2014-2016 Management of Infection Guidance for Primary Care
Management of Infection Guidance for Primary Care 2014-2016 AIMS zz to provide a simple, effective, economical and empirical approach to the treatment of common infections zz to minimise the emergence of bacterial resistance in the community Adapted from PHE guidelines by: Dr Philippa Moore Approved by: GHNHSFT Antimicrobial Stewardship Committee Review date: June 2016 NOTE: Doses are oral and for adults unless otherwise stated. Please refer to BNF for further information. CONTENTS.................................................................Page Principles for use of guidelines............................................... 1 Upper respiratory tract infections ................................. 2-6 Sore Throat/Pharyngitis/Tonsillitis........................................... 2 Acute Otitis Media................................................................. 3 Acute Otitis Externa............................................................... 4 Acute Bacterial Parotitis.......................................................... 5 Acute Rhinosinusitis............................................................... 6 Lower Respiratory Tract Infections...............................7-10 Influenza and Influenza related pneumonia............................ 7 Acute Cough, Bronchitis/Infective Exacerbation COPD ........... 8 Community Acquired Pneumonia .......................................... 9 Hospital Acquired Pneumonia & Aspiration Pneumonia.........10 Meningitis.....................................................................11-12 Urinary Tract Infections .............................................. 13-16 Acute Prostatitis....................................................................14 UTI in Pregnancy...................................................................14 UTI in Children .....................................................................15 Acute Pyelonephritis & Recurrent UTI in Women...................16 Gastrointestinal Infections..........................................17-21 Helicobacter pylori Eradication, Oral Candidiasis............... 17-18 Infectious & Traveller’s Diarrhoea and Threadworm ..............19 Acute Diverticulitis .............................................................. 20 C.difficile Infection (new or relapsing) ..................................21 Genital Tract Infections............................................... 22-25 Vaginal Candidiasis.............................................................. 22 Chlamydia............................................................................ 23 Epididymitis ........................................................................ 23 Bacterial Vaginosis................................................................24 Trichomoniasis......................................................................24 PID ..................................................................................... 25 Skin & Soft Tissue Infections...................................... 26-35 Impetigo, Eczema................................................................ 26 Cellulitis............................................................................... 27 OPAT treatment for Cellulitis .......................................... 28-29 Leg Ulcers............................................................................ 30 Diabetic Ulcers..................................................................... 31 Panton Valentine Leucocidin (PVL) infections....................32-33 Animal & Human Bites ........................................................ 34 Scabies and Herpes Infections (VZV/HSV) ............................ 35 Dermatophyte Infections ................................................ 36-38 Conjunctivitis....................................................................... 38 Acne ................................................................................... 39 Wounds from Deliberate Self Harm ..................................... 40 MRSA Screening, Decolonisation and Treatment..... 41-43 Dental Infections.........................................................44-47 Antibiotic activities............................................................... 48 PRINCIPLES OF TREATMENT 1. This guidance is based on the best available evidence but professional judgement should be used and patients should be involved in treatment decisions. 2. It is important to initiate antibiotics as soon as possible in severe infection. 3. A dose and duration for treatment of adults is usually suggested but may need modification for age, weight, and renal function. Children’s doses are provided when appropriate. In severe or recurrent cases consider a larger dose or longer course. Please refer to the BNF for further dosing and interaction information (e.g. interactions between macrolides and statins) if needed and please check for hypersensitivity. 4. Lower threshold for antibiotics in immunocompromised or those with multiple comorbidities; consider culture and seek advice. 5. Prescribe an antibiotic only when there is likely to be a clear clinical benefit. 6. Consider a no, or delayed, antibiotic strategy for acute self limiting upper respiratory tract infections. 7. Limit prescribing over the telephone to exceptional cases. 8. Use simple generic antibiotics if possible. Avoid broad spectrum antibiotics (eg Co-amoxiclav, Quinolones and Cephalosporins) when narrow spectrum antibiotics remain effective, as they increase risk of Clostridium difficile, MRSA and resistant UTIs. 9. Avoid widespread use of topical antibiotics (especially those agents also available as systemic preparations e.g. fucidin). 10.In pregnancy take specimens to inform treatment; avoid Tetracyclines and Quinolones, and avoid where possible Aminoglycosides, high dose Metronidazole (2g) unless benefit outweighs risk. Short-term use of Nitrofurantoin is not expected to cause foetal problems (avoid at term, theoretical risk of neonatal haemolysis) . Trimethoprim is also unlikely to cause problems unless poor dietary folate intake or taking another folate antagonist e.g. an antiepileptic. 11.Where a ‘best guess’ therapy has failed or special circumstances exist, microbiological advice can be obtained via 0300 422 2222. Daytime Ext 5050 12.Check Map of Medicine for diagnostic pathways. 