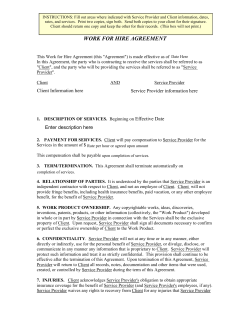
First+Plus Provider Manual 2014
First+Plus Provider Manual 2014 INTRODUCTION CONTACT INFORMATION FIRST+PLUS PROVIDERS RECRUITMENT MAP ENROLLMENT AND ELIGIBILITY FIRST+PLUS PRODUCT DESCRIPTION BENEFIT CHARTS EMERGENCY AND URGENT CARE ADDITIONAL BENEFITS PROVIDER ROLES AND RESPONSIBILITIES PAGE 3 PAGE 5 PAGE 6 PAGE 8 PAGE 11 PAGE 21 PAGE 23 PAGE 24 COMPLIANCE WITH THE CONTRACT, REGULATIONS AND THIS MANUAL GENERAL MEDICARE AND FEDERAL REGULATIONS CONTRACT REQUIREMENTS CODE OF CONDUCT CONFLICT OF INTEREST POLICY PROVIDER AND MEMBER COMMUNICATIONS MEDICAL RECORDS RESPONSABILITIES OF ALL PROVIDERS THE ROLE OF THE PRIMARY CARE PRACTITITIONER (PCP) ROLE AND RESPONSABILITIES OF THE SPECIALISTS PANEL CLOSURE REOPENING OF PANEL SANCTIONS UNDER FEDERAL HEALTH PROGRAMS AND STATE LAW APPOINTMENT STANDARDS CONTRACTING PROVIDER GRIEVANCES PROCESS CREDENTIALING PAGE 32 PAGE 35 NETWORK ADEQUACY PRIMARY SOURCE VERIFICATION REQUIREMENTS PROVIDER ORIENTATION RE-CREDENTIALING TERMINATION DUTY TO REPORT CERTAIN TERMINATION MEMBER NOTIFICATION PAGE 39 GRIEVANCES AND APPEALS GRIEVANCE PROCESS MEMBER RIGHTS APPEALS PROCESS APPEAL RECORDS PAGE 41 MEDICAL AFFAIRS UTILIZATION MANAGEMENT AUTHORIZATION PROCESS PRIOR AUTHORIZATIONS AUTHORIZATION REQUIREMENTS ADMISSION REVIEW QUALITY IMPROVEMENT SPECIAL NEEDS PLAN QUALITY IMPROVEMENT PROGRAM Provider Manual 2014 PAGE 55 1 ANNUAL MEDICAL ASSESMENT FORM (AMAF) PAGE 79 BILLING AND CLAIMS PAGE 87 DEFINITION CMS 1500 FORM AND REQUIERED FILE UB-04 FORM AND REQUIERED FILE ADA FORM AND REQUIERED FILE TIMELY CLAIMS SUBMISION LIST EOB CODE DESCRIPTION ELECTRONIC BILLING FRAUD, WASTE & ABUSE ADDITIONAL INFORMATION Provider Manual 2014 PAGE 315 PAGE 319 PAGE 327 2 INTRODUCTION Welcome to First Plus, First Medicals’ Medicare Advantage plan. As a member of the First+Plus Provider Network you are an important member of our service delivery team, and we thank you for joining us as we pursue our commitment to improve the health and wellbeing of our Members. The purpose of the Provider Manual is to serve as a resource and reference guide for our providers. You may use it as a guide to answer questions concerning: eligibility verification, identification cards, re-credentialing process, medical management and quality improvement programs; as well as billing and claim procedures. This manual may be shared with your office manager and office personnel. This manual is not intended to replace your written provider agreement currently in place with First+Plus. You will receive updates periodically from the First+Plus Provider Services Department. If you should have any questions regarding any of the material contained in this provider manual, please do not hesitate to contact the First+Plus Provider Services Department at 1-866-505-5885. The provider manual is available on line at www.firstpluspr.com First+Plus Overview First+Plus Medicare Advantage offers the comprehensive coverage and healthcare choices Medicare beneficiaries deserve. One important benefit of a PPO (Preferred Provider Organization) plan is that Medicare beneficiaries can receive services from out-of-network providers for an additional out-of –pocket cost. Of course, the members maximize their First+Plus benefits by using in-network plan providers. • Network Provider – “Provider” is the general term we use for doctors, other health care professionals, hospitals, and other health care facilities that are licensed or certified by Medicare and by the State to provide health care services. We call them “network providers” when they have an agreement with our plan to accept our payment as payment in full, and in some cases to coordinate as well as provide covered services to members of our plan. Our plan pays network providers based on the agreements it has with the providers or if the providers agree to provide you with plan-covered services. Network providers may also be referred to as “plan providers.” • Preferred Provider is the provider a member selected when he/she enrolled in First+Plus. In most cases a Preferred Provider is a general practitioner, internal medicine or family doctor. However, because preferred provider organization (PPO), o A member may select a physician in another specialty, i.e. Cardiology, Oncology, Oby -Gyn. This provider should be knowledgeable about the members Medical Provider Manual 2014 3 History, and should available to assist the member in coordinating the health services the member needs. • Covered services is the general term we use to mean all of the health care services and supplies that are covered by First+Plus. • Non-plan providers are providers with which we have not arranged to coordinate or provide covered services to members of our plan. Out-of-network providers are providers that are not employed, owned, or operated by our plan or are not under contract to deliver covered services. A member with PPO coverage may Use non-plan providers to get covered services. However, out-of-pocket costs may be higher than if the member used plan providers. • Specialist is a doctor who provides health care services for a specific disease or part of the body. Examples include oncologists (who care for patients with cancer), or cardiologists (who care for patients with heart conditions). A member may get care from specialists without a referral from another doctor. If the member uses our plan specialists, the costs for covered services will be lower than if they used non-plan providers. • Primary Care Physician (PCP) (First Care Plus, First+Plus Complete and First+Plus Platino) Primary Care Physician is virtually any physician in the First+Plus network, including specialists, who meets state requirements and is trained to give basic medical care. A PCP will manage member’s health care and provide prevention care and treatment to common medical conditions. They will help monitor, arrange and coordinate health care covered services. Our Plan Objectives are to: • • • • • Improve the healthcare of our Members Increase quality and continuity of care to our Members Decrease inappropriate usage of health care resources, e.g. emergency room visits for non-emergency situations Achieve and maintain cost-effectiveness and efficiency Promote Provider and Member satisfaction Provider Manual 2014 4 CONTACT INFORMATION If you have any questions or concerns, please call or write to First+Plus Provider Services Department. We will be happy to help you. Our business hours are Monday thru Friday from 8:00am to 5:00pm. Provider Services Provider and Credential Services Phone Number: 1-866-505-5885 Fax Provider Department: (787) 300-3908 Fax Credentialing: (787) 300-3907 Providers Services Address: PO BOX 195080 San Juan, PR 00919 Medical Affairs Pre-authorization Fax Number: (787) 705-9347 / (787) 622-0729 Patient Admissions (Uticorp): (787) 765-3303 Customer Services Member Services Phone Number 1-888-767-7717 For Pre-authorization status and Case Management Notifications please contact Customer Service Department TTY 1-877-672-4242 * Fax Number: (787) 300-3906 *This number requires special telephone equipment. Calls to this number are free. Claims Department Claims Department Address: PO Box 19559 San Juan, PR 00919-5559 Main Office Location Extension Villa Caparra #530 Marginal Buchanan, Guaynabo, PR 00966 Provider Manual 2014 5 FIRST+PLUS PROVIDER RECRUITMENT MAP Provider Manual 2014 6 You may contact the First+Plus Provider Services department for questions regarding: • • • • • • • Changes in provider information, including group or clinic name, address, telephone number, Medicare number or Federal Tax ID number. Your effective date and date anticipated for accepting new members. Contract administration issues. Credentialing and re-credentialing issues. Reimbursement issues, fee schedules, coding questions. Specific information concerning First+Plus policies and procedures. Training for billing and claim submission. The Provider Services staff at First+Plus is responsible for: • • • • • • • • Developing and maintaining a comprehensive provider network. Monitoring provider adherence to the availability and accessibility standards. Assisting providers with any problems or concerns that they may have in providing Members with services. Providing clarification of Insurance Commission office of Puerto Rico, and Centers for Medicaid and Medicare Services policies, regulations, and procedures. Assisting providers with the complaint/grievances and appeals processes. Conducting provider orientation sessions, in-service and specialized training. Distributing provider satisfaction surveys and reporting the results to the appropriate committees. Generating and distributing the Provider Newsletter and/or other provider communications. Provider Manual 2014 7 ENROLLMENT AND ELIGIBILITY For a Medicare Eligible beneficiary to enroll in the First+Plus plan, the prospective Member must: • • • • Be enrolled in both Medicare Parts A and B Reside within the service area Not have end stage renal disease Additional requirements apply to Platino and Gobierno First+Plus Product. For more information, please contact the Customer Service Department at 1-888-767-7717 Monday through Friday from 8:00 AM to 8:00 PM Verifying Eligibility Procedure: If you need to verify eligibility for a First+Plus Member, you may do so by contacting Member Services or by visiting our website at www.firstpluspr.com. Customer Services Representatives are available Monday through Friday from 8:00 AM to 8:00 PM at 1-888-767-7717. You may call the Member Services Department for provider questions including, but not limited to: • Member Eligibility • Benefits and coverage questions • Claim denial • New member contract status The Centers for Medicare and Medicaid (CMS) The Centers for Medicare and Medicaid Services (CMS) is the federal agency that administers the Medicare program. The CMS contracts with, and regulates, Medicare Health Plans (including First Medical) and Medicare Private Fee-for-Service organizations. Here are three ways to get information directly from Medicare: • Call 1-800-MEDICARE (1-800-633-4227), 24 hours a day, 7 days a week. TTY users should call 1-877-486-2048. • Visit the Medicare website (http://www.medicare.gov). • Read Medicare & You 2013 Handbook. Every year in the fall, this booklet is mailed to people with Medicare. It has a summary of Medicare benefits, rights and protections, and answers to the most frequently asked questions about Medicare. You can get it at the Medicare website (http://www.medicare.gov) or by calling 1-800-MEDICARE (1-800633-4227), 24 hours a day, 7 days a week. TTY users should call 1-877-486-2048. Provider Manual 2014 8 Sample ID Card: Enrollees must use their First+Plus ID card to be eligible for benefits through the First+Plus Health Plan network. Each First+Plus Member is issued a Member identification card to present to all health care providers when seeking health care services. The member will also receive a letter that will have the Member’s name, Member identification number or “ID number”, the Preferred Provider name and telephone number. This card identifies the Member as a First+Plus Member. Members should not show you their red, white and blue card for Original Medicare. If a member uses his/her red, white and blue Medicare card instead of his/her First+Plus ID, even though he/she is a member of First+Plus, the Medicare program will not pay for these services and neither will First+Plus. The member will have to pay the full cost for services. Please Note: • The I.D. card does not guarantee eligibility. It is for identification purposes only. • Eligibility must be verified prior to each visit at www.firstpluspr.com. Failure to verify eligibility may result in non-payment of claims. • If the Member does not have an identification card, you must call Customer Service to determine eligibility. • Members may have a copy of their certification form of enrollment as interim proof of Membership until a card is issued and mailed. The Description of the Subscriber card (shown on page 26) will identify the member as being part of First+ Plus and will contain important information. Provider Manual 2014 9 DESCRIPTION OF THE FIRST+PLUS 2014 MEMBER’S CARDS Provider Manual 2014 10 FIRST+PLUS PRODUCT DESCRIPTION Benefit Charts First+Plus Advantage Service Area: Entire Island Delivery System Service Área Out-pf Pocket Maximum Monthly Part B Premium buydown Inpatient Services Inpatient Hospital Care Inpatient Psych/Alcohol and Drug Abuse Skill Nursing Home Health Outpatient Services PCP Visit Specialist Visits OP MH/SA OPD Surgery Ambulance (Ground $ Air Transportation) Emergency Room (worldwide) Urgent Care (worldwide) Outpatient Rehabilitation Services: Physical, Occupational and Speech Therapy DME Prosthetic / Orthotics Diabetes Monitoring X-rays / Radiology Radiology- (Diag. & Ther.) Laboratory Part B Drugs covered under Original Medicare Preventive/Screening Services Bone Mass Measurement Colorectal Screening Immunizations: Pneumonia Vaccine, Flu, Shot, Hepatitis B, Anti-Rabies Vaccine Mammography Screen Pap Test Pelvic Exam Prostate Cancer Screening Exams (for men over age 50) Additional Physical Exams (1 per year) Routine Vision Exams Lens / Contacts Routine Hearing Exam Hearing Aids Medicare Covered Chiropractic Routine Chiropractic Routine Podiatry Routine Dental (Exam & Cleaning 2 per year and X-ray 1 per year) Comprehensive Dental Coverage (1) PPO Entire Island $6,700/$10,000 $10 In- Network Coverage $0 / $50 per admit $0 / $50 per admit CIF, 100 days lifetime limit CIF In- Network Coverage $4 co pay $12 co pay $12 co pay $0/$30 co pay $15 co pay $60 co pay CIF $20 co pay Out of Network coverage 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share 20% cost share 20% cost share Same as in-network Same as in-network with 20% cost share 10% / 20% cost share 10% / 20% cost share 0% / 20% cost share 10% cost share 10% cost share CIF 15% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share In- Network Coverage CIF CIF CIF Out of Network coverage Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share CIF CIF CIF