optom brochure
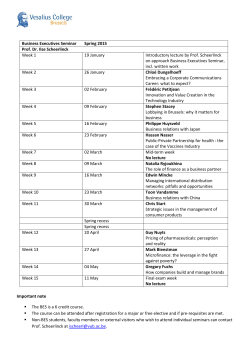
Optomax Conference Perth Sunday 3 May 2015 McCusker Auditorium Harry Perkins Institute limited tickets $349* *earlybird pricing there’s only 50 *earlybird tix available day e n o n i oints p D P ace C f o t & face c i t u nce e ape r r e e f h n t o early day C y e r n u o o All y ndly e i r f y l fami ime t d n m a u inim Work M / s t poin m u m i m.au Max .co x a m pto o t a ow n r e t Regis 31.5 Accredited CPD Points applied for Speakers Th e Au st ralia n I nst it u t e of Opt omet r y C o n f e r e n c e 2 0 1 1 Maximum CPD. Minimum Time. A/Prof Angus Turner Dr Angus Turner completed medical training at The University of Western Australia (UWA), before studying at Oxford University and completing a Masters of Evidence Based Medicine. Ophthalmology training was undertaken in Melbourne, followed by post-graduate training at University of Sydney in refractive surgical procedures. As Director of Outback Vision, Dr Turner is actively involved in the delivery of specialist outreach services to remote and Indigenous communities in the Kimberley, Pilbara, Goldfields, Great Southern, and South West regions. Dr Turner is an Associate Professor at UWA, where he is engaged in a number of research projects at the Lions Eye Institute, focusing on service delivery for remote and Indigenous people. Dr Turner is also a consultant at Fremantle Hospital and an ophthalmology teacher for the Rural Clinical School. A/Prof Steven Wiffen MB BS, FRACO, FRACS Associate Professor Wiffen trained in ophthalmology in Western Australia before undertaking fellowships at the CorneoPlastic Unit, East Grinstead, UK, and at the Mayo Clinic, Rochester, Minnesota, USA Associate Professor Wiffen is a consultant ophthalmologist at Fremantle Hospital and a Senior Lecturer at UWA He is Director of the Lions Eye Bank of Western Australia. Dr Jean-Louis deSousa Dr deSousa trained in ophthalmology in Perth before completing fellowships in ophthalmic plastic and reconstructive surgery in Oxford and East Grinstead in the UK. He is a member of the Australian and New Zealand Society of Ophthalmic Plastic Surgeons. A consultant ophthalmologist at Royal Perth Hospital he also provides ophthalmic services to the central wheatbelt from Merredin. Dr deSousa is the WA representative for continuing professional development and a basic sciences examiner for RANZCO. Prof Geoffrey Crawford MBBS, FRANZCO, FRACS Professor Crawford completed his ophthalmic training in Western Australia before undertaking further sub-speciality training in cornea and refractive surgery at Moorfields Eye Hospital, London, and Emory University, Atlanta, USA He is a Professor of Ophthalmology at the Centre for Ophthalmology and Visual Science, University of Western Australia He is Director of Surgical Services and a Corneal and Refractive surgeon at the Lions Eye Institute, Perth and is also a consultant ophthalmic surgeon at Royal Perth and Princess Margaret Hospitals. Professor Crawford has held many positions within RANZCO including Director of Continuing Professional Development, inaugural Chairman of the Programme Committee and Chairman of Examiners. He is a co-inventor of the AlphaCor artificial cornea and developed the techniques of its insertion. He also introduced LASIK surgery to Western Australia Dr Andrea Ang MBBS, MPH. Dr Ang completed her ophthalmic training in Western Australia before embarking on a Cornea, External Diseases, and Anterior Segment Fellowship at the Cincinnati Eye Institute, Ohio, USA She is currently completing a second Cornea Fellowship at the Singapore National Eye Centre, Singapore She was awarded a UWA Overseas Medical Fellowship and has written several publications and book chapters on ocular surface disease during her Fellowship. Her interests include ocular surface reconstruction techniques including limbal stem cell transplantation and keratoprostheses, and lamellar keratoplasty techniques, including anterior lamellar keratoplasty and Descemet’s stripping endothelial keratoplasty. Prof Ian McAllister Professor McAllister undertook training in Western Australia with additional sub-specialty training in vitreoretinal disorders in the USA He is Director of Clinical Services at Lions Eye Institute and a consultant ophthalmologist at King Edward Memorial Hospital for Women and the Royal Perth, Sir Charles Gairdner and Princess Margaret Hospitals. Professor McAllister is actively involved in research for cures for vitreoretinal disorders, especially retinal vascular disorders, and has held six NHMRC grants in this area He has been involved for many years in state wide diabetic retinopathy screening and treatment services and coordinates and reviews photographs from diabetic screening in remote parts of Western Australia Professor McAllister is currently vice chairman of the Ophthalmic Research Institute of Australia and has