1 UPPER RESPIRATORY TRACT INFECTIONS: Sore Throat/Pharyngitis/Tonsillitis zz Avoid antibiotics as 90% resolve in 7 days without antibiotics and pain only reduced by 16 hours. zz Centor Criteria: History of fever Absence of cough Tender anterior cervical lymphadenopathy Tonsillar exudates A low Centor score (0-2) has a high negative predictive value (80%) and indicates low chance of Group A Beta Haemolytic Streptococci (GABHS). A Centor score of 3 or 4 suggests the chance of GABHS is 40%. If a patient is unwell with a Centor score of 3-or-4 then the chance of developing Quinsy is 1:60. zz If Centor score 3 of 4: consider 2 or 3 day delayed prescription, or immediate antibiotics. zz Antibiotics to prevent Quinsy NNT (Number Needed to Treat): more than 4000 zz Antibiotics to prevent Otitis media: NNT200 First line: PHENOXYMETHYLPENICILLIN 500mg QDS, or 1g BD, oral for 10 days (use QDS when severe) RCT in <18yr olds shows 10 days had lower relapse. If allergic to Penicillin: CLARITHROMYCIN 250-500mg BD oral 5 days 2 Acute Otitis Media (child doses) Optimise analgesia and target antibiotics. zz OM resolves in 60% in 24 hours without antibiotics zz Antibiotics only reduce pain at 2 days (NNT 15) and do not prevent deafness. zz Consider 2 or 3-day delayed prescription, or immediate antibiotics for pain relief if: Less than 2 years with bilateral acute otitis media (NNT4) or bulging membrane and 4 or more marked symptoms All ages with otorrhoea, NNT3 Antibiotics to prevent mastoiditis: NNT more than 4000 First line: AMOXICILLIN oral for 5 days Doses for children: <7 days: 7-28 days: 1 month to 18 years: 30mg/kg BD (max 62.5mg/dose) 30mg/kg TDS (max 62.5mg/dose) 40mg/kg TDS (Max 500mg per dose) ERYTHROMYCIN oral for 5 days Under 1 month 12.5 mg/kg QDS 1 month-2 yrs 125mg QDS 2-8 yrs 250mg QDS 8-18 yrs 250-500mg QDS If allergic to Penicillin: 3 Acute Otitis Externa First use aural toilet (if available) and analgesia zz Cure rates similar at 7 days for topical acetic acid or antibiotic with or without steroid zz Acute severe otitis externa may be caused by Staphylococcus aureus or Beta-haemolytic Streptococci zz If cellulitis or disease extending outside ear canal, start oral antibiotics and refer zz Malignant otitis externa is usually caused by Pseudomonas aeruginosa and presents with unrelenting pain that interferes with sleep and persists even after swelling of the external ear canal has resolved with topical antibiotic treatment. Facial nerve palsy may be present. Patients are usually elderly, and may be diabetics, immunocompromised or healthy individuals. IV antibiotics are required and the patient should be referred. First line: ACETIC ACID 2% 1 spray TDS for 7 days Second line: NEOMYCIN SULPHATE WITH CORTICOSTEROID (Otomize®) 3 metered sprays TDS for 7-14 days If there is a stable eardrum perforation: CIPROFLOXACIN drops: 3 drops TDS for 7-14 days Use eye drop solution as ear drops: unlicensed indication but BNF recommended. 4 Acute Bacterial Parotitis zz Usually unilateral swelling of parotid gland with potential abscess formation. zz Can be associated with poor dental hygiene, dental caries and dehydration. zz The most common cause is Staph aureus (including MRSA). zz Can be associated with trismus and a stone may be palpable in the parotid duct or visible on a plain X-ray. zz Take a parotid duct pus swab for bacterial culture if pus seen from parotid duct. zz Typical courses are 5 days but up to 10 days treatment may be needed for severe infection. FLUCLOXACILLIN 500mg QDS oral for 5 days If anaerobic infection suspected/poor dentition: ADD METRONIDAZOLE 400mg TDS oral for 5 days If Penicillin allergic: CLINDAMYCIN 450mg QDS oral for 5 days If known MRSA carrier: DOXYCYCLINE 200mg OD oral for 5 days If anaerobic infection suspected/poor dentition: ADD METRONIDAZOLE 400mg TDS oral for 5 days zz If symptoms are slow to resolve further days of antibiotics may be necessary, up to 14 days. zz Surgical intervention to drain an abscess may be necessary. 5 Acute Rhinosinusitis Avoid antibiotics as 80% resolve within 14 days without, and they only offer marginal benefit after 7 days, NNT15 Use adequate analgesia Consider 7-day delayed prescription or immediate antibiotics when purulent nasal discharge, NNT8. IF treatment is required: First line: OR OR If poor response: AMOXICILLIN 500mg TDS oral for 7 days (1g TDS if severe) DOXYCYCLINE 200mg STAT/100mg OD oral for 7 days PHENOXYMETHYLPENICILLIN 500mg QDS oral for 7 days AZITHROMYCIN 500mg OD for 3 days In persistent infection use an agent with anti-anaerobic activity (e.g. Co-amoxiclav.) For persistent symptoms: CO-AMOXICLAV 625mg TDS oral for 7 days OR If Penicillin allergic: CLINDAMYCIN 450mg QDS oral for 7 days 6 Influenza – See PHE influenza website Annual vaccination is essential for all those at risk of complications of influenza. For otherwise healthy adults, antivirals are not recommended. Treat ‘at risk’ patients: when influenza is circulating in the community and within 48 hours of onset or in a care home where influenza is likely. At risk: pregnant (including up to 2 weeks post partum), 65 years or over, chronic respiratory disease (including COPD and asthma), significant cardiovascular disease (not hypertension), immunocompromised, diabetes mellitus, chronic neurological, renal or liver disease. Use OSELTAMIVIR 75 mg oral capsules BD oral for 5 days Unless pregnant or suspected resistance to Oseltamivir then use: ZANAMIVIR 10 mg BD inhaled for 5 days (2 inhalations by diskhaler) and seek advice. For prophylaxis see NICE influenza website. Patients under 13 years see PHE influenza website. Influenza Related Pneumonia DOXYCYCLINE 200mg OD oral for 7 days OR CO-AMOXICLAV 625mg TDS oral for 7 days OR CLARITHROMYCIN 500mg BD oral for 7 days If poor response and Penicillin allergic: LEVOFLOXACIN 500mg OD oral for 7 days Levofloxacin may be used BD initially for more severe cases. Reduce to OD when clearly improving. 7 LOWER RESPIRATORY TRACT INFECTIONS: Note: Low doses of Penicillins are more likely to select out resistance. Do NOT use quinolones (Ciprofloxacin, Ofloxacin) first line due to poor pneumococcal activity. Reserve all quinolones (including Levofloxacin) for proven resistant organisms. Avoid Tetracyclines in pregnancy. Acute Cough, Bronchitis Antibiotics have little benefit if no co-morbidity. Consider 7 day delayed antibiotic with symptomatic advice and patient leaflet. Symptom resolution can take 3 weeks. Consider immediate antibiotics if over 80yrs and ONE of: hospitalisation in the last year, oral steroids, diabetic, congestive heart failure. Or over 65yrs and TWO of the above. AMOXICILLIN 500mg TDS oral for 5 days OR DOXYCYCLINE 200mg STAT/100mg OD oral for 5 days Acute Exacerbation of Copd Treat exacerbations promptly with antibiotics if purulent sputum and increased shortness of breath and/or increased sputum volume. 30% are viral, 30-50% bacterial, the rest undetermined. Some patients may need longer treatment. Risk factors for resistant organisms include co-morbid disease, severe COPD, frequent exacerbations, antibiotics in the last 3 months. AMOXICILLIN 500mg TDS oral for 5-7 days OR DOXYCYCLINE 200mg OD oral 5-7 days OR CLARITHROMYCIN 500mg BD oral for 5-7 days If resistance risk factors: CO-AMOXICLAV 625mg TDS oral for 5-7 days 8 Community Acquired Pneumonia – Treatment in the community Use CRB-65 score to help guide and review. Each scores 1: Confusion (AMT less than 8); Respiratory rate (over 30/min); BP (systolic less than 90 or diastolic less than 60); Age 65 or over. Score 0: suitable for home treatment Score 1-2: assessment, consider hospital referral/admission Score 3-4: urgent hospital admission Give immediate IM Benzylpenicillin or Amoxicillin 1g po if delayed admission or life threatening. For Influenza-related pneumonia see page 7. Mycoplasma infection is rare in over 65yrs. If CRB-65 is 0: AMOXICILLIN 500mg TDS oral for 7 days OR CLARITHROMYCIN 500mg BD oral for 7 days OR DOXYCYCLINE 200mg OD oral for 7 days If CRB-65 is 1/2 and at home: AMOXICILLIN 500mg TDS oral AND CLARITHROMYCIN 500mg BD oral for 7–10 days If Penicillin allergic: CLARITHROMYCIN 500mg BD oral for 7–10 days (monotherapy) DOXYCYCLINE 200mg OD oral for 7-10 days OR 9 Hospital Acquired Pneumonia Treatment in the community zz Patients who have recently been discharged from hospital (within 5 days) may have a hospital acquired pneumonia that is more likely be resistant to first line antibiotics. zz If poor response to treatment consult a Microbiologist If home treatment is appropriate: CO-AMOXICLAV 625mg TDS oral for 7 days If Penicillin allergic: LEVOFLOXACIN 500mg OD oral for 7 days Levofloxacin may be used BD initially for more severe cases. Reduce to OD when clearly improving. Aspiration Pneumonia If home treatment is appropriate: CO-AMOXICLAV 625mg TDS oral for 7 days If Penicillin allergic: LEVOFLOXACIN 500mg OD oral for 7 days PLUS METRONIDAZOLE 400mg TDS oral for 7 days Levofloxacin may be used BD initially for more severe cases. Reduce to OD when clearly improving. 