CIF Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share In-Network Coverage CIF $100.00 (per years) CIF (once annually) $300 (every three years) CIF $12 co pay (two per year) $12 co pay (two per year) CIF Out of Network Coverage Same as in-network with 20% cost share Same as in-network with 20% visual examination cost and 50% visual equipment cost 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Not Covered Not Covered Legend: CIF-Covered in Full First Plus Advantage 2014 Provider Manual 2014 Out of Network Coverage 11 First+Plus Advantage Plus Service Área: Entire Island Delivery System Service Área Out-of-Pocket Maximum Monthly Part B Premium buydown Inpatient Services Inpatient Hospital Care Inpatient Psych/Alcohol and Drug Abuse Skill Nursing Home Health Outpatient Services PCP Visit Specialist Visits OP MH/SA OPD Surgery Ambulance (Ground $ Air Transportation) Emergency Room (worldwide) Urgent Care (worldwide) Outpatient Rehabilitation Services: Physical, Occupational and Speech Therapy DME Prosthetic / Orthotics Diabetes Monitoring Radiology- (Diag. & Ther.) X-rays / Radiology Laboratory Part B Drugs covered under Original Medicare Preventive/Screening Services Bone Mass Measurement Colorectal Screening Immunizations: Pneumonia Vaccine, Flu, Shot, Hepatitis B, Anti-Rabies Vaccine Mammography Screen Pap Test Pelvic Exam Prostate Cancer Screening Exams (for men over age 50) Additional Physical Exams (1 per year) Routine Vision Exams Lens / Contacts Routine Hearing Exam (1 per year) Hearing Aids (every three years) Medicare Covered Chiropractic Routine Chiropractic Routine Podiatry Routine Dental (Exam & Cleaning 2 per year and X-ray 1 per year) Comprehensive Dental Coverage Part D Plan Type Cost Sharing up to ICL Gap Coverage PPO Entire Island $6,700/$10,000 $0 In- Network Coverage $0 / $50 per admit $0 / $50 per admit CIF, 100 days lifetime limit CIF In- Network Coverage $4 co pay $12 co pay $12 co pay $0/$30 co pay $15 co pay $60 co pay CIF $25 co pay Out of Network coverage 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share 20% cost share 20% cost share Same as in-network Same as in-network with 20% cost share 10% / 20% cost share 10% / 20% cost share CIF $10 co pay 15% cost share CIF 15% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share In- Network Coverage CIF CIF CIF Out of Network coverage Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share CIF CIF CIF CIF Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share In-Network Coverage CIF $100.00 (per years) Out of Network Coverage Same as in-network with 20% cost share Same as in-network with 20% visual examination cost and 50% visual equipment cost 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share CIF $300 CIF $12 co pay (two per year) $12 co pay (two per year) CIF Not covered In-Network Coverage Enhanced $6/$12/$35/$55/25% $6/$12 Generic Only Legend: CIF-Covered in Full First Plus Advantage Plus 2014 Provider Manual 2014 Out of Network Coverage 12 Not covered Out of Network Coverage Same as in-network First+Plus Gobierno Plus Service Area: Entire Island Delivery System Service Área Proposed Monthly Premium Monthly Part B Premium buydown Inpatient Services Inpatient Hospital Care Inpatient Psych/Alcohol and Drug Abuse Skill Nursing Home Health Outpatient Services PCP Visit Specialist Visits OPD Surgery Ambulance (Ground $ Air Transportation) Emergency Room (worldwide) Urgent Care (worldwide) Outpatient Rehabilitation Services: Physical, Occupational and Speech Therapy OP MH/SA DME Prosthetic / Orthotics Diabetes Monitoring Radiology-(Diag, & Ther.) X-rays / Radiology Laboratory Part B Drugs covered under Original Medicare Preventive/Screening Services Bone Mass Measurement Colorectal Screening Immunizations: Pneumonia Vaccine, Flu, Shot, Hepatitis B, Anti-Rabies Vaccine Mammography Screen Pap Test Pelvic Exam Prostate Cancer Screening Exams (for men over age 50) Additional Physical Exams (1 per year) Routine Vision Exams Lens / Contacts Routine Hearing Exam (1 per year) Hearing Aids (every three years) Routine Chiropractic Routine Podiatry Routine Dental (Exam & Cleaning 2 per year and X-ray 1 per year) Comprehensive Dental Coverage Part D Plan Type Cost Sharing up to ICL Gap Coverage Copayments Above Catastrophic Limit Plan Type PPO Entire Island $0 $0 In- Network Coverage $0/$50 unlimited CIF, 190 days lifetime limit CIF, 100 days lifetime limit CIF In- Network Coverage $4 co pay $12 co pay $0/$30 co pay $15 co pay $45 co pay CIF $25 co pay Out of Network coverage 20% cost share Same as in-network with 20% cost share 20% cost share 20% cost share Same as in-network Same as in-network with 20% cost share $12 co pay 10%/20% cost share 10%/20% cost share 0%/20% cost share 15% co pay $10 co pay CIF 15% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share In- Network Coverage CIF CIF CIF Out of Network coverage Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share CIF CIF CIF CIF Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share In-Network Coverage CIF $100.00 (per years) Out of Network Coverage Same as in-network with 20% cost share Same as in-network with 20% visual examination cost and 50% visual equipment cost 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share CIF $300 $12 co pay (two per year) $12 co pay (two per year) CIF Not Covered In-Network Coverage Enhanced $4/$8/$30/$60/25% $4/$8 Generic Only Max of $2.55/$6.35 or 5% Enhanced Legend: CIF-Covered in Full First First Plus Gobierno Plus 2014 Provider Manual 2014 Out of Network Coverage 13 Not Covered Out of Network Coverage Same as in-network Same as in-network First+Plus Gobierno Premium Service Area: Entire Island Delivery System Service Área Proposed Monthly Premium Monthly Part B Premium buydown Inpatient Services Inpatient Hospital Care Inpatient Psych/Alcohol and Drug Abuse Skill Nursing Home Health Outpatient Services PCP Visit Specialist Visits OPD Surgery Ambulance (Ground $ Air Transportation) Emergency Room (worldwide) Urgent Care (worldwide) Outpatient Rehabilitation Services: Physical, Occupational and Speech Therapy OP MH/SA DME Prosthetic / Orthotics Diabetes Monitoring Radiology-(Diag & Ther.) X-rays / Radiology Laboratory Part B Drugs covered under Original Medicare Preventive/Screening Services Bone Mass Measurement Colorectal Screening Immunizations: Pneumonia Vaccine, Flu, Shot, Hepatitis B, Anti-Rabies Vaccine Mammography Screen Pap Test Pelvic Exam Prostate Cancer Screening Exams (for men over age 50) Additional Physical Exams (1 per year) Routine Vision Exams Lens / Contacts Routine Hearing Exam (1 per year) Hearing Aids (every three years) Routine Chiropractic Routine Podiatry Routine Dental (Exam & Cleaning 2 per year and X-ray 1 per year) Comprehensive Dental Coverage Part D Plan Type Cost Sharing up to ICL Gap Coverage Copayments Above Catastrophic Limit Plan Type PPO Entire Island $100 $25 In- Network Coverage CIF, unlimited CIF, 190 days lifetime limit CIF, 100 days lifetime limit CIF In- Network Coverage $0 $5 CIF CIF $50 co pay CIF $10 co pay Out of Network coverage 20% cost share Same as in-network with 20% cost share 20% cost share 20% cost share Same as in-network Same as in-network with 20% cost share $5 co pay 10%/20% cost share 10%/20% cost share 0%/20% cost share 10% CIF CIF 10% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share In- Network Coverage CIF CIF CIF Out of Network coverage Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share CIF CIF CIF CIF Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share In-Network Coverage CIF $100.00 (per years) Out of Network Coverage Same as in-network with 20% cost share Same as in-network with 20% visual examination cost and 50% visual equipment cost 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share CIF $400 CIF (4 per year) CIF (4 per year) CIF $1,000..00 (every years) In-Network Coverage Enhanced $3/$6/$20/$30/25% $3 /$6 Generic Only Max of $2.55/$6.35 or 5% Enhanced Legend: CIF-Covered in Full First Plus Gobierno Premium 2014 Provider Manual 2014 Out of Network Coverage 14 Same as in-network with 20% cost share Out of Network Coverage Same as in-network Same as in-network First+Plus Gobierno Premium II Service Area: Entire Island Delivery System Service Área Proposed Monthly Premium Monthly Part B Premium buydown Inpatient Services Inpatient Hospital Care Inpatient Psych/Alcohol and Drug Abuse Skill Nursing Home Health Outpatient Services PCP Visit Specialist Visits OPD Surgery Ambulance Emergency Room (worldwide) Urgent Care (worldwide) Outpatient Rehabilitation Services: Physical, Occupational and Speech Therapy OP MH/SA DME Prosthetic / Orthotics Diabetes Monitoring Radiology-(Diag, & Ther.) X-rays / Radiology Laboratory Part B Drugs covered under Original Medicare Preventive/Screening Services Bone Mass Measurement Colorectal Screening Immunizations: Pneumonia Vaccine, Flu, Shot, Hepatitis B, Anti-Rabies Vaccine Mammography Screen Pap Test Pelvic Exam Prostate Cancer Screening Exams (for men over age 50) Additional Physical Exams (1 per year) Routine Vision Exams Lens / Contacts Routine Hearing Exam (1 per year) Hearing Aids (every three years) Routine Chiropractic Routine Podiatry Routine Dental (Exam & Cleaning 2 per year and X-ray 1 per year) Comprehensive Dental Coverage Part D Plan Type Cost Sharing up to ICL Gap Coverage Copayments Above Catastrophic Limit Plan Type PPO Entire Island $100 $0 In- Network Coverage CIF, unlimited CIF, 190 days lifetime limit CIF, 100 days lifetime limit CIF In- Network Coverage CIF $5 co pay CIF CIF $45 co pay CIF $5 co pay Out of Network coverage 20% cost share Same as in-network with 20% cost share 20% cost share 20% cost share Same as in-network Same as in-network with 20% cost share $5 co pay 10%/20% cost share 10%/20% cost share 0%/20% cost share 10% cost share CIF CIF 5% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share In- Network Coverage CIF CIF CIF Out of Network coverage Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share CIF CIF CIF CIF Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share In-Network Coverage CIF $100.00 (per years) Out of Network Coverage Same as in-network with 20% cost share Same as in-network with 20% visual examination cost and 50% visual equipment cost 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share Same as in-network with 20% cost share CIF $400 CIF (4 per year) CIF (6 per year) CIF $1,000.00 (every years) In-Network Coverage Enhanced $0/$3/$15/$25/25% $0/$3 Generic Only $2.55/$2.55/$6.35 or 5% Enhanced Legend: CIF-Covered in Full Gobierno Premium II 2014 Provider Manual 2014 Out of Network Coverage 15 Same as in-network with 20% cost share Out of Network Coverage Same as in-network Same as in-network First+Plus First Care+Plus (HMO) Service Área: Entire Island Delivery System Service Área Out-of-Pocket Maximun Monthly Part B Premium buydown Inpatient Services Inpatient Hospital Care Inpatient Psych/Alcohol and Drug Abuse Skill Nursing Home Health Outpatient Services PCP Visit Specialist Visits OP MH/SA OPD Surgery Ambulance (Ground $ Air Transportation) Emergency Room (worldwide) Urgent Care (worldwide) Outpatient Rehabilitation Services: Physical, Occupational and Speech Therapy OP MH/SA DME Prosthetic / Orthotics Diabetes Monitoring Radiology (Diag. & Ther.) X-rays / Radiology Laboratory Part B Drugs covered under Original Medicare Preventive/Screening Services Bone Mass Measurement Colorectal Screening Immunizations: Pneumonia Vaccine, Flu, Shot, Hepatitis B, Anti-Rabies Vaccine Mammography Screen Pap Test Pelvic Exam Prostate Cancer Screening Exams (for men over age 50) Additional Physical Exams (1 per year) Routine Vision Exams Lens / Contacts Routine Hearing Exam (1 per year) Hearing Aids (every three years) Routine Chiropractic Routine Podiatry Routine Dental (Exam & Cleaning 2 per year and X-ray 1 per year) OTC Drugs/Diabetic Supplies Comprehensive Dental Coverage Part D Plan Type Cost Sharing up to ICL Gap Coverage Plan Type Legend: CIF-Covered in Full First Plus First Care+Plus 201 Provider Manual 2014 16 HMO Entire Island $6,700 $0 In- Network Coverage $0 / $50 per admit $0 / $50 per admit CIF, 100 days lifetime limit CIF In- Network Coverage CIF $6 co pay $6 co pay $0 / $30 co pay CIF $50 co pay CIF $15 co pay CIF 10% / 20% cost share 10% / 20% cost share 0% / 20% cost share 15% cost share CIF CIF 10% cost share In- Network Coverage CIF CIF CIF CIF CIF CIF CIF In-Network Coverage CIF $100.00 (per years) CIF $300 $6 co pay (4 per year) $6 co pay (4 per year) CIF $20.00 (per quarter) $450.00 (per year) In-Network Coverage Enhanced $5/$10/$25/$50/25% $5 / $10 Generic Only Enhanced First+Plus Complete (SNP) HMO Service Area: Entire Island Delivery System Service Área Outh-of-Pocket Maximum Monthly Part B Premium buydown Inpatient Services Inpatient Hospital Care Inpatient Psych/Alcohol and Drug Abuse Skill Nursing Home Health Outpatient Services PCP Visit Specialist Visits OP MH/SA OPD Surgery Ambulance (Ground $ Air Transportation) Emergency Room (worldwide) Urgent Care (worldwide) Outpatient Rehabilitation Services: Physical, Occupational and Speech Therapy DME Prosthetic / Orthotics Diabetes Monitoring Radiology-(Diag. & Ther.) X-rays / Radiology Laboratory Part B Drugs covered under Original Medicare Preventive/Screening Services Bone Mass Measurement Colorectal Screening Immunizations: Pneumonia Vaccine, Flu, Shot, Hepatitis B, Anti-Rabies Vaccine Mammography Screen Pap Test Pelvic Exam Prostate Cancer Screening Exams (for men over age 50) Additional Physical Exams (1 per year) Routine Vision Exams Lens / Contacts Routine Hearing Exam Hearing Aids Routine Chiropractic Routine Podiatry Routine Dental (Exam & Cleaning 2 per year and X-ray 1 per year) Comprehensive Dental Coverage OTC Drugs/Diabetic Supplies Nutritionist Part D Plan Type Cost Sharing up to ICL Gap Coverage Plan Type HMO Entire Island $6,700 $0 In- Network Coverage $0/$50 per admit CIF, 190 days lifetime limit CIF, 100 days lifetime limit CIF In- Network Coverage CIF $10 co pay $10 co pay $0/$30 $40 co pay $55 co pay CIF $20 co pay 10%/20% cost share 10%/20% cost share 0%/20% cost share 15% cost share $15 