In Translation Graft-Induced Dyskinesias in Parkinson’s Disease: What Is It All About?
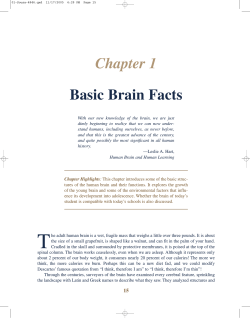
Cell Stem Cell In Translation Graft-Induced Dyskinesias in Parkinson’s Disease: What Is It All About? Roger A. Barker1,* and Wei-Li Kuan1 1Brain Repair Centre and Department of Neurology, University of Cambridge, Cambridge CB2 0PY, UK *Correspondence: [email protected] DOI 10.1016/j.stem.2010.07.003 The treatment of Parkinson’s disease with grafts of fetal ventral mesencephalic tissue has shown some success, but can result in graft-induced dyskinesias (GIDs). Recently in Science Translational Medicine, Politis et al. (2010) demonstrate that GIDs may originate from serotoninergic neurons that are cografted in these transplants. Parkinson’s disease (PD) is a common termed graft-induced dyskinesias (GIDs) neurodegenerative disorder of the central (reviewed in Goya et al., 2007). GIDs are nervous system (CNS). PD is character- phenomenologically different from LIDs ized by the loss of neurons at a number and are not obviously related to L-dopa of CNS and non-CNS sites, which is medication and persist in the absence of accompanied by the formation of a-synu- anti-PD medication. The etiology of GIDs clein-positive Lewy bodies (Braak et al., 2006). The etiology of this condition remains obscure in the Normal A majority of cases, although nearly 50 DA 5HT years ago it was recognized that patients experience degeneration of the nigrostriatal dopaminergic pathway, and that using dopaminergic DAT 5-HTT drugs to substitute for this loss can ameliorate many of the symptoms in the short term. However, these agents are not curative and with time complications arise with their use, Postsynaptic c dopamine dopam receptors including the development of unpreGID B dictable motor responses (on-off phenomena) and the genesis of DA 5HT abnormal, involuntary dyskinetic movements (L-dopa-induced dyskinesias, LIDs). As a result, more definDAT T 5-HTT 5 itive reparative strategies have been sought, one of which involves using grafts containing fetal dopaminergic neuroblasts derived from the developing human ventral mesencephalon Postsynaptic c dopamine dopam receptors (VM). These transplants, when placed into the striatum of patients with PD, Buspirone Treatment C can produce clear clinical benefits, albeit inconsistently (Goya et al., DA 5HT 2007). The heterogeneity of patient responses has always been an area of concern, but an additional serious DAT AT 5HT1A problem with this approach was iden5-HTT 5-H tified in the early part of this century during two double-blind, placebobuspirone controlled trials. These studies revealed that the grafts themselves Postsynaptic dopamine receptors could induce dyskinetic movements, 148 Cell Stem Cell 7, August 6, 2010 ª2010 Elsevier Inc. has been the subject of intense debate, and a predominant hypothesis under examination names dopamine (DA) as the causative agent and suggests that the grafts either release too much dopamine or release it unevenly across the striatal complex (Figure 1; Ma et al., 2002). Recently, however, attention has turned toward the population of serotoninergic or 5-hydroxytryptamine (5HT) neurons within the graft, which arise developmentally just caudal to the VM and are therefore also transplanted. This suggestion that the 5HT cells within the VM transplant may be important has its origins in recent work on LIDs, where it has been shown that exogenously supplied L-dopa Figure 1. Proposed Mechanism of Buspirone Attenuation of GID (A) In the graft of all patients there is a mixture of dopaminergic and serotonergic neurons, the release of dopamine (orange dots) can be regulated by presynaptic dopamine transporters (DAT), and the release of 5HT (blue dots) by serotonin transporters (5-HTT). In patients without GIDs, these neurons take up their own neurotransmitter and there is no real dialog between them. (B) In patients with GIDs, the serotonergic terminals hyperinnervate the striatum in the grafted patient, and large amounts of 5HT are released, which may be able to reverse or alter the capacity of the DAT, thereby causing a greater release of dopamine from the grafted dopaminergic nerve terminals. In addition, the 5HT transporter can also take up dopamine and then release it as a false transmitter from the 5HT nerve terminal. (C) Buspirone, a selective 5HT1A agonist, was used to activate the presynaptic 5HT1A receptor to dampen the release of serotonin from serotonergic terminals. Reduced levels of 5HT leads to a change in DAT and 5-HTT activity and restores more regulated dopamine release from the grafted dopaminergic neurons. Cell Stem Cell In Translation can be converted, stored, and released by the serotonergic terminals (Tanaka et al., 1999) but not inactivated because such cells lack dopamine transporters. Nevertheless, targeting the presynaptic inhibitory serotonergic receptors can attenuate LIDs in a rat model of PD (Mun˜oz et al., 2008), and selective lesioning of serotonergic afferent projections to the striatum can almost completely abolish their development (Carta et al., 2007). It is therefore logical to assume that some similar