10 MENINGITIS Suspected Meningococcal Disease Transfer all patients to hospital immediately. IF time before admission and non blanching rash, give IV antibiotics unless definite history of hypersensitivity. Give IM if a vein cannot be found (see local PGD). Gloucestershire NHS organisations recommend Cefotaxime first line for the following reasons: Cefotaxime has better blood brain barrier penetration Cefotaxime has a broader spectrum of action and is effective against Penicillin resistant Pneumococci, Penicillin resistant Meningococci and Haemophilus influenzae (organisms that have all caused meningitis in patients in Gloucestershire) Cefotaxime can be given in Penicillin allergy unless history of Penicillin immediate type or severe hypersensitivity. Cephalosporins are given to patients with meningitis in hospital and therefore Cefotaxime is consistent with hospital treatment. Patients with meningitis usually come from community settings at lower risk of C. difficile. Cefotaxime, like Benzylpenicillin, can be given IV or IM, and has a reasonably long shelf-life for storage. First line: CEFOTAXIME Ideally give IV but IV or IM Adults and children 12 years and over: CEFOTAXIME 1g Children, including neonates, under 12 years and under 50kg: CEFOTAXIME 50mg/kg to a maximum of 1g 11 MENINGITIS Suspected Meningococcal Disease continued OR BENZYLPENICILLIN Ideally give IV but IV or IM Children under 1 yr: 300mg Children 1 - 9 yrs: 600mg Age 10 years or over: 1200mg Prevention of Secondary Case of Meningitis: Only prescribe prophylaxis following advice from Public Health Doctor: 9am–5pm: 0845 504 8668 Out of hours: Contact on-call Public Health Doctor 0844 257 8195 or via switchboard 0300 422 2222 First line (PHE Meningococcal Guidelines Feb 2011): CIPROFLOXACIN 500mg STAT oral (adult) Children 1 month - 4 yrs: 125mg STAT oral Children 5 - 12 yrs: 250mg STAT oral Age 12 years or over: 500mg STAT oral Second line: RIFAMPICIN 600mg BD oral for 2 days Children under 1 yr: Children 1-12 yrs: Age 12 years and over: 5mg/kg BD oral for 2 days 10mg/kg BD oral for 2 days 600mg BD oral for 2 days 12 URINARY TRACT INFECTIONS – (See PHE UTI quick reference guide) zz In the elderly (over 65 years), do not treat asymptomatic bacteriuria; it is common but is not associated with increased morbidity. zz Catheter in situ: antibiotics will not eradicate asymptomatic bacteriuria: only treat if symptomatically unwell or pyelonephritis likely. Do not use prophylactic antibiotics for catheter changes unless history of catheter-change-associated UTI or trauma. Uncomplicated UTI in Men and Women (no fever or flank pain) Women with severe / 3 or more symptoms: treat Women with mild / 2 or fewer symptoms: use urine dipstick and presence of cloudy urine to guide treatment. With 2 symptoms, nitrite and blood/leucocytes has 92% positive predictive value; Negative nitrite, leucs and blood: 76% negative predictive value. Men: Consider prostatitis and send pre-treatment MSU OR if symptoms mild/non-specific, use negative dipstick to exclude UTI. TRIMETHOPRIM 200mg BD oral Avoid in established renal failure (GFR less than 15 ml/min) OR NITROFURANTOIN 100mg m/r BD oral Contraindicated in renal failure. Not recommended if GFR less than 60 ml/min or creatinine over 150 umol/l. Use 3 days in women, 7 days in men Second line: Perform culture in all treatment failures Amoxicillin resistance is common, only use if susceptible. Community multi-resistant Extended-Spectrum-Beta-Lactamase (ESBL) E. coli are increasing: consider Nitrofurantoin if susceptible or Fosfomycin 3g stat in women, plus second 3g dose in men 3 days later. Give 2-3 hours before food. Fosfomycin is only available on a named patient basis: community pharmacists can order via IDIS, Specials Lab or Quantum. 13 Acute Prostatitis zz Send MSU for culture and start antibiotics. zz 4 week course may prevent chronic prostatitis. zz Quinolones achieve higher prostate levels. CIPROFLOXACIN 500mg BD oral for 28 days OR OFLOXACIN 200mg BD oral for 28 days Second line: TRIMETHOPRIM 200mg BD oral for 28 days Uti in Pregnancy zz Send MSU for culture & sensitivity and start empirical antibiotics. zz Short-term use of Nitrofurantoin in pregnancy is unlikely to cause problems to the foetus, although avoid at term (may produce neonatal haemolysis). zz Avoid Trimethoprim if low folate status or on folate antagonist (e.g. antiepileptic or proguanil) First line: NITROFURANTOIN 100mg m/r BD oral for 7 days Nitrofurantoin is contraindicated in renal failure (GFR less than 60 ml/min or creatinine over 150 umol/l). OR if susceptible......................... AMOXICILLIN 500mg TDS oral for 7 days Second line: TRIMETHOPRIM 200mg BD oral for 7 days (off label). Give folic acid if first trimester. Or: CEFALEXIN 500mg BD oral for 7 days 14 Uti in Children zz Children under 3 months: refer urgently for assessment. zz Children 3 or more months old: use positive nitrite to start antibiotics. Send pre-treatment MSU for all. zz Imaging: only refer if child is under 6 months, recurrent or atypical UTI (see NICE guidelines) TRIMETHOPRIM OR NITROFURANTOIN Lower UTI: Nitrofurantoin is contraindicated in renal failure (GFR less than 60 ml/min or creatinine over 150 umol/l). If susceptible AMOXICILLIN CEFALEXIN See BNF for oral dosage Second line: Treat lower UTI for 3 days. Upper UTI: CO-AMOXICLAV CEFIXIME See BNF for oral dosage Second line: Treat upper UTI for 7-10 days. 15 Acute Pyelonephritis If admission not needed, send MSU for culture and sensitivities and start empirical antibiotics. If no response within 24 hours admit. CIPROFLOXACIN 500mg BD oral 7 days OR CO-AMOXICLAV 625mg TDS oral 14 days Recurrent UTI in non-pregnant women (at least 3 UTIs per year) Cranberry products or post coital or standby antibiotics are options. Standby antibiotics may be more suitable for less frequent recurrences. Nightly antibiotics: reduces UTIs but adverse effects Prophylactic: NITROFURANTOIN 50mg-100mg oral Nitrofurantoin is contraindicated in renal failure (GFR less than 60 ml/min or creatinine over 150 umol/l). OR TRIMETHOPRIM 100mg oral Post coital: STAT (off label) Prophylactic: OD at night 16 GASTRO-INTESTINAL TRACT INFECTIONS Eradication of Helicobacter pylori – Also see PHE HP quick reference guide zz Eradication is beneficial in known Duodenal Ulcer (DU), Gastric Ulcer (GU) or low grade MALToma. zz In Non Ulcer Dyspepsia (NUD), the NNT is 14 for symptom relief. zz Consider test and treat in persistent