SPORTS CONCUSSION EDUCATION SEMINAR For Parents, Coaches, and School
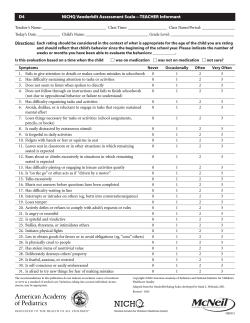
SPORTS CONCUSSION EDUCATION SEMINAR For Parents, Coaches, and School Administrators Presented by the Vanderbilt Sports Concussion Center Vanderbilt University Medical Center Nashville, TN What is the Vanderbilt Sports Concussion Center? • Collaborative effort among VUMC sports medicine providers to standardize diagnosis, treatment, and management of concussed athletes using state of the art, evidence-based care while advancing the current standard of care throughout the community through public and provider education and the discovery of new knowledge. VSCC – Scope of Care • Middle and high school athletes – All Nashville metro and Williamson county high schools and several private schools • “Club” sports teams – lacrosse, soccer, hockey • College teams – Vanderbilt University, Belmont University • Professional teams – Nashville Predators (NHL), Nashville Sounds (AAA baseball) • US Olympic Equestrian team and elite riders (USEF) • Many individual athletes of all levels • • • • • VSCC - Providers Primary care sports medicine Neurosurgery Neuropsychology Certified athletic trainers Affiliated consultants – neuroradiology, neurology, pediatrics, ENT, rehab services, psychiatry, counseling, physical and occupational therapists • Only comprehensive sports concussion center in the region VSCC – Locations • Campus - Vanderbilt Sports Medicine (VOI), Children’s Hospital, Neurosurgery (VAV) • One Hundred Oaks • Cool Springs – Orthopedics and Neurosurgery • Vanderbilt Bone and Joint Clinic, Franklin • Brentwood Primary Care • Outreach clinics – Murray, KY; Mt. Juliet, TN VSCC - services • Team coverage – Comprehensive concussion plan – Coach/parent/athlete education – Individual preseason baseline testing (history, cognitive, and balance) – Injury assessment and evaluation – Supervised return to play – Access to all resources for complex or refractory cases VSCC - education • Many resources on our website: – www.vanderbiltsportsconcussion.com • • • • “Quick facts” brochures In-services for ATCs and staff Annual CME updates Numerous outreach seminars and courses for physicians, trainers, and other providers Why are we here today? • Data shows that an overwhelming majority of youth sports concussions occur in practices or games where no athletic trainer or physician is present • We want to educate coaches, parents and school officials about basic concussion diagnosis and treatment so that these important injuries are recognized and more severe injuries are prevented But we are NOT here to… • Get rid of football (or any other sport) • Frighten everyone that all sports are dangerous and cause long term brain damage • Turn everyone into a concussion expert or brain surgeon in 2 hours Program objectives • Understand what is a concussion and what are common signs and symptoms • Discuss initial treatment and transport • Outline how we return someone to play after injury • Review baseline testing • Describe current evidence about long term outcomes • Update prevention strategies Unrestricted Educational Grant Robert Parish, CEO April 30, 2013: Nashville Concussion: Definition, Demographics, Signs & Symptoms Andrew Gregory, MD, FAAP, FACSM Associate Professor Orthopedics & Pediatrics Team Physician, Vanderbilt & Belmont Universities Is this a concussion? • 11 yo was swinging on a tree limb, fell 5-6’ and hit the back of his head on the ground • Loses consciousness for one min according to other kids • Then has headaches and blurry vision • Vomits twice Is this a concussion? • Seen at the Emergency Room - “normal exam”, CT Scan negative • Goes back to school with headaches needing Ibuprofen • Headaches get worse with physical activity (including practicing with his travel baseball team) Self Reported Symptoms • • • • • • • Headache – 3/6 Trouble Sleeping – 3/6 Drowsiness – 2/6 Sensitivity to light – 2/6 Feeling like “in a fog” – 1/6 Difficulty concentrating – 1/6 All others - 0/6 Did this child have a concussion? What is a Concussion? • Lots of terms – Ding, bell rung, shaking off the cobwebs, closed head injury, mild traumatic brain injury (mTBI) • “A trauma induced alteration in mental status that may or may not involve loss of consciousness” —AAN 1997 • Headache plus… • Transient Neurological Phenomenon Definition of Concussion 1. Caused either by a direct blow to the head, face, neck or elsewhere on the body with a resultant force transmitted to the brain. 2. Typically results in the rapid onset of short-lived changes in neurological function that resolves spontaneously. 