“Recovering A-NEW” A Culturally Competent Cognitive/Behavioral Treatment Model
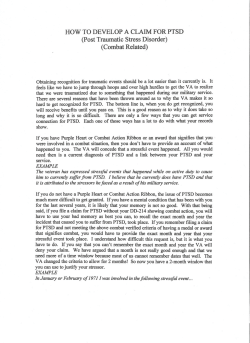
“Recovering A-NEW” A Culturally Competent Cognitive/Behavioral Treatment Model Ground Zero: The Urban War Zone Presenter(s): Ronald Beavers, Ph.D. Shawna Charles, Ph.D. Cand. [email protected] Veterans Service Outreach Program-VSOP of PIF, Inc. Los Angeles, California Authored By: Ronald Beavers Ground Zero: The Urban War Zone Goals Today • Think about best care • Think about priorities for change in treatment of women with Trauma • Questions: – What are special challenges of treatment in the community? – What are most important changes in practice to adjust treatment for women with Trauma? – What will have most impact? – What can be changed? Historic Changes? • Improvements… – Continued implementation of Community Stressors for PTSD/SUD – First routine screening that is cultural competent for PTSD in South Los Angeles Ground Zero: Urban War Zone – Court Mandated individual sessions immediately, 3 to 6 months after court ordered – PTSD/SUD Cultural Practice Guidelines – Significant Community interest in evidencebased care (Recovering A-New) – Efforts to better integrate TX, and Social care – Access and appropriate care – Training initiatives – Community integration of mental health planning, and services – Community research on PTSD/MH in CBO’s CBO’s Fundamentals are Strong • • • • Caring professionals Extensive system of care Performance orientation Expertise related to problems of community, e.g. … – PTSD – SUD – Anger – Guilt – Bereavement • Support for innovation Community Treatment More Visible? • Federal Gov’t and Local Officials City/County Departments attention, with political relevance • Greater importance of: – – – – Accountability Outcome measurement Accessibility of services Community Customer satisfaction Ground Zero: The Urban War Zone Stressors Crime Type 2006 Total Per 100,000 People National per 100,000 People Overall Los Angeles Crime Index 135985 3505.3 4479.3 Los Angeles Violent Crimes 30526 786.9 553.5 Los Angeles Murders 480 12.4 7 Los Angeles Rapes 1059 27.3 33.1 Los Angeles Robberies 14353 370 205.8 Los Angeles Aggravated Assaults 14634 377.2 336.5 Los Angeles Property Crimes 105459 2718.4 3906.1 Los Angeles Burglaries 20359 524.8 813.2 Los Angeles Larceny/Thefts 59711 1539.2 2601.7 Los Angeles Motor Vehicle Thefts 25389 654.4 501.5 Los Angeles Arsons 1 2356 60.73 N/A Based on the final 2008 FBI Crime Reports. LA City Crime Report 2007 - 2008 Challenges for Community in Delivering Best Care for Re-entry, and All • New issues (Re-entry) • Familiar problems, new twists • Historic problems, continuing challenges (Inadequate and a disparity in mental/health care, i.e., South Central even before Watts Riot (1965 ) New Issues • African American Men Access to Appropriate Care • Women and Their Children • Appropriate Assessing and Diagnosing** – Family involvement – Importance of cultural competency – Clinical and Social functioning Younger Clients • Stage-of-life issues – Still working/desire to work – School issues – Significant family roles • Son or daughter • Parent • Spouse – Finding and forming relationships – Activity levels higher – Integration with civilian life • Provider-patient discrepancies in age? • Q: When do you think it went wrong? Women Clients • More women with PTSD/SUD into Community care • Are we ready? – Specialist women services – Female staff – General climate • How integrate with men? – Trauma/SUD work Focus on Functioning/Role Maintenance? • Marriage-family-work-social connection: These suffered in returning to the community. • These represent quality of life, that PTSD disrupts • If returnees fail or experience significant impairment in these domains, this may help maintain PTSD • Should we organize treatment around partner, family, work, social, and PTSD? Family Issues • Partner conflict-divorce prevention • Sexual functioning • Parenting skills • Domestic violence • Budgeting skills • Impact on family members Spouse/Partner/Family Involvement in Care? • Not just the province of family clinics • Partners/Parents – Include in assessment process – Involve in