Annual Report - Morehead Memorial Hospital
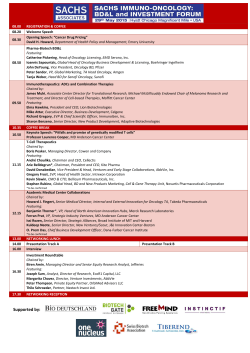
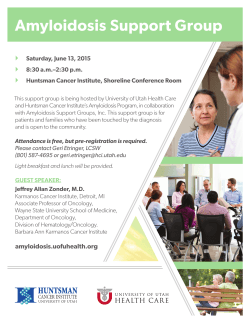
Morehead Memorial Hospital Cancer Program 2014 Annual Report using 2013 Statistical Data John Smith Jr. • Dalton McMichael Cancer Center John Smith, Jr.•Dalton McMichael Cancer Center The Smith-McMichael Cancer Center, built in 1994, was made possible by generous gifts from John Smith, Jr. and Dalton McMichael. According to the National Cancer Institute, Rockingham County was the 5th highest county in North Carolina for cancer incidence per capita. The Cancer Center, located on the Morehead Memorial Hospital campus, serves as an undeniable necessary resource for the citizens and neighbors of Rockingham County. The cancer program at Morehead Memorial Hospital, a community hospital, has repeatedly earned three-year accreditation by the American College of Surgeons (ACS) Commission on Cancer. Morehead Memorial Hospital is one of 53 hospitals in North Carolina with the ACoS accreditation. The Center has been continuously accredited since 1998. Since its inception, the commission’s goal has been to reduce the morbidity and mortality of cancer through education, standard setting and monitoring of quality of care. The standards continue to promote multidisciplinary and quality patient-centered care which we strive to uphold. Introduction The John Smith Jr-Dalton McMichael Cancer Center at Morehead Memorial Hospital marked a major milestone in 2014 as it commemorated the 20th anniversary of providing excellent services to our patients and their families. Since its inception, the Cancer Center continues to grow and flourish as it provides state-of-the-art cancer treatment to patients and their families in Rockingham County and the surrounding areas. It has been an exciting year in the Cancer Center and I would like to highlight some of the major accomplishments. The Cancer Center recently underwent a major transition as Novant Health became the managing entity of medical oncology. This change will maximize our resources, improve cancer care and provide long-term stability to the Cancer Center. The Cancer Center recently hired two full-time oncologists who provide exceptional care to the cancer patients. We were very fortunate to employ Dr. Boris Darovsky and Dr. Eric Neijstrom. They have both provided excellent cancer treatment to the patients of Rockingham County for many years. Dr. Kenneth Karb recently retired and he will certainly be missed. We wish him only the best in his new endeavor as the Medical Director of Hospice of Rockingham County. The Cancer Center is working hard to establish a Regional Breast Center and to obtain accreditation for the center. The Commission on Cancer of the American College of Surgeons conducted a survey of the cancer program at Morehead Memorial Hospital earlier this year. Dr. Frederick L. Greene a senior surgeon at Carolinas Medical Center performed the survey. He provided excellent feedback and information to help us to continue improving our Cancer Center and the services we provide. We were delighted to be awarded the highest accreditation for a three-year term. I feel very privileged to be a part of this exceptional cancer program and I am very optimistic regarding the future of the Cancer Center and Morehead Memorial Hospital. I am extremely impressed by the dedication and hard work of all the staff at the cancer center. In conclusion, I would just like to say "it's a New Day "at the John Smith Jr.-Dalton McMichael Cancer Center. We are committed to providing the most comprehensive, state of the art, and compassionate care for our cancer patients and their families. Over the next 20 years the Cancer Center will continue to expand and enhance the excellent services provided to meet the needs of our community. Marc DeMason, MD Cancer Committee Chairman Table of Contents Cancer Committee ............................................................................................ 2 Goals and Improvements .............................................................................. 3 Highlights of the Year ..................................................................................... 4 Diagnostic/Therapeutic Services ............................................................... 6 Support Services ............................................................................................... 7 Patient Education and Support ................................................................. 12 Community Education, Awareness and Screening Activities ....... 13 Professional Education ................................................................................ 14 Cancer Registry ............................................................................................... 15 2013 Cancer Registry Statistics ............................................................... 