been chairman of the Research Board for many years. A/Prof Mei-Ling Tay-Kearney Associate Professor Tay-Kearney completed her medical training in Perth, Western Australia before pursuing postgraduate study at Johns Hopkins Hospital in Baltimore, USA In 2003 Associate Professor Tay-Kearney was appointed Head of Department of Ophthalmology at Royal Perth Hospital. She is a Senior Lecturer at UWA and a member of the Australian Society for HIV Medicine and the Australian Uveitis Study Group. She is the Chair of Qualifications and Education as well as an Examiner for the RANZCO Part 2 College examinations. Dr Vignesh Raja Dr. Vignesh Raja is a consultant ophthalmologist and vitreo-retinal surgeon at the Sir Charles Gairdner Hospital (SCGH). He has recently been appointed as the Head of Department of Ophthalmology at SCGH. Dr. Raja undertook his primary medical degree in India and completed his 3-year Masters in Ophthalmology from the world’s largest eye care system – the Aravind Eye Hospital and Postgraduate Institute of Ophthalmology. He pursued further specialist registrar training in Ophthalmology in the United Kingdom from 2004 -2012, completing fellowships in glaucoma and vitreo-retinal surgery at Liverpool and Oxford respectively. Dr. Raja moved to Perth in 2013 to do his second fellowship in medical and surgical retina with Prof. Ian Constable at SCGH and the Lion’s Eye Institute. In August 2014, Dr. Raja commenced private practice at the Joondalup Eye Clinic where he offers specialist consultations and treatments for cataract, glaucoma and medical & surgical retinal conditions. Prof Ian Constable Professor Ian Constable AO was the Lions Foundation Professor of Ophthalmology at the University of Western Australia 1975-2008 and continues to work as a Professor at that University. His principal interests are surgery of the retina and cataract as well as diagnosis and management of medical retinal conditions. He is Past President of the Asia Pacific Academy of Ophthalmology and the Asia Pacific Vitreoretinal Society and is the founding Chairman of the Asia Pacific Association of Ophthalmology Professors. He has published over 400 peer-reviewed articles and was the Chairman of the WA State Science Council from 2000 to 2006. He continues a busy clinical practice based at the Lions Eye Institute and Sir Charles Gairdner Hospital. Dr Antonio Giubilato Dr Antonio Giubilato underwent specialty fellowship training in glaucoma at the Royal Victorian Eye and Ear Hospital after training in ophthalmology in Perth, Western Australia. This included both clinical and surgical management of glaucoma as well as research into new therapies for the condition. He is presently consultant ophthalmologist in the Glaucoma Clinic at Royal Perth Hospital and also consults at Bentley Hospital for public patients. Dr Giubilato is currently Director of Training for the WA branch of RANZCO and an LSSF Board Member. Talk Synopsis Bridging eye health divides with technology A/Prof Angus Turner Retinal vein occlusion: pathogenesis, treatments and trials Prof Ian McAllister A review of the latest telehealth applications helping bring optometrists and ophthalmologists together to care for regional towns. The imaging and technology applications will be discussed with a series of clinical case presentations to demonstrate telehealth and outline eye health management of common presentations. This lecture will cover new treatment techniques in the management in retinal vein occlusion will cover the current approaches with their advantages and disadvantages. It will also examine how techniques can be modified in the future to produce more reliable and safer visual results. Diagnosis and management of Fuch’s dystrophy and endothelial failure A/Prof Steve Wiffen “Doctor, what is wrong with my eye?” A/Prof Mei-Ling Tay-Kearney Causes of corneal endothelial failure will be discussed along with management strategies and differential diagnosis. The pathogenisis of Fuchs’ dystrophy will be discussed in detail. Assessment and management of ptosis Dr Jean-Louis deSousa There are many causes of blepharoptosis, some associated with serious and life threatening disease though most are a source of mild visual and cosmetic symptoms. Treatment varies depending on the cause and is not always surgical. An understanding of the anatomy and physiology of the upper eyelid retractors forms the basis of accurate assessment and management of blepharoptosis. Diagnosis and management of Acanthameoba Prof Geoffrey Crawford Acanthamoeba can cause devastating visual complications and is more commonly found in contact lens wearers in western countries. This presentation will cover the differential diagnosis and possible treatments. Corneal dystrophies: diagnosis, differentials and management Dr Andrea Ang Corneal dystrophies are rare but understanding the management options for patients is important. Inflammatory