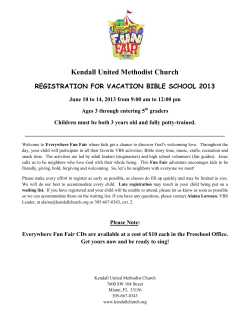
living wills how to ensure your wishes are known when you can no
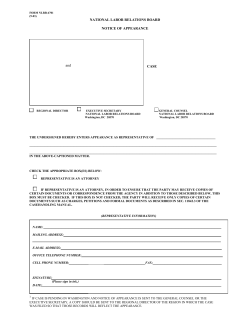
living wills how to ensure your wishes are known when you can no longer make yourself understood what do you need? a lasting power of attorney, living will or advance statement? a draft living will form for your use also informed consent to treatment why it is important do not resuscitate orders their implications for patients and family What is The Patients Association? Our Aims The Patients Association listens to the concerns of patients and focuses all its work on what matters to them. We are the first port of call for many who seek help with their health care problems. We aim to empower them to make informed choices and speak up for themselves with confidence and conviction. The Patients Association, established in l963, is a national voluntary organisation and registered charity. It is run by an elected Council and is completely independent of government, although we work with them on specific projects for a better and more responsive service. • “listening to patients and speaking up for change” The NHS exists for patients; it is there to serve them. We represent all patients – and we are all patients sooner or later. What can we do for you? • Advice to patients through fact sheets, good practice material and self-help guides • Speak up for patients to government, health professionals and managers and elected representatives from Westminster to local councils • Campaign for improved health services from the patient’s point of view so that a consumer-led health system provides the most effective and efficient service • Provide individual confidential practical guidance on all health services whether NHS or private • Provide a platform for patients to influence the health agenda of the UK through our regular Taking the Pulse surveys • Publish accurate up to date advice through our library of information • Speak up for change to the media on the basis of what you tell us • Offer local activities through our Eyes and Ears health network • Convey your views to other charities through our Network for Patients Please note that we cannot give clinical advice Join us at www.patients-association.com or call 0208 423 9111 Helpline 0845 698 4455 1 Contents 2 Consent to treatment 4 Do not resuscitate orders 20 What is it? What the law says 4 What does DNR mean? 20 What information do I need? 4 When does it happen? 20 Who should provide it? 5 What risks should I know about? 5 Should the family be consulted? 20 What about my specific questions? 5 Appropriate use of DNR’s 21 Questions to ask your Doctor 5 Who takes the decision? 21 Can I refuse treatment? 6 Safeguards 21 Can I insist on specific treatment? 6 What if I lost the ability to make decisions for myself? 6 Useful addresses 22 Can children make decisions about medical treatment 6 What does a consent form look like? 7 Draft Living Will form 24 Living Wills 12 What are they and why are they important? 12 How the Mental Capacity Act 2005 changed things in England and Wales 12 What happens in Scotland and Northern Ireland? 13 Powers of the Court of Protection 14 Lasting Power of Attorney and Enduring Power of Attorney 14 Specific situations and treatment 15 What a Living Will cannot ask for 16 Do I need to consult anyone about a Living Will 16 Do I need to tell anyone once I have made a Living Will 17 Conditions for validity 17 Charges 18 Interaction of Living Wills and Lasting Powers 18 Special rules applying to life sustaining treatment 18 3 Consent to Medical Treatment What is it? What the law says - In England and Wales Consent is central to medical treatment. Consent means more than simply agreeing to have a particular course of treatment or a medical procedure. It signifies that by signing the consent form the patient understands what the treatment will involve and what the anticipated benefits and risks of treatment are and that the consent has been given without duress. A patient is competent if he or she can: comprehend information presented in a clear way, believe it and remember it long enough to consider it and come to a decision. What information do I need to give consent? Who should provide it? It is the responsibility of the doctor providing the treatment to ensure you have been given the appropriate information. Good practice states that the doctor should do this, and seek your consent. It is acceptable for someone else to do this on their behalf, provided they are suitably trained and qualified to know the treatment or procedure in question. What risks should I know about? Doctors should tell you about frequently occurring risks associated with the treatment you need, even if small. They are not expected to tell you about every possible risk. They should tell you about any serious side-effects or complications, even if there is only a small chance of them happening. All of this should be explained in clear language, and your doctor should check to ensure you have understood properly. What about my specific questions? The information necessary for consent will vary according to the proposed treatment or procedure and the individual patient’s needs. There are standard points that should always apply: You are entitled to ask questions about your treatment and your doctor is under a duty to answer honestly and, as far as possible, in as much detail as you require. • The diagnosis, prognosis, further investigations that may be necessary and what they consist of Possible questions to ask your