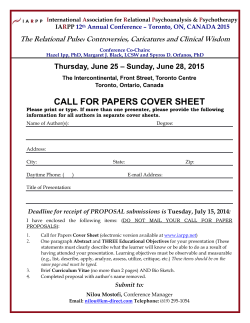
CHARTING NEW GROUND: - Speech
CHARTING NEW GROUND: Interprofessional approaches to dysphagia management TORONTO, ON October 4-6, 2015 Toronto Airport Marriott Hotel | 901 Dixon Road PROGRAM The Canadian Association of Occupational Therapists (CAOT), Dietitians of Canada (DC) and Speech-Language and Audiology Canada (SAC) are pleased to offer this interprofessional workshop intended for experienced clinicians seeking to advance their knowledge and skills in dysphagia assessment and management. The workshop will delve into areas of practice that may take you out of your comfort zone, challenge your assumptions and help you realize the power and benefits of interprofessional practice. The workshop has been specifically designed to engage clinicians from different disciplines so that we may all learn more about the areas of expertise and skills our colleagues bring to the table when discussing challenging cases. If you are interested in honing your clinical skills and taking your team contributions to the next level, this workshop is for you. LEARNING OBJECTIVES 2 At the conclusion of the workshop, participants will be able to: Identify the impact of dysphagia on the individual and family. Identify hydration, food texture and nutrient density concerns of texture-modified diets. Articulate the importance and effectiveness of the interprofessional team on client outcomes and quality of life. Recognize the interrelationships between respiration, positioning and eating. Explain the unique skills each clinician brings to the team. Describe a clear ethical framework to help guide decision making when ethical challenges arise in dysphagia management. Describe various approaches to assessment for swallowing disorders and the appropriate use of those approaches in different settings and for different populations. An additional objective of this program is to diversify and strengthen the professional network of skilled clinicians from across the country. Describe the current evidence for use of adaptive and compensatory strategies in dysphagia management. A certificate of completion will be provided at the conclusion of the workshop. PROGRAM AT A GLANCE 6:00 p.m. – 8:30 p.m. SUNDAY, OCTOBER 4, 2015 MONDAY, OCTOBER 5, 2015 Welcome and opening remarks Dinner The client’s lived experience 8:00 a.m. Breakfast 9:00 a.m. What is interprofessional dysphagia practice and why should we care? 10:30 a.m. Break 10:50 a.m. Case-based discussions 12:30 p.m. Lunch and sponsor showcase TUESDAY, OCTOBER 6, 2015 1:30 p.m. Interactive breakout sessions (2 x 45-minute sessions) 3:15 p.m. Break 3:35 p.m. Continuation of interactive breakout sessions (1 x 45-minute session) 4:20 p.m. Another brick in the wall – What have we learned? 4:45 p.m. Concluding remarks 7:30 a.m. Breakfast 8:00 a.m. Opening remarks 8:15 a.m. Ethical considerations in dysphagia management 10:00 a.m. Break 10:20 a.m. Optimizing clinical assessment – What does it involve? 12:30 p.m. Lunch – Meet a mentor 1:00 p.m. Putting the pieces together – Going back to the real world! 2:30 p.m. Advocating for interprofessional practice – Wrap-up discussion 3:00 p.m. Workshop evaluation and closing 3 SESSION DESCRIPTIONS SUNDAY, OCTOBER 4, 2015 MONDAY, OCTOBER 5, 2015 7:00 p.m. The client’s lived experience Speakers: TBC We begin our program with inspirational stories from people living with dysphagia. Through a guided interview process, we will hear first-hand from those experiencing or dealing with the consequences of dysphagia and about their interactions with diverse members of the professional health care team. By opening our program with the client’s voice, we ground our next two days of learning in an empathetic and client-focused perspective. 8:00 a.m. Breakfast 9:00 a.m. What is interprofessional dysphagia practice and why should we care? This opening address will begin our program with the challenging question: What does interprofessional dysphagia practice mean and why should we embrace it? Using evidence-based competencies for interprofessional education and collaboration, this interactive session facilitated by Lynne Sinclair will encourage us to explore how effective communication and role clarity will enable best client outcomes. 10:30 a.m. Morning break 10:50 a.m. Case-based discussions Dysphagia affects individuals across the lifespan living in various settings. Using multiple cases, our speakers will facilitate small group discussions through which complex practice issues experienced every day will be explored. Cases presented will be tailored to various practice settings, age groups, socio-cultural-educational profiles of clients, urban/rural setting, availability of resources and professionals on the team. Participants will be invited to delve into the care plans for the sample clients and consider innovative approaches to intervention. 