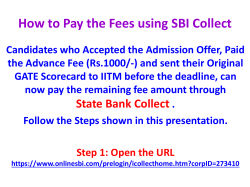
P r o
P r o v id e r M a n u a l 2 0 1 3 -2 0 1 4 Rev. 12.2013 Page 1 Of 81 INDEX Introduction …………………………………………………………………….……….… 5 ……………………………………………...……… 6 APS Healthcare Puerto Rico, Inc. ……………………………………………….… 6 Member Rights and Responsibilities MEMBER RIGHTS ……………………………………………………………….… 6 MEMBER RESPONSIBILITIES Provider Operations …………………………………………………... 8 ……………………………………………………………………… 9 PROVIDER STANDARDS ………………………………………………………… 9 FACILITY STANDARDS ……………………………………………………….… 11 SERVICE STANDARDS ……………………………………………………….… 12 ON-CALL COVERAGE ………………………………………………………...… 14 CREDENTIALING/RECREDENTIALING PROVIDER APPEAL RIGHTS PROVIDER EDUCATION ……………………………………… 15 ………………………………………………..… 19 ……………………………………………………..… 20 ON SITE EVALUATION PROCESS TREATMENT RECORD REVIEW ………………………………………….… 21 ……………………………………………… 22 TREATMENT DOCUMENTATION GUIDELINES Utilization Management …………………………….. 22 ………………………………………………………………… 24 CLINICAL PROCEDURES …………………………………………………….… 26 CLINICAL PRACTICE GUIDELINES ………………………………………...… 31 INTRODUCCTION TO APS-PR HEALTHCARE MEDICAL NECESSITY AND LEVEL OF CARE DETERMINATION CRITERIA DEFINITIONS FOR LEVELS OF CARE 23-HOURS OBSERVATION Rev. 12.2013 ……..... 31 ………………………………………... 32 ……………………………………………………... 34 Page 2 Of 81 INPATIENT (ACUTE CARE) ………………………………………………….… 34 INPATIENT DETOXIFICATION ………………………………………………… 35 INPATIENT REHABILITATION ……………………………………………….… 36 PARTIAL HOSPITALIZATION- PSYCHIATRIC CARE: (ADULT, CHILD/ADOLESCENT) ……………………………………………..… 37 PARTIAL HOSPITALIZATION- SUBSTANCE DEPENDENCE: (ADULT/ADOLESCENT) ………………………………………………………… 38 OUTPATIENT DETOXIFICATION (AMBULATORY DETOXIFICATION) ………………………………………...… 39 INTENSIVE OUTPATIENT THERAPY PSYCHIATRIC CARE: (ADULT, CHILD/ADOLESCENT) ……………………………………………..… 40 INTENSIVE OUTPATIENT THERAPY SUBSTANCE DEPENDENCE: (ADULT/ADOLESCENT) ………………………………………………………… 41 OUTPATIENT CARE …………………………………………………………..… 42 RESIDENTIAL TREATMENT (RTC, DOMICILIARY CARE) PSYCHIATRIC CARE: (CHILD/ADOLESCENT) ……………………………... 43 RESIDENTIAL TREATMENT (RTC, DOMICILIARY CARE) SUBSTANCE DEPENDENCE: (ADULT/ADOLESCENT) …………………… 44 METHADONE MAINTENANCE ………………………………………………… 46 ELECTROCONVULSIVE THERAPY (ECT) PSYCHOLOGICAL TESTING …………………………………… 47 ………………………………………………...… 48 ADVERSE DETERMINATION AND APPEALS PROCESS REPORTING ADVERSE OCCURRANCES ANCILLARY SERVICES ……………….… 49 …………………………………… 49 ……………………………………………………….… 50 MIXED PSYCHIATRIC/MEDICAL PROTOCOL ……………………………… 50 Customer Service ……………………………………………………………………..… 51 TERMINATED MEMBERS ……………………………………………………… 51 Rev. 12.2013 Page 3 Of 81 GRIEVANCE SYSTEM …………………...……………………………………… 52 RETROSPECTIVE-REVIEW Claims Department ………………………………………………….… 56 ……………………………………………………………………… 57 CLAIMS QUALITY MEASUREMENT PROGRAM REIMBURSEMENT PROCEDURES …………………………………………… 58 MEMBER HOLD HARMLESS PROVISION Quality Improvement Program PURPOSE AND GOALS ………………………….… 57 …………………………………… 62 ……………………………………………………...… 63 ……………………………………………………….… 63 STRUCTURE OF THE QUALITY IMPROVEMENT PROGRAM PROGRAM SCOPE AND CONTENT ………………………………………..… 72 RESOURCES DEDICATED TO QUALITY IMPROVEMENT CONFIDENTIALITY ……………….. 79 ………………………………………………………………. 81 EVALUATION AND UPDATE Rev. 12.2013 ………….… 63 …………………………………………………… 81 Page 4 Of 81 INTRODUCTION Welcome to APS Healthcare Puerto Rico, Inc. As a Participating Provider, you join a select network of facilities and treatment programs working with an innovative managed behavioral health organization. APS-PR has developed a provider network to help increase the effectiveness and promote the rational use of mental health and chemical dependency resources. In close collaboration with our participating provider network, such processes as case management, quality assurance and utilization review, help ensure that our services will safeguard quality while managing costs. This Provider Manual was developed to answer your questions and to serve as a reference source for your office staff. While many questions will be addressed by this guide, please feel free to contact our Provider Relations Department for additional assistance at 1-800-503-7929 X 2742. From time to time it may be necessary to update this Manual. You will receive replacement sections with explanations of changes, additions or deletions. Periodically you will also receive APS Healthcare Puerto Rico, Inc. informational communications and Provider Newsletters. APS-PR provides a partnership with you which offers referrals and prompt reimbursement for your services. The information contained herein is applicable to all network providers; however, authorization and claims-submission procedures vary by customer. Please refer to the member’s identification card to determine authorization and claims payment procedures. QUESTIONS OR COMMENTS Specific policy or procedural questions which are not addressed in this manual may be directed to the Provider Relations Department of APS Healthcare Puerto Rico, Inc. Comments or questions regarding the Provider Manual itself should be directed to: APS Healthcare Puerto Rico, Inc. Provider Relations Department P.O. Box 71474 San Juan, P.R. 00936-8574 Phone: 1 (800) 503-7929 Rev. 12.2013 Page 5 Of 81 APS HEALTHCARE PUERTO RICO, INC. As a managed behavioral healthcare company, APS-PR has the expertise to provide: administrative, consultative and case management services to our providers and members. APS-PR offers twenty-four (24) hour on call service for Members and Providers by trained and experienced professionals. Assessment and referral services are provided to the most appropriate and available level of care. A multi-disciplinary team approach is used. Psychiatric nurses (RN), master’s level social workers (MSW), or psychologists conduct patient interviews telephonically and review treatments for providers delivering clinical services. Psychiatrists are on staff and available for consultation whenever necessary. Treatment planning with our clinical care managers is coordinated with our providers from initial assessment and throughout treatment. We believe that the relationship between treatment standards and clinical judgment is one of assistance and collaboration rather than one of control. The intent of treatment standards is to inform clinical judgment, not to overrule the clinician’s professional experience. However, in an effort to have consistency in the clinical decision making process, APSPR has formulated a set of clinical guidelines upon which our clinicians base their decisions. The clinical criteria are based upon reasonable scientific evidence in the field of behavioral healthcare and are contained under section III under APS-PR Utilization Management criteria. To obtain an additional set of the APS Healthcare Puerto Rico, Inc. clinical criteria, please call (800) 503-7929 ext. 3027. [ I ] Member Rights and Responsibilities APS-PR providers should be familiar with the APS-PR Members Rights and Responsibilities Statement. A copy of these should either be displayed in your office or given to the member prior to your rendering any services. A. MEMBER RIGHTS 1. Members have the right to be provided care and treatment with dignity and respect; as individuals who have personal needs, feelings, preferences and requirements. 2. Members have the right to impartial services and access to treatment, regardless of race, religion, gender, ethnicity, age, or disability. 3. Members have the right to privacy in their treatment, in their care and in fulfillment of their personal needs. 4. Members have the right to be treated by staff/providers who communicate in a language/format they understand. Rev. 12.2013 Page 6 Of 81 5. Members have the right to be fully informed of all services available, any charges for or limitations to those services and available alternative treatment. 6. Members have the right to be provided an individualized treatment plan and to participate in decision making regarding their treatment planning. 7. Members have the right to be fully informed, in a language/format they understand, of their rights as clients and of all rules and regulations governing their conduct as clients in this program. 8. Members have the right to be fully informed of all diagnostic and/or treatment procedures, medication treatments, including the benefits and risks, any research projects involving their treatment through APS-PR and to receive information necessary to give informed consent prior to the start of any procedures, treatment or research project. 9. Members have the right to a candid discussion of appropriate or medically necessary treatment options for their conditions. Members have the right to know treatment options regardless of the cost and whether they are covered services. 10. Members have the right to refuse treatment without compromising their access to the organization’s services to the extent permitted by law, and to be informed of the consequences of this refusal. However, the provider reserves the right to discontinue treatment should the extent of their refusal make reasonable and responsible treatment possible. 11. Members have the right to continuity of care. As long as they remain eligible for services through APS-PR, members will not be discharged or transferred except for therapeutic reasons, for their personal welfare, or for the welfare of others. Should their transfer or discharge become necessary, members will be given the reasons and plan, as well as reasonable advance notice, unless an emergency situation exists. 12. Members have the right to voice opinions, recommendations, complaints, or appeals in relation to APS-PR policies, members’ rights and responsibilities or the care provided without fear of restraint, interference, coercion, discrimination, or reprisal. 13. Members have the right to be free from physical, chemical and mental abuse. 14. Members have the right to confidentiality management of their medical records as established by HIPAA Law. 15. Members have the right to refuse to perform any services for the program, or for other clients, unless they are a part of their therapeutic plan of treatment, which they have approved. Rev. 12.2013 Page 7 Of 81 16. Members have the right to be informed in advance of any non-staff visitors to a facility/office and the right to privacy if they do not wish to see visitors, or participate in activities while visitors are present. 17. Members have the right to receive information necessary to give informed consent prior to being involved in activities, which include the use of tape recorders, video tape equipment, one-way observation mirrors, photography, or any other techniques. 18. Members have the right to receive information regarding the authorization and certification /non-certification processes, benefit plan services included and excluded; co-payments; the provider network available for their care at the time they seek to access care; clinical guidelines, members rights and responsibilities; and how to file a claim. 19. Members have the right to file an appeal for review by an individual uninvolved in the original determination. B. MEMBER RESPONSIBILITIES 1. Members have the responsibility to provide, to the extent possible, information that APS-PR and its providers need in order to care for them. 2. Members have a responsibility to follow the plans and instructions for care that they have agreed upon with their provider(s). 3. Members have the responsibility to follow administrative guidelines and codes of conduct in the provider facility. 4. Members have the responsibility to attend appointments free from the influence of alcohol and illegal substances. 5. Members have a responsibility to participate, to the degree possible, in understanding their behavioral health problems and developing mutually agreedupon treatment goals. 6. Members have a responsibility to follow APS-PR policies and processes as described in their handbook/packet regarding authorization and certification/noncertification; benefit plan eligibility; benefit plan services included and excluded; copayments; the provider network available to them and how to file a claim. [ II ] PROVIDER OPERATIONS Rev. 12.2013 Page 8 Of 81 The Provider Operations Area, operating through its Provider Relations Department, acts as a liaison between all participating providers (PCPs, Specialists, Hospitals, and Ancillary Services), and the departments within the organization. The Provider Operations Area is made up of a team of approximately six managed care professionals supervised by the Provider Relations Manager. This person is directly responsible for supervising the daily operations for the department. These processes include: Recruitment, Servicing, Credentialing and Re-credentialing among others. Provider Operations are dedicated to assist APS-PR providers with the following: * * * * * * * * * Orientation of new APS-PR providers and their staff Education of APS-PR providers regarding policies and procedures Conducting Site Visits Producing and distributing provider newsletters Resolving problems for providers Contracting providers Network development Recruitment of specialized providers Working with providers in the development and implementation of financial reviews and effective referral patterns. A. PROVIDER STANDARDS 1. Access Standards When APS-PR contacts a provider with a referral or a member in ongoing treatment calls a provider to schedule an appointment, it is expected that the provider will be able to offer an appointment to the member within APS-PR standards of accessibility. The following scheduling standards supersede all lesser scheduling standards in the provider agreement: 2. Emergent Care APS-PR has divided emergent care into two types: life-threatening and non-lifethreatening. When a member presents with a life-threatening emergency they should be seen immediately. Members who present with a non-life-threatening emergency should be offered an appointment within six (6) hours of contact. Life-threatening Emergent Care is required when a member has made a suicide attempt or is in immediate danger of making a suicide or homicide attempt. It may be appropriate for the member to be treated in the Emergency Room of a hospital on those occasions. Non-life threatening Emergent Care applies to those situations when the patient is markedly distressed, has limited resources, and when there is a strong potential for rapid instability. Rev. 12.2013 Page 9 Of 81 3. Urgent Care Urgent care is required when a member is markedly distressed but has the resources to avoid imminent instability. It also pertains to members being discharged from the inpatient, partial day hospital, or intensive outpatient levels of care. When a member requires urgent care an appointment should be offered within twenty four (24) hours of contact. 4. Routine Care An appointment is to be offered within five (5) business days of the initial referral for routine care. When accepting referrals, providers should be able to schedule ongoing appointments in a timely manner. Every attempt should be made to accommodate members within these access standards. It is important that the provider document the first appointment offered, specially when the member fits either the emergent or urgent criteria or refuses appointments that fall within the APS-PR access standards. If a provider is unable to meet these standards, the provider is to notify APS-PR so that alternative arrangements can be made. Any provider who is consistently unable to schedule appointments within the time frames described above will be presented to APS-PR’s Credentialing Committee for review and action. When a member contacts his or her provider by telephone for any reason, it is expected that the provider or an office administrator will return the member’s call promptly. Emergent phone calls are to be returned within thirty (30) minutes. Urgent calls are to be returned within one (1) hour. Routine calls are to be returned by the next business day. APS-PR network providers are responsible for the ongoing care of any member for whom a referral has been accepted. It is expected that answering machine messages and answering services provide patients with a number to contact the provider in the case of an emergency. A message that states that the patient should go to the Emergency Room of a hospital is not acceptable. If on-call responsibilities are rotated in a group practice or with clinicians who do not participate with APS-PR, it is the responsibility of the primary clinician to see that APS-PR’s referral and authorization procedures are followed. 5. New Patients/Clients A) Please remember that you must accept new referrals from APS-PR on the same basis as you are accepting non-APS-PR members; without regard to race, religion, gender, color, sexual orientation, place of residence, national origin, age or physical or mental health status. B) The only times you may refuse a APS-PR referral are: Rev. 12.2013 Page 10 Of 81 • • The patient requires treatment that is outside the scope of your clinical licensure or expertise. Your panel is closed to all new patients. Note: If you decide to stop accepting any new patients, you must give APS-PR 30 days advance notice in writing. 6. Preferential Turns As an APS provider you are expected to establish a system of preferential turns, regardless of your specialty- that allow residents of the island municipalities of Vieques and Culebra. A system of preferential turns refers to a policy that you as a provider must establish in order to give priority in treating enrollees from the islands of Vieques and Culebra, so they may be seen by a provider within a reasonable time after arriving in the Provider’s office. The priority in turns given to these enrollees is necessary due to their remote place of residence and the increased length of time required in getting back to those island municipalities. All providers must be aware that this is a requirement established by Articles 1-4 of the Law No. 86 of August 16, 1997 and Articles 1-5 of Law No. 200 of August 5, 2004. 7. Report Requirements Provider must comply with reporting requirements as established by ASES and APSPR, and particularly with the requirements to submit Encounter Data, Claims Data, UM Data, for all services provided, and to report all instances of suspected Fraud and Abuse among others. All reports submitted by Provider to APS-PR have to be labeled with the Provider’s NPI. Reports Other reports may be required by APS-PR as needed according with the terms of the provider contract or the contract between APS-PR and the ASES. B. FACILITY STANDARDS Our facility standards refer to the inpatient and outpatient sites where members receive services. These standards address the appearance, safety and licensure, if applicable, of the office or facility. The following standards are required of APS-PR facility providers: • • • • • • • Visible signs clearly identify the facility; The exterior of the building is clean and well maintained; Parking is adequate and nearby; The area surrounding the facility is safe when exiting at night; The waiting room has adequate seating for patients; The facility is clean and in good repair (this includes the waiting room, admission area, patient rooms and halls, offices, kitchen, dining area, rest rooms and common areas); The facility meets the requirements of the Americans with Disabilities Act (ADA); Rev. 12.2013 Page 11 Of 81 • • • • • • • • • Emergency phone numbers (police, fire, ambulance) are posted in common staff areas; Fire extinguishers are readily available; Smoking is restricted to an outdoor location or a separately ventilated room; Medications are protected from public access; All hospital units and inpatient and outpatient programs are licensed by the state; If eligible, the hospital or facility is accredited by the Joint Commission for the Accreditation of Health Care Organizations (JCAHO); If sanctioned by JCAHO, the provider has submitted an acceptable corrective action plan; If eligible, the provider is Medicare approved; If eligible, the provider is Medicaid approved. C. SERVICE STANDARDS 1. The following service standards apply to all providers: • • • • • • • • • • • • • • • • There is at least one staff member available for patient intake during business hours; Routine phone calls from patients are returned by the next business day; Urgent calls from patients are returned within one (1) hour; Emergent calls from patients are returned within thirty (30) minutes; The provider informs all patients on how the provider is to be contacted during and after business hours in an urgent or emergent situation; Unless the situation is life threatening, patients are not directed to go to an emergency room; Routine initial outpatient appointments are scheduled within five (5) business days of receiving a referral; Urgent outpatient appointments are scheduled within twenty four (24) hours of the referral or contact from a member in ongoing treatment; Emergency outpatient appointments are scheduled immediately if the patient has a life-threatening emergency or within six (6) hours of the referral or contact from a member in non-life-threatening emergencies; Providers are trained in de-escalation techniques; Patient education materials are distributed routinely; Providers are encouraged to receive training in brief therapy; Providers are trained and/or experienced in working effectively with Managed Behavioral Health Care Organizations; HMO Members can be charged an amount when an appointment is canceled with less than twenty-four (24) hours notice or when the member fails to provide any notice as establish by the Office of the Health Advocate (Oficina del Procurador de la Salud); this is not applicable to Medicaid Eligible Persons enrolled in MISalud; Release of information to the member’s Primary Care Physician (PCP) as part of the intake process, if applicable; Member Rights and Responsibilities statement is displayed or distributed to the member prior to rendering service. Rev. 12.2013 Page 12 Of 81 2. The following service standards apply only to those providers contracted with APS-PR to provide inpatient, residential, partial hospitalization, intensive outpatient services or twenty-three (23) hours evaluation and observation services: • • • • • • • • • • • • • • • Visitors are required to sign a confidentiality statement prior to entering patient areas; Provider adheres to written admission criteria; If services are not provided in a general hospital, arrangements are in place for transporting patients in the case of a medical emergency; Examination rooms are available to perform the case history and physical examination of patients; Crash carts or emergency boxes are available for the medical emergencies; Clinical staff to patient ratio are adequate; Staff is trained annually in de-escalation techniques; Treatment is individually tailored to meet the needs of each patient; Adult and adolescent patients are separated by units or by patient rooms; Adolescent and child patients are separated by units or by patient rooms; The Initial Treatment Plan is completed within twelve (12) hours of admission; The case history and physical examination of the patients are completed within twenty-four (24) hours of admission; The Psychosocial Assessment is completed within twenty-four (24) hours of admission; The Initial Psychiatric Assessment including Mental Status Exam and DSM-IV diagnosis is completed within twelve (12) hours of admission; Discharge planning begins upon admission and includes scheduling a postdischarge outpatient appointment within forty-eight (48) hours of discharge. 