uninvestigated dyspepsia zz Do not offer eradication for Gastro-Oesophageal Reflux Disease (GORD). zz Do not use Clarithromycin or Metronidazole if used in the past year for any infection. First line: PPI (use cheapest) BD oral PLUS CLARITHROMYCIN 250mg BD oral PLUS METRONIDAZOLE 400mg BD oral OR PPI (use cheapest) BD oral PLUS CLARITHROMYCIN 500mg BD oral PLUS AMOXICILLIN 1g BD oral (Note higher dose Clarithromycin when used with Amoxicillin rather than Metronidazole) All oral for 7 days For MALToma use 14 days 17 GASTRO-INTESTINAL TRACT INFECTIONS Eradication of Helicobacter pylori – CONTINUED Managing symptom relapse zz DU/GU relapse: retest for H. pylori using breath test or faecal antigen test (if available) OR consider endoscopy for biopsy culture and sensitivity. zz NUD: do not retest, offer PPI or H2RA Second line: PLUS PLUS 2 unused antibiotics out of: PPI BD oral BISMUTHATE (DE-NOL tabs) 240mg BD oral AMOXICILLIN 1g BD oral METRONIDAZOLE 400mg TDS oral TETRACYCLINE 500mg QDS oral CLARITHROMYCIN 500mg BD oral For relapse or MALToma use 14 days – If further advice is required please contact a Microbiologist and see PHE Helicobacter pylori quick reference guide. Oral Candidiasis Antifungal agents absorbed from the gastrointestinal tract prevent oral candidiasis in patients receiving treatment for cancer. Drugs fully absorbed (Fluconazole, Ketaconazole, Itraconazole) and partially absorbed (Miconazole, Clotrimazole) are effective compared with placebo or no treatment. See BNF for licensed dosage. 18 Infectious Diarrhoea Also see PHE Infectious Diarrhoea quick reference guide Refer previously healthy children with acute painful or bloody diarrhoea to exclude E. coli 0157 infection: refer to PHE guidelines. Antibiotics should NOT be prescribed. Antibiotic therapy is not indicated unless the patient is systemically unwell. If patient systemically unwell and Campylobacter suspected (e.g. undercooked meat and abdominal pain), consider: CLARITHROMYCIN 250-500mg BD oral for 5-7 days if treated early. Traveller’s Diarrhoea Only consider standby antibiotics for remote areas or people at high-risk of severe illness with traveller’s diarrhoea. If standby treatment appropriate give: CIPROFLOXACIN 500mg BD oral for 3 days (private Rx). If Quinolone resistance high (e.g. South Asia): consider: BISMUTH SUBSALICYLATE (Pepto-Bismol) 2 tablets QDS oral as prophylaxis or for 2 days treatment. Threadworms Treat all household contacts at the same time PLUS advise hygiene measures for 2 weeks (hand hygiene, pants at night, morning shower, PLUS wash sleepwear, bed linen, dust, and vacuum on day one. Over 6 months: MEBENDAZOLE 100mg STAT oral (off label if under 2 years old) 3-6 months: PIPERAZINE/SENNA sachet 2.5ml spoon STAT oral, repeat after 2 weeks Under 3 months: 6 weeks hygiene measures 19 Acute Diverticulitis Diverticulosis should be managed with a high fibre diet. Pain may occur in diverticular disease (without infection) that can be managed with oral Paracetamol. People with mild, uncomplicated acute diverticulitis can be managed at home with Paracetamol, clear fluids, and oral antibiotics (see CKS guidelines). IF treatment required: First Line: CO-AMOXICLAV 625mg TDS oral for 7 days If Penicillin allergic: CIPROFLOXACIN 500mg BD oral for 7 days PLUS METRONIDAZOLE 400mg TDS oral for 7 days Bristol Stool Chart NB: Cephalosporins are NOT recommended (e.g. see CKS guidelines) Type 1 Separate hard lumps, like nuts (hard to pass) Type 2 Sausage-shaped but lumpy Type 3 Like a sausage but with cracks on the surface Type 4 Like a sausage or snake, smooth and soft Type 5 Soft blobs with clear-cut edges Type 6 Fluffy pieces with ragged edges, a mushy stool Type 7 Watery, no solid pieces. Entirely liquid. 20 Clostridium difficile INFECTION zzStop unnecessary antibiotics and/or PPIs and H2RAs. zzAvoid antimotility agents e.g. Loperamide or Opiates. zzHistorically 70% respond to Metronidazole in 5 days, 92% in 14 days; use longer courses if slow response. zzNew strains e.g. 027 may not respond well to Metronidazole, change to Vancomycin if poor response by 5-7 days. zzSevere if Temp over 38.5oC; WCC over 15/L, rising creatinine or signs/symptoms of severe colitis, or known ribotype 027 (may cause more severe disease): use Vancomycin. Review progress closely and/or consider hospital referral. zzNote in very severe disease, diarrhoea may be absent. 1st/2nd episodes: METRONIDAZOLE 400mg oral TDS 10-14 days 3rd episode/severe: VANCOMYCIN 125mg oral QDS 10-14 days Relapsing disease: VANCOMYCIN 125mg oral QDS 14 days (until settled), then 125mg oral BD 7 days, then 125mg oral OD 7 days, then 125mg oral alternate days 7 days, then 125mg oral every 3rd day for 14 days For those at high risk of C. difficile consider primary prophylactic probiotics. Advise probiotics for relapsing disease (most evidence for Actimel). Fidaxomicin may also be considered for those with relapsing disease. This should only be prescribed after discussion with a Microbiologist. 21 GENITAL TRACT INFECTIONS – UK NATIONAL GUIDELINES Contact UKTIS for information on foetal risks if the patient is pregnant. See PHE Vaginal Discharge and Chlamydia quick reference guide or BASHH website zz People with risk factors should be screened for Chlamydia, Gonorrhoea, HIV, Syphilis. zz Refer individuals and partners to GUM service. zz Risk factors for STIs: under 25y, no condom use, recent (less than 12mths) or frequent change of sexual partner, previous STI, symptomatic partner. Vaginal Candidiasis All topical and oral azoles give 75% cure. CLOTRIMAZOLE 500mg pessary or 10% cream STAT OR FLUCONAZOLE 150mg STAT oral In pregnancy: avoid oral azoles and use intravaginal treatment: see below. CLOTRIMAZOLE 100mg pessary at night for 6 nights OR MICONAZOLE 2% cream 5g intravaginally BD for 7 days 22 Chlamydia trachomatis Infection/Urethritis See PHE Chlamydia quick reference guide zz Opportunistically screen all aged 15-25 years. zz Treat partners and refer to GUM service. AZITHROMYCIN 1g STAT oral OR DOXYCYCLINE 100mg BD oral for 7 days (Doxycycline can also be used at 200mg OD) In pregnancy or breastfeeding: AZITHROMYCIN 1g STAT oral (off label) OR OR ERYTHROMYCIN 500mg QDS oral for 7 days AMOXICILLIN 500mg TDS oral for 7 days zz For pregnancy or breastfeeding Azithromycin is the most effective option. zz Due to the lower cure rate in pregnancy, test for cure 6 weeks after treatment. Suspected Epididymitis in men OFLOXACIN 200mg BD oral for 14 days OR DOXYCYCLINE 100mg BD oral for 14 days (Doxycycline can also be used at 200mg OD) If high risk of Gonorrhoea: ADD CEFTRIAXONE 500mg STAT im Note: oral/other Cephalosporins are NOT considered an appropriate substitute due to low tissue levels leading to resistance (BASHH 2011 guidelines). For Acute Prostatitis see page 14 23 Bacterial Vaginosis zz Oral Metronidazole is as effective as topical treatment but is cheaper. zz There is less relapse at 4 weeks with a 7 day course than 2g stat. zz In pregnancy and breast feeding avoid the 2g stat dose. zz Treating partners does not reduce relapse. METRONIDAZOLE 400mg BD oral for 7 days OR METRONIDAZOLE 2g STAT oral (avoid in pregnancy and breast feeding) OR METRONIDAZOLE 0.75% vaginal gel 5g applicatorful at night for 5 nights OR CLINDAMYCIN 2% cream 5g applicatorful at night for 7 nights