process may be taking place in the VM transplants (Mendez et al., 2008), and as such these cells could be at least partially responsible for the development of GID. In a new study published recently in Science Translational Medicine (Politis et al., 2010), the authors use PET imaging and the specific serotonin transporter ligand, 11C-DASB, to explore this possibility in two VM-grafted PD patients that exhibit GIDs. Their results indicate that these patients have a 5HT hyperinnervation of the grafted striatum, which in itself is not surprising given what we already know about the pathology of such grafts. However, the authors extend their findings to show that a specific 5HT1A agonist, buspirone, lessens the GIDs without any worsening of the patients’ underlying Parkinsonism. This result suggests that the drug works relatively selectively by activating the presynaptic 5HT autoreceptor (Figure 1), which in turn leads to a reduction in dopamine release from the transplanted neurons. This hypothesis is intriguing, yet it remains unclear how exactly this dialog between the serotonin and dopaminergic neurons leads to GIDs. For example, one would anticipate that the grafted dopaminergic neurons should take up any excessive dopamine released within the transplant. However, the authors propose that the defect stems from changes in how the dopamine transporter behaves during serotoninergic hyperinnervation. There is evidence from other studies to suggest that the dopamine transporter can change its activity and direction of dopamine flux as a function of 5HT, but activity modulation of this sort has not been shown in this study in these patients. Furthermore, it is not clear why only some transplanted patients develop GIDs, given that all VM grafts contain a proportion of developing 5HT neurons. Indeed, even in the two cases reported by Politis and colleagues, the extent of GIDs is similar despite the presence of different levels of 5HT reinnervation within the striatum. Finally, according to the authors’ model, it would be expected that GIDs should worsen with L-dopa therapy, and yet this pattern has not been observed thus far. Overall, the findings reported in this paper highlight the importance of nondopaminergic networks in the genesis of dyskinesias, and therefore attention must be paid to this relationship in new trials of fetal VM transplants for PD. In contrast, these findings may present a less serious issue for the world of stem cell transplantation in PD, given that the goal of the field has always been to produce a relatively uniform population of true nigral dopaminergic neurons. Achieving this goal seems increasingly likely, although no consensus yet exists as to the definition of a true nigral dopaminergic neuron (Li et al., 2008). Nevertheless, multipotent stem cell sources can be engineered to selectively generate specific cell fates and the current data from Lindvall and colleagues suggests that it will be important to avoid the genesis of 5HT neurons in this setting. However, it is likely that Politis et al. have only partly explained the source of GIDs and that the location of the transplanted dopaminergic neurons within the striatal complex and their local innerva- tion capabilities also contribute to the genesis of these abnormal movements (Carlsson et al., 2006). Finally, it is worth noting that this study shows that dopaminergic cell transplants produce benefits on motor control that may take years to mature, as is evident by the reduction in UPDRS more than 13–16 years after grafting. Thus, judging the success or otherwise of (stem) cellular repair approaches to PD will, and cannot, be ultimately achieved via studies with short follow-up periods. REFERENCES Braak, H., Bohl, J.R., Mu¨ller, C.M., Ru¨b, U., de Vos, R.A., and Del Tredici. Stanley Fahn, K. (2006). Lecture 2005. Mov. Disord. 21, 2042–2051. Carlsson, T., Winkler, C., Lundblad, M., Cenci, M.A., Bjo¨rklund, A., and Kirik, D. (2006). Neurobiol. Dis. 21, 657–668. Carta, M., Carlsson, T., Kirik, D., and Bjo¨rklund, A. (2007). Brain 130, 1819–1833. Goya, R.L., Kuan, W.L., and Barker, R.A. (2007). Expert Opin. Biol. Ther. 7, 1487–1498. Li, J.Y., Christophersen, N.S., Hall, V., Soulet, D., and Brundin, P. (2008). Trends Neurosci. 31, 146–153. Ma, Y., Feigin, A., Dhawan, V., Fukuda, M., Shi, Q., Greene, P., Breeze, R., Fahn, S., Freed, C., and Eidelberg, D. (2002). Ann. Neurol. 52, 628–634. Mendez, I., Vin˜uela, A., Astradsson, A., Mukhida, K., Hallett, P., Robertson, H., Tierney, T., Holness, R., Dagher, A., Trojanowski, J.Q., and Isacson, O. (2008). Nat. Med. 14, 507–509. Mun˜oz, A., Li, Q., Gardoni, F., Marcello, E., Qin, C., Carlsson, T., Kirik, D., Luca, M.D., Bjo¨rklund, A., Bezard, E., and Carta, M. (2008). Brain 131, 3380–3394. Politis, M., Wu, K., Loane, C., Quinn, N.P., Brooks, D.J., Rehncrona, S., Bjorklund, A., Lindvall, O., and Piccini, P. (2010). Science Translational Medicine. Published online June 23, 2010. 10.1126/scitranslmed.3000976. Tanaka, H., Kannari, K., Maeda, T., Tomiyama, M., Suda, T., and Matsunaga, M. (1999). Neuroreport 10, 631–634. Cell Stem Cell 7, August 6, 2010 ª2010 Elsevier Inc. 149
© Copyright 2026