3. The following service standards apply to hospitals and programs with acute mental health units only: • • • • • • • • • • Patients are seen by an MD at least once within any 24 hour period. Admissions are accepted twenty-four (24) hours per day, seven (7) days per week; Acute units are locked; All hallways can be monitored from the nursing station(s) directly or with the use of video equipment; Patients do not have access to potentially harmful objects; Shower heads are recessed or do not bear weight (suicide-proof); Patient rooms are free from any weight-bearing objects; Patient rooms are free of electrical cords that are twelve (12) inches or longer in length; Medically complex patients who are at-risk for suicide and are in rooms that require electrical cords are monitored at least every fifteen (15) minutes; Light fixtures are recessed or are protected by a non-breakable device; Rev. 12.2013 Page 13 Of 81 • • • • • Windows and mirrors are shatterproof or protected by a non-breakable device; All objects within the seclusion room are secured; One piece toilet seats are used in the seclusion area rest room; Patients in seclusion and in the adjacent bathroom can be viewed by staff at all times; Staff is trained annually in the use of de-escalation techniques to avoid the use of seclusion unless absolutely necessary. 4. The following service standards apply to only those hospitals and programs who provide substance abuse services: • • • • • • Patients are seen at least once within any 24 hour period. If provided, admissions for medical detoxification are accepted twenty-four (24) hours per day, seven (7) days per week; Beds dedicated to patients admitted for detoxification are nearest to the nursing station; Staff includes providers with substance abuse certification; Urine/drug screens are conducted routinely; An aftercare or APS-PR prevention program is offered to all patients for a period of at least six (6) months. D. ON-CALL COVERAGE 1. Covering Providers If a provider is temporarily unavailable to members who are in active treatment, the provider is responsible for arranging adequate emergency coverage during the provider’s absence. APS-PR must be notified of all coverage arrangements. Covering providers must adhere to all of APS-PR’s administrative requirements, including, but not limited to: authorization procedures, accessibility standards and co-payment collection. The covering provider must be of equivalent licensure level and must accept APS-PR’s fee schedule allowance. When arranging emergency coverage, network providers are not required to work with a participating APS-PR provider but it is suggested. If the provider who is covering is not participating with APS-PR, the APS-PR provider is responsible for obtaining authorization for coverage from APS-PR. All claims generated by the covering provider should include the authorization number and should indicate the provider for whom services are being covered. Payment for claims submitted without this documentation will be denied. 2. Suspending Referrals When a provider is temporarily unable to schedule initial appointments within five (5) business days or if the provider is unable to accept new referrals due to a leave of absence, vacation or any other reason, the provider is to notify APS-PR in writing. A Rev. 12.2013 Page 14 Of 81 letter stating the reason for the provider’s inability to accept referrals and the time frame during which referrals are to be suspended should be submitted to the attention of the Provider Relations Department. E. CREDENTIALING/RECREDENTIALING 1. Initial Credentialing All prospective providers undergo an evaluation of their professional credentials and experience. The purpose of the credentialing process is to ensure that all APS-PR providers meet the criteria established by the APS-PR Credentialing Committee. The credentialing process also ensures compliance with the guidelines established by the National Committee for Quality Assurance (NCQA) and Center for Medicare and Medicaid Services (CMS). The credentialing process is initiated with the submission of a signed agreement and a complete application to APS-PR. The application is carefully reviewed for completeness and adherence to the APS-PR credentialing criteria. Accepted applications with supporting documents are submitted for primary source verification and then forwarded to the APS-PR Credentialing Committee for peer review and disposition. All applicants are informed in writing of acceptance into or rejection from the APS-PR network. The Credentialing Committee is chaired by the Medical Director and also includes network providers in order to provide peer review. If you are interested in joining the committee, please call us. 2. Primary Source Verification Choosing the practitioners who will work well in the delivery system is the responsibility of APS-PR. Well-defined policies and procedures describe the requirements and the process used to evaluate practitioners. (a) Application reviewed for completeness. Any application more than one hundred and eighty (180) days beyond the signature date requires a current signature to confirm that all the information remains accurate and correct. (b) License Verification through the appropriate state licensing board is either written or oral. (c) Liability Insurance; Must be active and meet minimum coverage required (1 million/3 million for Hospitals, Programs, Agencies, M.D. and D.O. Ph.D. and MSW level requires 1 million/1 million coverage). Additional verification is required only if there is a positive history in the past five (5) years of claims or sanctions. Rev. 12.2013 Page 15 Of 81 (d) Positive history of claims requires written explanation from the provider to be reviewed by the Area Credentialing Committee. (e) Hospital Privileges: Verified in writing through Privilege Verification Form (Required for MD and DO). (f) Board Certification: Copy of entry into ABMS compendium. (g) If not Board Certified then residency must be verified in writing with verification of residency form. (h) Education verified at highest level, attained orally with the University or in writing. For MD and DO this is not required if Board Certified or if the residency is verified. (i) A copy of a valid DEA or CDS certificate (if applicable). (j) National Provider Data Bank (NPDB) inquiry queried for all providers. If there are any loss of privileges, malpractice history or other sanctions found they will be reviewed on a case by case basis by the Area Credentialing Committee. (k) Medicare/Medicaid Sanctions after 3/3/97 are queried by virtue of NPDB. (l) Provider is reviewed by the APS-PR Credentialing Committee for final approval. (m)Educational Commission for Foreign Medical Graduates (ECFMG) must be included for Foreign Graduates. (n) Curriculum Vitae: The last five years must be documented and APS-PR explained. The credentialing specialist will notify the applicant of missing data elements and secure the required information. If the credentialing specialist is unable to secure the required information within a predetermined time, the credentialing process will cease and the applicant will be notified in writing of the action with cause. Confirmation of primary source verification is expected to be submitted to the Credentialing Committee in sixty (60) days for US educated/trained providers and ninety (90) days for foreign educated/trained providers following receipt of a completed application and supporting documents. A portfolio with copies of the supporting documents of each applicant will be submitted to APS-PR Credentialing Committee. 3. Re-credentialing As a participating provider, you will undergo a triennial (every 3 years) re-examination of your credentials. The process will be initiated six months (6) prior to the anniversary date of the contract or employment. The re-examination of your credentials will be combined with an objective evaluation of your history with APS-PR related to: Rev. 12.2013 Page 16 Of 81 (a) Delivery of Quality Care that is congruent with APS-PR’ philosophy and treatment protocols. (b) Participation in Quality Improvement activities (c) Utilization Management (compliance and track record) (d) Patient Satisfaction (survey results and complaint tracking) (e) Medical Records (meeting objective criteria for completeness and legibility) (f) Results of office site visits. (g) Quality of Care Issues (h) Complaints and Grievances history All of the above described information will be reviewed by the Credentialing Committee who will decide whether participation in the APS-PR network will be continued. You will be notified in writing of the decisions of the committee. If the re-credentialing process is not completed within 3 years, you will be terminated from the network and will need to apply to APS-PR as a new provider. 4. Quality Reviews In addition to the normal re-credentialing cycle, providers may be reviewed between cycles when quality performance monitors indicate the need for such a review. APS-PR monitors the quality of provider services by tracking complaints received from members, clients, organizations or APS-PR staff. Complaints are weighted according to the seriousness of the complaint or by the number of less serious complaints received. In all cases, a Provider Relations staff member will contact provider to gain additional information about the content of the complaint before a weight is assigned. In most instances, APS-PR will work with the provider to either educate them in cases where lack of knowledge on the part of the provider led to the complaints, or to develop an Action Plan with the provider to bring them into compliance. In certain instances when, either because of the number of complaints or the seriousness of the complaint, the provider file will be reviewed by the Credentialing Committee who will make recommendations regarding the network status of the provider as well as regarding actions to be taken by APS-PR. A provider may be suspended or terminated from the network as a result of the review of the Credentialing Committee. Possible actions which can be taken by APS-PR include, but are not limited to a Site Visit of the practitioner, a Treatment Record review of APS-PR members in treatment with practitioner, contact by the APS-PR Medical Director or his/her delegate to further discuss the issues, suspension or termination from the network. 5. Additional Events Causing Early Termination or Suspension: Not withstanding any other provision in the Provider Service Agreement, The Credentialing Committee may terminate a provider’s credentialing status at any time upon notice to the Physician of the occurrence of any of the following events; Rev. 12.2013 Page 17 Of 81 (a) Provider’s conviction of a felony or misdemeanor or involving moral turpitude. (b) Professional incompetence of Provider, or non-performance of professional responsibility. (c) Provider’s failure to comply with quality improvement and utilization review procedure and standards, as established by APS-PR, including, but not limited to, appointment availability, billing practices, utilization, provision of services, cost effective use of inpatient services unless adequately justified as determined by APSPR surveys or outcome studies and failure to meet timeline requirements of the credentialing program. (d) Provider’s physical disability resulting from alcohol or drug abuse, which impairs physician’s ability to practice his or her profession in a competent manner; or loss or suspension of the licenses required to fulfill the Agreement. (e) Provider’s failure to maintain membership on the Medical Staff of his/her primary admitting facility or failure to maintain adequate malpractice or general liability insurance. (f) Provider’s failure to provide satisfactory personal and professional references and credentials, or to provide verifiable information regarding past employment, training, hospital affiliation, or professional licensing for him/herself or any paraprofessional under his/her supervision. (g) Provider being a party to or having been a party to malpractice or other litigation or arbitration that has resulted in material judgments, settlements or awards against Physician. (h) Provider’s solicitation of Member’s during the initial and any succeeding term of the Agreement, or knowingly or directly advising any APS-PR Member to become enrolled with any other Health Maintenance Organization, Physician Organization, or any other similar hospitalization or medical payment plan or insurance program. (i) APS-PR’s inability to maintain agreements with hospitals, physicians, and ancillary service providers who collectively constitute a service delivery system, or the loss of business in the provider’s service area. APS-PR reserves the right to suspend or terminate a provider immediately. In all cases, APS-PR will notify the provider in writing that these actions have or are about to occur and inform them of the reasons for these actions, and offer the provider the right to appeal the decision and review APS-PR documentation. F. PROVIDER APPEAL RIGHTS Rev. 12.2013 Page 18 Of 81 1. Appeals Process To assure providers the right to appeal decisions made by APS-PR, an appeals policy and procedure was implemented for situations in which a credentialing or recredentialing determination or a review of quality of care or service issues result in alteration of provider privileges. The policy also indicates that as part of its responsibility to safe- guard client members, APS-PR will notify the appropriate authorities when a provider is terminated due to a serious quality deficiency. Upon notification of the adverse determination, providers have 30 business days to appeal. The appeal should be sent to the Provider Relations Manager at the address provided below. Upon receipt, the appeal is date stamped and forwarded to the chair of the Provider Appeals Sub Committee, who convenes the sub-committee. The subcommittee reviews the appeal, conducts an investigation of the data and renders a final determination. The investigation includes a review of the substance of the appeal, including all aspects of the clinical care involved when appropriate. The provider may be asked to submit additional information or confirm data. In addition, queries to the National Practitioner Data Bank, State Licensing Authority, Federation of State Medical Boards (FSMB) and if appropriate, facilities where the practitioner has admitting privileges may be made by the Provider Appeals Sub-committee. SEND APPEALS TO: APS HEALTHCARE PUERTO RICO, INC. PROVIDER RELATIONS DEPT. P.O. Box 71474 San Juan, PR 00936-8574 The final determination, made within twenty days of the appeal, may be to uphold, modify or reverse the original determination. In any case, provider notification by the Provider Appeals Sub Committee must be made within five business days of the final determination. If circumstances beyond the committee’s control occur, the Provider Appeals Sub Committee may be given an additional ten days to provide the determination. The provider notification letter contains the final determination and the reasons behind any delay. The Provider Appeals Sub Committee maintains a provider appeals log to track and trend the data and information. This aggregated data and information is submitted to the Network Committee on a quarterly basis for review and incorporation into the network quality improvement report submitted to the APS-PR Quality Improvement Committee. 2. Reporting of Termination Decisions In accordance with Federal Law, the National Practitioner Data Bank and the State Licensing Agency shall be informed of APS-PR’s decision to terminate a provider: Rev. 12.2013 Page 19 Of 81 APS-PR will report to the National Practitioner Data Bank and the appropriate licensing agencies all providers who have been suspended or terminated for quality of care issues. The provider is apprised during the sanctioning process that a report may be sent to the licensing agencies and boards. The provider will then be afforded the opportunity to further clarify issues and provide additional relevant information. In all cases, providers will be given the right to appeal any credentialing or re-credentialing decision to the APS-PR Provider Appeals Subcommittee. G. PROVIDER EDUCATION 1. Provider Orientation Program When new business is implemented in a market, APS-PR sponsors a Provider Orientation Program for all network providers and appropriate administrative staff. The purpose of this program is to orient new providers to APS-PR’s clinical philosophy, operational policies and administrative procedures. The APS-PR Provider Manual is reviewed and providers are briefed on APS-PR’s relationships with local clients. The Provider Orientation Program is APS-PR’s first step in the development of long lasting partnerships with providers. The Provider Orientation Program allows for the solicitation of valuable input and feedback from network providers. 2. Provider Relations Department APS-PR maintains a team to answer provider questions through an 800 number. The phone lines are open from 8:30 a.m.- 5:30 p.m. Monday - Friday. The phone # is 1-800503-7929 extension 2742. Also, providers can be attended in person at APS Central Office by previous appointment. 3. Change of Address or Tax Identification Number Any change of a provider’s name, address, phone number, facsimile number, or tax identification number is to be submitted in writing to the attention of the Provider Relations Department. The request should be signed and dated by the provider and will be accepted by mail or facsimile. To ensure timely claims processing, APS-PR is to be notified as soon as a change occurs. If a requested change requires re-contracting or amending a provider’s current agreement, the agreement or amendment must be executed before the change becomes effective. For example, if a provider resigns from one APS-PR practice group and then joins another, both APS-PR practice group agreements will be amended. If a provider resigns from an APS-PR practice group to establish an independent practice, the provider will no longer be considered active unless accepted into the network as an independent practitioner. 4. Provider Satisfaction Survey Rev. 12.2013 Page 20 Of 81 In our effort to continually improve our business practices and our relationships with providers, APS-PR PR will survey network providers annually to determine their level of satisfaction with APS-PR . Providers are contractually obligated to participate in these surveys as well as any other Quality Improvement Activities. The APS-PR Quality Improvement Committee will distribute the results of these surveys in the aggregate to each of APS-PR’s customers as well as to the network providers, via the Provider Newsletter. Corrective actions may be taken by APS-PR to address problems that have surfaced through the surveys in order to enhance the relationship between providers and APS-PR. 5. Provider Newsletter Every quarter, APS-PR distributes a Provider Network Newsletter to all network providers. The newsletters update providers on APS-PR’s products and operational procedures. It also provides a forum for sharing information about managed behavioral health care conferences and resources. H. ON SITE EVALUATION PROCESS In accordance with the APS-PR Provider standards and the guidelines set forth by NCQA, an On Site Evaluation will be completed with selected hospitals, programs, individual practitioners and practice groups. As part of the credentialing process, an on site evaluation may be conducted for these providers prior to acceptance to the network, every three years Thereafter as part of the re-credentialing process, or earlier if quality concerns are identified by the Credentialing Committee. A Provider Operations staff member will meet with the provider to discuss the role of the provider and of APS-PR in the provision of behavioral healthcare services to our members. APS-PR policies and procedures will be reviewed and the provider’s adherence to APS-PR standards will be evaluated. The evaluation will consist of a review of the provider accessibility to APS-PR members, the provider’s medical record keeping standards, and the provider’s office site appearance. Records must be kept in locked files maintained in an area that protects the confidentiality of the patient, and are not accessible to the general public. At the conclusion of the evaluation, the provider will be informed of any deficiencies and given the opportunity to submit a corrective action plan to redress those areas. The corrective action plan must be submitted to the Credentialing Committee in writing within thirty (30) days of the site visit. I. TREATMENT RECORD REVIEW 1. In addition to On Site Evaluations, APS-PR may also conduct reviews of Provider’s treatment records in accordance with Law 408 , HIPPA and national standards such as Rev. 12.2013 Page 21 Of 81 NCQA and AMA The providers included in the annual treatment record review sample is based upon the volume of work done for APS-PR. Treatment records may be reviewed on site in the providers office or APS-PR may request that the records be copied and forwarded by mail to APS-PR for review. In any case, the records should be blinded as the identity of the member and will be treated confidentially by APS-PR. Please see below for the Treatment Record documentation standards that are congruent to those of NCQA. J. TREATMENT DOCUMENTATION GUIDELINES 1. Each page in the record contains the patient’s name or identification number. 2. Each record includes the patient’s address, employer or school, home and work telephone numbers including emergency contacts, marital or legal status, appropriate consent forms (including consent for treatment) and guardianship information if relevant. 3. All entries in the treatment record include the responsible clinician’s name, professional degree, and relevant identification number if applicable. 4. All entries are dated. 5. The record is legible to someone other than the writer and in ink. 6. Relevant medical conditions are listed, prominently identified, and revised. 7. Presenting problems, along with relevant psychological and social conditions affecting the patient’s medical and psychiatric status are documented. 8. Assessment of severity and imminence of potential harm to self or others is completed and documented at least once and then as often as appropriate.1 9. Special status situations, such as imminent risk of harm, suicidal ideation, or elopement potential, are prominently noted, documented, and revised in compliance with written protocols. 10. Each record indicates what medications have been prescribed, the dosages of each, and the dates of initial prescription or refills. 11. Allergies and adverse reactions are clearly documented. 1 CRITICAL INDICATOR Rev. 12.2013 Page 22 Of 81 12. A medical and psychiatric history is documented (for example: including previous treatment dates, provider identification, therapeutic interventions and responses, sources of clinical data, relevant family information, results of laboratory tests, and consultation reports). 