Asian Cardiovascular and Thoracic Annals
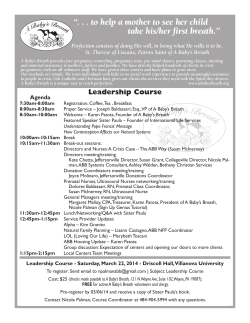
Asian Cardiovascular and Thoracic Annals http://aan.sagepub.com/ Can Chest Trauma Patients Provide Breath Sample with Lion SD-400 Alcometer? Sridhar Rathinam, David Luke, Prakash Nanjaiah, Maninder S Kalkat and Richard S Steyn Asian Cardiovascular and Thoracic Annals 2009 17: 282 DOI: 10.1177/0218492309104774 The online version of this article can be found at: http://aan.sagepub.com/content/17/3/282 Published by: http://www.sagepublications.com On behalf of: The Asian Society for Cardiovascular Surgery Additional services and information for Asian Cardiovascular and Thoracic Annals can be found at: Email Alerts: http://aan.sagepub.com/cgi/alerts Subscriptions: http://aan.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav >> Version of Record - Jun 1, 2009 What is This? Downloaded from aan.sagepub.com by guest on October 6, 2014 ORIGINAL ARTICLE Can Chest Trauma Patients Provide Breath Sample With Lion SD-400 Alcometer? Sridhar Rathinam, FRCSEd(CTh), David Luke, MRCS, Prakash Nanjaiah, MRCS, Maninder S Kalkat, FRCSEd(CTh), Richard S Steyn, FRCSEd(CTh) Regional Department of Thoracic Surgery Birmingham Heartlands Hospital Bordesley Green East, Birmingham, UK ABSTRACT Various investigators have addressed the minimum lung function required to activate breathalyzers, and the impact of comorbid respiratory illness. We postulated that subjects with significant chest trauma may have difficulty in providing an adequate breathalyzer sample. A prospective self-controlled study of 20 patients who underwent thoracotomy was conducted between August 2005 and December 2005, using a Lion Alcometer SD-400. The mean age of the patients was 69.3 years (range, 37–83 years). Preoperatively, their mean forced expiratory volume was 1.97 L (range, 1.19–2.46 L), and peak expiratory flow rate was 240 L min1 (range, 126–520 L min1). Postoperatively, mean forced expiratory volume was 1.14 L (range, 0.34–2.2 L) and peak expiratory flow rate was 179 L min1 (range, 36–492 L min1). These decreases were highly significant. All patients activated the breathalyzer device preoperatively, but only 2 (10%) could activate it postoperatively. Extrapolating this to patients with chest injury, most may find it impossible to activate breathalyzers. (Asian Cardiovasc Thorac Ann 2009;17:282–4) KEYWORDS: Alcohol Drinking, Breath Tests, Thoracic Injuries, Thoracic Surgery. INTRODUCTION British police have been using roadside alcohol testing since 1967, and it is now mandatory in drivers stopped with a suspicion of drinking.1 As with many other police forces, they also screen drivers involved in collisions. Drivers are initially tested with a breathalyzer at the roadside.2 If positive, evidential breath testing is performed again at a police station. Various investigators have addressed the impact of comorbid respiratory illnesses and the minimum lung function required to activate various breathalyzers.3–5 It is accepted that chronic obstructive pulmonary disease may cause difficulty in undertaking such tests, and that forced expiratory volume in the 1st second (FEV1) and forced vital capacity (FVC) are the most reliable indicators. Significant chest trauma may also cause difficulty in providing a breath sample. This depends on the significance and severity of the injury. This study was conducted to determine whether a breathalyzer can be activated by a person with significant chest trauma. Patients who had undergone thoracic surgery were used as models of chest trauma due to vehicle collision. PATIENTS AND METHODS A prospective self-controlled study was performed in 20 patients who underwent thoracic surgical procedures in Birmingham Heartlands Hospital between August and December 2005. Ethics committee approval was obtained, and the patients were counseled and consented into the study. Thoracotomy with lung resection was used as a model of rib fractures with pulmonary contusion, and sternotomy was used as a model of sternal fracture. We excluded patients who could not activate the breathalyzer preoperatively and those with a tracheostomy or tracheal problems who could not use the device. The mean age was 69.3 years Richard S Steyn, FRCSEd(CTh) Tel: þ44 121 424 2562 Fax: þ44 121 424 0562 Email: [email protected] Regional