Management of Intracranial Pressure ICP Dynamics
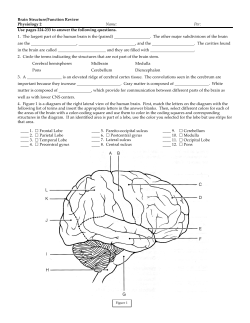
Management of Intracranial Pressure Thomas J. Wolfe, MD, and Michel T. Torbey, MD, MPH Corresponding author Thomas J. Wolfe, MD Department of Neurology, Medical College of Wisconsin and Froedtert Hospital, 9200 West Wisconsin Avenue, Milwaukee, WI 53226, USA. E-mail: [email protected] Current Neurology and Neuroscience Reports 2009, 9:477–485 Current Medicine Group LLC ISSN 1528-4042 Copyright © 2009 by Current Medicine Group LLC Although intracranial hypertension may arise from diverse pathology, several basic principles remain paramount to understanding its dynamics; however, the management of elevated intracranial pressure (ICP) may be very complex. Initial management of common ICP exacerbants is important, such as addressing venous outflow obstruction with upright midline head positioning and treating agitation and pain with sedation and analgesia. Surgical decompression of mass effect may rapidly improve ICP elevation, but the impact on outcome is unclear. Considerable effort has been put forth to understand the roles of multimodal intensive care monitoring, osmolar therapy, cerebral metabolic suppression, and temperature augmentation in the advanced management of elevated ICP. Establishing a protocol-driven approach to the management of ICP enables the rapid bedside assessment of multiple physiologic variables to implement appropriate treatments, which limit the risk of developing secondary brain injury. Introduction Numerous neurologic and nonneurologic diseases may contribute to the formation of intracranial hypertension. Through advances in emergency response systems and neuroimaging, the rapid identification of these patients has become easier, allowing for earlier initiation of treatment. Recent technical innovations in neuromonitoring and the establishment of specialized neurointensive care units may allow for improvements in morbidity and mortality rates attributable to elevated intracranial pressure (ICP). We present a review of ICP physiology and data to support the evidence-based management of these patients. In addition, we present a possible treatment algorithm for refractory intracranial hypertension, incorporating the application of multimodal monitoring in the neurointensive care unit. ICP Dynamics The cranial vault of a normal adult is a noncompliant structure containing an average volume of approximately 1500 mL, comprising 88% brain matter, 7.5% blood, and 4.5% cerebrospinal fluid (CSF) [1]. The Monroe-Kellie hypothesis contends that to maintain a constant ICP, any increase in the volume of an intracranial element must be met with an equal compensatory decrease in the volume of another component, or pressure will increase. Because of the skull’s noncompliance, uncompensated changes in the volume of any given component may have an impact on ICP, with a potential exponential increase in ICP. Normal ICP is not constant throughout life; healthy adults and older children have a normal ICP of 10 to 15 mm Hg, whereas the ICP of young children and infants is more than half this value [2,3]. There is level II evidence to support treatment initiation if ICP levels remain persistently above 20 mm Hg [4]. For the purposes of this review and the proposed treatment algorithm (Fig. 1), sustained ICP elevation greater than 20 mm Hg without stimulation fulfi lls the criteria for intervention. Cerebral blood flow and perfusion pressure The brain receives 15% to 20% of total cardiac output, which at rest is approximately 800 mL/min, and absorbs 25% of all oxygen consumed by the body [5]. Systemic mean arterial perfusion pressure (MAP) is the most important factor in maintaining cerebral perfusion. Cerebral perfusion pressure (CPP), the pressure at which the brain is perfused, is determined by taking the difference between MAP and ICP (CPP = MAP – ICP), where MAP = (1/3 systolic blood pressure [BP]) + (2/3 diastolic BP). Normally, cerebral blood flow (CBF) is estimated to be 50 mL/100 g per minute. When CBF falls below 12 mL/100 g per minute, irreversible ischemic injury occurs [5]. Maintaining a constant CBF depends on autoregulation, a complex system of arterial and venous modulation. Autoregulation has three main levels of control: myogenic, metabolic, and neurogenic [5,6]. Pressure autoregulation refers to the cerebrovascular system’s ability to maintain normal levels of CBF with CPP between 50 and 150 mm Hg, mediated mainly by the variable vascular resistance of arteriolar myogenic responses. The metabolic regulation of arteriolar vascular resistance is variably affected by CO2, O2, pH/lactate formation, adenosine, and nitric oxide. Neurogenic regulation refers to sympathetic tone on the cerebral arteries leading to mild tonic vasoconstriction, allowing for higher limits on the autoregulation curve; in contrast, the 478 I Critical Care Figure 1. Medical College of Wisconsin algorithm for the management of increased intracranial pressure (ICP). Multimodal monitoring and second-tier therapies can be introduced for refractory elevations in ICP. CPP—cerebral perfusion pressure; EAC—external auditory canal; Hct—hematocrit; MAP—mean arterial pressure; PtO2—parenchymal oxygen