13. For children and adolescents, prenatal and prenatal events, along with a complete developmental history (physical, psychological, social, intellectual, and academic) are documented. 14. For patients 12 and older, documentation includes past and present use of cigarettes, alcohol, illicit drugs, and prescription medication(s). 15. A mental status evaluation documents the patient’s affect, speech, mood, thought content, judgment, insight, attention or concentration, memory, and impulse control. 16. A DSM-IV diagnosis is documented, consistent with the presenting problems, history, mental status examination, and/or other assessments. 17. Treatment plans are consistent with diagnoses and have both objective measurable goals and estimated timeframes for goal attainment or problem resolution. 18. The focus of treatment interventions is consistent with the treatment plan goals and objectives. 19. Informed consent for medication and the patient’s understanding of the treatment plan is documented. (For MDs/DOs only) 20. Patients who become homicidal, suicidal, or unable to conduct activities of daily living are promptly referred to the appropriate level of care. 21. The treatment record documents preventive services, as appropriate (e.g., relapse prevention, stress management, wellness programs, lifestyle changes, and referrals to community resources). 22. 2 Treatment record provides evidence of practitioner attempting to obtain consent to communicate with other behavioral healthcare providers or practitioners when appropriate. 23. 2 3 3 Treatment record provides evidence of communication and coordination of care with other behavioral healthcare providers or practitioners if they exist. CRITICAL INDICATOR CRITICAL INDICATOR Rev. 12.2013 Page 23 Of 81 24. 4 Treatment record provides evidence of practitioner attempting to obtain consent to communicate with primary care physician (PCP) or other ancillary providers/health care institutions when appropriate. 25. 5Treatment record provides evidence of coordination of care with primary care provider (PCP) or other ancillary providers/health care institutions when they exist. 26. The treatment record documents dates of follow-up appointments or, as appropriate, a discharge plan. APS-PR reviews a random sample of treatment records. Records are selected from APS-PR enrollees that have started treatment with the practitioner during the prior year. To ensure the confidentiality of patient information, APS-PR reviewers or vendors use the following procedures: • • • • Reviewers are licensed healthcare professionals with a contractual and professional obligation to maintain confidentiality; The provider is given advanced notice of the review. The provider is requested to blind all patient-identifying information, and The records remain at the provider’s office throughout on-site review. Three (3) treatment records are reviewed at each individual practitioner site. At ambulatory organizational provider sites at least 10 records are reviewed, selected across all practitioners at the site. Providers receive written notification of their results within 90 days of the review. They receive their completed tool along with the record keeping toolkit. Compliance with the standards requires an overall score of 60%. Compliance with Critical Indicator #15, assess of severity and imminence of self harm and requires a score of 80%. Compliance with Critical Indicators 34, 35, 36 and 37 requires a score of 60%. Providers who fall below the acceptable threshold (above) are referred to the Provider Quality Monitoring Committee for further review and follow-up. Results of the provider treatment record keeping review are documented in the provider file and reviewed at the time of re-credentialing. [ III ] UTILIZATION MANAGEMENT APS-PR was founded upon the belief that quality and successful outcomes in behavioral healthcare are achieved by providing access to the most appropriate care, at the right time and in the least restrictive setting. In order to accomplish this ambitious goal, APS-PR maintains an experienced staff of licensed clinicians on-site Monday through Friday from 8 a.m. to 6 p.m., with availability 24 hours a day, seven days a week. These clinicians bring to APS-PR significant mental health and substance abuse (MH/SA) inpatient and outpatient experience gained in the field, together with a 4 5 CRITICAL INDICATOR CRITICAL INDICATOR Rev. 12.2013 Page 24 Of 81 successful history of managing the utilization of behavioral healthcare services for our 8 million members. The APS-PR Utilization Management (UM) process begins with a comprehensive clinical intake including risk assessment. Fulfilling more than the traditional role of determining medical necessity, we design our systems to serve as a resource to patients, families and providers. Further, our clinical staff is always looking for opportunities to develop and implement alternatives to the more typical adversarial utilization review. For example, outpatient providers have the convenient option of using the APS-PR automated Outpatient Treatment Review (OTR) form to submit clinical information and obtain authorization for routine cases via fax. This process can be completed without having to speak to a care manager. The APS-PR Clinical Triage Tool system provides active, next day follow-up for all members who have been identified through triage as “Urgent” or “Emergent”. Using our Utilization Management Guidelines, written medical necessity criteria consistent with national practice standards, our care managers work pro-actively with both the patient and the provider to build consensus around the appropriate level of care, treatment plan and goal. A copy of the most current APS-PR Utilization Management Guidelines is included in this manual. Utilizing a full continuum of care consisting of network providers who have been credentialed to National Committee for Quality Assurance (NCQA) standards, our care managers monitor the quality of care and provide ongoing clinical review of a member’s treatment in collaboration with our provider partners throughout the entire process. In addition, care managers maintain linkage with the PCP in order to ensure effective coordination of care. In those instances where care managers and providers have difficulty determining the proper diagnosis, course of treatment or proper level of care, our physician advisors are available to offer assistance. Another critical tool that aids APS-PR care managers in tracking and coordinating ongoing care is our award-winning information system. The APS-PR clinical staff uses this system to verify and track eligibility and benefits, document complaints about APSPR clinical or service issues, authorize services, document the electronic medical record, generate certifications, initiate provider searches and document appeals. This system also assists in tracking communications with primary care physicians and other service agencies. A. CLINICAL PROCEDURES The procedures described in this section apply only when a provider is treating a member who has a behavioral health care benefit plan that is managed by APS Healthcare Puerto Rico, Inc. Rev. 12.2013 Page 25 Of 81 1. Referral and Authorization Procedures APS-PR maintains a twenty-four (24) hours, toll free telephone through which members, their families, primary care physicians and providers may request referrals for behavioral health care services. Members are not required to obtain a referral from a PCP to access behavioral health services, though APS-PR will work with a PCP to obtain a referral should the occasion present itself. 2. Initial/Concurrent Review An APS-PR Member Referral Coordinator processes member requests for routine referrals during business hours. An APS-PR Member Referral Coordinator verifies eligibility, updates demographic information, and educates members regarding their benefits. In most instances, these call are received from the member actually seeking treatment. However, APS-PR will work with a PCPs or family members with the permission of the member seeking treatment. The Member Referral Coordinator conducts a very brief, objective screening to ensure that the member’s situation is non-urgent. (Any suspected urgent situation is transferred to a Care Manager to handle the call.) Once this is established, the Member Referral Coordinator searches the network for a provider who offers services that best match the member’s clinical needs. The member is given the name and telephone number of a geographically accessible network provider. The member is then instructed to contact the provider to schedule an appointment. If a member is referred to a practice group, APS remind the member to ask for an APS-PR credentialed provider within the group at the time the appointment is made. The APS-PR Member Referral Coordinator enters an authorization number into the APS-PR data system, linking the provider with the member. The authorization number, co-payment or coinsurance requirements are mailed to the provider once a week. For those providers who do not have fax numbers, the authorization notice is mailed to the provider. Authorization for additional treatment sessions is based upon medical necessity and the availability of benefits. To request authorization for additional sessions either complete and fax the APS-PR Outpatient Treatment Review Form or call the APS-PR Care Management Department to conduct a clinical review at least one week prior to the last authorized session or send by fax or by mail an APS-PR Treatment Plan Form. This review will include, but is not limited to, the following information: presenting problem, DSM-IV diagnosis (all 5 axes), current symptoms, prior psychiatric and substance abuse history and treatment, mental status, medications (dosage and side effects), medical complications and significant medical history, treatment plan and progress. The Care Manager’s decision to authorize further sessions will be based on medical necessity. When treatment has been terminated with a member, the provider is to inform APS-PR. At that time, any unused authorized sessions will be credited to the member’s benefit. Rev. 12.2013 Page 26 Of 81 3. Medication Management When a member who is receiving ongoing outpatient psychotherapy requires a referral to a psychiatrist for a medication evaluation or for ongoing medication management, the primary therapist is to contact APS-PR to obtain a referral for that member. When in agreement with the provider’s recommendation, the APS-PR Care Manager will authorize a psychiatric evaluation. Upon review of the evaluation with the psychiatrist, the Care Manager will authorize medication management visits. When a member is in treatment with both a therapist and a psychiatrist, both providers are expected to work together in the coordination of that member’s care. Ongoing authorization for medication management can be obtained by either faxing the required clinical information on APS-PR’ medication management form, or by contacting an APS-PR care manager for a telephone interview. 4. High Risk Indicators APS-PR Care Managers closely monitor all members identified as at risk due to the following conditions, characteristics or past treatment histories: Criteria for the admission to the Program of High Risk 1. Re-admission within 30 days after the discharge 2. Two or more suicide/homicide attempts within 30 days 3. Homicide attempt 4. Admission of children less than 12 years of age 5. Admission of children less than 12 years of age with psychotic episode. 6. Specific cases identified by the Health Plan, the Consultant of Medical Affairs, APSPR-PR Clinical Practitioners, or Clinic Administrators Should you identify a member with a high-risk indicator, contact APS-PR’s Care Management Department. 5. Hospital and Program Services When a member demonstrates a need for admission to an inpatient facility, a partial hospitalization program, an intensive outpatient program or an evaluation for these or any other services, a call to APS-PR must be made to request authorization for services or to schedule an evaluation to determine the most appropriate level of care. All hospital and program admissions must be pre-authorized unless there is a lifethreatening medical emergency (see Emergency Services). The Care Manager will schedule an evaluation or admission based on the information provided by the caller. The Care Manager, in conjunction with the hospital or program’s attending physician or designee, will review the clinical information to determine the type and intensity of treatment that would most benefit the member. The decision to authorize an admission to a hospital or a program will be based on medical necessity. Rev. 12.2013 Page 27 Of 81 When a Care Manager authorizes an admission, a preliminary treatment plan is formulated and the authorized length of stay or number of sessions is communicated to the hospital or program. When additional sessions or days are required, the attending physician or designee is to call APS-PR to discuss further treatment prior to the last day of authorized services. 6. Emergency Services In accepting a referral from APS-PR, network providers accept the responsibility of providing twenty-four (24) hour urgent and emergency services for our members. Patients in active treatment should be given instructions on how to contact their provider or a covering provider in the case of an emergency. Members who have behavioral health care benefits that are managed by APS-PR are instructed to go to an emergency room only when the member, acting reasonably, believes that an emergency condition exists. As stated previously, it is expected that answering machine messages and/or answering services provide patients with a number to contact the provider in an emergency. A message that states that the patient should go to the emergency room is not acceptable. In the member’s Group Membership Agreement, a “medical emergency” is defined as the sudden onset of a medical condition manifesting itself by acute symptoms of sufficient severity such that the absence of immediate medical attention could reasonably result in: permanently placing the members health in jeopardy; severe impairment to bodily function; serious and permanent dysfunction to any body organ or part. Emergency services are delivered by a provider in cases where the provider has conducted a clinical diagnostic interview sufficient to determine that the member is harmful to self or others and in need of immediate intervention to foster member safety. Intervention may include safe transport if medical necessity applies, and any of the following: inpatient evaluation, a 23-hour observation bed, inpatient admission, or inpatient detoxification. The member is the clinical responsibility of the provider who arranges transportation and provides clinical support while continuously monitoring the member to prevent harm. Intervention should be immediate and constant until the clinical situation is de-escalated. Once an intervention is completed, the provider is requested to call the care manager within six (6) hours to report the outcome and review the next level of care requirements for precertification. If a colleague or office staff member is available, contacting the care manager immediately for authorization and assistance is recommended. The member’s behavioral health care provider is expected to triage all other urgent and emergency situations. APS-PR Care Managers are available through our 800 number Rev. 12.2013 Page 28 Of 81 twenty-four (24) hours per day to assist providers with emergency cases. Contact a Care Manager whenever a member requires emergency attention. APS Healthcare Puerto Rico, Inc. must be notified by the hospital, admitting physician and/or patient of an emergency admission within two (2) hours of the admission. Once notified, procedures for assigning an authorized length of stay are the same as for elective admissions. When a provider is contacted by a patient in need of an outpatient emergency intervention, the provider is to call APS-PR to obtain authorization. If the member requires a service that the provider cannot offer, the provider is to contact the Care Management Department to arrange for the required intervention. 7. Discharge Planning Discharge planning begins at the initiation of all hospital and program services. It includes preparing the patient and the family for the next level of care and arranging for placement or provision of additional services. APS-PR Care Managers will work with hospitals and programs to assure a smooth transition and the use of participating providers for follow-up care within 5 days of discharge. 8. Electroconvulsive Therapy (ECT) APS-PR follows guidelines consistent with national standards on electroconvulsive therapy (ECT) as promulgated by the American Psychiatric Association’s task force on electroconvulsive therapy. When covered under a member’s Group Medical Agreement, outpatient and inpatient electroconvulsive therapy may be authorized by an APS-PR Physician Advisor. Inpatient and outpatient ECT must be conducted at a network facility by a network psychiatrist who is an ECT sub-specialist. Inpatient ECT must be conducted during an authorized inpatient stay. An APS-PR Physician Advisor will authorize a specific number of inpatient or outpatient ECT sessions based on medical necessity. 9. Psychological Testing As behavioral health care shifts its focus to target specific clinical outcomes, the role of psychological testing becomes more refined and discrete. Psychological testing is to be used as an adjunct to assist clinicians with complex differential diagnoses. All psychological testing, inpatient and outpatient, requires pre-authorization from a APSPR Care Manager. 10. Neuropsychological Testing The task of neuropsychological testing is to understand the behavioral, cognitive or emotional difficulties of adults and children brought forth by cerebral dysfunction. Rev. 12.2013 Page 29 Of 81 Neuropsychological testing is used predominantly for medical-surgical or comorbid conditions. APS-PR will consider authorizing neuropsychological testing for psychiatric conditions only after a neurological assessment and a psychiatric assessment have been conducted. Approval of neuropsychological testing will be based on the necessity to refine or differentiate a psychiatric diagnosis resulting in a modification and/or enhancement of the treatment plan. An expert neuropsychology consultant or a physician advisor who is board certified in neurology is used to make decisions in this area. Requests for neurological testing when a definitive organic condition is present will be referred to the members Health Plan or PCP. 11. Referrals to Other Providers One of APS-PR’s highest priorities is to offer its members a fully integrated system of care. We strive to develop networks of providers which offer a spectrum of behavioral health care services and specialties available today. When a provider recognizes that a member would benefit from additional behavioral health care services, such as group therapy, a medication evaluation or an intensive outpatient program, the provider is to contact the Care Management Department to request an authorization to another APSPR provider. Referrals for medical/surgical services are to be coordinated through the member’s medical plan and/or Primary Care Physician. 12. Primary Care Liaison Program APS-PR’ clinical philosophy places an emphasis on the integration on behavioral and medical health care. The purpose of the Primary Care Liaison Program is to assure the coordination and integration of care provided to HMO members by APS-PR network providers and the members’ Primary Care Physician. APS-PR maintains that the successful coordination and integration of the behavioral and medical health care delivery system results in improved quality of care and outcomes as well as reduced costs due to increased efficiency. In the last few years, an increase in awareness has occurred in the medical community of the need for PCP contact with medical and behavioral health specialists who treat their patients. Many psychiatric problems present as medical conditions and many medical problems present with psychiatric symptoms. While APS-PR recognizes problems that exist in maintaining member confidentiality, we also understand the benefit of an informed PCP as to a patient’s whole health care. Such information is relevant when the provider patients: • • • • Are taking prescription drugs or medications; had a recent inpatient stay for mental health or substance abuse; Have a substance abuse problem that affects their physical health; or Represents a danger to themselves. Rev. 12.2013 Page 30 Of 81 APS-PR providers will provide the member’s PCP with the following information: • • • • • • list of medication and changes in medication prescribed by the behavioral health care provider (psychiatrist); indications of side effects of medications and/or drug interactions; suspected medical/physical conditions; impatient hospitalization with or without physical comorbidity; significant substance use; potential effects on the member’s physical condition and/or medical care due to proposed or active behavioral health care treatment; In order to communicate with the member’s PCP, the provider will need to have the member sign an Authorization for Release of Information. Providers should educate their members about the benefits of their PCP being informed of the initiation and progress of their behavioral health care. A Release of Information sample form is included as an attachment of this manual. B. CLINICAL PRACTICE GUIDELINES NCQA requires that APS-PR adopt and disseminate practice guidelines that are relevant to its membership. In order to meet the intent of these NCQA standards, APSPR endorses practice guidelines published by other professional organizations. APSPR providers are informed of the adoption of these guidelines and about how providers may obtain copies via mailings. APS-PR provider practices are expected to conform to the treatment protocols contained in adopted guidelines. Compliance with the practice guidelines will be assessed via treatment record reviews conducted by APS-PR annually. C. INTRODUCCTION TO THE MEDICAL NECESSITY AND LEVELS OF CARE DETERMINATION CRITERIA OF APS-PR APS-PR believes that patients are best treated in the least restrictive environment consistent with the patient’s symptoms, support and safety requirements. The goal of treatment is the restoration of the patient to optimal functionality and independence. This document is intended to be a starting point and common reference for clinical discussion. As such, it focuses on the patient’s clinical history, presenting symptoms and available resources in recommending a level of care. We recognize that resources for the full continuum of care do not exist in all locations. In those cases, we will recommend a higher level of care than medically necessary in order to assure safe and effective treatment. “Medical Necessity” as the term is used here, means that care which is determined to be effective, appropriate and necessary to treat a given patient’s disorder. Each level of care is indicated as either Psychiatric or Substance Dependence (except for the outpatient level of care which subsumes both) and review for level of care determination proceeds in a logical progression to confirm: Rev. 12.2013 Page 31 Of 81 • • • • The presence of a properly diagnosed mental health or substance abuse disorder amenable to treatment; Symptoms of sufficient severity to meet the required criteria for admission; The illness by accepted medical standards is expected to improve significantly through medically necessary and appropriate care as it relates to the level of care requested; and Clinical requirements for continuing care at that level. Discharge criteria, program content, treatment interventions etc., are not included in an attempt to avoid being too prescriptive and preempting clinical discourse. Therefore, determinations for discharge from a given level of care are clear: when the patient no longer appears to meet the required criteria for continuing care at a given level of acuity, discharge to a lower level of care is recommended. As an integral part of our quality improvement process, we will review annually and revise this document as needed based upon developments in the professional literature and feedback from all participants in treatment reviews. However, we welcome your comments and suggestions at any time. D. DEFINITIONS FOR LEVELS OF CARE APS-PR recognizes the following as distinct levels of care: Psychiatric Services: 1. Acute Inpatient—The highest intensity of medical and nursing services provided within a structured environment providing 24 hours skilled nursing and medical care. Full and immediate access to ancillary medical care must be available for those programs not housed within general medical centers. 