Healthy Eating During Pregnancy Specific nutrient requirements Nutritional requirements during pregnancy
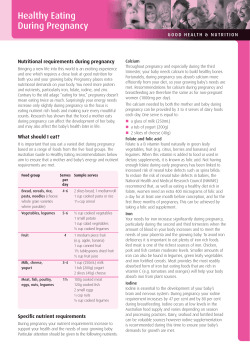
Healthy Eating During Pregnancy G O O D H E A LT H & N U T R I T I O N Nutritional requirements during pregnancy Specific nutrient requirements Bringing a new life into this world is an exciting experience, and one which requires a close look at good nutrition for both the mother and her growing baby. Pregnancy places greater nutritional demands on your body. You need more energy, protein and nutrients, particularly iron and folate. Research has shown that the food a mother eats during pregnancy can affect the development of her baby, and may also affect the baby’s health later in life. Calcium Throughout pregnancy and especially during the third trimester, your baby needs enough calcium to build healthy bones. Fortunately, during pregnancy you absorb calcium more efficiently from your diet, so your growing baby’s needs are met. Recommendations for calcium during pregnancy and breastfeeding are therefore the same as for non-pregnant women (1000mg per day). What do I eat? It is important that you eat a varied diet during pregnancy based on a range of foods from the five food groups. The Australian Guide to Healthy Eating recommendations below aim to ensure that a mother and baby’s energy and nutrient requirements are met. Food group Serves Sample serves per day Bread, cereals, rice, 4-6 pasta, noodles (choose whole grain varieties where possible) 2 slices bread, 1 medium roll 1 cup cooked pasta or rice 11/3 cup cereal Vegetables, legumes 5-6 ½ cup cooked vegetables 1 small potato 1 cup salad vegetables ½ cup cooked legumes Fruit 4 1 medium piece fruit (e.g. apple, banana) 1 cup canned fruit 1½ tablespoons dried fruit ½ cup fruit juice Milk, cheese, 3-4 yogurt 1 cup (250mL) milk 1 tub (200g) yogurt 2 slices (40g) cheese Meat, fish, poultry, 1 eggs, nuts, legumes 100g cooked meat 120g cooked fish 2 small eggs 1/3 cup nuts ½ cup cooked legumes The calcium needed by both the mother and baby during pregnancy can be provided by 3 to 4 serves of dairy foods each day. One serve is equal to: a glass of milk (250mL) a tub of yogurt (200g) 2 slices of cheese (40g) Iron You need much more iron during pregnancy, particularly during the second and third trimesters when the amount of blood in your body increases, and to meet the needs of your placenta and the growing baby. To avoid iron deficiency during pregnancy it is therefore important to eat plenty of iron rich foods. Red meat is one of the richest sources of iron. Chicken and pork contain moderate levels. Smaller amounts of iron can also be found in legumes, green leafy vegetables and iron fortified cereals. Meat provides the most readily absorbed form of iron but eating foods that are rich in vitamin C (e.g. tomatoes and oranges) will help your body absorb iron from plant sources. Folate and folic acid Folate is a B vitamin found naturally in green leafy vegetables, fruit (e.g. citrus, berries and bananas) and legumes. When this vitamin is added to food or used in dietary supplements, it is known as folic acid. Not having enough folate during early pregnancy has been linked to neural tube defects such as spina bifida. To reduce the risk of neural tube defects in babies, the National Health and Medical Research Council (NHMRC) recommend that, as well as eating a healthy diet rich in folate, women should take an extra 400 micrograms of folic acid a day for at least one month before conception, and for the first three months of pregnancy. This can be done by taking a folic acid supplement. Protein More protein is needed during pregnancy to support your baby’s growth and changes in your own body such as increased breast tissue. In general, a healthy balanced diet will provide enough protein to meet your needs during pregnancy. Healthy Eating During Pregnancy Nutrition issues for pregnant women Listeriosis Listeriosis is an illness caused by a bacteria type called Listeria. Listeriosis usually results from eating food contaminated with Listeria bacteria. It can be a serious illness for