Epidural haematoma after a combined spinal–epidural
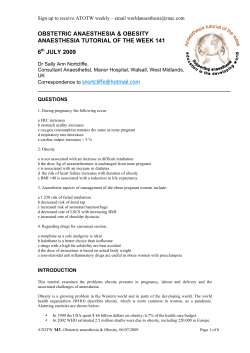
British Journal of Anaesthesia 96 (2): 262–5 (2006) doi:10.1093/bja/aei297 Advance Access publication December 16, 2005 Case Report Epidural haematoma after a combined spinal–epidural anaesthetic in a patient treated with clopidogrel and dalteparin N. L. K. Tam1*, C. Pac-Soo1 and P. M. Pretorius2 1 Department of Anaesthesia, Wycombe General Hospital, Queen Alexandra Road, High Wycombe, Buckinghamshire HP11 2TT, UK. 2Department of Neuroradiology, The Radcliffe Infirmary, Woodstock Road, Oxford OX2 6HE, UK *Corresponding author. E-mail: [email protected] Br J Anaesth 2006; 96: 262–5 Keywords: anaesthetic techniques, epidural; blood, anticoagulation; complications, haematoma; complications, spinal injury Accepted for publication: November 10, 2005 Antiplatelet agents are being increasingly used as they are beneficial in reducing the incidence of cerebro-vascular and ischaemic cardiac events in at-risk populations. Newer more potent agents such as the thienopyridine derivatives are being introduced into clinical practice but their effect, especially in combination with other anticoagulants, on the risk of developing an epidural haematoma after neuraxial blockade is not well documented. We report a case of an epidural haematoma in a patient who was administered low molecular weight heparin (LMWH) prophylactically against the development of deep vein thrombosis perioperatively and received a combined spinal–epidural analgesia for a knee arthroplasty. She had also been taking regular clopidogrel which had been stopped 7 days before surgery. Case report An 80-yr-old woman weighing 56 kg was admitted for an elective left total knee arthroplasty. Her significant past medical history included atrial fibrillation, moderate tricuspid regurgitation, congestive cardiac failure and haemorrhagic gastritis following ingestion of low dose aspirin. Her current medications included clopidogrel 75 mg once daily, furosemide 20 mg once daily, verapamil 120 mg once daily, lansoprazole 30 mg once daily and risedronate 35 mg once weekly. The clopidogrel was stopped 7 days before elective surgery. The results of her routine preoperative blood investigations revealed a normal clotting screen with an activated partial thromboplastin time of 32 s, prothrombin time of 10 s and a normal platelet count of 356·109 litre 1. Plasma urea and creatinine were raised at 10.2 mmol litre 1 (normal range 2.5–7.5) and 116 mmol litre 1 (normal range 50–110), respectively. On a previous hospital admission, plasma urea was noted to be 15.6 mmol litre 1 and plasma creatinine 186 mmol litre 1, indicating that the patient has impaired renal function. The patient received dalteparin (LMWH) 5000 units s.c. the night before, 10 h before elective surgery for prophylaxis against the development of deep vein thrombosis. The following day, in theatre the patient underwent a combined spinal–epidural anaesthetic. A 16 gauge Tuohy needle was inserted at the L4/5 inter-vertebral space in the midline and the epidural space was identified using the loss of resistance to saline technique. A 12 cm, 24 gauge Sprotte spinal needle was advanced into the sub-arachnoid space through the Tuohy needle and heavy bupivacaine 0.5% (2 ml) and diamorphine 300 mg injected. An epidural catheter was then threaded into the epidural space and secured over the patient’s back. The procedures were reported as atraumatic with no bloody tap or blood in the catheter. The sensory level was assessed using ethyl chloride spray and the upper limit of the sensory blockade was T4 on the right and T6 on the left. Surgery proceeded with the patient receiving propofol sedation via a target controlled infusion pump. After surgery, in the post anaesthetic care unit, a test dose of lidocaine 1% (3 ml) was injected into the epidural catheter. After 10 min there was no change in the cardiovascular or neurological status of the patient, excluding The Board of Management and Trustees of the British Journal of Anaesthesia 2005. All rights reserved. For Permissions, please e-mail: [email protected] Downloaded from http://bja.oxfordjournals.org/ by guest on September 