Chemotherapy Dosing in Special Populations Sabine Kaestner MSci Pharm, PhD
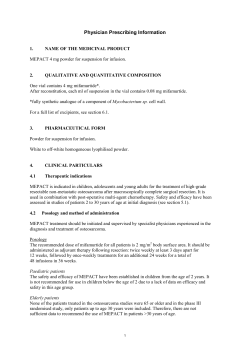
Chemotherapy Dosing in Special Populations Sabine Kaestner MSci Pharm, PhD Plymouth Hospitals Trust Plymouth, UK [email protected] 1 Disclosure Sabine Kaestner, MSci Pharm, PhD has no real or apparent conflicts of interest to report 2 Learning Objectives Indicate which patient-related factors may affect the pharmacokinetics (PK) and pharmacodynamics (PD) of cancer chemotherapy drugs in special populations Assess and discuss the potential clinical impact of different approaches to chemotherapy dose modifications in special populations Identify sources for inaccuracies and errors in chemotherapy dosage calculations/modifications 3 Lecture Outline Dosing of chemotherapy drugs: Background Chemotherapy dosing in • Amputees • • • Obese patients Elderly Pregnant patients 4 Dosing of Chemotherapy Drugs: Background 5 Cancer Chemotherapy Characteristics • Narrow therapeutic window • Intrapatient variability Therapeutic & toxic effects • Interpatient variability Patient-specific doses … 6 Cancer Chemotherapy … but treatment effects difficult to measure Disease progression Drugs in combinations What should be measured? – Tumour regression – Disease-free or overall survival – Surrogate markers (PK) Follow-up? 7 Chemotherapy Dose Traditionally based on body surface area (BSA) • • • Used for interspecies scaling Often poorly correlated with drug clearance Generally fails to reduce PK variability, some exceptions • Does not account for several factors affecting drug clearance Calvert-formula for carboplatin dose an exception Kaestner SA, Sewell GJ. Clin Oncol (R Coll Radiol). 2007;19:23-37. 8 BSA vs Drug Clearance: 5-Fluorouracil (5-FU) 9 Chemotherapy Dose Modifications Dose reductions or delays, because of • Excessive toxicity • Hepatic and renal impairment • Age or obesity • Previous chemotherapy treatment Dose escalations?? • Not as common • Potential for underdosing Bonadonna G, et al. N Engl J Med. 1995;332:901-6. 10 Chemotherapy Dosing in Amputees 11 Chemotherapy Dose Various approaches • Standard BSA dosing Pre-amputation height and weight? • Dose modification based on BSA reduction Formulae to subtract area of appropriate limb • Dose modification based on weight reduction O’Marcaigh AS, et al. J Pediatr Hematol Oncol. 1995;17:172-5. Colangelo PM, et al. Am J Hosp Pharm. 1984;41:2650-5. 12 Any Evidence Supporting Dose Modifications? No evidence No common guidelines regarding dose modifications • Need for trials and standardisation Amputation clearly not the only factor • Young, old, comorbidities, medications, pharmacogenetics … Use professional judgement? 13 PK in Amputees Drug distribution • • • Change in body composition ↓ Size of vascular system Cardiac output may change Drug metabolism (and excretion) unlikely to change Note: renal function estimates based on serum creatinine inaccurate in amputees Duong CD, Loh JY. J Oncol Pharm Pract. 2006;12:223-36. 14 Chemotherapy Dosing in Obese Patients 15 Obesity and Cancer Overweight/obesity (body mass index [BMI] > 25 and 30 kg/m22) ⇒ ↑ cancer risk • UK study, 1.2 million women Lack of physical activity ⇒ ↑ breast cancer risk Increasing BMI associated with poorer cancer survival • Due to delayed diagnoses or insufficient treatment? Reeves GK, et al. BMJ. 2007;335:1134. Epub. Tao MH, et al. Am J Epidemiol. 2006;163:101-7. 16 Dose Modifications in Obesity Obesity associated with large first-cycle dose reductions Reluctance to prescribe full doses due to fear of excessive toxicity Doses rarely escalated in subsequent cycles ⇒ Potential for underdosing (should not reduce < 85% of standard dose intensity [DI]) No evidence Griggs JJ, et al. Arch Intern Med. 2005;165:1267-73. 