3. May result in structural brain changes, but the symptoms largely reflect a functional disturbance rather than a structural injury. 4. Usually follows a progressive course of improvement 5. Imaging studies (brain CT/MRI) are usually normal. Signs and Symptoms of Concussion Signs • • • • • • • • • • Appears dazed or stunned Confused about assignment Forgets plays Is unsure of game, score, or opponent Moves clumsily Answers questions slowly Loses consciousness Shows behavior or personality change Forgets events prior to play (retrograde) Forgets events after hit (posttraumatic) Symptoms • • • • • • • • Headache Nausea Balance problems or dizziness Double vision Sensitivity to light or noise Feeling sluggish Feeling “foggy” Concentration or memory problems • Change in sleep pattern (appears later) • Feeling fatigued Common symptoms of concussion from a series of injured high school athletes • Three most common symptoms: 1. Headaches (55%) 2. Dizziness (42%) 3. Blurred vision (16%) • • 46% experienced either cognitive or memory problems 9% had loss of consciousness (“knocked out”) Do you have to be “knocked out” to have a concussion? • NO!!!!! • In fact, only a SMALL number of concussed athletes were “knocked out” • Many studies have now shown that amnesia (inability to remember) is a much more common sign of concussion and ALWAYS indicates that a brain injury has occurred What are the “Grades” of a concussion? • In the past concussions were often classified into grade 1, 2, or 3 based on the severity and duration of symptoms at the time of injury • Many research studies have showed that these grading scales were useless in predicting the severity of injury or how long to recover • Grading scales are no longer used If you have a history of a previous concussion are you more likely to have a longer duration of symptoms? • Available research says “yes” Does having a concussion increase your chances for a future concussion? • Some research says “yes” • 92% of the in-season repeat concussions occurred within 7-10 days of first Epidemiology of Concussion • 1.5-3.8 million reported cases of brain injury per year in the US (CDC) • 20% (300,000-760,000) are sports-related • 53,000 deaths each year • 70-90,000 permanently disabled • Highest sports incidence: ages 1524 • Cost estimated at > $60 billion annually HS RIO™ Injury Surveillance System • Internet-based high school sports-related injury surveillance system • Weekly data capture 2005 - 2010 academic years • Representative sample of 100 US high schools – Geography (4 US census regions) – Size (≤1,000 vs >1,000 students) • 20 sports – Boys’ - football, soccer, basketball, wrestling, baseball, lacrosse, ice hockey, swimming & diving, track & field, volleyball – Girls’ - volleyball, soccer, basketball, softball, lacrosse, field hockey, gymnastics , swimming & diving, track & field, cheerleading 26 Concussion Rates, 2005- 2010 Rates per 1,000 Athletic Exposures # of Concussion s National Estimate s Practice Competition Overall Football 1392 357,114 1.3 11.4 2.9 B Soccer 182 89,237 0.3 3.0 1.1 G Soccer 243 132,062 0.3 4.6 1.6 G Vball 54 17,326 0.2 0.6 0.3 B Bball 111 27,404 0.2 1.3 0.6 G Bball 184 47,439 0.4 2.7 1.1 Wrestling 152 33,979 0.6 1.9 1.0 Baseball 32 9,569 0.1 0.4 0.2 Softball 66 23,692 0.4 0.8 0.5 Sport Includes concussions resulting in <1 day time loss (non time loss = 2% of all concussions) 27 Concussion Severity 2005-2010 0% 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Football B Soccer Sport G Soccer G Volleyball B Basketball G Basketball Wrestling Baseball Softball Time lost (days) 1-2 days 3-6 days 7-9 days 10-21 days Time lost means days missed from sport due to concussion 22 Days + 28 Concussion Mechanisms 2005-2010 Includes only time loss concussions 29 Activity Associated with Concussions, Soccer 2005-2010 Boys’ soccer Girls’ soccer Heading ball 36% 30% Goaltending 17% 13% General play 10% 11% Defending 9% 17% Chasing loose ball 11% 15% Ball handling/dribbling 6% 5% Receiving pass 6% 3% Activity Includes only time loss concussions 30 Activity Associations Basketball 2005 - 2010 Boys’ basketball Girls’ Basketball Rebounding 30% 21% Chasing loose ball 17% 17% Defending 20% 27% General play 14% 7% Shooting 10% 6% Ball handling/dribbling 6% 10% Receiving pass 1% 7% Activity Includes only time loss concussions 31 Activity Associations Baseball/Softball 2005 -2010 Activity Baseball Softball Batting 37% 8% Running bases 22% 4% Fielding 15% 25% Pitching 6% 5% Catching 6% 33% Sliding 12% 5% * Includes only time loss concussions 32 