쐽 Iloperidone ꔴ SPECIAL CONCERNS
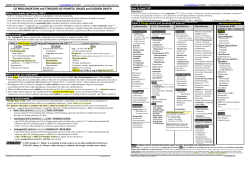
Iloperidone 쐽 SPECIAL CONCERNS ( EYE -loh- PER -i-done) Classification(s): Antipsychotic. RX: Fanapt. INDICATIONS/USES Acute treatment of schizophrenia in adults. NOTE: When deciding whether to prescribe iloperidone, consider the drug is associated with prolongation of the QTc interval. ACTION/KINETICS Action Mechanism is unknown. High affinity for dopamine D2, D3 and serotonin 5-HT2A receptors; moderate affinity for dopamine D4, serotonin 5HT6 and 7, and norepinephrine NEalpha 1 receptors; and, low affinity for serotonin 5-HT1A, dopamine D1, and histamine H1 receptors. Manifests moderate incidence of sedation and orthostatic hypotension and a low incidence of extrapyramidal symptoms, anticholinergic effects, and weight gain. Pharmacokinetics Well absorbed; relative bioavailability: 96%. Peak plasma levels: 2–4 hr. Can be given without regard to meals. Metabolized primarily by three pathways: carbonyl reduction, hydroxylation (mediated by CYP2D6), and O-demethylation (mediated by CYP3A4); there are both extensive and poor metabolizers. One of the metabolites (P88) is active. Excreted in both the urine (about 50%) and feces (about 20%). t1/2, elimination: 18, 26, and 23 hr, respectively, for iloperidone, P88, and P95 (another metabolite) in extensive metabolizers and 33, 37, and 31 hr, respectively, for poor metabolizers. Plasma protein binding: About 95%. CONTRAINDICATIONS Hypersensitivity to iloperidone or any component of the product. Use with other drugs known to prolong QTc. Use in those with hepatic impairment, in those with dementia-related psychosis, in those with congenital long QT syndrome, in those with a history of cardiac arrhythmias, in those with a history of significant CV illness (e.g., QT prolongation, recent acute MI, uncompensated heart failure). Lactation. ꔴ (1) Increased mortality in elderly clients with dementia-related psychosis. Elderly clients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analysis of 17 placebocontrolled trials (modal duration, 10 weeks), largely in clients taking atypical antipsychotic drugs, revealed a risk of death in the drugtreated clients of between 1.6 and 1.7 times the risk of death in placebo-treated clients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated clients was about 4.5%, compared with a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either CV (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. (2) Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to antipsychotic drug as opposed to some characteristic(s) of the clients is not clear. (3) Iloperidone is not approved for the treatment of clients with dementia-related psychosis. ꔴ ● Use with caution with known CV disease (e.g., heart failure, history of MI ischemia, conduction abnormalities), CV disease, or conditions that predispose to hypotension (e.g., dehydration, hypovolemia, antihypertensive drugs). ● Use with caution in those at risk for aspiration pneumonia (e.g., elderly especially those with advanced Alzheimer’s dementia). ● Those with Parkinson’s disease or dementia have an increased sensitivity to antipsychotic drugs. ● Use with caution when used with other CNS drugs and alcohol. ● Safety and efficacy not known in children and adolescents. SIDE EFFECTS Most Common Dizziness, dry mouth, fatigue, nasal congestion, somnolence, tachycardia, orthostatic hypotension, increased weight. CNS: Dizziness, somnolence, extrapyramidal disorder, tremor, lethargy, tardive dyskinesia, extra- pyramidal symptoms (akathisia, bradykinesia, dyskinesia, Parkinsonism, tremor), dystonia, pseudoparkinsonism, vertigo, depression (may be significant), seizures, suicide attempt, paresthesia, psychomotor hyperactivity, restlessness, amnesia, aggression, delusion, hostility, paranoia, confusional