co pay CIF 15% cost share In- Network Coverage CIF CIF CIF CIF CIF CIF CIF In-Network Coverage CIF $100.00 (per years) CIF (once annually) $300 (every three years) $10 co pay (1 per year) CIF (8 per year) CIF $300.00 (every years) $15.00 (per quarter) CIF (4 per years) In-Network Coverage Enhanced $6/$12/$30/$50/25% $6/$12 Generic Only Enhanced Leyend: CIF-Covered in Full First Plus First Complete (SNP) 2014 Provider Manual 2014 17 First+Plus Platino (HMO) Service Área: Entire Island Delivery System Service Área Proposed Monthly Premium Monthly Part B Premium reimbursement Inpatient Services Inpatient Hospital Care Inpatient Psych/Alcohol and Drug Abuse Skill Nursing Home Health Outpatient Services PCP Visit Specialist Visits OPD Surgery Ambulance (Ground $ Air Transportation) Emergency Room (worldwide) Urgent Care (worldwide) OP MH/SA Outpatient Rehabilitation Services: Physical, Occupational and Speech Therapy DME Prosthetic / Orthotics Diabetes Monitoring Radiology CT/MRI/PET X-rays / Radiology Laboratory Part B Drugs covered under Original Medicare Preventive/Screening Services Bone Mass Measurement Colorectal Screening Immunizations: Pneumonia Vaccine, Flu, Shot, Hepatitis B, Anti-Rabies Vaccine Mammography Screen Pap Test Pelvic Exam Prostate Cancer Screening Exams (for men over age 50) Additional Physical Exams (1 per year) Routine Vision Exams Lens / Contacts Routine Hearing Exam Hearing Aids Routine Chiropractic Routine Podiatry Routine Dental (Exam & Cleaning 2 per year and X-ray 1 per year) Comprehensive Dental Coverage OTC Drugs/Diabetic Supplies Nutritionist Part D Plan Type Deductible Cost Sharing up to ICL HMO Entire Island $6,700 $10 In- Network Coverage CIF CIF, 190 days lifetime limit CIF, 100 days lifetime limit CIF In- Network Coverage CIF CIF CIF CIF CIF CIF CIF CIF CIF CIF CIF CIF CIF CIF CIF In- Network Coverage CIF CIF CIF CIF CIF CIF CIF In-Network Coverage CIF $100.00 (per years) CIF (once annually) $300 (every three years) CIF (2 per year) CIF $400.00 (per year) $400.00 (per year) $20.00 (2 per quarter) CIF (2 per year) Enhanced $0/$3 $0/$3 Generic Only Enhanced Legend: CIF-Covered in Full First Plus Platino 2014 Provider Manual 2014 18 First+Plus Smart Value (HMO) Service Area: Entire Island Delivery System Service Área Out-of-Pocket Maximum Monthly Part B Premium buydown Inpatient Services Inpatient Hospital Care (unlimited) Inpatient Psych/Alcohol and Drug Abuse (190 days lifetime limit) Skill Nursing (100 days per benefit period) Home Health Outpatient Services PCP Visit Specialist Visits OPD Surgery Ambulance Emergency Room (worldwide) Urgent Care (worldwide) OP MH/SA Outpatient Rehabilitation Services: Physical, Occupational and Speech Therapy DME Prosthetic / Orthotics Diabetes Monitoring Radiology (Diag. &Ther.) X-rays / Radiology Laboratory Part B Drugs covered under Original Medicare Preventive/Screening Services Bone Mass Measurement Colorectal Screening Immunizations: Pneumonia Vaccine, Flu, Shot, Hepatitis B, Anti-Rabies Vaccine Mammography Screen Pap Test Pelvic Exam Prostate Cancer Screening Exams (for men over age 50) Additional Physical Exams (1 per year) Routine Vision Exams Lens / Contacts Routine Hearing Exam Hearing Aids Routine Chiropractic Routine Podiatry Routine Dental (Exam & Cleaning 2 per year and X-ray 1 per year) Comprehensive Dental Coverage Part D Plan Type Cost Sharing up to ICL Gap Coverage Plan Type Legend: CIF-Covered in Full Smart Value 2014 Provider Manual 2014 19 HMO Entire Island $6,700 $70 In- Network Coverage $250/$475 per admit $250/$475 per admit $40/days 21-100 CIF In- Network Coverage 20% cost share 20% cost share 25% cost share 20% cost share $65 co pay 20% cost share 20% cost share 25% cost share 20% cost share 20% cost share 20% cost share 20% cost share 20% cost share 20% cost share 20% cost share In- Network Coverage CIF CIF CIF CIF CIF CIF CIF In-Network Coverage CIF $100.00 (per years) CIF (once annually) $300 (every three years) 20% (1 per year) 20% (1 per year) Not Covered Not Covered In-Network Coverage Enhanced $7/$15/$40/$65/25% $7/$15 Generic only Enhanced First+Plus Smart Premium (HMO) Service Área: Entire Island Delivery System Service Área Proposed Monthly Premium Monthly Part B Premium reimbursement Inpatient Services Inpatient Hospital Care (unlimited) Inpatient Psych/Alcohol and Drug Abuse (190 days lifetime limit) Skill Nursing (100 days per benefit period) Home Health Outpatient Services PCP Visit Specialist Visits OPD Surgery Ambulance Emergency Room (worldwide) Urgent Care (worldwide) OP MH/SA Outpatient Rehabilitation Services: Physical, Occupational and Speech Therapy DME Prosthetic / Orthotics Diabetes Monitoring Radiology (Diag &Ther.) X-rays / Radiology Laboratory Part B Drugs covered under Original Medicare Preventive/Screening Services Bone Mass Measurement Colorectal Screening Immunizations: Pneumonia Vaccine, Flu, Shot, Hepatitis B, Anti-Rabies Vaccine Mammography Screen Pap Test Pelvic Exam Prostate Cancer Screening Exams (for men over age 50) Additional Physical Exams (1 per year) Routine Vision Exams Lens / Contacts Routine Hearing Exam Hearing Aids Routine Chiropractic (one per year) Routine Podiatry (one per year) Routine Dental (Exam & Cleaning 2 per year and X-ray 1 per year) Comprehensive Dental Coverage (1) Part D Plan Type Cost Sharing up to ICL Gap Coverage Legend: CIF-Covered in Full Smart Premium 2014 Provider Manual 2014 20 HMO Entire Island $6,700 $30 In- Network Coverage $50/$150 per admit $50/$150 per admit CIF CIF In- Network Coverage $5 co pay $20 co pay $30/$80 co pay $50 co pay $65 co pay CIF $20 co pay $30 co pay 10%/20% cost share 10%/20% cost share 0%/20% cost share 20% cost share $10 co pay CIF 20% cost share In- Network Coverage CIF CIF CIF CIF CIF CIF CIF In-Network Coverage CIF $100.00 (per years) CIF (once annually) $300 (every three years) 20% (1 per year) 20% (1 per year) CIF Not Covered Enhanced $5/$10/$35/$55/25% $7/$15 Generic only EMERGENCY AND URGENT CARE First+Plus does not require pre-authorization for emergency or urgent care. Claims billed for an emergency or urgent visit will be paid. Although the claims system is designed to suspend claims for certain services that usually require pre-authorization, should a claim for emergency or urgent services be suspended, the claims examiner has the ability to override the authorization requirement and pay the claim. Medical Emergency: A “medical emergency” is when a member has medical symptoms that require immediate medical attention to prevent loss of life, loss of a limb, or loss of function of a limb. The medical symptoms may be an illness, injury, severe pain, or a medical condition that is quickly getting worse. If a member has a medical emergency: • The member should get medical help as quickly as possible. Call 911 for help or go to the nearest emergency room. The member does not need to get an approval or a referral from the PCP. • Make sure that First+Plus knows about the member’s emergency, because we will need to be involved in following up on the emergency care. • First+Plus will help manage and follow up on emergency care. First+Plus will talk with the doctors who are giving emergency care to help manage and follow up on the member’s care. When the doctors who are giving the emergency care indicate the member’s condition is stable and the medical emergency is over, what happens next is called “post-stabilization care.” Follow-up care (post-stabilization care) will be covered according to Medicare guidelines. In general, we will try to arrange for plan providers to take over the care as soon as the member’s medical condition and the circumstances. Emergency covered services: • Members can get covered emergency medical care whenever they need it. • Ambulance services are covered in situations where other means of transportation in Puerto Rico would endanger the member’s health. Urgently needed care (this is different from a medical emergency) “Urgently needed care” is when a member needs medical attention right away for an unforeseen illness or injury, and it is not reasonable given the situation for the member to get Provider Manual 2014 21 medical care from other plan providers. In these cases, the member’s health is not in serious danger. How a member gets “urgently needed care” depends on whether the member needs it when he/she is in the plan’s service area, or outside the plan’s service area. What is the difference between a “medical emergency” and “urgently needed care”? The main difference between an urgent need for care and a medical emergency is in the danger to the member’s health. “Urgently needed care” is if the member needs medical help immediately, but his/her health is not in serious danger. A “medical emergency” is if the member believes that his/her health is in serious danger. Getting urgently needed care in the plan’s service area: If a member has a sudden illness or injury that is not a medical emergency, and he/she is in the plan’s service area, the member should call his/her doctor or First+Plus. The member can get urgently needed care from a non-plan provider. However, using our plan providers will result in lower costs. Getting urgently needed care OUTSIDE the plan’s service area: First+Plus covers urgently needed care that a member gets from non-plan providers when the member is outside the plan’s service area. If the member needs urgent care while outside the plan’s service area, we prefer that the member contacts their preferred provider first, whenever possible. If treated for an urgent care condition while out of the service area, we prefer that the member return to the service area to get follow-up care from plan providers. However, we will cover follow-up care that a member gets from non-plan providers outside the plan’s service area as long as the care still meets the definition of “urgently needed care.” Provider Manual 2014 22 ADDITIONAL BENEFITS Renal Dialysis and Post-stabilization Care First+Plus will have procedures to authorize payment for out-of-network services. However, particular services will be monitored for timely processing of payment. These services include out-of-plan Emergency and Urgent Care services, Renal Dialysis and Post-stabilization services. First+Plus prefers to coordinate member care as it relates to Renal Dialysis and PostStabilization care in order to ensure that the member receives the most appropriate care for his or her individual circumstances. Obtaining pre-authorization is recommended to ensure a comprehensive treatment plan is developed, which may include coordinating care at an out-ofnetwork facility to accommodate the patient’s needs. If a claim for these services should be suspended, the examiner would pay in accordance with an authorization if one is on file. If no authorization is on file, and it is evident that the services were an emergency, the authorization requirement would be overridden and the claim would be paid. If there is any question as to the medical necessity, the claim is referred to the Medical Affairs department for review. Once a determination is made, the claim is referred back to the Claims department, and the claim is paid accordingly. Women’s Care: Consistent with First+Plus access philosophy, women have direct access to a women’s health care specialist within the network for women’s routine and preventative health care services. Women may also have access to services outside of the First+Plus network, under the PPO coverage. Members are not required to obtain a referral or authorization to visit an OB/GYN. Provider Manual 2014 23 PROVIDER ROLES AND RESPONSIBILITIES Compliance with the Contract, Regulations and this Manual: First+Plus is subject to certain requirements as set forth by the Centers for Medicare and Medicaid Services for this health plan. The First+Plus provider contract requires compliance with our plan contract and with federal regulations governing Medicare Advantage Health Plans and the plan’s policies and procedures. Those requirements are set forth in the First+Plus provider contract, this manual and from time to time in provider newsletters and other communications and notices sent by First+Plus. General Medicare and Federal Regulations: A First+Plus provider is required to not contract with, subcontract or employ individuals or persons with ownership with a 5 percent or more controlling interest, who have been convicted of criminal offenses related to their involvement in Medicaid, Medicare or social services under Title XX of Social Security Act and thus has been excluded from participation in any Federal Health Care Program under Sec. 1128 or 1128A of the Act A. First+Plus providers must verify all CMS Exclusions Lists such as Office of Inspector General (OIG / http://www.oig.hhs.gov/) and Exclude Parties List System (EPLS /http://www.epls.gov ) every time a First+Plus Provider hires new personnel and then monthly, to ensure that none of its employees are listed on either lists. These revisions must be documented and archived by providers for evidence to be presented to First+Plus and/or CMS upon request. First+Plus Provider shall immediately notify First+Plus in writing of any action to restrict, revoke, or suspend the licenses or certificates that are necessary for the provider to operate; any changes in its business address (es), any debarment, suspension or exclusion of you, your employees, contractors, subcontractors, directors, officers or owner with a 5 percent or more controlling interest; and any other serious situation that could interfere with provider responsibilities. • If a First+Plus provider files an affidavit with CMS stating that they will furnish Medicarecovered services to Medicare beneficiaries only through private (direct) contracts with the beneficiaries under Section 1802(b) of the Social Security Act (i.e. they will not accept payment from Medicare), then their contract with First+Plus will terminate concurrently. A First+Plus provider must provide notice to First+Plus within five (5) days of providing any notice with CMS. • First+Plus providers must provide Covered Services to all Members, including those with ethnic