17 Dose Modifications in Obesity Examples of different approaches • • • • • BSA doses “capped” at 2.0 - 2.2 m22 BSA based on lean body mass (LBM) or ideal body weight (IBW) BSA based on average between actual weight and IBW Cap according to BMI Reduce dose empirically ⇒ Varies between prescribers/institutions Baker SD, et al. J Natl Cancer Inst. 1995;87:333-4. Green B, Duffull SB. Br J Clin Pharmacol. 2004;58:119-33. 18 Considerations Use of total body weight: up to 25% - 30% dose increases BSA does not reflect body composition What contributes to the large BSA? • Patient 1 Weight: 95 kg Height: 160 cm ⇒ BSA: 2 m22 BMI: 37 kg/m22 • Patient 2 Weight: 80 kg Height: 180 cm ⇒ BSA: 2 m22 BMI: 25 kg/m22 19 What Are the Clinical Outcomes? Full doses do not seem to increase toxicity in obese Full doses may even give reduced toxicity compared with in non-obese Therapeutic effects • May diminish beneficial impact of adjuvant chemotherapy • Use of actual body weight associated with improved overall survival • More studies needed Poikonen P, et al. Acta Oncol. 2001;40:67-71. 20 Is There a Better Approach? PK alterations in obesity • Drug distribution Body composition ↑ Alpha 1-acid glycoprotein • Metabolism Phase 1 processes – Activity or amount of selected CYP450 enzymes may be elevated Phase 2 processes – ↑ Glucuronidation and sulfation Baker SD, et al. J Natl Cancer Inst. 1995;87:333-4; Morgan DJ, Bray KM. Clin Pharmacokinet. 1994;26:292-307; Blouin RA, et al. Clin Pharm. 1987;6:706-14. 21 Is There a Better Approach? PK alterations in obesity • Excretion ↑ Glomerular filtration and tubular secretion Note: Renal function estimates may be inaccurate in obese Serum creatinine alone not useful Lack of PK data for cytotoxic drugs in obesity Herrington JD, et al. Cancer Chemother Pharmacol. 2006;57:241-7. 22 PK of Selected Cytotoxic Drugs Recent report for drugs with different elimination pathways Elimination Pathway Clearance in Obese Cisplatin Renal tubular secretion (unbound) ↑ Paclitaxel CYP2C8, CYP3A4 ↑ Troxacitabine Renal filtration ↑ Carboplatin Renal filtration ↔ Docetaxel CYP3A4 ↔ Drug Irinotecan/SN-38 hCE2/CYP3A4/UGT1A1 ↔ Topotecan Renal tubular secretion ↔ Doxorubicin Aldoketoreductases Sparreboom A, et al. J Clin Oncol. 2007;25:4707-13. ↔ men ↓ women 23 Conclusions Various factors may alter drug clearance in obesity Large potential for underdosing with “capped” doses and additional errors may be introduced More studies needed, but … • All obese are not the same • Impact of obesity “itself” unlikely to override factors known to influence drug disposition e.g. pharmacogenetics (DPD and UGT1A1 enzymes) 24 Chemotherapy Dosing in the Elderly 25 Cancer and Age When are we classified as “elderly” patients? Diagnosis and treatment complicated by background pathophysiology, comorbidity, etc. Ageing alters biology of cancer • DNA damage • Host antitumour response 60% of new cancer diagnoses in patients >65 y. Yancik R. Cancer. 1997;80:1273-83. 26 Treatment Considerations Age “Poor prognosis” “Poor tolerance” Ageing and treatment response • Cancer cells less aggressive, more resistant, less responsive PK and PD may increase susceptibility to adverse effects (AEs) • Reduced clearance • Vulnerability and comorbidity, e.g. cardiovascular cardiovascular hepatic hepatic renal renal nervous nervous & & respiratory respiratory systems systems 27 Treatment Considerations 28 Treatment Considerations ⇒ “Is it worth it?” Benefit varies with likelihood of cancer-related death Quality of life? Life expectancy often underestimated (UK data): Remaining years Age Male Female 65 16.9 19.7 75 10.2 12.2 85 5.5 6.5 The Office for National Statistics. Available at: www.statistics.gov.uk/StatBase/Product.asp?vlnk=14459. 