treatment planning if possible – Involve in treatment • Management of current stressors, social activities, positive recreation • Couples functioning? – Couples conflict resolution/problem solving? – Mechanisms? • SO or couples groups • Cognitive-behavioral couples therapy? • Workshops Treatment Works, when you Work-it! ++ +- - Healthy-life Style Treatment/Drug free lacking No Support Poor habits Denial Non-Tx. AUTHENTIC ADAPTIVE ADOPTIVE __ Social Malady Disease/Death ABERRANT "Seven Virtues of Ma’at" ORDER : BALANCE: HARMONY: COMPASSION: RECIPROCITY: JUSTICE: TRUTH: The Recovering A-New: What are we facing S.C. LA Our Morbidity reflects the needs in treatment which address the populations that is of greater risk for trauma, e.g., youth in intercities, community combat, rape victims, murder, abused youth (physically and/or sexually) and the ever increasing domestic violence; these primary variables can have constellated features and manifesting other complex disorders. The Recovering A-New: What are we facing S.C. LA Cont. • The population that is most affected are African Americans, Latinos, adolescents and women, which appear to be greater impacted and are at higher risk in the actual manifestation of Post Traumatic Stress Disorder; this sometimes precipitate the use of alcohol and/or illicit chemicals to psychologically numbing, and avoidance from the sometimes overwhelming symptoms of Post Traumatic Stress Disorder PTSD. This material is more culturally competent that address the critical as well as complex issues which encompass the different levels of trauma, and its impact on this population. Possible Topics in Couples Skills Training • What is PTSD? • Triggers for PTSD symptoms • Planning together to manage problem • Coping with problem situations – Social isolation – Parenting – Anger – Substance abuse • Communication training – Communication of positive emotions • Commitment to change • Self-care for significant others PTSD/SUD CBO’s In Recovery? • SESSION PSYCHO-EDUCATION In/Out Patient (Cultural Relevance) • MONTH ONE Trauma and Addiction (CoMorbidity): Overview Disease of Chemical Dependency Mental Health, Anxiety and Trauma Progress/Symptoms Guilt, Shame, and Recovery Self-help Group, and Individual Session CBO’s in Tx.Recovery Cont. • GROUP: CONTINUING TRAUMA AND RECOVERY PLANNING/RELAPSE PREVENTION (Four (4) times per month) SESSION • MONTH ONE High Risk Factors - Individual Planning Session • MONTH TWO Signs and Symptoms - Individual Planning Session • MONTH THREE Hypervigilance, Startled Response, Memory Make a focus of treatment • Work Success support groups – Coping skills training adapted to changing faulty belief systems. Cultural Specialized Support Groups SPECIALIZED TRACTS (One (1) tract per month) • SPIRITUALITY TRACT WEEK ONE: Spiritual (Becoming Grounded) Recovery WEEK TWO: Open Discussion WEEK THREE Spiritual Recovery - Developing the Inner Voice WEEK FOUR: Having Fun with Spirituality • GRIEF AND LOSS TRACT WEEK ONE: The Grief Process WEEK TWO: Grief and Chemical Dependency WEEK THREE: Cognitive Therapy WEEK FOUR: Behavioral Change Exercise Coping with my anger and solving difficult situations Familiar Problems, The Boogieman • Drug/Alcohol problems • PTSD Drug/Alcohol Problems? Abusing substances… 1. Makes PTSD symptoms worse. Substances can make you feel more depressed, more suicidal, less stable. Even if substance abuse appears to “solve” some PTSD symptoms for a short while (such as getting to sleep or “numbing out” for a few hours), in the long run it never solves them. • 1. Prevents you from knowing yourself. With substances, you get lost. To heal from PTSD, you need to become more and more aware of who you really are—without substances. • 1. Does not get your needs met. You may be using substances to feel loved, to accept yourself, to feel less pain, to feel nurtured. However, substances cannot give you these. You need to learn safe coping methods to gratify these very important needs. Alcohol/Substance Abuse • Screen all patients for PTSD/trauma exposure and alcohol/sa • Integrate PTSD and SA programming? – Patient education – Concurrent PTSD/SA protocols • Seeking Safety (Najavits, 