Black oesophagus Meng-Chiung Lin , Heng-Cheng Chu
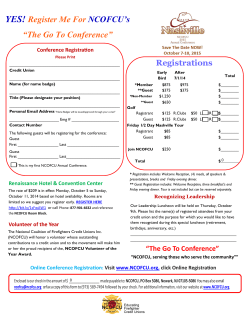
QJM Advance Access published May 13, 2015 Black oesophagus Meng-Chiung Lin1,2, Heng-Cheng Chu 1, Peng-Jen Chen 1 1 Division of Gastroenterology, Department of Internal Medicine , Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan 2 Department of Internal Medicine, Taichiung Armed Forces General Hospital, Taichiung, Taiwan Corresponding author: Peng-Jen Chen Tel.: +886 2 87923311#12983; Fax: +886 2 87927248; E-mail: [email protected] There are no potential conflicts of interest, including full disclosure of any financial arrangements between any authors. The authors transfer all copyright ownership of the above manuscript to in the event the work is published. © The Author 2015. Published by Oxford University Press on behalf of the Association of Physicians. All rights reserved. For Permissions, please email: [email protected] Downloaded from by guest on July 7, 2015 Division of Gastroenterology, Department of Internal Medicine, Tri-Service General Hospital, National Defense Medical Center, N 325, sec 2, Cheng-Gong Rd, Neihu 114, Taipei, Taiwan A 70-year old male with medical history of hypertensive cardiovascular disease , diabetes mellitus (DM) with chronic renal insufficiency, atrial fibrillation (Af), sick sinus syndrome (SSS), and adenocarcinoma of prostate, presented with a 2-day history of melena, and hematemesis. On examination, he was afebrile and hemodynamically stable. Excepts for slight tachycardia (HR:110 beats/min) and epigastric tendereness, no other abnormalities were noted. Laboratory analysis revealed hemoglobin of 14.5 g/dL, and creatinine of 1.7mg/dL, respectively. The fecal occult blood test is positive. Esophagogastroduodenoscopy (EGD) revealed diffuse as well as sharp demarcation at the gastroesophageal (GE) junction, which were suggestive of acute necrotizing esophagus (Fig. 1a). However, tissue sampling was not performed due to multiple comorbidity and potential perforation. After combination treatment with oral sucralfate and proton-pump inhibitor (PPI) for two weeks, a follow-up EGD showed complete resolution of previous black mucosa (Fig. 1b). Acute esophageal necrosis (AEN), also known as “black oesophagus” or “acute necrotizing esophagitis ”, is a rare clinical scenario with hemorrhagic manifestations mostly1. The exact pathophysiology of AEN still remain unclear. However, it is believed to be multifactorial. It is generally seen in individual with Downloaded from by guest on July 7, 2015 black pigmentation with extensive ulcerative mucosa in the mid-to-distal esophagus ischemia-associated phenomena, such as unstable hemodynamic compromise , back flow injury due to transient gastric outlet obstruction, and cardiovascular event, and excessive alcohol abuse2. Generally, risk factors of ANE are male, the elderly, poor general conditions (including malnutrition, multiple comorbidity), excessive alcohol abuse and immunocompromised state3. Opportunistic cytomegalovirus and herpes simplex virus infections were also reported to be the possible etiologies4,5 Clinical history of caustic ingestion or previous foreign body associated injury should be first taken and excluded. Other diagnostic considerations to exclude include Except for intravenous PPI, no standardized treatment therapy is recommended for treating AEN. Removal of the identified etiology, maintain perfusion and supportive care are best strategies. Surgery is only preserved for those with severe complications. As Ben Soussan E reported in a prospective 1-year study, the mortality rate of AEN is 50%(4/8). However, all the mortality cases were attributed to coexist illness instead of the disease itself.6 In conclusion, we present a case of AEN. Our patient’s gender, advanced age, habit of alcohol abuse, and debilitating medical conditions (HCVD, diabetes, Af, maligancy) fit well with risks factors of AEN. Now, he remains symptom free and recovery from endoscopy. Downloaded from by guest on July 7, 2015 acanthosis nigricans, pseudomelanosis, melanosis and malignant melanoma. Reference 1. Reichart M, Busch OR, Bruno MJ, Van Lanschot JJ. Black esophagus: a view in the dark. Dis Esophagus 2000;13:311-313. 2. Endo T, Sakamoto J, Sato K, et al. Acute esophageal necrosis caused by alcohol abuse. World J Gastroenterol. 2005;11(35):5568–70. 3. Grigoriy E. Gurvits, Alexander Shapsis, Nancy Lau, Nicholas Gualtieri, and James G. Robilotti. Acute esophageal necrosis: a rare syndrome. J Gastroenterol 2007; 42:29–38. esophagus associated with herpes esophagitis. Gastrointest Endosc 1999; 49: 105-7. 5. Barjas E, Pires S, Lopes J, Valente A, Oliveira E, Palma R Cytomegalovirus acute necrotizing esophagitis. Endoscopy. 2001 Aug;33(8):735. 6. Ben Soussan E, Savoye G, Hochain P, Hervé S, Antonietti M, Lemoine F, et al. Acute esophageal necrosis: a 1-year prospective study. Gastrointest Endosc 2002; 56: 213-217. Downloaded from by guest on July 7, 2015 4. Cattan P, Cuillerier E, Cellier C, Carnot F, Landi B, Dusolel A, et al. Black Figure 1. Endoscopic views of esophageal findings. (a, b), a) AEN is characterized by a circumferential & black-brownish appearing of the esophageal mucosa with abrupt ending at the GE junction, b) recovery of AEN with healing ulceration in distal esophagus. Downloaded from by guest on July 7, 2015 Downloaded from by guest on July 7, 2015 71x49mm (300 x 300 DPI) Downloaded from by guest on July 7, 2015 70x49mm (300 x 300 DPI)
© Copyright 2026