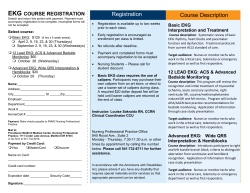
T The Basics of Neonatal EKG Interpretation C
C A R D I A C S E R I E S #15 The Basics of Neonatal EKG Interpretation Lyn Vargo, RNC, MSN, NNP T HE ELECTROCARDIOGRAM (EKG) CAN PROVIDE THE measurements found in a normal neonate would be considneonatal nurse with information about an infant’s ered abnormal in an adults For this reason, it is imperative heart rate, the conduction system of the neonatal heart, and that the appropriate age-adjusted tables be used to interpret the formation of normal and abnormal electrical impulses.’ EKG measurements. Clinicallv, the EKG is used to make deductions about the This article reviews the basic physiologic principles of the cardiac impulse and the EKG. It electrid’ hctivity of the heart and then relates these principles to inferences about cardiac pathology.2 The EKG is easily obtained the unique findings of the This article reviews the basic physiologic principles of the and is noninvasive. A 12-lead neonate and premature infant. cardiac impulse and the EKG. It then relates these findings EKG is most often used in evaluto the unique findings of the neonate and premature infant. ating cardiac arrhythmias, atrial EXAMINING Emphasis is placed on familiarizing nurses with the tktors or ventricular hypertrophy, eiecEKG PAPER afkting the basic neonatal EKG and on the usetirlness of An actual tracing of the trolyte abnormalities, myocardial cardiac rhythm strips and 12-lead EKGs. Topics addressed include evaluation of neonatal heart rate, examination of heart’s electrical activity can be or pericardial infections, myocarcomponents of the cardiac cycle, identification of possible made by a recording machine on dial ischemia and infarction, and cardiac dystimction, recognition of electrolyte imbalances, heat-sensitive EKG paper. EKG congenital heart disease.s and effects of digoxin administration on cardiac rhythm. paper is graph paper composed The normal EKG of the of small and large squares. Each neonate is very different from small square measures 1 mm by that of the older infant, child, or 1 mm, and each large square measures 5 mm by 5 mm. One adult (Figure 1). The EKG of the full-term neonate is slightly large square contains 25 small squares (Figure 2). different from that of the premature infant (Table 1). EKG paper measures two elements: time and voltage.’ In Changes occur in the normal EKG during the first minutes, routine EKG interpretation, the recording speed of the paper hours, days, weeks, and months of life.4 The major changes is 25 mm (about I inch) per second. (If the speed is any slowtake place during the first year of life. Thereafter, changes are er or faster, this must be noted because it will change the relatively minor. The differences between a neonate’s EKG EKG pattern and alter measurements.) Time is measured on and the EKG of an older patient are caused by the unique hemodynamics of fetal and transitional circulation, by overall , the horizontal axis, reading left to right. Each small square equals 0.04 second, and each large square equals 0.2 second changes in physiology, by changes in the size and position of (Figure 2). In the top border of the EKG paper, every 7.5 cm the heart chambers relative to one another, and by changes in is marked by a heavy black vertical line. The distance between the size and position of the heart relative to the rest of the one line and the next equals 3 seconds (Figure 3).6 By meabody. It is especially important to understand these differsuring along the horizontal asis of the EKG paper, you can ences when evaluating a neonate’s EKG because most of the Accepted for publication April 199% Revised June 1998. NEONAT~~L VOL. 17, NO. 8, DECEMBER 1998 N E T W O R K 7 ~ FIGURE 1 m Comparison of neonatal 124ead EKG to adult 12-lead EKG. Not reproduced to scale. N E 0 N A T A L N E T 8’ 0 R Ii 8 DECEMREK 1998. VOL. I - . r\;O. 8 TABLE 1 n FIGURE 2 m Standard EKG paper. Findings of Premature Infant’s EKG Compared to EKG of Full-Term Infant Small squares measure 1 mm by 1 mm. Large squares measure 5 mm by 5 mm. Less right ventricular dominance (or more left ventricular dominance) than the full-term infant Lower voltages of the QRS complex and T wave in the standard leads Relatively shorter PR, QRS, and QT intervals than the fullterm infant More variability in the EKG overall Adapted from: Park MK, and Guntheroth WC. 1992. How to Read Pediutric ECGs, 3rd ed. St. Louis: Mosby-Year Book, 33-34. L 00.4 second of % I determine the duration of any part the cardiac cycle and the actual heart rate. Voltage (or nmplitztde) is measured on the vertical axis of the EKG paper. Voltage measures the height and depth of a cardiac impulse or its upward or downward deflection. It also measures the depression or elevation of baseline segments of the cardiac impulse.’ Each small square equals 1 mm of amplitude. Ten millimeters of amplitude (two large squares) equal 1 millivolt (mV) (Figure 2). With a single-lead rhythm strip, the voltage measurement is not as important as the time measurement. This is because the amplitude of the impulse is usually adjusted so that the impulses can be clearly visualized and measured. With a 12-lead EKG, the amplitude of deflections is used for diagnostic purposes. CARDIAC RHYTHM STRIP (LEAD II) V E R S U S 12-LEAD EKG Two categories of EKGs are commonly used in the care of neonates: single-lead cardiac rhythm strips and 12-lead EKGs. Both are important tools in the cardiac evaluation of the neonate and provide valuabIe information about the heart and conduction system. At the infant’s bedside, single-lead EKG rhythm strip provides one view (or angle) of cardiac activity. It can give general information about heart rate and identify deviations in normal cardiac rhythm instantaneously. The ability to accurately assess the single-lead rhythm strip for identification of possiFIGURE 3 n ble cardiac dysmnction is critical for the bedside nurse and is the focus of this article. There are limitations to the singIe-lead EKG rhythm strip, though, and it is imperative that the neonatal nurse be aware of these. As stated, the single-lead EKG rhythm strip provides only one view of cardiac activity. For a more complete view of the heart, a 12-lead EKG is required. A 12-lead EKG provides an examination of the entire heart because it assesses the heart from several different angles. Each of the leads presents a different pattern or a slightly different view of the same cardiac activity.’ This gives us a more complete picture of the electrical activity of the heart than is possible with a cardiac rhythm strip. Because of the difference between rhythm strips and a 12-lead EKG, rhythm strips (although invaluable as a screening tool for rate and rhythm) should not be used to diagnose cardiac conditions. A 12-lead EKG is necessary for accurate diagnosis of cardiac conditions. The 12-lead EKG is one important tool used in the complete cardiac evaluation of the newborn. The electrical record that it provides gives valuable information about the heart’s structure and its function.’ However, the 12-lead EKG does not provide a complete assessment of mechanical function. For example, it will not show how well the heart is contracting in an infant with acute pulmonary edema. Nor does it always directly depict structural abnormalities.8 . EKG paper showing black vertical markings above gridlines. The distance between two of these marks measures 7.5 cm and is equal to 3 seconds. N VOL. 17, NO. 8, DECElMBER 1 9 9 8 EONATAL N E T W O R K 9 FIGURE 4 n Cardiac depolarization and reoolarization. POLARIZED RESTING CELL DEPOLARIZING CELL DEPOLARIZED CELL REPOLARIZING CELL c + - lular ion, potassium, which exerts only a relatively weak positive charge inside the cell.’ This difference benveen the inner and outer cell membranes is actively maintained by a pump mechanism called the sodium-potassium pump. At some point, the sodium-potassium pump is no longer able to maintain the separation of charges between the cell membranes, and the process of depolarization and myocardial contraction occurs.7 In depolarization, the sodium and calcium ions enter the cell. The influx of sodium and calcium ions pushes the potassium ions out of the cell. This causes a reversal of the charges between the cell membranes. The outside of the cell is now negatively charged and the inside of the cell is positively charged, and the cardiac stimulation occurs in a wavelike fashion throughout the heart (Figure 4)’ Repolarization is an electrical phenomenon that occurs after stimulation, when the mvocytes regain their resting negatively charged interior (Figure 4).’ Repolarization must occur before depolarization can occur again. In repolarization, the sodium-potassium pump actively pumps the sodium and calcium ions out of the cell and the potassium ions into the cell to reestablish the electrical charge across the cell membrane.’ For individual mvocytes, depolarization and repolarization occur in the same direction. For the entire myocardium, depolarization occurs from the endocardium (innermost layer) to the epicardium (outermost layer), and repolarization occurs in the opposite direction.R D Depolarization and repolarization. The resting heart muscle cell, A, is polarized; that is, it carries an electrical charge, with the outside of the cell positively charged and the inside negatively charged. When the cell is stimulated (I), as in 6, it begins to depolarize (stippled area). The fully depolarized cell, C, is positively charged on the inside and negatively charged on the outside. Repolarization, D, occurs when the stimulated cell returns to the resting state. The direction of depolarization and repolarization is represented by orrows. Depolarization (stimulation) of the atria produces the P wave on the ECG, whereas depolarization of the ventricles produces the QRS complex. Repolarization of the ventricles produces the ST-T complex. From: Goldberger AL, and Coldberger E. 1994. Clinical flectrocardiogrophy, 5th ed. St. Louis: Mosby-Year Book, 8. Reprinted by permission. To be most effective, the 12-lead EKG must be used in conjunction with other tools for assessing structure and function. THE ELECTRICAL IMPULSE AND THE EKG The heart acts much like an electrical generator. Currents flowing from the heart travel within the entire body and create a cardiac electrical field that forms repetitive patterns. The basic EKG complex is a representation of these currents in the body.4 In general, an upward deflection of a wave on an EKG complex is called a positive deflection and a downaard deflection is called a nefiative deflection. ,4 deflection that is partly positive and partI!. negative is called hipbasic. A segment that is flat on the baseline is isoelectC8 There are three phases to the cardiac cycle. They are i 1) polarization, 12 ) depolarization, and (3) repolarization. During the polarization (or resting) phase of the cardiac qrcle, the heart’s mvocytes (muscle cells) have a negativel! charged interior and a positively charged exterior (Figure 4). This is due to the differential between the primary extracellular ions, sodium and calcium, i\Thich esert a strong positi1.e charge outside the cell, and the primary intracel- NEONATAL I (1 THE CARDIAC CYCLE One cardiac cycle consists of a P wave, followed by the QRS complex, followed by the T wave. These cardiac cycles occur successively on an EKG tracing. These waves and complexes also produce the PR interval, the QT interval (which are discussed later), and the ST segment (Figure 5).6 Evaluating and measuring the various components of the cardiac qcle in a systematic fashion vield, information about the heart rate, the regularity of the heartbeat, and the general state of the conduction system. The ceils in the cardiac conduction system differ from the other cells in the heart in that the! can depolarize spontaneously. This abilitv is called azrtornaticiq. In the health!. heart, the cells of the atria and ventricles \vill not depolarize spontaneousl!y thev will an.ait a stimulus from the sinoatrial (SA) node.9 The S_i node, located NETWORK DECFh4HF.K 1998. \ OL. I - . Ii<). 8 FIGURE 5 n FIGURE 6 intervals and segments of the cardiac cycle. l Diagram of heart conduction system. SA node AV node Bundle of His Left bundle branch Right bundle branch Purkinje Fibers Adapted from: Park MK. 1996. Pediatric Curdiology for Practitioners, 3rd ed. St. Louis: Mosby-Year Book, 41. Reprinted by permission. From: Park MK, and Cuntheroth WC. 1992. How to Read Pediatric KCs, 3rd ed. St. Louis: Mosby-Year Book, 1. Reprinted by permission. in the posterior wall of the right atrium, is the normal heart’s dominant pacemaker (Figure 6). It generally initiates the impulse wave ofdepolarization. This wave proceeds outward from the SA node, and both atria are stimulated to contract.’ The normal P wave of the cardiac impulse represents the depokuization and contraction of the atria (Figure 5). The first half of the P wave represents depolarization of the right atrium, and the second half represents depolarization of the left atrium. When atriai depolarization is stimulated by other pacemakers, the shape and direction of the P wave will be altered.2 Following depolarization of the atria, the cardiac impulse travels to the atrioventricular (AV) node (Figure 6). The AV node is located in the lower part of the right atrium very close to the interatrial septum.’ The AV node is the only pathway that allows the cardiac impulse to travel from the atria to the ventricles through the fibrous AV valves (mitral and tricuspid).’ The AV node also serves as a backup pacemaker if SA node firing or atria1 depolarization should fail to 0ccur.l The stimulus of depolarization is delayed slightly through the AV node as blood flows through the AV valves into the ventricles. Once the impulse has reached the ventricular conduction system, it proceeds very rapidly through the His-Purkinje system. This system consists of the bundle of His, the right and left bundle branches, their terminal ramifications, and the Purkinje fibers (Figure 6).9 The bundle of His is located in the top left corner of the right ventricle and at the top of the interventricular septum.’ It carries the cardiac impulse horn the AV junction to the lower conduction system of the ventricles. The VOL. right and left bundle branches are the major bifurcations of the bundle of His. These branches subdivide further to become the Purkinje fibers. These fibers carry the cardiac impulse to the myoqites of the ventricles via their terminal filaments.’ Right and left ventricular depoiarizadon occur virtually simultaneously.2 Any part of the ventricles, as well as the Purkinje fibers, may serve as a backup pacemaker should the higher pacemakers fail to function. Ventricular or Purkinje pacemaker sites tend to be less regular, slower, and more unreIiabIe than higher pacemaker sites, however.’ The depolarization of the ventricles is represented as the QRS complex on the EKG (Figure 5). The first downward deflection of the QRS complex is called the Q wave. It is produced primarily by depolarization of the ventricular septum.6 On a 12-lead EKG, the presence or absence of Q waves in certain leads can be abnormal. Thus, for example, the absence of Q waves in V6 may indicate L-transposition of the great arteries (congenitally corrected transposition), single ventricle, mirror image dextrocardia, or left bundle branch block. The presence of Q waves in V, may indicate severe right ventricular hypertrophy, L-transposition of the great arteries, or single ventricle; it may occasionally be normal in newborns.6 The first upward deflection of the QRS complex is cahed the R wave. Following any upward deflection of the QRS complex, the next downward deflection is called the S wave.’ Ventricular repolarization is represented on the basic EKG complex as the ST segment and . N EONATAL N ETWORK 17, NO. 8, DECElMBER 1 9 9 8 11 I FIGURE 7 n Quick method for determining heart rate (1). Use the first R wave that falls on a heavy black line as a starting point. The line that the next R wave falls on determines the rate. FIGURE 9 H Quick method for determining heart rate (3). Count the number of RR cycles in six large squares (I .2 seconds) and multiply by 50. In this example, there are 3 R-R cycles. Therefore, the heart rate is 3 x 50 = 150 bpm (enlarged in size). . Six large squares = 1.2 seconds I . _ __.. : 1 _ 2 From: Dubin D. 1996. Ropid lnterpretotion of EKG, 8th ed. Tampa, Florida: Cover, 77. Reprinted by permission. the T wave. The ST segment, which occurs after the QRS and just before the T wave (Figure 5), is usually referred to as the plateau phase of ventricular repolarizatiom8 The normal ST segment is flat and level with the basic EKG complex. Elevation or depression of this segment can be pathologically significant (see “Examining the ST Segment” later in this article). The T wave represents that period of time when the repolarization of the ventricles is occurring rapidly and efficiently.s Occasionall!; a U wave may be present on a normal basic EKG complex tracing. The U Leave should folio\\; and be in the same direction as, the T uvave. Its mechanism is not k n o w n , b u t i t may b e c o m e t a l l e r i n h!Fokalemia.9 EVALUATING THE HEART RATE There are several quick and easy methods for determining the heart rate using the single-lead rhythm strip or a 12-lead ERG. In the first method, the first R \vave that falls directly on a FIGURE 8 m Quick method for determining heart rate (2). Count the number of RR cycles between hhro vertical marks and multiply by 20. In this example, there are 6 RR cycles between two vertical marks. Therefore, the heart rate is 6 x 20= 120 bpm. 4 ...... 