Document 258939
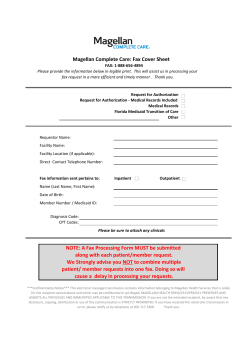
Magellan Behavioral Health of Pennsylvania, Inc. BHRS/RTF Treatment Authorization Cover Sheet Registration ONLY Bucks County Date of Birth (MM/DD/YYYY): Lehigh County / Montgomery County Magellan Provider MIS #: MA ID #: Provider Phone: MAGELLAN USE ONLY Outcome Prob CPT Mod1 Mod2 Code Type 599 H0032 001 U2 HK 599 H2019 001 EP 599 H2019 001 UA EP 599 H0032 001 HP EP 599 H0032 001 U5 HO 599 H2021 001 EP 599 H2021 001 HQ EP 599 H2033 001 EP 599 H2019 001 HA 599 H0046 001 U8 SC ACT 62 Consumers – TSS SERVICES IN SCHOOL ONLY 599 H2021 001 EP # of Units Requested FBA Mobile Therapy Mand Mtg - MT BSC BSC Autism Specialty TSS TSS Aide MST FFT FFSBS TSS ACT62 Northampton County Provider Name: Member Name: Services Being Requested MIS # Reviewed By: Follow-Up By: Treatment Authorization Request Delaware County / MAGELLAN USE ONLY Start Date (MM/DD/YYYY) End Date (MM/DD/YYYY) T. Foster/Host Home 231 001 200 252 202 S5145 99221-1 unit 99231-addtl H0019 H0019 H0019 RTF – JCAHO 151 RTF – Non JCAHO RTF – Non JCAHO (CISC) RTF–Group Home BHRS After school 599 H2015 Therapeutic Summer Camp 561 H2012 Mod3 - - EXT: DIAGNOSIS CODE Approved? Axis I: EP Axis II: - Axis III: Axis IV: Axis V: DIAGNOSIS 001 001 001 001 EP HE HQ EP 001 SC EP 001 EP By checking this box the provider attests that current POMS information has been submitted online. POMS data MUST be updated at least annually. MAGELLAN USE ONLY Date of Eval: Date of ITM: / / / / Date Info Due: Date Info Received: / / / / Date Info Requested: / / Date Info Accepted: / / Magellan Behavioral Health of Pennsylvania, Inc. (Magellan) is a subsidiary of Magellan Health Services, Inc. ©2004-2011 Magellan Health Services. This document is the proprietary information of Magellan. Select One: (“X”) Initial Reauthorization Rev 01/26/2011 Date Revised BHRS TAR Instructions Effective February 1, 2011 Magellan Behavioral Health of Pennsylvania, Inc. (Magellan) has reviewed the requirements for ACT 62 referrals and feedback from providers involved with the new regulations. Magellan has found that we are now in a position to move to a streamlined approach for the authorization process for these individuals. On February 1, 2011, Magellan put into effect the following procedures for managing Pennsylvania HealthChoices members with the Act 62 benefit. ACT 62 Members – Services Authorized by Commercial Plan • Commercial plan is responsible for primary coverage and authorization. • Providers DO NOT submit any material to Magellan (Pennsylvania HealthChoices) when the primary payor is a commercial plan, except in two situations below: Exception #1: TSS Hours in the Setting of School – Place of Service 03 • Commercial plans are not covering services provided in the school setting at this time. o Please use the identified portion for ACT 62 TSS Services for requesting TSS in a school setting (Example 1 below). o Magellan (Pennsylvania HealthChoices) will review the packet and make a medical necessity determination for the school hours. o The Magellan (Pennsylvania HealthChoices) timeframe will be used for authorization periods up to one year. EXAMPLE 1 - TSS Line for requesting School Hours ONLY Services Being Requested TSS ACT62 MAGELLAN USE ONLY Outcome CPT Prob Mod Mod Mod Appr(MM/DD/YYYY) (MM/DD/YYYY) Code Type 1 2 3 oved? ACT 62 Consumers – TSS SERVICES IN SCHOOL ONLY 599 H2021 001 EP # of Units Requested Start Date End Date Exception #2: ACT 62 Members – Services Partially Authorized by Commercial Plan • In the situation where the provider receives a partial medical necessity denial by the health plan, the provider is expected to grieve the medical necessity denial. Upon exhausting the grievance process, the provider may submit the authorization request to Magellan (Pennsylvania HealthChoices) for medical necessity consideration. Preauthorization and retrospective procedures apply. Co-Payments and Deductibles o Magellan (Pennsylvania HealthChoices) will pay the member’s portion of the co-payments and deductibles without authorization. o Providers should submit a claim using the contract procedure code and modifiers for Magellan (Pennsylvania HealthChoices) and include a copy of the commercial plan EOP. Denial of Payment by Commercial Plan When an Authorization Had Been Given • Provider is expected to appeal the denied claim for the service that had been originally authorized. • If the provider receives written communication stating that the member does not have Act 62 coverage, Magellan (Pennsylvania HealthChoices) will review denials by the commercial plan as described by the Medicaid Retrospective Review of Treatment Services policy. Magellan Behavioral Health of Pennsylvania, Inc. (Magellan) is a subsidiary of Magellan Health Services, Inc. ©2004-2011 Magellan Health Services. This document is the proprietary information of Magellan. Rev 01/26/2011
© Copyright 2026