17 Endometrial Cancer: Comparison/Survival Data ............................. 20 Appendix ........................................................................................................... 22 1|Page Cancer Committee The Cancer Committee is a multidisciplinary group comprised of members from the diagnostic and therapeutic specialties. The committee guides the identification, development, implementation and evaluation of cancer-related activities at Morehead Memorial Hospital. The committee meets bimonthly to accomplish these activities. The following is a list of Cancer Committee members for 2014: Marc DeMason, MD, FACS, Surgery, Cancer Liaison Physician, Chair, Cancer Committee Boris Darovsky, MD, PhD, Medical Oncology Mark Jordan, MD, Pathology James Palermo, MD, Radiation Oncology William McLeod, MD, FRC(S)C, FACOG, OB/GYN Taylor Stroud, MD, Radiology Adaline Brown, RHIT, CCS, CTR, Cancer Registry Coordinator Torrey Goard, BS, Health Education Services Tamara Hunt, VP Physician and Ambulatory Services, Cancer Program Administrator Jonathan Terrell, MS, DABR Cancer Program Co-Administrator Jackie Largin, RN, BSN, OCN, Cancer Center, Clinical Team Leader Susan Netherland, RN, BSN, MBA, Quality Management Susie Pool, MS, RRT, Social Worker Cheryl Williams, BS, CME Coordinator, Cancer Conference Coordinator 2|Page Annual Goals and Improvements Clinical All newly diagnosed breast cancer patients are being followed up on after their diagnosis to ensure proper management of their disease. They are being referred to the surgeon for further evaluation and all patients presented at Tumor Board are being tracked by the assistant to the Pathologist. Programmatic Pursue accreditation as a NAPBC Breast Center • A subcommittee has been formed and had one meeting • Standards have been reviewed by all members • Accreditation for breast ultrasound will be submitted in January 2015 • A site visit was made to an accredited center • A meeting to explore offering genetic testing was held in December • Will plan to apply for accreditation in 2015. Improvements • Radiation Oncology updated their patient monitoring devices with consolidated flat screen displays thus allowing increased focus during treatment. • A blanket warmer was added to the Cancer Center to increase the comfort of our patients during their oncology treatments • Radiation Oncology recruited a resident Medical Physicist to manage the quality of patient treatment plans and delivery as well as manage the Radiation Oncology department. • Medical Oncology Pharmacist, Barry Siegel, adopted EPIC’s Beacon Oncology Software to follow Novant standards of treatment for highly emetogenic regimes. • Radiation Oncology amended policy to promote reporting of “Near-Miss” events in an effort to address potential pitfalls before they manifest themselves. This is a key component in promoting a culture of patient safety. 3|Page Highlights of the Year Resident Medical Physicist On June 9th, Morehead Memorial Hospital recruited Jonathan Terrell, M.S., DABR for the role of Medical Physicist and Radiation Oncology Manager. Jonathan joins the Smith McMichael Cancer Center touting 7 years of experience and board certification through the American Board of Radiology. Jonathan graduated from Appalachian State University with a Bachelor of Science in Applied Physics and Applied Mathematics in 2002 and a Master of Science in Applied Physics from the University of North Carolina at Charlotte in 2007. The position was previously staffed with a contracted physicist through Cone Health of Greensboro, NC. Shared Services Agreement with Novant Health On July 1st, Morehead Memorial Hospital entered into a shared services agreement with Novant Health. This relationship paved the way for the appointment of Howard Ainsley as our Chief Executive Officer. Mr. Ainsley joins us from Hilo, HI after serving as CEO for the East Hawaii Region of Hawaii Health Systems. Additionally, affiliation with Novant Health will offer Morehead increased negotiation leverage with outside vendors providing services to our health system. Certified Nurses Ensure Quality of Care The Smith-McMichael Cancer Center demonstrates an ongoing commitment to quality cancer care, professional development, and patient care by having five oncology certified nurses on staff; Jackie Largin, RN (clinical team leader), Tori Agee, RN, Ida Barnes, RN, Lynn Wilbourne, RN, and Karen Woods, RN, who received her certification in 2012. Bonnie Pritchett, RN maintains chemotherapy certification. To receive Accreditation with Commendation from the American College of Surgeons Commission on Cancer, at least 25% of chemotherapy trained nurses must hold a current oncology certification. Eighty-three percent of the chemotherapy nurses at The Smith-McMichael Cancer Center hold this certification. In Morehead Memorial Hospital’s most recent accreditation survey by DNV Healthcare, the surveyor noted that it was very unusual to have five certified nurses at a cancer center, particularly a small community facility. 