doctor • Explanation of the treatment options, including having no treatment • The risks and benefits of each option including the risk of success or failure • Details of who will be involved in your treatment and what each will do • Your right to a second opinion if you are unhappy with the current advice being given • Who will provide the treatment or perform the surgery? • How much experience does the person providing the treatment have? For example, how many procedures have they performed in the last year and what was the complication rate? • What are the likely risks and benefits associated with the procedure? • What is the risk of the procedure not working at all? Is there any other treatment possible? • What are the alternatives and their risks and benefits? • What is the rate of healthcare acquired infection on this ward now? • What aftercare in the community can I expect if something goes wrong? 4 5 Can I refuse treatment? What does a consent form look like? Yes – if you are aged 18 years or older, and have mental capacity (sufficient understanding to make decisions about medical treatment) no one can make a decision on your behalf. The right to refuse treatment is absolute and such decisions have to be respected. Consent forms will vary from hospital to hospital and Trust to Trust. The Patients Association continues to campaign for a standard NHS form and for patients to have proper time to study the form in advance of the treatment or procedure to which it relates. Can I insist on specific treatment? No – doctors or other healthcare professionals cannot be made to provide treatment which they consider to be inappropriate or unnecessary. You are entitled to choose between different treatments if more than one option is available, or to decline treatment altogether. You should feel free to ask to see the consent form before your admission. Some clinicians already give patients the consent form in this way and patients can encourage others to do the same just by asking. Consent Form Sample below Patient agreement to investigation or treatment Patient details (or pre-printed label) What if I lost the ability to make decisions for myself? In the absence of a Living Will or Lasting Power of Attorney – Health and Welfare, doctors are required to act in the best interests of their patient. Patient’s surname/family name.......................................................................................... Patient’s first names........................................................................................................... Date of birth........................................................................................................................ Responsible health professional........................................................................................ Can children make decisions about medical treatment? Yes – in some situations, but the courts can authorise treatment against a child’s wishes if it is in the child’s best interests. Children aged 16 years or older can consent to undergo medical treatment including surgery even if their parents do not agree. For children under the age of 16, there is not the same legal right to consent to treatment, but if they are considered to be mature enough to give consent a doctor can provide treatment. Job title............................................................................................................................... NHS number (or other identifier)........................................................................................ Male Female Special requirements......................................................................................................... (eg other language/other communication method) To be retained in patient’s notes Patient identifier/label Scotland See page 9 Name of proposed procedure or course of treatment (include brief explanation if medical term not clear)...................................................................................................... Northern Ireland See page 9 6 ........................................................................................................................................... 7 Statement of health professional (to be filled in by health professional with appropriate knowledge of proposed procedure, as specified in consent policy) Statement of interpreter (where appropriate) I have explained the procedure to the patient. In particular,~ I have explained: Signed:......................................................................... Date:............................................. I have interpreted the information above to the patient to the best of my ability and in a way in which I believe s/he can understand. Name (PRINT).................................................................................................................... The intended benefits ............................................................................................................... ............................................................................................................... Serious or frequently occurring risks ............................................................................................................... ............................................................................................................... Any extra procedures which may become necessary during the procedure blood transfusion............................................................................... other