29 Chemotherapy Dosage Underrepresentation in clinical trials Lack of evidence Age >65 years frequently associated with no chemotherapy or reduced doses Chronological age alone does not • Contraindicate chemotherapy • Justify empiric dose reductions Elderly a more heterogeneous population than young Griggs JJ, et al. Arch Intern Med. 2005;165:1267-73. 30 A Multidisciplinary Assessment Concomitant medications and interactions Compliance Functional status Social support Histological diagnosis Life expectancy Clinical stage Comorbidity Nutritional status Physiological functions Performance status Psychological status Alternatives to chemotherapy Likely response to treatment Aim of chemotherapy Basic screening tools have been evaluated Aapro MS. J Clin Oncol. 2005;23:2121-2; COIN Guidelines. Clin Oncol (R Coll Radiol). 2001;13:S211. 31 PK in Elderly: General Changes Bioavailability and distribution • ↓ Gastrointestinal absorption and motility • ↓ Lean body mass • ↑ Adipose tissue • ↓ Albumin (15%–20%) • Haemoglobin? Hurria A, Lichtman SM. Cancer Control. 2007;14:32-43; Wildiers H, et al. Clin Pharmacokinet. 2003;42:1213-42. 32 PK in Elderly: General Changes Metabolism and excretion • ↓ Hepatic volume and perfusion • Phase 1 reactions modified ↓ Some CYP450 activity • ↔ Phase 2 reactions • ↓ Renal filtration (1 mL/min/year >40 y in the majority) Note: Serum creatinine for estimating renal function inaccurate in elderly Aapro MS. J Clin Oncol. 2005;23:2121-2; Hurria A, Lichtman SM. Cancer Control. 2007;14:32-43; Wildiers H, et al. Clin Pharmacokinet. 2003;42:1213-42; Lichtman SM, Villani G. Cancer Control. 2000;7:548-56; Marx GM, et al. Ann Oncol. 2004;15:291-5. 33 Chemotherapy PK/PD in Elderly PK and PD data exist for selected drugs Most studies find no significant difference in PK PD may differ independently of PK Few drug doses may have to be adjusted purely based on age Observations not always consistent • Study inclusion criteria? ⇒ Some examples 34 Chemotherapy PK/PD in Elderly Drug Dose Modification Age-Related PK? CL ↓/↔ F? Comments Myelosuppression ↑, non-PK related Etoposide Age Renal imp. Gemcitabine Hepatic imp. Renal imp. Methotrexate Age? Renal imp. CL ↓ Toxicity may be increased. Folinic acid rescue important. 5-FU Renal imp. CL ↔ Stomatitis risk ↑ Capecitabine Renal imp. CL ↔ F↔ Topotecan Renal imp. Irinotecan Plasma proteins? Vinorelbine Severe hepatic imp. CL ↓/↔ − CL ↔ Temozolomide Minimal toxicity in elderly CL ↔ Diarrhoea risk ↑ Favourable toxicity profile Myelosuppression ↑, non-PK related Imp. = impairment, CL = clearance, F = bioavailability, 5-FU = 5-fluorouracil Hurria A, Lichtman SM. Cancer Control. 2007;14:32-43; Wildiers H, et al. Clin Pharmacokinet. 2003;42:1213-42; 35 Lichtman SM, Villani G. Cancer Control. 2000;7:548-56. Chemotherapy PK/PD in Elderly Drug Dose Modification Age-Related PK? CL ↓/↔ Comments Cardiotoxicity ↑. Often avoided, great care needed (esp. with trastuzumab). Add dexrazoxane. Liposomal formulations may be beneficial. Doxorubicin Hepatic imp. Idarubicin Renal imp. Epirubicin Hepatic imp. Mitoxantrone Hepatic imp. CL ↔ Paclitaxel Docetaxel Hepatic imp. CL ↓/↔ Cisplatin Age? Renal imp. Plasma proteins CL ↓ Enhanced toxicity. Age an independent factor for CL ↓ Carboplatin Renal imp. CL ↔ Care when using serum creatinine-based formulae Oxaliplatin Renal imp. Erythrocytes? CL ↔ Lack of nephrotoxicity, lower haematotoxicity than cis/carbo CL ↔ Myelosuppression ↑, mesna Cyclophosphamide - CL ↔ Well tolerated Well tolerated, esp. weekly Favourable toxicity profile Care if concurrent treatment with other neurotoxic drugs Hurria A, Lichtman SM. Cancer Control. 