2. Residential Treatment— Care provided at a subacute level with skilled nursing care. These may be intermediate care facilities (ICF) or have other licensing designations that may vary by state. 3. Partial Hospital— an intensive, non-residential, level of service where multidisciplinary, medical and nursing services are required. This care is provided in a structured setting, similar to inpatient intensity, meeting for more than four hours (and, generally, less than eight hours) daily. 4. Intensive Outpatient—Multidisciplinary, structured services provided at a greater frequency and intensity than routine outpatient treatment. These are generally up to four hours per day, up to five days per week. Common treatment modalities include individual, family, group and medication therapies. Rev. 12.2013 Page 32 Of 81 5. Outpatient—The least intensive level of service. Typically provided in an office setting from 60 to 90 minutes (for group therapies) per day. 6. 23-Hour Observation—“23-hour beds” are defined as a period of up to 23 hours during which services are provided at less than an acute level of care. It is indicated for those situations where full criteria are not met because of external factors relative to information gathering or risk assessment yet the patient clearly at risk for harm to self or others. Substance Abuse Services: 1. Inpatient Detoxification—Detoxification services provided in a 24 hours hospital setting with full nursing and medical care. Generally provided on inpatient psychiatric units, services can also be given on a medical/surgical unit when needed for safety or in the absence of adequate services elsewhere. 2. Inpatient Rehabilitation—Twenty-four hour per day supervised care for a substance dependence diagnosis not requiring full nursing and medical services. 3. Residential Treatment—Care provided at a sub-acute level with skilled nursing care. These may be intermediate care facilities (ICF) or have other licensing designations that may vary by state. 4. Outpatient/Ambulatory Detoxification—Detoxification services delivered within a structured program having medical and nursing supervision where physiological consequences of withdrawal have not life-threatening potential. 5. Partial Hospital—An intensive, non-residential, level of care where multidisciplinary, medical and nursing services are required. This care is provided in a structured setting, similar in intensity to inpatient, meeting for more than four hours (and, generally, less than eight hours) daily. Such care is appropriate for substance abuse treatment when provided in conjunction with ambulatory detoxification or when medical comorbidity or other complications make less intensive levels of care unsafe or inadequate. 6. Intensive Outpatient Programs—Multidisciplinary, structured services provided at a frequency of up to four hours daily, up to five days per week for the treatment of a substance dependence disorder. 7. Outpatient—For substance dependence disorders, this is not a recommended level of care. However, exceptions may exist for which this will be a necessary level of care (see: Level of Care Determination Criteria). E. 23-Hour Observation (ALL TYPES OF CARE, ALL AGE GROUPS) Rev. 12.2013 Page 33 Of 81 (Note: “23-hour beds” are defined as a period of up to 23 hours during which services are provided at less than an acute level of care. It is indicated for those situations where full criteria are not met because of external factors relative to information gathering or risk assessment yet the patient clearly at risk for harm to self or others.) A. Medical Necessity—(All must be met to consider for treatment.) 1. The patient must have been assessed, to a reasonable degree of medical certainty, as having a psychiatric illness or substance abuse disorder by a licensed health professional. 2. Symptoms of this illness must accord with those described in the Diagnostic and Statistical Manual of Mental Disorders, Edition IV (DSM-IV). 3. The diagnosis must have been arrived at prior to admission in a face-to-face encounter between the professional and patient. B. Admission Criteria—(Either 1 or 2 and 3 are sufficient to recommend treatment.) 1. The presenting clinical problem likely represents a transient disruption of the patient’s clinical baseline which will likely remit with a period of structure and observation. or 2. The patient presents with a significant history of sedative/hypnotic dependence representing a genuine risk of rapidly developing signs and symptoms of withdrawal, which will meet inpatient detoxification criteria and 3. The presenting clinical problem represents a clear, proximal risk of harm to self or others. F. Inpatient (Acute Care) PSYCHIATRIC: (ADULT, CHILD, ADOLESCENT*) A. Medical Necessity—(All are required to consider for admission.) 1. The patient must have been diagnosed with a psychiatric illness by a licensed mental health professional. 2. Symptoms of this illness must accord with those described in the Diagnostic and Statistical Manual of Mental Disorders, Edition IV (DSM-IV). 3. The diagnosis must have been arrived at prior to admission in a face-to-face encounter between the professional and patient. B. Admission Criteria - (At least one criterion needs to be met to recommend admission). Rev. 12.2013 Page 34 Of 81 1. 2. 3. 4. Patient presents suicidal ideation and intention, which represent significant or imminent risk of self harm, that 24 hours hospitalization and observation are necessary for the patient’s safety. Patient presents with a recent history of grossly disrupted and/or violent behavior representing clear and present danger of serious harm to others. The patient’s psychiatric condition impairs his/her basic functional capacity as to represent a genuine and proximal risk of danger to self such that 24hour intensive nursing and medical treatment are required. Diagnosis and/or treatment is/are clearly unsafe or impossible to provide in an outpatient setting and can only be accomplished with 24 hours intensive nursing and medical care. C. Continuing Care Criteria - (At least one criterion needs to be met to recommend admission). 1. 2. 3. Daily physician and staff progress notes clearly describe the patient’s lack of progress despite adequate clinical intervention and/or the emergence of new symptoms sufficient to meet acute care criteria. Daily physician progress notes indicate serious medical complications of pharmacotherapy or other somatic treatments such that transition to a lower level of care represents clear risk of harm. Daily progress notes indicate that attempts to transition to a lower level of care have resulted in a reemergence of symptoms sufficient to meet acute care criteria. * Additional Child/Adolescent Criterion—(Must be met for continuing care.) Documented evidence of significant family involvement at least three times weekly or clearly documented evidence that such is medically contraindicated. G. Inpatient Detoxification SUBSTANCE DEPENDENCE: (ADULT/ADOLESCENT*) A. Medical Necessity—(All are required to consider for admission.) 1. The patient must have been diagnosed with a substance dependence disorder by a licensed mental health professional or equivalent licensed substance abuse professional. 2. Symptoms of this illness must accord with those described in the Diagnostic and Statistical Manual of Mental Disorders, Edition IV (DSM-IV). 3. The diagnosis must have been arrived at prior to admission in a face-to-face encounter between the professional and patient. B. Admission Criteria—(All three required for admission.) Rev. 12.2013 Page 35 Of 81 1. The patient has a documented history of severe, continuous dependence on alcohol and/or sedative/hypnotic drugs and withdrawal from the substance of abuse represents a genuine potential for serious physical harm. 2. Detoxification services are either not available on an outpatient basis or require 24 hours intensive nursing and medical treatment on an inpatient basis for medical reasons of safety. 3. The patient currently exhibits severe signs and symptoms of active withdrawal and/or has a history of medically documented withdrawal seizures or delirium tremens. C. Continuing Care Criteria—(Both criteria must be met to recommend continuing care.) 1. Daily physician documentation of physical signs and symptoms of active withdrawal which require 24 hours intensive nursing and medical care. 2. Clear, documented clinical evidence of the need for skilled nursing and medical treatment for active withdrawal. * Additional Adolescent Criterion—(Must be met to recommend continuing care.) Documented evidence of family involvement in both family therapy as well as family education and support or clearly documented evidence that such is medically contraindicated. H. Inpatient Rehabilitation SUBSTANCE DEPENDENCE: (ADULT/ADOLESCENT*) A. Medical Necessity—(All are required to consider for admission.) 1. The patient must have been diagnosed with a substance dependence disorder by a licensed mental health professional or equivalent licensed substance abuse professional. 2. Symptoms of this illness must accord with those described in the Diagnostic and Statistical Manual of Mental Disorders, Edition IV (DSM-IV). 3. The diagnosis must have been arrived at prior to admission in a face-to-face encounter between the professional and patient. B. Admission Criteria—(All criteria must be met to recommend admission.) 1. Documentation of a history of severe and continuous alcohol and/or substance dependence. 2. The patient’s psychosocial support system is so impaired as to preclude effective outpatient therapy (e.g. family are active abusers) or outpatient therapy is clearly unsafe at this time because direct physical harm will be an immediate consequence of a return to substance abuse (e.g. pancreatitis, endocarditis). Rev. 12.2013 Page 36 Of 81 C. Continuing Care Criteria—(All criteria must be met to recommend continuing care.) 1. Daily physician progress notes indicate continuing clinical problems (other than placement issues) or the emergence of new clinical problems that are severe enough to meet admission criteria. 2. Family involvement in treatment and discharge planning at least three times weekly and introduction to family supports (e.g., Al-Anon, Nar-Anon) or clear documentation that such is medically contraindicated or inappropriate. 3. A lower level of care is either clearly unsafe or physically unavailable. 4. Documentation of patient participation in abstinence-based groups (e.g. NA, AA) and discharge planning which includes attendance in these or similar community-based supports. * Additional Adolescent Criterion—(Must be met to recommend continued care.) Documented evidence of family involvement in both family therapy as well as family education and support or clearly documented evidence that such is medically contraindicated. I. Partial Hospitalization PSYCHIATRIC CARE: (ADULT, CHILD/ADOLESCENT*) (Note: Partial Hospitalization is a level of care tantamount to the acute level of care with the singular exception that the patient does not require 24 hours medical and nursing care. It is intended to be provided up to eight hours per day, up to seven times per week.) Medical Necessity—(All are required to consider for admission.) A. 1. The patient must have been diagnosed with a psychiatric disorder by a licensed mental health professional. 2. Symptoms of this illness must accord with those described in the Diagnostic and Statistical Manual of Mental Disorders, Edition IV (DSM-IV). 3. The diagnosis must have been arrived at prior to admission in a face-to-face encounter between the professional and patient. Admission Criteria—(All criteria must be met to recommend admission.) B. 1. The patient’s mental condition requires skilled medical and nursing observation (e.g. serial mental status checks, medication administration, monitor vital signs) and is likely to improve with this intervention. 2. Clinical documentation clearly indicates that the patient could not be treated safely at a lower level of care or that partial hospitalization could safely substitute for acute inpatient care. Rev. 12.2013 Page 37 Of 81 3. The patient’s psychosocial supports are such that the patient can be supervised and maintained without clinical supervision for that period of time outside the program. 4. The patient’s condition requires multidisciplinary intervention for four (or more) hours daily and more than three days per week. C. Continuing Care Criteria—(All criteria must be met to recommend continuing care.) 1. Despite adequate treatment, the patient continues to exhibit signs and symptoms that led to the admission, or new problems have emerged which themselves meet the criteria for PHP admission. 2. The patient’s problems must be clearly documented in the medical record and there must be a progress note by the provider for each day of treatment. 3. There must be clear clinical documentation that transition of the patient to a lower level of care would result in exacerbation or re-emergence of symptoms sufficient to meet PHP admission criteria. * Additional Child/Adolescent Criterion—(Must be met to recommend continuing care) There is documented evidence of significant family involvement at least twice weekly or clear documentation that such is medically contraindicated. J. Partial Hospitalization SUBSTANCE DEPENDENCE: (ADULT/ADOLESCENT*) (Note: Partial Hospitalization (PHP) is a level of care tantamount to the acute level of care with the singular exception that the patient does not require 24 hours medical and nursing care. It is intended to be provided up to eight hours per day, up to seven times per week.) Medical Necessity—(All are required to consider for admission.) A. 1. The patient must have been diagnosed with a substance dependence disorder by a licensed mental health professional or equivalent licensed substance abuse professional. 2. Symptoms of this illness must accord with those described in the Diagnostic and Statistical Manual of Mental Disorders, Edition IV (DSM-IV). 3. The diagnosis must have been arrived at prior to admission in a face-to-face encounter between the professional and patient. Admission Criteria—(All criteria must be met to recommend admission.) B. 1. Clinical documentation of a need for multidisciplinary, highly structured, coordinated treatment of a substance-related disorder which clearly indicates Rev. 12.2013 Page 38 Of 81 that the patient could not be treated safely at a lower level of care or that partial hospitalization can safely substitute for acute inpatient care. 2. The patient’s psychosocial supports are such that the patient can be supervised and maintained without clinical supervision for that period of time outside the program. 3. The patient’s condition requires intensive medical and nursing care more than four hours daily and more than three days per week. 4. In cases with numerous treatment failures, evidence that the patient has recently worked to complete a course of treatment but has not been able to complete his/her treatment goals in that setting. Documentation must be provided which confirms the therapeutic potential of this intervention to enable recovery. Continuing Care Criteria (All criteria must be met to recommend continuing care.) C. 1. Despite adequate treatment, the patient continues to exhibit signs and symptoms that led to the admission, or new problems have emerged which themselves meet the criteria for PHP admission. 2. The patient has established a recovery plan, which includes: APS-PR triggers, sober support systems, meeting schedules, and commitment to lifestyle changes to encourage recovery and prevent APS-PR. 3. The patient demonstrates consistent work on treatment goals, the ability to self-report difficulties in the treatment progress, and has the ability to use cognitive/behavioral interventions to alter behavior patterns. * Additional Criterion for Adolescents—(Must be met to recommend continuing care) Documented evidence of family involvement in both family therapy as well as family education and support at least three times weekly or clearly documented evidence that this is medically contraindicated. K. Outpatient Detoxification (Ambulatory Detoxification) SUBSTANCE DEPENDENCE: (ADULT/ADOLESCENT*) (Note: This level of care is intended for those patients who require detoxification prior to starting rehabilitative therapy for chemical dependence but do not require inpatient treatment for safety. It is appropriate for individuals who are not medically compromised and who are unlikely to develop medically dangerous symptoms of withdrawal. Such patients require intensive medical and nursing care but do not require 24 hours observation and support.) Medical Necessity—(All are required to consider for treatment) A. 1. The patient must have been diagnosed with a substance dependence disorder by a licensed clinical professional or equivalent licensed substance abuse professional. Rev. 12.2013 Page 39 Of 81 2. Symptoms of this illness must accord with those described in the Diagnostic and Statistical Manual of Mental Disorders, Edition IV (DSM-IV). 3. The diagnosis must have been arrived at prior to admission in a face-to-face encounter between the professional and patient. B. Treatment Criteria—(All criteria must be met to recommend treatment) 1. The patient requires skilled medical and nursing care in order to accomplish safe detoxification. 2. Clinical documentation clearly indicates that the patient could not be treated safely at a lower level of care. 3. The patient’s psychosocial supports are such that the patient can be supervised and maintained without clinical supervision for that period of time outside direct supervision. 4. The patient’s condition is such that s/he is able to comprehend instructions and access medical help if needed. C. Continuing Care Criteria—(All criteria must be met to recommend continuing care.) 1. The patient continues to display signs and symptoms consistent with withdrawal, which represent a proximal risk of harm if not treated. 2. These problems must be clearly documented in the medical record, and there must be a progress note by a physician for each day the patient is present. 3. There must be documentation for each day of treatment that attempts to transition the patient to a lower level of care would result in re-emergence of symptoms sufficient to meet admission criteria. 4. Evidence of patient awareness that detox is an initial phase of treatment and contracts for continuing treatment at a lower level of care. • Additional Criterion for Adolescents: For adolescents, there must be clearly documented evidence of parental (or equivalent guardianship) consent to and understanding of treatment as well as documented assessment of capacity to support and maintain the patient after hours. L. Intensive Outpatient Therapy PSYCHIATRIC CARE: (ADULT, CHILD/ADOLESCENT*) This level of care includes services at lesser levels of acuity than partial hospitalization. It is intended to be provided less than four hours daily but may be offered up to seven days weekly. A. Medical Necessity—(All are required to consider for treatment.) Rev. 12.2013 Page 40 Of 81 1. The patient must have been diagnosed with a psychiatric disorder by a licensed mental health professional. 2. Symptoms of this illness must accord with those described in the Diagnostic and Statistical Manual of Mental Disorders, Edition IV (DSM-IV). 3. The diagnosis must have been arrived at prior to admission in a face-to-face encounter between the professional and patient. B. Admission Criteria—(All criteria must be met to recommend treatment.) 1. There is documentation of significant and acute deterioration in social, occupational, educational or family functioning. 2. The proposed treatment plan addresses the signs and symptoms consistent with the observed deterioration in functioning. 3. The patient’s condition will benefit from the proposed intervention. 4. There is at least moderate impairment (a GAF less than 70). C. Continuing Care Criteria—(All criteria must be met to recommend continuing care.) 1. The patient continues to exhibit signs and symptoms consistent with admission criteria. 2. The treatment plan reflects ongoing interventions to alleviate these impairments. 3. Clinical documentation supports that attempts to transition to a lower level of care would likely result in exacerbation of the illness. • Additional Criterion For Children/Adolescents: There is clear documented evidence of significant family involvement with and adherence to treatment or clear evidence that this is medically contraindicated. M. Intensive Outpatient Therapy SUBSTANCE DEPENDENCE: (ADULT/ADOLESCENT*) This level of care includes services at lesser levels of acuity than partial hospitalization. It is intended to be provided less than four hours daily but may be offered up to seven days weekly. A. Medical Necessity— (All are required to consider for treatment.) 1. The patient must have been diagnosed with a substance dependence disorder by a licensed clinical professional or equivalent licensed substance abuse professional. 2. Symptoms of this illness must accord with those described in the Diagnostic and Statistical Manual of Mental Disorders, Edition IV (DSM-IV). 3. The diagnosis must have been arrived at prior to admission in a face-to-face Rev. 12.2013 Page 41 Of 81 encounter between the professional and patient. B. Admission Criteria—(All criteria must be met to recommend treatment.) 