5 _ 6 I : j . . .: .._ .: 3 __.. .j ., ,_. heavy black line is used as a starting point. The subsequent hea\? black lines are numbered 300, 150, 100, and 75, respectivellr. The line that the next R wave falls upon determines-the approximate rate (Figure 7).7 A second method for determining the heart rate uses the vertical marks in the upper border of the single-lead EKG rhythm strip paper. Because the distance between bvo of these marks equals three seconds, the heart rate can be calculated by counting the number of RR c!~cles between two vertical marks and multiplying by 20 (Figure S).h A third method for determining the heart rate is counting the number of RR c\lcles in six large squares (1.2 seconds) and multiplying this figure by 50 (Figure 9).6 The normal range for neonatal heart rate is 80 to 160 beats per minute (bpm), although some healthy term neonates n-ill ha\-e a heart rate as low as 70 bpm when in deep sleep. Neonates cannot tolerate a heart rate consistently higher than 200 bpm for an extended period of time. This condition, which is called s?~~p~nnenb-icula; tacl~cardia, represents a medical emergency and requires immediate ilitervention.‘” E\‘ALI’ATING THE CARDIAC CYCLE Once the heart rate has been determined b! the single-lead EKG rhythm strip or the l2-lead EKG, several other areas on the EKG rh!rthm strip can be used to help evaluate the cardiac cycle. Definiti\re diagnosis should be made onI>. from a 12.lead EKG, but the rhythm strip can used to idcntic potential problems requiring more definitive e\.aluation. Components of the . rhythm strip that should be examined systematically are the basic cardiac rhythm; the presence or absence of the P wave and basic P wave configuration; the PR, QRS, and QT intervals; the ST segment; and the T wave configuration. I address each of these areas separately. QRS amplitude, QRS axis, T axis, and QRS-T angle are routinely evaluated on a 12-lead EKG, but these factors cannot be evaluated on a basic rhythm strip. Cardiac monitors used in neonatal nurseries generally offer a choice of leads I, II, and III. Lead II is the one that reads from the right arm to the left foot, assuming that the leads have been placed correctly. Lead II is closest to the normal heart’s vector following the pattern of normal conduction. This is because the SA node is near the top righthand comer the heart and the direction of impulse is from the right shoulder toward the left leg. For this reason, lead II is generally thought to be the most appropriate lead for standard monitoring. 1 1 of Examining the Cardiac Rhythm Rhythm refers to the regularity of the EKG pattern. Is the pattern consistent or inconsistent? The P-to-P intervals and the R-to-R intervals should be the same over a six-second period. If the intervals are inconsistent, the pattern is irregular.’ Sinus rhythm is the normal cardiac rhythm at any given age.t2 In sinus rhythm, there is only one P wave, which occurs consistently before each QRS complex. The QRS complex is consistently followed by a T wave (Figure 10). The pattern should repeat itself at regular intervals. This is because the SA node generates impulses at a generally constant rate within physiologic limits.7 A discussion of irregular cardiac rhythm patterns is beyond the scope of this article. In general, there are irregular rhythms, escape rhythms, premature beats, tachyarrhythmias, and heart blocks7 Examining the P Wave Configuration The P wave, which represents depolarization of the atria, should be upright (positive) in lead II. The P wave should be rounded and consistent in shape and direction within each cardiac cycle (Figure S). l A P wave that looks like a steeple can indicate right atrial enlargement; a P wave that is broad and