partial pressure; SjO2—jugular bulb venous oxygen saturation. parasympathetic nervous system plays little role in cerebral autoregulation [5]. Measuring the limits of cerebral vascular autoregulation is possible using transcranial Doppler technology by comparing beat-to-beat spontaneous variability in systemic BP with CBF velocities [6]. If CPP levels fall below the lower limit of autoregulation, CBF will fall and contribute to oligemia. If CPP exceeds the upper limit of autoregulation, an excess of CBF would occur beyond the metabolic necessity of the brain. This is an uncoupled increase in CBF, or luxury perfusion. Recent animal data suggest that the lower limit of cerebral autoregulation rises as ICP increases, which might mandate a progressively higher CPP goal to maintain constant CBF [7]. Causes of elevated ICP Acute identification and treatment of the primary cause of elevated ICP are necessary to reduce the risk of developing further secondary injury, and other, secondary causes of ICP elevation also must be addressed [8]. Common causes of ICP elevation are outlined in Table 1. Patterns of ICP elevation The natural history of intracranial hypertension depends on the underlying pathogenesis. In traumatic brain injury with a mass lesion, elevations in ICP may present acutely, prompting urgent surgical intervention. In a prospective evaluation of the time course of intracranial hypertension following traumatic brain injury (TBI), half the patients had their highest ICP within 3 days of the injury, whereas 25% had the highest mean ICP after 5 days [9]. The patients who experienced the later peak in ICP tended to have a poorer clinical grade and were more refractory to treatment. O’Phelan et al. [10] also described a significant number of patients who experienced late peak rises in ICP, and identified four patterns of ICP elevation following severe TBI: increases beginning within 72 hours (early); increases beginning after 72 hours (late); early Management of Intracranial Pressure I Wolfe and Torbey I 479 Table 1. Causes of elevated intracranial pressure Primary intracranial pathology Primary extracranial pathology Traumatic injury (contusion, diffuse axonal injury) Hypoxia Intracranial hemorrhages (epidural, subdural, subarachnoid, parenchymal, tumoral) Hypercarbia Ischemic infarction with cytotoxic edema Hypertension Neoplasm and associated vasogenic edema Hyponatremia Hydrocephalus Jugular venous obstruction Infection (meningitis, encephalitis, abscess, neurocysticercosis, malaria) Agitation and valsalva Status epilepticus Mechanical ventilation (when peak end expiratory pressure > baseline intracranial pressure) Postoperative: hemorrhage, retraction, edema, or cerebrospinal fluid obstruction Hyperpyrexia Convulsive seizure or depolarizing paralytic Hepatic failure High-altitude cerebral edema Toxins and medications (lead, tetracycline, doxycycline, rofecoxib, retinoic acid) increases with resolution, followed by a second rise after 72 hours (bimodal); and continuously increased ICP. Disease processes that develop delayed edema formation (eg, ischemic stroke, hematomas) may require extended monitoring periods, with cranial imaging to guide the discontinuation of monitoring. Prolonged ventriculostomy use or permanent CSF shunt placement may be required for hydrocephalus following subarachnoid hemorrhage or mass effect onto the normal CSF-draining pathway. ICP Monitoring Indications for ICP monitoring Headache, nausea and vomiting, somnolence, and pupillary dilatation are signs of elevated ICP. Although papilledema is a specific indicator of intracranial hypertension, it may be present only in a minority of patients [8]. Imaging guidance (midline shift, effaced basal cisterns) also may assist in the identification of patients with a suspected increase in ICP, but significant ICP elevations may occur without these fi ndings. The Brain Trauma Foundation has formulated guidelines for the use of ICP monitors, helping standardize the approach to their placement [11]. Level II evidence exists to support monitoring in all salvageable patients with a severe TBI (Glasgow Coma Scale score of 3–8 after resuscitation) and an abnormal CT scan. An abnormal CT scan of the head is defi ned as one that reveals hematomas, contusions, swelling, herniation, or compressed basal cisterns. Level III evidence supports monitoring in patients with severe TBI who have a normal CT scan, if two or more of the following features are noted at admission: age over 40 years, unilateral or bilateral motor posturing, or systolic BP less than 90 mm Hg. Some variability exists in patient selection for the placement of an ICP monitor because of the lack of prospective randomized trials sup- porting their role. Shafi et al. [12•] reported a retrospective analysis of the National Trauma Data Bank suggesting a 45% reduction in survival when ICP monitoring was performed according to guidelines similar to those stated previously; only 43% of patients meeting guideline criteria underwent ICP monitoring. The significance of this fi nding is unclear and may represent morbidity related to the treatment prompted by monitoring, or may suggest that the patient’s severity of injury was overestimated at the time of monitor