eye disease grand rounds, diagnosis and management Analysis of the optic nerve in glaucoma using OCT Dr Vignesh Raja This talk will focus on the diagnostic capability and pitfalls of analysis of the optic nerve head in glaucoma using OCT technology, mainly the Cirrus HD-OCT and the Heidelberg Spectralis. This talk aims to highlight new parameters used in the evaluation of the glaucomatous optic nerve head and its significance in day-to-day practice. Gene therapy development in the context of wet macular degeneration Prof Ian Constable Wet AMD provides a crucial link between Optometry and Ophthalmology as it demands prompt diagnosis , urgent fluoresceine angiography and intravitreal injection. IV injections have become a huge cost burden and long term imposition on patients and their carers.Gene therapy developed in Perth may offer good control with less injections.Results in the first safety cohort of 6 patients are now published. The proceedure has proven to be convenient and safe. Results in our 27 active gene therapy cohort and randomized 13 controls will be independantly analysed in May/ June 2015. Cataract and Glaucoma Dr Antonio Giubilato IOP - Myths, Truths, Interpretation and Management Dr Antonio Giubilato Angle closure glaucoma has a number of mechanisms- pupil block, lens size,ciliary block and plateau iris . The lens/cataract has an integral role in the pathogenesis of angle closure . The interrelationship between the role of the lens and other mechanisms will be discussed and in particular the role of lens surgery in angle closure will be put into context. In Open Angle Glaucoma especially secondary causes e.g. Pseudo-exfoliation there remains a role for lens surgery . Cataract surgery alone in glaucoma patients may result in a small drop in IOP. After Trabeculectomy surgery significant rates of cataract formation occur. Cataract surgery after glaucoma surgery can result in glaucoma surgery failure . In open angle glaucoma cataract surgery should not be considered a treatment for glaucoma . However , The question “is my patient better off having cataract surgery prior to glaucoma surgery ?” should be asked. Whilst IOP is no longer included in the definition of glaucomas optic neuropathy it is integral in the management of glaucoma as it remains the only modifiable risk factor. IOP measurement is affected by numerous factors and the interpretation of “one off IOP measurements “can be difficult . IOP can be measured by different techniques with variable accuracy. The lowering of IOP in glaucoma management should aim to slow the disease by setting clinically appropriate target IOPs. A review of how to measure IOP including the reliability of different instruments and how IOP can vary with different ocular condition will be presented. In addition the interpretation of “one off IOP readings “ in glaucoma management will be discussed . The setting of clinically achievable target pressures and how to interpret the adequacy of management will evaluated Program Sunday 3 May 2015 McCusker Auditorium Harry Perkins Institute 7.45 Registration 8:00 Bridging eye health divides with technology A/Prof Angus Turner 9:20 Diagnosis and management of Fuch’s dystrophy and endothelial failure A/Prof Steve Wiffen 10:00 Assessment and management of ptosis Dr Jean-Louis deSousa 10:40 Diagnosis and management of Acanthameoba Prof Geoffrey Crawford 11:20 Corneal dystrophies: diagnosis, differentials and management Dr Andrea Ang 12:00 Lunch 12:30 Retinal vein occlusion: pathogenesis, treatments and trials Prof Ian McAllister 13:50 “Doctor, what is wrong with my eye?” A/Prof Mei-Ling Tay-Kearney 15:10 Analysis of the optic nerve in glaucoma using OCT Dr Vignesh Raja 15:50 Gene therapy development in the context of wet macular degeneration Prof Ian Constable 16:30 Cataract and Glaucoma Dr Antonio Giubilato 17:10 IOP - Myths, Truths, Interpretation and Management Dr Antonia Giubilato Register Th e Au st ralia n I nst it u t e of Opt omet r y C o n f e r e n c e 2 0 1 1 Maximum CPD. Minimum Time. Dates & Time How to Pay Sunday 3 May 2015 8:00 - 17:50 Registrations are open online now at www.optomax.com.au Cost Enquiries Earlybird*$349 Full $449 *earlybird pricing available for first 50 registrants only Maximum CPD points are achieved by successful completion of the assessment Web: Email: www.optomax.com.au [email protected] Terms & Conditions Terms and conditions apply, please see the website for details. Venue & Access McCusker Auditorium Harry Perkins Institute QQ Block, Sir Charles Gairdner Hospital 6 Verdun Street, Nedlands WA 6009 Cancellations If received more than 14 days prior to the event a full refund less $50 administration fee is applicable. After that date no refund is available. Parking Sir Charles Gairdner Hospital is well served by public transport. Parking is available onsite. register online www.optomax.com.au
© Copyright 2026