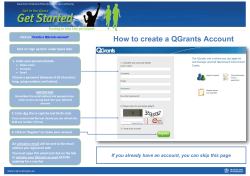
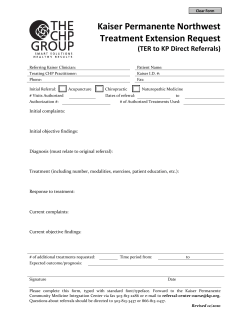
Illustrating “how to” implement the Top 20 Actions for Change
Illustrating “how to” implement the Top 20 Actions for Change Storyboard Examples of Improvement Work Cancer Service Improvement Programme Illustrating “how to” implement the Top 20 Actions for Change Storyboard Examples of Improvement Work Cancer Service Improvement Programme © Crown copyright 2005 ISBN: 0-7559-4758-4 Scottish Executive St Andrew’s House Edinburgh EH1 3DG Produced for the Scottish Executive by Astron B42431 11/05 Published by the Scottish Executive, November, 2005 100% of this documment is printed on recycled paper and is 100% recyclable. List of Contents Introduction 1 Referral 5 Consultation/Investigation/Diagnosis (CID) 15 Multi Disciplinary Team (MDT) 35 Treatment 43 Contacts 59 Top 20 Actions for Change Storyboard Examples of Improvement Work: Introduction The Cancer Service Improvement Programme (CSIP) is working in support of improvement. The focus of the work is to enable clinical teams and their support staff to make changes happen and to encourage the implementation of successful changes. Hundreds of staff at grass roots level along with patients and their families have worked together to highlight where further improvements to cancer services can be made. The team uses a tried and tested model for improvement, which has been used worldwide to make change happen in health care. The PDSA cycle, plan, do, study, act – gives teams the discipline to plan a change, implement it, measure its effect and act on the results. We have gathered real examples from across Scotland of improvement work. The examples offer a practical guide of “how to” implement the Top 20 Actions for Change. The examples in this booklet are only a snapshot of the improvements (over 500) achieved throughout Scotland. They illustrate changes at key stages of the care pathway. This work is fully supported by the Cancer Service Improvement Programme’s Regional Facilitators who are ready to help you implement the changes appropriate to your local area. The Top 20 Actions for Change are widely available to the Scottish NHS to support a faster pace of change across Scotland. Pauline Ferguson National Programme Manager Cancer Service Improvement Programme Centre for Change and Innovation October 2005 1 Top 20 Actions for Change Maximum 62 days from urgent Primary PATIENT EXPERIENCE AIMS HOW Information on where these improvements have taken place is on the reverse of this leaflet. Thinking something was wrong Early Detection Rapid Diagnosis CONSULTATION/INVESTIGATION/ DIAGNOSIS (CID) GP REFERRAL “Eliminate delay and enable appropriate processing of referrals.” 1. Clear GP symptom-related referral guidelines. “Timely management of investigations and results to provide early communication of diagnosis.” 2. Electronic/faxed referral to a central point. 1. Pre-booking/scheduling of investigations and appointments. 3. Referral to a service, not a consultant. 2. Dedicated or fast-track clinics with rapid reporting. 4. Direct referral to specialist service from diagnostics. 3. Reduce consultant vetting of investigation requests. 5. No vetting or, as a minimum, daily team vetting of all referrals. 4. Telephone consultation/ communication of results. 6. Single route of referral and access for endoscopy services. 6. Reduce follow-up appointments at out-patient clinics. GOOD COMMUNICATION IS THE KEY 2 5. Specialist nurse-led clinics. Care referral to 1st definitive treatment Seeing someone in the NHS, having tests and being told what was wrong Receiving treatment Improve treatment and care 62 DAYS MULTIDISCIPLINARY TEAM MEETING (MDT) TREATMENT “Ensures that a fully informed discussion of all patients diagnosed with cancer takes place and appropriately formulated treatment plan is documented.” “No needless delays.” 1. Co-ordination of treatment processes across network to ensure optimum use of capacity, e.g. theatre time. 2. Planned management of annual leave and public holidays. 1. Clear responsibility for co-ordination of MDT to ensure all necessary information is available at MDT for treatment decision-making. 3. Streamlining of booking processes for chemotherapy and radiotherapy. 4. Efficient system for appropriate referral to palliative care. 2. MDT used to refer on for treatment, i.e. investigations, surgery, oncology. 3. Timely communication with GP of MDT decision. 4. Video conferencing/Telemedicine links to be used where attendance is limited. 3 4 Referral GP Referral “Eliminate delay and enable appropriate processing of referrals.” 1. Clear GP symptom-related referral guidelines. 2. Electronic/faxed referral to a central point. 3. Referral to a service, not a consultant. 4. Direct referral to specialist service from diagnostics. 5. No vetting or, as a minimum, daily team vetting of all referrals. 6. Single route of referral and access for endoscopy services. 5 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Routine information regarding PSA blood testing Top 20 Referral In Oban and outlying rural areas, all patients are sent out routine information explaining implications of PSA blood testing before first consultation. Making It Happen Following discussion with the Urology Nurse Practitioner and Local General Practitioner it became evident that patient undergoing PSA blood testing in primary care or in hospital outpatient department were not informed in a uniform fashion. Both parties were keen for uniform verbal and written information for all patients. Appropriate patient information leaflets were chosen and agreed on. PSA information leaflets are sent out to all patients in local and outlying areas with the appointment card for first consultation. Implementation Advice Implementation was quick and easy with cooperation of outpatient department staff and Primary health care teams. Impact All patients receive uniform information about PSA blood testing. Contact Rosemary Noon Urology Nurse Practitioner Vale of Leven Hospital [email protected] 01631 789 059 6 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Clear GP symptom–related referral guidelines. Top 20 Referral 1 In Borders General Hospital, the medical director discussed with general practitioners (GP’s) the need to provide accurate and full history details of patients with suspected lung cancer. This has resulted in referral letters being processed without the need of secretarial staff to retrieve the necessary information from the GP practices. Making it Happen The lung cancer team highlighted that some of the GP referral letters did not have enough information in them regarding the patients condition. This information is essential to make the first consultation at the hospital efficient and aid to a prompt diagnosis. The medical director wrote a letter to all GP’s requesting that they provide appropriate information to allow swift progression from receipt of referral letter to the patient receiving an out patient appointment. Impact The benefit of this change has been: • Increase in the quality of the information within the referral letters • Hospital secretaries have not had to phone the GP practices requesting additional information • A reduction of 1 to 2 days processing time between receiving the referral letter and making an out patient appointment Contact Dr John Gaddie, Consultant Respiratory Physician Borders General Hospital [email protected] 01896 754 333 7 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Electronic/faxed referral to a central point Top 20 Referral 2 In Argyll and Clyde, Oban Hospital services a rural area with 4 outlying outpatient clinics. Staff have developed electronic/faxed referral to a central point in Oban for all urgent suspected cancer referrals. This now means all urgent referrals are seen quickly at a central point for first consultation/assessment. Making It Happen Waiting time for 1st consultation time reduced by 1 week if from outlying area • y Au gu st Ju l e ay M Ju n M ar ch Following discussion it was decided to appoint all urgent patients to 1 central point where they could be seen quickly. 5 4 3 2 1 0 Ap ril No. of Weeks Before the change, it was discovered that there was a variable referral system, with referrals coming into outlying rural clinics and the main district general hospital urology service by several methods, casing delays in appointing some patients. Month (2005) Staff from Outpatients department contacted and visited all GP practices with SCI Gateway team and assessed their requirements to allow GPs to refer electronically to a central point in Oban. Impact The benefits from this change are: • • An IT system was developed to allow practices with incompatible software packages to refer electronically. • • IT education and support was offered to all appropriate practice. • Practices that couldn’t refer electronically were encouraged to fax referrals to the central point. • A urology proforma was developed by the urology nurse practitioner and a local GP which stated that all urgent suspected cancer referrals should come directly to a central point. • 1 central referral point allowing referrals to be vetted and appointed on a daily basis. All urgent patients seen in an equitable time and at a central point. Waiting time for first consultation reduced by 1 week if from outlying area. Next Steps Review of guideline and monitoring of service to ensure that single point of referral is being maintained. Implementation Advice Contact The General Practitioner was very keen on a structured framework for referral to support and guide primary care staff. Examples of referral proformas were sourced from other areas by Cancer Service Improvement Programme Facilitator and utilised to reduce workload. Rosemary Noon Urology Nurse Practitioner, Vale of Leven Hospital [email protected] Tel: 01631 789059 8 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Electronic /faxed referral to a central point Top 20 Referral 2 In Elgin, referrals to the lung team are being faxed directly to the central point in Aberdeen Royal to be vetted on a daily basis. Making It Happen Impact Prior to the change, referrals to the lung team by GP’s in Elgin were received at Elgin hospital and were only vetted on a 2 weekly basis when a respiratory consultant from Aberdeen Royal was undertaking an outreach clinic. The benefit from this change has been: This method built in delay appointment for the patient. to first This was highlighted at a mapping event with the lung team and following this staff in Elgin are now faxing these referrals directly to the central referral point in Aberdeen Royal. This has reduced the potential time to making an appointment from 2 weeks to 2 days. One central focus for referrals allows these to be triaged on a daily basis and appointed as early as possible Potential time to appointment for Elgin patients has been reduced Next Steps Ensure sustainability of service. Continued review of guideline and monitoring of process to ensure that the single point of referral is maintained. Review the use and implementation of a similar system for inter-hospital referrals to streamline all referrals to the Lung team. Implementation Advice Appropriate protocol in place within outlying hospitals to ensure referrals do not wait for triaging. Contact Dr Joe Legge, Respiratory Physician Aberdeen Royal Infirmary, Aberdeen [email protected] 01224 681 818 9 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Electronic /faxed referral to a central point Top 20 Referral 2 In Grampian, doctors, radiographers and admin staff, have reduced the delay for receiving a chest x-ray from a maximum of 2 weeks to 2 days. GP’s can now fax a chest x-ray request to Woodend Hospital and Aberdeen Royal Infirmary X-ray departments with the patient’s contact details. The x-ray staff will then contact the patient and ask them to attend for their x-ray the same day or the next day. Making It Happen weeks to 2 days contributing to a reduction in time to diagnosis for all GP referrals to the Lung Service. Prior to the change, referral letters from GP’s to the hospital requesting a chest x-ray were dictated, typed and signed in the GP practice then sent by mail to the hospital. Once received by the x-ray departments, appointments were allocated and the patient sent an appointment. Implementation Advice Consultation and communication with Primary Care colleagues is essential. This process took a maximum of 2 weeks to complete. Impact Once the x-ray was reported this was sent back to the GP for them to review and refer onto a specialist if appropriate. The benefits from this change have been: Reduction in time to x-ray appointment from a maximum of 3 days to 2 days After a team mapping event, a PDSA cycle was tested. Chest x-ray requests were faxed to the department from the GP practices with the patient’s contact details. These requests are dealt with on a daily basis and the patient contacted directly by the x-ray staff to arrange an appointment on either the same day or the next day. The intranet guideline for referral of suspicious lung cancer was reviewed and updated following the mapping event and a reminder letter sent to all GP practices in Grampian advising of the updated guideline. Direct communication with the patient to ensure they can attend for x-ray minimising cancellations and re-appointments. Next Steps Ensure sustainability of service and continued communication with Primary Care. Contact In this way the time to receiving a chest x-ray has reduced from a maximum of 2 Dr Joe Legge, Respiratory Physician Aberdeen Royal Infirmary, Aberdeen [email protected] 01224 681 818 10 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Referral to a service, not a named consultant Top 20 Referral 3 In Tayside, doctors, nurses, managers and medical records staff, asked GP’s to add “Colorectal” to the referral letter. A letter was written to all GP practices in Tayside. The number of patients waiting for a hospital appointment has now reduced. Making It Happen Reduction in time taken to vet GP referral letters from a maximum of 8 weeks to 3 days 9 8 7 6 Weeks Prior to this change, referral letters sent into the hospital by GP’s about patients with colorectal symptoms were all received within medical records, then sent through the hospital internal mail to one doctor to be vetted. They were batched together with all the other general surgical referrals. 