12:30 p.m. Lunch and sponsor showcase 4 1:30 p.m. Interactive breakout sessions (2 x 45-minute sessions) Six interactive breakout sessions are available for participants to have an “up close and personal” view of integral components of dysphagia care. Each session will be presented twice. Every participant will have an opportunity to attend three of the six available 45-minute sessions. Please select your preferred sessions on the registration form. A: Health starts with the mouth: Putting theory to practice Joyce Wimmer, RDH Oral health is important to overall health. We know the theory behind providing oral care but do we know how to do it? “Putting theory to practice” will be a fun and interactive session that will help to answer some of your questions about providing oral care to your clients. B: How safe is water? Exploring the evidence for and against water protocols Catriona Steele, PhD, CCC-SLP, S-LP(C) The evidence supporting water protocols has been evolving. Dysphagia clinicians should be aware of the latest evidence and how to apply it to the populations they serve. This session will summarize recent empirical evidence regarding water protocols as applied to people who aspirate thin liquids. Interactive discussions will be used to identify ideal candidates and highlight protocol rules that will promote safe intake of water where possible. C: “Client has a tracheostomy tube.” What is that and what does it mean for the client? Janet Fraser, RRT Breathing is one of the most important physiological processes in the body but it is often at odds with the emotional desire to eat orally. When a client’s breathing has become impaired to the point of needing a tracheostomy tube, swallowing and oral feeding management needs special care. The impact of respiratory impairments, shortness of breath, tracheostomy tubes and mechanical ventilation will be the focus of this hands-on session. 5 SESSION DESCRIPTIONS D: The thin and the thick of it: The new International Dysphagia Diet Standards Andrea Buchholz, PhD, RD and Peter Lam, RD Texture-modified foods and thickened liquids are a cornerstone of dysphagia management but there can be challenges in applying them in practice. This session will highlight the International Dysphagia Diet Standards and allow participants to taste, test and explore the many nutritional considerations of food and liquid modifications. E: “One position doesn’t fit all”: The role of postural management in dysphagia Jan Duivestein, MRSc, OT/PT and Heather Lambert, PhD, erg, OT(C) Many individuals with dysphagia experience difficulty with posture and positioning during mealtimes. Posture can affect respiration, swallowing, GI function and physical function. This session will provide a review of the literature on posture and positioning, as well as how it impacts individuals with dysphagia. Participants will have the opportunity to discuss and experience postural challenges and potential solutions. F: Medication: Its impact on swallowing Nathalie Blouin, MD Medication is an important issue when taking care of clients with swallowing difficulties. It can cause dysphagia, complicate a pre-existing condition and deepen the burden of taking medication. This session will review the principle categories of medication which cause dysphagia and discuss management techniques. 3:15 p.m. Afternoon break 3:35 p.m. Continuation of interactive breakout sessions (1 x 45 minute session) 6 4:20 p.m. Another brick in the wall – What have we learned? Wrapping up Day 1 will be a facilitated group discussion related to providing optimal care for people with dysphagia. This will be an opportunity for questions to the presenters and to reflect on learnings of the day about the nature of differing scopes of practice, the interprofessional team or specifics of care as explored in the breakout sessions. 5:00 p.m. Close 7 SESSION DESCRIPTIONS TUESDAY, OCTOBER 6, 2015 7:30 a.m. Breakfast 8:00 a.m. Opening remarks 8:15 a.m. Between soup and love: Ethical considerations in dysphagia management Ann Munro- Heesters, PhD (ABD) Ethics is an integral part of the practice of all health care professionals but it typically comes to our attention when we are confronted with values that conflict with or challenge our own. End-of-life care and the abortion debate are typically cited as sources of value disagreement, but the topic of eating can also elicit powerful responses. Food doesn’t cease to be personally, socially or culturally significant merely because swallowing has become unsafe. A range of cases, drawn from real life, will be used to explore how an ethical lens can help us see what we may overlook in an effort to provide safe, responsible and professional care. Participants will be encouraged to share their own cases and experiences to enhance the learnings of the group. 