1. The patient has a history of recent and/or continuous substance abuse/dependence which is meeting DSM-IV criteria but who is stable and competent enough to be adequately treated at this level of intervention. 2. There is clinical evidence which shows that the support of 12-step groups (or other self-help groups) plus regular outpatient care is inadequate to assure abstinence and recovery. 3. In cases with numerous treatment failures, evidence that the patient has recently worked to complete a course of treatment but has not been able to complete his/her treatment goals in that setting. Documentation must be provided which confirms the therapeutic potential of this intervention to enable recovery. C. Continuing Care Criteria—(All must be met to recommend continuing care.) 1. The patient continues to exhibit signs and symptoms consistent with admission criteria. 2. The patient demonstrates consistent work on treatment goals, the ability to self-report difficulties in the treatment progress, and has the ability to use cognitive/behavioral interventions to alter behavior patterns. 3. The patient’s abstinence is monitored through random urine screens and specific modifications to the treatment plan are made in response to positive urines. 4. The treatment plan identifies individual problems in recovery, prioritizes them and has a focused plan for resolution. 5. Documented evidence of family involvement in both family therapy as well as family education and support or clearly documented evidence that this is medically contraindicated. N. Outpatient Care PSYCHIATRIC/SUBSTANCE DEPENDENCE This level of care is the least intensive level of treatment and represents the majority of care delivered. It is intended from 15 minutes (medication management) up to 90 minutes (group therapy) per day not more than twice weekly. A. Medical Necessity - (All are required to consider for treatment.) 1. The patient must have been diagnosed with a psychiatric or Substance dependence disorder by a licensed mental health professional or equivalent licensed substance abuse professional. 2. Symptoms of this illness must accord with those described in the Diagnostic and Statistical Manual of Mental Disorders, Edition IV (DSM-IV). Rev. 12.2013 Page 42 Of 81 3. The diagnosis must have been arrived at prior to admission in a face-to-face encounter between the professional and patient. B. Admission Criteria—(All must be met to recommend treatment.) 1. As a consequence of a DSM-IV diagnosis, the individual is experiencing significant impairment in functioning in one or more of the following areas: • social, • occupational, • educational or • family role. 2. The proposed treatment plan is focused on: • adaptive responses to present impairments, • clearly defined and measurable goals and • a defined time frame. 3. The patient has the requisite cognitive and emotional skills necessary to benefit from the proposed treatment plan. C. Continuing Care Criteria - (All must be met to recommend continuing care.) 1. There is evidence that the patient is working to complete treatment goals and is attending sessions as scheduled. 2. The patient continues to exhibit impairment requiring further treatment (GAF <70). 3. The treatment plan clearly addresses the impairments necessitating ongoing care. 4. If the GAF is >70, the patient has a diagnosis of a persistent DSM-IV disorder which requires maintenance treatment to avoid recurrence of symptoms. O. Residential Treatment (RTC, Domiciliary Care) PSYCHIATRIC CARE: (CHILD/ADOLESCENT) (Note: Residential Treatment is defined as 24 hours, supervised, inpatient level of care provided to children and adolescents who have long-term illnesses not likely to respond to short-term interventions. They should provide, in addition to diagnostic and treatment services, instruction and support toward attainment of basic living skills, which will enable them to live in the community upon discharge.) A. Medical Necessity - (All are required to consider for admission.) 1. The child or adolescent has been diagnosed with a psychiatric disorder by a licensed mental health professional. 2. Symptoms of this illness accord with those described in the Diagnostic and Statistical Manual of Mental Disorders, Edition IV (DSM-IV). Rev. 12.2013 Page 43 Of 81 3. The diagnosis must have been arrived at prior to admission in a face-to-face encounter between the professional and patient. B. Admission Criteria - (All must be met to recommend admission.) 1. There is clear clinical evidence that the child/adolescent has a severe mental illness, which requires a level of intensity of services not available in the community. 2. The illness or disorder is likely to improve with active treatment. 3. Without this intervention, there is clear evidence that the child/adolescent will likely decompensate and represent a proximal risk of serious harm to self or others. C. Continuing Care Criteria—(All must be met to recommend continuing care.) 1. The patient continues to exhibit signs and symptoms consistent with admission criteria. 2. There is a complete, multidisciplinary, individualized treatment plan, which includes input from the patient and family. 3. The treatment plan defines clear, measurable objectives leading to a goal of return to the community. 4. There is documented evidence of active psychiatric care which is symptomfocused and specific to the child/adolescent’s diagnosis. 5. There is documented evidence of active family therapy at least weekly or clearly documented evidence that such is either impossible or medically contraindicated. P. Residential Treatment (RTC, Domiciliary Care) SUBSTANCE DEPENDENCE: (ADULT/ADOLESCENT) (Note: Residential Treatment for substance dependence is defined as 24 hours, supervised, inpatient level of care provided to adults and adolescents who have longterm substance use disorders not likely to respond to short-term interventions. They should provide, in addition to diagnostic and treatment services, instruction and support toward attainment of basic skills, which will enable them to maintain sobriety in the community upon discharge.) A. Medical Necessity - (All are required to consider for admission.) 1. The patient must have been diagnosed with a substance dependence disorder by a licensed clinical professional or equivalent licensed substance abuse professional. 2. Symptoms of this illness must accord with those described in the Diagnostic and Statistical Manual of Mental Disorders, Edition IV (DSM-IV). 3. The diagnosis must have been arrived at prior to admission in a face-to-face Rev. 12.2013 Page 44 Of 81 encounter between the professional and patient. B. Admission Criteria—(All must be met to recommend admission.) 1. There is a clearly documented history of significant impairment in all realms of life as a consequence of a substance abuse disorder. 2. Evidence that the patient has recently worked to complete a course of treatment but has not been able to complete his/her treatment goals in a less restrictive environment. 3. There is credible clinical evidence that, without 24 hours support and care, the patient is likely to suffer serious harm or present a risk of same to others as a direct consequence of the substance abuse disorder and/or related behavioral disturbance. 4. The patient’s external support systems are inadequate to sustain treatment at a lower level of care. C. Continuing Care Criteria (All must be met to recommend continuing care.) 1. The patient continues to exhibit signs and symptoms consistent with admission criteria. 2. There is documented evidence of active participation in and compliance with treatment by the patient. 3. There is a complete, multidisciplinary, individualized treatment plan, which includes input from the patient and family. 4. The treatment plan defines clear, measurable objectives leading to a goal of return to the community. 5. There is documented evidence of active family therapy at least weekly or clearly documented evidence that such is either impossible or medically contraindicated. 6. There is evidence that return to the community at the time of review would likely lead to relapse and represent a proximal risk of serious harm to self or others as a direct consequence of the substance abuse disorder and/or related behavioral disturbance. Q. Methadone Maintenance NoteThe purpose of methadone maintenance is the stabilization of an opiate addiction. Multidisciplinary, structured services are provided at a frequency of up to two hours daily, up to six days per week. Such care is appropriate for members meeting all federal and state requirements for enrollment in this treatment modality at a licensed facility. Treatment includes but is not restricted to administration of methadone, medical supervision of dosage and dispensing, individual and group therapy. A. Medical Necessity(All are required to consider for admission.) Rev. 12.2013 Page 45 Of 81 1. The patient must have been diagnosed with an active opiate addiction by a licensed mental health professional or equivalent licensed substance abuse professional. Symptoms of this addiction must accord with those described in the Diagnostic and Statistical Manual of Mental Disorders, Edition IV (DSMIV). 2. The patient must meet all federal and state requirements for this treatment modality. This includes documentation of prior failure at abstinence based treatment modalities. 3. The diagnosis must have been arrived at prior to admission and in a face to face encounter between the professional and the patient. B. Admission Criteria(All criteria must be met to recommend admission.) 1. The patient has a history of prior failures at abstinence based treatment modalities, recent and continuous opiate addiction which meets DSM-IV criteria, but who is stable enough to utilize an outpatient treatment modality. 2. The patient has established a contract for behavioral changes while in treatment that supports stabilization of his opiate addiction. These include abstinence from other proscribed drugs and intoxicants, random urinalysis and breathalyzer tests to verify abstinence, attendance at all required therapy sessions, and agreement to conditions for involuntary detoxification if stabilization in methadone maintenance is not demonstrated through progress in completing treatment goals. 3. In cases with recent, prior treatment failures in this treatment modality, documentation must be provided that confirms the therapeutic potential for stabilization in this treatment intervention. C. Continuing Care Criteria(All criteria must be met to recommend continuing care.) 1. The patient continues to exhibit signs and symptoms consistent with admission criteria. 2. The patient demonstrates consistent work on treatment goals, the ability to self-report difficulties with treatment progress, and the use of cognitive/behavioral interventions to alter behavior patterns. 3. The patient's abstinence is verified through random urinalysis and breathalyzer tests. Specific modifications in the treatment plan are developed in response to positive tests, and monitoring of these modifications documents treatment progress or continued need for treatment modifications. 4. The treatment plan identifies specific, individual problems with stabilization. It develops treatment strategies to resolve each problem and monitors the patient's completion of the treatment strategies. 5. Prior to a transition to a lower level of treatment intensity, the treatment plan identifies the conditions of stabilization that must be consistently demonstrated to remain at the lower level of intensity. Conversely, there is a Rev. 12.2013 Page 46 Of 81 contract to return to a higher level of intensity if the conditions are not consistently met. 6. Because of the continuing treatment goal of opiate stabilization the treatment plan will identify all instances of substance substitution, cross addictions, cross tolerance, triggers for using, and prevention actions for each identified trigger. 7. Where non-compliance with the treatment plan or avoidance of developing strategies for the treatment plan are demonstrated, the necessity for involuntary detoxification must be discussed as a preliminary to noncertification of continued treatment. R. Electroconvulsive Therapy (ECT) (Note: A course of treatment is generally 6 to 12 ECT. If there is no discernible clinical improvement after 6 to 10 treatments, indications for continued ECT should be formally reassessed. The determination of inpatient or outpatient settings as the appropriate level of care for administering ECT is determined separately based on the patient’s clinical symptoms as they relate to our other levels of care criteria). A. Medical Necessity(All are required to consider for treatment) 1. The patient must have been diagnosed with a psychiatric illness by a licensed mental health professional. 2. Symptoms of this illness must accord with those described in the Diagnostic and Statistical Manual of Mental Disorders, Edition IV (DSM-IV) and must be amenable to ECT. 3. The diagnosis must be based upon a face-to-face evaluation between the professional and patient 4. The psychiatrist who will perform the proposed ECT has completed a face to face evaluation of the patient prior to his recommendation of the procedure. B. ECT Criteria - (If the patient meets one of the 3 criterion, is sufficient for recommendation for treatment) 1. When at least two courses of medication at maximum doses for adequate length of time has been ineffective or the symptoms requires a rapid response from one of the following diagnostic conditions: • • • Severe depression with significant risk of suicide Severe mania Catatonia 2. When the member has a history of a positive response to ECT and a lack of response to medicine in the past 3. Comorbidity when the use of psychotropic medication is compromised by the medical condition; Rev. 12.2013 Page 47 Of 81 S. Psychological Testing APS-PR. believes that members recommended for outpatient testing are best treated when the purpose of the testing, the extent of testing, the instruments used, and the use of results and recommendations are understood by both parties. The goal of outpatient testing is an increased understanding of the patient not readily available by other means. This can include the patient's diagnosis, dynamics, therapeutic capabilities, or treatment planning recommendations. Psychological testing has a wide variety of instruments and techniques as well as post-test interpretation of the results that need to be included in request evaluations. Testing for purposes other than psychological/psychiatric treatment are excluded from the benefit. Examples of this type of testing include occupational placement testing, disability testing, educational testing, neurological testing and forensic testing. Cases requesting neuro-psychological testing with possible indicators of organic damage or history of head trauma, anoxia, heavy metal exposure or diagnosis secondary to a medical condition will be coordinated with the medical plan under the mixed medical protocol. Neurological testing that establishes an organic basis for the changes in psychological functioning will continue to follow the protocol for mixed medical management. Cases completing a neurological evaluation which rules out an organic basis for symptoms will continue the evaluation process under the criterion. A. Medical Necessity - (must meet All of the following criterion) 1. The patient must have been diagnosed with a psychiatric illness by a licensed mental health professional. 2. Symptoms of this illness must accord with those described in the Diagnostic and Statistical Manual of Mental Disorders, Edition IV (DSM-IV). 3. The diagnosis must be based upon a face-to-face evaluation between the professional and patient. 4. The request for psychological testing must come from a Ph.D. psychologist or psychiatrist who has completed a face to face evaluation of the member. 5. The request for neuropsychological testing must come from a neuropsychologist or psychiatrist who has completed a face to face evaluation of the member. A neurologist may also request neuro-psychological testing. B. Psychological Testing Criteria - (needs to meet criterion 1 and 2, 3, or 4) 1. The results of the testing needs, with reasonable medical certainty, to potentially alter the treatment plan; and 2. Diagnosis and treatment approaches fluctuate, contradictory information is evident and clinical direction requires an increased understanding of the member; or Rev. 12.2013 Page 48 Of 81 3. The member's therapeutic response is significantly different from the anticipated response and additional assessment and investigation has failed to alter the therapeutic dynamics; or 4. Significant disruption in the member's performance of life skills which is not accounted for by assessment, history, diagnosis, or ongoing observation. T. ADVERSE DETERMINATIONAND APPEALS PROCESS When appropriate APS-PR UM criteria is not met for the requested level of care, or during a concurrent review, the physician advisor reviews the potential adverse determination. Attending physicians/providers requesting the services may be contacted by the physician advisor for additional information. If upon reviewing the additional clinical information obtained, the Physician Advisor agrees that the requested level of care does not meet APS-PR UM criteria, a non-certification will be completed. In all cases, the provider is offered an alternative treatment option and provided the clinical rationale for the adverse determination. Notification is provided by phone and in writing to the provider or facility (if appropriate), and the member. The adverse determination notifications include the principle reason(s) for the determination, instructions on how to request an appeal of the determination and the alternative treatment option recommended. In cases where the patient is in active treatment in any intensive level of care, an expedited appeal completed within 72 hours of receiving all clinical information, will be offered. Further details on the appeal process will be given later. U. REPORTING ADVERSE OCCURRANCES Adverse occurrences are defined as suicides, attempted suicides, homicides, attempted homicides, physical or sexual abuse. If a APS-PR member experiences such an occurrence, the provider is to report the incident to APS-PR immediately. APS-PR will supply the provider with a risk management protocol to assist the provider in an intervention. Notification of APS-PR does not substitute for nor take precedence over state or federally mandated reporting requirements for abuse, neglect or danger to self or others. APS HEALTHCARE PUERTO RICO, INC. P.O. Box 71474 San Juan, PR 00936-8574 PHONE: (800) 503-7929 x. 3161 V. ANCILLARY SERVICES APS-PR., HMO Plan customers maintain contracts with laboratory, radiology and other specialty providers. When these services are used in conjunction with an HMO member’s behavioral health care, the APS-PR provider is responsible for coordinating those services with the member’s Primary Care Physician (PCP). Rev. 12.2013 Page 49 Of 81 1. Laboratory Services Each of APS-PR Plan customers maintains contracts with laboratory providers. All lab work must be done through these contracted providers. The provider ordering the lab work will not be billed when using the participating laboratory. Use of any other laboratory service will be the financial responsibility of the physician who orders the test(s). APS-PR providers must use the APS-PR Plan’s contracted laboratory provider for all outpatient lab tests. A listing of the HMO Plan’s contracted laboratory locations can be found in the member’s Provider Directory. This information may also be obtained by calling the local HMO Plan at the number listed on the member’s plan identification card. 2. Radiology For HMO members, all radiology services require a referral from the member’s Primary Care Physician (PCP). Please contact the member’s PCP to coordinate these services. CAT-Scan and MRI procedures also require prior authorization from the member’s PCP. 3. Pharmacy Services HMO members with a prescription rider to their policy (indicated on their identification care with an Rx), can fill prescriptions at any participating pharmacy. A complete listing of participating pharmacies can be found in the member’s Provider Directory. To learn whether a medication is a formulary medication for any individual plan, it is necessary to contact the members HMO plan at the number on the back of the member’s identification card. For questions related to your mental health medications or prescription drugs, members should call the APS-PR’s Pharmacy Department. W. MIXED PSYCHIATRIC/MEDICAL PROTOCOL In order to promote the access and the delivery of quality care for members with both medical-surgical and behavioral health conditions, APS-PR and the HMO customers work together to successfully coordinate members’ care. Except in cases of medical emergency, APS-PR or the HMO Plan contacts their counterpart prior to treatment being rendered to coordinate the approval for the required or requested treatment. Medical necessity, level of care criteria and administrative procedures are determined by the payor responsible for claims adjudication. Pre-certification and concurrent review requirements are determined by the benefit plan design. If questions arise concerning the coordination of a member’s medical-surgical and behavioral health services, APSPR providers may contact APS-PR Care Management. Members utilizing outpatient laboratory, pharmacy and other diagnostic service providers are to be referred to those providers contracted by the HMO Plan. In such circumstances, the APS-PR provider is responsible for coordinating these services with the member’s Primary Care Physician. Rev. 12.2013 Page 50 Of 81 [ IV ] CUSTOMER SERVICE Customer Services Representatives are available Monday through Friday from 7:00 a.m. to 7:00 p.m. E.S.T. The primary function of the Customer Service Representatives is assisting members to interact with APS-PR and participating physicians and providers. Customer Service can be reached at (800) 503-7929 ext. 192710. Specific functions of the Member Relations Department include, but are not limited to: * * * * Verifying Customer Eligibility and Benefits for Specialists, Hospitals, and Ancillary Providers. Resolving Customer Complaints and Appeals.. Explaining APS-PR Policy, Procedures, and Benefits to Customers. Enhancing Customer utilization of health plan services. A. TERMINATED MEMBERS Authorizations from APS-PR are not a guarantee of payment. APS-PR authorizes services based on benefit eligibility information available at the time the authorization decision is granted. If the member’s benefits are terminated between the time an authorization is granted and the date of service, APS-PR will not reimburse the provider for services provided (Unless specifically prohibited by law). In this situation, a provider may bill the member directly for the services delivered at their usual and customary fee. If APS-PR determines that a provider has been paid for services delivered to an ineligible member, APS-PR reserves the right to collect the amount of the overpayment from the provider or to withhold the overpaid amount from future payments. In instances when a members benefits are terminated or benefits end for any reason, providers are expected to work with APS-PR and the member to transition the member to other care that is appropriate. 