2007;14:32-43; Wildiers H, et al. Clin Pharmacokinet. 2003;42:1213-42; 36 Lichtman SM, Villani G. Cancer Control. 2000;7:548-56. Supportive Therapy Crucial for treatment completion Hydration status important • Poor hydration may lead to reduced clearance Prophylactic haematopoietic growth factors (GFs) often recommended • Do not have to compromise DI • Cost-effective • Results in non-haematologic dose-limiting toxicity, e.g. gastrointestinal, neuropathy, and mucositis Repetto L, et al. Eur J Cancer. 2003;39:2264-72. Wildiers H, et al. Clin Pharmacokinet. 2003;42:1213-42. 37 Conclusions Poor prognostic outcomes not universal Age not contraindication for treatment Response poor in frail but other elderly should be treated as younger patients Dose reduction = simplistic approach Dose optimisation through full geriatric assessment May start with lower dose but should escalate if well tolerated Treat complications early Balducci L. Cancer Control. 2001;8:1-25. 38 Chemotherapy Dosing in Pregnant Patients 39 Cancer During Pregnancy Estimated to complicate 0.02 to 0.1% of pregnancies ∼10% of those <40 y diagnosed with breast cancer are pregnant Increasing incidence expected as women delay childbearing Common cancers: cervical, breast, lymphoma, and malignant melanoma Cancer in pregnancy. Available at: www.motherisk.org; Woo JC, et al. Arch Surg. 2003;138:91-9. 40 Treatment Goals Limited knowledge about effect of cancer on pregnancy and vice versa Goals • Save the mother’s life • Treat curable malignant disease • Protect the foetus and newborn from harmful treatment effects • Retain the mother’s reproductive system intact for future pregnancies 41 Options Termination of pregnancy • Treatment formerly considered indication for abortion • Not effective intervention (no survival benefit) Some exceptions Continuation of pregnancy with modified treatment regimens Postpone treatment until after delivery • Close monitoring of tumour growth Berry DL, et al. J Clin Oncol. 1999;17:855-61. 42 Risks Continuation of pregnancy with treatment • Which modifications? • Risks to the foetus • Increased risk of miscarriage, prematurity, stillbirth Continuation of pregnancy without treatment • Therapeutic delay May not be disadvantage in ER+ breast cancer • Metastasis risk in both mother and foetus Pereg D, et al. Haematologica. 2007;92:1230-7. 43 Treatment Options Surgery Chemotherapy • Modified schedule • Supportive care, e.g. Antiemetics Lack of data using GFs Radiotherapy contraindicated 44 Potential Adverse Effects “Life-saving vs life-threatening” Potential direct effects on foetus • • • • Malformations Neurologic development Intrauterine death miscarriage/stillbirth Intrauterine growth retardation and/or prematurity Effects on physical (e.g. heart, kidney) and mental development Epstein RJ. BMC Cancer. 2007;7:92. Epub; Cancer in pregnancy. Available at: www.motherisk.org 45 Potential Adverse Effects Potential effects on newborn/long-term • “Normal” chemotherapy AEs Haematologic toxicity – infectious complications – haemorrhage • • • Alopecia Ototoxicity Cardiotoxicity Respiratory complications Secondary malignancies Infertility Cardonick E, et al. Lancet Oncol. 2004;5:283-91; Cancer in pregnancy. Available at: www.motherisk.org 46 Chemotherapy Modifications Timing of treatment Choice of drugs Dosage Scheduling 47 Timing of Treatment No chemotherapy during first trimester • Teratogenic during organogenesis ∼ 8 weeks • Malformation risk 10% with single agent, 25% with combinations • Eyes, genitals and CNS remain vulnerable Second and third trimesters • Reduced hazard to foetus • “Planned” timing of delivery account for expected bone marrow depression Contraindicated during breast-feeding Cardonick E, et al. Lancet Oncol. 