Trichomoniasis Treat partners simultaneously and refer to GUM service. In pregnancy or breastfeeding: avoid 2g single dose Metronidazole. Consider topical Clotrimazole for symptom relief (not cure) if Metronidazole declined. METRONIDAZOLE 400mg BD oral for 5-7 days OR METRONIDAZOLE 2g STAT oral (avoid in pregnancy and breast feeding) Symptom relief in pregnancy (if Metronidazole declined): CLOTRIMAZOLE 100mg pessary at night for 6 nights 24 Pelvic Inflammatory Disease (PID) zz Refer woman and contacts to GUM service zz Always culture for Gonorrhoea and test for Chlamydia zz 28% of Gonorrhoea isolates are now resistant to Quinolones. If Gonorrhoea likely (partner has it, severe symptoms, sex abroad), consider GUM referral as IM Ceftriaxone required. AZITHROMYCIN 1g oral STAT PLUS OFLOXACIN 400mg BD oral 14 days PLUS METRONIDAZOLE 400mg BD oral 14 days If high risk of Gonorrhoea: CEFTRIAXONE 500mg STAT im Note: oral/other Cephalosporins are NOT considered an appropriate substitute due to low tissue levels leading to resistance (BASHH 2011 guidelines). PLUS DOXYCYCLINE100mg BD oral 14 days (Doxycycline can also be used at 200mg OD) PLUS METRONIDAZOLE 400mg BD oral 14 days For pregnancy or breastfeeding: CEFTRIAXONE 500mg STAT im Note: oral/other Cephalosporins are NOT considered an appropriate substitute as noted above. PLUS METRONIDAZOLE 400mg BD oral 14 days (Warn women about taste of Metronidazole in breast milk) PLUS ERYTHROMYCIN 500mg BD oral for 14 days (OR AZITHROMYCIN 1g STAT then 500mg OD oral for 4 days) 25 Skin/Soft Tissue Infections For MRSA screening and suppression see PHE MRSA quick reference guide. For abbreviated version on MRSA screening and suppression see pages 31-33 Impetigo zz For extensive, severe or bullous impetigo use oral antibiotics. zz Reserve topical antibiotics for very localised lesions to reduce the risk of resistance. zz Reserve Mupirocin for MRSA. For localised lesions only: FUSIDIC ACID TDS topically for 5 days For MRSA localised lesions only: MUPIROCIN TDS topically for 5 days For more severe/non-localised lesions: FLUCLOXACILLIN 500mg QDS oral for 7 days If Penicillin allergic: CLARITHROMYCIN 250-500mg BD oral for 7 days Eczema If no visible signs of infection, use of antibiotics (alone or with steroids) encourages resistance and does not improve healing. In eczema with visible signs of infection, use treatment as in impetigo. 26 Cellulitis If patient is afebrile and healthy other than cellulitis, use oral Flucloxacillin alone. zz If river or sea water exposure, discuss with Microbiologist. zz If febrile and ill, admit for IV treatment. zz Clarithromycin is more likely to be successful in limited area cellulitis; for extensive cellulitis with or without lymphangitis use Clindamycin. zz Stop Clindamycin if diarrhoea occurs. FLUCLOXACILLIN 500mg QDS oral for 7 days, up to 1g QDS for 14 days if slow response. OR CLARITHROMYCIN alone 500mg BD for 7 days CLINDAMYCIN 300mg-450mg QDS for 7 days Increase both to 14 days if slow response. If known MRSA carrier: DOXYCYCLINE 200mg OD oral for 7-14 days For more severe cases: ADD RIFAMPICIN 450mg BD oral for 7-14 days If facial cellulitis: CO-AMOXICLAV 500/125mg TDS for 7-14 days, If Penicillin allergic: CLINDAMYCIN 300mg-450mg QDS for 7-14 days If Penicillin allergic: For MRSA localised lesions only: DOXYCYCLINE 200mg OD oral for 7-14 days ADD RIFAMPICIN 450mg BD oral for 7-14 days See over for pages on OPAT. 27 Outpatient Home (IV) Antibiotic Therapy (OPAT) for Cellulitis (class 2) zz Home IV antibiotics may prevent hospital admissions for treatable conditions such as cellulitis class 2. zz OPAT Home IV team contact Pager: 07659 113695 Assessment of grade of cellulitis (Eron/Dall criteria): Class 1 Class 2 Class 3 Class 4 Healthy patients with cellulitis, up to 15 cm diameter, with or without fever Healthy patients or patient with peripheral vascular disease, diabetes or obesity with cellulitis more than 15 cm with or without fever. Patient in whom oral antibiotics have failed Patients with fever and mental status change, physical findings of gangrene, crepitus bullae or open draining wounds (requires hospital admission) Patients with systemic complication of severe infection which includes hypotension, renal failure and acute respiratory distress syndrome (requires hospital admission) First line: CEFTRIAXONE 2g OD iv until oral switch Second line or if severely Penicillin allergic, or Cephalosporin allergic, or high risk of C. difficile infection or MRSA carrier:DAPTOMYCIN 4mg/kg OD iv until oral switch Since Daptomycin is expensive and can be used at higher doses, round up the dose to the nearest whole vial (350mg or 500mg). Less than 60kg: 4mg/kg iv od; 60-80kg: 350mg iv od 80-125kg: 500mg iv od; Greater than 125kg: 850mg iv od Creatine (Phospho) Kinase (CK/CPK), should be measured before/as treatment starts and monitored weekly thereafter whilst Daptomycin continues. Discontinue if unexplained muscular symptoms develop or CK markedly elevated (5x normal before treatment) or marked elevation occurs on treatment. 28 OutPatient Home (IV) Antibiotic Therapy (OPAT) For Cellulitis (class 2) Antibiotics will be switched to oral once clear clinical response. Oral switch as per page 27. Inclusion criteria zzPatient is over 18 years of age and registered with a Gloucestershire GP (or 16 – 18 discuss with IV team) zzIV therapy is needed to treat a patient who has been diagnosed with class II cellulitis (see classification above) as alternative routes of drug delivery are not feasible or appropriate. Healthcare staff are able to gain suitable IV access zzThe medical and psychological condition of the patient is suitable and stable and hospitalisation is not needed and complex nursing/medical intervention is not required. Consider increased package of care for individual patients if necessary. zzThe patient must have received a comprehensive assessment by the clinician responsible for their care and/ or a member of the District Nursing team. zzA satisfactory home condition exists i.e. running water, telephone and the patient and carer understand the implications, risks and benefits of the treatment plan and have given informed consent. Exclusion criteria zz The patient does not meet criteria for inclusion zz Patient has facial, orbital or palmar cellulitis, received IV antibiotics for cellulitis of the same site within the preceding month, peripheral IV access not obtainable/reliable, current substance misuse, pregnancy or signs of rapid extensions/necrosis suggestive of necrotising fasciitis zz Co-morbidities such as: Immunosuppression, Unstable diabetes, Peripheral Vascular disease, Alcoholism. 