procedure (please specify) ............................................................................................................... I have also discussed what the procedure is likely to involve, the benefits and risks of any available alternative treatments (including no treatment) and any particular concerns of this patient. The following leaflet/tape has been provided ............................................................................................................... This procedure will involve: Top copy accepted by patient: yes/no (please ring) Statement of patient Patient identifier/label Please read this form carefully. If your treatment has been planned in advance, you should already have your own copy of page 2 which describes the benefits and risks of the proposed treatment. If not, you will be offered a copy now. If you have any further questions, do ask – we are here to help you. You have the right to change your mind at any time, including after you have signed this form. I agree to the procedure or course of treatment described on this form. I understand that you cannot give me a guarantee that a particular person will perform the procedure. The person will, however, have appropriate experience. I understand that I will have the opportunity to discuss the details of anaesthesia with an anaesthetist before the procedure, unless the urgency of my situation prevents this. (This only applies to patients having general or regional anaesthesia.) I understand that any procedure in addition to those described on this form will only be carried out if it is necessary to save my life or to prevent serious harm to my health. I have been told about additional procedures which may become necessary during my treatment. I have listed below any procedures which I do not wish to be carried out without further discussion. general and/or regional anaesthesia local anaesthesia sedation ........................................................................................................................................... Signed:................................................. Date:........................................ Name (PRINT).................................................................................................................... Name (PRINT):..................................... Job title:................................... A witness should sign below if the patient is unable to sign but has indicated his or her consent. Young people/children may also like a parent to sign here (see notes). Contact details (if patient wishes to discuss options later) ............................................................................................................... Signed:......................................................................... Date:............................................. Patient’s signature........................................................ Date:............................................. Name (PRINT).................................................................................................................... 8 9 Confirmation of consent (to be completed by a health professional when the patient is admitted for the procedure, if the patient has signed the form in advance) On behalf of the team treating the patient, I have confirmed with the patient that s/he has no further questions and wishes the procedure to go ahead. Signed:................................................. Date:........................................ Name (PRINT):..................................... Job title:................................... Important notes: (tick if applicable) Patient has withdrawn consent (ask patient to sign /date here) When NOT to use this form If the patient is 18 or over and is not legally competent to give consent, you should use form 4 (form for adults who are unable to consent to investigation or treatment) instead of this form. A patient will not be legally competent to give consent if: ............................................................................................................... • they are unable to comprehend and retain information material to the decision See also advance directive/living will (eg Jehovah’s Witness form) Guidance to health professionals (to be read in conjunction with consent policy) What a consent form is for This form documents the patient’s agreement to go ahead with the investigation or treatment you have proposed. It is not a legal waiver – if patients, for example, do not receive enough information on which to base their decision, then the consent may not be valid, even though the form has been signed. Patients are also entitled to change their mind after signing the form, if they retain capacity to do so. The form should act as an aide-memoire to health professionals and patients, by providing a check-list of the kind of information patients should be offered, and by enabling the patient to have a written record of the main points discussed. In no way, however, should the written information provided for the patient be regarded as a substitute for face-to-face discussions with the patient. The law on consent See the Department of Health’s Reference guide to consent for examination or treatment for a comprehensive summary of the law on consent (also available at www.doh.gov.uk/consent). Who can give consent Everyone aged 16 or more is presumed to be competent to give consent for themselves, unless the opposite is demonstrated. If a child under the age of 16 has “sufficient understanding