backgrounds, physical or mental disabilities, and limited English proficiency, in a culturally competent manner. Provider Manual 2014 24 • Plus First+Plus providers must provide disabled covered members with the necessary assistance to effectively communicate with the participating provider and their staffs, as required by the Americans with Disabilities Act. • Providers shall comply with all applicable Medicare laws and regulations. • All providers are to understand and comply with the First+Plus policies on the confidential treatment of member information in all settings and must abide by all the federal and state laws regarding confidentiality and disclosure of medical records or other health and enrollment information. • All providers are to treat members protected health information (PHI), including medical records, confidentially and in compliance with all federal and state laws and regulations. • First+Plus members have the right to appeal any Plan decision that involves issues of information, confidentiality and privacy. First+Plus Contract Requirements: The Agreement with First+Plus contains numerous important provisions, which are synopsized below. In some situations, a First+Plus contracted provider may subcontract with another provider to provide services to a First+Plus Member. In all cases, any such subcontracts must include the following provisions: • Providers understand that First+Plus is responsible for overall administration of the health plan including all final coverage determinations and monitoring of its contracted provider’s compliance with federal regulations. • First+Plus is responsible for all marketing of the health plan and providers are not authorized to act as agents of First+Plus in marketing. Only First+Plus (and CMS) approved marketing materials may be provided to beneficiaries to explain the First+Plus program. • Providers will comply with First+Plus Utilization/Medical Management Policies and procedures. • Providers will comply with First+Plus Quality Management Programs. • No Balance Billing of Members with the exception of applicable co-payments or coinsurances. • A First+Plus contracted provider agrees not to impose any charges on any First+Plus Member for Covered Benefits shown in the Evidence of Coverage. Further, contracted providers agree to accept the First+Plus payment as payment in full and agree not to seek compensation from a First+Plus Member for services provided to that Member, even in the event of non-payment by First+Plus. Provider Manual 2014 25 • Services shall be provided in a culturally competent manner constituent with professionally recognized standards of care. Providers shall not discriminate based upon health status factors. Providers shall ensure that their office hours do not discriminate against Medicare enrollees. • First+Plus Providers must not discriminate against Members based on their health status. Further, Providers must ensure that Members are not unlawfully discriminated against on the basis of race, color, creed, national origin, ancestry, religion, sex, marital status, age, physical or mental handicap, or in any other manner prohibited by state or federal law. • First+Plus requires that all providers participate in periodic audits and/or site surveys for evaluating compliance with First+Plus Quality Management standards and regulatory requirements. • Provider agrees to audits and inspections by CMS the U.S. department of Health and Human Services and/or its designees, and to cooperate, assists and provided information as requested. • First+Plus Providers must provide all covered benefits in a manner consistent with professionally recognized standards of health care. • First+Plus Providers must cooperate with the plan’s grievance and appeals procedures that protect beneficiary and member rights. • First+Plus Providers have specific continuity of care obligations in the event that the First+Plus Agreement terminates for any reason, including a provider’s de-participation or if First+Plus becomes insolvent. In the event of insolvency, First+Plus Providers must continue to provide care to Members through the period in which their CMS payments have been made to First+Plus. Additionally, if the Member is hospitalized, services must be provided until termination of CMS’s agreement with First+Plus or, in the event of First+Plus insolvency, through the date of the Member’s discharge. Review the First+Plus contract for any additional sections or provisions not discussed in this section. In addition, the description of the contract provisions listed in this section does not constitute the complete disclosure of all requirements placed on providers contracted with First+Plus. Contracted providers should refer to their First+Plus contract for further information. Provider And Member Communications: Participating Providers are responsible to maintain the provider-member relationship with each Member. Nothing contained in the First+Plus us Agreement or this Manual is intended to interfere with such provider-member relationship. First+Plus shall not prohibit or restrict any provider for disclosing to any enrollee, patient, or designated representative any information that the provider deems appropriate regarding a condition or a course of treatment with an enrollee including the availability of other therapies, test, etc. First+Plus shall not prohibit or restrict a health care professional acting within the lawful scope of practice, from advocating on the behalf of an individual who is a patient and enrolled under First+Plus. Providers shall not be prohibited Provider Manual 2014 26 from discussing the risks, benefits and consequences of treatment or non- treatment with the enrollee, patient or designated representative. Patients shall have the opportunity to refuse treatment and to express preferences about future treatment decisions. The participating physician shall have the sole responsibility for the medical care and treatment of Members. In the event that a First+Plus Provider terminates their participation or relationship with the Plan, First+Plus has the exclusive right and responsibility to communicate with its Members regarding those changes; participating providers should not send independent notices to First+Plus Members. Medical Records: Provider agrees to safeguard beneficiary privacy and confidentiality and assure accuracy of beneficiary health records • All providers must maintain documents for at least (10) ten years or (10) years from the age of majority. • Encounter must be record and the data must be certified on record, for completeness and truthfulness. • Copies of consent forms, when applicable, should be maintained in the record. • Files must be kept private in accordance with HIPPA. • Provider agrees to maintain enrollee health records in accordance with standards established by First+Plus PPO, which shall take into account professional standards. Enrollee Health records shall: 1. Identify the enrollee. 2. Identify all providers who participate in the enrollee’s care and information on services furnishes by these providers. 3. A problem list; including significant illnesses and medical and psychological conditions for the enrollee. 4. Presenting complaints, diagnoses, and treatment plans for the enrollee. 5. Prescribed medication, including dosages and dates of initial or refill prescriptions for the enrollee. 6. Information on allergies and adverse reactions (or a notation that the patient has no known allergies or history of adverse reaction). 7. Information on advanced directives. 8. Past medical history, physical examination, necessary treatments, and possible risk factors for the enrollee relevant to the particular treatment. 9. Must be legible. 10. Noted medication allergies and adverse reactions. Provider Manual 2014 27 11. There must be a completed immunizations record in all records. 12. All entries in the record must be signed or initialed and dated. • Pursuant to the Federal Patient Self Determination Act, Hospitals, Skilled Nursing Facilities, Home Health Agencies, Providers of Home Health care must maintain written policies and procedures concerning advanced directives with respect to all adult individuals receiving medical care by or through the provider. Providers must document in an individual’s medical records whether or not the individual has executed an advanced directive. Providers must provide written information to individual concerning: 1. An individual’s rights under state law to make decisions regarding medical care. 2. The providers (or facilities) written policy with regard to implementing such rights. • Providers will only provide copies of medical records to other providers and insurance companies if the member has signed a release form allowing them to do so. • Provider must transfer these records in a timely manner. • Provider agrees to reviews by First+Plus to monitor and assess enrollee records with respect to improving content, legibility, organization, and completeness of the records. Responsibilities of all Providers: The Provider must provide service in a manner consistent with professionally recognized standards of care and in culturally component manner. The Role of the Primary Care Practitioner (PCP): Not all the Firs+Plus members are required to select a Primary Care Practitioner (PCP). The PCP serves as the member’s initial and most important contact for receiving medically necessary covered services. The PCP provides or coordinates care each member. This includes: • Maintaining a current medical record for each member, including documentation of all medical services (PCP and specialty) provided to the member • Coordinate a member’s care needed from specialty physicians or other healthcare providers by referring to providers in the First+Plus network of providers. Except in emergency situations, if services are not available within the First+Plus network of providers, then the Preferred Provider must contact First+Plus Medical Management team to obtain prior authorization to refer a Member to a non-participating provider prior to the care being rendered. • If a Member is referred to an emergency room, the Preferred Provider is responsible for contacting First+Plus to provide notice of his or her authorization of the emergency visit. • Provide direction and follow-up care for those Members who have received emergency services. Provider Manual 2014 28 • Providing periodic physical examinations as outlined in the Preventive Health Guidelines. • Providing routine injections and immunizations. • Providing health education and information. Roles of Specialists: The role of a First+Plus participating specialist is to provide consulting expertise, as well as specialty diagnostic, surgical and other medical care for First+Plus Members. First+Plus expects a participating specialist to support the role of a Preferred Provider in coordinating and managing a Member's health care by providing only those specific services for which the member has been referred, and promptly returning the Member to the Preferred Provider as soon as medically appropriate. Open, prompt communication with the Preferred Provider concerning follow-up instructions, circumstances of further visit requirements, medications, lab work, x-rays, etc. are essential to the coordination of care. The First+Plus Specialist’s responsibilities include: • The specialist must provide a report to the Members Preferred Provider within five (5) working days of rendering care or as soon as possible in the event that legitimate delays result from lab tests, x-rays, pathology reports, etc. • If further care is required beyond the scope of the original referral, the specialist must contact the Member's Preferred Provider to determine if an additional referral or authorization it necessary before providing additional treatment. • If a specialist is consulted during an emergency room visit, a referral is not required for providing that care; however, authorization may be required for any follow-up care provided after the emergency room visit. • If a specialist is called in for a consultation during an observation or hospital stay, no referral is required for providing that care in the hospital. However, for any follow-up care provided after that hospitalization, an authorization may be required. • Specialists should order all laboratory testing, radiology studies or other diagnostic testing through a contracted, in-plan facility unless an emergency situation clearly indicates emergency lab or radiology services are required. First+Plus has specific, contracted laboratory and radiology service providers in all regions. There are specific First+Plus policies within each region that outline which of these services may be rendered in an office setting. If you have any questions, please contact our Provider Department. Panel Closure: Occasionally Preferred Providers will request closure of their panel to new First+Plus Members. First+Plus requires a 90-day written notice to the Provider Services department prior to the proposed effective date of such closure. This panel closure must be in writing. During the 90-day period between notification of closure and revision of the provider directories to reflect such closure, Preferred Provider must continue to accept Members who select them. First+Plus will continue to list closed Preferred Providers in First+Plus provider directories with a notation designating them as “not accepting new members”. Provider Manual 2014 29 Reopening of Panel: When a Preferred Provider requests to re-open their panel to new members, the preferred provider will send a written notice to the Provider Services Department requesting re-opening of their panel and the effective date of the re-opening. Sanctions Under Federal Health Programs and State Law: Participating providers must ensure that no management’s staff or other persons who have been convicted of criminal offenses related to their involvement in Medicaid, Medicare or other Federal Health Care Programs are employed or subcontracted by the participating provider. As some fully stated, providers must disclose to First+Plus whether the provider or any staff member or subcontractor has any prior violation, fine, suspension, termination or other administrative action taken under Medicare laws or the federal government. Participating providers must notify to First+Plus immediately if any such sanction is imposed on the provider, a staff member or subcontractor. Appointment Availability Standards: First+Plus has adopted the following standards for access: Prompt access to providers is vital for care to Members. The First+Plus policy on Provider/Plan Access Standards was developed with this core value in mind. The standards listed in this policy support the value of service as it seeks to anticipate, understand and respond to individuals, organizations, nursing facility and community needs as Members access healthcare services. First+Plus is committed to assuring the care the Member is entitled to, be delivered in the correct setting, correct timeframe and correct manner. Below is an outline of the standards developed by First+Plus: A. Access to Medical Care: 1. First+Plus requires health care providers to provide access to health care services without excessive scheduling delays. Providers will have policies and procedures in place to properly identify emergency conditions and appropriately triage such cases. Triage involves identifying which cases can be managed in the office/nursing facility or making alternative arrangements, e.g. immediate care service or emergency room for cases which cannot be safely managed in the office/or nursing facility setting. 