29 Leg Ulcers – See PHE Leg Ulcer quick reference guide zz Ulcers are always colonised with bacteria. zz Antibiotics do not improve healing unless there is active infection (e.g. cellulitis, increased pain; enlarging ulcer, purulent exudate, new odour or pyrexia). zz If there is active infection, send pre-treatment swab. zz Review antibiotics after culture results. If signs of active infection: FLUCLOXACILLIN 500mg QDS oral 7 days, If Penicillin allergic: increased to 14 days if slow response. CLARITHROMYCIN 500mg BD oral 7-14 days Leg Ulcers: MRSA See PHE MRSA quick reference guide zz Most leg ulcers that grow MRSA on culture are only colonised and do not require antibiotic treatment, (see also section on decolonisation, pages 41-42). zz For active MRSA infection use antibiotic sensitivities to guide treatment. If severe infection or no response to monotherapy after 24-48 hours, seek advice from Microbiologist on combination therapy. zz If active infection, MRSA confirmed or suspected from previous culture results, infection not severe, and admission not required: DOXYCYCLINE 200mg OD oral for 7-14 days OR IF susceptible: CLINDAMYCIN 450mg QDS oral for 7-14 days Stop Clindamycin if diarrhoea occurs 30 Diabetic Ulcers without Osteomyelitis zz Ulcers are always colonised with bacteria and treatment should only be given if there are signs of active infection. zz Longer courses may be needed for infections that are slow to respond If signs of active infection: CO-AMOXICLAV 625mg TDS oral for 7-14 days If Penicillin allergic: CLINDAMYCIN 450mg QDS oral for 7-14 days If suspected MRSA: DOXYCYCLINE 200mg OD oral for 7-14 days Diabetic Ulcers With Osteomyelitis zz Ulcers that probe to bone are likely to have associated osteomyeltitis. zz Tissue samples may help direct therapy; superficial swabs are of less predictive value for underlying causative organisms. Deep swabs taken after clearance of superficial debris may be useful. zz Patients should be referred for specialist assessment. IV antibiotics are often needed at least initially. zz Duration of treatment depends on resolution of the osteomyelitis and 12 or more weeks of treatment may be needed. zz If MRSA is suspected treatment must be discussed with a Microbiologist. CIPROFLOXACIN 750mg BD oral PLUS CLINDAMYCIN 450mg QDS oral Typical course would be for at least 6 weeks. 31 Panton-Valentine Leucocidin (PVL) See PHE PVL quick reference guide zzPanton-Valentine Leucocidin (PVL) is a toxin produced by approximately 2% of Staphylococcus aureus. These can be MSSA or MRSA strains. zzPVL can cause, albeit rarely, severe invasive infections in healthy people. zzPVL is also associated with persistent recurrent pustules, carbuncles, boils or abscesses. Send swabs for culture in these clinical scenarios. zzRisk factors for PVL include: nursing homes, close contact communities or sports, sharing equipment, poor hygiene. zzPVL abscesses should be incised and drained. zzMinor furunculosis, folliculitis, and small abscesses without cellulitis do not need antibiotic treatment (may need incision and drainage). zzTopical antibiotics are not usually appropriate. If treatment of skin and soft tissue infection is required: For MSSA use: FLUCLOXACILLIN 500mg QDS oral 5-7 days For penicillin allergy: CLINDAMYCIN 450mg QDS oral for 5-7 days For MRSA use (after checking susceptibility): DOXYCYCLINE 200mg OD oral for 5-7 days OR (if susceptible) Stop Clindamycin if diarrhoea occurs CLINDAMYCIN 450mg QDS oral for 5-7 days For more severe infection but not requiring hospital admission: ADD RIFAMPICIN 300mg BD oral for 5-7 days 32 Panton-Valentine Leucocidin (PVL) decolonisation (suppression) therapy After successful treatment of PVL infections, decolonisation is recommended: Use: NASAL 2% MUPIROCIN 3 times a day for 5 days Apply matchstick-head sized amount of ointment to inner surface of each nostril. Patients should be able to taste Mupirocin at back of the throat. PLUS SKIN 4% Chlorhexidine Gluconate DAILY topically as body-wash for 5 days TWICE DURING 5 DAYS as shampoo Second line for skin (e.g. if patient has irritant dermatitis): OCTENISAN DAILY topically as body- wash for 5 days TWICE DURING 5 DAYS as shampoo Moisten skin and apply undiluted antiseptic then rinse. Particularly apply to known carriage sites (axilla, groin and perineum). Wash hair using antiseptic body-wash/shampoo at least twice during the 5 days. After washing, use clean towels, sheets and clothing DAILY. Launder items separately from other family members, using as high a temperature as fabric allows. Consider also spring cleaning of house including soft furnishings. Family/close contacts should also be screened and offered decolonisation if found to be carriers. Contact PHE Health Protection Unit for further advice (Telephone office hours: 0845 504 8668) 33 Animal and Human Bites Thorough irrigation is important. Human: zz Assess risk of tetanus, HIV, hepatitis B and C and discuss with Microbiologist if appropriate. zz Antibiotic prophylaxis is advised. Animal: zz Assess risk of tetanus and rabies. zz Antibiotic prophylaxis advised for cat bite/puncture wound; bite involving hand, foot, face, joint, tendon, ligament; immunocompromised, diabetic, asplenic or cirrhotic. First line animal & human prophylaxis and treatment: CO-AMOXICLAV 375-625mg TDS oral for 7 days If Penicillin allergic: METRONIDAZOLE 200-400mg TDS oral for 7 days PLUS DOXYCYCLINE (cat/dog/human) 100mg BD oral for 7 days OR PLUS METRONIDAZOLE 200-400mg TDS oral for 7 days CLARITHROMYCIN (human only) 250-500mg BD oral for 7 days Review at 24 & 48 hours 34 Scabies zz Treat all home and sexual contacts within 24 hours. zz Treat whole body from ear/chin downwards and under nails. zz If under 2 years or elderly, also treat the face and scalp. PERMETHRIN 5% CREAM 2 applications topically one week apart If allergy: MALATHION 0.5% AQUEOUS LIQUID 2 applications topically one week apart Varicella Zoster/Chickenpox zz If pregnant / immunocompromised / neonate: seek urgent specialist advice. zz Chicken pox: Consider Aciclovir IF within 24 hrs of rash onset and over 14 yrs old, or severe pain or dense/oral rash, or secondary household case, or on steroids, or smoker. Shingles: Treat if over 50 yrs old, and within 72 hrs of rash onset (post herpetic neuralgia is rare in under 50’s), or if active ophthalmic disease, or Ramsey Hunt, or eczema. If indicated: ACICLOVIR 800mg 5 times day oral for 7 days Second line if compliance a problem, as ten times cost VALACICLOVIR 1g TDS oral for 7 days OR FAMCICLOVIR 250mg TDS oral for 7 days Cold Sores Cold sores resolve after 7-10 days without treatment. Topical antivirals applied prodromally reduce duration by 12-24 hrs only. 35 Dermatophyte Infection of the Proximal Fingernail or Toenail See PHE Fungal Skin and Nail infections quick reference guide zz Take nail clippings zz Start therapy only if infection is confirmed by laboratory. zz Terbinafine is more effective than azoles. zz Liver reactions occur rarely with oral antifungals. zz If Candida or non-dermatophyte infection confirmed, use oral Itraconazole. zz For children seek specialist advice. Superficial infection on the top surface of nail plate only: 5% AMOROLFINE NAIL LACQUER 1-2 times weekly fingers 6 months First line: TERBINAFINE 250mg OD oral fingers 6-12 weeks toes 3-6 months toes 12 months Second line (infections with Candida spp or non-dermatophyte moulds): ITRACONAZOLE 200mg BD oral for 7 days monthly fingers 2 courses toes 3 courses 36 Dermatophyte Infection Of The Skin zz Terbinafine is fungicidal so treatment time is shorter than with fungistatic imidazoles. zz If Candida is possible, use imidazole. zz If intractable send skin scrapings. If infection confirmed, use oral Terbinafine/Itraconazole. zz Discuss scalp infections with specialist. 