10:00 a.m. Morning break 10:20 a.m. Optimizing clinical assessment – What does it involve? Practices for dysphagia clinical assessments are highly varied among clinicians and professions. The million dollar question: what components should be part of a practical, holistic dysphagia evaluation? In this session, participants will have a chance to work in small interprofessional groups and to discuss and design the components of a dysphagia evaluation using each other’s professional perspective and expertise. 8 12:30 p.m. Lunch – Meet a mentor Mentorship is a way to grow professionally throughout one’s career. There is great merit in the mentor-mentee relationship for both parties. This program is an attempt to bring together those with diverse skills in dysphagia assessment and management, and it may be, through conversation and networking, that you will find just the right contact who will help broaden or deepen your practice skills. 1:15 p.m. Putting the pieces together: Going back to the real world! Interprofessional practice is considered best practice in our current health care environment. Despite this, many challenges still exist for clinicians in their day-to-day practice. Using a mock case, these challenges will be explored with the intent of identifying innovative means of promoting and improving interprofessional dysphagia practice in your setting. 2:45 p.m. Advocating for interprofessional practice: Wrap-up discussion 3:00 p.m. Final remarks 9 SPEAKERS NATHALIE BLOUIN, MD Dr. Nathalie Blouin is a family doctor working at the Institut Universitaire de Gériatrie de Montréal. She is Associate Professor in the Family Medicine Department of the Université de Montréal and Director of the Interdisciplinary Dysphagia Clinic that she helped create in 1997. Her clinical work is concentrated in geriatric rehabilitation, and especially dysphagia, following strokes or deconditioning after acute illnesses. ANDREA BUCHHOLZ, PHD, RD Andrea Buchholz is a registered dietitian, and Associate Professor and Curriculum Chair of the Applied Human Nutrition program in the Department of Family Relations and Applied Nutrition, University of Guelph. She teaches clinical nutrition and applied clinical skills, including dysphagia screening and dietary management, at the undergraduate and graduate levels. JAN DUIVESTEIN, MRSC, OT/PT Janice Duivestein is a combined trained therapist (OT/PT) who has worked in the area of eating, drinking and swallowing with children and adults for over 25 years. She is privileged to work in team environments and highly values the skills and knowledge of her fellow team members. As well as her clinical work, Jan provides education about dysphagia to students in the occupational therapy program at the University of British Columbia, as well as to other health professionals. 10 JANET FRASER, RRT Janet Fraser is a registered respiratory therapist with an astonishing (but unnamed) number of years of experience in health care. As a member of the interdisciplinary Respiratory Services team at West Park Healthcare Centre in Toronto, she has been involved in the care of hundreds of individuals with tracheostomy tubes. PETER LAM, RD, CFE Peter Lam is the co-chair of the International Dysphagia Diet Standardisation Initiative working with an interprofessional team of professionals from around the world to develop standardised terminology for texture modified diets and thickened liquids. Peter provides nutrition, food service and professional practice consultation to health care, food service and hospitality industry clients. He is an appointed clinical instructor at the University of British Columbia. HEATHER LAMBERT, PHD, ERG., OT(C) Heather Lambert is a faculty lecturer at McGill University’s School of Physical and Occupational Therapy. Her research and clinical interests centre on the bedside assessment and management of ingestive difficulties. She is the author of The McGill Ingestive Skills Assessment, a quantitative bedside screening tool for adults. As a private clinician, she assessed and treated clients with dysphagia from 1996 – 2011. 