2002) (Beavers, 2010) • Moderation training? • Increase collaboration between PTSD and SA treatment? PTSD • TBI complicate treatment for some? • Importance of driving behavior – Need for in vivo exposure methods • How integrate older and younger Client’s? Historic Problems, and A Solution to our Problem • Lack of cultural specific evidence-based care, application of Practice Guidelines • Lack of culture competency in program evaluation • Mental health stigma • OUR SOLUTION Recovering A-NEW, a Culturally Competent CBT Model evidence-based developed in South Central Los Angeles (Beavers, 2010) Evidence-Based Care/Practice Guidelines • What are leading treatments for PTSD? • Can we deliver them to our community atlarge? • Therapy in the ABPsi’s LCPP Practice Guideline, that is effective. • Significant benefit – Strongly recommended – Cognitive Therapy – Exposure Therapy – Stress Inoculation Training – Behavioral Change Models • Best developed treatments combine the two elements – e.g., Cognitive Processing Therapy (Resick & Schnicke, 1993) Behavioral Change (Nobles, Goddard and Cavill) NTU (Phillips); Recovering A-NEW (Beavers) • Not standard care Trauma-Focused Treatment in CBO’s • Provided for AA, and other minorities In HSA’s • Individual trauma processing – Provided frequently – Requires extended individual care • Group trauma processing – Most common form of trauma-focused treatment – Usually connecting/bonding and telling – Emphasis on safety/trust, support – Powerful, positive emotional experience – Not clear about benefits CB Theoretical Models of PTSD • Behavioral Model (Keane) • Cognitive Models – Emotion Processing Theory (Foa) – Dual Representation Theory (Brewin) – Cognitive Theory of PTSD (Ehlers & Clark) Behavioral Model of PTSD (Keane et al., 1985) • Based on Mowrer’s Two-Factor Learning Theory – Factor 1: Classical Conditioning : Traumatic Event (UCS) paired with Neutral Stimuli (External and Internal) leads to them becoming triggers (CS) of trauma-related distress (CRs). – Factor 2: Operant Conditioning : Trauma triggers (CS) are avoided (or escaped) reducing distress in the short term (- reinforcement) • Failure to Extinguish CR Behavioral Model of PTSD (Nobels, Goddard, and Cavil et al., 1995 • • • • ATHUENTIC ADAPTED ADOPTED ABBERANT • Moving from Aberrant to Authentic State. • ‘African Centered Behavioral Change Model’ Treatment Implications of Behavioral Model • Habituation to trauma-related distress • Repeated exposure to trauma triggers (CS) (external and internal) in absence of negative consequences (UCS) (i.e. extinction of CS) • Discrimination between dangerous and safe situations Emotion Processing Theory (Foa) • PTSD as impaired emotional processing of trauma • Very large pathological fear structure of traumatic event – Contains trauma stimuli, responses, and meaning elements – Easily activated (ambiguous stimuli) and disruptively intense – Disorganized and fragmented – Unrealistic elements – Harmless stimuli associated with escape or avoidance responses – Contain erroneous evaluations or interpretations • “Anxiety will persist until escape” • “Fear will cause harm” (go crazy, become ill) • “These consequences are terrible” Treatment Implications Of Emotional Processing Theory of PTSD • Fear structure must be activated – Exposure • New corrective information must be provided that is inconsistent with pathological elements of fear structure. Via… – Safety – Habituation – Acceptance • Narratives change in successive retellings – Fewer unfinished thoughts, repetitions – Increased reading level of narrative Imaginal Exposure Tactics • 45-90 minutes • Ask for (sensory) details of scene to increase access to memories – Details of scene – Sensory details – As if happening now (use first person to describe) • Ensure slow attention to emotional aspects of memory • Include attention to thoughts and feelings at time of traumatization • Watch for emotional avoidance Exposure Therapy Points (Rothbaum) • Patients should remain in exposure situation long enough for their anxiety to decrease. • Patients should be allowed to progress at their own pace. • Patients should be praised for exposures completed and