5 4 3 2 After vetting and categorising into urgent, soon and routine, the letters were sent back to medical records and placed onto an appointment waiting system. 1 0 Jan-2004 Feb-2004 Apr-2004 Jun-2004 Months This process took a maximum of 8 weeks to complete. After a team mapping event, a PDSA cycle was tested. A letter was sent to all GP practices in Tayside to request that the word “Colorectal” be added to the referral letters to distinguish them from the general surgical referrals when received in medical records. The letters are still vetted, but the doctor responsible now hands the letters with “colorectal” highlighted to the Colorectal Clinical Nurse Specialist who now either allocates appropriate clinic appointments or organises investigations before returning the letters by hand to medical records. Jan-2005 Aug-2005 Ninewells Hospital and Medical School, Dundee, Scotland Reduction in vetting referral letters from a maximum of 8 weeks to 2 weeks Referral letters are now being reviewed by the Colorectal Clinical Nurse Specialist and dealt with appropriately Approximately 2500 patients are referred each year to general surgery in Tayside and most of these referrals have colorectal symptoms, therefore this change will benefit these patients. Next Steps Reduce the time to vet referral letters further by allowing the Colorectal Clinical Nurse Specialist access to the electronic referral system to view all referral to the colorectal service, thus allowing “on line” review and decisions transferred back to medical records electronically by email. Implementation Advice Consultation and communication with Primary Care colleagues is essential. Contact Impact Jackie Kerrigan, Macmillan Colorectal Nurse Specialist, Ninewells Hospital, Dundee [email protected] 01382 425 563 The benefits from this change have been: 11 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Direct referral to a specialist service from diagnostics Top 20 Referral 4 In Dundee, doctors, radiologists and clerical staff have made a number of simple changes to their working practices which has reduced the time that patients wait to be seen by a respiratory physician. Previously patients could wait on average 23 days to be seen. This has now been reduced to an average of 10.5 days. Radiology staff are now making a direct referral to the Respiratory clinic after reporting a highly suspicious chest x-ray. Details of the results and the patient appointment are sent to the GP. Time from GP referral to 1st specialist hospital appointment Making It Happen 25 23 20 15 15 14 Days Prior to the change, patients would be asked to attend the open access radiology service for a chest x-ray. The results were reported & would be dictated and sent back directly to the patient’s GP. The GP would then review the result, see the patient and recommend a referral to the hospital specialist. 12 10.5 10 8 This method built in a considerable delay for the patient and the time to diagnosis and subsequent treatment could be significant. 5 This was highlighted at a lung team mapping event and after discussion it was agreed to test direct referral from Radiology to the Hospital Specialist. 0 Apr - Jul 03 Nov-03 Feb-04 Jun-04 Months After the x-ray was taken, if felt suspicious of cancer the Radiographer would highlight this as urgent. It would be reported and typed within 48 hours. The secretary would then contact the Hospital Chest Clinic and arrange an appointment for the patient at the hospital. The Chest Clinic sends or telephones the appointment to the patient. The x-ray report is returned to the GP with result and the date of the patient’s hospital clinic appointment. Oct-04 Feb-05 Ninewells Hospital and Medical School, Dundee, Scotland Time from GP referral to seeing a Specialist has reduced from an average of 23 days to 10.5 days. Patients are being diagnosed and therefore starting treatment, as appropriate, more quickly. Alleviating patient’s anxiety by seeing and diagnosing more quickly. Next Steps Implementation Advice Ensure sustainability of service. Continued review of process to maintain shortest waiting times for patients, aim is to maintain time at an average of 10 days. Consultation and communication with Primary Care colleagues is essential. Patients being referred for a chest x-ray need to be made aware that they may receive a further appointment from the Hospital Chest Clinic. Contact Impact Dr Peter Brown, Respiratory Physician Ninewells Hospital, Dundee [email protected] 01382 660 111 The benefit from this change has been: 12 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE No vetting or, as a minimum, daily team vettng of all referrals Top 20 Referral 5 In Lothian, consultant gynaecologists and nursing staff have developed a system for daily vetting of referral letters to ensure that there is no delay for patients to be seen by a consultant. Making It Happen Impact Prior to the change, all consultants had different vetting patterns and in some cases were vetting referral letters only once a week. In addition, if a consultant were absent, the letters waited for vetting until they returned, leading to a potential delay of up to 39 days just for a consultant to see a letter. Impact of the change over time 70 65 62 60 Number of days 55 50 45 39 40 35 30 At a process mapping event, the team identified that a daily vetting rota would eradicate this delay in the patient’s journey. This idea was tested using PDSA (plan, do, study, act) cycles. Through discussion and team working, a rota was established and a consultant and senior OPD nurses now vet letters every day. Letters are categorised into urgent,, soon or routine and appointments are made accordingly. 25 20 Treatment Target 15 Days 10 5 1 0 Nov-04 Dec-04 Jan-05 Feb-05 Mar-05 Apr-05 Time to vet letters The benefits of this change are: Now all referral letters are seen and the patient’s appointment is made the day the referral letter arrives at the hospital. Patients who require to be seen urgently are now given an appointment within 7 days of the letter arriving at the hospital which means that patients are seen by a consultant and can begin the process of diagnosis and commence treatment up to 39 days sooner than before. Urgent referrals are identified within 1 day instead of up to 39 days Patients are seen by a consultant within 8 days of urgent GP referral instead of a potential of 46 days Diagnostic processes & treatment can begin 46 days sooner than before Next Steps The team are continually auditing sustainability of the change to ensure that all patients who are referred urgently for gynaecological cancer are not delayed by the vetting process. Implementation Advice Contact If it is difficult to get the whole team on board, use the PDSA (plan, do, study, act) model of improvement to test the change – this is a good way to persuade ‘reluctant’ team members of the benefits to patients and the service. Dr David Farquharson, Clinical Director Centre for Reproductive Health, Edinburgh Royal Infirmary. [email protected] 0131 536 1000 13 14 Consultation/Investigation/ Diagnosis (CID) Consultation/Investigation/Diagnosis (CID) “Timely management of investigtions and results to provide early communication of diagnosis.” 1. Pre-booking/scheduling of investigations and appointments. 2. Dedicated or fast-track clinics with rapid reporting. 3. Reduce consultant vetting of investigation requests. 4. Telephone consultation/communication of results. 5. Specialist nurse-led clinics. 6. Reduce follow-up appointments at out-patient clinics. 15 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Pre-booking/scheduling of investigations and appointments Top 20 CID 1 Coagulation as a routine investigation: In the Edinburgh Royal Infirmary, all new patients referred to the respiratory clinic with a suspected lung cancer have a routine blood test to establish their clotting factor. Making It Happen The clinical nurse specialist discussed with the clinical team, the need to ensure that coagulation screening is included in the blood investigation request whilst the patient is in the outpatient department. This is essential for the patient to progress to the bronchoscopy unit for further investigations. Prior to the change, when the patient arrived for a bronchoscopy without a recent coagulation screen, bloods were taken and the patient had to wait until the report was available. This process could result in a possible wait of several hours, for the patient. Implementation Advice Appropriate protocol in place within outlying hospitals to ensure referrals do not wait for triaging. Impact Having the results readily available means that the patient can have the bronchoscopy done without delay. Contact Gillian Whitson Oncology Specialist Nurse New Royal Infirmary Edinburgh [email protected] 0131 536 1000 16 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Pre-booking/scheduling of investigations and appointments Top 20 CID 1 In Dundee, closer working by doctors and clerical staff has helped reduce the delay for patients receiving tests that will assist with providing a diagnosis. Patients now leave the chest clinic after their first appointment with the respiratory physician with dates for their bronchoscopy, CT scan and return outpatient appointment. The clinic receptionist now co-ordinates all tests for patients before they leave. This not only means that the patient leaves knowing exactly what is happening next but also in recent months the time to diagnosis has shortened. Making It Happen the smooth patients. Prior to the change, patients would see the Physician and then leave the hospital being advised that an appointment for a CT scan and bronchoscopy would be sent to them. The physician would then send a request for a CT scan and bronchoscopy to the appropriate departments. The requests would be mailed and once received appointments made and sent to the patient. After receiving the tests the patient was required to contact the Chest Clinic to say they had now had their tests and a return outpatient appointment to see the Physician would be made. running of appointments for Impact The benefits from this change are: This method built in a considerable delay for the patient and the time to diagnosis and subsequent treatment could be significant. This was highlighted at a mapping event with the lung team and after discussion it was agreed that the patient should be able to leave their first appointment with dates for their investigations and return appointment for the results. Time to investigations has been reduced. Patients know exactly the next steps in their journey on leaving their first appointment. Potential anxiety is lessened as they know exactly when and where the next investigations are going to be and are not sitting at home waiting for appointments. Time to diagnosis is reduced. Next Steps Ensure sustainability of service. Continued review of process to ensure minimum waiting times for investigations are achieved. Ensure patient information and support available following appointment. The Receptionist at the Chest Clinic now maintains an updated list of next available CT scan slots and bronchoscopy slots. Once the patient leaves their outpatient appointment they agree their scan and bronchoscopy date and receive the appropriate information leaflets regarding these with their date to return to see the Physician. The MDT Coordinator and Specialist Nurse are on hand should the patient wish more information. Contact Dr Peter Brown, Respiratory Physician Ninewells Hospital, Dundee [email protected] 01382 660 111 Implementation Advice Communication