state, mania, catatonia, mood swings, panic attack, OCD, bulimia nervosa, delirium, psychogenic polydipsia, impulse-control disorder. Impaired judgment, thinking, or motor skills. GI: Nausea, dry mouth, diarrhea, abdominal discomfort, dysphagia, gastritis, salivary hypersecretion, fecal incontinence, mouth ulceration, aphthous stomatitis, duodenal ulcer, esophageal ulcer, esophagitis, hiatal hernia, hyperchlorhydria, lip ulceration, GERD, reflux esophagitis, stomatitis, cholelithiasis. CV: Tachycardia, bradycardia, orthostatic hypotension, hypotension, syncope, palpitations, arrhythmia, first-degree AV block, CHF, acute cardiac failure. Prolongation of QT interval leading to arrhythmia (including torsades de pointes and sudden death). NOTE: Elderly clients with dementia-related psychosis are at an increased risk of death and CV-related side effects, including stroke. Respiratory: Nasopharyngitis, URTI, bronchopneumonia, nasal congestion, dyspnea, epistaxis, asthma, rhinorrhea, sinus congestion, nasal dryness, dry throat, sleep apnea syndrome, exertional dyspnea. Musculoskeletal: Arthralgia, joint pain, musculoskeletal stiffness, difficulty walking, myalgia, muscle spasms, torticollis, restless legs syndrome. Dermatologic: Rash, skin pigmentation (especially in women on long-term therapy). GU: Ejaculation failure, priapism, decreased/loss of libido, anorgasmia, urinary incontinence, dysuria, pollakiuria, enuresis, nephrolithiasis, urinary retention, acute renal failure, erectile dysfunction, testicular pain, amenorrhea, breast pain, irregular menses, gynecomastia, menorrhagia, metrorrhagia, menstrual irregularities, urinary retention, postmenopausal hemorrhage, prostatitis. Metabolic/Endocrine: Hyperglycemia, diabetes mellitus, hypothyroidism. Hematologic: Leukopenia, neutropenia, anemia, iron deficiency anemia, thrombocytopenia, agranulocytosis. Ophthalmic: Blurred vision, conjunctivitis (including allergic), dry eyes, blepharitis, eyelid edema, eye swelling, lenticular/corneal opacities, cataract, hyperemia, nystagmus. Otic: Tinnitus. Body as a whole: Fatigue, weight gain/loss, edema, thirst, hyperthermia, dehydration, fluid reten- tion. Miscellaneous: Neuromalignant syndrome (including symptoms of hyperpyrexia, muscle rigidity, altered mental status, catatonic signs, irregular pulse or BP, tachycardia, diaphoresis, cardiac dysrhythmia, rhabdomyolysis, acute renal failure). Disruption of control of body temperature, increased appetite. LABORATORY TEST CONSIDERATIONS e Neutrophils. a H&H. Hyperprolactinemia, hypokalemia. DRUG INTERACTIONS Amiodarone / Prolongation of QTc interval c cardiac arrhythmias, including torsades de pointes; use together contraindicated Chlorpromazine / Prolongation of QTc interval c cardiac arrhythmias, including torsades de pointes; use together contraindicated Fluoxetine / e Iloperidone blood levels R/T inhibition of CYP2D6 Gatifloxacin / Prolongation of QTc interval c cardiac arrhythmias, including torsades de pointes; use together contraindicated Ketoconazole / e Iloperidone blood levels R/T inhibition of CYP3A4 Methadone / Prolongation of QTc interval c cardiac arrhythmias, including torsades de pointes; use together contraindicated Moxifloxacin / Prolongation of QTc interval c cardiac arrhythmias, including torsades de pointes; use together contraindicated Paroxetine / e Iloperidone blood levels R/T inhibition of CYP2D6 Pentamidine / Prolongation of QTc interval c cardiac arrhythmias, including torsades de pointes; use together contraindicated Procainamide / Prolongation of QTc interval c cardiac arrhythmias, including torsades de pointes; use together contraindicated Quinidine / Prolongation of QTc interval c cardiac arrhythmias, including torsades de pointes; use together contraindicated Sotalol / Prolongation of