9, 2014 We report a case of a spinal–epidural haematoma occurring in a patient after a combined spinal– epidural anaesthetic. She had been taking clopidogrel and had received perioperative dalteparin for thromboprophylaxis. Despite adhering to standard guidelines concerning administration of low molecular weight heparin perioperatively and stopping the clopidogrel 7 days before the anaesthetic, the patient developed an epidural haematoma. Epidural haematoma after spinal–epidural anaesthetic Discussion The development of a spinal haematoma is a rare but potentially devastating complication of central neuraxial blockade. Its true incidence is unknown and due to its rarity it is very difficult to evaluate risk factors prospectively and any properly powered study would require many thousands of patients to investigate this. Therefore, data on the incidence A B Fig 1 Axial T2 weighted images at the T12 (A) and L1 (B) levels demonstrate a large epidural haematoma returning low signal (black arrows in A and B). There is compression of the conus medullaris with increased signal in the conus indicating a compressive myelopathy (white arrow in A). At the L1 level, there is compression of the cauda equina (white arrow in B). of spinal haematoma following neuraxial blockade are mainly based on audit studies and case reports. Tryba1 reported that the incidence of spinal haematoma after epidural and spinal anaesthesia are 1 in 150 000 and 1 in 220 000, respectively. The incidence of spontaneous spinal haematoma is rarer still and is estimated at 1 patient per 1 000 000 patients per year.2 Several factors increase the risk of patients developing a spinal haematoma following neuraxial blockade.3 These include advanced age, female gender, bony spinal pathology that may necessitate multiple attempts resulting in traumatic insertion of either spinal or epidural needle or catheter and coagulopathy. Altered patient’s blood coagulation, due either to an inherent coagulopathy or to the administration of 263 Downloaded from http://bja.oxfordjournals.org/ by guest on September 9, 2014 sub-arachnoid placement of the catheter. A continuous infusion of 0.25% bupivacaine was then started, initially at 7 ml h 1 for postoperative analgesia. Subsequently that evening the patient reported increasing pain over the operated site and also over her lumbar back region. A bolus dose of 10 ml 0.25% bupivacaine was administered via the epidural catheter and the rate of infusion increased to 9 ml h 1. The intensity of the pain subsequently decreased and the infusion rate was reduced to 6 ml h 1. Thromboprophylaxis was resumed using a single daily dosing regimen of dalteparin 5000 units s.c. and local guidelines were adhered to, that is, the second dose of the LMWH was administered 24 h after the initial preoperative dose and in the case described here, it was 14 h after the insertion of the epidural catheter. The following day after surgery, the patient was inadvertently administered a dose of clopidogrel 75 mg together with her usual medications. The physiotherapist, during her daily visit, noted some numbness and weakness of the right, nonperated leg which she attributed to the epidural analgesia. Assessment of the left leg was not possible because of the recent knee surgery. The epidural analgesia was maintained for a total duration of 72 h until the third postoperative day when the catheter was removed. This was 12 h after the last dose of dalteparin and 48 h after the inadvertent single dose of clopidogrel. Assessment of the patient 5 h after removal of the epidural catheter showed that motor weakness was still present in the right leg. This was again attributed to persistent epidural block. The patient continued to have weakness of the hip flexors and quadriceps together with reduced sensation over the dorsum of the right foot. Neurosurgical opinion was sought but as the magnetic resonance imaging (MRI) facility was not available in the hospital at the time of the incident, there was a further delay of 48 h before the patient was transferred to a neurosurgical centre. At the neurosurgical centre, an MRI of the spine was performed and it revealed an epidural haematoma at the T12/L1 level (Fig. 