1. APS-PR is prohibited from retaliating against a Group or any Member, including refusing to renew or canceling coverage under the existing agreement, because Group or Member, or a person acting on behalf of Group or Member, reasonably filed a complaint against APS-PR or appealed a decision of APS-PR relating to the Member, including, but not limited to, a medical necessity determination. APS-PR also is prohibited from retaliating against a Participating Provider for reasonably filing a complaint against APS-PR or appealing a decision of APS-PR for issues pertaining to themselves or on behalf of a Group or Member. B. GRIEVANCE SYSTEM All contracted providers should provide services of optimal quality at all times. APSPR Healthcare registers and responds to verbal and written complaints and grievances received from beneficiaries or its authorized representative. All Rev. 12.2013 Page 51 Of 81 comments are important and are viewed as a potential opportunity for improvement in the care provided by contracted providers. APS-PR has a grievance system in place to address enrollees concerns and appeals of service decisions for all Lines of business. Appeal process for members with Puerto Rico Government Health Insurance The Grievance System includes Complaints, Grievances, Appeals and in some circumstances the Administrative Law Hearing. 1. Definitions: a. Complaint- as expressions of dissatisfaction about any matter other than an Action that are resolved at the point of contact rather than through filing a formal Grievance; b. Grievance- is the procedure for filing an expression of dissatisfaction about any matter other than an Action c. Action- The denial or limited authorization of a requested service, including the type or level of service; the reduction, suspension, or termination of a previously authorized service; the denial, in whole or in part, of payment for a service; the failure to provide services in a timely manner, as defined by this Contract; The failure of the Contractor to act within the timeframes provided in 42 CFR 438.408(b) d. Appeal- is the request for review of an Action. e. Administrative law Hearing- The appeal process administered by the Government of Puerto Rico and as required by federal law, available to Enrollees after they exhaust the Contractor’s Grievance System and Complaint Process. 2. Complaints process (APS-PR) has established a process for receiving and handling complaints which a complainant may have about an aspect of the APS-PR’s operation, such as dissatisfaction with plan administration; appeal of an Adverse Determination; the denial, reduction or termination of a service; the way a service is provided; or disenrollment decisions. APS-PR follows a consistent procedure in responding to complaints including the following: a. A beneficiary or its authorized representative shall file a complaint within 15 calendar after the date of occurrence; b. Filing of a compliant may be orally or in written; c. APS-PR will resolved the compliant in 72 hours or less; Rev. 12.2013 Page 52 Of 81 d. The resolution notice shall include the right to file a grievance or appeal and information on how the member can request for an administrative law hearing. 3. Grievances- a beneficiary or its authorized representative may file a grievance through APS-PR or the Health Advocate Office of Puerto Rico, either orally or in written. A provider may file a grievance on behalf of a beneficiary only when the enrollee has granted written consent to do so. APS-PR follows a consistent procedure in responding to grievances including the following: a. The grievance has to be filed within 60 calendar days after the event. APS-PR may extend this timeframe by up to 14 calendar days; b. The grievance will be responded no later than 30 calendar days from the date it was received. If the grievance involves a minor, the timeframe is 20 days. c. After the investigation is performed, a notice of resolution is issued containing the basis for the resolution. 4. Appeals process- It involves a formal petition by an Enrollee, an Enrollee’s Authorized Representative, or the Enrollee’s Provider, acting on behalf of the Enrollee with the Enrollee’s written consent, to reconsider a decision (an action). There are two kinds of appeal that can be requested: expedited appeals or standard appeals: a. Expedited appeals- shall be resolved in 72 hours since it was requested. The expedited appeal resolution timeframe can be granted to the enrollee based on the information provided or when the provider indicates (when filing the appeal on behalf of the enrollee) that taking the time for standard resolution could seriously jeopardize the enrollee’s health or ability to attain, maintain, or regain maximum function. An expedited appeal may be filed orally and verbally. The 72 hours resolution timeframe may be extended for up to 14 calendar days; b. Standard Appeals- shall be resolved no later than 45 calendar days since it was requested The 45 calendar days resolution timeframe may be extended for up to 14 calendar days. APS-PR follows a consistent procedure in responding to appeals including the following: c. The Enrollee, the Enrollee’s Authorized Representative, or the Provider acting on behalf of the Enrollee with the Enrollee’s written consent, may file an Appeal to the Contractor during a period no less than twenty (20) Calendar Days and not to exceed ninety (90) Calendar Rev. 12.2013 Page 53 Of 81 Days from the date on the APS-PR Notice of Action or Notice of Adverse determination; d. The provider acting on behalf of the Enrollee with the Enrollee’s written consent will be given an opportunity to present evidence and allegations in writing. In those cases in which the appeal is requested by the Provider acting on behalf of the enrollee, the APS-PR Appeals Coordinator shall ensure the provider submits a form of consent completed an sign by the enrollee before proceeding with the appeal. This is regardless it is an expedited or a standard appeal. e. APS-PR shall provide written notice of all appeals resolution. Such notice shall include the following information: i. The right to request an Administrative La Hearing; ii. How to request and Administrative Law Hearing; iii. The right to continue to receive benefits pending the Administrative Law Hearing; iv. How to request the continuation of benefits; and v. Notification that if the APS’s-PR action is upheld in a hearing, the enrollee may be liable for the costs of any continued benefits. 5. Administrative Law Hearing- the ASES may grant an Administrative Law Hearing if the enrollee or the providers acting on behalf the enrollee requests it regardless the APS-PR appeal process has been used. The process applicable to the Administrative law Hearing are govern by the following steps: a. If the enrollee (or the provider acting on behalf of the enrollee with its written consent) file an appeal of an action with APS-PR first, ASES will allow an Administrative Law Hearing not less than 20 calendar days and no later than 90 days from receipt of the APS-PR appeal resolution notice; b. If the enrollee seeks for an Administrative Law Hearing without recourse to the APS-PR appeal process, the ASS will allow it as expeditiously as the enrollee’s health requires it, but no later than 3 calendar days after the ASES receives directly from the enrollee a hearing request on a decision to deny a service, when it is determined by the ASES that taking the time for a standard resolution could seriously jeopardize the enrollee’s life or health or its ability to attain, maintain, or regain maximum function; c. The decision issued by the ASES as a result of the Administrative Law Hearing is subject to appeal before the Court of Appeals of the Commonwealth of Puerto Rico. Rev. 12.2013 Page 54 Of 81 Appeal process for Medicare Advantage and Commercial Behavioral Health Insurance Plan Appeals In the case of Medicare Advantage and Commercial BH Health Plans, APS-PR will adhere to the standards established by the Centers for Medicaid and Medicare Services (CMS) for handling appeals. This means that APS-PR will make timely handle and process appeals based on the standard and expedited timeframes established by CMS. An Appeal is the request for review of an APS-PR adverse determination. It is a formal petition by an Enrollee, an Enrollee’s Authorized Representative. If a provider wishes to appeal a standard pre-service determination, he/she may do so if such appeal is based on a difference of a clinical nature and not for refusing to follow APS-PR processes. Appeals made by the provider on behalf of a beneficiary must be made in writing and must be made after acquiring the beneficiary’s written consent. Additionally, beneficiaries who submit expedited requests or facilities that submit expedited requests on behalf of the beneficiary must send APS-PR a written signed request for appeal. A party may request a standard reconsideration by filing a signed, written request with the APS-PR. A member or the provider acting as the members appointed representative will have a period of sixty (60) days from the date of the notice of the organization determination sent by APS-PR to submit the corresponding appeal. The provider acting on behalf of the Enrollee with the Enrollee’s written consent will be given an opportunity to present evidence and allegations in writing. Upon reconsideration of an adverse organization determination, APS-PR will make its determination as expeditiously as the enrollee’s health condition requires. This must be no later than thirty (30) calendar days from the date APS-PR receives the request for standard reconsiderations (appeals). The time frame will be extended by up to 14 calendar days by APS-PR if the enrollee requests the extension or if APS-PR requires additional information and documents how such delay is in the interest of the enrollee. Hospitals are required to provide APS-PR access to obtain all necessary medical records and other pertinent information within the required time limits to resolve the appeal. APS-PR will mail an acknowledgement letter to the enrollee to confirm the facts and basis of the appeal, and request that the enrollee sign and return the acknowledgement letter. The letter must explain that until the acknowledgement letter is returned, no final decision can be issued; APS-PR will not issue a final decision on the appeal until it receives the signed acknowledgement letter, or other signed document relevant to the appeal request; and If APS-PR does not receive a returned, signed acknowledgement by the conclusion of the appeal timeframe, plus extension, it will forward the case to the independent review entity with a request for dismissal (if applicable). Rev. 12.2013 Page 55 Of 81 An enrollee or any physician may request that APS-PR expedite a reconsideration (appeal) of a determination, in situations where applying the standard procedure could seriously jeopardize the enrollees life, health, or ability to regain maximum function. In light of the short time frame for deciding expedited reconsiderations, a physician does not need to be an authorized representative to request an expedited reconsideration on behalf of the enrollee. A request for payment of a service already provided to an enrollee is not eligible to be reviewed as an expedited reconsideration. If APS-PR denies a request for an expedited reconsideration, it must automatically transfer the request to the standard reconsideration process and then make its determination as expeditiously as the enrollee’s health condition requires, but no later than within 30 calendar days from the date the appeal was received. APS-PR shall provide the enrollee with prompt oral notice of the denial of the request for reconsideration and the enrollee’s rights, and subsequently mail to the enrollee within 3 calendar days of the oral notification, a written letter. If the Medicare health plan approves a request for an expedited reconsideration, then it must complete the expedited reconsideration and give the enrollee (and the physician involved, as appropriate) notice of its reconsideration as expeditiously as the enrollee’s health condition requires, but no later than 72 hours after receiving the request. To properly submit an appeal on behalf of a beneficiary the hospital or facility will be required to contact one of our Appeals Coordinators at (787) 503-7929, Extensions 193035 or 193079. C. RETROSPECTIVE-REVIEW Retrospective reviews are defined as a review conducted after services have been provided to the patient. These reviews are conducted when a patient has received treatment without authorization, or when the pre-certification by a contracted provider or facility was not feasible, the provider is not contract by APS-PR (this happens mostly when the services are furnished out of the services area). The APS-PR Appeals Coordinator facilitates all retrospective reviews. In the case of a patient who has been discharged from inpatient care and no precertification has occurred, an administrative/contractual non-certification determination will be made. A review for medical necessity may occur if the written appeal indicates the provider could not determine if the patient had insurance requiring pre-certification. When the patient remains in treatment, an administrative / contractual non-certification is made for the days prior to the call for authorization and a care manager begins ongoing reviews of the case with the provider for continuing stay criteria. An administrative/contractual non-certification applies to claims generated appeals, calls for pre-certifications outside the contractual limitations and cases where the patient is discharged and the facility decides to call APS-PR for authorization. All care managers can approve services when the APS-PR criteria are met. When there is doubt or question as to whether a patient meets the criteria for the requested level of care, the physician advisor / peer reviewer is Rev. 12.2013 Page 56 Of 81 contacted to review the case and to determine if there will be a non-certification of the requested services. In all non- certification cases, the provider is offered an alternative treatment option and receives instructions regarding the appeals process. If the retrospective review is with regard to outpatient treatment, the patient’s medical record also undergoes a review with a determination. When the pre-certification of the patient was outside the timelines for pre-certification, the case is administratively / contractually denied. The provider may appeal this decision, which requires he/she to submit the complete medical record for review. An initial review of the medical record is completed by the Appeals Coordinator with supervision by a clinician, if necessary; to ensure that there is no medical necessity issues involved that warranted being out of the pre-certification time line. The record is then submitted to administration for a benefits / contract review to again ensure the appropriateness of the administrative / contractual denial. [ V ] CLAIMS DEPARTMENT The claims system is an on-line adjudication system that is fully integrated with all supporting files necessary for validation and extraction of key data elements vital to quick and accurate claims payment. During the on-line adjudication process, the system is able to automatically access the membership, benefits, authorization and provider files in a matter of seconds, requiring manual intervention only if an error situation occurs. In addition, all codes (ICD9, DSM IV TR, CPT and Revenue Codes) are validated against code file tables to maintain the integrity of the data. Further, the adjudication process edits each claim transaction line against the claims transaction file to detect any possible duplicate transactions. Since all processing occurs in a real time on-line environment, accurate, up-to-the-minute information is available continuously. APS-PR also utilizes scanning and an automatic adjudication process to streamline the administrative work associated with claims handling. This technology allows a scanned claim to automatically adjudicate in the same manner as a paper claim. When normal adjudication edits occur, the claim is pended for manual review. A. CLAIMS QUALITY MEASUREMENT PROGRAM Claims Accuracy – Selection Criteria The claims system allows us to select claims to audit for accuracy according to two different sets of criteria: random selection and dollar amount. For each claims examiner, an employee file is maintained in the processing system that allows us to designate the number of claims randomly selected for auditing and a specific payment dollar amount for which all claims with payment amounts at or above that amount will be selected for auditing. The number of claims randomly selected for audit is based on the experience level and performance of the individual examiner. Throughout the department, all claims with payment amounts of $1,500 or more are selected for Rev. 12.2013 Page 57 Of 81 auditing. Claims selected for auditing are held in a suspended status until they are reviewed and released by an Auditor or a Supervisor. 1. Measurement Methods Claims selected for audit are thoroughly reviewed for accuracy. Errors found during the review process are classified according to two categories: payment and non-payment. Payment errors are those errors that would affect the payment of the claims in any way. Non-payment errors are those errors that would not affect the payment of the claims. This data is then used in the following manner to measure claims accuracy: 2. Payment Error Percentage Number of claims that contained payment errors divided by the number of claims sampled. 3. Overall Error Percentage Number of claims that contained both payment and non-payment errors divided by the total number of claims sampled. During the auditing, all errors are captured, categorized and discussed with the Claims Examiner. However, for measuring purposes, each claim that contains multiple errors is counted as either a payment error claim or a non-payment error claim, with payment errors always taking precedence over non-payment errors. Our standards for accuracy are 98% Payment Accuracy and 95% Overall Accuracy. B. REIMBURSEMENT PROCEDURES 1. Collection of Co-payment Members typically have a co-payment or co-insurance obligation for behavioral health care services. The APS-PR Customer Service Representative will inform the provider of the member’s co-payment amount when the referral is made. It is the provider’s responsibility to collect the member’s co-payment at the time of service. The remainder of the provider’s contracted fee will be reimbursed by APS-PR. If a member refuses to remit the co-payment to a provider, the provider is to contact the Customer Service Department at APS-PR. APS-PR will attempt to resolve the situation so that the member may receive services. Members who have questions concerning their financial responsibility in the provision of behavioral health care services should be directed to contact APS-PR’s Customer Service Department. 2. Balance Billing Rev. 12.2013 Page 58 Of 81 Under federal law, HMO members cannot be billed for moneys due from an insurer for covered services. In contracting with APS-PR, a provider agrees that the collection of the member’s co-payment or co-insurance is his/her responsibility and that he will not bill the member in excess of this amount. The only time you may submit a bill to a APS-PR member is if you have obtained prior written acknowledgment from your client/patient that you will be engaging in a treatment plan that is either not covered by the plan or not authorized as medically necessary by APS-PR. 3. Waiver of Co-payment (a) It is APS-PR policy to adhere to our client’s non-waiver of co-payment guidelines. As such, APS-PR will not waive a member’s co-payment or coinsurance responsibility under any circumstances. (b) We subscribe to the trend in the healthcare industry toward the consumer’s awareness of their own health care expenditures by requiring a shared financial responsibility between enrollees and health care payers. This trend is seen in the shift from employers who provide full health insurance coverage to that of employers purchasing benefit packages in which employees are contributing a larger portion of their health care costs. (c) APS-PR providers may independently waive the co-payment or coinsurance responsibility of any member. A decision to waive members financial contribution to the services provided is neither sanctioned nor prohibited by APS-PR. In such a case, APS-PR will reimburse the provider at the contracted rate for the service provided less the co-payment or coinsurance amount. 4. Submission of Claims To ensure timely processing, complete patient and provider information should be submitted with all claims. The HCFA 1500 is to be used for outpatient services and the UB-92 should be used for the submission of all institutional claims. The address of the payor for each member’s benefits will be listed on the identification card. Submit all claims to the appropriate address within ninety (90) days of the date of service or date of discharge. Submit claims to the following address: APS Healthcare Puerto Rico, Inc. Claims Department P.O. Box 71474 San Juan, PR 00936-8574 When submitting claims to APS-PR, it is requested that regular charges are billed. APS-PR will pay for authorized covered services, less the co-payment or coinsurance amount, at the rate listed on the provider’s agreement or billed charges, whichever is lower. Rev. 12.2013 Page 59 Of 81 All HCFA 1500s and UB92s should contain standard required information. To speed the processing of claims, please follow the guidelines listed below: All Claims • Member name and ID Number as they appear on the member’s ID card. • CPTIV Code or Revenue Code that corresponds to the services included in your provider contract. • The APS-PR authorization number should be listed in box 23 of the HCFA 1500 and box 63 of the UB92. • Complete information concerning other insurance • The Tax Identification Number of the group, facility, or individual that holds the contact with APS-PR and has been authorized to render the services being billed. Providers contracted with APS-PR as a member of a group practice must bill with the Tax Identification Number of the group practice and not their individual social security number. 5. HCFA 1500 Instructions: HCFA 1500s are sent through a Scanning Process using Optical Character Recognition. This process can allow us to significantly reduce processing time if the claims documents are completed according to the following guidelines. • Red and White forms only • Typewritten data with dark print • Data must be correctly printed within the boxes (Data that is not aligned correctly, or when multiple data elements appear in a box designed for one, the claim cannot be scanned.) • The provider address must appear correctly in box 33. • Rendering provider name must appear correctly in box 31. A signature may also appear in this box. • Cannot be marked with any rubber stamps or contain any handwritten information outside of boxes, 12, 13, (patient/member signatures) and 31 (rendering provider signature.) 