11 SPEAKERS ANN MUNRO-HEESTERS, PHD (ABD) Ann Heesters is the Associate Director of Bioethics at the University Health Network, Chair of the UHN Rehabilitation Science and Medicine Research Ethics Board and is a Bioethicist with the University of Toronto’s Joint Centre for Bioethics. She has an abiding interest in standards of practice for health care ethicists and helped to draft a code of ethics for ethicists with her colleagues on Clinical Ethics Consultation Affairs, a committee of the a.m.erican Society of Bioethics and Humanities. She was a founding member of Practicing Healthcare Ethicists Exploring Professionalization, which is now a non-profit board called Canadian Association of Practicing Healthcare Ethicists (CAPHE). LYNNE SINCLAIR, MA Lynne Sinclair is an educational consultant, physiotherapist and the Innovative Program and External Development Lead at the Centre for Interprofessional Education, University of Toronto (U of T). She holds an Assistant Professor position with the Department of Physical Therapy at University of Toronto and has been in the Faculty of Medicine, University of Toronto for over 20 years. Lynne is widely invited as a keynote speaker for conferences, educational events and courses. She has taught all over Canada, the USA, Australia and Saudi Arabia. Lynne’s passion for physical therapy and interprofessional education was ignited during her 7 years at Toronto Rehabilitation Institute where she was the Director of Education for twelve health disciplines. 12 CATRIONA STEELE, PHD, CCC-SLP, S-LP(C) Catriona Steele is a speech-language pathologist and scientist at Toronto Rehabilitation Institute. She also teaches in the Masters of Health Science program in Speech-Language Pathology at the University of Toronto. Her primary research interest is in the rehabilitation of oropharyngeal swallowing disorders (dysphagia). Her research explores both basic principles underlying clinical interventions for dysphagia and clinical outcomes following rehabilitative treatment. She has a special interest in the use of surface EMG biofeedback as a tool in dysphagia rehabilitation. MELANIE TAPSON, S-LP(C) Melanie Tapson is a speech-language pathologist who works primarily in dysphagia and voice therapy. Melanie’s extensive experience as a professional performer combined with her training as a teacher, researcher, and speech-language pathologist provides her with a unique perspective on client care. She believes that treating voice and swallowing disorders require a holistic, team-driven approach, and she is a fierce advocate for prehabilitation, or preventative voice care, to keep artists and voice users in top form. JOYCE WIMMER, RDH Joyce Wimmer has worked as a dental hygienist since 1995 and was recently appointed clinical instructor at George Brown College. Throughout her professional career, as a clinician and educator, she has demonstrated her commitment by showing the importance of oral health as it is related to overall health to not only clients of all ages, but also on interprofessional care teams. 13 WORKSHOP REGISTRATION REGISTRATION FEES (PLUS TAXES): (Includes dinner on October 4, breakfast, lunch and breaks on October 5 and 6 and workshop materials) Registrations received by September 7, 2015 $435 for members of CAOT, DC or SAC $650 for non-members Registrations received after September 7, 2015 $535 for members of CAOT, DC or SAC $795 for non-members Registrations will not be accepted after Friday, September 25, 2015 at 5:00 p.m. (Eastern Time). PAYMENT RECEIPT: Upon registering, you will receive an email confirmation and statement. The statement is your receipt. REGISTRATION CANCELLATION: Written notice of cancellation is required by September 7, 2015 and is subject to an administrative fee of $100 plus taxes. For cancellations received after this date, no refund will be provided. EVENT CANCELLATION: We reserve the right to cancel this workshop should the number of registrations not reach minimum requirements. PHOTO RELEASE: Photography may occur during this event for use on association promotional materials, websites and social media. By virtue of your attendance, you give permission to use your likeness. 14 REGISTRATION CONTACT: FRANCES SCOVIL Tel: (416) 642-9308 [email protected] BOOK YOUR HOTEL ROOM Make your hotel reservation by using the Toronto Airport Marriott Hotel’s online group reservation system at Marriott Reservations or by calling Marriott’s Reservations tollfree number (800) 905-2811. The Group Rate of $139 plus applicable local taxes is guaranteed for reservations made on or before the cut-off date of Monday, September 7, 2015. If using the tollfree number, specify that you should be included under the Canadian Association of Occupational Therapists room block. Any reservations made after the cut-off date shall be at the Hotel’s then current available rate. SPONSORSHIP CONTACT: CHRISTINA LAMONTAGNE [email protected] GEORGETTE HARRIS [email protected] MICHELLE JACKSON [email protected] PROGRAM PLANNING SUBCOMMITTEE ANDREA BUCHHOLZ HEATHER LAMBERT CATRIONA STEELE JAN DUIVESTEIN PETER LAM MELANIE TAPSON EVENT MANAGEMENT GROUP JOANNE CHARLEBOIS CARLA DI GIRONIMO CORINNE EISENBRAUN JANET CRAIK JAN DUIVESTEIN PETER LAM 15 OCTOBER 4 - 6, 2015 Toronto Airport Marriott Hotel 901 Dixon Road Toronto, ON CHARTING NEW GROUND: Interprofessional approaches to dysphagia management
© Copyright 2026