between Radiology, Bronchoscopy and the Chest Clinic is vital for 17 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Pre-booking/scheduling of investigations and appointments Top 20 CID 1 In Victoria Hospital, South Glasgow, radiologists and secretarial staff are now using an electronic system to alert secretarial staff to prioritise typing of abnormal chest x-ray reports. This now means that the GP’s are alerted to suspicious chest x-ray results allowing them to refer the patient to the respiratory unit quicker and reducing a previous delay. Making It Happen Prior to the change, all abnormal chest x-ray reports were sent back to the referring GP by post. The GP’s then had to then re refer patients to the hospital to see a respiratory specialist. This meant it took approximately 10 days for the report to get back to the GP. After a process mapping event staff agreed to try out a PDSA (Plan, do, study, act) change cycle to reduce the time taken to get the report back to the GP. Implementation An electronic prioritising system was put in place for reporting and reports are typed within 24 hours. The GP now gets a telephone call with the abnormal results and the written report is then authorised and sent to GP by fax within 7 days. Impact This has reduced the time taken for abnormal reports to be sent to the GP by 4 days All abnormal chest x-ray reports are dealt with promptly The GP is alerted to abnormal results allowing a speedier referral to a respiratory specialist Contact Dr Joe Sarvesvaran, Consultant Respiratory Physician Victoria Hospital, South Glasgow [email protected] 0141 201 6000 18 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Pre-booking/scheduling of all investigations and appointments Top 20 CID 1 In the Victoria Infirmary, South Glasgow, doctors, nurses and clerical staff have made changes to the timing of new patient appointments. All new patients being seen at the respiratory clinic are now guaranteed to have all their lung function test carried out in a timely and appropriate manner. Patients now have all relevant tests on the same day, instead of making two visits to the hospital. Making it Happen Patients who had been referred by their GP to be seen by a respiratory physician for suspected lung cancer, were waiting a long times at the out patient clinic for a lung function test. Some patients had to return on a different day as it was too late for this test to be completed if their appointment was later in the afternoon. After reviewing this, it was agreed to make appointments for these new patients at the start of the clinic. This would allow plenty of time to complete all appropriate tests in the one day. Impact The benefits of this change are: • • All patients have their lung function tests done on the 1 day saving them a hospital journey for a return appointment. Patients are waiting less for their lung function test and all patients are leaving the clinic by 5 pm. Contact Dr Joe Sarvesvaran, Consultant Respiratory Physician Victoria Hospital, South Glasgow [email protected] 0141 201 6000 19 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Pre-booking/scheduling of all investigations and appointments Top 20 CID 1 In Glasgow, a surgeon, clinic and radiology staff have reduced the waiting time for a patient to have a barium enema. They did this by simply improving the communication between the clinics and the radiology department. Making it Happen Impact Prior to the change, 20% of patients were not attending for their pre arranged barium enema investigation, meaning approximately 1 in 5 of these investigation slots were being lost or wasted. This was highlighted by staff at a colorectal process mapping event. The benefits from this change have been: All patients now wait a maximum of 2 weeks for their barium enema, a reduction of up to 6 weeks The patients now know the date and time of their barium enema before they leave the out patients clinic The DNA rate as been reduced from and average of 20.5% before the change to and average of 11.9% after the change After the patients had been seen by a doctor in the out patients clinic and the doctor had referred them for a barium enema, they went home and waited for an appointment to be sent to them by post along with a bowel preparation kit. The waiting time for this investigation was 2 – 3 weeks for urgent referral and over 8 weeks for routine referrals Next Steps To further reduce the DNA rates Full explanation of the barium enema and bowel preparation to be given at the out patient clinic The patients telephone number to be written on the barium enema request card so that cancelled appointments can be re allocated quicker. A PDSA cycle was tested to reduce the “did not attend rate” (DNA) and to increase the efficiency of the barium enema appointments. This involved sending a list of available barium enema appointment slots to the out patient clinic every Monday morning. If required the patients were then given an available appointment before they left the clinic along with the bowel preparation. Contact Dr Fatui Poon, Consultant Radiologist Glasgow Royal Infirmary, Glasgow 0141 201 4000 Reduction in Did Not Attend (DNA) rate for Barium Enema Investigation 0.35 0.3 Percentage 0.25 0.2 0.15 0.1 0.05 0 Apr-2003 May2003 Jun2003 Jul-2003 Aug2003 Sep2003 Oct-2003 Nov2003 Month 20 Dec2003 Jan2004 Feb2004 Mar2004 Apr-2004 May2004 Dec2004 Greater Glasgow Health Board, Glasgow, Scotland CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Dedicated or fast track clinics with rapid reporting Top 20 CID 2 The radiology department at Borders General Hospital identified a need to act more quickly when abnormalities show up on chest x-rays. Radiographers can identify abnormal chest x-rays and have reduced delays by up to 1 week. Making It Happen Prior to the change, chest x-ray films were sent for reporting as part of the routine list. This meant a potential delay of 2 – 4 days for the potentially urgent abnormal chest x-ray to be reported. The consultant radiologist trained ALL radiographers to recognise chest abnormalities, which require rapid reporting. This was achieved by providing in house training sessions for radiographers. Implementation When an x-ray highlights a chest abnormality, the radiographer seeks specialist advice to allow same day reporting. Impact Film/Images are being promptly reported. The report is being sent back to the GP with advice to refer urgently to the lung physician. This has reduced the delay by up to 1 week. Contact Dr John Reid, Consultant Radiologist Borders General Hospital [email protected] 01896 826 421 21 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Dedicated or fast track clinics with rapid reporting Top 20 CID 2 Dedicated Lung Cancer Clinic: Patients attending their GP with highly suspicious symptoms suggestive of lung cancer are now directly referred to the dedicated Lung Cancer Clinic at the Western General Hospital, Edinburgh. Making It Happen At a process mapping event for lung cancer service in the Western General Hospital Edinburgh, it was recognised that several delays occurred for patients suspected of lung cancer receiving their first appointment with the respiratory physician. A dedicated lung cancer clinic for patients referred with suspicious symptoms was implemented. Previously, the chest clinic was held on a Monday morning when the radiology department was working to maximum capacity, catching up with weekend work and added pressure/demand from patients being sent from the clinic. This meant that sometimes arrangements had to be made for patients to return on a different day for their CT Scan. Holding the clinic on a Wednesday has ensured that patients have a CT scan on the same day as attending the clinic. The radiologist discusses scan results with the physician and patients are given results at their clinic appointment, ensuring a rapid diagnosis. Clinical nurse specialist clinic attendance means prompt advice and support can be implemented when the patient is given the diagnosis. Implementation Referrals to the dedicated lung clinic are made by fax/phone to the lung physician secretary who provides an appointment for the next lung clinic, in some cases the next day. Information is also provided for the patient at this stage. Having this speedy referral process to the specialist clinic means that referral to the Multi-Disciplinary Team meeting (where each case is discussed and treatment plans are decided) is quicker and patients receives their treatment options promptly. Prior to implementation of the clinic, the % of patients referred to treatment within 62 days is shown in the table below. The clinic was fully implemented in August 2004 (3rd quarter). The 4th quarter demonstrates a significant increase in this percentage. DEDICATED LUNG CANCER CLINIC – WESTERN GENERAL HOSPITAL EDINBURGH Quarter in 2004 % of patients from referral to 1st treatment 1ST 48.5% 2ND 58.5% RD 3 4TH 64.7% 92.3% The change was implemented in August 04 and 4th quarter measurement above is for period 1/10/04 – 31/12/04. Impact Patients now have a CT Scan while attending the dedicated clinic. Clinical nurse specialist support is available for the duration of the clinic. Patients with suspicious symptoms are seen much quicker. Change impacts and benefits approximately 372 patients a year referred to the service. Contact Dr Ron Fergusson, Consultant Respiratory Physician Western General Hospital, Edinburgh [email protected] 0131 537 1779 22 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Dedicated or fast track clinics with rapid reporting Top 20 CID 2 In Highland, the Nurse Endoscopist has changed the way she works to enable her to work in endoscopy every day undertaking investigations for patients referred with colorectal symptoms. This allows her to attend and contribute to the weekly meeting where staff discuss all patients diagnosed with colorectal cancer and decide upon a treatment plan for each patient. Making It Happen The nurse endoscopist can: Prior to the change the Nurse Endoscopist undertook colonoscopy investigations working alongside a consultant, on a part time basis, at a rectal bleeding clinic. This working arrangement did not allow her to attend the weekly multidisciplinary meeting where the colorectal team discuss all patients diagnosed with colorectal cancer and decide upon a treatment plan for each patient. now attend the weekly multidisciplinary meeting and contribute to the patients treatment plan now undertake an extra 12 colonoscopy investigations a week. This has happened as a result of a consultant freeing up sessions to undertake different work This meant the nurse endoscopist could not input to the discussion to decide the best treatment plan, despite being the person undertaking the investigation that diagnosed the cancer. able to undertake additional colonoscopies when other sessions in endoscopy are cancelled as a result of consultants annual leave or their emergency on-call commitments This was highlighted at a mapping event with the colorectal team and after discussion with the manager, funding was made available to let the endoscopy nurse work full time. implement a Nurse led colonoscopy service and communicate results of investigation to patients on the same day Contact Impact Isla MacDonald, Nurse Endoscopist Raigmore Hospital, Inverness [email protected] 01463 704 000 The benefits from this change have been: 23 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Dedicated or fast track clinics with rapid reporting Top 20 CID 2 In Dundee, doctors, nurses, radiologists and admin staff are working together to reduce the time to diagnosis for patients with frank haematuria. Patients are receiving all of their investigations at one visit instead of three or more. Making It Happen Prior to the change, patients were required to visit the hospital on several occasions to see the Hospital Specialist and receive 3 separate investigations in order to receive their diagnosis. Time to diagnosis for patients has been reduced Reduced number of visits to hospital for patients Co-ordinated approach to care, ensuring patients know exactly what is happening next and when Elimination of delays between investigations and diagnosis This method built in a considerable delay for the patient and the time to diagnosis and subsequent treatment could be significant. The urology team were keen to improve the time to diagnosis for patients and reduce the number of visits to hospital. The fast track system for patients with frank haematuria has been tested and implemented in Dundee. 