1% TERBINAFINE BD TOPICAL for 1-2 weeks OR IMIDAZOLE BD TOPICAL for 1-2 weeks after healing (i.e. for 4-6 weeks) For athletes’ foot only: UNDECANOATES (Mycota®) BD TOPICAL for 1-2 weeks after healing (i.e. for 4-6 weeks) Candida Infection of the Skin zz Confirm by laboratory zz Treat with 1% azole cream but use lotion if treating paronychia zz Seek advice for nail infection 1% AZOLE CREAM BD TOPICAL for 1-2 weeks (In case of paronychia treat until swelling goes) 37 Pityriasis Veriscolor zz Scratching the surface of the lesion should demonstrate mild scaling 1% AZOLE CREAM OD- BD TOPICAL OR 1% TERBINAFINE OD –BD TOPICAL OR SHAMPOO CONTAINING KETOCONAZOLE OD-BD TOPICAL All usually for 1 week Conjunctivitis zz Treat if severe as most infections are viral or self-limiting. zz Bacterial conjunctivitis is usually unilateral and also self-limiting (65% resolve on placebo by day 5). It is characterised by red eye with mucopurulent, not watery, discharge. zz Fusidic acid has less Gram-negative activity If severe: CHLORAMPHENICOL 0.5% DROPS PLUS 1% OINTMENT 4 HRLY (whilst awake) AT NIGHT OR CHLORAMPHENICOL 1% OINTMENT 3-4 times DAILY OR FUSIDIC ACID 1% GEL BD topically Continue for 48 hrs after symptom resolution 38 Acne For all grades of acne dispel myths and give general advice, improvement may not be seen for 2+ months with any treatment. See Clinical Knowledge Summaries for more information. zz Mild acne: mainly non-inflammatory comedones, usually limited in its extent. zz Moderate acne: a mixture of non-inflammatory comedones and inflammatory papules and pustules, may extend to the shoulders and back. zz Severe acne: nodules and cysts (nodulocystic acne), as well as a preponderance of inflammatory papules and pustules, may be extensive. Mild/Moderate Acne: First line: BENZOYL PEROXIDE: use lowest strength first, see BNF. Useful especially if papules and pustules are present. OR TOPICAL RETINOID (tretinoin, isotretinoin or adapalene) use lowest strength first, see BNF. Consider prescribing a standard combined oral contraceptive in women who require contraception, particularly if the acne is having a negative psychosocial impact. Topical antibiotics are of limited benefit and resistance is increasing. Moderate/Severe Acne: Use a topical agent (above) with a Tetracycline (little difference in efficacy between most, but Minocycline NOT recommended): OXYTETRACYCLINE 500mg BD oral OR DOXYCYCLINE 100mg OD oral OR LIMECYCLINE 408mg OD oral Review efficacy at 3 months, usually given for 6+ months up to 2 years. Second line options are available: see CKS, BNF or discuss with a Dermatologist or Microbiologist. 39 Wounds from Deliberate Self Harm zz Wounds resulting from deliberate self harm should be assessed for need for empirical treatment antibiotics. zz There is no evidence for antibiotic prophylaxis being of benefit. zz Repeated courses of antibiotics in patients who repeatedly deliberately self harm may precipitate C. difficile infection. zz Consider whether tetanus vaccination/booster is required. zz Superficial wounds: lacerations, burns The majority of superficial wounds will NOT need antibiotic therapy if there is no sign of local infection. Antibiotics should not be given prophylactically. Local wound toilet is appropriate especially following foreign body removal or if contamination with dirt. If evidence of local infection, take a wound swab for MC&S. Treatment should be adjusted according to results. zz Deep wounds (penetrating the fascial layer), insertion of foreign bodies per vagina, per rectum, etc with penetration of mucosal surface, Antibiotics should not routinely be prescribed. The wound should be regularly assessed for evidence of infection. Foreign bodies should be removed and local wound toileting should be performed. First Line IF REQUIRED: FLUCLOXACILLIN 500mg QDS oral for 5 days If Penicillin allergic: CLARITHROMYCIN 500mg BD oral for 5 days Second Line: or if likely anaerobic wound infection: CO-AMOXICLAV 375-625mg TDS oral 5 days OR If Penicillin allergic: CLINDAMYCIN 300-450mg QDS oral for 5 days 40 Skin/Soft Tissue – MRSA Screening, Decolonisation and Treatment Adapted from PHE MRSA quick reference guide and also see BSAC guidelines How do I screen a patient for MRSA? In most cases, patients should be swabbed as close to elective admission as possible. Swab anterior nares (nose): Wipe a swab around inside rim of patient’s nose for 5 seconds (both nares with the same swab). Also swab skin lesions or wounds: includes skin lesions or wounds, sites of catheters, catheter urine, groin/perineum, tracheostomy and other skin breaks and sputum from patients with a productive cough. Label the bacteriology form “MRSA screen”. Interpreting the L aboratory Result Only MRSA will be looked for when swabs are labelled “MRSA screen”. Positive cultures are reported as “MRSA isolated”. Negative cultures are reported as “MRSA not isolated”. After the first swab, laboratories do not usually report antibiotic susceptibilities. Decolonisation (Suppression) of MRSA Regimens aim to reduce MRSA below detection level at time of risk, to decrease chance of infection and spread. Decolonisation/Suppression should usually take place in the 5 days prior to operation, as it may not be successful in the long term. Nasal and skin treatments may only suppress MRSA, therefore always advise admitting ward of patient’s MRSA status, to allow appropriate pre-operative preparation and prophylaxis. Systemic treatment should only be prescribed in line with local policy for established infection. How do I suppress MRSA? To reduce persistent MRSA carriage, treat underlying skin conditions (e.g. eczema, dermatitis), remove and/or replace invasive devices and treat skin breaks. Choice of skin regimen for patients with underlying skin conditions should consider the potential for skin irritation. Where necessary, seek advice from Dermatologist or Microbiologist. 41 Decolonisation (Suppression) of MRSA Always use both nasal and skin regimens NASAL 2% MUPIROCIN in paraffin base 3 times a day for 5 days Apply matchstick-head sized amount of ointment to inner surface of each nostril. Patients should be able to taste Mupirocin at back of the throat. PLUS SKIN 4% CHLORHEXIDINE GLUCONATE body-wash/ shampoo. DAILY for 5 days. OR Second line e.g. if patient has irritant dermatitis): OCTENISAN body-wash/ shampoo. DAILY for 5 days. Moisten skin and apply undiluted antiseptic then rinse. Particularly apply to known carriage sites (axilla, groin & perineum). Wash hair using antiseptic body-wash/shampoo at least twice during the 5 days. After washing, use clean towels, sheets and clothing. Launder items separately from other family members, using as high a temperature as fabric allows. 42 MRSA TREATMENT What do I use to treat a patient with MRSA Infection? MRSA can cause infection at any site. Deep seated infection e.g. osteomyelitis may not respond to antibiotics alone and may need surgical intervention. Skin and Soft Tissue Infection and UTI or RTI zz Total daily dose dependant on severity of infection. zz Severe soft tissue infection may require up to three weeks antibiotics. zz For osteomyelitis or septic arthritis please consult a Micro-biologist. First line if sensitive: DOXYCYCLINE 200mg OD oral for 7-10 days Second line if sensitive: RIFAMPICIN 600mg OD or BD oral 7-10 days PLUS OR FUSIDIC ACID 500mg TDS oral 7-10 days If sensitive: CLINDAMYCIN 450mg QDS oral for 7-10 days Stop Clindamycin if diarrhoea occurs Patients with severe or deep seated infection may be discharged from hospital to complete a course of: LINEZOLID 600mg BD oral Note that this drug has a maximum 28 day license, and requires monitoring of FBC weekly, and assessment of the risk of peripheral neuropathy including optic neuropathy: see BNF or seek specialist advice if not previously prescribed. 