notched can indicate left atria1 enlargement.” The maximum duration of N VOL. 17, NO. 8, D E C E M B E R 1 9 9 8 FIGURE 10 n Example of sinus rhythm. Note the P wave, which occurs consistently oefore each QRS complex. The QRS is consistently followed by a T wave. The pattern repeats itself at regular intervals. the P Wave in infants less than 12 months of age is 0.08 seconds. A prolonged P wave is an indication of let? atrial hypertrophv.h Examining the PR Interval The PR interval represents the time necessary for atria1 depolarization and the delay of the impulse at the AV node.6 The PR interval starts at the beginning of the P wave and extends to the beginning of the QRS comples (Figure 5).l The PR interval varies with heart rate and age; Table 2 gives normal values for neonates. A prolonged PR interval (first-degree AV block) indicates an abnormally long delay in the conduction of the impulse through the AV node. It may be seen in myocarditis, atriai septal defect, endocardial cushion defect, Ebstein’s anomaly, digitalis toxicity, hyperkalemia, ischemia, or profound hypoxia; it may also be seen in an otherwise normal heart.6 A shortened PR interval indicates that an abnormal accessory conduction pathway is being used to excite the ventricles3 This may be seen with Wolff-Parkinson-White (WPW) syndrome or in a normal heart with a low right atria1 pacemaker.5 Variable PR intervals . TABLE 2 I Normal Values for Neonates for PR Interval and QRS Duration Age Group Less than 1 day 1 to 2 days 3 to 6 days 1 to 3 weeks 1 to 2 months PR interval (seconds) 0.08-O. 16 C-1’) 0.08-0.14 C.77) 0.07-0.14 Cl 0) 0.07-0.14 Cl 0) 0.07-O. 13 Cl 0) QRS Duration Vl 0.03-0.07 CO% 0.03-0.07 CO51 0.03-0.07 CO% 0.03-0.08 CO51 0.03-0.08 CO% Adapted from: Carson A. 1998. Electrocardiography. In The Science and Practice of Pediatric Cardiol~, 2nd ed., Carson A, et al., eds. Baltimore: Williams & Wilkins, 736. Reprinted by permission. EONATAL N E T W O R K 13 IFIGURE 11 n Wenckebach phenomenon. _ _ __.__._; ._ .- ._- _-.--;.-.--.. / ._..~.__~.~_ __._ ___._.; . _ __ ._L...,. ._ -___. _ _. _ . . . . _ __.__._ _ . . .._....__.__._...... _ _..-. ./ . . b are seen with the irregular rhythms of wandering atrial pacemaker and Wenckebach phenomenon (Figure 11).6 Examining QRS Duration The QBS duration represents the amount of time necessary for ventricular depolarization to take place.6 It is measured from the beginning to the end of ventricular depolarization and should be measured in a lead with a Q wave (Figure 5). QRS duration will increase with age.5 Table 2 gives normal values for neonates. The initial EKG of a premature infant will have a shorter QRS duration than the initial EKG of a term infant.2 Most ventricular conduction disturbances result in prolonged QRS duration. These disturbances include right and left bundle branch blocks, WI%’ syndrome, hyperkalemia, premature ventricular contractions, dysfunction of the myocardium related to metabolic or ischemic problems, ventricular tachycardia, and implanted ventricular pacemaker.‘” Examining the QT Interval The QT interval starts at the onset of the QRS complex and ends at the termination of the T wave (Figure 5). It measures the amount of time required for both ventricular depolarization (QRS duration) and ventricular repolarization to take place. When measuring the QT interval, use the longest interval in any lead.” The QT interval varies with the heart rate, and this must be corrected for using Bazett’s formula, lvhich nil1 vield a corrected QT (QTc) interval: QTc interval = QT JXCZZ A QTc interval of greater than 0.44 seconds is considered abnormal at most ages, but some newborns may have a normal QTc of 0.47 seconds.5 A prolonged QT interval may be seen in hypocalcemia, viral myocarditis, head injury, or cerebrovascular accident.6 QT prolongation ma) also indicate the therapeutic effect of an antiarrhythmic drug such as procainamide.2 A shortened QT interval may be seen in hypercalcemia and digitalis effect.12 Examining the ST Segment The ST segment is the portion of the EKG between the termination of the S wave (after ventricular depolarization) and the beginning of the T wave (before ventricular repolarization) (F&m-e 5).s The ST segment should be isoelectric, although it may be depressed or elevated on a 12-lead EKG