and 10 intelligence to enable him or her to understand fully what is proposed”, then he or she will be competent to give consent for himself or herself. Young people aged 16 and 17, and legally ‘competent’ younger children, may therefore sign this form for themselves, but may like a parent to countersign as well. If the child is not able to give consent for himself or herself, some-one with parental responsibility may do so on their behalf and a separate form is available for this purpose. Even where a child is able to give consent for himself or herself, you should always involve those with parental responsibility in the child’s care, unless the child specifically asks you not to do so. If a patient is mentally competent to give consent but is physically unable to sign a form, you should complete this form as usual, and ask an independent witness to confirm that the patient has given consent orally or non-verbally. and/or • they are unable to weigh and use this information in coming to a decision. You should always take all reasonable steps (for example involving more specialist colleagues) to support a patient in making their own decision, before concluding that they are unable to do so. Relatives cannot be asked to sign this form on behalf of an adult who is not legally competent to consent for himself or herself. Information Information about what the treatment will involve, its benefits and risks (including sideeffects and complications) and the alternatives to the particular procedure proposed, is crucial for patients when making up their minds. The courts have stated that patients should be told about ‘significant risks which would affect the judgement of a reasonable patient’. ‘Significant’ has not been legally defined, but the GMC requires doctors to tell patients about ‘serious or frequently occurring’ risks. In addition if patients make clear they have particular concerns about certain kinds of risk, you should make sure they are informed about these risks, even if they are very small or rare. You should always answer questions honestly. Sometimes, patients may make it clear that they do not want to have any information about the options, but want you to decide on their behalf. In such circumstances, you should do your best to ensure that the patient receives at least very basic information about what is proposed. Where information is refused, you should document this on page 2 of the form or in the patient’s notes. 11 LIVING WILLS What are they and why are they important? A Will is a statement of what you want done with your property after you die. Making a Will ensures certainty after your death so that those whom you wish to inherit your property can do so in an orderly way and avoid confusion or dispute. A Living Will (which is the same as an Advance Directive or Advance Decision) is a statement of what health treatment you want or do not want once you lack the mental capacity to tell people for yourself. It is designed to ensure that in the event that your capacity to make clear your own views is no longer present, your views are nonetheless clear to your family and clinicians, again to avoid confusion or dispute. The importance of Living Wills has grown as medicine has advanced and life is preserved where previously death would have been inevitable. How that life is lived and whether or not it is perceived as having sufficient quality lies behind the desire of individuals to decide what is worthwhile in advance of the actual situation. How the Mental Capacity Act 2005 changed things in England and Wales Living Wills have been around for some time. Such documents were helpful to a relative required to make life-affecting decisions on behalf of someone unable to communicate effectively. They were accepted as legal and binding. It was unlawful to ignore a Living Will or Advance Directive if the circumstances exactly matched those in the directive. However one great problem was that the appointment of someone to make decisions for you was not binding. All you could do was to appoint a Health Care Proxy who could represent your views but who could be ignored by those treating you. 12 The Mental Capacity Act, which came into force in England and Wales in 2007, changed this. It provides for the first time a statutory basis for Living Wills (the previous law was based on common law principles) and a framework which enables you to consider and record in advance how you wish to be treated when you are unable to express your own views. In particular, you can appoint a Welfare Attorney and set out your own views and specifically state whether or not your Welfare Attorney may make decisions on your behalf about acceptance and refusal of life sustaining treatment. What happens in Scotland and Northern Ireland Please note the Mental Capacity Act 2005 does not apply in: Scotland: where the Adults with Incapacity (Scotland) Act 2000 introduced a system for safeguarding the welfare and managing the finances and property of adults (age 16 and over) who lack capacity. It allows other people e.g. doctors, to make decisions on behalf of these adults, subject to safeguards. The Act aims to ensure that solutions focus on the needs of the individual. Thus the continuing debate in Scotland about whether Living Wills should have overriding authority appears to have decided that they should not despite the Act making no explicit reference to them. Northern Ireland: where currently there is no law permitting Living Wills. For further information we advise you to contact Age Concern. (see Address Book) The