Navigating the Insurance Appeal Maze - How to Win and Get Coverage
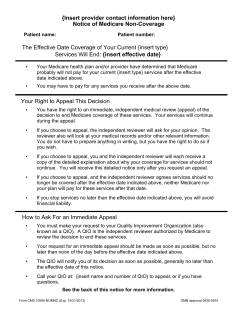
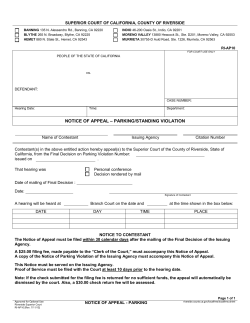
Navigating the Insurance Appeal Maze - How to Win and Get Coverage March 26, 2014 Niketa Sheth Senior Vice President, Quality of Life Christopher & Dana Reeve Foundation Bernadette Mauro Director, Information and Resource Services Christopher & Dana Reeve Foundation Bill Cawley Manager, Peer & Family Support Program Christopher & Dana Reeve Foundation Carlos Caprioli Information Specialist and Translator Christopher & Dana Reeve Foundation Appealing Medicare Coverage Decisions Medicare Summary Notice (MSN) • Review your “Medicare Summary Notice (MSN).” If you disagree with a coverage or payment decision, you can appeal. • You’ll get an MSN in the mail every 3 months. You must file an appeal within 120 days of the date you receive the MSN. Source: Medicare.gov 5 Levels of Appeal (Original Medicare) 1. Redetermination by the company that handles claims for Medicare 2. Reconsideration by a Qualified Independent Contractor (QIC) 3. Hearing before an Administrative Law Judge (ALJ) 4. Review by the Medicare Appeals Council (Appeals Council) 5. Judicial Review by a Federal District Court Source: Medicare.gov Level 1: Redetermination Options for Requesting a Redetermination: 1. Fill out a standard CMS "Redetermination Request Form" and send it to the Medicare contractor at the address listed on the MSN. 2. Send a copy of the MSN to the company that handles bills for Medicare (listed on the MSN) asking for a review. 3. Send a letter to the company that handles bills for Medicare. Source: Medicare.gov Level 2: Reconsideration Options for Submitting a Reconsideration Request: 1. Fill out a "Medicare Reconsideration Request Form.” 2. Submit a written request to the QIC. Source: Medicare.gov Level 3: Hearing Before an Administrative Law Judge (ALJ) Options for Requesting a Hearing: 1. Fill out a "Request for Medicare Hearing by an Administrative Law Judge" form. 2. Submit a written request to the OMHA office that will handle your ALJ hearing. Source: Medicare.gov Level 4: Review by the Medicare Appeals Council Options for Requesting an Appeals Council Review: 1. Fill out a "Request for Review of an Administrative Law Judge (ALJ) Medicare Decision/Dismissal" form. 2. Submit a written request to the Appeals Council. Source: Medicare.gov Level 5: Judicial Review by a Federal District Court • To get a judicial review in federal district court, the amount of your case must meet a minimum dollar amount. For 2014, the minimum dollar amount is $1,430. You may be able to combine claims to meet this dollar amount. Follow the directions in the decision letter you got in level 4 to file a complaint. • If you want your doctor or other prescriber (for prescription drug appeals) to request this level of appeal on your behalf, you’ll need to submit an “Appointment of Representative” form. Source: Medicare.gov Original Medicare vs. Medicare Advantage Coverage and Payment Notices • • Original Medicare: Medicare Summary Notices (“Initial Determinations”) Medicare Advantage and Part D Drug Plans: Explanation of Benefit Statements (“Organizational Determinations”) Appeals Deadlines for the First Level of the Appeal Process • • Original Medicare: 120 Days Medicare Advantage and Part D Drug Plans: 60 Days Qualified Independent Contractor (QIC) vs. Independent Review Entity (IRE) • In the second level of the appeal process, a Qualified Independent Contractor (QIC) is the organization that decides on appeal under Original Medicare. For Medicare Advantage and Part D, an Independent Review Entity (IRE) makes the decision. Source: Health Assistance Partnership – Medicare Appeals Rights and Procedures Appealing Medicaid Coverage Decisions Know Your Rights! • Prior written notice of adverse action • Fair hearing before an impartial decision-maker • Continued benefits pending a final decision • Timely decision measured from the date the complaint is first made Source: Kaiser Family Foundation: A Guide to the Medicaid Appeals Process Written Notices At least 10 days (typically) before taking an action that affects a beneficiary’s coverage, state Medicaid agencies must send a notice that includes (among others) the following information: • The action (e.g., denying a claim) • An explanation for the action • Explanation of your right to request a hearing and the process for requesting a hearing in your state • Your rights for hearing