1A and B). The patient underwent an urgent T12 to L2 laminectomy and evacuation of the haematoma. There was minimal improvement in the neurological symptoms affecting her right leg in the first 24 h after surgery. Her neurological progress continues to be assessed by the neurosurgical team and 1 month after surgery there had not been any significant improvement in her symptoms. Tam et al. adjustment may be necessary for patients with a creatinine clearance of <30 ml min 1. The anaesthetist involved reported that the procedure itself was atraumatic, that is, there was no report of blood in the epidural needle or catheter and the needle was inserted at the L4/5 interspace. However, the neurosurgeon who evacuated the haematoma reported that the catheter appeared to have been inserted at a higher level of L2/3 and that the epidural haematoma extended from T12 to L2, compressing mainly the right side of the thecal sac. Identification of body surface landmarks for neuraxial blockade is frequently inaccurate11 and probably accounts for the discrepancy observed between the neurosurgical findings and the level of insertion reported by the anaesthetist. The discrepancy may well have been compounded by the finding that the patient had osteoporotic wedge compression fractures of the bodies of T12, L1 and L2 vertebrae and partial collapse of L3 as identified by the MRI scan. Spinal haematomas may also occur at the time of removal of the epidural catheter. However, we do not believe that this was the case in our patient. Although the effect of clopidogrel on the inhibition of platelet aggregation has been shown to occur 2–3 days after administration,12 the abnormal neurology had been noted in the patient before receiving the inadvertent dose of clopidogrel and there had not been any further reported increase in motor or sensory symptoms after the catheter had been removed. It is very important to diagnose spinal haematomas early on so that prompt investigation and treatment are initiated. However, this is often difficult to achieve because the increasing motor and sensory blockade are often attributed to the action of the local anaesthetic agent. This has been highlighted in the American Society of Anesthesiologists Closed Claims database which reported that delays in diagnosis of spinal haematomas was often due to attributing the postoperative weakness or numbness to persisting local anaesthetic effect rather than spinal cord ischaemia.13 Successful neurological recovery following evacuation of a spinal haematoma depends on the interval between onset of symptoms and timing of surgery. Lawton and colleagues14 have observed an improved outcome in patients that were operated on within 12 h of developing symptoms compared with those operated on later. Vandermeulen and colleagues4 have suggested an even shorter interval of <8 h for successful recovery. This case highlights the need for continued vigilance and close neurological monitoring regarding the use of epidural anaesthesia in the presence of combinations of anticoagulant agents and antiplatelet agents. References 264 1 Tryba M. Epidural regional anesthesia and low molecular heparin: pro. Anasthesiol Intensivmed Notfallmed Schmerzther 1993; 3: 179–81 (in German) 2 Holtas S, Heiling M, Lonntoft M. Spontaneous spinal epidural hematoma: findings at MR imaging and clinical correlation. Radiology 1996; 199: 409–13 Downloaded from http://bja.oxfordjournals.org/ by guest on September 9, 2014 anticoagulants is recognized as an important risk factor in the development of spinal haematoma.3 4 Vandermeulen and colleagues4 reviewed the literature between 1906 and 1994 and reported 61 cases of spinal haematoma following spinal or epidural anaesthesia. In 42 of these patients (68%) there was evidence of abnormal clotting; 25 had received i.v. or s.c. unfractionated heparin or LMWH before or after neuraxial block and a further five had undergone vascular surgical procedures and are presumed to have received intraoperative heparin. Twelve patients were being treated with either antiplatelet medication, dextran 70, oral anticoagulants or thrombolytics immediately before or after neuraxial blockade. LMWH is increasingly being used