QTc interval c cardiac arrhythmias, including torsades de pointes; use together contraindicated Thioridazine / Prolongation of QTc interval c cardiac arrhythmias, including torsades de pointes; use together contraindicated HOW SUPPLIED Tablets: 1 mg, 2 mg, 4 mg, 6 mg, 8 mg, 10 mg, 12 mg. DOSAGE TABLETS Schizophrenia in adults. Adults, initial: 1 mg twice a day on day 1; then, 2, 4, 6, 8, 10, and 12 mg twice a day on days, 2, 3, 4, 5, 6, and 7 respectively. Maintenance: 6–12 mg twice a day. Maximum dose: 12 mg twice a day (i.e., 24 mg/day). No data are available to determine the length of treatment; however, those responding should be continued beyond the acute response. Periodically reassess to determine the need for continued treatment. NURSING IMPLICATIONS IMPLEMENTATION/ADMINISTRATION/STORAGE 1. Dosage adjustment is not routinely indicated on the basis of age, gender, race, or renal impairment. 2. Can be given without regard to meals. 3. Titrate slowly from a starting dose to avoid orthostatic hypotension (iloperidone is an alpha-adrenergic blocker). 4. Clients must be titrated to an effective dose. Thus, control of symptoms may be delayed during the first 1–2 weeks of therapy compared with some other antipsychotic drugs that do not require similar titration. 5. Reduce the dose of iloperidone by one-half if coadministered with strong CYP2D6 inhibitors (e.g., fluoxetine, paroxetine). When the CYP2D6 inhibitor is withdrawn, increase the iloperidone dose to where it was before. 6. Reduce the dose of iloperidone by one-half if coadministered with strong CYP3A4 inhibitors (e.g., clarithromycin, ketoconazole). When the CYP3A4 inhibitor is withdrawn, increase the iloperidone dose to where it was before. 7. Poor metabolizers of CYP2D6 have a higher exposure to iloperidone compared with extensive metabolizers. Laboratory tests can determine CYP2D6 poor metabolizers. 8. Whenever a client has had an interval of more than 3 days off iloperidone, reinitiate using a titration schedule. 9. When switching from other antipsychotics, immediate discontinuation may be appropri- ate for some clients but not others. In all cases, the period of overlapping medications should be minimized. 10. Store from 15–30°C (59–86°F). Protect from light and moisture. ASSESSMENT 1. Note reasons for therapy, clinical, and behavioral manifestations, other agents trialed and outcome. 2. Assess for any history of CVD, QT prolongation, arrhythmias, or dementia related psychosis. 3. Monitor VS, ECG, weight, CBC, K+, Mg++, BS, renal and LFTs. CLIENT/FAMILY TEACHING 1. Review dosing guidelines and take as prescribed with or without food. Drug is started at a low dose and titrated up slowly to prevent sudden drop in BP. 2. Avoid activities that require mental alertness until drug effects realized; may impair judgment, thinking, or motor skills. 3. Change positions slowly to prevent a sudden drop in BP. Hot tubs, hot showers, or baths may aggravate dizziness. 4. Practice reliable contraception, report if pregnancy suspected. 5. May alter temperature regulation. Avoid alcohol, CNS depressants, OTC agents, strenuous exercise, overheating, or dehydration. 6. Report any suicide ideations, change in ability to interact or increased psychosis. 7. Any S&S of NMS (neuroleptic malignant syndrome): increased temperature, muscle rigidity, irregular heart rate/BP, arrhythmias, or severe diaphoresis require immediate attention. 8. Report any movements that become involuntary, slow, repetitive, rhythmical (tardive dyskinesia) in select or groups of muscles; may become irreversible. 9. Keep all F/U to assess response and for adverse SE. OUTCOMES/EVALUATE ● Improvement in PANSS and DSM III/IV-TR schizophrenia criteria ● Improved behavioral and emotional presentation ● a Delusions/suspiciousness and hostility
© Copyright 2026