Department of Thoracic Surgery, Birmingham Hertlands Hospital, Bordesley Green East, Birmingham B9 5SS, United Kingdom. doi: 10.1177/0218492309104774 ß SAGE Publications 2009 Los Angeles, London, New Delhi and Singapore ASIAN CARDIOVASCULAR & THORACIC ANNALS 2009, VOL. 17, NO. 3 282 Downloaded from aan.sagepub.com by guest on October 6, 2014 Rathinam Chest Trauma and Breathalyzers Table 1. Surgical procedures in 20 patients Procedure Mean Age (years) Male Total Lobectomy Decortication Pneumonectomy Wedge excision Exploratory thoracotomy Median sternotomy Repair of diaphragm 71.8 60 59 70 75 79 60 5 5 0 3 2 1 1 7 5 1 3 2 1 1 Figure 2. Changes in forced expiratory volume in 1st sec (FEV1) before and after surgery. 3.5 adequate analgesia and the evaluation was performed after they had recovered from physiotherapy exercises. We felt this was equivalent to a chest trauma patient receiving morphine for analgesia. The spirometry was repeated on this occasion, and recorded. FEV1 in litters 3 2.5 2 1.5 1 Changes in FEV1 and PEFR were analyzed using paired Student t tests. A value of p < 0.05 was considered significant. 0.5 0 Pre Op FEV1 Post Op FEV1 Figure 1. The Lion Alcometer SD-400. RESULTS Preoperatively, the mean FEV1 was 1.97 L (range, 1.19–2.46 L), and mean PEFR was 240 L min1 (range, 126–520 L min1). Thoracic epidural pain relief was used in 12 patients, and 8 had intrathecal morphine followed by morphine infusion. After surgery, there was a decrease in both FEV1 and PEFR, irrespective of the surgical procedure (Figure 2). Postoperatively, the mean FEV1 was 1.14 L (range, 0.34–2.2 L) and PEFR was 179 L min1 (range, 36–492 L min1). The decreases in FEV1 and PEFR in the postoperative period were both highly significant ( p ¼ 0.000). All patients were able to activate the device preoperatively, but only 2 (10%) could activate it postoperatively; these 2 patients were males who had undergone decortication. (range, 37–83 years), and 17 (85%) patients were male. All underwent spirometry to assess lung function, as part of their preoperative assessment. Operative procedures are listed in Table 1. A median sternotomy was performed in 1 patient, and the others underwent a posterolateral thoracotomy. All patients had general anesthesia and double-lumen endotracheal intubation with single-lung anesthesia. They were extubated on the operating table, and transferred to the thoracic highdependency unit. The Lion Alcometer SD-400 is a microprocessorcontrolled multi-filtering infrared spectrometer that incorporates a flow meter to measure FEV1 and peak expiratory flow rate (PRFR), which trigger the device. The spectrometer analyses the breath sample for alcohol (Figure 1). We investigated patients’ ability to activate the device without alcohol (dry activation). Preoperatively, patients were briefed about the device and its function, and it was used according to the manufacturer’s instructions.6 The Alcometer was calibrated, and a disposable mouth piece was attached. The patient was asked to take a deep breath in, and exhale into the device through the mouth. When the device is activated, there is a change of indicator color from red to green. The best of 3 attempts was taken into consideration. Inability to activate the device after 3 attempts was accepted as failure. This procedure was repeated on the 2nd postoperative day. We ensured that patients had 2009, VOL. 17, NO. 3 DISCUSSION Various studies have investigated the impact of lung function on ability to activate a breathalyzer. FEV1 is a significant indicator of ability to activate a breathalyzer, but the threshold value may vary with the type of device. Briggs and colleagues3 suggested that subjects with FEV1 < 1.5 L or FEV1 < 50% of predicted were unlikely to activate the Alcometer. Another study suggested higher minimum values, showing that subjects with FEV1 < 2 L and FVC < 2.6 L were unable to use any device.4 More recently, Honeybourne and colleagues5 reported continuing difficulties in the ability of some subjects to use the Lion Intoxilyser 6000 breath alcohol device, which is the model used by police in the 283 ASIAN CARDIOVASCULAR & THORACIC ANNALS Downloaded from aan.sagepub.com by guest on October 6, 2014 Rathinam Chest Trauma and Breathalyzers UK, in a study attempting to validate this device