placement. Guidelines for the use of ICP monitoring for pathology other than trauma are less clearly established. However, adopting inclusion criteria similar to those used for TBI may help guide appropriate application in patients with nontraumatic intracranial hypertension. Clinical deterioration and imaging consistent with mass effect may serve as important selection criteria. ICP monitors and waveforms Various intracranial monitoring devices exist, with the ventricular drain being the gold standard [8]. Ventricular catheters can be zeroed repetitively, whereas parenchymal or subarachnoid bolt strain monitors are subject to delayed drift and cannot be re-zeroed after placement. Ventricular catheters also offer a therapeutic function, allowing CSF volume reduction. Normal ICP waveforms are similar to the arterial waveform, with a fi rst peak correlating with systole, a second peak correlating with aortic valve closure, and a third peak correlating with antegrade arterial flow during diastole; with reduced brain compliance, the second peak may be higher than the fi rst. Self-perpetuating ICP elevations (plateau waves) may occur when reductions in CBF lead to vasodilation and subsequent increases in ICP that in turn impair CBF, ultimately leading to further vasodilation and increases in ICP. 480 I Critical Care Initial Clinical Management of ICP The initial management of patients suspected of having elevated ICP should include resuscitation to ensure airway protection, normal oxygenation monitored with pulse oximetry and arterial blood gases (O2 saturation > 90% or Pao2 > 60 mm Hg), and systolic BP greater than 90 mm Hg. Insurance of euvolemia and strict monitoring of in/out balance with a Foley catheter are necessary. Head of bed should be maintained at 30°, and the patient’s head should remain in midline positioning, without jugular compression, to promote venous return. For patients with loss of consciousness and cranial imaging abnormalities, prophylactic antiepileptic medication should be considered to limit the possibility of seizure-related ischemia and hypertension. Sedation should be initiated (allowing for clinical assessments) and paralysis considered; the use of non-depolarizing paralytics is preferred to avoid ICP elevations associated with muscular contraction. Hyperventilation should be used only acutely to achieve Pco2 of approximately 33 mm Hg; prolonged hyperventilation should be avoided because of the sustained changes in autoregulation that may occur, and extensive acute reduction in Pco2 may cause vasoconstriction, contributing to cerebral ischemia. The initial CPP goal should be maintained at greater than 60 mm Hg; values less than 60 mm Hg may be associated with worsened mortality [13], although CPP greater than 70 mm Hg has not been shown to improve outcome [14]. Surgical Intervention Surgical decompression of an intracranial space-occupying lesion remains an acute intervention that can have an immediate impact on ICP elevations that are refractory to medical therapies, often with a durable effect. Decompressive craniectomy has been evaluated as the primary surgical intervention for hemorrhagic contusion following TBI, illustrating safety and efficacy, with reductions in both mortality and the need for additional surgery [15]. Although patients undergoing craniectomy had somewhat improved outcomes compared with those undergoing craniotomy with focal lesion evacuation, there was no difference in hospital or rehabilitation length of stay. A 40% rate of improved outcome in patients undergoing craniectomy for severe TBI has been seen, with older age as a potential exclusionary criterion [16]. The impact of decompressive craniectomy on cerebral oxygenation, vascular reactivity, and neurochemistry following severe TBI was assessed, suggesting that in patients who had good functional outcomes, these physiologic parameters normalized [17]. These fi ndings may offer insight into factors that can help aid in prognostication. The HAMLET (Hemicraniectomy After Middle Cerebral Artery Infarction With Life-Threatening Edema) trial specifically enrolled patients with middle cerebral artery infarction and life-threatening mass effect from edema prospectively at multiple centers [18]. This trial in 64 patients found an absolute risk reduction in mortality of 38%. In addition, poor outcomes may be reduced if the procedure is performed within 48 hours of stroke onset, a benefit that may not persist if delayed up to 96 hours; this benefit on functional outcome has not been validated. The RESCUEicp (Randomised Evaluation of Surgery With Craniectomy for Uncontrollable Elevation of Intra-Cranial Pressure) trial is an international multicenter prospective randomized trial that will assess the efficacy of craniectomy in the management of ICP elevation attributable to many different causes [19••]. As of April 2009, one third of an anticipated 600 patients were enrolled. Once completed, this study should help defi ne the role of craniectomy in ICP management. Although surgery may have an acute impact on ICP, its use in the management of ICP should be considered on an individual basis, as the effect on meaningful outcome has not been fully proven for all patients. Second-Tier