Mental Capacity Act has a Code of Practice that provides guidance, not only for making an advance decision, but for those who may have to act upon one – relatives or medical staff. It explains how to assess whether someone is mentally competent to make a particular decision, and also what it means to “act in someone’s best interests”. Chapter 9 of the Code gives a very helpful explanation of how Living Wills interact with Lasting Powers of Attorney – Health and Welfare. The Code is as important for those called up to act upon an advance decision as for those making one, because a doctor is always under an obligation to make sure that patients consent to treatment. But if someone is admitted to hospital when unable to make or communicate decisions about treatment, then medical staff are under a professional obligation to act in that patient’s best interests as they see it. In such cases, knowing the patient’s 13 view of best interests becomes crucial. The existence of an advance decision refusing the proposed treatment overrides any obligation for carers to decide for themselves what is in a patient’s best interests. In those circumstances they must respect the patient’s stated wishes even if it leads to that person’s death. It is legally binding. The importance of Living Wills is shown when there is no advance decision. Medical Staff will almost certainly do their utmost to keep the patient alive at all costs. They may do this even when a relative is convinced this is not what the patient would have wanted. If there is a question of the patient’s mental capacity then, in the absence of an advance decision made by the patient when of sound mind, the Mental Capacity Act provides a mechanism to allow someone to be appointed to act on their behalf. The Court of Protection was set up to do this. Powers of the Court of Protection The Court of Protection has a long history but when the Mental Capacity Act came into force in 2007, the old court was abolished and a new Court (confusingly given the same name) established. Its purpose is to safeguard the interests of anyone with limited mental capacity and in particular to manage the affairs of those who have not made Lasting Powers of Attorney and who have lost the capacity to manage their own affairs. The Court will find itself arbitrating in disputes between family members over who should take charge. Lasting Power of Attorney and Enduring Power of Attorney As the Office of the Public Guardian (see address book)) makes clear, Lasting Powers of Attorney (LPA) are very important documents. You need to have complete trust in those to whom you give such a power that they will act in your best interests. You are strongly advised to take professional advice. 14 You may have taken out an Enduring Power of Attorney (EPA) in the past. The Mental Capacity Act replaces EPAs with a different power of attorney called a Lasting Power of Attorney (LPA). You cannot make any changes to an existing EPA, or take out a new one, but if you already have one you can make a Health and Welfare LPA to run alongside the EPA. It is essential to understand that an EPA deals with finances and property only. It gives no authority whatsoever to make health and welfare decisions. A new Lasting Power (whether for Property and Affairs or for Health and Welfare) must be registered with the Office of the Public Guardian before it can be used. That is an absolute requirement and there is no way round it. It can be registered by you or by the person(s) to whom you have given the Power. An EPA created before 01/10/2007 can still be registered by your Attorney(s) if they have reason to believe that you are or are becoming mentally incapable of managing your affairs. It cannot be registered by you. You may therefore decide that you will need two forms of LPA: one to cover who should have responsibility for managing your financial affairs, and another for who should oversee health or welfare matters – like where you are to live, obtaining access to your medical records, and above all, having authority to refuse or consent to life-sustaining treatment when you are near death. An LPA does not need to be drawn up by a lawyer but for such an important document it is sensible to take qualified advice, and there will be a fee payable, as well as a registration fee which must be paid to the Office of the Public Guardian Unlike the old EPA, as any LPA must be registered with the Office of the Public Guardian before it can be used, you should look for detailed guidance and advice on the website: www.publicguardian.gov.uk Living Wills must relate to specific situations and treatments Situations will include: • being unconscious and unlikely to regain consciousness • suffering from an incurable or irreversible condition likely to result in death within a short period • disability either physical or mental so severe that you will be totally dependent on another permanently 15 Treatments will include • where burdens and risk outweigh potential benefit a Health and Welfare LPA really understand your feelings about pain, dignity, and quality of life. • research or experimentation unlikely to benefit you personally Do I need to tell anyone once I have made a Living Will? • those which postpone death You should make sure it is added to your medical notes so that it can be found easily. Give copies to your GP, next of kin, executors of your Will and your solicitor. We suggest you carry a card with you, similar to an organ donation card, which at the least informs people that your Living Will exists and