in patients with chronic lung disease. The device usually requires a minimum sample volume of 1.2 L, with flow rate maintained 412 L min1. A Canadian study on the device used by Ontario police indicated that all patients with FVC41.43 L could perform the test, whereas 75% of those with FVC < 1 L caused by airway obstruction were unable to provide an adequate sample.7 These findings highlight the need for adequate lung function to maintain a steady airflow through the device to activate it. injuries in road accidents may be associated with brain concussion and other injuries, shock, and fear. A limitation of this study is that the mean age of the patients is probably higher than that of motorists driving under the influence of alcohol. Further studies may be needed in a younger cohort. Extrapolating these findings in patients who had chest surgery, we can assume that presently available devices are difficult to activate by drivers who suffer chest trauma. This group require alternative methods to estimate alcohol levels. Anyone who fails to provide an adequate breath sample for alcohol testing may be charged with refusing to supply a sample, unless he convinces the police officer that he is genuinely unable to do so.4 Rib fractures, pain, pulmonary contusions, and impaired diaphragmatic movement all contribute to diminished lung function after chest injuries. Ventilatory capacity (FEV1) and vital capacity are reduced, and the residual volume is increased after chest injury.8 In a study using mathematical models, it was shown that failure to achieve full inspiration reduces the breath alcohol content at full exhalation, and reduced inhaled volume and can lead to inability to provide an adequate breath volume.9 It also demonstrated that alcohol exchange within the airways during the single-exhalation breath test is dependent on lung size. This may lead to bias against people with smaller lung size.9 ACKNOWLEDGMENT The Lion Alcometer SD-400 was provided by Lion Laboratories. REFERENCES We postulated that patients with significant chest injuries would not be able activate the breath analysis device due to pain and compromised respiratory function. In testing this hypothesis on patients undergoing thoracic surgical procedures, we chose the 2nd postoperative day because they were on patient-controlled morphine analgesia rather than epidural or intrathecal morphine, which are not comparable to the morphine analgesia provided by pre-hospital care practitioners or accident and emergency departments. Their decrease in lung function highlights the importance of pain and loss of chest wall mechanics in a postoperative or post-chest injury patient, in spite of adequate analgesia. Thoracic operations are a form of controlled trauma, but chest ASIAN CARDIOVASCULAR & THORACIC ANNALS 1. Moudgil H. Evidential alcohol breath testing. BMJ Jan 2003. Available at: http://www.bmj.com/cgi/eletters/325/7377/1403#. 2. Berger A. Clinical review: how does it work? Alcohol breath testing. BMJ 2002;325:1403. 3. Briggs JE, Patel H, Butterfield K, Honeybourne D. The effects of chronic obstructive airways disease on the ability to drive and to use a roadside Alcometer. Respir Med 1990;84:43–6. 4. Gomm PJ, Osselton MD, Broster CG, Johnson NM, Upton K. Study into the ability of patients with impaired lung function to use breath alcohol testing devices. Med Sci Law 1991;31: 221–5. 5. Honeybourne D, Moore AJ, Butterfield AK, Azzan L. A study to investigate the ability of subjects with chronic lung disease to provide evidential breath samples using the Lion Intoxilyser 6000 UK breath alcohol device. Respir Med 2000;94:684–8. 6. Lion Alcometer SD-400. Available at: http://www. lionlaboratories.com/files/sd-400.pdf. Accessed January 29, 2008. 7. Prabhu MB, Hurst TS, Cockcroft DW, Baule C, Semenoff J. Airflow obstruction and roadside breath alcohol testing. Chest 1991;100:585–6. 8. Little RA, Yates DW, Atkins RE, Bithell P, Stansfield M. The effects of minor and moderately severe accidental chest injuries on pulmonary function in man. Arch Emerg Med 1984; 1:29–38. 9. Hlastala MP, Anderson JC. The impact of breathing pattern and lung size on the alcohol breath test. Ann Biomed Eng 2007; 35:264–72. 284 Downloaded from aan.sagepub.com by guest on October 6, 2014 2009, VOL. 17, NO. 3
© Copyright 2026