Medical Management of ICP When ICP elevations remain refractory to initial medical therapy and the patient does not meet surgical criteria, or if the pressure remains elevated following surgery, more intensive measures must be implemented. No large prospectively validated randomized trials have been performed to evaluate the use of multimodal monitoring on outcome, or the relative efficacy of one intervention over the others. Despite this limitation, the application of these interventions and newer technology allow for improving goal-directed care. Forming an evidence-based treatment algorithm enables the rapid interpretation of multiple physiologic parameters. Figure 1 is an example of the protocol employed at our institution. Some potential adverse effects encountered during ICP management are outlined in Table 2. Multimodal monitoring Multimodal neuromonitoring may allow insight into the deranged cerebral metabolic balance that occurs following a brain injury or stroke. Although the measurement of ICP and evaluation of CPP remain the foundation of current intracranial hypertension management, the adjunctive use of more complex monitoring methodology may help limit secondary injury. CBF is closely linked to the metabolism of oxygen, and the arteriovenous difference in oxygen content (AVTO2) can be measured to evaluate the adequacy of cerebral perfusion. The monitoring of a jugular bulb venous oximetry (SjO2) can be achieved with bedside catheter placement and provides a continuous estimate of cerebral venous oxygen saturation; suggested normal values for SjO2 range from 50% to 65% [20]. In Figure 1, strict SjO2 targets are set higher to reduce the chances of hypoxemia. If frequent or sustained hyperventilation is utilized, SjO2 monitoring may help prevent vasoconstriction-related ischemia. Similarly, when cerebral perfusion is inadequate or below the lower threshold for Management of Intracranial Pressure I Wolfe and Torbey I 481 Table 2. Some potential adverse effects associated with intracranial pressure treatments Treatment Adverse effects Seizure prophylaxis Encephalopathy Sedation Neuromuscular blockade/chemical paralysis Loss of clinical examination Myopathy Prolonged paralysis Raised intracranial pressure (with muscular contraction from depolarizing blockers) Hyperventilation Vasoconstriction-related ischemia Chronic changes in autoregulation Intracranial pressure monitoring Intracranial hemorrhage (epidural, subdural, parenchymal, ventricular) Infection Pain at insertion site Mannitol/osmotic diuretics Congestive heart failure Volume depletion Pulmonary and peripheral edema Electrolyte abnormalities (pseudo-hyponatremia) Osmotic nephropathy (especially when volume depleted) Hypertonic saline Congestive heart failure Hypotension (during bolus) Pulmonary and peripheral edema Hyperchloremic metabolic acidosis Osmotic myelinolysis Rebound edema on discontinuation Pharmacologic metabolic suppression Barbiturates Sedation/loss of clinical examination Respiratory depression and hypercarbia Hypotension and cardiac suppression Infection Propofol Similar to barbiturates Propofol infusion syndrome Acute refractory bradycardia leading to asystole, with one or more of the following: Metabolic acidosis Rhabdomyolysis Hyperlipidemia (triglycerides) Enlarged or fatty liver Therapeutic hypothermia Electrolyte abnormalities (hypokalemia, hypocalcemia) Cardiac suppression, both atrial and ventricular arrhythmias (including asymptomatic electrocardiographic changes) Infection due to immune suppression Reduced creatinine clearance (during the active phase of hypothermia) Pancreatitis autoregulation, low levels of SjO2 and high AVTO2 might represent excessive O2 extraction. With pressure-passive elevations of ICP, when the upper limit of autoregulation is exceeded or autoregulation is lost, high values of SjO2 482 I Critical Care and low AVTO2 may be seen because of an uncoupled increase in luxury perfusion. The exact significance of parenchymal oxygen tension (PbO2) is unclear, but its application in ICP management is important. It has been seen that SjO2 of approximately 50% correlates with PbO2 of approximately 8.5 mm Hg (range, 3–12 mm Hg); PbO2 is possibly a more durable method for longer monitoring [21]. In a small cohort of TBI patients, it was determined that measurements of PbO2 more accurately represented CBF and the cerebral AVTO2 than direct measurement of total cerebral oxygen delivery or oxygen metabolism [22]. If this relationship is validated, these fi ndings may preempt the need for SjO2 or AVTO2 monitoring while PbO2 is being assessed, especially in patients with cervical spine injury or cerebral venous occlusion. In a larger prospective trial implementing treatment thresholds of PbO2 greater than 20 mm Hg and ICP greater than 20 mm Hg, reduced mortality rates were seen using an ICP/PbO2-directed protocol [23]. Improved 6-month outcomes over standard ICP/CPP therapy also were seen. The assessment of autoregulation also may be possible through oxygen pressure reactivity assessment, which correlates with cerebrovascular pressure reactivity [24]. These detailed evaluations may be appropriate mostly for patients with refractory ICP despite escalating therapies and