representation (e.g., yourself, legal counsel, other spokesperson) • An explanation of the circumstances under which your benefits will continue if a hearing is requested Source: Kaiser Family Foundation: A Guide to the Medicaid Appeals Process Requesting a Hearing Requirements for requesting a hearing vary by state, but will be outlined in the written notice of action you receive in the mail. • Remember: – Be aware of your state’s established timeframe for requesting a hearing (generally between 20 and 90 days from the date a notice of action is mailed) – Your request can only be denied if you withdraw the request in writing or fail to appear – If you are currently receiving services, you have the right to request that those services continue until a final hearing decision is issued NOTE: If you receive services through a Managed Care Organization (MCO), you have a right to a hearing; however, you may be required to exhaust the MCO’s appeal process first. Source: Kaiser Family Foundation: A Guide to the Medicaid Appeals Process Preparing for Your Hearing Gather Documents: Prepare a list of / copy all of the documents, photos, or other materials you want the hearing officer to use in making the decision. This includes letters from doctors, medical records, letters or emails to and from Medicaid or your caseworkers. Prepare a Written Statement: Write down the important facts of your case and why you think Medicaid’s action is wrong (e.g., the services are medically necessary). You will be able to make opening remarks before the testimony and closing remarks after. You can give the hearing officer a “brief” before the hearing, if you are able. A brief is a written document with the facts, your arguments, and supporting evidence. • Bring Your Medicaid Notice: Ask the hearing officer to review the notice. If you think the notice left out any important information, say so. • Identify Witnesses: Find witnesses who can help support your side of the case (e.g., your doctor or nurse, caregivers, family members, etc.). If your witnesses cannot attend the hearing, ask them to write a letter explaining why your services are medically necessary. Get the letter notarized, if possible. • Prepare Questions: Prepare a list of questions you want to ask your witnesses, as well as witnesses attending your hearing on behalf of Medicaid. Source: Protection and Advocacy for People with Disabilities, Inc. Hearing Decisions You will receive a decision in writing within 90 days of the date you asked for a hearing. • If you win… – Medicaid will make corrective payments, retroactively • If Medicaid wins… – Medicaid will notify you of your right to have the hearing decision reviewed by a state court – If you received services throughout the hearing, you may have to reimburse Medicaid for those services Source: Kaiser Family Foundation: A Guide to the Medicaid Appeals Process Appealing a Private Insurer’s Decision Not to Pay Internal Appeal • An appeal directly to your insurance company • Must be filed within 180 days of claim denial • Complete all insurance company forms or write to your insurance company with your name, claim number, and health insurance ID number • Submit any other information you want the insurance company to consider when evaluating your appeal • At the end of the internal appeals process, your insurance company must provide you with a written decision Source: marketplace.cms.gov External Appeal • Must be filed in writing and within the timeframe established by your health insurance company (typically within 60 days of the date your insurer sent you a final decision) • You may appoint a representative to file the review on your behalf • The written final denial of your internal appeal will include the contact information for the independent third party that will handle your external review • The external reviewer will issue a final decision – your insurance company must accept the reviewer’s decision • External reviews are decided as soon as possible (no later than 60 days after the request was received) • You may qualify for an expedited external review Source: marketplace.cms.gov Tips for a Successful Appeal Tips for a Successful Appeal • Know the appeals process (e.g., deadlines, options, etc.) • Keep accurate and comprehensive records (e.g., medical records, denial letters, letters from your provider(s), your own personal notes, etc.) • Ask your doctor for a letter of medical necessity • Be persistent! We Can Help! Questions? ???
© Copyright 2026