Football Concussions 2010 Concussions resulting from player-to-player contact Type of contact: head to head (66%), head to other body site (26%), head to playing surface (8%) Position of head during contact: head-up (38%), headdown (25%), no flexion (4%), unknown (33%) Direction of impact: front (45%), side (22%), top (8%), back (5%), unknown (20%) Did athlete see impact coming: yes (37%), no (27%), unknown (37%) 33 Girls’ Soccer Concussions 2010 Concussions resulting from player-to-player contact Type of contact: head to head (48%), head to other body site (45%), head to playing surface (7%) Position of head during contact: head-up (21%), headdown (26%), no flexion (7%), unknown (46%) Direction of impact: front (24%), side (43%), top (3%), back (14%), unknown (16%) Did athlete see impact coming: yes (55%), no (25%), unknown (20%) 34 Summary • Concussion is a temporary disruption of ANY function of the brain caused by trauma • All coaches and parents should become familiar with common signs and symptoms of concussion and be alert for them • No return to play if concussion is suspected • Grading scales are no longer used • ANY athlete in ANY sport at ANY age is at risk for concussion Sports Concussion: Immediate, short-and long-term effects on the brain Gary Solomon, Ph.D., FACPN Associate Professor of Neurological Surgery, Psychiatry, and Orthopaedic Surgery & Rehabilitation Co-Director, Vanderbilt Sports Concussion Center Team Neuropsychologist, Nashville Predators Consulting Neuropsychologist, Tennessee Titans Disclosures/Competing Interests • I receive royalties from book sales. • I receive consulting fees from the Nashville Predators and Tennessee Titans. • I am involved in beta testing a new version of ImPACT and receive free use of the test during the testing; I am a member of the ImPACT Professional Advisory Board and am reimbursed for travel expenses to Board meetings • This presentation is not endorsed by any organization with which I am affiliated. Objectives: 1. Overview of the brain 2. What happens in the brain during a concussion--immediate, short, and long-term effects 3. How long it takes for the brain to recover from a concussion 4. Potential long-term effects a. Post-Concussion Syndrome (PCS) b. Chronic Traumatic Encephalopathy (CTE) Average Adult Human Brain Weight = 1350 g (~3 lbs.) Width = 140 mm (5.6”) Length = 167 mm (6.68”) Height = 93 mm (3.72”) Brain = 2% of Total Body Weight Average Adolescent Brain is Smaller We can think of the brain as a computer it is composed of hardware (structure) and software (function) Hardware (Structure) = brain tissue Software (Function) = Electrical and chemical processes ongoing within the brain tissue that allows us to sense, think, feel, and act Sports related concussions rarely cause a hardware problem (structural injury) When structural injuries do occur, they are usually due to tearing of a blood vessel (resulting in an epidural or subdural hematoma) or in some cases, tearing of nerve cells (traumatic axonal injury) However, these structural injuries are extremely rare in sports. This is why the structural CT or MRI scan is normal 99+% of the time after a sports concussion Sports concussion usually causes a disruption in brain function (software problem), which leads to the signs and symptoms described previously The disruption in brain function has been termed “the chemical cascade” The Chemical Cascade of Concussion Blood flow to the brain is reduced immediately after a concussion The brain operates on 2 kinds of fuel: glucose and oxygen The brain gets glucose and oxygen from the blood supply But because the brain is getting less blood flow after a concussion, the brain is not getting the typical amount of fuel (energy) The difference between the energy the brain is getting and what the brain needs to operate fully results in an energy crisis and the symptoms PET Scans in Head Injury (Glucose) Marvin Bergsneider, M.D., and David Hovda, Ph.D. UCLA School of Medicine fMRI Scan (Oxygen) Drs. Mark Lovell and Micky Collins University of Pittsburgh Medical Center Drs. Victoria Morgan and Megan Strother, Vanderbilt The short term effects of concussion are age- and possibly gender dependent Younger athletes take longer to recover than older athletes, probably because the brain is not fully developed physically until about age 23 Many studies have indicated that females may take longer to recover than males, although a recent VSCC study did not support this Other factors affecting the duration and intensity of symptoms after a concussion can include concussion history and