encouraged to push themselves further. • The clinician should acknowledge how difficult exposure therapy is for the patient. Therapeutic Comments During Imaginal Exposure (Rothbaum) • You’re doing fine, stay with the image. • You’ve done very well. It took some courage to stick it out. • Stay with your feelings. • I know this is difficult. You’re doing a good job. • Stay with the image, you are safe here. • Feel safe and let go of the feelings. Dual Representation Theory (Brewin) • Trauma can lead to 2 types of memory – Verbally-accessible memories (VAMS) (Cortical) • Representations of conscious experience of the trauma • Can be deliberately retrieved • Especially, “meanings” – Situationally-accessible memories (SAMS) (Limbic) • Representations of non-conscious experience • Cannot be deliberately accessed • Representations accessed automatically when in presence of trauma cues/reminders • Conditioned emotional responses Dual Representation Theory (Cont) • 3 endpoints of emotional processing – Completion/integration – Chronic emotional processing (Rumination) • Permanent preoccupation with consequences of trauma and intrusive memories – Premature inhibition of processing • • • • Results from avoidance Continued phobic avoidance Somatization Vulnerable to reactivation later in life Treatment Implications Of Dual Representation Theory of PTSD • SAMS (hot spots) should be identified and transferred into VAMS (cortical inhibition) – Exposure • These new VAMS will compete with the SAMS when triggers are encountered Cognitive Theory of PTSD • Two key processes lead to sense of threat – Differences in appraisal of trauma and sequelae (e.g., intrusive symptoms) – Differences in nature of memory and link to other memories • Perceived threat also motivates behavioral and cognitive responses that prevent cognitive change and therefore maintain the disorder Cognitive Theory of PTSD • Memories characterized by – Mainly sensory impressions – Sense that “happening right now” – Original emotions and sensory impressions are reexperienced – Affect without recollection – Involuntary reexperiencing triggered by wide range of stimuli and situations Treatment Implications Of Cognitive Theory of PTSD • Trauma memory needs to be elaborated and integrated into context of individual’s preceding and subsequent experience • Problematic appraisals that maintain sense of threat need to be modified • Dysfunctional coping strategies that prevent recovery need to be dropped Cognitive Theory of PTSD (Ehlers and Clark) • Individuals with PTSD have “idiosyncratic negative appraisals of the traumatic event and/or its sequelae that have the common effect of creating a sense of serious current threat” • (Ehlers & Clark, 2000, p. 320) Meaning of PTSD • I am a failure Some Negative Appraisals among Female Client’s – I will always be sick and useless. – I let my hommies down because I couldn’t help (watch their back). – I make bad decisions. – Bad things happened because of me. – I am a failure because I was afraid. – I will never have a normal life or normal relationships. – I am an awful person because I couldn't stop that child from being shot. – I wasn’t strong enough (punkn’t out). – I am ashamed of myself and my actions. – I can’t ever get out of this! – I should have been able to stop what was going on around me. Some Negative Appraisals (cont) – I should have been able to save m brother. – I wish I could get out of the hood. – I am the only person I know who got so screwed up from community everyone else is dead. – Know one cares about us. – I can no longer be a good person, etc.). – My friend got killed for nothing. – It seems like everyone besides my hommies hate us and don’t want us around. – If I get close to someone, I’ll hurt them or they might hurt me. – Once a rejection, always a rejection. I’ll never be able to be a normal person again. – My family don’t understand the person I’ve become. Cognitive Processing Therapy • Developed to help trauma survivors… – Understand how thoughts and emotions are interconnected – Accept and integrate the trauma as an event that actually occurred and cannot be ignored – Experience fully the range of traumarelated