4|Page Certification benefits patients, families, nurses and employers. Certification signifies to the patients and families that the nurse taking care of them or their loved ones has the knowledge, experience and expertise to do so. It strengthens patients’ confidence in the nurse and offers peace of mind at a time in their lives when things are so uncertain. Certification also offers both professional and personal accomplishment to the individual nurse. Novant Health Oncology Specialists In mid-December, Cone Health relinquished the medical oncology practice at the Smith McMichael Cancer Center to Novant Health. Formally titled Novant Health Oncology Specialists Eden, NHOSE leases approximately half of the physical space at the Cancer Center. With excellent management and continuity of care, NHOSE retained all previous Morehead medical oncology employees. Patients should expect to see familiar faces when returning for care. Aligning with Novant, Dr. Boris Darovsky and Eric Neijstrom set up shop as our resident medical oncologists. Dr. Darovsky returns to us after a brief sabbatical and Dr. Neijstrom joins us from Annie Penn Hospital in Reidsville, NC. Both physicians are highly regarded in the medical community and a true asset to Rockingham County and the surrounding population. New Physicians Join Morehead Staff New physicians who provide care to cancer patients joined the Medical Staff. They included: • Scott Humble, MD Pathology • Eric S. Neijstrom, MD Medical Oncology 5|Page Diagnostic/Therapeutic and Laboratory Services Diagnostic, therapeutic and laboratory services continue to provide a full scope of services to support the needs of the cancer program. Services are listed below: • Needle Localization • Ultrasound Guided Core Biopsy • Sentinel Node Injection • Diagnostic Imaging • CT Scanning • CT Guided Biopsy • Magnetic Resonance Imaging (MRI) • Nuclear Medicine • Digital Mammography • Bone Densitometry • Ultrasound • Hematology • Blood Chemistry • Blood Bank • Wide Variety of Pathology Services 6|Page Support Services Medical Oncology A cancer diagnosis changes a person’s life. It can be frightening and overwhelming. Patients and families are the primary focus of care. The Smith-McMichael Cancer Center takes pride in providing compassionate care in a constantly evolving environment. Medical oncologists and oncology nurses play an integral role in assisting patients and their families in their cancer journey. The complex needs of patients with cancer and their families require specialty competencies, knowledge and skill of the oncology nurses. The center is staffed with all registered nurses and is proud to report that 83% of the cancer center’s nurses are nationally certified. A multidisciplinary team approach is used to meet and deliver quality care to the cancer patient. Patient care is provided through collaboration between staff from medical oncology, radiation oncology, surgeons, pharmacy, social services, dietary services, rehabilitation services, home health services, the chaplain and hospice. The cancer patient interacts with the medical oncology nurse more than with any other member of the team and they become like family. The medical oncology nurse uses the standards, recommendations and guidelines from the Oncology Nursing Society to develop nursing policies and procedures to provide physical, emotional and psychological support to the patient and their family. The medical oncology nurses are challenged on a daily basis to deal with the numerous symptoms, including pain and fatigue, cancer patients experience as a result of their cancer or its treatments. Radiation Oncology The radiation oncology team utilizes 3-Dimensional Conformal, Intensity Modulated, Image Guided, and Electron Beam Radiation Therapies to accurately target and treat physician defined areas. Our seasoned team consists of a Receptionist, Nurse, Dosimetrist, Physicist, Radiation Therapists, and Radiation Oncologists. As part of recent transitions, our Receptionist is dedicated solely to the operations of radiation oncology. They are the first face you will see when you walk in the door. Daily interactions with staff will have them feeling like family. We truly pride ourselves in quality patient interactions and service from all areas of the department. 