co-existing disorders such as ADHD, learning disabilities, sleep disorders, psychiatric illness, and migraine headaches To get back to the computer analogy, when we have a software problem, we usually shut down the computer and re-boot it. After a concussion the brain typically repairs (re-boots) itself. But how long does it take? First, there is no FDA-approved medication for concussion, although many drugs are used to treat the symptoms of concussion In general and on average, the short term effects of concussion resolve within: 7 days for professional athletes 7-10 days for collegiate athletes 7-14 days for high school athletes 7-21 days for younger athletes >90% of athletes with sport-related concussions recover within a month Second Impact Syndrome (SIS) However, if an athlete does not recover fully from an initial concussion and sustains another concussion before the first has cleared completely, then he may be at risk for Second Impact Syndrome (SIS) SIS is a very rare condition and typically occurs in teen aged males SIS has never been reported in females or in professional athletes SIS occurs when an athlete sustains an initial concussion that is unrecognized, not reported, or has not fully healed, SIS occurs when an athlete sustains an initial concussion that is unrecognized, not reported, or has not fully healed The brain remains in a vulnerable state from the initial concussion (energy crisis) The athlete then sustains a second concussion which causes additional chemical changes in the brain that lead to severe brain swelling The brain is encased in a hard skull and can only expand within certain limits SIS usually results in permanent disability or death __________________________________________________________ Effective January 1, 2014 Sports Concussion: Long Term Effects Post-Concussion Syndrome (PCS) Chronic Traumatic Encephalopathy (CTE) Post-Concussion Syndrome (PCS) The term was first used by an article by Strauss and Savitsky in 1934 Multiple definitions abound and vary somewhat, but all involve a constellation of symptoms after a blow to the head Symptoms common to most definitions include a persistence of the initial concussion symptoms, including headaches, dizziness, fatigue, irritability, forgetfulness, poor concentration, blurred vision, sensitivity to light and noise, frustration, sleep disturbance, difficulty thinking, nausea, depression, increased emotionality The diagnosis is made anywhere from 6 weeks to 3 months post-injury Most of the scientific research on PCS has been done on civilians, and more recently, on military personnel experiencing blast injuries Studies of PCS in athletes are now being conducted In general, less than 10% of athletes are diagnosed with PCS Most of these athletes recover within 6-12 months, although there is a small group that remains symptomatic longer PCS typically involves multiple factors and usually requires a multi-disciplinary treatment approach Chronic Traumatic Encephalopathy (CTE) • Punch-Drunk Syndrome (Martland, 1928, JAMA) • Dementia Pugilistica (Millspaugh, 1937, US Navy Medical Bulletin) • Psychopathic deterioration of pugilists (Courville, 1962, Bulletin Los Angeles Neurological Society) • Chronic traumatic encephalopathy (Miller, 1966, Proceedings of The Royal Society of Medicine) • Chronic traumatic brain injury (Jordan et al., 1997, JAMA) CTE has receive a resurgence of interest due to several professional athletes (especially football players) being diagnosed with CTE after death The current definitions of CTE are somewhat different but common elements include the appearance of a tau protein in brain tissue, found on autopsy Mood, behavioral, and cognitive changes occur prior to death CTE is an evolving area of study and merits close scientific investigation with well designed, well controlled research CTE, like most neurodegenerative disorders, is a multifaceted brain disease that involves a variety of genetic, athletic exposure, and lifestyle factors “…a cause and effect relationship has not yet been demonstrated between CTE and concussions or exposure to contact sports.” Thanks to all of you for being here today, and special thanks to Rawlings for their support Concussion Baseline Testing Tim Lee, MHA, MS, ATC Coordinator, VSCC What is baseline testing? • Baseline testing is a series of standardized exams used to assess an athlete’s balance, brain function, and symptoms. • Results of the baseline test can be used to compare to a follow-up exam if the athlete has a suspected concussion What is included in VSCC baseline testing? 