3 clinics per week are now run seeing 3 patients each day. The patients receive information leaflets and an appointment card with times to arrive at ultrasound and then endoscopy for their tests. At the end of their tests the nurse specialist and consultant will discuss with the patient their next steps. Next Steps Ensure sustainability of service. Continued review of process to ensure minimum waiting times for investigations are achieved. Spread of service to Perth and Angus. Potential for Nurse Specialist to contact patients with negative results by telephone to minimise outpatients appointments and delay to receiving results for patients. Implementation Advice Communication between Radiology, Endoscopy and the Urology Team is vital for the smooth running of the clinic for patients. Contact Impact Mr Chris Goodman, Consultant Urologist Ninewells Hospital, Dundee [email protected] 01382 660 111 The benefits from this change have been: Reduction in time to diagnosis for patients with frank haematuria from an average of 90 - 30 days 100 90 80 70 Delay - Diagnosis to informing patient Delay Ultrasound to Intravenous Ultrasound Delay flexible cystoscopy to ultrasound scan Delay received to flexible cystoscopy Delay referral to received Days 60 50 40 30 Ninewells Hospital and Medical School, Dundee, Scotland 20 10 0 Before After 24 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Dedicated or fast track clinics with rapid reporting Top 20 CID 2 Rapid PSA Reporting – Prostate Specific Antigen: In Oban, all patients being referred to the nurse led prostatic assessment clinic have a routine PSA blood test. This now means that patients are seen 1 week sooner. Making It Happen Reduction of 8 days reporting PSA blood samples Blood testing for PSA levels could be carried out by the GP prior to a clinic appointment or at the first consultation at the prostatic assessment clinic. No. of Weeks 5 Before, all primary care blood samples came into laboratories at Oban hospital before being transferred to a Paisley hospital for testing. This procedure took on average 10 days and was reported by mail. 4 3 2 1 Laboratory staff investigated other more efficient ways of testing and reporting PSA blood samples. Impact The benefits from this change are: A reduction of 8 days in reporting PSA blood samples Next day electronic reporting for blood tests A reduction of 2 weeks delay towards diagnosis for patients Contact Rosemary Noon Urology Nurse Practitioner, Vale of Leven Hospital [email protected] Tel: 01631 789059 25 ug us t A Ju ly ay M Month (2005) Implementation Advice Ju ne M Following consultation with other hospitals, the procedure to test and report PSA was changed and the samples were sent to another Argyll and Clyde laboratory where the results could be reported electronically. A pr il ar c h 0 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Dedicated or Fast-track clinics with rapid reporting Top 20 CID 2 In Glasgow, within urology services, a multidisciplinary team are working together to reduce the time to diagnose patients with frank haematuria. This change resulted in several improvements for patients. Making It Happen • At a Cancer Service Improvement Programme (CSIP) mapping event it was highlighted that urology patients were required to visit their local hospital several times to see a doctor and have tests. Each visit was to a different department and patient information and support services were not coordinated. Elimination of delay between investigations Reduced number of visits to hospital departments Improved communication and support systems for patients Improved communication and coordination between departments • • • Staff decided to develop a one stop fast track haematuria system where patients could be seen quickly and diagnosed in 1 day. Reduction of 3 months to diagnosis 100 90 80 70 60 50 40 30 20 10 0 1 day Se pt us t ug ly A Ju ne Ju A pr il 1 clinic a week is run with 5 patients every day. The patients receive detailed information leaflets with their appointment card explaining the diagnostic tests and format for the clinic. • Every patient sees a specialist nurse who performs a full assessment and gives the patient a support phone number. • Patients have a consultation with results and next steps before leaving the urology department = 1 ay • 90 days M No. of Days The urology, radiology and primary care teams were keen to develop a team diagnostics approach where patients would undergo all three diagnostic procedures in one day and information and communication would be coordinated. Month (2005) Next steps Since this is a new service, reviews will be 3 monthly, assessing capacity and demand to ensure sustainability of service. Contact Mr Naeem Akhtar – Consultant Urologist [email protected] tel 0141 201 1100 Dr Paul Duffy – Consultant Radiologist [email protected] tel: 0141 201 1558 Sister Una Daly [email protected] tel : 0141 201 1559 Dr George Barlow – GP [email protected] 0141 427 1581 Implementation Advice A multidisciplinary steering group was formed. Precise preparation and collaboration is essential. The lead cancer Gp was instrumental in gaining primary care support and formulating policies to inform and guide primary care staff. Impact The benefits from this change are: • Reduction of on average 3 months to diagnosis for patients 26 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Reduce consultant vetting of investigation requests Top 20 CID 3 Daily vetting of radiology requests: In Dumfries and Galloway, radiology requests are vetted by a radiologist on arrival in the department, reducing delay to investigation and diagnosis. Making It Happen Impact At the process mapping event the team identified that radiology request could sit in the radiology department for 2 – 3 days before being seen by a radiologist for prioritisation. This was adding a delay of 2 – 3 days for patients to have their investigations carried out and to start their treatment. Now when radiology requests arrive in the department, clerical staff ensures that they are seen by a consultant radiologist the same day. An appointment is made, patients have their investigation carried out, diagnosis is made and treatment can begin 2 - 3 days sooner than before. Radiology Request Radiology Wait for vetting Appointed Request Investigation Vetted same day Appointed Investigation 2- 3 days This change has benefited ALL patients requiring urgent radiological investigation. The consultant radiologist discussed this problem with the team & it was agreed that the clerical staff would show referrals to a consultant radiologist when they arrive in the department so that appointments can be made 2 – 3 days sooner. In tandem with many other improvement ideas implemented in Dumfries & Galloway’s for patients with suspected gynaecological cancer, this system has helped to achieve 92.9% of patients with ovarian cancer being treated within 62 days of GP referral. Prior to working with CSIP to redesign the service only 72.7% of patients met the target – an increase of 20.2% since 2002. Implementation Advice This was very easy to implement by consultation & communication to ensure that the whole team were aware of the new process. Contact Sustainability should be monitored by audit so that any slippage can be immediately rectified Dr David Hill, Consultant Radiologist Radiology Department, Dumfries and Galloway Royal Infirmary [email protected] 01387 246 246 27 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Telephone consultation/communication of results Top 20 CID 4 In Dumfries and Galloway, the radiologist has developed a system to ensure that the GP is informed of a negative report following radiological investigations, requested by a hospital consultant. Making It Happen The radiologist developed a process within the department at Dumfries and Galloway Royal Infirmary to ensure that the negative report is sent to the GP at the same time that it is given to the referring consultant. Prior to this change, the information was communicated by letter from the consultant, after receiving the report from the radiologist. Impact This reduces the delay for patients being given results. GPs now receive notification of results 7-10 days sooner, than prior to the change. Contact Dr David Hill, Consultant Radiologist Radiology Department, Dumfries and Galloway Royal Infirmary [email protected] 01387 246 246 28 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Telephone consultation/communication of results Top 20 CID 4 In Paisley, nurses and doctors can now obtain urgent test results within 48 hours. This happens by phoning the laboratories in Glasgow rather than waiting for up to 7 days to receive written reports. Making It Happen Prior to the change, it was identified at a process mapping event that there was a delay in receiving blood results form the laboratory in Glasgow. This was caused by the time taken to post them form Glasgow to Paisley. The doctors required to have these results available before patients with gynaecological cancer could start their treatment. It took up to 7 days for these results to be posted. Implementation The doctor in Paisley wrote to all other doctors to ensure they mark the blood tests ‘urgent’, and to inform them of a telephone number to call for results within 48 hours, instead of waiting for the written results in the post. This information is also displayed on a sheet within easy access in the Gynaecology wards. Impact All consultants now know to telephone the Glasgow laboratory for urgent results within 48 hours, and patients do not have to wait so long for their results. Patients can be presented earlier at the Multidisciplinary Team Meeting (MDT) and therefore have their treatment started earlier. Reduction in delay of up to 5 days. Contact Dr Laura Cassidy, Consultant Gynaecologist Royal Alexandra Hospital, Paisley [email protected] Tel : 01475 504 839 29 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Telephone consultation/communication of results Top 20 CID 4 In Tayside, the colorectal clinical nurse specialist telephoned and sent letters to patients at home who had waited the longest for an out patient appointment after being referred by a GP with colorectal symptoms. This reduced the time patients had to wait to be seen at hospital. Making It Happen The benefits from this change have been: At a CSIP colorectal service mapping event it was discovered that there were 460 patients listed on an out patient electronic system, waiting to be allocated an appointment, with the longest waiting 15 months. Combined with colorectal patient and carer interviews: “Unhappy at the time I had to wait to be seen at The number of patients waiting was reduced from 463 to 5 The maximum wait was reduced from 15 to 1 month The percentage of patients achieving the 62 day target from GP referral to first treatment has increased from 60% to 80 % hospital after referred by GP” (6 months) Increase from 60 - 80% of patients treated within 62 days from urgent GP referral to 1st treatment 1.2 Implementation Advice 1 0.8 Percentage The Colorectal Clinical Nurse Specialist (CNS) telephoned the first 25 patients who had waited the longest, then a letter was sent to the next 200 patients. The patients were all asked if they would like a telephone consultation by the CNS and then they were either given an appropriate out patient appointment or sent for an investigation, all this was coordinated by the CNS. 0.6 0.4 0.2 The CNS found this to be time consuming at first but felt it was a worth while exercise as she is now fully aware, and has become much more involved in the referral process and complete patient journey. 0 Jul - Sept 04 Mar-05 Months May-05 Reduction in waiting time from 15 months to 1 month for first out patient appointment 500 Implementation of new, nurse led, out patient clinics in Dundee and Angus. 