7|Page Nutritional Services While eating healthy is important to all of us, it is essential for those who are being treated for cancer. Eating a healthy diet can help a patient feel better, maintain strength and weight, increase energy levels, improve tolerance of treatment side effects, and improve the body’s immune function for decreased recovery and healing times. Both cancer and its treatment may affect the patient’s appetite and tolerance to certain foods. Therefore, all cancer patients and their families are provided medical nutrition therapy by a registered dietitian upon request from the patient, the physician, or another health care provider. This service includes: • A complete nutritional assessment to determine the patient's nutritional needs during cancer treatments and how to best meet those needs; • Education about the direct and indirect relationship of diet and cancer; and, • Nutrition counseling to assist patients in making dietary changes to improve their health and the outcome of their treatments. Rehabilitative Services Rehabilitative Services help to accelerate recovery and help patients achieve their maximum potential through physical therapy, occupational therapy, speech therapy and lymphedema therapy services. All therapies are provided in an acute care, skilled nursing facility and/or an outpatient facility. Lymphedema services require a physician’s referral to begin treatment. Patients will receive complete decongestive therapy including manual lymph drainage massage, compression bandaging, garment fitting/management, remedial exercises, and patient/caregiver education. Consultations for lymphedema risk/prevention are also given and require a physician referral. Most of the lymphedema services are provided in the outpatient setting, but can be performed in the other settings unique to Morehead Memorial Hospital. 8|Page Social Services The role of the social worker at the Smith-McMichael Cancer Center involves collaborating with other community agencies to meet the needs of the patients, community and hospital. This service extends to the Virginia agencies as well due to the significant number of patients from Virginia receiving services at Smith-McMichael. At the point of cancer diagnosis, the social worker meets with all self-pay patients to review all options for both the patient and the organization. Eligibility requirements for all programs are determined and the patient is guided through the process for applying for disability, Medicaid, PCIP, or financial assistance. Patients are connected with the Department of Social Services for Medicaid, food stamps, and emergency services applications. Rockingham County Aging Disability and Transit Services (RCATS) assist with transportation needs for treatment and follow-up if a patient meets the criteria. Area health departments offer medication assistance programs for those without any type of medication insurance coverage. Caregivers of Rockingham County provide volunteer services without charge to disabled and elderly individuals who qualify. Some of the services include transportation, companionship, light housekeeping and meals. Pharmaceutical patient care funds are assessed for replacement medications/free oral medications for those who qualify. Copay assistance is also sought on an ongoing basis. Home Health agencies, durable medical equipment companies, hospice agencies, private care nursing, local pharmacies, Red Cross, and the Salvation Army are just a few of the agencies providing services for our patients. National organizations such as the American Cancer Society, Leukemia and Lymphoma Society, Colon Cancer Alliance, Cancercare, Blue Note Fund, Chris4Life, Lymphoma Research Foundation, and Chronic Disease Fund provide financial assistance and copay assistance for expensive chemotherapy medications. Extraordinarily fortunate for this community, the Morehead Memorial Hospital Foundation and the Barry L. Joyce Cancer Support Fund offer financial assistance for our patients. The Foundation has provided transportation, medication and nutritional support for many of our patients. Supplemental nutritional drinks can cost as much as $2 per bottle with a patient needing six bottles per day. This cost quickly becomes a burden when it is the only source of nutrition. Patients are often faced with paying for treatment needs while sacrificing payment of other bills. After consultations with the social worker, options are sought to assist with these varied expenses. The Barry L. Joyce Cancer Support Fund provides assistance to residents of Rockingham County. Some of the resources approved for patients have been payment of utility bills, 9|Page medications, gas, food, clothing, specialized equipment and even dentures. Over 800 Rockingham County residents have received assistance from the Barry L. Joyce Cancer Support Fund in 2014. The “Junkyard” provides sodas, bottle water, chips, cookies, candies, and even fruits for cancer center staff to purchase for breaks. All profits are used to provide patients with resources when other options have been depleted or do not provide individual needs. Adult diapers, aluminum free deodorants, aloe vera gel, nonprescription medications and supplements are just a few of the items purchased for patients with Junkyard funds. The Center also receives donations from the community