6. Coordination of Benefits Coordination of benefits (COB) guidelines are used by APS-PR to arrange payment when an individual is covered under more than one group health policy. The first determination of the primary insurer is based on the employee relationship. The policy held by a person through their employer for that person. for claims insurance employeris primary When dependent children of married parents are covered under more than one policy, APS-PR follows the guidelines of the National Association of Insurance Carriers (NAIC), which recommend using the “birthday rule” to determine primary coverage. This rule states that the policy of the parent whose birthday falls first in the calendar year, using Rev. 12.2013 Page 60 Of 81 month and day only, is primary for the children. When both parents have the same birthday, the primary insurance carrier is determined by the policy effective date. When dependent children of divorced or separated parents are covered under more than one group health policy, the following order is used to determine the sequence in which benefits are paid: 1) 2) 3) 4) the policy of the parent with custody of the children; the policy of the spouse of the parent with custody of the children; the policy of the non-custodial parent; the policy of the spouse of the non-custodial parent. If it is determined that APS-PR is the responsible party as a secondary payor, an authorization for services is still required in order for APS-PR to reimburse the provider for services rendered. Medicare covers medical expenses as the primary carrier for retired persons over age sixty-five (65), disabled individuals and persons with End-State Renal Disease (ESRD). Medicare is typically the primary carrier for Medicare beneficiaries over age 65. However, there are situations, working aged beneficiaries and certain ESRD patients, when the typical rules do not apply. Please contact APS-PR customer service if you need assistance in determining if Medicare is the primary or secondary carrier. When Medicare is the primary carrier, APS-PR will reimburse providers for any applicable deductible and coinsurance. Once the deductible is met, Medicare Part A covers inpatient hospital services, home health services and institutional services. Medicare Part B covers eighty percent (80%) of the allowed amount for physicians services and other outpatient services. All other State and Federal laws governing COB are followed even if not explicitly stated here. 7. Claims Payment Appeals Should a provider disagree with the manner in which a claim was paid or the reason for a denial of payment, the provider may appeal to APS-PR. When submitting an appeal, all pertinent information and a written request is to be sent to APS-PR at the following address: APS Healthcare Puerto Rico, Inc. P.O. Box 71474 San Juan, PR 00936-8574 Phone: (800) 503-7929 ext. 3015 Appeals are to be filed within ninety (90) days of the date the claim was originally processed. A response will be sent to the provider within thirty (30) days of receipt of all information necessary to review the appeal. . Rev. 12.2013 Page 61 Of 81 8. Missed Appointments/No-Shows A member may not be charged for canceled appointments if the member has provided at least twenty-four (24) hours notice of cancellation. The office policy of the provider on canceling appointments should be communicated to members at the commencement of treatment. A provider may only collect a co-payment from a member who cancels an appointment without twenty-four (24) hours notice or who fails to give any notice at all (no-show). Missed appointments and no-shows do not count against APS-PR member’s maximum benefit allowance and APS-PR assumes no liability for the collection of such charges. The collection of charges from members who have benefit plans that are not managed by APS-PR is determined by the payor. The payor’s telephone number, listed on the member’s identification card should be called to determine reimbursement in these cases. NOTE: This does not apply to MiSalud members may not be charged for canceled appointments. C. MEMBER HOLD HARMLESS PROVISION 1. Charges to APS-PR Members Providers and Physicians agree to collect applicable co-payments, if any, from Members at the time services are provided by the Provider or Physician. The Provider and Physician shall look only to APS-PR for compensation for Necessary Covered Services. In addition, Provider and Physician shall under no circumstances, including the termination of the existing Agreement or the insolvency of APS-PR or breech of the existing Agreement, assert any claim for compensation against Members or persons acting on their behalf for Covered Services in excess of applicable co-payments. Providers and Physicians agree to provide continuation of services until discharge of any Members confined in an inpatient facility on the date of insolvency or other cessation of operations or through the premium-paid period for which member has made prepayment, or on whose behalf prepayment has been made. Provider and Physician further agree that this provision shall survive the termination of the existing Provider Agreement regardless of the cause giving rise for termination and shall be construed to be for the benefit of the APS-PR Member/enrollee, and that this provision supersedes any oral or written contrary agreement now existing or hereafter entered into between Provider and/or Physician and Member, enrollee, or persons acting on their behalf. 2. Explanation of Benefits (EOB) With every APS-PR check, an Explanation of Benefits (EOB) report is issued. An example of the Explanation of Benefits is included as an attachment to this manual. Rev. 12.2013 Page 62 Of 81 [ VI ] QUALITY IMPROVEMENT PROGRAM I. Purpose and Goals This document describes the scope, structure and function of APS-PR behavioral health quality improvement program. The purpose of the quality improvement program is to provide the operational structure and processes necessary to achieve the goals and objectives established by the APS-PR Board of Directors and other quality oversight committee. II. Structure of the Quality Improvement Program A. Authority and Responsibility The APS-PR Board of Directors are the ultimate authority and accountability for the quality of care and service delivered to health plan division enrollees, and is the highest level of oversight for the quality improvement program. The APS-PR Boards of Directors delegate their oversight responsibilities to the APS-PR Corporate Quality Improvement Committee (CQIC). The APS-PR CQIC delegates operational responsibility for the HPD quality improvement program to the Health Plan Quality Improvement Committee (HPQIC). B. Designated Behavioral Health Care Practitioner The implementation of the HPD’s quality improvement process is under the direction of the Corporate Medical Director, Quality Improvement. The Corporate Medical Director, Quality Improvement delegates day to day implementation of the health plan division’s QI program to the Corporate Director, Behavioral Health Quality Improvement. He or she is responsible for: • • • • • The oversight of the implementation of the QI Work plan. Supporting the QI committee structure in conducting its activities. Tracking identified opportunities for improvement. Facilitating and supporting all areas in data collection and analysis, as well as in designing interventions. Providing leadership and training in completing external regulatory and accreditation reviews. The Corporate Director of Behavioral Health Quality Improvement is a licensed, behavioral health practitioner. C. Input from Medical Delivery Systems The APS-PR HPD includes input and representation from medical delivery systems in a number of ways. These include: Rev. 12.2013 Page 63 Of 81 • • • • Participation in Managed Care Organization (MCO) partners QI Committee activity. Regular QI workgroups with MCO and APS-PR QI staff. Joint development and implementation of prevention and clinical improvement programs. Annual oversight audits by MCO partners. During these audits MCOs make recommendations and develop action plans as appropriate with APS-PR. This input from MCOs is documented in appropriate committee minutes and focuses on both clinical and service improvement activities. APS-PR Board of Directors The APS-PR Healthcare Board of Directors is APS-PR governing body and provides oversight and direction to the QI Program. At least five of the Directors are nonemployees of APS-PR. The APS-PR Board of Directors’ membership is composed of: • • • • Chief Executive Officer, APS-PR Chief Financial Officer, APS-PR APS-PR Legal Counsel Directors from External Organizations (5) The APS-PR Board of Directors meets on a quarterly basis, maintains minutes of its meetings and annually reviews and approves the health plan division’s QI Program Description. The APS-PR Board of Directors has delegated oversight responsibility of the HPD QI Program to the APS-PR Corporate Quality Improvement Committee. However, the APS-PR Board of Directors retains the final responsibility for the health plan division’s operations and performance. 1. APS-PR Corporate Quality Improvement Committee Reports to: APS-PR Board of Directors and CNR Health Partners Board of Directors Reporting Process: Annual submission of Health Plan Division Behavioral Health QI Program Description Meeting Frequency: At least quarterly. Membership: • Vice President, Corporate Quality Improvement (Chair) • President, Behavioral Health • Vice President, Clinical Services • President, Health Plan Division • President, Employee Assistance Programs • President, Employer Division • Medical Director, Health Plan Division • Corporate Medical Director, Quality Improvement • Vice President, Medical Services • APS Legal Counsel Rev. 12.2013 Page 64 Of 81 • • • • • • • • • • • • Chief Information Officer Corporate Director, Behavioral Health Quality Improvement Corporate Director, Credentialing Executive Vice President, Sales and Marketing Chief Executive Officer, APS-PR Vice President, Operations - APS Northwest Vice President, Public Sector Operations Vice President, Behavioral Health Services - APS Wisconsin Executive and Medical Director - APS Hawaii Chief Information Officer Vice President, Marketing Chief Financial Officer Roles and Functions of Committee: The functions of this committee include the following: • Annually review and approve the QI Program Descriptions from each APS-PR division. • Annually review and approve the QI Work Plans and the annual evaluation of the QI Programs from each APS-PR division. • Oversee all quality improvement activities of subcommittees. • Monitor allocation of resources needed to achieve APS-PR quality improvement goals. • Annually review and approve the Utilization Management Program documents and Utilization Management Review Criteria from each APS-PR division. • Provide final approval of clinical guidelines. At least 50% of the voting members are required for a quorum. A simple majority of voting members present is required for approvals. 2. APS Policy and Procedure Committee Reports to: APS Corporate Quality Improvement Committee Reporting Process: Submission of written, approved minutes by the committee chair. Verbal presentations of subcommittee recommendations, reports, and policy activities. Verbal presentations and written reports as required. Meeting Frequency: At least four times per year Membership: • Vice President, Corporate Quality Improvement (Chair) • Manager, Quality Improvement - Health Plan Division • Manager, Quality Improvement - APS Hawaii • Manager, Quality Improvement - APS Medical Services • Director, Quality Improvement - APS Puerto Rico • Coordinator, Quality Improvement - APS Wisconsin • Medical Director - APS Northwest • APS Legal Counsel Rev. 12.2013 Page 65 Of 81 Roles and Functions of Committee: The functions of this committee include the following: • To develop and approve processes for the development and adoption of policies and procedures throughout APS-PR. • To review and approve corporate-wide policy and procedures. • To ensure the annual review and revision, when needed, of APS-PR policies and procedures. • To develop and maintain an organized system of tracking and storing policies and procedures. • To ensure that staff receive training on policies relevant to their job duties. 4. APS Chief Privacy Officer The APS Privacy Officer has the primary responsibility for ensuring that the enterprise’s privacy policies and procedures are accurate and, as appropriate, are integrated into the operations of the Business Units. Roles and Responsibilities of the APS Chief Privacy Officer The APS Chief Privacy Officer has the following responsibilities: • Creating and developing privacy policies and procedures. • Arranging for responses to all employee questions concerning privacy issues that may or may not be readily answered from this policy. • Directly or through designees, receiving, documenting, and taking action in response to any complaints made by customers, employees or any other individuals regarding APS’s privacy practices and procedures. • Developing training programs and materials that educate employees on the policies and procedures for safeguarding the privacy of PHI. • Maintaining the accuracy of the enterprise’s privacy policies. This includes reviewing federal and state laws and regulations and changing the APS-PR policies and procedures as necessary and appropriate to comply with changes in the law. • Maintaining the accuracy of the Notice of Privacy Practices as set forth in the APSPR Notice Policy. If a privacy practice that is described in the Notice of Privacy Practices changes, the Privacy Officer must direct and oversee a change in the Notice of Privacy Practices. • Developing and approving mechanisms to oversee the application of privacy policies. • Identifying opportunities for reducing collection of unnecessary enrollee data or deidentifying data as close to its source as possible. • Approving levels of authorized use and access to data across the delivery system. • Reviewing and approving/denying both internal and external requests to use enrollee data. • Facilitating an appeals process to address enrollee concerns regarding confidentiality of data. • Overseeing mechanisms for adhering to specific requests to limit access to data. • Approving research projects that involve the release of enrollee data. Rev. 12.2013 Page 66 Of 81 5. ASP PR Quality Improvement Committee Reports to: APS Corporate Quality Improvement Committee Reporting Process: Submission of written, approved meeting minutes on a quarterly basis. Submission of a QI program, work plan and evaluation on annual basis. Verbal presentations and written reports as required. Meeting Frequency: At least quarterly Membership: • Medical Director (Chair) • Director Quality Improvement • President and Chief Executive Officer • Chief Clinical Officer • Clinics Director • Appeals Coordinator (Non-voting staff) • Client Services Specialist (Non-voting staff) • Pharmacy Director • Providers Director • Senior Member Referral (Non-voting staff) • UM Manager Roles and Responsibilities of APS-PR QIC • Annually review and approve the APS-PR Behavioral Health QI Program Description. • Annually review and approve the evaluation the effectiveness of the PR implementation of its QI program and the QI Work Plan. • Annually review and approve the APS-PR Behavioral Health Utilization Management Program documents and adopt the APS-PR Behavioral Health Utilization Management Review Criteria. • Oversee all quality improvement activities of committee subcommittees as specified in the PR Quality Improvement Work Plan. • Monitor the findings of the clinical and service performance measures and implement corrective actions for improvement. • Oversee continuity and coordination of care activities. • Recommend decisions on content of APS-PR policies and procedures. • Review results of satisfaction surveys and other performance studies. Identify and prioritize opportunities for improvement. Develop action plans or QI activities based on study results. • Ensure adequate resources and training are in place to support the QI program. • Ensure compliance with state, federal and external accrediting bodies. • Provide final review and oversight of delegated activities. • Identify potential clinical measurement activities that are relevant to the health plan division’s enrollees. • Develop clinical monitors and data collection specifications. Rev. 12.2013 Page 67 Of 81 • • • • • • • • • • • Review and analyze data related to clinical quality measurement activities, including clinical studies, clinical practice guidelines and preventive behavioral health programs. Identify opportunities for improvement. Develop and oversee the implementation of interventions related to clinical quality improvement activities. Provide input and recommendations to the HP QIC related to clinical quality improvement activities. Identify potential service measurement activities that are relevant to the health plan division’s enrollees and practitioners/providers. Develop data collection strategies and tools to evaluate enrollee and practitioner/provider satisfaction. Review and analyze data from satisfaction surveys, complaints and appeals. Review and analyze data related to availability and accessibility monitoring activities. Identify opportunities for improvement. Develop and oversee the implementation of interventions related to service quality improvement activities. Provide input and recommendations to the PR Quality Improvement Committee related to service quality improvement activities. At least 50% of the voting members are required for a quorum. A simple majority of voting members present is required for approvals. 6. Utilization Management Committee Reports to: PR Quality Improvement Committee Reporting Process: Submission of written, approved minutes by the committee chair. Verbal presentations of subcommittee recommendations, reports, and service activities. Verbal presentations and written reports as required. Meeting Frequency: At least quarterly Membership: • Medical Director, Chair • Chief Executive Officer • Chief Clinical Officer • Clinical Services Director/Clinics • QI Director • UM Manager • Member Referral Supervisor • Pharmacy Department Director Roles and Functions of Committee: The functions of this committee include the following: • Annually, review and revise the APS-PR Behavioral Health Utilization Management Program and Behavioral Health Utilization Management Review Criteria • Develop the annual UM Work Plan and UM Evaluation for PR Division. Rev. 12.2013 Page 68 Of 81 • • • Provide input and make recommendations on utilization management policies and procedures. Identify opportunities to improve utilization management processes and support implementation of improvement activities. Regularly review and monitor data related to key utilization management indicators. At least 50% of the voting members are required for a quorum. A simple majority of voting members present is required for approvals. 7. Provider Advisory Group The Provider Advisory Group (PAG) provides for structured input from external practitioners to be utilized in the development and implementation of the behavioral health QI program and activities for the APS-PR. The APS-PR PAG members are drawn from a variety of APS-PR’ networks where APS-PR has health plan business. Practitioners participate via teleconference. Reports to: The PR Quality Improvement Committee Reporting Process: Submission of written meeting minutes on a quarterly basis. Verbal presentations and written reports as requested. Meeting Frequency: At least quarterly Membership: Practitioners/providers represent medical delivery systems and behavioral health specialties from the following: • Medical Director (Chair) • Provider’s Director • Quality Improvement Director • Psychiatrist • Psychologist • Social Worker • Substance Abuse Provider Roles and Functions of Committee: The functions of this panel include the following: • Support the development of appropriate clinical practice guidelines and guideline monitoring. • Review and make recommendations regarding requests for new technology. • Review APS-PR policies and procedures and make recommendations as they relate to the practitioner community. • Provide input in the development and review of APS-PR utilization management criteria. • Provide clinical input into the development of appropriate preventive health and other quality improvement programs. • Provides input on continuity and coordination of behavioral healthcare. • Evaluate and provide feedback on the results of provider satisfaction survey activities. • Assist in developing provider education and communication processes and tools. • Serve as consultants to APS-PR representing practitioner viewpoints and concerns. Rev. 12.2013 Page 69 Of 81 8. Member Advisory Panel APS-PR has a Member Advisory Panel (MAP) that provides input and feedback on quality and service activities to both operations centers’ quality committees. The MAP consists of enrollees from a variety of sites where APS-PR manages behavioral health accounts. APS-PR quality improvement staff facilitates the meetings. As needed, APSPR can procure additional feedback from the panel members related to specific clinical and service issues through focused mailings. Reports to: PR Quality Improvement Committee. Reporting Process: Submission of written minutes for each meeting, to include documentation of Member Panel feedback/focused input. Meeting Frequency: At least twice a year. Other feedback procured by structured and focused mailings on an as needed basis. Membership: The membership for the MAP includes behavioral health enrollees chosen from various APS-PR sites where health plan business is managed. Roles and Functions of Committee: The functions of this panel include the following: • Provide consumer input into the QI process. • Assist in identifying key quality indicators affecting consumers. • Review and make recommendations around preventive behavioral health programs. • Review and make recommendations regarding routine correspondence directed to members for clarity, readability and utility. • Provide comments on the results of consumer satisfaction surveys and outcome studies. • Review and make recommendations regarding APS-PR policies and procedures as they relate to consumers. • Serve as consultants to APS-PR representing member viewpoints and concerns. 