463 Contact 400 Number of patients 350 300 Jackie Kerrigan, Macmillan Colorectal Nurse Specialist Ninewells Hospital, Dundee [email protected] 01382 425 563 290 250 220 200 190 Page 150 100 70 50 40 25 5 0 Jan-2004 Feb-2004 Mar-2004 Apr-2004 May-2004 Month Jun-2004 Jul-2004 Jul-05 Ninewells Hospital and Medical School, Dundee, Scotland Next Steps Impact 450 Dec-04 Mar-2005 Ninewells Hospital and Medical School, Dundee, Scotland 30 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Telephone consultation/communication of results Top 20 CID 4 Telephoning patients to tell them their appointment details for the multidisciplinary clinic has eliminated a potential delay of 7 days for patients starting their cancer treatment. Making It Happen In Fife, a Clinical Nurse Specialist noticed that several patients were not attending the multidisciplinary clinic & discovered this was because the appointments were being posted to patients too late for them to be able to attend. This caused a delay of 7 days in patients starting their treatment for cancer. This problem has been easily resolved, the Clinical Nurse Specialist now gets a copy o the list of patients due to attend the clinic, she then telephones the patients at home to inform them of the date and time of their appointment. She also makes sure they have transport organised to attend the out patient clinic. Impact The benefits of this change are: • • • No patients have missed their out patient clinic appointment All patients are now starting their treatment up to 7 days earlier This change, along with several other improvements, has contributed to 100% of patients with ovarian cancer meeting the 62 day target Contact Jane McCafferty, Gynaecology Clinical Nurse Specialist Forth Park Hospital, Kirkcaldy [email protected] Tel : 01592 643355 31 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Specialist nurse-led clinics Top 20 CID 5 In Inverclyde, the colorectal nurse specialist has increased the capacity of the out patient clinic by establishing her own out patient service for patients with low risk colorectal symptoms. Making It Happen Prior to the change, all patients referred to the hospital with colorectal symptoms were seen by a doctor. After a process mapping event, it was highlighted that the current wait to be seen by a doctor was 11 weeks. A nurse led clinic was established for patients referred by their GP with low risk colorectal symptoms. All referrals are still vetted by a doctor and then suitable patients are allocated a time see the specialist nurse. This new nurse led clinic runs fortnightly alongside the doctor’s clinic. Impact A patient survey was carried out and patients said: “we are very pleased with the service they received from the nurse” The specialist nurse can see an additional 4 patients every 2 weeks The waiting time for this new nurse led clinic is approximately 1 month less than the wait to see a doctor. Patients are satisfied with nurse led service. Contact Iain Watt, Consultant Surgeon Inverclyde Royal Hospital, Greenock [email protected] 01475 633777 32 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Specialist nurse led clinics Top 20 CID 5 In Highland, doctors and nurses worked together to develop a new specialist nurse clinic. Patients who previously had colorectal surgery now have a check up by the consultant and then are seen at agreed regular intervals by the colorectal specialist nurse for continued routine checks. The colorectal specialist nurse has also improved the way she communicates with the GP after the patient has had surgery for colorectal cancer. Making It Happen Prior to the change, all patients who had colorectal surgery were seen by the consultant for their routine post surgery check and at each follow up appointment. The colorectal clinical nurse specialists (CNS) have undergone extra training and follow new procedures and protocols written in conjunction with the colorectal consultant. This has enabled them to now review patients at agreed intervals following colorectal surgery. This change has freed up clinic spaces in the outpatients clinic, enabling the consultant to see additional new patients. Impact The colorectal patients continue to benefit from a multidisciplinary team approach after their surgery and are aware that they will have regular follow up appointments with support and guidance from the clinical nurse specialist. Specialist nurse led clinics Top 20 CID 5 The colorectal specialist nurse has also improved the way she communicates with the GP after the patient has had surgery for colorectal cancer. Making It Happen Before the change the nurses and the doctors each sent a separate letter to let the GP know that their patients had been in hospital and were now discharged following their operation in Raigmore Hospital. This was a result of the nurses not having access to the electronic system the doctors record the information after surgery that the GP required. used to After a process mapping event the nurses gained access to this electronic system and add information to the same letter the doctor uses. Impact This had resulted in less administration time for the nurse and will allow GP’s to get information they need to care of the patients at home more quickly. Contact Mr James Docherty, Colorectal Surgeon Raigmore Hospital, Inverness [email protected] 01463 704 000 33 CANCER SERVICE IMPROVEMENT PROGRAMME EXAMPLES OF CHANGE Reduce follow-up appointments at outpatient clinics Top 20 CID 6 In Highland, the nurse endoscopist now telephones patients at home after an endoscope investigation to ask how they are feeling. This now means that patients do not have to come back to the out patient department in the hospital for a check up. 1 to 1 consultation with no interruptions or observers i.e. medical students Making It Happen Prior to the change, all patients who had undergone an endoscope investigation was given an out patients appointment to return to the hospital for a routine check up. It was discovered that when the patients attended for this check up, they were asked how they were feeling and if fine were discharged from the hospital back to the care of their GP. No further examination and no time limits on consultation Impact on service Increased capacity in the out patient clinic by 3 to 4 appointment slots per week, allowing the doctors to see additional new patients The nurse endoscopist commented: The nurse endoscopist now asks the patients after their investigation and before they leave the hospital whether they would agree to her phoning them at home to ask how they are feeling instead of an additional out patients’ appointment. “Can give more advice and reassurance” The nurse has a record of what type of investigation the patients had and uses structured questions when telephoning the patients at home, three months after their investigation. “Patient always thanks me for phoning them” Comments from patients include: Next Steps “Good, does that mean I don’t have to come back?” A new information leaflet has been developed and will be given to patients before they leave the hospital. This will explain the new telephone consultation and will include the contact details of the nurse endoscopist. Impact for patients Patient now aware what the next step is Patients don’t have to travel back to the hospital for their check up “Patients are much more relaxed and cooperative when at home Contact Isla MacDonald, Nurse Endoscopist Raigmore Hospital, Inverness [email protected] 01463 704 000 No extra time off work or child care to organise 34 Multi Disciplinary Team (MDT) Multi Disciplinary Team (MDT) “Ensures that a fully informed discussion of all patients diagnosed with cancer takes place and appropriately formulated treatment plan is documented.” 1. Clear responsibility for co-ordination of MDT to ensure all necessary information is available at MDT for treatment decision-making. 2. MDT used to refer on for treatment, i.e. investigations, surgery, oncology. 3. Timely communication with GP of MDT decision. 4. Video conferencing/Telemedicine links to be used where attendance is limited. 35 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Clear responsibility for co-ordination of MDT to ensure all necessary information is available at MDT for treatment decision making. Top 20 MDT 1 In Victoria Hospital, Glasgow, changes have been made to the format for discussing patients and agreeing appropriate treatment plans at the multidisciplinary team meeting (MDT). This has been achieved by doctors, nurses and secretarial staff introducing a proforma to be used when discussing each patient at the weekly meeting. Making it Happen At the weekly multidisciplinary team meeting (MDT) patients who had been recently diagnosed with lung cancer are discussed and an appropriate treatment plan is formulated. Prior to the change, the way in which patients were discussed was not coordinated and each week the meeting ran overtime, not leaving enough time to discuss every patient. This discussion for some patients meant a delay of up to 1 week. Implementation Advice The team developed a proforma sheet that is completed prior to the meeting with all the relevant information needed to make a decision on the next stage of treatment. The form is then updated at the MDT meeting, documenting the agreed treatment plan. This change was reviewed after a few weeks and it was decided to transfer the information collected on the form to an electronic system. This data is now used to review the clinical decision making and outcomes of care. Impact The benefit of this change has been: • All newly diagnosed lung cancer patients are discussed each week without delay Contact Dr Joe Sarvesvaran, Respiratory Physician Victoria Hospital, Glasgow [email protected] 0141 201 6000 36 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Clear responsibility for co-ordination of MDT to ensure all necessary information is available at MDT for treatment decision making. Top 20 MDT 1 Timely communication with GP of MDT decision Top 20 MDT 3 In Grampian, doctors and nurses now meet weekly to discuss all patients who have been diagnosed with upper GI cancer to discuss an individual treatment plan for each patient. They have also developed a new form that is used at this multidisciplinary team meeting to record the decisions made about each patient. This is then faxed to the patient’s GP the next day. This means GP’s now have timely information about their patients which may contribute to improved care for patients at home once they have been discharged from hospital. Making It Happen Prior to this change, there was no formal multi-disciplinary team (MDT) meeting to discuss all patients diagnosed with upper GI cancer and decide on an individual treatment plan for each patient. After a process mapping event, it was suggested that a formal weekly MDT meeting should be established on a Monday. A list of all patients to be discussed is typed and sent the Thursday before the meeting, to all the doctors and nurses who attend. This allows time to prepare the correct documentation required to make the best treatment decision for each patient. A form is used to record decisions and the resulting treatment plan. This is faxed to the patients GP the following day. Impact All patients diagnosed with upper GI cancer are discussed by a multi –disciplinary team and a treatment plan formulated GP’s now have timely information about their patients Next Steps The doctors and nurses from the palliative care team are also to be included in the weekly multidisciplinary team meeting. The weekly list of patients who are to be discussed is to be sent to them also so they can also attend the meeting and input to the patients treatment plan, when required. Contact Mr Ken Park, Consultant Surgeon Aberdeen Royal Infirmary, Aberdeen [email protected] 01224 554 534 37 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Clear responsibility for co-ordination of MDT to ensure all necessary information is available at MDT for treatment decision making. Top 20 MDT 1 Top 20 MDT 3 Timely communication with GP of MDT decision In Tayside, a multi-disciplinary team (MDT) Meeting Co-ordinator has been appointed within each site specific cancer team. The co-ordinator organises the weekly MDT meeting and communicates quickly with the GP about the patient’s treatment options. Making It Happen Previously, the clinical nurse specialist organised the weekly MDT meetings involving multiple administrative tasks and was time consuming. This was identified as an issue at a Cancer Service Improvement Programme cancer team mapping event. patients treatment was agreed, this was a maximum of 40 days. The current cancer audit co-ordinator’s role was expanded to include the organisation and administration of the weekly MDT meeting. The GP now has information to support the care of the patient in the community. The co-ordinator now makes sure that all the patient case notes and relevant investigation results are available for the meeting. Next Steps Now, the GP receives a faxed copy of the form detailing the result of a discussion held at the MDT within 24 to 48 hours. GP’s will be contacted and asked for feedback on the usefulness, content and timeliness of the new faxed forms and comments will be used to further develop and improve the communication with GP’s after the MDT meeting. Once the treatment plan is documented the co-ordinator faxes the plan to the GP as soon as possible after the MDT meeting either on the same day or next morning. This now happens after the breast, lung, upper GI, colorectal and urology cancer MDT meetings. Contact Jillian Galloway, Clinical Team Manager Ward 32, Ninewells Hospital, Dundee [email protected] 01382 660 111 Impact Prior to the change, a small audit was undertaken in one GP practice, looking at the time in days, a letter took to be typed, posted and received within the practice after the 38 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE MDT used to refer on for treatment, i.e. investigations, surgery, oncology Top 20 MDT 2 Introduction of the MDT electronic proforma on the Clinical Oncology System (COS)/LINX System has improved the management of the lung cancer patients meeting, held in the Western General Hospital, Edinburgh. Making It Happen Prior to the change, it was difficult for those attending the MDT meeting to follow instructions and decisions. Collaboration between IT personnel and the clinical team enabled the development of an electronic MDT form. Impact The COS system is displayed on the wall for all participants to see during the MDT meeting. This allows the decisions and treatment options for