history of ≥3 concussions were 3x more likely to suffer a concussion than those with no history Guskiewicz K et al. JAMA 2003, 290: 2549-2555 Return to Play X Safety concerns for returning an athlete to play too soon X Current return to play guidelines Recurrent Concussions X 30% of those with history of ≥3 concussions had symptoms >1 week compared to 14.6% to those with 1 previous concussion X 11/12 who suffered a same season concussion occurred with 10 days of first injury X 9/12 occurred within first 7 days Guskiewicz K et al. JAMA 2003, 290: 2549-2555 7 05/18/2015 Special Considerations for Children Special Considerations for Children X A child’s brain is still developing in multiple ways X Children take longer to recover than older adolescents and adults X Physical activity X Recovery patterns have not been studied well in children <15 years old X Computer and video games X Television Recommend to hold out of activity until asymptomatic for a few days X Texting X Reading X School related activities X Special Considerations for Children X 90% of college athletes recover within 7 days but only 50% of high school athletes had completely symptom free at 7 days X Counsel on activities that can worsen symptoms Stepwise Return to Play X Each stage should take at least 24 hours X If symptoms return the patient should drop back to the previous level and rest for 24 hours before resuming progression McCrea et al. JAMA 2003. X Cognitive rest X Communication with teachers & school 8 05/18/2015 Stepwise Return to Play X X X Stage 1 Stepwise Return to Play X Stage 4 X No activity X Non-contact drills X Complete physical and mental rest until asymptomatic X May start resistance training X *Consider Neuropsych testing Stage 2 X Light aerobic exercise X Walking, swimming, stationary bike Stage 3 X Sport specific exercise which adds movement X Stage 5 X Stage 6 X X Full contact practice Return to competition 9 05/18/2015 Acute Knee Injuries History of Injury X Mechanism of Injury? X Discuss immediate symptoms X X Did they hear/feel a pop? X Did the knee immediately swell? X Where was the location of initial pain? X Were they able to bear weight or continue playing? Chronological description of symptoms up to the point of evaluation Questions I Always Ask X Current location of pain? X Are they having TRUE “locking”? X Any instability, looseness or wobbly feeling in the knee? X Any swelling or effusion? X X Meniscus tear, loose body Ligamentous injury, patellar dislocation X Immediate effusion suggests ACL tear X Slightly delayed effusion could be patellar dislocation, fracture, meniscus tear 10 05/18/2015 Effusion Traumatic Effusion=Get a MRI X Patellar Dislocation 2/3rds of the time the patient has suffered an ACL injury if there is immediate swelling after a twisting injury with a pop. Patellar Dislocation X Often caused by twisting episode X Patella usually spontaneously reduces X Treatment includes immobilization for 1-2 weeks followed by optional patellar stabilization brace X PT works to restore motion and improve strength X Recurrence after primary episode is 17% 11 05/18/2015 Hip and Pelvis Injuries X 12 yo felt a painful pop in right groin when kicking soccer ball X What Hip & Pelvis Injuries X Avulsion injuries to are possible at multiple growth plates in the pelvis X Anterior superior iliac spine (ASIS) X Anterior inferior iliac spine (AIIS) X Ischial tuberosity X X X X Sartorius origin is your differential? Treatment X Ice, NSAIDS, crutches, gentle stretching and range of motion X Return to sport 4-8 weeks when strength back to 90% of opposite side Rectus Femoris origin Hamstring origin Male athletes 14-17 yo, female athletes 12-15 yo 12 05/18/2015 Phases of Pitching X High valgus tension forces and high radial head/capitellum compression forces occur Little League Elbow (medial apophyseal injury) X Usually affects Little League age pitchers 9-12 years old X Repetitive valgus overload can lead to microtrauma in the medial epicondyle apophysis X Older pitchers with closed growth plates would stress their ulnar collateral ligament instead 13 05/18/2015 Little League Elbow (medial apophyseal injury) X Xrays of bilateral sides can show apophysis widening X Treatment is rest from throwing X Focus on core and posterior shoulder strengthening during rehab during period of rest Little Leaguer Shoulder – 13 yo “Little Leaguer’s Shoulder” X Widening of proximal humeral growth plate X Mild shoulder pain that increases with pitching X Xrays comparing bilateral sides can be helpful “Little Leaguer’s Shoulder” X Tx: No throwing for 6-8 weeks or until all pain resolved X Start core exercises immediately and start rotator cuff exercises once pain improved 14 05/18/2015 11 yo with heel pain Osgood Schlatter Disease Sever’s Disease (calcaneal apophysitis) X #1 Cause of heel pain in 8-12 year olds X Often occurs during/after rapid bone growth leaving the muscle/tendon complex tight X Xrays not necessary X Treatment includes ice, decreasing volume of activity, CAM boot if severe pain Osgood Schlatter Disease 15 05/18/2015 Patellofemoral Pain Syndrome Snapping Hip Iliopsoas tendon X One of most common adolescent musculoskeletal complaints X Often complain of vague anterior knee pain around patella X Worse with stairs, squatting, hills X Exam: Often quite normal. X IT band Single leg squats can illicit pain Images from Dr. Thomas Byrd, Nashville, TN 14 yo girl with left lateral hip pain Foam Roller – for IT Band stretching X Pain at left iliac crest playing volleyball. X Worse with twisting and jogging. X Pain comes and goes, worse during and after activity Bicycling.com 16 05/18/2015 Iliac crest apophysitis Iliac Crest Apophysitis Pitch Counts “When Can My Child Throw a Curveball?” www.stopsportsinjuries.org Jodieotte.com 17 05/18/2015 “When Can My Child Throw a Curveball?” Thanks! X Please email with questions at any time X [email protected] X Twitter - @MizzouSportsDoc www.stopsportsinjuries.org 18
© Copyright 2026