2. Medical Appointments: The maximum time period between a request for an appointment/or visit to the nursing facility and the date offered will be: Provider Manual 2014 30 a. Life Threatening, Emergent problem: Immediate access. b. Urgent Care: Same Day Defined as services provided for the relief of acute pain, initial treatment of acute infection, or a medical condition that requires medical attention, but a brief time lapse before care is obtained does not endanger life or permanent health. Urgent conditions include, but are not limited to, minor sprains, fractures, pain, heat exhaustion and breathing difficulties, other than those of sudden onset and persistent severity. c. Preventive Care: 30 days Defined as a preventive health evaluation without medical symptoms for existing members. I.e. routine exam, annual physical. d. Routine Care: 7-14 days or earlier based on the population. Defined as non-urgent symptomatic condition that is medically stable. Special attention will need to be given based on the geriatric population and how symptoms are presented. e. Pregnant woman in their first trimester are to be provided preventive care visit within 14 days of request. f. Pregnant woman in their second trimester are to be provided preventive care visit within 7 days of request. g. Pregnant woman in their third trimester are to be provided preventive care visit within 3 days of request. Note: If a provider’s schedule cannot accommodate the Member requesting an Urgent Care or Routine Care appointment within these time intervals, an appointment will be offered with an alternative provider, nurse provider, physician assistant or certified nurse midwife at the same location, or if none are available, at another location. The Member may choose to decline alternatives and accept a delayed appointment with the provider. Provider Manual 2014 31 CONTRACTED PROVIDER GRIEVANCES PROCESS First+Plus has established an internal process to meet all grievances arising from contracted providers. Participating provider must exhaust the following administrative procedures before initiating the grievance process: Administrative Procedures 1. Verify if the claim was denied in full o partially due to billing errors, and or lack of required documentation to process the claim accordingly 2. If after reviewing the explanation of payment reason codes you are still in disagreement with the action taken by First+Plus, you should submit a request for re-evaluation of the claim through the regular adjustment process. 3. You should complete and submit the form “Auditoria de Facturas”, a copy of the claim with the corresponding corrections if applicable, and any supporting documentation needed for the evaluation of the claim. Please remember that submitting a claim for reevaluation does not guarantee that the claim will be adjusted for payment. 4. The provider of services has twenty (20) days after the receipt of initial denial notification forwarded by First+Plus, to submit the request for the adjustment to the following address: First+Plus Claims Department P.O. Box 195559 San Juan, Puerto Rico 00919-5559 Or hand delivered the claims to our office address located at: First+Plus Ext. Villa Caparra #530 Marginal Buchanan, Guaynabo, P.R. 00966 5. You will be notified through the Explanation of Payment (Voucher) of the result of the evaluation, and in some instances you might receive a letter with the decision taken on your adjustment request. 6. If you received an adverse determination and still do not agree with that determination, then you can proceed to submit a Grievance following the process detailed below. Provider Manual 2014 32 Grievance Process (You must have exhausted the Administrative Procedures described above before submitting a request for a Grievance) 1. The provider must complete the Grievance Form (Page 44) in its entirety and send by mail or deliver it personally to the offices of First Plus. 2. This grievance must include a copy of the claim, and the relevant information necessary to evaluate the case. This includes but is not limited to copy of the Payment Voucher, evidence of claim submission, among others. 3. If submitted by mail please send the documents to: First+Plus Provider’s Department P.O. Box 195080 San Juan, Puerto Rico 00919 4. You will be notified in writing of the results of your grievance. 5. Failure to comply with the above process, the grievances will be dismissed. The provider will receive a letter notifying the reason for the dismissal. The claims will be channeled through regular adjustment process. If you have any questions or require additional information, please contact us at 1-866-505-5885 or (787) 620-1649. Monday to Friday 8:00 am to 5:00 pm. Provider Manual 2014 33 Provider Manual 2014 34 CREDENTIALING First+Plus has developed a systematic method for assessing provider applicants against the Plans credentialing and re-credentialing standards for providers. Upon receipt of a completed application, primary source verification is conducted by a credentials verification organization within 180 days of application date. Following the verification of credentials, First+Plus Credentialing Committee review each application, makes recommendations for participation or continued participation and makes the final approval. Providers who choose to opt out of the Medicare program will not be allowed to participate with the Plan due to them opt out status with the Medicare program. First+Plus requires all providers applying for participation must meet all credentialing standards in accordance with the procedure outlined below. Any physician failing to meet the minimum standards will not be recommended for acceptance into the network. • First+Plus does not discriminate in terms of participation, reimbursement, or indemnification, against any health care professional acting within the scope of his/her license. • First+Plus does not discriminate against professionals who serve high-risk populations or who specializes in the treatment of costly conditions. • First+Plus does not discriminate against any health care professionals in terms of participation reimbursement or indemnification. • First+Plus does not discriminate against any professional who serves high-risk population or who specialize in the treatment of costly conditions. Providers are considered without regard to race, creed, color, gender, age, sexual orientation, national origin or handicap, unless the latter affects the ability of the practitioner to provide quality healthcare. First Medical First+Plus will provide written notice with explanation to a provider that is denied participation in the program. Each practitioner is required to complete a provider application in which the provider has certified that the information contained in the application for membership is true and correct in all aspects and does not fail to state a material fact that would make it otherwise misleading. The First+Plus application contains questions regarding physical and mental health status, illegal drug use, history of loss of license, felony convictions, and history of loss of privileges or disciplinary action. This application must be signed and dated by the practitioner. Network Adequacy: First+Plus will identify all providers necessary to ensure the adequacy of the network in compliance with all CMS regulations. First+Plus will evaluate the network, taking into consideration a Member’s ability to access commonly used services within the regular mandated Provider Manual 2014 35 travel time, or as reasonable patterns of care would allow (Metro Area: General Physician, Internal Medicine, General Practice and Family Practice (15) and Specialty (30) Minutes. Rural area: All Providers (30) minutes. Primary Source: All health care providers including physicians, dentists, chiropractors, podiatrists and any other allied health professionals who request admittance into the First+Plus network must have their credentials verified through state, federal, governmental agencies, licensing bodies, hospitals or schools that have supervised the appropriation of such licenses, qualifications and appointments. This is done through primary source verification of credentials through the respective primary sources: • Current, valid, unrestricted state license to practice • Verification of appropriate education and training • Board certified, if applicable, by a recognized certification program • Malpractice history • Medicare/Medicaid sanctions • Medicare Opt-Out First+Plus ensures compliance with Federal requirements prohibiting employment or contracts excluded from participation under either Medicare or Medicaid. New Providers: First+Plus verifies the primary source of all new providers against the Medicare sanctions list prior to entry into the First+Plus network. In addition First+Plus will review providers against the Medicare opt out list, provided by the local carrier, to ensure that new providers have not opted out of Medicare. Any provider found to have existing sanctions or to have opted out of Medicare will be excluded from participation in the First+Plus network. If currently participating: First+Plus reviews the list of sanctioned Medicare providers and the Medicare opt out list on a quarterly basis for existing members. Upon confirmation of provider sanction information or that the provider has elected to opt out of the Medicare program, the panel will be closed and the name suppressed from printing in a future directory. Simultaneously, the Credentialing Department may request information from the provider and reporting agency to determine if there are further details of the sanction. If the information is consistent and the provider has been barred from participation from Medicare and/or his or her license has been the subject of a disciplinary action (including but not limited to: censure, reprimand, loss of license, suspension etc.), termination procedures will follow immediately. Provider Manual 2014 36 Provider Orientation: First+Plus will provide an orientation to providers approved in the credentialing process to ensure that the providers fully understand the plan and compliance regulations. Re-Credentialing; First+Plus requires all plan providers to be re-credentialed every three years. The Provider must submit updated credentials in order to be re-credentialed. In addition, the provider will be reviewed utilizing internal information obtained from the necessary departments. Termination: First+Plus reserves the right to terminate a provider’s contract immediately, with written notice, under the following circumstances: • • • • • • • • • • • Conviction for any criminal offense related to the practice. Failure to comply with First Plus credentialing standards and procedure. Final disciplinary action is taken by a governmental regulatory agency that impairs the provider’s ability to practice; There is a determination of fraud. There is an imminent harm to patient care. Failure to comply with quality assurance, peer review and utilization procedures. Unprofessional conduct as defined by the Medical Examiner’s Board Professional Ethics Code. Revocation, reduction, or suspension of privileges at any Participating Hospital or any hospital where PHYSICIAN conducts his principal practice. failure by PHYSICIAN to meet the Conditions of Participation' specified hereinafter; Discrimination against First + Plus Members. Repeated failure of Provider’s to comply with the terms of the agreement. A letter of notification will be sent to the provider. Within 60 days of receipt of the termination letter, the provider can submit a written request to First+Plus for a hearing to consider the proposed action. The hearing must be scheduled within the 30-day period following First+Plus receipt of the provider’s written request. The Hearing Panel will be appointed by First+Plus and must have at least three members, the majority of which must be a clinical peer. A “clinical peer” is defined as a provider having the same or substantially similar specialty as the provider under review. If the panel assembled has more than three members, the majority of the panel’s members must be clinical peers. The hearing panel will render its decision as promptly as possible, and will notify the provider of its decision in writing. The panel may decide to reinstate, conditionally reinstate, or terminate the provider. Termination will become final at the later of these dates: 60 days after the notice of intent to terminate or 30 days after the panel’s determination letter has been sent to the provider. Under no