the patient to be recorded during the meeting. This provides a much more cohesive approach to decision making at the meeting. Contact Richard Renton, Clinical Systems Analyst The Royal Hospital for Sick Children/Lothian University Hospitals Division [email protected] 0131 536 0060 39 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Timely communication with GP of MDT decision Top 20 MDT 3 In Fife, all patients with gynaecological cancer are discussed at the weekly multi-disciplinary team (MDT) meeting in the Edinburgh Cancer Centre. The clinical nurse specialist (CNS) now faxes a copy of the MDT decision to the patients’ GP to ensure seamless & timely communication. Impact Making It Happen Prior to the change, the team identified that GPs were not being informed of the decision made at the gynaecology MDT until several weeks later. This lead to a lack of continuity & support for patients at a crucial stage in their pathway. Patients often contact their GP to ask for news from the hospital about their results & what treatment they need. Better informed GPs, improved knowledge of treatment plans and the stage of patients’ pathway Better informed reducing anxiety. patients & Contact This problem was discussed by the team but without an MDT co-ordinator it was difficult to decide who should be responsible for undertaking the task of faxing the MDT proforma to the patient’s GP. The CNS for Fife was keen to improve communication for her patients so a PDSA (plan, do, study, act) cycle was developed to test the change. Jane McCafferty, Clinical Nurse Specialist Forth Park Hospital, Kirkcaldy [email protected] 01592 643 355 Now the Fife CNS, who attends the meeting every week, sends a copy of the MDT proforma by fax to her patients’ GP and the referring gynaecology oncologist in Fife. Implementation Advice Although this is essentially an administrative task, it does have significant clinical implications for patients and helps to improve communication between the hospital and the GP. Ideally this task should be done by an MDT co-ordinator but if none is available, it is important to gain commitment from another team member to ensure that GPs are informed quickly what the next steps are for their patients. 40 carers, CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Video conferencing/telemedicine links to be used where attendance of at MDT’s is limited Top 20 MDT 4 In Tayside, the day, time and venue for the uro-oncology weekly multidisciplinary team (MDT) meeting has been changed to facilitate weekly participation of consultant staff in Perth and Stracathro via teleconferencing. Making It Happen Previously, the consultant urologists in Perth and Stracathro could only attend the MDT meeting held in Dundee on a 4 weekly basis due to other clinical commitments. This meant that their patients case notes and information had to be sent to Dundee for discussion at the MDT by their consultant colleagues. This was unsatisfactory from a full discussion of patient diagnosis and treatment by the referring consultant and from a teaching perspective. In addition, delays/issues with a transfer of case notes between sites caused subsequent delays for patients at clinics. Following a process mapping event, where these issues were again highlighted as problems for the service, the team agreed to review the MDT arrangements. The day and timing of the weekly meeting has now been changed to allow consultants from all 3 sites to participate via teleconferencing. The venue of the meeting has also been changed to facilitate this with the potential to move to video conferencing in the near future. Impact All urology consultants can attend the weekly MDT meeting facilitating full and early discussion of all patients with urological cancer and their future treatment plans. Patient case notes are no longer transferring between sites thus minimising potential delays for future clinic appointments. Next Steps Continue to monitor the attendance at the MDT meeting to ensure the change is an improvement. Move to video conferencing to further facilitate discussion and contact between sites. Contact Mr Chris Goodman, Consultant Urologist Ninewells Hospital, Dundee [email protected] 01382 660 111 41 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Video conferencing/telemedicine links to be used where attendance at MDT’s is limited Top 20 MDT 4 Electronic transfer of radiological images: Radiological images are electronically transferred to the Western General Hospital from St John’s Hospital to ensure the appropriate images are available for use at the weekly lung multi-disciplinary team (MDT) meeting. Making It Happen Prior to the change, the radiological team at St Johns Hospital in Livingston saved duplicated images to CD-ROM for the consultant to take to the MDT meeting at the Western General Hospital in Edinburgh. Before this change, the consultant was required to carry all images to Edinburgh for the meeting. If all images were not available, discussion might be delayed until the following MDT meeting. This process always had the potential to miss the crucial image if a complete compliment of images were not available and included. Discussion with the Information Technology Department was undertaken to establish if radiological images could be transferred to the Western General Hospital from St John’s Hospital in Livingston. Implementation Advice This was not an easy change to achieve. Full discussion with the IT department was necessary to take it forward. Impact The change now ensures that all images are available for the weekly MDT meeting and allows full discussion of the patient removing any potential delay in the journey. Contact Diana Borthwick, Clinical Nurse Specialist Lung Cancer Support Wetern General Hospital, Edinburgh 0131 537 1767 42 Treatment Treatment “No needless delays.” 1. Co-ordination of treatment processes across network to ensure optimum use of capacity, e.g. theatre time. 2. Planned management of annual leave and public holidays. 3. Streamlining of booking processes for chemotherapy and radiotherapy. 4. Efficient system for appropriate referral to palliative care. 43 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Improved communication Top 20 Treatment In Dumfries and Galloway Royal Infirmary the clinical nurse specialist, for colorectal cancer has developed a process for alerting the team if a patient is admitted with medical problems during their chemotherapy treatment plan. Making It Happen Prior to the change if patients undergoing chemotherapy were admitted to the hospital with medical problems this could result in potential difficulties if the information was not communicated to the chemotherapy team. The clinical nurse specialist developed a system to ensure that patients undergoing chemotherapy who were admitted to the hospital with medical difficulties were brought to the attention of the chemotherapy team. This is done by placing a sticker on the front of the case note, at the beginning of chemotherapy treatment, indicating where staff can obtain advice regarding the patient’s chemotherapy status. This system has been disseminated to a wide range of staff over 2 hospital sites to ensure compliance when patients are admitted. Impact This ensures that patients receive prompt care when abnormalities occur. Prior to this change it was difficult to track patients if they were having problems. Now problems can be resolved much more quickly if they are communicated to the team. Staff anxiety has been reduced, as they can contact another member of staff for advice and support when the patient is admitted between their chemotherapy sessions. Contact Isabel Williams, Colorectal Nurse Specialist Dumfries and Galloway Royal Infirmary [email protected] 01387 244 288 44 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Co-ordination of treatment processes across network to ensure optimum use of capacity. Top 20 Treatment 1 In Aberdeen, doctors and managers have reduced the time it takes to have an operation after being diagnosed with colorectal cancer. This was achieved by coordinating the time available for doctors and arranging a suitable day and time for patients to have their surgery. Making It Happen Prior to the change, the maximum time patients had to wait for their surgery after being diagnosed with colorectal cancer was 3 months. Following a colorectal team process mapping event, a PDSA (plan, do, study, act) improvement was tested whereby a manager agreed to be the central point of contact and co-ordinate the date and time of surgery, when patients were referred to a doctor for colorectal surgery. Previously, two doctors were undertaking the majority of the surgery and after discussion, it was agreed that an additional doctor would also be responsible for this work. The manager now receives the details of all patients referred to the colorectal service for surgery and co-ordinates which doctor the patient will see at the outpatient clinic and which doctor will carry out the resulting surgery. Impact This managed co-ordination has now reduced the wait for patients receiving surgery from 3 months to 2 weeks. Contact Mr Terry O’Kelly, Consultant Surgeon Aberdeen Royal Infirmary, Aberdeen [email protected] 01224 554 534 45 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Co-ordination of treatment processes across the network to ensure optimum use of capacity, e.g. theatre time Top 20 Treatment 1 In Ninewells Hospital, Dundee and Borders General Hospital, improved communication between the specialist nursing staff and the surgical team in Edinburgh is ensuring that patients referred for surgery, but who are not suitable, are urgently referred back to their local team for discussion and commencement of alternative treatment. This ensures that patients are not left waiting for a number of weeks before knowing what treatment they can pursue and also ensures patients receive appropriate support and information during this time from the Macmillan lung cancer nurses. Making It Happen Impact Prior to the change, patients who were referred to Edinburgh as potential surgical candidates but who were subsequently found to be inappropriate, had to wait several weeks for a follow up appointment locally and the time to commencing alternative treatment could be significant Time to treatment following positive mediastinoscopy 40 35 30 25 Days 20 15 10 Following the identification of this issue at the lung team mapping event, the lung specialist nursing staff agreed with the thoracic surgical team, that a telephone call would be made on the day of the test result which ruled out surgery to advise of this. The lung specialist nurse then ensures that the patient receives the next available appointment with the local clinician and is further discussed at the multi disciplinary team (MDT) meeting to decide on an alternative method of treatment. The lung nurse specialist then contacts the patient directly and informs of their next appointment and the next steps in the process for them. 5 0 Nov-03 Dec-03 Jan-04 Feb-04 Mar-04 Months The benefit from this change has been Patients who are not suitable for surgery are getting back into the local system more quickly and minimising time to treatment Patients are informed as early as possible of the results and the next steps for them Local support, information/advice is in place for patients from the lung nurse specialist Implementation Advice Next Steps Good communication between the two teams to minimise time to treatment. Ensure maintenance of this communication system between the two teams. Contact Lynn McAllister, Lung Cancer Specialist Nurse Ninewells Hospital, Dundee [email protected] 01382 660 111 46 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Co-ordination of treatment processes across network to ensure optimum use of capacity Top 20 Treatment 1 Top 20 Treatment 2 Planned management of annual leave and public holidays The South East of Scotland Cancer Network’s (SCAN) gynaecology cancer team ensure that expert gynaecology oncology treatment is co-ordinated across the network. Making It Happen Process mapping of the pathway of patients with gynaecological cancer took place in all SCAN regions during 2003 – 2004. At each mapping event the teams identified that if the local gynaecologist was absent, patients had to wait until they returned for their surgery to take place, this could be up to 21 days. In addition, if a consultant was absent, his or her theatre list was often not used. Implementation Advice This change requires consultation, commitment & co-operation between managers, doctors & nurses across the network. Impact The SCAN gynaecology lead estimated that this reduction in capacity could be met by consultants within the network working as a ‘team’ Through consultation & agreement within the network, delays to surgical treatment have now been reduced by consultants working across the network. Formal arrangements are in place for consultants from Lothian to operate on patients in their local hospital or for patients to have their surgery in Edinburgh. Reduction of up to 21 days in wait for surgery Patients being operated on locally whenever possible – less travelling for patients & carers True spirit of network working Less waste of theatre capacity Better communication Contact The waste of theatre capacity when consultants are absent has also been addressed. Consultants now advise one another when they will not be using their list so that the theatre time can be used by their colleagues. Dr David Farquharson, Clinical Director Centre for Reproductive Health, Edinburgh Royal Infirmary, Edinburgh [email protected] 0131 536 1000 47 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Streamlining of booking processes for chemotherapy Top 20 Treatment 3 In Dundee, nursing and administration staff now have a weekly discussion about the numbers of patients who currently receive, and those who are waiting to start their chemotherapy. This meeting is arranged to maximise the current slots used for chemotherapy within two areas of the hospital, and to reduce the time patients have to wait to receive their chemotherapy treatment. Making It Happen Percentage of lung cancer patients receiving chemotherapy treatment within local guidelines (increased from 33% to 89%) 1 Within the hospital there are two areas where patients can receive their chemotherapy treatment - a day unit that is open Monday to Friday 9 am to 5 pm and a separate unit open five days a week, day and night. Patients were booked into these two units independently depending on which type of treatment they were to receive. If there was no space in the day unit, the patients had their first treatment in the five day unit, then transferred to the day unit to complete their treatment. 