of crocheted/knitted scarves/hats, medical equipment, and nutritional supplements. Some of the contributors include the Danville Cancer Association, The Jerry Chaney Fund, Southern Area Agency on Aging Cancer Fund, Martinsville Family Pharmacy, and various other service entities. Chaplaincy Services The spiritual needs of our patients are met by a team of individuals. Utilizing a Chaplaincy On Call program, Morehead is able to care for those when they need it most. These pastoral visits include one or more of the following: • Informal spiritual assessments, active and empathic listening, pastoral presence and support, and, if requested, prayer; • Relevant printed support materials (“Care Notes”) for patients and families; and, • Education and counseling for cancer patients regarding advance directives and DNR (Do Not Resuscitate) or MOST (Medical Order for Scope of Treatment) orders as needed, primarily with inpatients. Hospice Hospice of Rockingham County, Inc. has provided the highest quality end-of-life care to over 6,000 local residents in the past 27 years. Using an interdisciplinary approach, Hospice of Rockingham County, Inc. provides care to patients in their own homes, assisted living facilities, nursing homes, independent living facilities, or the Hospice Home. The hospice team includes nursing, social work, chaplaincy, hospice aides, trained volunteers, and the patient’s physician and touts over 250 years of collective service. Research 10 | P a g e Information about the availability of cancer-related clinical trials is provided to our patients. Physicians will discuss clinical trials and will refer patients as appropriate. Advance Healthcare Directives Regular community sessions for the completion of an advance directive – Health Care Power of Attorney and/or Advance Directive for a Natural Death (“Living Will”) – are held for the benefit of the community under the leadership of Chaplaincy Services. Hospital staff members serve as notaries and community members as witnesses. Individuals register for the sessions, and materials are provided to help them understand the need for advance directives. Afterwards, extra copies are made for the participants, and instructions are given for the placement of these copies. A copy is placed in the hospital’s Health Information Management Department if the individual has a medical record there. The Social Worker at the Cancer Center assists patients who desire to complete their advance directives while at the Cancer Center. Pharmacy The Oncology Pharmacy is located in the Smith-McMichael Cancer Center and is staffed Monday through Friday by a pharmacist and pharmacy lab technician. This pharmacy complies with the latest USP 797 regulations for sterile pharmacy compounding and hazardous medicinal compounding. The pharmacist maintains a profile on each patient and prepares all of the approximately 11,000 chemotherapy preparations that are administered each year at the Cancer Center. The pharmacist serves as a resource to patients for drug counseling or for information on any aspect of their therapy regimen, including drug education, side-effects management, drug procurement and pain control. The pharmacist, with support from the Department of Pharmacy Services, works closely with the other members of the oncology staff to ensure the safe and effective use of chemotherapy agents. Our pharmacists review the current literature and attend seminars to stay abreast of the latest developments in cancer care, including cytotoxic drug therapy, changes in cancer practice guidelines, and clinical trial availability. Patient Education and Support 11 | P a g e Patient/Family Education and Support The oncology nurse is vital when it comes to educating the patient. Patients and family interrelate with nurses more than any other member of the healthcare team, providing a great opportunity for the nurse to educate and reinforce the teaching at each encounter. Nursing staff uses Oncology Nursing Society standards-based care to: • Counsel patients and families for any cancer-related needs; • Prepare patient education materials; and, • Provide education to the community on cancer-related topics. A variety of teaching tools and methods are used to educate the patient and family. The choice of tools or methods used is based on each individual patient’s needs and abilities. Printed materials, visual, and audiovisual educational materials are used in conjunction with verbal discussion and continued reinforcement. These materials are from The National Cancer Institute, the American Cancer Society and various pharmaceutical companies. Patients receiving chemotherapy or radiation therapy are verbally informed, as well as given written information on possible side effects of their therapy, home management, and how and when to contact the nurse or the physician. Support Groups/Services • Chair Yoga • Survivorship