875-8722 • • • • Clinical Visit Neurologic history Symptoms Checklist Modified Balance Error Scoring System (mBESS) ImPACT (Immediate Post Concussion Assessment and Cognitive Testing)Test What is included in VSCC baseline testing? • On-Site/Mass Testing • Symptoms Checklist • ImPACT (Immediate Post Concussion Assessment and Cognitive Testing)Test VSCC Neurological History Symptoms Checklist Consent Form mBESS Testing ImPACT Test • Module 1: Word Discrimination • Module 2: Design Memory • Module 3: X’s and O’s • Module 4: Symbol Matching • Module 5: Color Match • Module 6: Three Letter Memory _______________________________________________ These subtests yield scores in Verbal Memory, Visual Memory, Visual Motor (Processing) Speed, and Reaction Time When should an athlete be baseline tested? • Pre-season, before contact • Currently, ages 12 years old up. How often should an athlete be baseline tested? • Every 2 years • Unless an athlete has suffered a concussion, has a new diagnosis of ADD/ADHD, or learning disability • mBESS and symptoms checklists should be performed yearly. Who should administer the baseline test? • A trained healthcare professional (MD, DO, ATC, PhD, PT) • The testing environment should be quiet and free from distractions • Computer-based testing should not be performed at home or anywhere without supervision Who should interpret the test results? • A healthcare professional trained in concussion management What are we looking for in these tests after a concussion? • We are expecting that the athlete’s test scores on all the measures will have returned to the baseline values. • This would indicate that the athlete has most likely recovered from the concussion. Concussion Baseline Testing for All Now Available [email protected] ------------------------------------------------------------------------------A concussion is an urgent medical problem and we strive to evaluate patients within 72 hours of injury. Call us to make an appointment. (615) 875-VSCC (8722) Sports Concussion: Sideline and Initial Management Jim Fiechtl, MD Assistant Professor: Depts. Of EM and Orthopedics Vanderbilt Bone and Joint Clinic Vanderbilt Bone & Joint Disclosures • Unfortunately, I have no financial disclosures to make, but I am always willing to listen. Vanderbilt Bone & Joint Objectives • • • • How to recognize? What we are doing on the sideline? What to do in the first 48 hours? What is this TSSAA form? Vanderbilt Bone & Joint Who is concussed? http://i.cdn.turner.com/si/multimedia/photo_gallery/0910/cfb.impact.injuries/images/tim-tebow.3.jpg Vanderbilt Bone & Joint Who is concussed? http://www.cbssports.com/mcc/blogs/entry/24156338/29747154 Vanderbilt Bone & Joint Who is concussed? http://theother87.files.wordpress.com/2011/05/youth-soccer.jpg Vanderbilt Bone & Joint Who does the evaluation? • Anyone trained – Means someone has been trained – Coach – Certified Athletic Trainer – Physician – Team Parent http://www.trophies2go.com/team-mom-trophy Vanderbilt Bone & Joint What are we looking for? • Lying on the ground/slow to get up – Are they unconscious? • • • • Unsteady or wobbly Grabbing their head Dazed, blank look Confused, running wrong plays Pocket Concussion Recognition Tool™ Vanderbilt Bone & Joint Lying Motionless • If unconscious, assume a cervical spine injury – C-spine control – Activate Emergency Action Plan • Take your time – ensure safety • Needs to go to Emergency Department http://mnhopper1s.files.wordpress.com/2011/10/spine.jpg?w=4 20&h=337 Vanderbilt Bone & Joint Able to Move • • • • Take your time – ensure safety Move them to a ‘quiet’ area on the sideline Give the player a few minutes to catch breath Observe Vanderbilt Bone & Joint Sideline Assessment • Maddocks’ Questions – What city and stadium? – Opponent? – Month and day? – Remember being injured, score of the game, the play, etc • Memory and Cognition – Months, 3 objects, numbers backwards Vanderbilt Bone & Joint Sideline Assessment • Brief Neuro Exam – – – – Cranial nerves Strength Balance Cerebellar Vanderbilt Bone & Joint When can they go back in? They’re done for the day. Vanderbilt Bone & Joint Who needs a trip to the ER? • Worsening headache or symptoms • Drowsy, hard to awaken • Repeated vomiting • Unusual behavior • Seizures • Weakness or numbness in arms or legs • Slurred speech, unsteady walking Putukian. BJSM 2013;47:285-8. Vanderbilt Bone & Joint http://ia.mediaimdb.com/images/M/MV5BMjA0NjI0ODgzNF5BMl5BanBn XkFtZTcwMDAxNDUyMQ@@._V1_SY317_CR20,0,214,317 Once in the ER… • To Scan or Not To Scan – Why not scan everyone? • Multiple prediction rules Vanderbilt Bone & Joint What Does this all Mean? • Think about Headache Plus – the Sills Criteria – – – – – – – – – Worsening Persistent Vomiting Altered (GCS < 15) Older (> 60) Prolonged amnesia (> 2 hours) Seizure Fracture Social Situation Anticoagulants Vanderbilt Bone & Joint Now, what do we do – Initial Management • Rest, Rest, Rest – Brain Rest: limit screen time, noises – Physical Rest: no exertion • Medications – Acetaminophen over Ibuprofen, certainly over Aspirin • Let them sleep – Don’t awaken every 2 hours • Symptoms can develop over 24-48 hours Vanderbilt Bone & Joint Post-injury Follow-up • Who needs follow-up? – Everyone will need medical clearance – ED can not clear you back to sport • Timing? – Emergent v. Clinic • School assistance • Additional medications and/or specialty referrals Vanderbilt Bone & Joint Summary • Someone trained at every event • Recognize and remove from the game – No return to play on the same day • • • • Remember what leads to an ER trip Rest – brain and body Can evolve over 24-48 hours Needs medical clearance for return to play – Provide additional resources, school help Vanderbilt Bone & Joint Post Injury Management and Rehab Or, What do I do now? Allen Sills, MD, FACS Associate Professor of Neurosurgery, Orthopedic Surgery and Rehabilitation Co-Director, Vanderbilt Sports Concussion Center Team Neurosurgeon - Nashville Predators Consulting Neurosurgeon to: Vanderbilt University Athletics Belmont University Athletics US Olympic Equestrian Team Federation Equestrian Internationale (FEI) Concussion in Sport Group Outline • What is a comprehensive concussion plan and who should have one? • How do we safely return someone to play after a concussion? • What does “return to learn” mean? • When should ImPACT testing be repeated? • What to do when symptoms continue for more than a few days? Comprehensive Concussion Plan Comprehensive Concussion Plan • Defines goals, key personnel, groups to be served • Discusses prevention and equipment • Details baseline evaluations • Delineates immediate management • Identifies “red flags” for urgent medical evaluation or transfer to ER • Determines follow up care • Return to Play (RTP) protocol Concussion Plan • Not a “rigid recipe” but rather a roadmap to a common destination – Allows for rest stops and sightseeing – individual flexibility! • But it is not OK to just “wing it”! – Increases liability – Decreases credibility • No need to reinvent the wheel Return to Play “When can my boy get back out there where he belongs?” Return to Play - goals • Return athlete to play as soon as possible after brain injury has healed • Emphasize actions and treatments that enhance and promote recovery • Avoid actions and treatments that hinder recovery • Return to play really begins as soon as concussion is diagnosed Same Day Return to Play • Once any athlete at any age has been diagnosed with any concussion they are done for that day – – – – No exceptions! No such thing as a ding! No grading scale Be aware that some injuries may evolve over time and symptoms may be delayed – Serial evaluations are helpful Acute treatment • First 48 hrs – Physical AND cognitive rest – Avoid tasks which increase symptoms • “overstimulation” of brain • Simplify brain inputs – “live like the Andy Griffith show” – Some symptoms may evolve • especially headache, concentration Acute treatment • First 48 hrs – Encourage sleep • Don’t need the every hour wakeup! • “excessive” sleep probably OK – School OK depending on tolerance • Low threshold for absence – generally avoid until no symptoms for 24 hours – Meds – Tylenol usually adequate – Red flags – immediate referral for medical eval • Previous talk – ER physician CANNOT CLEAR FOR RETURN TO PLAY!!! After 48 hours • Reassess by practitioner trained in concussion management • NO role for ImPACT testing in this stage – May increase symptoms – Practice effect – Does not change plan • Once asymptomatic for 24 hrs can return to class – If symptoms in class may need to modify schedule Return to play stages Return to Play progression • After a concussion, we want to GRADUALLY increase exertion in a progressive manner to see if the athlete has symtoms – Athletes may have no symptoms at rest but symptoms may emerge with exertion – This means the brain has not fully healed from the concussion Return to Play progression • Steps should be spelled out in your concussion plan • Should be overseen by someone trained in concussion management – Athletic trainer – Physical therapist – Physician (MD/DO), nurse practitioner (NP) or physician’s assistant (PA) experienced in athletic