emotions – Analyze and confront maladaptive beliefs – Explore how prior experiences and beliefs affected reactions and were affected by trauma Session Outline • 1: Introduction and education • 2: The meaning of the event • 3: Identification of thoughts and feelings • 4: Remembering the trauma • 5: Identification of stuck points • 6: Challenging questions • 7: Faulty thinking patterns Session Outline (continued) • • • • • 8: Safety issues 9: Trust issues 10: Power and control issues 11: Esteem issues 12: Intimacy issues and meaning of the event Rationale for CPT • • • • Strong evidence- and theory-base Likely to be palatable for clients and therapists Manual and materials well-developed Some key design features – Most systematic application of cognitive therapy to PTSD – Impact statement first – Session 4 begins exposure – Well-structured homework tasks taking treatment out to the client’s world – Modular themes (Self and Other)… • Safety • Trust • Power and control • Esteem • Intimacy Assessing Cognitions • Trauma-related worries and concerns • Assessment during exposure therapy • Inventories – Posttraumatic Cognitions Inventory • Foa, E.B., Ehlers, A., Clark, D.M., Tolin, D.F., & Orsillo, S.M. (1999). The Posttraumatic Cognitions Inventory (PTCI): Development and validation. Psychological Assessment, 11, 303-314. Anger • Challenge in establishing relationship • Anger programming – – – – – – – – – Goal of treatment Time out/Cool down Anger self-monitoring Identifying anger situations Relaxation/breathing Anger discrimination Self-talk/cognitive therapy Exercise Risk analysis (violence, guns) Guilt • Formal target of treatment • Cognitive therapy for guilt – Cognitive Processing Therapy (Resick & Schnicke, 1993) – Kubany protocol (Kubany, 1998) • Guilt assessment – Trauma-Related Guilt Inventory (Kubany et al., 1996) Bereavement • Assessment – Inventory of Complicated Grief-Revised (Prigerson et al., 1995) • Treatment for traumatic or complicated grief – Education about grief – Restructuring of cognitive distortions about events – Looking at function of anger in bereavement – Restoring positive memories of the deceased – Restoration and acknowledgment of caring feelings toward deceased – Retelling the story of the death – Learning to tolerate painful feelings Assessment Implications • • • • • Warzone experiences Marital/partner relationship Family functioning Work functioning Social environment and behaviors • Activity patterns Systematic Assessment of Community Affiliation Experiences • In PTSD treatment settings… – Consider using High Risk and Trauma Inventory (MISSISSIPPI-C Trauma scale, PCL-C, Sexual Trauma Scale; King, King, & Vogt, 2003) Community Risk and Resilience Inventory • 2 pre-disruption factors – Prior stressors – Childhood family environment • 10 Ground Zero: Urban War Zone factors – Sense of preparedness – Difficult living and working environment – Concerns about life and family disruptions – Deployment social support – Sexual harassment experiences – General harassment – Perceived threat – Severe Hostile experiences – Exposure to aftermath of Violence – Self-reports of nuclear, biological, or chemical exposures • 2 post-disrupiton of trauma factors – Post- clinical and social support – Post-effective (CC) coping with stressors Existing Conflicts • Nature and frequency – Family – Friends – Workplace • Sources of conflict • Key behaviors of others • Coping skills of returnee Community, Social Interaction and Behaviors • Who are supports? – How much contact? – What happens? • Who are problems? – How much contact? – What happens? • Social activities? – – – – How often? What kinds of activities? What happens? Enjoyment? Stress? Healthy Activity Structure • How doe s/he spend time? • Family/partner activities • Social activities – Time alone vs. with others • Recreational activities – Pleasurable? • Work or volunteer work • Spiritual practices/Churchgoing • Problem activities • Counseling/Support groups, e.g., AA, CA, and NA • Keep journals of activities Preventing-Relapse Social Withdrawal/Isolation? • Social isolation as setting for dysfunctional behavior • Need active sustained intervention – Formal treatment