Meetings • Look Good...Feel Better • Community of Hope Support Group • Lymphedema Clinic • Speech Therapy 12 | P a g e Community Education, Awareness, and Screening Activities Morehead Memorial Hospital and Health Education Services provide prevention and education services to the local community throughout the year. These collaborative activities utilize employees from many hospital departments as well as employees and resources from the American Cancer Society. Displays are taken to health fairs throughout the community on topics of general cancer, specific cancers, and hospital cancer services. Health education services participated directly in four major health fairs to provide cancer education information. In addition to providing direct screening and health assessment services, the hospital is committed to providing cancer education through media to the community. Two 30-minute radio programs on breast cancer were produced and aired on a local radio station. Also, a breast cancer television spot aired throughout the month of October on a local television station. A free community colon cancer screening was offered. Seventy-one hemoccult kits were given out. Two came back abnormal and were referred for follow-up. Morehead Memorial Hospital also works diligently to support our local cancer organizations, the American Cancer Society, and Susan G. Komen for the Cure. In 2012 and in 2013, Morehead Memorial Hospital, together with collaborating partners, received a grant from Susan G. Komen for $40,000 to provide free screening and diagnostic mammograms to women in need. In Rockingham County 206 women were served through these funds. Morehead directly screened 55 women of which 15 were abnormal and required further follow-up. www.morehead.org The hospital’s web site features a recently updated Smith-McMichael Cancer Center web page. Featured items include Patient Education, Patient Support Services and the previous year’s annual report. 13 | P a g e Professional Education Staff Education Committed to maintaining the highest professional standards and keeping abreast of the latest treatments and technologies, staff participates in ongoing cancer education. Each year, continuing education with emphasis on oncology is completed by staff. The nurses read credible, evidence-based oncology educational resources, such as “The Clinical Journal of Oncology Nursing,” “The Oncology Nursing Forum,” and “ONS Connect,” to assist in maintaining their expertise and knowledge. These are all official journals of the Oncology Nursing Society. The radiation therapists achieve and maintain their expertise and knowledge by reading the publications of the ASRT (American Society of Radiologic Technologists, Radiation Therapists). The staff also attends cancer conferences, Tumor Board and in-services, read other professional journals that pertain to their specialty, and consult current peer-reviewed literature on cancer and the care of the cancer patient. Physician Education CME programs presented at Morehead Memorial Hospital related to cancer and the treatment of cancer included the following: Preventing Complications In Mechanically Ventilated Patients Sarah S. Lewis, MD STEMI and Hypothermia Brian C. Hiestand, MD Breast Density and Breast Cancer Screening Beth Brown, MD Customer Service for Physicians Physician Panel ResMeds Solution for COPD Mike Shafer Use of the MoCA (Montreal Cognitive Assessment) James Parsons, MD Computerized Physician Order Entry Dionne Galloway, MD Diagnosis, Staging, and Management of Lung Cancer Boris Darovsky, MD All were approved for one hour AMA PRA Category 1 Credit™ and for one hour American Academy of Family Physicians Prescribed credit. 14 | P a g e Cancer Conferences (Tumor Board) Morehead Memorial Hospital had 22 cancer conferences in 2014 with each approved for one hour AMA Category 1 credit and AAFP Prescribed credit. According to the American College of Surgeons Commission on Cancer requirements for hospitals our size, the number of cases must equal or exceed 15% of the annual analytical caseload, and these cases must be representative of the hospital’s cancer case mix. The total number of analytical cases added to the database in 2013 was 330. Thus, 50 cases were the required number for presentation. The actual number presented in 2014 was 108. The average attendance at the monthly Tumor Board was 27 with all physician specialties involved in cancer patient care being represented at each conference. These included surgeons, at least one medical oncologist, a radiation oncologist, a pathologist and a diagnostic radiologist. Cancer Registry The Cancer Registry for Morehead Memorial Hospital was established January 1, 1995 to collect, manage, and analyze statistical data on all cancer patients diagnosed and/or treated at the hospital and the Smith-McMichael Cancer Center. The registry’s program is patterned to