9. Credentialing Committee Reports to: APS-PR Quality Improvement Committee Reporting Process: Submission of written minutes approved by the committee chair. Verbal and written presentation of recommendations for credentialing and recredentialing decisions for network participation to the HP QIC. Meeting Frequency: At least monthly Membership: • Medical Director (Chair) • Network Practitioner: Psychiatrist • Network Practitioner: Psychologist • Network Practitioner: Child and Adolescent Practitioner • Network Practitioner: Social Worker/Other Masters-level • Network Practitioner: Substance Abuse Counselor • Network Practitioner: Inpatient Practitioner Rev. 12.2013 Page 70 Of 81 • • • Corporate Director, Credentialing (non-voting member) Credentialing Supervisor (non-voting staff) Provider Director (non-voting staff) Roles and Functions of Committee: The functions of this committee include the following: • Oversee and conduct the credentialing and recredentialing of practitioners and providers, and conduct peer review and approval of credentialing status to network practitioners and providers. • Credential provider entities, such as inpatient facilities. • Make recommendations on content of credentialing policies and procedures for practitioners and providers. • Review quality of care issues related to individual practitioners or providers and make recommendations as appropriate. • Review and approve oversight activities related to delegated credentialing arrangements. 10. Practitioner Appeals Committee Reports to: APS-PR Quality Improvement Committee Reporting Process: Submission of written minutes approved by the committee chair. Verbal and written presentation of recommendations related to appeal outcome. Meeting Frequency: As needed basis Membership: • Medical Director, (Chair, non-voting member) • At least 3 clinical professionals who are not in direct economic competition with the practitioner under review. For review of physician practitioners all members will be licensed physicians. For review of non-physician practitioners at least one member will be a physician and at least one member will be in the discipline of the practitioner under review. • Chief Clinical Officer (non-voting staff) • Provider Director (non-voting staff) • Credentialing Supervisor (non-voting staff) • APS-PR Legal Counsel (non-voting staff) • Quality Improvement Director (non-voting staff) Roles and Functions of Committee: The functions of this committee include the following: • Complete review of all materials relevant to practitioner appeals related to APS-PR’ modification or termination of network participation. • Determine appeal outcome to overturn, overturn with conditions or uphold prior Credentialing Committee decision on practitioners network participation. III. Program Scope and Content Rev. 12.2013 Page 71 Of 81 The scope of the quality improvement program encompasses the assessment, monitoring and improvement of all aspects of care and service received by enrollees, including the following: • care delivered in inpatient, outpatient and alternative settings at all acuity levels; • all types of behavioral health care services delivered by all types of practitioners and providers; and • services delivered by APS-PR and its contractors. The APS-PR implements an annual Quality Improvement Work Plan (see Attachment 1). This work plan details the specific activities, objectives and performance standards encompassed by the current Quality Improvement Program Description. The Quality Improvement Work Plan includes the specific objectives of the quality improvement activity, including performance goals or standards, the persons accountable for coordinating and ensuring the activity is completed, the critical action steps to complete the activity and the target date for completion of the activity. An overview of these activities is presented below. A. Quality Management Methods and Monitors APS-PR’ quality improvement methods include a four-stage process for identifying and improving the quality of clinical care and service rendered by APS-PR and APS-PR practitioners: • Identification of monitors of important aspects of care and service • Identification of opportunities for improvement as a result of monitoring clinical care and service • Implementation of interventions addressing the identified opportunities for improvement, and • Remeasurement to determine if the interventions were effective in improving clinical cares and service. B. Clinical Quality Improvement Activities 1. Clinical Studies a. Improving Follow-up after Behavioral Health Hospitalization Description: Annual measure of the % of members hospitalized for behavioral health diagnoses that receive 5, 7 and 30 day follow-up after discharge. Objective: To improve performance to the rates indicated below: • Commercial 5 day – 50% • Commercial 7 day - 65% • Commercial 30 day-70% • Medicaid 5 day - 60% • Medicaid 7 day – 70% • Medicaid 30 day- 85% • Medicare 5 day – 45% • Medicare 7 day –50% Rev. 12.2013 Page 72 Of 81 • Medicare 30 day-65% b. Improving Appropriate Antidepressant Medication Management Description: Annual measurement of the following: • % of enrollees with depression on antidepressant medication that had at least 3 follow-up contacts Objective: To establish a baseline rate for the monitor above and identify an opportunity for improvement as appropriate: Description: Annual measurement of the following: • % of enrollees with depression on antidepressant medication that remained on the medication for 12 weeks. Objective: To measure the rates indicated below: Description: Annual measurement of the following: % of enrollees with depression on antidepressant medication that remained on the medication for 6 months • Objective: To measure the rates indicated below: c. Evaluating the Availability of Psychotherapy and/or Medication Management for Patients with Schizophrenia Description: Annual measurement of the % of patients (Medicaid) with Schizophrenia who were seen by a psychiatrist for medication management or psychotherapy at least 4 times during the 12 months prior to their last date of service in the measurement period. Objective: To establish a baseline rate for the monitor above and identify an opportunity for improvement as appropriate. 2. Clinical Practice Guideline Monitoring and Improvement a. The Treatment of Major Depression in Adults Description: Annual monitoring of the following elements across all products: • % of patients where the major depression diagnosis met the DSM-IV-TR criteria for the disorder. • % of patients with mild or moderate major depression, in treatment with a nonprescribing practitioner, referred for medication evaluation if no improvement after 6 sessions or 3 months. • % of patient with severe major depression, in treatment with a non-prescribing practitioner, referred for medication evaluation after 3 or less sessions. • % of patients with major depression with psychotic features that were treated with one of the following: antidepressant plus an antipsychotic medication or ECT. • % of patients with major depression and an Axis II diagnosis of a personality disorder that are receiving psychotherapy. Rev. 12.2013 Page 73 Of 81 Objective: To establish baseline rates for the monitors above and identify any opportunities for improvement as appropriate. b. The Treatment of Bipolar Disorder Description: Annual monitoring of the following elements across all products: • % of patients diagnosed with bipolar disorder that continue to have psychiatric management 6 months after initial session or discharge from an inpatient episode. • % of patients diagnosed with bipolar disorder that are in psychotherapy for at least 6 months after the initial session. Objective: • To establish baseline rates for the monitors above and identify opportunities for improvement as appropriate. 3. Preventive Behavioral Health Programs a. Attention Deficit Hyperactivity Disorder in Children: Parenting Skills Training Description: Program for parents of children 12 years of age and younger diagnosed with ADHD. The program goals are to: • Prevent or minimize stress related symptoms in parents developed as a consequence of parenting a difficult child. • Prevent additional psychiatric co-morbidity resulting from dysfunctional parentchild interactions due to ADHD symptoms. • Reduce the disability associated with ADHD in children. Objective: To improve the following aspects of the program: • To increase parent program participation. • Improve the effectiveness of the program by providing emerging, detailed ADHD information on an ongoing basis to all parents of children currently in treatment for ADHD. b. Education and Treatment Compliance for Adults with Depression Description: Program for adults diagnosed with depression. The program goals are to: • Reduce the length of the symptomatic period through compliance with treatment. • Reduce the prevalence of major depressive disorder in the population. Objective: To improve the following aspects of the program: • To establish program to offer education and treatment compliance for adults with depression. • Improve the effectiveness of the program by providing information/materials about medication topics. • Evaluate possible methods of expanding the program to reach out to enrollees not in treatment with screening, referral and educational activities. • Add access questions to surveys sent to all APS-PR program participants to complete further analysis on timing of program initiation. 4. Assessment of Continuity and Coordination of Care Rev. 12.2013 Page 74 Of 81 Two types of continuity and coordination of care are monitored: between behavioral health practitioners and providers, and between behavioral health practitioners and general medical care a. Assessing the Exchange of Information Across all Levels of Behavioral Health Care and between Behavioral Healthcare Practitioners and Provider Types Description: Assessment of whether behavioral health practitioners and/or providers forward relevant information to each other. • Annual clinical treatment record review (elements 34 and 35) • Annual provider coordination of care chart audits (elements 1-5) • Annual assessment of clinical guidelines • Treatment of Depression in Adults (monitor #6) • Annual assessment of providers’ policies and procedures regarding exchange of information Objective: To improve the performance on the following monitors: • Improvement in practitioners attempting to obtain consent to communicate with other behavioral health practitioners (Measures #1) to 80%. • Improvement in providers attempting to communicate and communicating with other behavioral health practitioners to (Measure #4-60%, Measure #5-80%, and Measure #6-60%, Measure #7-60%) b. Assessing Appropriate and Timely Access to Behavioral Health Practitioners Description: Assessments related to access to and follow-up with practitioners. • Annual studies to assess access and follow-up with practitioners • Ambulatory Follow-up of Patients Discharged from the Inpatient Level of Care with a Behavioral Health Diagnosis • Antidepressant Medication Management • Quarterly appointment access monitoring • Annual assessment of clinical guidelines • Treatment of Depression in Adults (monitor #15) • Annual review, revision and training on policies relating to appropriate referrals for medication management Objective: To improve the performance on the following monitors: • Improving the ambulatory follow up of patients discharged from inpatient care (Measure #9) to 75% within 30 days. • Improving the attendance to follow-up appointments and medication compliance for patients on antidepressant medication as determined with each MCO partner. (Measure #11, #12, and #13) c. Assessing the Exchange of Information Between Behavioral Health Care Practitioners, Providers and Primary Care Physicians (PCPs) and other Medical Providers Description: Assessment of whether behavioral health practitioners forward relevant information to PCPs using the following data sources: • Annual provider coordination of care chart audits Rev. 12.2013 Page 75 Of 81 Annual clinical treatment record review (elements 36 and 37) Annual assessment of clinical guidelines • Treatment of Depression in Adults (monitor #5) • Annual practitioner satisfaction survey (question # 22) • Annual enrollee satisfaction survey (question # XX) Objective: To improve the performance on the following monitors: • #2-% of provider charts with evidence consent was obtained to communication with PCP or other medical practitioners/providers to 50% • #3-% of provider charts with evidence of communication with PCP or other medical practitioners/.providers to 50% • #4-% of provider charts where communication with PCP or other medical practitioner/providers took place within 7 days of discharge to 50%. • #5-% of clinical treatment records with evidence the BH practitioner obtained consent to communicate with the PCP or other medical practitioner/ provider to 80%. • • d. Management of Treatment Access and Follow-up for Co-Existing Medical and Behavioral Health Disorders Description: APS-PR implements the following activities to ensure coordination of care for members with co-existing health problems: • Collaboration with MCO care managers for enrollees with co-existing medical disorders • Provision of psychiatric consults to patients in inpatient medical beds. • Assessment of provider policies and procedures regarding exchange of information. Objective: To collect data on measures related to this aspect of care coordination. e. Implementation of a Primary or Secondary Preventive Behavioral Health Program with Medical Delivery Systems Description: APS-PR implements the following preventive health programs with its MCO partners • Attention Deficit Hyperactivity Disorder in Children: Parenting Skills Training • Education and Treatment Compliance for Adults with Depression Objective: To improve the performance on the following monitors: • #46-To increase the % of MCOs participating in the ADHD program to 20%. 5. Treatment Record Documentation a. Monitoring of Treatment Records for Compliance Description: Bi-annual monitoring of treatment records for all high volume practitioners. Objective: To improve compliance with the following record keeping standards: • #8-Consent for treatment forms signed to 80%. • #15-Assessment of severity and imminence of potential harm to self or others is completed and documented at least once and then as often as appropriate to 80%. Rev. 12.2013 Page 76 Of 81 • • • • • • #25-Mental status exam is completed that includes assessment and documentation of the patient’s affect, speech, mood, thought content, judgement, insight, attention or concentration, memory or impulse control to 80%. #31-Informed consent for medication is documented and the patient’s understanding of the treatment plan is documented (prescribing practitioners only) to 80%. #34-Treatment record provides evidence of practitioner attempting to obtain consent to communicate with other behavioral health providers or practitioners to 80%. #36-Treatment record provides evidence of practitioner attempting to obtain consent to communicate with primary care physician (PCP) or other ancillary providers when appropriate to 80%. #39-For children and adolescents, prenatal and perinatal events are documented to 80%. #40-For children and adolescents, complete developmental history is documented to 80%. 6. Improving Patient Safety a. Supporting Patient Safety through Monitoring of Clinical Record-keeping Practices Description: Bi-annual monitoring of clinical record keeping practices that support patient safety. The following documentation elements are monitored: • Medication allergies or adverse reactions (or lack of) are clearly noted • The medical record is legible • Assessment of severity and imminence of potential harm to self or others is completed and tracked. • Relevant medical conditions are listed, prominently identified and revised. Objective: To increase the % of records with documentation of • Medication allergies and adverse reactions to 80% • Assessment of severity and imminence of potential harm to self or other to 80%. b. Identifying and Investigating Individual Quality of Care Issues and Adverse Incidents Impacting Patient Safety Description: Identify, investigate, resolve and track individual quality of care issues and adverse incidents that impact patient safety. Objective: To continue to identify, investigate and resolve individual quality of care issues within processing standards. c. Ensuring Patient Education on Medication Side Effects Description: Annual enrollee satisfaction survey which measures the % of enrollees reporting that in the last 12 months, they were told of side effects of medications to watch for. Objective: To continue to monitor the % of enrollees that report being informed about medication side effects. Rev. 12.2013 Page 77 Of 81 d. Enrollee Education about Patient Safety Issues Description: Research, development and distribution of educational articles regarding patient safety issues in APS-PR enrollee newsletters or other direct enrollee mailings. Objective: To distribute at least 2 educational articles related to medication safety to enrollees. C. Service Quality Improvement Activities 1. Availability and Accessibility a. Monitoring the Availability of Behavioral Health Practitioners and Providers Description: Completion of the following activities: • Measurement of performance against cultural availability needs of the membership. • Annual measurement of performance against numeric and geographic standards for the availability of practitioners and providers. b. Providing Enrollees with Appropriate Access to Care Description: Annual assessment of member access to non-life threatening emergency care, urgent care and routine care. 2. Satisfaction Surveys a. Enrollee Satisfaction Survey (Medicaid) Description: APS-PR conducts an annual enrollee satisfaction survey, using the ECHO tool, measuring overall satisfaction with APS-PR and satisfaction with: • Services • Utilization Management Processes • Accessibility and availability • Treatment quality • Patient safety issues • Continuity and coordination of care • Cultural availability and accessibility Objective: To improve performance of the following satisfaction measurements: • Increase to 85% the satisfaction rate with the APS-PR referral process. • Increase to 50% the % of enrollees reporting they received information on self help or support groups. • Increase to 85% the % of enrollees reporting they were given information about their rights as a patient. b. Practitioner Satisfaction Survey (Medicaid, Commercial and Medicare) Description: APS-PR conducts an annual practitioner satisfaction survey measuring overall satisfaction with APS-PR and satisfaction with: • Utilization Management Processes • Customer Services • Network • Provider Relations Services Rev. 12.2013 Page 78 Of 81 PCP communication Objective: To improve performance of the following satisfaction measurements: • • • • • Improve to 85% satisfaction with the ease of referring to a psychiatrist for an evaluation. Improve to 85% satisfaction with the timeliness and accuracy of claims payment. Improve to 85% satisfaction with the number of sessions authorized. Improve to 85% satisfaction with the time it takes APS-PR to notify practitioners of their network status. C. Routine Monitors On at least a quarterly basis data are compiled and reviewed by the APS PR Quality Improvement Committee for the following routine monitors: • • • • • • • • Utilization management statistics Credentialing performance indicators Member and practitioner complaints processing Appeals processing Care management quality assurance audits Customer service representative quality assurance audits Telephone performance for member services and practitioner/provider services Claims processing IV. Resources Dedicated to Quality Improvement 1. Human Resources Dedicated to Quality Improvement Quality improvement is an ongoing and integrative process at APS-PR. APS-PR provides quality improvement support and involvement at the corporate and health plan division levels. This structure promotes an efficient use of resources and sharing of ideas and data. Tables V.1.a, V.1.b and V.1.c illustrate resources APS-PR dedicates to quality improvement activities. Table IV.1.a: Quality Improvement Resources-Health Plan Division APS-PR Position Medical Director Quality Improvement Director President and Chief Executive Officer Chief Clinical Officer QI Supervisor Data Analyst Rev. 12.2013 Page 79 Of 81 FTE Equivalent .5 1.0 .25 .25 1.0 2.0 APS-PR Position Client Services Specialist TOTAL FTE Equivalent 2.0 4 Table IV.1.b: APS-PR Corporate Quality Improvement Resources APS-PR Position FTE Equivalent IS Staff .25 Compliance Officer .25 APS-PR Legal Counsel .25 TOTAL .75 2. Data and Information Systems Supporting Quality Improvement APS-PR requires access to a wide range of data to carry out its quality improvement activities. APS-PR also must manage the required data to support measurement and evaluation of its quality improvement activities. Table V.2.a shows the data and information systems that support quality improvement activities at APS-PR. Table IV.2.a: Data and Information Systems Supporting Quality Improvement System/Database Data Source/Function Paradigm Utilization and Case Management System, Claims Payment, Eligibility, Network Information, Customer Service Logs. Complaints Data Base Complaint tracking and reporting. Non-Cert/Appeals Logs Denial and appeal tracking and reporting. Quality of Care Issues Tracks and reports individual quality of care issues Geo-Access Software Reports on geographic availability of practitioners and providers V. Confidentiality APS-PR Healthcare and its subsidiaries and affiliates are committed to ensuring that privacy practices regarding individually identifiable health information comply with industry best practices, covenants given to its clients (“ Covered Entities and Business Associates”) and, as applicable, all federal and state laws and regulations including but not limited to the Standards for Privacy of Individually Identifiable Health Information promulgated pursuant to the Health Insurance Portability and Accountability Act (“HIPAA”) (“the HIPAA Privacy Rule” or “the Privacy Rule”). Consequently, APS-PR is committed to maintaining an administrative structure, reporting procedures, due diligence procedures, training programs and other methodologies of an effective compliance program relative to the use and disclosure of its customers’ protected health information (“PHI”). The APS Chief Privacy Officer is responsible for development and implementation of APS-PR’s confidentiality policies and procedures. Rev. 12.2013 Page 80 Of 81 VI. Evaluation and Update An evaluation of the effectiveness of the APS-PR Behavioral Health QI Program is prepared annually. Key components include: • • • • Summary of quality assessment activities Summary of quality improvement activities, projects and focus studies Evaluation of the overall effectiveness of the quality improvement program Progress toward improving safe clinical practices throughout the network The evaluation is reviewed and approved by the APS-PR QIC. The evaluation is forwarded to the APS Corporate Quality Improvement Committee (CQIC) for review and final approval. The APS-PR Behavioral Health Quality Improvement Program Description is reviewed and updated annually. The updated APS-PR Behavioral Health Quality Improvement Program Description is approved by the APS-PR QIC. Following approval by the APSPR QIC, the program description is forwarded to the APS CQIC for review and final approval. Required reviews and approvals are reflected in the minutes of each of the appropriate committees. Rev. 12.2013 Page 81 Of 81
© Copyright 2026