up to 1 mm in infants in the limb leads and up to 2 mm in the left precordial leads. Abnormal shift of the ST segment will occur in pericarditis, severe ventricular hypertrophv with strain (abnormal ventricular repolarization), digitalis effect, myocardial ischemia and infarction, hyperkalemia or hypokalemia, and intracranial injur!.,x+12 T wrave changes are often associated with ST segment shifts.12 Examining the T Wave The T wave represents ventricular repolarizanon. It should have a smooth, curved form, but it . r FIGURE 12 R EKG findinqs FIGURE 13 n S-T segment in hypercalcemia and hypocaicemia. of hypokalemia and hyperkalemia. SERUM K Depressed ST Segment (2.5 mEq/L Hypercalcemia Normal Hypocalcemia Normal From: Park MK, and Cuntheroth WC. 1992. How to Reod Pediatric EC&, > 6.0 mEq/L & >9.0 mEq/L Absent P Wave Sinusoidal Wave From: Park MK, and Cuntheroth WC. 1992. How to Read Pediatric ECGs, 3rd ed. St. Louis: Mosby-Year Book, 108. Reprinted by permission. may be notched or slightly asymmetric (Figure 5). The amplitude of the T wave varies widely with many physiologic processes. On a 12-lead EKG, in ‘any infant over 48 hours of age, it should be greater than 2 mm in leads I, II, and V6.s Tall, peaked T waves may be seen in hyperkalemia, lef‘t ventricular hypertrophy, cerebrovascular accident, and posterior myocardial infarction. Flat or low T waves may be seen in normal newborns. They may also be seen in hypokalemia, hypothyroidism, hyper- or hypoglycemia, pericarditis, myocarditis, myocardial ischemia, shock, anemia, and digitalis effect.6 EXAMINING THE EKG FOR ELECTROLYTE EFFECTS IN NEONATES Various electrolyte imbalances will affect the cardiac impulse. The most common electrolyte imbalances that cause EKG changes are hypo- and hyperkalemia and hypo- and hypercalcemia. Hypokalemia will produce the least specific EKG changes. When the serum potassium level falls below 2.5 milliequivalents (mEq)/liter, a prominent U wave may be present. In addition, there may be prolongation of the QTc interval, flat or biphasic T waves, and ST segment depression (Figure 12).12 Arrhythmias are not usuallv seen with hypokalemia unless the infant is receiving digitalis, in which case tachycardia arrhythmias are the most comrnon.5 Hypokalemia may be seen, for esample, in a neonate with congestive heart failure on chronic diuretics. With hyperkalemia, the potassium IeveI is easily predicted by the EKG (Figure 12).5 With levels greater than 6 mEq/liter, tall, peaked T waves will become apparent. At Ievels greater than 7.5 mEq/liter, the PR interval will become N VOL. 17. NO. 8, DECEiMBER 1 9 9 8 3rd ed. St. Louis: Mosby-Year Book, 107. Reprinted by permission. Tall T Wave EONATAL prolonged, the QRS duration will lengthen, and the T waves will be peaked. At levels greater than 9 mEq/liter, the P waves will disappear and wide, bizarre QRS complexes will be present. Eventually, ventricular fibrillation or asystole will occur.6’12 Hvperkalemia mav be seen in an extremely dehydrated 24-week gestational infant in the first few days of life. Hypocalcemia will cause prolongation of the ST segment, and this will lengthen the QT interval (Figure 13).s The T wave is delayed, but not widened.8 Hypocalcemia may be seen in an alkalotic intant being hyperventilated for persistent pulmonary hypertension of the newborn. Hypercalcemia will shorten the ST segment, and this will shorten the QT interval (Figure 13). Hypercalcemia mav also slow the sinus rate or cause SA block or sinus arrest. Digitalisinduced arrhythmias may be potentiated by hypercalcemia.” Hypercalcemia may be seen in the neonate with rapid infusion of calcium gluconate. EXAMINING THE EKG FOR DIGITALIS EFFECTS AND TOXICITY Digitalis toxicity in the neonate is more readily detected by monitoring the EKG than by evaluating serum digoxin levels, especially in the first three to five days after digitalization. A baseline EKG should be obtained before loading with digitalis. In addition, a rhythm strip should be assessed before starting maintenance digitalis and at regular intervals for three to five days thereafter. A pharmacokinetic steady state should be achieved within three to five days. In general, digitalis effects will be confined to ventricular repolarizanon, and digitalis toxicity will cause disturbances in the formation and conduction of the impulse.