medicine and concussion care Return to Play - stages • • • • • Phase “0” – cognitive exertion Phase 1 – aerobic exertion Phase 2 – functional testing progression Phase 3 – sport specific exertion Phase 4 – limited drills and non-contact practice • Phase 5 – full participation without restrictions • For most athletes 24 hour minimum per phase From the Vanderbilt University Athletics Mild Traumatic Brain Injury (mTBI)/Concussion Evaluation Guidelines (2012) RTP Phase 0 – Cognitive Exertion • No physical exertion until completion of full school day and all academic work with NO symptoms • If no school – find other cognitive tasks – Reading for comprehension Courtesy of Tracy Campbell, ATC • The athlete must be able to “Return to Learn” BEFORE they can begin the “Return to Play” pathway RTP Phase 1 – Aerobic Exertion • Begin exertion to raise HR under monitored conditions • Example: Functional exertion test – Bike 20 minutes @ 70 percent of predicted maximum heart rate(PMHR) – Rest for 15 minutes – Monitor symptoms – Incremental Treadmill Test 20 minutes From the Vanderbilt University Athletics Mild Traumatic Brain Injury (mTBI)/Concussion Evaluation Guidelines (2012) RTP Phase 2 – Functional Testing Progression • More complex movements at higher pace, but generally in a single plane • Examples: – – – – – – – Scissor step/quick step Jogs lateral shuffle Backpedal Sit-ups Push-ups Sprints From the Vanderbilt University Athletics Mild Traumatic Brain Injury (mTBI)/Concussion Evaluation Guidelines (2012) RTP Phase 3 – Sport Specific Exertion • Initial – Moderate aerobic exercises specific to sport – Duration approximately 10- 15 minutes with 5 minutes rest post session • Intermediate – Progressively difficult aerobic exercises specific to sport – Duration approximately 10- 15 minutes with 5 minutes rest post session – • Advanced – Demanding aerobic exercises specific to sport – Duration approximately 10- 15 minutes with 5 minutes rest post session From the Vanderbilt University Athletics Mild Traumatic Brain Injury (mTBI)/Concussion Evaluation Guidelines (2012) RTP Phase 3 – Sport Specific Exertion Example • SPORTS SPECIFIC EXERCISES - BASKETBALL • Initial – – – – • Intermediate – – – • 10 laps around floor—sprint straight away/slide baseline Sprints full court Backpedal lateral Shuffle Defensive zigzag Square drill Shooting/post drills—timed Advanced – Intervals 10 x 40 sec duration w/minute rest • • • • • • Each interval contains various movements Lateral shuffle Sprints Change of direction Jumping backpedal From the Vanderbilt University Athletics Mild Traumatic Brain Injury (mTBI)/Concussion Evaluation Guidelines (2012) RTP Phase 4 – Return to Limited Drills and Non-contact Practice • Non-contact training drills dependent upon sport • Athlete can practice with team but no contact • Consult team physician for full clearance From the Vanderbilt University Athletics Mild Traumatic Brain Injury (mTBI)/Concussion Evaluation Guidelines (2012) RTP Phase 5 – Return to Full Participation without restrictions • Full participation without restriction • For collision sports will usually practice full speed with contact before game action (if available) From the Vanderbilt University Athletics Mild Traumatic Brain Injury (mTBI)/Concussion Evaluation Guidelines (2012) RTP – How NOT to do it • “We didn’t let him practice all week and he feels good today (Thursday) so we’re gonna let him play Friday night.” • “He rested for 3 days then I put him on the bike today for 15 minutes and he did fine so I let him go to practice today” • “She felt bad all weekend but today she just has a slight headache and seemed ok in warmups so I let her go.” RTP – “Pearls” • If athlete has symptoms during one stage, then should rest for 24 hours and go back to previous stage • Careful observation during and after final stage / first game back – EDUCATION of athlete! • An extra few days in the RTP protocol might save your athlete a month, a season, or even a whole school year! When should ImPACT testing be repeated? • Purpose of repeat test is to make sure that brain function has returned to baseline – Especially if athlete is not being truthful about their symptoms! • NO reason to repeat test if athlete is still having symptoms When should ImPACT testing be repeated? • Can do test either prior to starting RTP protocol or at any stage as long as athlete is still without symptoms • ImPACT test alone cannot “clear” an athlete to return – it is a PART of an overall assessment to be used by a trained provider Prolonged Recovery JAE S. LEE / THE TENNESSEAN Pathways to Recovery • 2 general “pathways” to recovery have been identified – Standard (80 – 90%) • all symptoms resolve in 7 to14 days – Prolonged (10 – 20%) • Symptoms for > 30 days • This distinction appears over time and initial treatment principles are same Prolonged recovery • Definition: more than 30 days of symptoms • Symptoms may not be specific to concussion – Require other management strategies – Advanced imaging – Formal neuropsych testing Prolonged recovery • All of these patients will benefit from evaluation by a concussion specialist and a multi-disciplinary approach • Advanced interventions – Treat sleep / mood problems – Headache prophylaxis and treatment – Vestibular assessment and rehab for balance issues – Cognitive evaluation and therapy for persistent school problems Vanderbilt Sports Concussion Center • (615) 875 – VSCC (8722) • www.vanderbiltsportsconcussion.com • Specialists in: – – – – – – – – – – Sports medicine, neurosurgery, neurology Sports neuropsychology Headache management Sleep medicine Balance and vestibular problems Speech and cognitive therapy Ear, nose and throat Advanced MRI and imaging Physical and occupational therapists Supervised return to play Prolonged recovery – what to avoid • Avoid social and personal isolation for prolonged periods of time – – – – No school No sport No social activities No life! Summary • Everyone needs a concussion plan – You need a trained provider to evaluate athletes who sustain a concussion and to supervise their return to play • No RTP same day – no exceptions • Physical and cognitive rest in first 48 hrs • No physical exertion until asymptomatic with brain exertion • Stepwise RTP – be systematic • Athletes with prolonged recovery are unique and need specialist assessment Thanks! VSCC & Rawlings Concussion Education Program Prevention of Concussion: What Works, What Doesn’t and What’s Next April 30, 2013 Alex B. Diamond, D.O., M.P.H. Assistant Professor of Orthopaedics and Rehabilitation Assistant Professor of Pediatrics Medical Director, Program for Injury Prevention in Youth Sports (PIPYS) Vanderbilt University Medical Center Team Physician Vanderbilt & Belmont Universities Nashville Sounds & Nashville Predators Vanderbilt Sports Medicine Injury Prevention 101 Vanderbilt Sports Medicine Categories of Prevention • Primary – Preventing the injury from happening • Secondary – Reducing a possible injury’s severity • Tertiary – Working for the best outcome after an injury Vanderbilt Sports Medicine Injury Prevention is a Team Sport Vanderbilt Sports Medicine Emery CA et al. CJSM, 2006. Safety cannot be delegated, it is a shared responsibility of… • Parents • Coaches • Youth athletes • Safety advocates • Athletic trainers • Schools • Health professionals Vanderbilt Sports Medicine Approaches To Prevention Clinical Care Research Vanderbilt Sports Medicine Strategies for Concussion Prevention Vanderbilt Sports Medicine Concussion Prevention: Equipment • Football Helmets • Mouth Guards • Head Gear Vanderbilt Sports Medicine Virginia Tech National Impact Database. May 2012. Football Helmet Ratings: STAR Evaluation System • 5 Stars Reduction in concussion risk – Riddell 360 – Rawlings Quantum Plus – Riddell Revolution Speed • 4 Stars – – – – – – – Schutt ION 4D Schutt DNA Pro + Rawlings Impulse Xenith X1 Ridell Revolution Rawlings Quantum Riddell Revolution IQ • 3 Stars – Schutt Air XP – Xenith X2 • 2 Stars – Schutt Air Advantage • 1 Star – Riddell VSR4 • 0 Stars – Adams A2000 Pro Elite Vanderbilt Sports Medicine Mouth Guards • Effects of mouth guards on dental injuries and concussion in college basketball. – Labella et al. MSSE, 2002. (LOE 2) • Findings: – No difference in concussion rate – Significantly lower rate of dental trauma Vanderbilt Sports Medicine Head Gear in Soccer • Withnall et al. BJSM, 2005. – Three equipment types tested – No attenuation of mechanical forces due to heading ball – 33% reduction in acceleration forces from direct head-to-head contact – Further evidence needed for effect on injury or concussion prevention Vanderbilt Sports Medicine Navarro RR. Curr Sports Med Reports, 2011. Vanderbilt Sports Medicine McIntosh AS et al. BJSM, 2011. Summary of Helmet Benefits in Sports Vanderbilt Sports Medicine Headgear Fitting • Important across sports – A well maintained, properly fitted helmet required to provide advertised level of protection to athlete • Serious head injury (not concussion) – Frequently inspect equipment for wear and tear including cracks, defects and loss of proper fit • Hands-on demonstration – Rawlings Vanderbilt Sports Medicine
© Copyright 2026