require additional data processing hardware. Electrophysiologic monitoring in the neurointensive care unit is common. Recently, the concept of detecting neurologic deterioration using electroencephalography and somatosensory evoked potentials was defi ned [25]. Of the patients in this study who had elevations in ICP, 68% had worsening of evoked responses either before or during the worsened ICP. Interpretation of these bedside data could allow earlier thresholds for initiating an additional level of therapy. Intraparenchymal electrographic recording has been introduced as an addition to the multimetric bolt monitors. This technology may allow for detection of seizure activity surface electroencephalography cannot discern because of the underlying brain injury. Cerebral microdialysis is another method that is being refi ned for the evaluation of metabolism and biochemistry. Microdialysis catheters are placed within the parenchyma, and with the use of variably sized semipermeable membranes, molecules are collected and evaluated. Markers of glucose metabolism (lactate, pyruvate), excitotoxicity (glutamate), and membrane breakdown (glycerol) are most commonly evaluated using microdialysis [26•]. Although monitoring of microdiasylate glucose and lactate concentrations might help with tailoring glycemic control, the exact role of this evaluation in the routine management of ICP is not clear at this time. Osmolar therapy The blood–brain barrier (BBB) is relatively impermeable to most low molecular weight solutes present in blood (pre- dominantly sodium and chloride), as well as to the plasma proteins. The permeability of an osmotic agent across a semipermeable membrane such as the BBB is quantified by a reflection coefficient, where values approaching 0 represent high permeability and those approaching 1 have low permeability [27]. Therefore, an increase in plasma osmolality always leads to decreases in brain parenchymal fluid volume. The most frequently used osmoles today are mannitol and sodium (reflection coefficient ~ 0.9 and 1, respectively). Other osmolar solutes, such as glycerol, sorbitol, and urea, have lower reflection coefficients and may lead to increases in parenchymal total fluid volume after diffusing into the brain and exerting osmotic pressure. Analysis of perfusion imaging may allow insight into the integrity of the BBB following brain injury [28], possibly offering a marker for limitations on osmolar therapy use. Additional effects may be imparted by mannitol and hypertonic saline. Mannitol has been found to upregulate subsets of cerebral aquaporin receptors, which may facilitate the redistribution of water between normal and abnormal regions of the brain [29]. Hypertonic saline may also contribute to increases in CBF [30]. The rate of administration of an osmolar load may affect the efficacy of lowering ICP. Sustained administration and lower weight-based dosing of mannitol have been shown to have a less pronounced and less enduring impact on elevated ICP [31•]. Bolus dosing may create a higher osmolar gradient across the BBB, ultimately inducing a larger decrease in parenchymal fluid. When the efficacy of mannitol was compared with that of hypertonic saline, there was a significant decrease in ICP from hypertonic saline compared with mannitol, along with significant increases in MAP and CPP; improvements in cerebral oxygenation also have been seen with hypertonic saline [32]. This difference may be explained by the diuretic effect of mannitol, causing reductions in intravascular volume. Following initial dosing of mannitol during resuscitation, the adjunctive use of hypertonic saline should be considered for persistent ICP elevations. In refractory cases, mannitol and hypertonic sodium may be alternated or given simultaneously. Monitoring the serum osmolar gap is helpful for monitoring the extent of mannitol administration and estimating serum concentration. After initiating osmolar therapy with mannitol, the measured serum osmolality goal traditionally has been 320 mOsm/L. However, with the use of hypertonic sodium solutions for elevated ICP occurring more commonly, standardized osmolality goals may become obsolete. A more rational approach may be the osmolar gap calculation—gap = measured – calculated osmolality; calculated osmolality = (2Na) + (glucose/18) + (blood urea nitrogen/2.8)—to estimate serum levels and guide the administration of mannitol [33]. Gap values less than 10 would suggest it is safe for administration of additional mannitol, with an increased risk of adverse effects if gap persists at greater than 20. If hyperchloremic metabolic acidosis develops with hypertonic saline administration, hypertonic sodium Management of Intracranial Pressure bicarbonate solutions may serve as an effective alternative [34]; partial or complete substitution of chloride for acetate (bicarbonate equivalent) is another alternative. Metabolic suppression Metabolic suppression may be used to treat elevations in ICP, assuming tissue viability and coupling of blood flow to the metabolic demand of the brain. By inducing a reduced metabolic requirement, the amount of blood flow required by the brain also is reduced. Additional excitotoxic processes also may be