Provider Manual 2014 37 circumstances will First+Plus initiate termination actions against a provider solely because he/she: 1. Advocated on behalf of a member; 2. Filed a complaint against First+Plus with state or federal regulatory bodies; 3. Appealed a decision made by First+Plus; or 4. Provided information, filed a report, or requested a hearing or review. The Department of Health requires First+Plus to report the termination of a provider’s contract for any of the following reasons: Duty to Report Certain Terminations: The Department of Health requires First+Plus to report the termination of a provider’s contract for any of the following reasons: • Alleged mental or physical impairment, misconduct, or impairment of patient safety or welfare; • Voluntary or involuntary termination of contract or employment to avoid disciplinary action; • A determination of fraud or of imminent harm to patient’s health. If a provider is terminated or suspended for deficiency in the quality of his or her care, written notice of the action must be given to the licensing or disciplinary bodies or other appropriate authorities. Member Notification: Members will be notified of a provider’s termination from the First+Plus network within 15vdays of receipt of the notice of termination. Members will be informed of other providers in the First+Plus network that are in their geographic area and can provide the same services as the provider who has been terminated. FAX NUMBER TO SUBMIT DOCUMENTS: (787) 300-3907. Provider Manual 2014 38 GRIEVANCES AND APPEAL A Grievance is any complaint or dispute other than organization determination, expressing dissatisfaction with the manner in which First Plus or a delegated entity provides health care services, regardless of whether any remedial action can be taken. A beneficiary can file a complaint either in writing or verbally expressing dissatisfaction with any aspect of the operations, activities, or behavior of a plan sponsor, regardless of whether remedial action is requested. A grievance may also include a complaint that a plan sponsor refused to expedite a coverage determination, a re-determination, an organization determination or reconsideration, or invoked an extension to an Organization determination or reconsideration time frame. A beneficiary can file a grievance verbally or in writing via fax, email or regular mail. This complaint must be submitted within 60 calendar days from the day the event or incident occurred. For standard grievances, First+Plus will have to respond to the complaint in writing within 30 calendar days from the date received. We have 24 hours from the date received, to respond to an expedited grievance. First+Plus may extend the time frame by up to 14 calendar days if you ask for the extension, or if we justify a need for additional information and the delay is in the beneficiary best interest. If First+Plus make a coverage determination or an organizational determination and the beneficiary are not satisfied with this decision, he/she can file an appeal. An appeal is a formal way of asking us to review and change a coverage determination or an organizational determination we have made. All appeal requests must be submitted within 60 calendar days from which the initial determination was made. A beneficiary can file a Part D appeal verbally or in writing. For expedited requests First Plus, have 72 hours from the date received, to respond to a request in writing and 7 calendar days for a standard Part D appeal. To request a Part C Appeal, with the exception of an expedited request, the beneficiary must send a signed written request via fax, email or regular mail. For Part C service appeals, First+Plus have 30 calendar days to respond in writing and 72 hours for expedited requests. First Plus may extend this time frame by up to 14 calendar days if you ask for the extension, or if we justify a need for additional information and the delay is in your best interest For Part C appeals related to claims or reimbursements First Plus have 60 calendar days from the date received in writing to respond. Those appeals cannot be requested expedited, in addition the time frame extension does not apply. First Plus must keep track of all grievances and appeals in order to report data to CMS and to our members, upon request. To obtain more information, please contact our Provider Call Center at 1-866-505-5885. Our service hours are Monday to Friday 8:00 am to 5:00 pm. Provider Manual 2014 39 Submitting a Grievance or an Appeal To submit a grievance, an expedited grievance, a redetermination, or an expedited redetermination, the beneficiary can send us a signed written request or contact our Customer Service Department at 1-888-767-7717 or TTY /TDD users should call 1-877-672-4242. Our service hours are Monday to Friday 8:00 am to 8:00 pm. To request a Part C appeal the beneficiary or their representative must submit a signed written request to the Grievance and Appeals Department by fax at 787-300-3918 or by mail to the following address: First+Plus P.O. Box 195080 San Juan, PR 00919-5080 Through email: [email protected] If First Plus denies the beneficiary’s request in whole or in part, the beneficiary will receive a written decision explaining the denial reasons, and information on any dispute resolution options you may have. Remember, all types of Grievances and Appeals related to your Prescription Drug Coverage can be filed verbally by calling our Customer Services Department at 1-888-767-7717. If a beneficiary has an appeal related to Part C he/she must submit a signed written request. For more information on appeals and grievances, please call our Provider Call Center at 1-866505-5885 Monday to Friday from 8:00 am to 5:00pm Appointing a Representative A beneficiary or someone who he/she appoint as an authorized representative may file a grievance or appeal. A beneficiary can appoint a relative, friend, lawyer, advocate, doctor, or anyone else to act for him/her. Or, a beneficiary may already have someone authorized under Commonwealth law to act for you. If a beneficiary want someone to act for him/her who is not already authorized by the Court or under State law, then he/she and that person must sign and date a statement that gives the person legal permission to be your representative. The form is available on the following link, which will redirect you to the CMS website. http://www.cms.gov/cmsforms/downloads/cms1696.pdf Or in the First Plus web link under the grievance and Appeal section, the link is: http://www.firstpluspr.com/es/ Provider Manual 2014 40 MEDICAL AFFAIRS Utilization Management: First+Plus maintains a Utilization Management Program to ensure that First+Plus Members have timely access to appropriate, medically necessary, and cost-effective health care services. The Utilization Management Program addresses such issues as: preventive care, in-patient services, and ambulatory care. Responsibility for ensuring the implementation of all aspects of the Utilization Management Program has been delegated to the Plan’s Medical Director by the Board of Directors. The main goals of the Utilization Management Program are to ensure quality, relevant care while promoting appropriate utilization of medical services and Plan resources. The objectives of the Utilization Management Program are to: Provide a structured process to continually monitor and evaluate the delivery of health care and services to our enrollees by: • • • • • • • Establishing system-wide health management processes across the continuum of care. Establishing a process for provider feedback regarding utilization. Monitoring indicators to detect possible under- and over-utilization. Auditing utilization management decision timeliness on a monthly basis. Determining enrollee and provider satisfaction with medical management. Assessment of member benefits utilization on an annual basis to identify any changes and needs for member add-on benefits. Assure appropriate member access to services through analysis of Out of Network (OON) utilization patterns Improve Clinical Outcomes by: • • • • Collaboration, system-wide, to identify, develop, and implement clinical practice guidelines that address key health care needs of the enrollees. Implementation of clear, consistent UM Program. Implementing actions, when appropriate to improve under- and over-utilization. Collaboration with the Quality Department to assess and implement actions to improve continuity and coordination of care. Improve provider and enrollee satisfaction by: • • Assessing and improving UM satisfaction data from provider and enrollee surveys. Promoting appropriate utilization of Plan resources through efficiency of service. Provider Manual 2014 41 Meet or exceed established quality standards by: • • • • Measuring program performance HEDIS HOS CAHPS Utilization review staff is responsible for obtaining all pertinent clinical indications and medical record information necessary to perform assessments of service authorizations. The UM staff is responsible for application of utilization review criteria/guidelines (Milliman Care Guidelines®) to each individual case and for referral to the Medical Director when criteria are not met. The UM Department staff is responsible for identification of all potential or actual quality of care issues, and cases of over and under-utilization of health care services for First+Plus members during all components of review and authorization. Evidence Based Clinical Practice Guidelines First+Plus conducts its medical review and evaluation of health care services utilizing nationally recognized policies, standards of care, and evidence based clinical guidelines. Examples of such health care services include inpatient and outpatient care, durable medical equipment, medications, and other services required for coordinating care for our members. First+Plus staff uses such policies, standards, and guidelines from the Centers for Medicare and Medicaid Services (CMS) and its carriers, Milliman Care Guidelines ®, InterQual Guidelines® for Inpatient UM, national professional organizations (i.e. American Diabetes Association, American Heart Association) and other federal government organizations such as the Food and Drug Administration (FDA), the Centers for Disease Control and Prevention (CDC), and the Agency for Health Care Research and Quality (AHRQ). A list of the above mentioned organizations most commonly used and their websites are included below: 1. Center for Medicare and Medicaid Services (for contractors, providers, and other healthcare industry professionals) http://www.cms.gov/home/medicare.asp 2. Center for Medicare and Medicaid ( Special Needs Plans) https://www.cms.gov/SpecialNeedsPlans/ 3. First Coast Service Option , Medicare carrier for Puerto Rico http://www.fcso.com/ 4. Milliman Care Guidelines http://www.milliman.com/expertise/healthcare/products- tools/milliman-care-guidelines/ 5. American Diabetes Association http://professional.diabetes.org/?utm_source=Homepage&utm_medium=HeaderPro mo2&utm_content=ForProfessionals&utm_campaign=DP Provider Manual 2014 42 6. American Heart Association http://www.heart.org/HEARTORG/HealthcareResearch/HealthcareResearch_UCM_001093_SubHomePage.jsp 7. Agency for Health Care Research and Quality http://www.ahrq.gov/ 8. Food and Drug Administration http://www.fda.gov/ForHealthProfessionals/default.htm The comprehensive methods of review and authorization include the following processes: UM Committee Charter: Provide direction to the First+Plus Utilization Management Program and act as an advisory and oversight committee. Evaluate current and proposed utilization management programs for effectiveness and performance against goals. Analyze utilization, both under and over, and recommend direction or program changes, as needed. Recommend corrective actions based on clinical trends or changes in the standards of care. Review and approve guidelines for the delivery of health services to First+Plus members. Oversee and monitor all delegated UM activities. Authorization Process: First+Plus requires prior authorization for some procedures and services to ensure that the most appropriate care is provided for First+Plus members. This Prior Authorization Manual outlines the process for submitting prior authorization requests to First+Plus Medical Affairs Department for services included in the categories below. Prior Authorizations: Prior authorization is designed to promote the medical necessity of service, to prevent unanticipated denials of coverage and ensure that participating providers are utilized and that all services are provided at the appropriate level of care for the member’s needs. First+Plus precertification program reviews a specific list of medical services for medical necessity. First+Plus does not require prior authorization for the following services: • Emergency Services • Emergency Ambulance Services dispatched through 911 or its local equivalent, where other means of transportation would endanger the member’s health • Urgently needed services • Yearly routine physicals by in-plan providers: Colorectal and prostate screening exams. • Yearly Routine Eye Care Provider Manual 2014 43 • Influenza vaccine (yearly), Pneumococcal vaccines and Hepatitis B vaccines by in-plan providers • Renal Dialysis Services for those temporarily out of the service area • Basic Lab tests (i.e. CBC, BMP, UA) • Skeletal X-rays / chest X-rays • Clinical trials: Original Medicare covers routine costs of qualifying clinical trials. A member does not need to obtain a referral to join a clinical trial. However, it is recommended that the member inform First+Plus before they start a clinical trial so First+Plus can keep track of the member’s health care services. Authorization Requirements Submission of a referral form (Medical Certification Form & Authorization Request Form) and clinical information is required. The physician must provide medical justification including medical history, laboratories results, and previous studies for better decision making (i.e. progress notes, imaging reports, operative reports etc.). Prior Authorization is