meet the requirements of the American College of Surgeons Commission on Cancer and is designed to describe characteristics, modalities of therapy and patient survival experiences. The main objective of any cancer registry is to collect and abstract basic cancer information related to Morehead’s cancer population that will assist the various members of the medical community in evaluating the effectiveness of cancer treatments, which in turn can be used to improve patient outcomes. Physicians and hospital administrators use this data to evaluate staffing and equipment needs, cancer rates in our patient population, and diagnostic and therapeutic trends. This data is also used to evaluate compliance with national standards of care. A total of 416 cases were accessioned into the database in 2013. Of these, 330 were analytical cases. Analytic cases include all reportable cases first diagnosed and/or receiving all or part of their initial treatment at Morehead Memorial Hospital and/or Smith-McMichael Cancer Center in 2013. This includes patients receiving part of their initial therapy elsewhere. The other 86 cases were non-analytic cases, which includes cases seen for the first time at Morehead Memorial Hospital and/or Smith-McMichael Cancer Center for subsequent treatment but who received at least one complete course of treatment elsewhere. 15 | P a g e The cancer registry maintains lifetime follow-up on patients entered into the database. It also serves as a reminder to physicians and patients to schedule physical examinations to assure continued medical surveillance in hopes of improving early detection of recurrent or metastatic disease. Since January 1, 1995, a total of 5,228 cases have been accessioned into the database. Of these 2,970 are analytic cases that have to be followed at least annually or until they expire or reach 100 years of age. Of these, 2,970 patients have expired with a total of 2,257 to be followed. The American College of Surgeons Commission on Cancer requires at least an 80 percent follow-up rate on all analytic patients accessioned in the database since it was established. Our current follow-up rate is 92% percent. The American College of Surgeons Commission on Cancer also requires at least a 90 percent follow-up rate on all analytic patients accessioned into the database in the last five years. Our current follow-up rate is 91.9% percent. The registry also collected data to assist in the 2014 Patient Care Evaluation Studies looking at endometrial patients diagnosed from 2010-2013. In an effort to keep abreast of the many changes and current issues, the cancer registry staff attends various educational meetings throughout the year provided by the National Association of Cancer Registrars, Commission on Cancer and the North American Association of Central Cancer Registries. 16 | P a g e Cancer Cases Diagnosed in 2013 Gender Anatomical Site Head and Neck Stage Male Female 0 I II III IV N/A Unk Total 8 3 0 1 1 1 4 0 2 11 Digestive System 52 25 4 10 12 17 16 0 2 77 Respiratory System 44 41 0 14 4 20 32 0 3 85 Bones and Joints 0 0 0 0 0 0 0 0 0 0 Soft Tissue 1 1 0 1 0 0 0 0 1 2 12 3 3 6 2 0 1 1 0 15 Breast 1 67 13 17 18 3 5 0 1 68 Female Genital 0 21 0 6 3 3 3 0 2 21 Male Genital 39 0 0 4 14 3 2 0 0 39 Urinary System 11 4 4 2 0 1 2 1 1 15 Eye and Orbit 0 0 0 0 0 0 0 0 0 0 Brain and CNS 5 9 0 0 0 0 0 10 0 14 Endocrine System 5 4 0 1 0 1 2 3 0 9 12 7 0 3 1 2 5 0 3 19 Myeloma 3 6 0 0 0 0 0 8 0 9 Leukemia 4 6 0 0 0 0 0 7 0 10 Mesothelioma 1 0 0 0 1 0 0 0 0 1 Skin Lymphoma Miscellaneous 10 11 0 0 0 0 0 17 0 21 Stage 0: Carcinoma in situ (confined to its site of origin) Stage I, II, III: Higher numbers indicate more extensive disease/larger tumor size and /or spread of the cancer beyond the organ in which it first developed to nearby nodes and/or organs adjacent to the location of the primary tumor. Stage IV: The cancer has spread to another/other organ (s). 17 | P a g e Primary Site by County Primary Sites Rockingham Caswell Guilford Stokes Henry Pittsylvania Floyd Halifax Total Adrenal 0 0 0 0 0 1 0 0 1 Anus / Anal Canal 1 1 0 0 0 0 0 0 2 Brain / Spinal Cord 7 2 0 0 0 1 0 0 10 Breast 43 1 0 0 6 7 0 0 57 Cervix Uteri 2 0 0 0 0 0 0 0 2 Colon/Rectum 19 1 0 0 10 2 0 0 32 Uterian 8 0 0 0 2 3 0 0 13 Esophagus 4 0 0 0 0 1 0 0 5 Gallbladder 1 0 0 0 0 0 0 0 1 Gastric and Omental 1 0 0 0 0 0 0 0 1 Lymphoma 11 0 0 0 3 0 0 0 14 Hypopharynx 1 0 0 0 0 0 0 0 1 Kidney 2 0 0 0 1 0 0 0 3 Larynx 5 0 0 0 1 1 0 0 7 Lip / Oral Cavity 3 0 0 0 0 0 0 0 3 Liver 4 0 0 0 1 0 0 0 5 Lung 54 1 0 0 10 1 1 0 67 Major Salivary Glands 1 0 0 0 0 0 0 0 1 Melanoma of the Skin 8 0 0 0 1 1 0 2 12 Mesothelioma 1 0 0 0 0 0 0 0 1 Nasopharynx 1 0 0 0 0 0 0 0 1 Colon and Rectum 0 0 0 0 1 0 0 0 1 Oropharynx 3 0 0 0 0 0 0 0 3 Ovary 1 0 0 0 1 0 0 0 2 Pancreas 9 0 0 0 1 0 0 0 10 Penis 1 0 0 0 0 0 0 0 1 Prostate 16 3 0 1 1 0 0 0 21 Renal Pelvis/Ureter 1 0 0 0 0 0 0 0 1 