attenuated. Here, more emphasis has been placed on therapeutic hypothermia, which is an emerging therapy compared with pharmacologic suppression. Pharmacologic suppression Barbiturate therapy to induce electroencephalographic burst suppression has been a mainstay of pharmacologic metabolic suppression for elevated ICP, although it is not indicated for prophylactic administration [35]. Signifi cant morbidity may be associated with this therapy and should be reserved for cases of ICP refractory to standard fi rst-line medical care, and hemodynamic stability is mandatory before and after induction. Traditionally, an electroencephalogram has been used to monitor neural activity, although this may be assessed using bispectral index monitoring to allow for easier evaluation [36], especially in non–neurointensive care units. Barbiturate coma may lower ICP and improve cerebral oxygenation [37]. This improvement in cerebral oxygenation has been partly validated in additional reports, although in areas of impaired cerebral physiology, worsening oxygenation may be seen [38]. The worsening may reflect difficulties maintaining adequate CPP in regions of the brain with impaired autoregulation. Propofol, along with other sedative/hypnotics, has been used to induce sedation and coma in place of barbiturates, demonstrating safety and efficacy [35,39]. In addition to neural suppression caused by activation of the J-aminobutyric acid A receptor and inhibition of the N-methyl-d-aspartate receptor, propofol may have a direct neuroprotective effect [40]. The beneficial effects of propofol may be countered by cardiovascular suppression affecting CPP, leading to reduced cerebral flow in areas with impaired autoregulation. Therapeutic hypothermia and temperature augmentation Fever is common following brain injury, and avoidance of hyperthermia may be an important part of the management of brain injury from any cause [41•,42,43]. Intracranial temperature has been shown to be higher than core body temperature [42], representing an important treatment consideration because of the relationship between elevations in ICP and intracranial temperature. Fever reduction in acute brain injury also may significantly reduce systemic metabolic demand, although this may depend on control of shivering [43]. The adverse effects of temperature elevations above 37°C may be mediated by I Wolfe and Torbey I 483 multiple pathogenic mechanisms, including excitotoxicity, free radical generation, inflammation, apoptosis, and genetic differences in response to injury [44]. The application of mild therapeutic hypothermia, maintaining core body temperature near 33°C, is a novel strategy used to provide neuroprotection following brain injury in many clinical scenarios presenting with coma [41•]. Several modalities are available for the induction of hypothermia: external cooling devices, intravenous cold saline infusion, and intravascular cooling catheters. Each of these methods is associated with individual risks and benefits. There may be a treatment window for hypothermia induction to impart measurable clinical benefit, with a possible lack of benefit seen in instances of delayed application for TBI [45]. The rate of rewarming is another important aspect in treatment efficacy, with elevations beyond normothermia potentially imparting deleterious effects because of impaired cerebrovascular regulation [41•,46•,47]. Although initial reports supported the role of hypothermia induced within 6 hours of TBI, subsequent studies failed to show a benefit on neurologic recovery [48]. Patients with ICP elevations refractory to standard osmolar therapy may benefit from hypothermia, but any benefit over medication-induced metabolic suppression is unclear [49]. It is possible that if a patient fails to improve with pharmacologic metabolic suppression, there may not be any further improvement following induction of hypothermia, although it may act synergistically when a response is seen. If hypothermia is applied in the setting of refractory elevations in ICP, further reduction in temperature beyond 32°C has not been shown to impart further efficacy, and more complications may be encountered [50]. However, if recurrent elevations in ICP are encountered during rewarming, slowing the rate of rewarming or extending the duration of hypothermia may be necessary. This may pose a problem with regard to accurately assessing neurologic prognosis in a timely manner, because sedatives and paralytics often are required during hypothermia. Conclusions Recent advances in technology have allowed significant improvement in the management of intracranial hypertension. Using bedside physiologic data, including ICP transduction and waveform analysis and monitoring of SjO2 , PbO2 , and cerebral temperature, optimization of cerebral perfusion and oxygenation and prevention of additional secondary injury may be possible. Establishing protocols to aid in the management of intracranial hypertension may improve the quality of care through standardization of treatment, based on real-time physiologic analysis. Acknowledgment Dr. Wolfe is the 2009–2010 Daniel M. Soref Clinical Neurosciences fellow. 