‘z The earliest sign of digitalis effect is shortening of the QTc. Sagging of the ST segment, diminished T wave amplitude, and slowing of the heart rate may then follow. ProIongation of the PR interval (which could progress to second-degree AV block) is a very reliable sign of early digitalis toxicity. Profound sinus bradycardia or SA block and supraventricular arrhythmias are also signs of digitalis toxicity.13 Although isolated premature ventricular contractions may be seen with digitalis toxicity in the neonate, ventricular bigeminy or trigeminy is uncommon.12 N E T W O R K 15 . I FIGURE 14 m Example of artifact. This EKG demonstrates a wandering baseline caused by movement. ARTIFACT A@?act is defined as anv type of activity on the EKG that is noncardiac in origin. It can be caused by loose elecnodes, broken wires, hiccups, muscle tremors, patient movements, or elecuical interference.’ Artifact can appear on the EKG as a wandering or jagged baseline, as spikes in the cardiac cycle, as a masking of the entire cycle, or as a flat line if the electrodes have become loose (Figure 14). Knowing how to identi+ and correct art&act can be challenging. This is an important skill for the neonatal bedside nurse. CONCLUSIONS The EKG rhythm strip can provide valuable information about the general status of the neonatal heart and conduction system. NeonataI nurses who are familiar with the normal cardiac impulse and the factors affecting it are better able to use the EKG as a screening tool for identifying possible cardiac dysfunction, electrolyte imbalance, and drug effects in their patients. Understanding EKG basics, and the usefulness and limitations of the EKG, is essential in the care of neonates. ;z REFEREKCES Catalan0 JT. 1993. Guide to ECG Ana&i?ris. Philadelphia: JB Lippincort, l-47. Benson DW, and Duf$ CE. 1990. Electrocardiography. In Fetal and hieonatal Cnrdiolog?: Long W, ed. Philadelphia: WB Saunders, 236-248. Stromberg D. 1996. Electrocardiography In Pediatric nnd Neonatal Tests ami Procedures, Taeusch my, Christiansen RO, and Buescher ES, eds. Philadelphia: WB Saunders, 207-23 1. Liebman J, and Rudy Y. 1990. Electrocardiography. In Fetal, ,Xco~iamI. aud Ir!fnut Cardiac Disease, hioiler JH, and Seal K.-i, eds. Norwalk, Connecticut: Appleton & Lange, 179-238. Garson _I. 199s. Electrocardiograph!.. In T h e Sciemc ami APnice of Pediatric Cardiohgy, 2nd ed., Garson A, et al., eds. Baltimore: W’illiams & Wilkins, 735-783. 6. Park MK, and Guntheroth WG. 1992. How to Read Pediatric ECGs, 3rd ed. St. Louis: MosbyYear Book, l-130. 7. Dubin D. 1996. Rapid Interpretation of EKG’s, 8th ed. Tampa, Florida: Cover, 1-189. 8. Goldberger AL, and Goldberger E. 1994. Clinicai Electrocardiography, 5th cd. St. Louis: Mosbp-Year Book, 7-20. 9. Conover MB. 1992. Understanding Electrocaudiograpby, 6th ed. St. Louis: Mosby-Year Book, 1-51. 10. Vargo L. 1996. Cardiovascular assessment of the newborn. In Physical Assessment of the Newborn, 2nd ed., Tapper0 EP, and Honeyfield ME, eds. Petaluma, California: NICU Lw 77-91. 11. Woodrow l? 1998. An introduction to the reading of electrocardiograms. British Journal o f Nursing 7( 3): 135-142. 12. Park MK. 1997. The Pediatric Cardiology Handbook, 2nd ed. St. Louis: Mosby-Year Book, 25-58. 13. Park MK. 1996. Pediatric Cardiologgl for Practitioners, 3rd ed. St. Louis: Mosby-Year Book, 34-5 1. About the Author Lyn Va,;go is a neonatal muse practitioner in the NICU at St. John’s Mercy Medical Center in St. Louis, Missouri, and has worked in neonatal nursivg for the past 20 ?ears. She was co-coordiuator of the neonatal nurse practitioner program at St. John’s Mercy Medical Center porn 1989 to 1997. She zs presentIy a regional faculty member of the neonatal nurse pspctitionw program at the State liniversity of ,Xew York-Stan? Brook. She obtained her BSN and her MSA’ fT*om St. Louis Linirersir?; St. Louis. She is presentrjl~ working on her PhD i?i nursiq at l?nivcrsi~ of Missouri, St. Louis. She is a Ynevuber of NANN For further information, please contact: Lyn Vargo, RNC, MSN, SSP St. John’s Merq hlcdical Center Department of Seonatolo,? 621 South New Ballas 2009-B St. Louis, lM0 63141 [email protected] N~0y~T.41 XETWORK 16 DECEhlBER 1 9 9 8 , \‘OL. 17, N O . 8
© Copyright 2026