goal – Peer systems, task assignments • Isolation in moderation is healthy – Planned isolation • Facilitate affiliation with clean and sober Organizations? • Alumni activities: Can we create/support settings and activities for recovering people , socialize, support one another? Enhancing Cultural Inoculation: Jegna • One showing is worth a thousand telling's (jegna) • Knowing what to do vs. knowing how to do it • Cycle of… – – – – – Instruction Demonstration Rehearsal/practice (rituals) Feedback/coaching (jegna) Practice • Need over-learning Improving Services: Behavioral Tasks During Treatment • Action, not just talk – Communication, for example… • Call partner from home/work • Talk about conflict with peer – Inviting friendship… • Ask to activity and do it – Reducing isolation… • Go to activity in community and report – Buddy system Stigma • Most returnees appear to acknowledge having a problem – Returnees from Prison and/or SUD TX.: >80% of those who screened positive for SUD, MH, or PTSD • Interest in receiving help is much lower – 43% of positive screens LA County Dept. Health Services 2011 Perceived Barriers to Seeking MH Services • I don’t know where to get help (22%) • I don’t have adequate transportation (18%) • It’s difficult to schedule an appointment (45%) • Costs too much money (25%) • I don’t Trust (Men) (80%) • I Don’t Trust Women (40%) • I would be seen as weak (65%) • It would be too embarrassing (41%) • I don’t trust mental health professionals (66%) • Mental health care doesn’t work (25%) • What is PTSD? (75%) CBO’s Experience? • Pattern of first-time visits, not necessarily continuing in counseling (in/out patient) – 3 session education? – Telephone contacts? – Written materials? Organizing Services around their Needs? • • • • • Depression? Respect? Male/Female Client’s? Anxiety? SUD’s? Program/Outcome Evaluation • Systematic assessment and outcome evaluation? • Practice Guideline-Management of PTSD in Mental Health Specialty Care • Goal to promote use of standardized initial and follow-up assessments – Recommend routine use of self-administered checklists – Monitor follow-up status at least every 3 months, using interview and questionnaire methods • Not standard care • CBO’s PTSD/Alcohol Treatment Assessment (CBOPATA) To Improve CBO’s and Health Care Response? • Increase involvement of families in assessment and treatment • Increase focus on maintenance of work functioning • Develop alumni/peer-to-peer programs • Increase CBO’s implementation of evidence-based treatments – CPT • Establish simple outcome measurement – (CBOPATA) • Assure systematic assessment of Client experiences – DRRI Appropriate Care in Our Community!! The “Recovering A-NEW” Group Study: PTSD/Addiction Treatment Groups Group # 1 Baseline N= 13 participants 90 – 180 Days Group #2 Baseline N= 13 participants 90 – 180 Days Two (2) women were referred from program before completion After 90 days average group size N=9 One (1) left program before completion Three (3) women gave birth during participation Three (3) women gave birth during participation Four (4) participants discontinued all use of psychotropic medication 180 days Grp. participation average group size N=9 Two (2) pregnant Two (2) participants discontinued all use of psychotropic medication 180 days Grp. participation average group size N=9 Programs recidivism dropped to 8.66% and Retention 91.44% Total certifications for completion Trauma/Addiction Grp. N=10 Total certifications for completion Trauma/Addiction Grp. N=7 Certifications for completion N=17 Total N=26 After 90 days average group size N=9 Age of Women 19 -52 Mean age 35.5 HSA women all participated in no less than 16 session translating into 32 therapeutic hours. Program had >75 % recidivism Programs recidivism dropped to 8.66% and Retention 91.44% Two (2) pregnant Challenges for ABPsi • • • • Rate of changes is increasing! New skills are demanded Big change agenda Innovation must occur in context of heavy workload in the community • Change Readiness? – Are we ready to learn new approaches and skills? – Are we ready to move out of our “comfort zones” “Healthy Families Build Strong Communities
© Copyright 2026