required for the services included in the categories below: Durable Medical Equipment: Scooters Wheelchairs and accessories (All types & Bariatric) Beds and accessories (All types & Bariatric) Lifter Orthotics Prosthetics CPAP, BPAP Oxygen Continuous Passive Motion (CPM) Diabetes supplies Power nebulizers Infusion Pumps (All types) Mechanical Ventilator ( Home ) Negative Pressure Wound Therapy Bone Grow Stimulator Wearable Cardioverter Defibrillator Provider Manual 2014 44 Miscellaneous: Medical Surgical Trays Cardiac and Orthopedic Implants Polysomnography (Sleep Studies) Special EEG Test (24hrs) Oncotype Dx Test Specialized Services: Home Care Services Home Infusion Services Skilled Nursing Facility and Extended Care Facility Comprehensive Outpatient and Inpatient Rehabilitation Facility & Services (CORF) Specialized Therapies: Pain Management Medical Nutrition Services Physical Therapy/ST/OT Wound Care Hyperbaric Oxygen therapy (HBO) Pulmonary Rehabilitation Cardiac Rehabilitation SRS- Stereotactic Radiosurgery SBRT –Stereotactic Body Radiation Therapy IMRT -Intensity Modulated Radiation Therapy Medications: Part B Drugs ( J codes) Chemotherapy and administration Respiratory Drugs Surgeries: Bariatric surgeries Minimally Invasive Robotic Surgery (Da Vinci) Reconstructive and other potential cosmetic surgeries: Rhynoplasty, Abdominoplasty, Septoplasty, Blepharoplasty, Augmentation or Reduction of Breast, Face lift, Ptosis repair. Provider Manual 2014 45 Urology: Lithotripsy Cardiology Procedures: Permanent Cardiac Pacemaker trays and Pacing Cardioverter – Defibrillator Insertion and the Implantable Cardioverter Defibrillator (ICD) Enhanced External Counter pulsation (EECP/Vasotherapy) Nuclear Medicine Studies: PET CT Scans/PET Scans SPECT(Brain , Myocardial Perfusion ) SPECT + Pharmacology Agents Radiology: MRI w / without contrast MR Neurography (MRN) MR Venography (MRV) MRA CT Scans w / without contrast Cardiac CT Scan - Coronary CT Angiography CT Colonoscopy (Virtual Colonoscopy) Arthrography (CT and MR) ERCP/MRCP Others: Air Ambulance (Out of Puerto Rico) Ambulance Service Non –emergency Organ Transplant (all types Important Information: Expedited (Urgent) Pre-Service Referral: The organization makes decisions within 24-72 hours from receipt of the request. Standard (Routine) Pre-Service Referral: 24 hours up to 14 calendar days. Provider Manual 2014 46 The Physician must provide medical justification including medical history, laboratories results and previous studies for better decision making. Medical Necessity: Request to extend a course of treatment beyond the period of time or number of treatments previously approved. The organization makes decisions according to Expedited or Standard criteria. Emergency Referrals: NO AUTHORIZATION REQUIRED The Utilization Reviewers obtains medical record within twenty-four (24) hours of notification of admission (or next business day) by site visit to ensure the admission to the acute care hospital is appropriate/medically indicated in accordance with the illness or condition or to confirm information obtained during prior authorization of elective admissions. Inpatient Concurrent/Extended length of Stay Review: Concurrent review is the evaluation of a patient’s continued need for treatment and the appropriateness of current and proposed treatment, as well as the setting in which the treatment is being rendered or proposed. Concurrent review applies to all levels of inpatient care and partial hospitalization. If an admission or an extended stay does not meet the required criteria, a request for further review will be sent to the Medical Director. Medical necessity and appropriateness of setting and treatment review is performed by Utilization Reviewers that will actively track and manage the inpatient stays to ensure coordination of care with the member’s physicians. The First+Plus Case Management staff will give follow up to patients in extended length of stay (more than 10 days). Our Concurrent Management program is designed to ensure that all inpatient stays are medically indicated and that care is provided in the most appropriate setting using Inter Quall Guidelines®. Service highlights include: • • • • Notification from the Hospital’s Utilization Management Department for the initial review only to determine the medical necessity of the admission, and follow up. On site discussion of cases with Hospitals’ Case Management Department for periodical evaluation during a member’s course of hospitalization to assess the medical necessity and appropriateness of continued stay confinement at the requested level of care. Coordination of early proactive interventions and discharge planning in conjunction with the hospital’s Case Management Department to facilitate transition of care back to the member’s nursing facility and physicians. Identification of patients for enrollment in focused Case Management. Provider Manual 2014 47 Discharge Planning Review and Responsibilities: Discharge Planning begins as early as possible during an inpatient admission in collaboration with the hospital’s Case Management Department and the attending physician. Such planning is designed to facilitate transition of care back to the member’s nursing facility and physicians and identify any post-hospital care needs for the member. In addition, all First+Plus members admitted to a Medicare approved facility must receive notification of their discharge and appeal rights. If a First+Plus member disagrees with the pending discharge, the hospital must issue the Notice of Discharge and Medicare Appeals Rights as a part of the discharge appeal process. A copy of the letter must be filed in the member’s hospital record and faxed to the First+Plus UM Department at (787) 705-9347 / (787) 622-0729 to be filed in the member’s record. Retrospective Review: Retrospective Review is a review process performed by Utilization Reviewers after services have been rendered, to determine: • • • • If unauthorized services were medically necessary/appropriate. If services were rendered at the appropriate level of care and in a timely manner. If a quality of care issues exist. If Provider claims appeals are in order The institution is responsible of notifying the cases which hasn’t been review to First+Plus and to provide the appropriate information for case evaluation on a timely manner based on applicable regulations and contractual agreements. The attending physician and/or hospital/facility are notified in writing of the claim payment determinations via the EOB. The determination of services medical necessity is based on the analysis of the information provided and the application of nationally recognized clinical criteria. Benefits will be paid; adjustments can be made according to the review made. Ancillary Services (Home Health, Durable Medical Equipment, Hospice): Referrals for any ancillary services including Home Health and Durable Medical Equipment require authorization from the Utilization Management (UM) Department. Hospice referrals to a Medicare certified agency are initiated for tracking and trending purposes only. When a member enrolls in Medicare certified Hospice, the Hospice is reimbursed directly by Medicare Fee-ForService for all the Hospice services the member receives. While the member is enrolled in Hospice, their First+Plus coverage is limited to Non-Hospice Part D, and any Supplemental Benefits offered to our members. Skilled Nursing Facility (SNF) Review: When a member is transferred or admitted to Skilled Nursing Facility (SNF) Care, First+Plus uses Medicare SNF criteria and Inter Qual Guidelines® to determine appropriate level of care. All admissions to SNF require authorization by the First+Plus UM Department. Provider Manual 2014 48 Inpatient Rehabilitation Facility (IRF) Review: Intensive rehabilitation services are provided after an injury, illness or surgery. This service includes physical, occupational and speech therapy in a coordinated multidisciplinary setting. All admission to IRF requires authorization by the First+Plus UM Department. Case Management Program First+Plus uses a comprehensive, integrated approach for the treatment of chronic medical conditions and complex medical conditions that facilitates the physician-patient relationship, emphasize prevention and continually evaluate health outcomes. First+Plus conducts a health risk assessment on newly enrolled members and classified them as very high, high, moderate or low health risk. All First+Plus members s in a Special Need Plan are enrolled in the Case Management Program unless they opt-out from it. After the initial or annual Health Risk Assessment (HRA) members from the SNP products are stratified as specified above and different levels of interventions are applied by risk level. Members from other products who are identified as “high risk” or “disease specific” will be referred to a Case Manager in order for intervention to take place as soon as possible. Case Managers will contact those members and assess their medical and social situation and identify any problems that may adversely impact their health. Case Managers will also assist high-risk, frail elderly members with coordinating necessary medical service in accordance to risk stratification Level Primary care physicians and members receive copies of the Individualized Care Plans (ICP) developed based of the answers provided by the First+Plus members to the health risk assessments performed. The providers are encouraged to discuss and evaluate the recommendations included in the ICP with the member. The goals of the case manager is to provide comprehensive coordination of care and benefits for the SNP member, health promotion and prevention services. Specific functions of the case manager include but are not limited to: a) Perform the activities of assessment, planning, coaching, education and advocacy for members throughout the continuum of care, consistent with evidence based clinical guidelines. b) Collaborate and communicate with the member/family, the physician and other health care providers in the development and implementation of a care plan that is driven by the member’s goals for health improvement. c) Support in the accomplishment of the goals specified the individual member’s care plan. d) Provide members and their families with information and education that promotes self-care management. e) Involve the member and his/her family in the coordination of services. f) Assist members in their transition across health care settings by providing information, support and serving as a link between the member, family/caregiver and providers. g) Support members in optimizing the utilization of available benefits. h) Improve member and provider satisfaction. Provider Manual 2014 49 i) Ensure timely interventions that increase effectiveness and efficiency in care delivery. j) Promote the health, independence, and optimal functioning of members. First+Plus Case Managers communicate with members/caregivers on an ongoing basis, as needed, and document all follow-up in Case Management application. At a minimum, the case managers re-evaluate the Individualized Care Plan on an annual basis (365 days and /or before initial HRA) for any necessary revisions. The re-assessment takes in consideration the member’s progress towards identified goals, results of the annual HRA, findings from the ER frequent Report, and input from the member/caregiver in member with high risk level. Members who have chosen to opt out of the HRA and/or Case Management processes are flagged for re-contact in 12 months or if they are identified by Medical Affairs as high utilizes of key incidents of care such as Re admission Providers are encouraged to refer members that may benefit from the Case Management Program. Using the following form “Referral Form” (see form) For more information or any questions related to the Case management Program or Referral Form, please contact our customer service number at 1-888-767-7717. We are available Monday through Friday from 8:00am to 8:00pm. TTY users should call 1-877-672-4242 or fax request to (787) 705-9347 or (787) 622 -0729 Provider Manual 2014 50 Benefit during Disaster and Catastrophic Events First Plus has adopted this policy to comply with Section 160 of Chapter 4: Benefits and Beneficiary Protections of the Medicare Managed Care Manual and to provide guidance in case of a disaster or catastrophic event. Definitions Emergency: An emergency is a major disaster declared by the President of the United States; an emergency or disaster declared by a state Governor, including the Governor of Puerto Rico; or a public health emergency declared by the Secretary of the Department of Health and Human Services or by the Secretary of the Puerto Rico Health Department. Provider: Any Medicare provider or supplier (for example, hospital, skilled nursing facility, durable medical equipment, home health agency, outpatient physical therapy, comprehensive outpatient rehabilitation facility, renal dialysis facility, hospice, physician, non-physician Procedure 1. During an Emergency declaration, First Plus will take the following actions: a. Allow Part A/B and supplemental Part C plan benefits to be furnished at specified non-contracted facilities (note that Part A/B benefits must, per 42 CFR § 422.204(b)(3), be furnished at Medicare certified facilities); b. Waive in full, requirements for gatekeeper referrals where applicable; c. Temporarily reduce plan-approved out-of-network cost sharing to in-network cost-sharing amounts, where applicable; and d. Waive the 30-day notification requirement to enrollees as long as all the changes (such as reduction of cost-sharing and waiving authorization) benefit the enrollee. e. Activate a waiver to the pre-authorizations requirements. 