pregnant women, possibly causing miscarriage, premature birth or, in rare cases, stillbirth. The following guidelines from Food Standards Australia New Zealand (FSANZ) can help reduce your risk of listeriosis: Eat freshly cooked or freshly prepared foods; Avoid foods that are past their ‘best before’ or ‘use by’ date; Cook foods thoroughly (heating food kills Listeria); Reheat foods to steaming hot (eat refrigerated left-overs within a day); Avoid ready-to-eat food from salad bars, sandwich bars, delicatessens and smorgasbords; Only buy ready-to-eat hot food if it is steaming hot; and If eating out, order hot meals. Some foods are more easily contaminated by Listeria than others. Avoid the higher risk foods during pregnancy: Cold meats (ready-to-eat delicatessen meat); Raw or smoked seafood, ready-to-eat peeled prawns; Cold cooked chicken; Pâté; Pre-prepared or pre-packaged salads (fruit and vegetable) such as from salad bars; Soft, semi-soft and surface ripened cheeses (e.g. brie, camembert, ricotta, feta and blue cheese); Soft serve ice cream; and Unpasteurised dairy foods (N.B. almost all dairy foods produced in Australia must be pasteurised). If you are pregnant, make sure you have at least 3 serves of dairy foods a day so that you get enough calcium and other essential nutrients found in dairy. The following dairy foods are safe to consume: Fish Fish is a valuable source of nutrients, especially omega-3 oils. While the Dietary Guidelines for Australian Adults recommend eating fish for good health, some fish can contain high amounts of mercury, which could be harmful for the developing baby if a lot is eaten. FSANZ recommends that pregnant women should only eat: One serve (150g) per fortnight of shark (flake) or billfish (swordfish/broadbill and marlin) with no other fish to be eaten during that fortnight; or No more than one serve per week of orange roughy (deep sea perch) and catfish, with no other fish to be consumed during that week. Further information on mercury in fish can be found on the FSANZ website (www.foodstandards.gov.au). Alcohol and caffeine Drinking alcohol during pregnancy can harm your unborn baby and cause foetal alcohol syndrome. Unfortunately, there is very little research data about how much alcohol is safe to drink during pregnancy. The National Health and Medical Research Centre therefore recommended that alcohol be completely avoided during pregnancy. Similarly, studies have not clearly indicated a safe level of caffeine consumption during pregnancy. NSW Health recommends that pregnant women limit themselves to 200mg of caffeine daily. That is 2 cups of ground coffee or 2½ cups instant coffee, 4 cups medium-strength tea, 4 cups cocoa/hot chocolate or 6 cups of cola. Have a healthy pregnancy! Choosing a safe and healthy diet during pregnancy helps you and your baby. A varied diet with plenty of fruit and vegetables and 3 serves of dairy foods every day can help provide many of the essential nutrients needed at this special time of life. Pasteurised dairy products such as milk and yogurt; Hard cheeses such as cheddar or tasty cheese - store it in the fridge; Processed cheese, cheese spreads, plain cream cheese, plain cottage cheese (only purchase cheeses packaged by the manufacturer, and store them in the fridge); and Packaged frozen ice cream. Further information on Listeria and food can be found on the FSANZ website (www.foodstandards.gov.au). The information provided in this document is to be used as general health and nutrition education information only. All material is published with due care and attention, and in good faith. No responsibility can be accepted for omissions, typographical or printing errors, or situation changes that have taken place after publication. For further information on any of our resources, visit www.dairyaustralia.com.au/nutrition or call our consumer line on 1800 817 736. This brochure may be photocopied for non-profit or non-commercial applications. Dairy Australia ABN 60 105 227 987 Level 5, IBM Tower, 60 City Road, Southbank Victoria 3006 Australia ©Dairy Australia December 2008. DA0440
© Copyright 2026