43 DENTAL INFECTIONS Derived from the 2011 SDCEP Guidelines (Scottish Dental Clinical Effectiveness Programme) This guidance is not designed to be a definitive guide to oral conditions. It is for GPs for the management of acute oral conditions pending being seen by a dentist or dental specialist. GPs should not routinely be involved in dental treatment and, if possible, advice should be sought from the patient’s dentist, who should have an answer-phone message with details of how to access treatment out-of-hours, or NHS 111. Mucosal Ulceration and Inflammation (simple gingivitis) zz Temporary pain and swelling relief can be attained with saline mouthwash SIMPLE SALINE MOUTHWASH – (Half a teaspoon of salt dissolved in a glass of warm water) zz Use antiseptic mouthwash if more severe and pain limits oral hygiene to treat or prevent secondary infection CHLORHEXIDINE 0.12%-0.2% Rinse mouth for 1 minute BD with 5ml diluted in 5-10mls of water. Do not use within 30 minutes of toothpaste. zz The primary cause for mucosal ulceration or inflammation (aphthous ulcers, oral lichen planus, herpes simplex, oral cancer) needs to be evaluated and treated HYDROGEN PEROXIDE 6% Rinse mouth for 2 mins TDS with 15mls diluted in half a glass of warm water. For each always spit out after use. Use until lesions resolve or less pain allows oral hygiene. 44 Acute Necrotising Ulcerative Gingivitis zz Commence Metronidazole and refer to Dentist for scaling and oral hygiene advice METRONIDAZOLE 400mg TDS oral for 3 days zz Use Metronidazole in combination with antiseptic mouthwash if pain limits oral hygiene CHLORHEXIDINE 0.12%-0.2% Rinse mouth for 1 minute BD with 5ml diluted in 5-10mls of water. Do not use within 30 minutes of toothpaste. zz The primary cause for mucosal ulceration or inflammation (aphthous ulcers, oral lichen planus, herpes simplex, oral cancer) needs to be evaluated and treated HYDROGEN PEROXIDE 6% Rinse mouth for 2 mins TDS with 15mls diluted in half a glass of warm water. For each always spit out after use. Use until less pain allows oral hygiene. 45 Pericoronitis zz Pericoronitis is the inflammation and infection of perimolar soft tissue, often provoked by emerging molar teeth. zz Refer to Dentist for irrigation and debridement zz If persistent swelling or systemic symptoms use Metronidazole zz For severe infections ADD Amoxicillin to Metronidazole METRONIDAZOLE 400mg TDS oral for 3 days Second line or additional for severe infections (see above): AMOXICILLIN 500mg tds oral for 3 days zz Use antiseptic mouthwash if pain and trismus limit oral hygiene CHLORHEXIDINE 0.12%-0.2% Rinse mouth for 1 minute BD with 5ml diluted in 5-10mls of water. Do not use within 30 minutes of toothpaste. OR HYDROGEN PEROXIDE 6% Rinse mouth for 2 mins TDS with 15mls diluted in half a glass of warm water. For each always spit out after use. Use until lesions resolve or less pain allows oral hygiene. 46 Dental Abscess zz Regular analgesia should be first option until a dentist can be seen for urgent drainage; repeated courses of antibiotics for abscess are inappropriate. Repeated antibiotics alone, without drainage are ineffective in preventing spread of infection. zz Antibiotics are recommended if there are signs of severe infection, systemic symptoms or high risk of complications zz Use higher dose antibiotics for more severe infections zz Severe odontogenic infections; defined as cellulitis plus signs of sepsis, difficulty in swallowing, impending airway obstruction, Ludwigs angina. Refer urgently for admission to protect airway, achieve surgical drainage and IV antibiotics. zz The empirical use of Cephalosporins, Co-amoxiclav, Clarithromycin, and Clindamycin do not offer any advantage for most dental patients and should only be used if no response to first line drugs when referral is the preferred option If pus: Drain by local incision, tooth extraction or via root canal. Send pus for microbiology. AMOXICILLIN 500mg-1g TDS oral for 5 days (Review at 3 days) OR PHENOXYMETHYLPENICILLIN 500mg-1g QDS oral for 5 days (Review at 3 days) If penicillin allergy: CLARITHROMYCIN 500mg BD oral for 5 days (Review at 3 days) For severe or spreading infection (lymph node involvement, systemic signs, fever, malaise) ADD: METRONIDAZOLE 400mg TDS oral for 5 days For Metronidazole allergy use: CLINDAMYCIN 300mg QDS oral for 5 days 47 Antibiotic Activities (based on local data) Greater than 90% 80-90% sensitive 70-80% sensitive sensitive 50-70% sensitive Classes of antibiotics for Gram positive bacteria: Penicillins ACG Streps Strep pneumo Penicillin V 99% 93% Amoxicillin 99% Not tested Flucloxacillin Co-amoxiclav 99% No data Macrolides Erythromycin Not tested Not tested Clarithromycin 90% 89% Tetracyclines 80% 92% Cephalosporins Cefalexin No data No data Cefotaxime No data 98% Cefixime Others Trimethoprim Quinolones (e.g. Ciprofloxacin) Levofloxacin 99% Clindamycin No data No data Linezolid No data No data Teicoplanin (iv) No data No data Dapytomycin (iv) No data No data Gentamicin (iv) Enterococci Not tested 99% Not tested 99% Less than 50% sensitive Staph aureus 18% MRSA 0% by definition 100% Not tested Not tested Not tested Not tested Not tested 84% 95% Not tested 40% 94% Not tested Not tested Not tested No data No data No data Not tested Not tested Not tested 93% 86% (do not use alone) No data 100% 100% No data 99% 62% 24% No data 99% 100% No data 96% No data No data No data Antibiotics for Anaerobic bacteria: Metronidazole, Co-amoxiclav and Clindamycin all have activity against anaerobes. 48 Not tested/ not appropriate) Antibiotic Activities (based on local data) Classes of antibiotics for Gram negative bacteria Penicillins Haem influenza Moraxella catarrhalis Other Coliforms Pseudomonas aeruginosa Amoxicillin 74% Not tested 40% Not tested Co-amoxiclav 93% 99% 69% Not tested Macrolides Erythromycin 28% 96% Not tested Not tested Clarithromycin 35% 96% Not tested Not tested Tetracyclines 99% 99% Not tested Not tested Cephalosporins Cefalexin No data No data No data Not tested Cefotaxime 99% No data Not tested Not tested Cefixime 99% No data 95% No tested Others Trimethoprim No data No data Not tested Not tested Quinolones (eg Ciprofloxacin) 99% 99% 91% No data Gentamicin (iv) No data No data 96% No data Penicillin V, Clindamycin, Linezolid, Teicoplanin and Daptomycin have no anti-Gram negative activity. GP urine sensitivities: all causes UTI (based on local data) Amoxicillin 51% Nitrofurantoin 91% Trimethoprim 71% Ciprofloxacin 96% Others Co-amoxiclav 86% Cefalexin No data Fluconazole has activity against Candida albicans but limited activity against non-albicans Candida. For these consider Itraconazole if an oral agent is required, or consult a Microbiologist. All data collected or extrapolated from local primary care specimen sensitivities only, hence data not available for all drug/bug combinations. 49
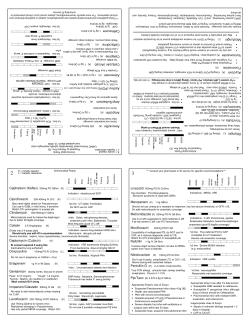
© Copyright 2026