2004;5:283-91; Cancer in pregnancy. Available at: www.motherisk.org 48 Choice of Drugs Characteristics affecting placental transfer • Lipophilicity, molecular weight, protein binding • P-glycoprotein and CYPs? Long t½½ of drug/metabolites a disadvantage Cytotoxic drugs from all classes have • Been used successfully in adjuvant chemotherapy Follow-up? • Induced all types of toxicity Cardonick E, et al. Lancet Oncol. 2004;5:283-91; Cancer in pregnancy. Available at: www.motherisk.org 49 Choice of Drugs Standard or modified regimens, may exclude certain drugs Examples • • • • Some antimetabolites considered especially toxic Trastuzumab avoided (anhydramnios common AE) Doxorubicin or epirubicin preferable to idarubicin CAF; cyclophosphamide 500 mg/m22, doxorubicin 50 mg/m22, 5-FU 1,000 mg/m22 used successfully in breast cancer • FOLFOX6 in rectal cancer: oxaliplatin 85 mg/m22, fol. acid 400 mg/m22, 5-FU 400 mg/m22 + 2,400 mg/m22 46 h infusion Berry DL, et al. J Clin Oncol.1999;17:855-61. Epstein RJ. BMC Cancer. 2007;7:92 epub. Gensheimer M, et al. Cancer Chemother Pharmacol. 2008; Mar 21. [Epub ahead of print]. 50 Dosage and Scheduling Lack of data May try weekly schedules Standard doses, but … inadequate or excessive? • Adjust for continuous change in body weight? Anecdotal evidence of increased toxicity postpartum Reduced dose What about PK? Cardonick E, et al. Lancet Oncol. 2004;5:283-91. suboptimal effect? Resistance? 51 PK and PD in Pregnancy Clinical and PK studies difficult Changes during pregnancy • Hormonal • Bioavailability and distribution • Metabolism and excretion 52 Bioavailability and Distribution ↓ Gastric emptying/motility ↑ Body water and adipose tissue ↑ Cardiac output ↓ Albumin concentration (haemodilution) An additional compartment: amniotic fluid Anger GJ, Piquette-Miller M. Clin Pharmacol Ther. 2008;83:184-7. FDA: PK in pregnancy. Available at: http://www.fda.gov/cder/guidance/5917dft.htm. 53 Metabolism and Excretion Phase 1 processes • ↑ CYP3A4 activity and amount • ↑ CYP2D6 activity • ↓ CYP1A2 activity Phase 2 processes • Conjugating enzyme activity altered • e.g. ↑ glucuronidation ↑ Hepatic blood flow ↑ Renal blood flow (50%−80%) Anger GJ, Piquette-Miller M. Clin Pharmacol Ther. 2008;83:184-7. FDA: PK in pregnancy. Available at: http://www.fda.gov/cder/guidance/5917dft.htm. 54 Conclusions Termination of pregnancy does not (in general) improve maternal prognosis However, Still lack of information on optimal dosing strategies and benefits/risks with chemotherapy Impossible to predict risks to mother and foetus/child Each new case must be treated individually 55 Overall Conclusions Various factors may influence chemotherapy PK and PD in the special populations discussed Put potential effects of these factors into context of • Pre-existing Pre-existing intraintra- and and interpatient interpatient variabilities variabilities (enzyme (enzyme activity, activity, pharmacogenetics, pharmacogenetics, etc.) etc.) • Tumour Tumour PK/biology PK/biology and and drug drug resistance resistance • Concomitant Concomitant medications medications and and illnesses illnesses Customary dosing approaches may result in suboptimal treatment outcomes Modern strategies desirable, e.g. • Combinations Combinations of of population population data data and and patient-specific patient-specific data data in in Bayesian Bayesian approaches approaches • TDM? TDM? 56
© Copyright 2026