Soft Tissue Sarcoma 1 0 0 0 0 0 0 0 1 Stomach 3 0 0 0 1 0 0 0 4 Testis 1 0 0 0 0 0 0 0 1 Thyroid 1 0 0 0 0 0 0 0 1 Thyroid 2 0 0 0 0 0 0 0 2 Unstageable Site 24 0 1 1 7 4 0 0 37 Urinary Bladder 6 0 0 0 0 0 0 0 6 Total 246 9 1 2 47 22 1 2 330 Because of our geographical location, many of our patients are from neighboring counties in Virginia, 21.8% from Virginia and 78.2% from NC 18 | P a g e Cases diagnosed and treated with any of the first course of treatment at Morehead after the registry’s reference dates are defined as analytic (Class of Case 0, 1, 2). All accessioned cases are assigned a Class of Case based on the nature of involvement of the facility in the care of the patient. Class of Case 0: Diagnosed at Morehead and all first course of treatment was elsewhere or a decision not to treat was made elsewhere. Class of Case 1: Diagnosed at Morehead and all or part of the first course of treatment was done at Morehead. Class of Case 2: Diagnosed at another facility and had all or part of their first course of treatment at Morehead. In 2013, we had a total of 330 analytical cases accessioned in the cancer registry database. Of these, 36(10.9%) were Class 0, 179 (54.2%) were Class 1 and 115 (34.9%) were Class 2. 19 | P a g e Review of Endometrial Cancer Cases Diagnosed & Treated at Morehead Memorial Hospital, 2000-2013 Written by William McLeod, MD Endometrial cancer is the most common gynecological malignancy in the developed world. Adenocarcinoma is the most common type. The mortality rate falls in the range of 1.7 to 2.4% per 100,000 women. 80% of patients present with abnormal uterine bleeding, the cardinal symptom of endometrial cancer. Approximately 68% of the women with the diagnosis of endometrial cancer have the disease confined to the uterus, translating into a 96% five year survival. Type I tumors, with favorable histology (grade I and II) make up 80% of endometrial cancers. These tumors have a good long term prognosis. Type II tumors account for 10 to 20% of endometrial cancers (grade III, clear cell and serous) have a poor prognosis. Purpose of the Review Limited by the small number of patients receiving care over the thirteen year period, we set out to ascertain if the quality of care maintains the standard of care. In addition, we would like to determine if there are any significant variations in access to care in our region. Data Collection from 2000 to 2013 In conjunction with MMH Smith-McMichael Cancer Center, a chart review of all cases of endometrial cancers managed were reviewed over a thirteen year period from 2000 to 2013 (94 total cases). The National Cancer Data Base (2000-2011) and Cancer Registry (2012, 2013) served as the resource base. The statistical analysis was compared with community cancer programs in all states (437) and the State of North Carolina (15). 20 | P a g e Results and Analysis Maintaining the standard of care is the good, therefore a comparison of all cases treated for corpus uteri cancers were compared to community cancer program (CCP-AS 437) hospitals in all states. MMH was similar to CCP-AS in multiple metrics. The age of diagnosis is similar between MMH and CCP-AS with the peak age between 50-59 years of age at 28% and 60-69 years of age at 28%, shown in Appendix I. Correlating with CCP-AS data, the stage of corpus uteri cancer is most often diagnosed in stage one as demonstrated in Appendix II. At the time, the most common histological type is endometrioid cancer followed by adenocarcinoma at both MMH and CCP-AS, Appendix III. Surgery is the first course of treatment in both MMH/CCP-AS. This is followed by surgery and radiation and reflects the early stage of diagnosis, Appendix IV. There was no difference in the co-morbidity medical conditions for individuals treated at MMH versus all CPP – AS. On the socio-economic front, insurance status of corpus uteri cancer treated at MMH vs. CCP-AS shows no significant differences, Appendix V. However, a noted difference between MMH and CCP-AS was observed in household incomes at the time of diagnosis: MMH has a 98% rate of patients with an income level below $39,000 versus 46% with CCP-AS, Appendix VI. For all treated patients, the distance traveled for treatment was less than 50 miles. Conclusion A total number of 131 patients were treated for endometrial cancer from the years 2000 to 2013. The review demonstrates access to care is good with no individual traveling more than 50 miles for treatment. The age, stage and histology at the time of diagnosis reflect national data. The first course of treatment is similar to national data. Income levels of the treated population reflect the demographics of the local geography and the access to quality care for corpus uteri cancer reflects the national data. 21 | P a g e Appendix I Appendix II 22 | P a g e Appendix III Appendix IV 23 | P a g e Appendix V Appendix VI 24 | P a g e
© Copyright 2026