0.9 0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0 Nov-2004 Before the change there was no discussion between the two areas on how many patients were currently receiving treatment and how many where still on a waiting list in each area. Dec-2004 Jan-2005 Feb-2005 Mar-2005 Apr-2005 Ninewells Hospital and Medical School, Dundee, Scotland The time for lung cancer patients waiting to start chemotherapy treatment has been reduced from 21 days to 14 days in four months Waiting time to start chemotherapy for lung cancer patients, 21 days reduced to 14 days Now the nurses in charge of both units meet weekly to plan the number of patients attending for their treatment in each area and try to utilise both areas to their maximum capacity. 25 20 Days 15 Impact 10 In the first 4 months 24 patients have improved benefited from the communication between both areas by completing their treatment in five day area. This has meant the patients see the same members of staff each time and it has increased the capacity in the day area. The percentage of lung cancer patients that now received their chemotherapy treatment within local guidelines has increased from 33% before the change to 89% after the change has been sustained for three months. 5 0 Nov-2004 Mar-2005 Months Apr-2005 Ninewells Hospital and Medical School, Dundee, Scotland Next Steps The existing electronic system used to record completed treatment is being reviewed for use as a booking system to aid the utilisation of both chemotherapy areas. Contact Jackie Davie, Senior Charge Nurse Ward 32, Ninewells Hospital, Dundee [email protected] 01382 660 111 48 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Streamlining of booking processes for chemotherapy and radiotherapy Top 20 Treatment 3 Radiotherapy Planning At the Edinburgh Cancer Centre, in order to optimise patient flow through the system, the ‘plan check’ step has been removed. Patients benefit from one less hospital visit AND can begin their treatment up to 10 days sooner. Making It Happen Before Historically, standard practice when planning radical radiotherapy has been for all patients to have two appointments; one for a planning CT scan and a second for the conventional simulator where the treatment plan is checked and verified (‘plan check’). (isocentre) according to a protocol. This is then marked on the patient with tattoos. Using special planning techniques the treatment is planned around this isocentre. As no ‘isocentre shifts’ occur, (these can be a potential source of errors) once the treatment is planned the patient can commence their radiotherapy. The position of the treatment is verified against reconstructed images from their CT scan (DRRs). Issue(s) As no immediate decisions are necessary, the CT SIM sessions do not require an Oncologist to be present, which increases the flexibility of appointments. Whereas, the conventional simulator sessions require immediate clinical decisions to be made so an Oncologist has to be present. Therefore patients requiring a conventional SIM session to verify their treatment set-up, are given the next available appointment coinciding with the appropriate consultant/team sessions so there maybe be up to 10 days between the two appointments causing a potential delay in the start of treatment. Impact The change has now been implemented for all patients receiving CT planned radiotherapy treatment for tumours in the pelvis. This has This means that patients can begin treatment up to 10 days sooner. From the patient perspective, the change means 1 less appointment for the patient to attend. Further work is on going to assess the feasibility of removing the ‘plan-check’ from other tumour sites such as lung. For example, a patient undergoing radical treatment of prostate cancer may be CT simulated on a Monday and not attend the conventional simulator until the Thursday of the following week during a planned urology session and would start their radiotherapy on the next Monday. Reduction of up to 10 days in wait for radiotherapy Patients also benefit from 1 less visit to hospital Contact Sara Erridge, Consultant Oncologist Edinburgh Cancer Centre Western General Hospital, Edinburgh [email protected] Implementation Advice When introducing any change to the process, it is imperative that no new errors occur. Therefore, a robust process was designed and audited prior to routine introduction. When the patients attend for their planning CT scan, specially trained radiographers establish the likely centre of the treatment volume 49 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Streamlining of booking processes for chemotherapy and radiotherapy Top 20 Treatment 3 At Hairmyres Hospital, the doctor has improved the process for referring patients to the oncology unit. He has done this by ensuring the nursing staff get a copy of all referral letters to enable them to book patients for their treatment immediately reducing the previous delay. Making It Happen Prior to the change, all referral letters were sent to doctors, who were not responsible for undertaking the process of booking patients for their treatment. It was highlighted at a process mapping event that this could cause a delay of up to 24 hours, before doctors passed on the letter to nurses to process. The copy of the referral letter now goes directly to the nurses, as well as the doctors and is now processed immediately. The secretaries now also send a letter back to the referring doctor to advise when the patient will commence their treatment. Impact Patients are now being booked for their treatment to commence 3 days sooner than before. Contact Dr Gary Osborne, Consultant Gynaecologist Hairmyres Hospital, Lanarkshire 01355 585 000 50 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Streamlining of booking processes for chemotherapy and radiotherapy Top 20 Treatment 3 Pre-registration of patients referred to the Beatson Oncology Clinic Timely communication between Lorn and Islands Hospital and the Beatson Oncology Clinic ensures that patients are pre-registered at the Beatson Oncology Clinic, allowing case notes to be available on 1st clinic visit and treatment to be booked up to 1 week earlier. Making It Happen Prior to the change, new patients referred from Lorne and Islands Hospital to the lung team at the Beatson Oncology Centre, were being appointed to the Oncology Clinic without notifying the Beatson Oncology Centre. This resulted in patients attending the clinic prior to being registered with the Beatson Oncology Centre. Since this change has been implemented improved communication takes place between the Beatson Oncology Centre lung secretary and Lorn and Islands hospital staff, prior to each clinic. This means that clinic lists are up to date, each patient is registered and that case notes are available for all patients. Impact Beatson Oncology Centre case notes cannot be compiled until the patient has been registered with the Beatson Oncology Centre. Patients cannot be booked for treatment until they have been registered as a Beatson Oncology Centre patient. The benefits of this change are: • • If the Beatson Oncology Centre lung team were not notified of new patients prior to the clinic, the patient would not be registered; a case note would not be available and the patient could not be booked for chemotherapy or radiotherapy treatment. As such, the patient’s treatment could be delayed by up to 1 week. • Improved communication between Beatson Oncology Centre Lung Team and Lorn and Islands Hospital Patient registered with Beatson Oncology Centre prior to clinic visit allows patient to be booked for treatment up to 1 week sooner Presence of case notes at 1st clinic visit Contact Implementation Advice Christine Douglas, Team Leader, Lung Team Medical Secretaries Beatson Oncology Centre, Glasgow [email protected] 0141 211 2000 To ensure that patients were processed through the system, as timeously as possible, staff at Lorn and Islands Hospital were asked to update the lung secretarial team if they were appointing lung patients to the Oncology Clinic. This enables the lung team to register the patient and ensure that Beatson Oncology Centre case notes are available at the patient’s 1st clinic appointment ensuring the patient can be referred and booked without further delays. 51 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Streamlining of booking processes for chemotherapy and radiotherapy Top 20 Treatment 3 Electronic Access to Pathology Reports: The Lung Secretarial Team at the Beatson Oncology Clinic can now electronically access pathology results for newly referred patients. Electronic access to other hospital pathology results has enabled patients to be appointed to Lung Oncology Clinics up to a 1 week sooner. Making It Happen Prior to the change, on referral to the Beatson Oncology Centre, the lung team secretarial staff were required to phone the referring hospital and request pathology results for the patient. Until these results had been obtained, patients could not be appointed to lung oncology clinics. The secretaries would often spend up to an hour on the phone tracing pathology results. Once the secretary had tracked down the pathology results they would request that these results were faxed to the lung team, to enable the patient to be appointed to the next clinic. Since this change has been implemented, the lung team secretarial staff are able to electronically access pathology results for patients referred to lung oncology. Secretaries are no longer spending time phoning other hospital sites to access these results. The lung team no longer has to wait 2-3 days for pathology results and patients can now be appointed to the next Oncology clinic, as pathology results are instantly accessible. If the results were unable to be faxed they would be sent to the lung team by post. Results that are sent by post can take 2-3 days to reach staff at the Beatson Oncology Centre. Appointments would be made, on the receipt of the pathology results. Consequently, if the results were sent by post, this would often mean that the patient’s appointment at the clinic would be delayed by 1 week as the results had not been received in time to appoint to the next clinic. The benefits from this change are: Impact • • • Instant access to electronic pathology results Secretaries no longer have to phone around hospitals, for results, saving up to 1 hour per patient. Patients can be appointed to next oncology clinic, saving a delay of up to 1 week. Implementation Advice Contact To enable the lung team secretarial staff to overcome the delays in accessing pathology results, it was agreed that electronic access to pathology reports should be provided to the lung secretarial team. This allows secretaries to access and print patient pathology reports from other hospital sites. Tanya McDonald, Acting Deputy Medical Records Manager Beatson Oncology Centre, Glasgow [email protected] 0141 211 2858 52 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Streamlining of booking processes for chemotherapy and radiotherapy Top 20 Treatment 3 Timely delivery of tapes & use of new/review dictation tapes A change of working practice by consultants and secretaries within the Lung Team at the Beatson Oncology Centre, has helped reduce