484 I Critical Care Disclosure No potential confl icts of interest relevant to this article were reported. References and Recommended Reading Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance Dóczi T: Volume regulation of the brain tissue—a survey. Acta Neurochir (Wien) 1993, 121:1–8. 2. Welch K: The intracranial pressure in infants. J Neurosurg 1980, 52:693–699. 3. Downard C, Hulka F, Mullins RJ, et al.: Relationship of cerebral perfusion pressure and survival in pediatric braininjured patients. J Trauma 2000, 49:654–658. 4. Bratton SL, Chestnut RM, Ghajar J, et al.: Intracranial pressure thresholds. J Neurotrauma 2007, 24(Suppl 1):55–58. 5. Franco Folino A: Cerebral autoregulation and syncope. Prog Cardiovasc Dis 2007, 50:49–80. 6. van Beek AH, Claassen JA, Rikkert MG, Jansen RW: Cerebral autoregulation: an overview of current concepts and methodology with special focus on the elderly. J Cereb Blood Flow Metab 2008, 28:1071–1085. 7. Brady KM, Lee JK, Kibler KK, et al.: The lower limit of cerebral blood flow autoregulation is increased with elevated intracranial pressure. Anesth Analg 2009, 108:1278–1283. 8. Rangel-Castilla L, Gopinath S, Robertson CS: Management of intracranial hypertension. Neurol Clin 2008, 26:521–541. 9. Stocchetti N, Colombo A, Ortolano F, et al.: Time course of intracranial hypertension after traumatic brain injury. J Neurotrauma 2007, 24:1339–1346. 10. O’Phelan KH, Park D, Efi rd JT, et al.: Patterns of increased intracranial pressure after severe traumatic brain injury. Neurocrit Care 2009, 10:280–286. 11. Bratton SL, Chestnut RM, Ghajar J, et al.: Indications for intracranial pressure monitoring. J Neurotrauma 2007, 24(Suppl 1):37–44. 12.• Shafi S, Diaz-Arrastia R, Madden C, Gentilello L: Intracranial pressure monitoring in brain-injured patients is associated with worsening of survival. J Trauma 2008, 64:335–340. The authors present controversial fi ndings suggesting that placement of intracranial monitoring devices based on criteria similar to current TBI guidelines may be associated with worsened clinical outcome. Although the validity is not clear, it reemphasizes the importance of considering patients individually for treatment, rather than strictly following a protocol. 13. Juul N, Morris GF, Marshall SB, et al.: Intracranial hypertension and cerebral perfusion pressure: influence on neurological deterioration and outcome in severe head injury. The Executive Committee of the International Selfotel Trial. J Neurosurg 2000, 92:1–6. 14. Bratton SL, Chestnut RM, Ghajar J, et al.: Cerebral perfusion thresholds. J Neurotrauma 2007, 24(Suppl 1):59–64. 15. Huang AP, Tu YK, Tsai YH, et al.: Decompressive craniectomy as the primary surgical intervention for hemorrhagic contusion. J Neurotrauma 2008, 25:1347–1354. 16. Morgalla MH, Will BE, Roser F, Tatagiba M: Do longterm results justify decompressive craniectomy after severe traumatic brain injury? J Neurosurg 2008, 109:685–690. 17. Ho CL, Wang CM, Lee KK, et al.: Cerebral oxygenation, vascular reactivity, and neurochemistry following decompressive craniectomy for severe traumatic brain injury. J Neurosurg 2008, 108:943–949. 1. Hofmeijer J, Kappelle LJ, Algra A, et al.: Surgical decompression for space-occupying cerebral infarction (the Hemicraniectomy After Middle Cerebral Artery infarction with Life-threatening Edema Trial [HAMLET]): a multicentre, open, randomised trial. Lancet Neurol 2009, 8:303–304. 19.•• Hutchinson PJ, Corteen E, Czosnyka M, et al.: Decompressive craniectomy in traumatic brain injury: the randomized multicenter RESCUEicp study (www.RESCUEicp.com). Acta Neurochir Suppl 2006, 96:17–20. This prospective randomized trial has not completed enrollment, but when accrual is complete, it will serve as one of the highest powered analyses of decompressive craniotomy for ICP elevation developing from multiple etiologies. These data will generally reflect global practice patterns, but subgroup analyses may further yield varying efficacy for specific causes of elevated ICP. 20. Robertson CS, Contant CF, Gokaslan ZL, et al.: Cerebral blood flow, arteriovenous oxygen difference, and outcome in head injured patients. J Neurol Neurosurg Psychiatry 1992, 55:594–603. 21. Kiening KL, Unterberg AW, Bardt TF, et al.: Monitoring of cerebral oxygenation in patients with severe head injuries: brain tissue PO2 versus jugular vein oxygen saturation. J Neurosurg 1996, 85:751–757. 22. Rosenthal G, Hemphill JC, Sorani M, et al.: Brain tissue oxygen tension is more indicative of oxygen diffusion than oxygen delivery and metabolism in patients with traumatic brain injury. Crit Care Med 2008, 36:1917–1924. 23. Narotam PK, Morrison JF, Nathoo N: Brain tissue oxygen monitoring in traumatic brain injury and major trauma: outcome analysis of a brain tissue oxygen-directed therapy. J Neurosurg 2009 May 22 (Epub ahead of print). 24. Jaeger M, Schuhmann MU, Soehle M, Meixensberger J: Continuous assessment of cerebrovascular autoregulation after traumatic brain injury using brain tissue oxygen pressure reactivity. Crit Care Med 2006, 34:1850–1852. 25. Amantini A, Fossi S, Grippo A, et al.: Continuous EEG-SEP monitoring in severe brain injury. Neurophysiol Clin 2009, 39:85–93. 26.