where it may be found. You will find one at the end of this guide. The important factor in all of this is that your views are known and accessible at the time they are needed. and specific treatments to which you consent • being fed or hydrated, but not by drip • to make you more comfortable • to safeguard your dignity • to relieve pain even though it may hasten death – this is helpful to cover the vague area between effective and fatal pain relief. Your wishes on organ donation may also be covered. What are the conditions for a Living Will or Lasting Power of Attorney to be valid? You must be over 18, and mentally competent. The information contained in your Living Will should ideally include: • Full name and address What a Living Will cannot ask for • Name, address and telephone number of your GP You cannot insist on a specific treatment. Clinical decisions are for the doctors at the time they have to be made. Euthanasia is illegal in the UK at present, so you cannot ask for a specific treatment that you know would kill you. • Date and your signature Do I need to consult anyone about a Living Will? No. However discussing such issues as Living Wills or Lasting Powers of Attorney are as important as the making of a Will, for the reasons previously stated. Discussion with a doctor will enable you to understand the options for treatment if they arise and help you formulate in your own mind what you do or do not wish to consent to. Remember Living Wills or Lasting Powers of Attorney (LPA) are for use in the eventuality that you are unable to make a decision. You must ensure the person(s) you choose to hold 16 • Date and signature of at least one witness over 18. Such a witness should not be a spouse, relative or partner, or a beneficiary of your Will or if a LPA, the attorney. • If you have decided to nominate someone to be consulted about treatment decisions or are writing a Lasting Power of Attorney, you need to include their name, address, and telephone number • Statement of your values and wishes • Treatment you are refusing (for refusal of life saving treatment please see page 14: Special Rules that apply to life sustaining treatment). • Clear statement of the medical situations which will activate it • It is strongly recommended that you review what you have written on a regular basis, to ensure you still feel the same way. If you make any revisions, they should be signed, dated and witnessed. 17 Charges If you use the services of a solicitor to draw up a Living Will, charges may range from £120 to £250 plus VAT, assuming it is straightforward. • Verbal Living Wills do NOT apply to life sustaining treatment – see the Code Chapter 9 paragraphs 24 to 28. A Lasting Power of Attorney should ideally be drawn up by a solicitor, and one used to this type of work. Charges will be more and there is a fee payable of £120 for registration of each type of Power. Interaction between Living Wills and Lasting Powers You should be aware that a Living Will overrules the terms of any Personal Welfare LPA signed before the Living Will, so an attorney under a Health and Welfare LPA cannot consent to any treatment which has been refused in a Living Will made AFTER the LPA was signed. But an LPA made after the Living Will will make the Living Will invalid IF the LPA gives the attorney the right to make decisions about the same treatment. Special rules applying to life saving or life sustaining treatment You should also be aware that if you wish to refuse lifesustaining treatment in advance special provisions apply. • Your statement must be in writing (not necessarily yours), as if you are too ill to write it may be written down at your direction • It must be signed, and if you cannot sign it may be signed at your direction • It must be witnessed and the witness must sign in the presence of the person making the Living Will • It must include an unambiguous written statement that the decision is to apply to the specific treatment even if life is at risk 18 19 Do Not Resuscitate Orders Appropriate use of DNR’s What does DNR mean? The most difficult decisions involve patients who know they are terminally ill, are suffering a lot of pain for example, but who could continue to live for several months. Do Not Resuscitate orders or DNR’s mean that a doctor is not required to resuscitate a patient if their heart stops. They are designed to prevent a patient’s unnecessary suffering but are regarded by some as a form of euthanasia. When does it happen? These orders may also be put on a patient’s file if the resuscitation would be unlikely to succeed, if the patient has stated they do not want to be resuscitated e.g in a Living Will or by being consistent in stating their view. The order may also be made if the clinical view is that it is not in the patient’s best interest. This is the most controversial reason for families and carers to accept because of its subjective nature. They will be placed on a patient’s file if the clinical judgement is that resuscitation will not be appropriate: Who takes the decision? • If it will not restart the heart or breathing • When there is no overall benefit to the patient • When the patient has previously indicated that they do not want resuscitation (as in a Living Will) • They are intended to prevent additional pointless suffering from the effects of the resuscitation itself, such as broken ribs or other fractures, ruptured organs or brain damage. Should the family be consulted? Both the British Medical Association and the Royal College of Nursing have guidance which says that families should be involved in any discussion on DNR orders. There may well be sensitivities, difficulty and distress but that is no reason not to talk to families. 