both for the prevention and treatment of deep vein thrombosis perioperatively. Its use is being associated with an increasing incidence of spinal haematoma following neuraxial blockade.5 The American Society of Regional Anesthesia and Pain Medicine (ASRA) consensus conference on neuraxial anaesthesia and anticoagulation held in 2003 recommended that when a LMWH is being used preoperatively, at least 10 h must elapse before performing neuraxial blockade and 6 h after the block if the drug is administered postoperatively.6 Clopidogrel is also increasingly being used for the secondary prevention of vascular events in patients with established atherosclerotic disease including ischaemic stroke, myocardial infarction and peripheral vascular disease. It is a thienopyridine derivative and exerts its antiplatelet effect distinctly from aspirin by binding irreversibly to the adenosine diphosphate receptors on platelets.7 There is little information on the risk of spinal haematoma following neuraxial blockade in patients treated with clopidogrel. Current recommendations from the ASRA conference suggest that clopidogrel should be stopped 7 days before neuraxial blockade, in line with the manufacturer’s recommendation regarding surgery and the use of clopidogrel.6 We believe that the epidural haematoma occurred at the time of placement of the catheter, despite adhering to guidelines with regard to clopidogrel use and administration of preoperative LMWH as mentioned above. Co-administration of anticoagulants to patients on regular antiplatelet medications may significantly increase the risk of spinal haematoma.8 The antiplatelet effect of clopidogrel is irreversible and it is possible that the period of 7 days before neuraxial blockade was in this case inadequate as it takes up to 10 days for new platelets to completely replace affected ones. It has also been shown that it takes 10 days for the bleeding time to return to normal after stopping clopidogrel.9 Furthermore, the effect of the initial preoperative dose of dalteparin may have been prolonged because the patient had impaired renal function. Chow and colleagues10 have shown in a recent study that there is a linear association between antifactor Xa and renal function in patients on enoxaparin and have suggested that dose Epidural haematoma after spinal–epidural anaesthetic 3 Horlocker TT, Wedel DJ. Anticoagulation and neuraxial block: historical perspective, anesthetic implications and risk management. Reg Anesth Pain Med 1998; 23: 129–34 4 Vandermeulen EP, van Aken H, Vermylen J. Anticoagulants and spinal–epidural anaesthesia. Anesth Analg 1994; 79: 1165–77 5 Schroeder DR. Statistics: detecting a rare adverse drug reaction using spontaneous reports. Reg Anesth Pain Med 1998; 23: 183–9 6 Horlocker TT, Benzon H, Brown DL, et al. Regional anaesthesia in the anticoagulated patient: defining the risks (the Second ASRA Consensus Conference on Neuraxial Anesthesia and Anticoagulation). Reg Anesth Pain Med 2003; 28: 172–97 7 Sharis PJ, Cannon CP, Loscalto J. The antiplatelet effects of ticlopidine and Clopidogrel. Ann Intern Med 1998; 129: 394–405 8 Urmey WF, Rowlingson J. Do antiplatelet agents contribute to the development of perioperative spinal hematoma? Reg Anesth Pain Med 1998; 23 (Suppl 2): 145–51 9 Keser AC. Antiplatelet agents and spinal anesthesia. Anesthetist 2000; 49: 234–5 10 Chow SL, Zammit K, West K, Dannenhoffer M, Lopez-Candales A. Correlation of antifactor Xa concentrations with renal function in patients on enoxaparin. J Clin Pharmacol 2003; 43: 586–90 11 Broadbent CR, Maxwell WB, Ferrie R, Wilson DJ, Gawne-Cain M, Russell R. Ability of anaesthetists to identify a marked lumbar interspace. Anaesthesia 2000; 55: 1122–6 12 Coukell AJ, Markham A. Clopidogrel. Drugs 1997; 54: 745–50 13 Cheney FW, Domino KB, Caplan RA, Posner KL. Nerve injury associated with anaesthesia. A closed claim analysis. Anesthesiology 1999; 90: 1062–9 14 Lawton MT, Porter RW, Heiserman JE, et al. Surgical management of spinal epidural hematoma: a relationship between surgical timing and neurological outcome. J Neurosurg 1995; 83: 1–7 Downloaded from http://bja.oxfordjournals.org/ by guest on September 9, 2014 265
© Copyright 2026