the typing backlog from the 4 weeks to 2 weeks. This is due to the introduction of separate new and review dictation tapes and the timely delivery of tapes after each clinic. Making It Happen This has boosted morale within secretarial teams and consultants are happier with the secretarial service provided. Prior to the change, lung team consultants used the same tapes to dictate new and review patient letters at clinics. This meant that lung team secretaries were not easily able to prioritise their workload. Reduction in typing backlog of tapes reduced from 4 to 2 weeks Furthermore, if secretaries wished to access new patient information they had to play through each tape to source this. In addition, secretaries were often not receiving clinic tapes until a number of days after the clinic had been held. These work practices meant that before the change, a 4 week typing backlog existed. Because of this, case notes were often not up to date at the patient’s next clinic appointment and consultants would be required to phone secretaries and ask them access the information required. Weeks 5 4 3 2 1 0 April May June July Month (2005) Implementation Advice Impact To help eliminate the 4 week typing backlog a number of changes were agreed. The lung team consultants agreed that they would dictate new and review patient letters on separate tapes. The consultants also agreed to deliver these tapes, to the secretaries as timeously as possible after each clinic. The benefits of this change include: • • • • Since these changes have been adopted, secretaries receive tapes after each clinic. Now the lung team secretaries can prioritise new patient dictation which is typed immediately. This means that when patients arrive for their next clinic appointment all relevant and up to date information is filed in the case note. Reduction of existing typing backlog of tapes from 4 weeks to 2 weeks Remove delays in dictation of new patient histories. Ability to prioritise workload Up to date patient case notes Contact Christine Douglas, Team Leader, Lung Team Medical Secretaries Beatson Oncology Centre, Glasgow [email protected] 0141 211 2000 53 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Streamlining of booking processes for chemotherapy and radiotherapy Top 20 Treatment 3 Provision of clear information relating to Outpatient clinics: Patients referred to the Beatson Oncology Clinic now receive clear information relating to their outpatient appointment and to the hospital where the clinic is being held. This has resulted in fewer patient queries to the lung secretarial team and less need for taxis to transfer patients between hospital sites. Making It Happen they have received fewer queries relating to location of clinics. Now staff have reported that they are no longer requiring to order taxis to transfer patients to other hospital clinics. Prior to the change, patients referred to the Beatson Oncology Centre were sent their clinic appointment on Beatson Oncology Centre headed appointment cards. For many patients this was confusing as the clinic they were to attend was being held in their referring hospital. The lung team secretarial staff reported that they were receiving a significant number of telephone queries from patients, asking which hospital the clinic was being held in. Staff also reported that patients often failed to attend their appointment as they were turning up at the Beatson Oncology Centre and not at the hospital where the clinic was being held. This resulted in a taxi being ordered to transfer the patient, or the patient’s appointment being cancelled and rearranged for the following week. Impact The benefits from this change are: • • • Improved communication between Beatson Oncology Centre and patients about follow up appointments Fewer enquiries being made regarding where clinic is to be held. Reduction in the number of taxis used to transfer patient to correct clinic, due to patients now attending the correct hospital site. Contact Implementation Advice To overcome this confusion it was decided to send patient appointments using the hospital headed appointment cards for the hospital where the clinic was being held. Tanya McDonald, Acting Deputy Medical Records Manager Beatson Oncology Centre, Glasgow [email protected] 0141 211 2858 Since this change has been implemented, the lung team secretarial staff have reported 54 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Streamlining of booking processes for chemotherapy and radiotherapy Top 20 Treatment 3 Increase the capacity within chemotherapy unit for patients receiving their treatment as in patients: In Tayside, doctors, nurses and managers have increased the number of patients that can receive chemotherapy treatment while staying overnight in the five day chemotherapy unit within Ninewells hospital. They have done this by introducing an additional chemotherapy out patient service using oral chemotherapy treatment in Perth Royal Infirmary, for patients being treated for colorectal cancer. Making It Happen Prior to the change, all patients who were having chemotherapy treatment for colorectal cancer came to the chemotherapy 5-day unit in Ninewells Hospital, regardless of where they lived, and stayed one or two nights. The chemotherapy was administered to these patients by the use of an intravenous infusion (drip). Percentage of lung cancer patients receiving chemotherapy treatment within local guidelines (increased from 33% to 89%) 1 0.9 0.8 0.7 0.6 0.5 0.4 A new outpatient chemotherapy clinic commenced in Perth Royal Infirmary, January 2005. 0.3 0.2 0.1 0 Nov-2004 This now means that patients who live in Perth or close vicinity can have their chemotherapy treatment for colorectal cancer by taking oral therapy (tablet format) given to them within an out patient clinic setting, instead of the previous intravenous infusion given on an inpatient basis. Jan-2005 Feb-2005 Mar-2005 Apr-2005 Ninewells Hospital and Medical School, Dundee, Scotland Next Steps It is hoped to adopt and spread this change to Ninewells Hospital, Dundee and offer this method of treatment to patients with colorectal cancer who live in Dundee. This will further increase the capacity within the 5-day inpatient chemotherapy unit. Impact Dec-2004 Patients now don’t have to stay overnight in hospital and can have their treatment closer to home in Perth and don’t have to travel to Dundee. Since commencement of clinic in January 2005, 23 patients have had their chemotherapy treatment this way, increasing capacity at Ninewells by the same number. All colorectal patients are now receiving their chemotherapy treatment within local guidelines. This change means the waiting time for chemotherapy for all cancer patients is reduced. Before, only 33% of lung cancer patients received their treatment within local guidelines, compared with 89% after the change was implemented and sustained for three months. Contact Jackie Davie, Senior Charge Nurse Ward 32, Ninewells Hospital, Dundee [email protected] 01382 660 111 55 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Efficient system for appropriate referral to palliative care Top 20 Treatment 4 In Victoria Hospital, Fife, referral to palliative care from the ward or multidisciplinary team (MDT) meeting now takes place on the same day. This removes potential referral delays to palliative care. Making It Happen Prior to this change, patients were referred to palliative care informally. No record of referral to palliative care was kept and no one member of staff was responsible for ensuring that the referral to palliative care was seamless and timely. This meant that problems with referral were often only highlighted once a delay had occurred. Referral to palliative care can be made by ward staff or directly from MDT. The nursing staff or junior doctor is responsible for telephoning the palliative care team with patient details. The referral form acts as a record of this referral and is placed in the patient case record. Implementation Advice It was important to make the ward staff and junior doctors aware of the correct procedures for referral to palliative care. These procedures will be communicated at regular and appropriate intervals to ensure that awareness does not drop due to staff turnover and junior doctor rotation. Impact Staff are now aware of the service provided by the palliative care team. A reduction in patient and staff anxiety. Murdina MacDonald, Lead Cancer Nurse Victoria Hospital, Fife [email protected] 01592 643355 The palliative care team developed a referral form to allow prompt referral to their service. Patients are now being promptly seen by the palliative care team to ensure appropriate care. The potential for blocking beds whilst awaiting palliative care consultation is reduced. Contact This system could allow a potential of 3-4 days delay to occur. 56 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Efficient system for appropriate referral to palliative care Top 20 Treatment 4 In Victoria Hospital, South Glasgow, doctors and nurses have improved access to the specialist palliative care team for patients with lung cancer. The palliative care specialist nurse now attends the weekly oncology ward round where she sees patients who need extra support in dealing with their diagnosis and treatment. This has increased the numbers of referrals to palliative care and the patients are benefiting as a result. Making It Happen It was highlighted at a Cancer Service Improvement Programme process mapping event that cancer patients were not being referred in a timely fashion to the palliative care service for extra support when dealing with their diagnosis or treatment. The oncologist invited the palliative care clinical specialist nurse to join the weekly oncology ward round. The specialist nurse now sees patients while they are in the oncology ward. Impact Staff involved feel there is an improvement in communication and information sharing and as a result referrals to the palliative care service are more appropriate Patients were asked for feedback about benefits of service and two patients recently referred to the service said they felt a benefit and symptom improvement Referral to palliative care have increased by 20% Contact Dr Joe Sarvesvaran, Consultant Respiratory Physician Victoria Hospital, South Glasgow [email protected] 0141 201 6000 57 CANCER SERVICE IMPROVEMENT PROGRAMME - EXAMPLES OF CHANGE Efficient system for appropriate referral into palliative care Top 20 Treatment 4 Nurse referral to palliative care has reduced a delay of 3 days for patients to receive treatment. Making It Happen In Fife there was a delay of 3 days for patients to be referred to the palliative care team from the gynaecology ward. This was because referral to this service could only be made by doctors. Doctors & nurses got together to agree on a system to eliminate this delay. The solution was simply to allow the clinical nurse specialist and the charge nurse to make the referral to the Specialist Palliative Care Team immediately after the ward round. The team have also developed a responsive patient pathway to ensure that the multidisciplinary team refer appropriately to either the gynaecological oncology nurse or the palliative care service. An education programme is also planned for all staff and will include these referral protocols. Impact The benefit of this change has been: • Patients are now seen by the palliative care team 3 days sooner • This change, along with several other improvements, has contributed to 100% of patients with ovarian cancer meeting the 62 day target Contact Jane McCafferty, Gynaecology Clinical Nurse Specialist Forth Park Hospital, Kirkcaldy [email protected] Tel: 01592 643355 58 Cancer Service Improvement Programme – Contacts Further information about the work of our programme is available on our website www.cci.scot.nhs.uk (click on National Programmes). Information you will find includes, conference write ups, presentations, publications, access to a wide variety of information and useful links to other work. Any member of the team would be happy to answer queries and provide further contract details and advice. Contact details for the Cancer Service Improvement Programme Team are below: Contact Details Programme Manager: Pauline Ferguson t. 07786 661937 e. [email protected] Information Manager: Marese O’Reilly t. 0141 249 6562 e. marese.o’[email protected] Regional Facilitators Dawn Sturrock t. 07717 422367 e. [email protected] Lynn Smith t. 07717 422362 e. [email protected] Louise Hamill t. 07717 422366 e. [email protected] Margaret Kelly t. 07717 422368 e. [email protected] Gordon McLean t. 07717 422363 e. [email protected] Information about CSIP and other CCI National Programmes is available at www.cci.scot.nhs.uk 59 ISBN 0-7559-4758-4 © Crown copyright 2005 Please visit our website www.cci.scot.nhs.uk click on national programmes then cancer service improvement programme Astron B42431 11/05 w w w 9 780755 947584 . s c o t l a n d . g o v . u k
© Copyright 2026