20 The professional guidance was drawn up following concerns that junior doctors were taking decisions in the absence of consultants. You should feel free to ask about the individual hospital’s procedures at the outset, rather than defer until a decision appears likely to be made. DNR’s should not be put in patients’ notes solely on the grounds of age. Safeguards Each NHS Trust must have a policy in place which has patients’ rights at its core, overseen by a non-executive director. It must be available easily for all concerned, monitored and audited. You should not be deterred from asking about this at any stage. Some hospitals may ask patients for their views when they first come into hospital. DNRs should be reviewed regularly, and especially if the patient’s condition changes. 21 Address Book ALZHEIMER’S SOCIETY Devon House, 58 St. Katharine’s Way, London E1W 1JX Tel: 0207 423 3500 Fax: 0207 423 3501 Email: [email protected] www.alzheimers.org.uk OFFICE OF THE PUBLIC GUARDIAN PO Box 15118, Birmingham B16 6GX Tel: 0300 456 0300 Mon-Fri, 9-5 (Wed 10-5) Fax: 0870 739 5780 Email: [email protected] www.publicguardian.gov.uk LAW SOCIETY OF SCOTLAND Tel: 0131 226 7411 Fax: 0131 225 2934 www.lawscot.org.uk DIRECT GOV www.direct.gov.uk official government website for Living Wills, Wills, LPA’s etc. SCOTTISH GOVERNMENT www.scotland.gov.uk OFFICE OF THE PUBLIC GUARDIAN – SCOTLAND Hadrian House, Callendar Business Park, Callendar Road, Falkirk FK1 1XR Tel: 01324 678300 Fax: 01324 678301 Email: [email protected] www.publicguardian-scotland.gov.uk AGE CONCERN NORTHERN IRELAND 3 Lower Crescent, Belfast BT7 1NR Tel: 028 9024 5729 Fax: 028 9023 5497 Email: [email protected] www.ageni.org LAW SOCIETY Tel: 0207 242 1222 Fax: 0207 831 0344 www.lawsociety.org.uk 22 23 Below are outline suggestions for a Living Will and also a Living Will card (which may be carried with you as with an organ donor card). Please remember that the information, especially telephone numbers, on both, must be kept up to date. You should also revise your Living Will regularly to ensure it states your current view in the light of medical technology. Living Will Card I ..................................................... NHS No: .......................... have made a Living Will which may be obtained from Name . ........................................... Tel . ................................... or If I am incapable of directing, participating effectively in or consenting to treatment, I direct that: 1. I do not want my life prolonged by medical treatment, procedure or intervention if, in the opinion of the consultant in charge of my care and another doctor, to do so would not result in my recovery and/or the severity of my illness means my life is nearing its end. 2. I do want pain relief, even if such treatment may shorten my life. Or you may wish to state instead: 3. I wish to be kept alive for as long as possible using all medical treatments, procedures and interventions available. You may also wish to add a clear statement of your values or religious beliefs on which your decision is based. Name . ........................................... Tel . ................................... I have appointed the following as my Health and Welfare Attorney(s) under my Lasting Power of Attorney (if applicable) or Name: . ................................................................................................................ Name . ........................................... Tel . ................................... Address: .............................................................................................................. ..................................................................... Tel: . ............................................. Living Will Details of GP: I (full name) ................................................................................ Name: . ................................................................................................................ Of (full address) ......................................................................... Address: .............................................................................................................. .................................................................................................... ..................................................................... Tel: . ............................................. NHS No: ..................................................................................... Signature:................................................... Date:........................................... have made this advance decision of my own free will, when of sound mind, after careful consideration. Witnessed by I have discussed this decision with a healthcare professional and am aware of the implications of my wishes. Name: . ................................................................................................................ Address: .............................................................................................................. ..................................................................... Tel: . ............................................. 24 25 Patients Association PO Box 935 Harrow Middlesex HA1 3YJ Helpline: 0845 6084455 Admin: 020 8423 9111 www.patients-association.com Registered charity no. 1006722
© Copyright 2026