• Tisdall MM, Smith M: Cerebral microdialysis: research technique or clinical tool. Br J Anaesth 2006, 97:18–25. Microdialysis is an emerging technique that is currently very labor intensive, making its widespread use difficult. Assuming its clinical utility continues to be demonstrated, this technique may theoretically become bundled in a single multimodal monitoring device. 27. Bhardwaj A: Osmotherapy in neurocritical care. Curr Neurol Neurosci Rep 2007, 7:513–521. 28. Dankbaar JW, Hom J, Schneider T, et al.: Dynamic perfusion CT assessment of the blood-brain barrier permeability: fi rst pass versus delayed acquisition. AJNR Am J Neuroradiol 2008, 29:1671–1676. 29. Arima H, Yamamoto N, Sobue K, et al.: Hyperosmolar mannitol simulates expression of aquaporins 4 and 9 through a p38 mitogen-activated protein kinase-dependent pathway in rat astrocytes. J Biol Chem 2003, 278:44525–44534. 30. Tseng MY, Al-Rawi PG, Pickard JD, et al.: Effect of hypertonic saline on cerebral blood flow in poor-grade patients with subarachnoid hemorrhage. Stroke 2003, 34:1389–1396. 31.• Keyrouz SG, Dhar R, Diringer MN: Variation in osmotic response to sustained mannitol administration. Neurocrit Care 2008, 9:204–209. This article highlights the importance of rapidly establishing an osmolar gradient to optimize the efficacy of treatment, rather than just having an increase in serum osmolality occur. 32. Oddo M, Levine JM, Frangos S, et al.: Effect of mannitol and hypertonic saline on cerebral oxygenation in patients with severe traumatic brain injury and refractory intracranial hypertension. J Neurol Neurosurg Psychiatry 2009, 80:916–920. 33. García-Morales EJ, Cariappa R, Parvin CA, et al.: Osmole gap in neurologic-neurosurgical intensive care unit: its normal value, calculation, and relationship with mannitol serum concentrations. Crit Care Med 2004, 32:986–991. 18. Management of Intracranial Pressure Smith R, Thomas M, Brown J: Raised intra-cranial pressure—sodium bicarbonate as an alternative hyperosmolar treatment. J Neurosurg Anesthesiol 2008, 20:158. 35. Bratton SL, Chestnut RM, Ghajar J, et al.: Guidelines for the management of severe traumatic brain injury. XI. Anesthetics, analgesics, and sedatives. J Neurotrauma 2007, 24(Suppl 1):S71–S76. 36. Cottenceau V, Petit L, Masson F, et al.: The use of bispectral index to monitor barbiturate coma in severely brain-injured patients with refractory intracranial hypertension. Anesth Analg 2008, 107:1676–1682. 37. Thorat JD, Wang EC, Lee KK, et al.: Barbiturate therapy for patients with refractory intracranial hypertension following severe traumatic brain injury: its effects on tissue oxygenation, brain temperature and autoregulation. J Clin Neurosci 2008, 15:143–148. 38. Chen HI, Malhotra NR, Oddo M, et al.: Barbiturate infusion for intractable intracranial hypertension and its effect on brain oxygenation. Neurosurgery 2008, 63:880–886. 39. Kelly DF, Goodale DB, Williams J, et al.: Propofol in the treatment of moderate and severe head injury: a randomized, prospective double-blinded pilot trial. J Neurosurg 1999, 90:1042–1052. 40. Kotani Y, Shimazawa M, Yoshimura S, et al.: The experimental and clinical pharmacology of propofol, an anesthetic agent with neuroprotective properties. CNS Neurosci Ther 2008, 14:95–106. 41.• Polderman KH: Induced hypothermia and fever control for prevention and treatment of neurological injuries. Lancet 2008, 371:1955–1969. The author reviews multiple potential mechanisms for the efficacy of temperature augmentation and therapeutic hypothermia in neurologic diseases. 34. I Wolfe and Torbey I 485 Rossi S, Zanier ER, Mauri I, et al.: Brain temperature, body core temperature, and intracranial pressure in acute cerebral damage. J Neurol Neurosurg Psychiatry 2001, 71:448–454. 43. Hata JS, Shelsky CR, Hindman BJ, et al.: A prospective, observational clinical trial of fever reduction to reduce systemic oxygen consumption in the setting of acute brain injury. Neurocrit Care 2008, 9:37–44. 44. Dietrich WD, Bramlett HM: Hyperthermia and central nervous system injury. Prog Brain Res 2007, 162:201–217. 45. Markgraf CG, Clifton GL, Moody MR: Treatment window for hypothermia in brain injury. J Neurosurg 2001, 95:979–983. 46.• Lavinio A, Timofeev I, Nortje J, et al.: Cerebrovascular reactivity during hypothermia and rewarming. Br J Anaesth 2007, 99:237–244. This publication offers insight into important aspects of successfully implementing and completing a hypothermia protocol, to optimize the efficacy of the treatment. 47. Soukup J, Zauner A, Doppenberg EM, et al.: The importance of brain temperature in patients after severe head injury: relationship to intracranial pressure, cerebral perfusion pressure, cerebral blood flow, and outcome. J Neurotrauma 2002, 19:559–571. 48. Clifton GL, Miller ER, Choi SC, et al.: Lack of effect of induction of hypothermia after acute brain injury. N Engl J Med 2001, 344:556–563. 49. Polderman KH, Tjong Tjin Joe R, Peerdeman SM, et al.: Effects of therapeutic hypothermia on intracranial pressure and outcome in patients with severe head injury. Intensive Care Med 2002, 28:1563–1573. 50. Shiozaki T, Nakajima Y, Taneda M, et al.: Efficacy of moderate hypothermia in patients with severe head injury and intracranial hypertension refractory to mild hypothermia. J Neurosurg 2003, 99:47–51. 42.
© Copyright 2026