2. Prior to the Emergency Event - Medical Affairs Pre-Authorization staff will identify providers with high volume of cases, cases with risk services and cases that requires transition in order to ensure their contingency plan is active. a. Medical Affairs Pre-Authorization staff performs outbound calls to the identified providers to validate the process they are taking to ensure continuity of care and services. b. For providers that are unable to perform contingency plan, the Transition Policy is activated. c. Medical Affairs Manager and/or Director contact First Plus Triage Nursing Line to inform them of the pre-authorizations waiver and to notify them to activate the Contingency Plan. Additionally, the Medical Affairs Manager and/or Director share the First+Plus Medical Affairs Management Contact List of the staff available to support the Contingency Plan. 3. Post- Emergency Event - Medical Affairs Management Team identifies the staff available and necessary to re-start the department operations as soon as possible. Provider Manual 2014 51 a. Medical Affairs staff performs a validation process with the identified providers delivering the care/services to monitor the continuity of care/services was performed. b. For providers that are unable to perform Contingency Plan, the Transition Policy is activated immediately. c. For members with potential life threatening services, Medical Affairs PreAuthorization staff performs an outbound call to validate the member has the necessary care/services. d. A report will be generated by Medical Affairs Management with the documentation of the actions performed prior and post the emergency event. 4. First Plus will continue to apply the abovementioned actions accordingly until the termination of the emergency. First Plus shall consider the following when deciding whether an emergency has been terminated or not: o In the case of a public health emergency, it terminates when it no longer exists or upon the expiration of the 30-day period beginning from the initial declaration, whichever occurs first. o For major disasters or emergencies, First Plus should pay particular attention to the termination of disaster or emergency incident periods listed on FEMA’s web site (http://www.fema.gov/news/disasters.fema). 5. First Plus will monitor CMS releases and ensure if further guidance to extend the emergency period or to shorten it has been issued. Provider Manual 2014 52 Provider Manual 2014 53 Provider Manual 2014 54 QUALITY IMPROVEMENT PROGRAM AND ITS SCOPE Medicare Advantage Organizations (MAOs) must implement and maintain a Quality Improvement Program (QI) as require under 42 CFR §422.152. As part of First+Plus commitment to comply with regulations and First Medical corporate commitment in provide excellent health services, First+Plus Quality Improvement Program has been developed to identify criteria to conduct quality projects based on clinical and non-clinical factors to address and identify areas for improvement. The mission of the Quality Improvement Program is to promote and continuously improve the highest quality of clinical care (medical and behavioral health) and quality of services provided to First Plus enrollees by providers and the health plan. The scope of the First+ Plus Quality Improvement Program includes the following: - Quality Projects and Programs o HEDIS Quality Project First+Plus HEDIS Quality Project is focused in the widely used set of performance measures in the health industry with the purpose of comply with quality metrics related to Care Effectiveness, Access/Availability of Care, Care Experience (Satisfaction Survey), Utilization and Health Plan Information, with the implementation of different strategies. . o Quality Improvement Project (QIP) First+Plus QIP has the goal to reduce hospital re-admissions of First+Plus members through the implementation of its Transition Care Management Program. o Chronic Care Improvement Program (CCIP) First+Plus CCIP is directed to its diabetic members with hypertension with the goal to improve their health status controlling their blood pressure. o Special Needs Plan Model of Care (MOC) First+Plus MOC has the objectives of: improve the services’ access for physical and mental health and for care transitions, ensure the appropriate utilization of health services, encourage the communication between providers, members and their care givers, and measure the results of this Model through health outcomes. o Satisfaction Surveys (CAHPS and HOS) The different Satisfaction Projects established by First+Plus are focused in to improve the satisfaction of its members with the provided services, the perception related to accessibility, physician-member relationship, the communication with the provider and their physical and mental health. o STARS Project Provider Manual 2014 55 First+Plus STARS Quality Project has the purpose of facilitate and evaluate health care services received by First+Plus members in order to be appropriate, cost-effective and to improve their health status. These objectives will be accomplished with the compliance of the quality standards required by CMS. o SNP Structure and Process Project First+Plus SNP Structure and Process Project is directed to comply with CMS and NCQA requirements to ensure the provision of quality services to First+Plus most vulnerable population. Monitoring Tools – First+Plus Quality Team has developed some quality indicators that are monitored regularly to ensure the compliance with the MOC requirements, HEDIS and STARS metrics and operational indicators that evaluate the quality of services provided by First+Plus departments. One of the most important components of the First+Plus Quality Improvement Program is its Quality Committee. This Committee is responsible for the development, implementation and oversight of the overall Quality Program for First+Plus. The Committee evaluates the results of quality improvement activities, utilization results, outcomes and recommends actions with the purpose of improve and maintain the health status of First+Plus members. The First+Plus Quality Improvement Program is approved by First Medical Board of Directors and is evaluated annually to identify barriers (if any) to comply with the quality goals proposed every year. Every First+Plus contracted provider is crucial to comply with the goals established in the Quality Program: supporting First+Plus Quality Projects and Programs and complying with the provider roles and responsibilities defined in every First+Plus Quality Project and Program. With the compliance of these roles and responsibilities, the provider will continue facilitate services with quality and excellence to First+Plus members. HEDIS Quality Project (Data and Information Group Health Effective) HEDIS is a Quality Project required by CMS to all Medicare Advantage organizations. It is a dynamic project that considers medical guidelines for establishing quality indicators that measure the performance in different areas of health care and services. It has 75 indicators and is divided into eight (8) domains of care: 1. 2. 3. 4. 5. 6. 7. 8. Effectiveness of care Access and availability of care Satisfaction in the care experience received Health Plan Stability Use of Service Cost of care Health Care Team Report Health Plan Information Provider Manual 2014 56 Some of the actions performed by First+Plus to support the efforts of its providers to impact HEDIS metrics are: • Frequent notifications with reference material related to the quality indicators, their measurement criteria, recommendations and results; • Individual notifications that includes the profile of the population under your care. These communications may include specific identification of those members in compliance and noncompliance with certain HEDIS metrics; • Development and implementation of quality initiatives that promote preventive health services and treatment; • Provide guidance on best coding practices and documentation of treatment offered. Also, First + Plus makes target actions to its members to impact HEDIS metrics such as: • Promote the doctor-patient relationship by facilitating the accessibility of preventive and treatment services necessary to improve and maintain good health in the population of First+ Plus members; • Motivate and educate members about the importance of meeting their health goals, treatment plan and preventive services through various educational strategies; • Facilitate coordination of annual preventive evaluation and/or treatment; • Development and implementation of quality initiatives that provide preventive services in order to improve or maintain their health status. First + Plus is committed to report HEDIS indicators according to the criteria and guidelines established by CMS. The results of these indicators are used to identify areas of improvement in the performance of the health plan and its contracted providers. Following are some of the HEDIS indicators that impact Stars Program as established by CMS. These indicators are reviewed and updated annually. (May apply additional details for the indicators following described and/or exclusions). Breast Cancer Screening (BCS) The percentage of women 40–69 years of age who had a mammogram to screen breast cancer. Colorectal Cancer Screening (COL) The percentage of members 50–75 years of age who had appropriate screening for colorectal cancer. Provider Manual 2014 57 Cholesterol Management for Patients With Cardiovascular Conditions (CMC)- Cholesterol Screening The percentage of members 18–75 years of age who were discharged alive for AMI, coronary artery bypass graft (CABG) or percutaneous coronary interventions (PCI) from January 1– November 1 of the year prior to the measurement year, or who had a diagnosis of ischemic vascular disease (IVD) during the measurement year and the year prior to the measurement year, who had each of the following during the measurement year: • LDL-C screening Comprehensive Diabetes Care- Cholesterol Screening The percentage of members 18–75 years of age with diabetes (type 1 and type 2) who had each of the following. • LDL-C screening Glaucoma Screening in Older Adults (GSO) The percentage of Medicare members 65 years and older who received a glaucoma eye exam by an eye care professional for early identification of glaucoma related conditions. Adult BMI Assessment (ABA) The percentage of members 18–74 years of age who had an outpatient visit and whose body mass index (BMI) was documented during the measurement year or the year prior to the measurement year. Care for Older Adults (COA) - Medication Review The percentage of adults 66 years and older who had each of the following during the measurement year: • Medication Review Care for Older Adults (COA) -Functional Status Assessment The percentage of adults 66 years and older who had each of the following during the measurement year: • Functional Status Assessment Care for Older Adults (COA) – Pain Management The percentage of adults 66 years and older who had each of the following during the measurement year: • Pain Management Provider Manual 2014 58 Osteoporosis Management in Women Who Had a Fracture (OMW) The percentage of women 67 years of age and older who suffered a fracture and who had either a bone mineral density (BMD) test or prescription for a drug to treat or prevent osteoporosis in the six months after the fracture. Comprehensive Diabetes Care- Eye Exam The percentage of members 18–75 years of age with diabetes (type 1 and type 2) who had each of the following: An eye screening for diabetic retinal disease. Comprehensive Diabetes Care-Nephropathy The percentage of members 18–75 years of age with diabetes (type 1 and type 2) who had each of the following. • Medical attention for nephropathy Comprehensive Diabetes Care- HbA1c Control The percentage of members 18–75 years of age with diabetes (type 1 and type 2) who had each of the following. • HbA1c poor control (>9.0%). • HbA1c control (<8.0%). Comprehensive Diabetes Care- LDL-C Control The percentage of members 18–75 years of age with diabetes (type 1 and type 2) who had each of the following. • LDL-C control (<100 mg/dL). Controlling High Blood Pressure (CBP) The percentage of members 18–85 years of age who had a diagnosis of hypertension (HTN) and whose BP was adequately controlled (<140/90) during the measurement year. Disease-Modifying Anti-Rheumatic Drug Therapy The percentage of members who were diagnosed with rheumatoid arthritis and who were dispensed at least one ambulatory prescription for a disease-modifying anti-rheumatic drug (DMARD). Plan All-Cause Readmissions (PCR) For members 18 years of age and older, the number of acute inpatient stays during the measurement year that were followed by an acute readmission for any diagnosis within 30 days and the predicted probability of an acute readmission. Provider Manual 2014 59 Listed below are other indicators specific to HEDIS (not related to Stars) that are evaluated as part of the Project: 1. Persistence of Beta-Blocker Treatment after a Heart Attack (PBH) The percentage of members 18 years of age and older during the measurement year who were hospitalized and discharged alive from July 1 of the year prior to the measurement year to June 30 of the measurement year with a diagnosis of AMI and who received persistent beta-blocker treatment for six months after discharge. 2. Antidepressant Medication Management (AMM) The percentage of members 18 years of age and older with a diagnosis of major depression and were newly treated with antidepressant medication, and who remained on an antidepressant medication treatment. Acute Phase antidepressant medications for 12 weeks, Effective Continuation Phase antidepressant medication treatment for at least 180 days (6 months). 3. Follow-Up after Hospitalization for Mental Illness (FUH) The percentage of discharges who were hospitalized for treatment of selected mental health disorders and who had an outpatient visit, an intensive outpatient encounter or partial hospitalization with a mental health practitioner. Two rates are reported: the percentage of discharges for which the member received follow-up within 7 and 30 days of discharge. 4. Frequency of Selected Procedures (FSP) This measure summarizes the utilization of frequently performed procedures that often show wide regional variation and have generated concern regarding potentially inappropriate utilization. Medical Record Review Project The Medical Record Review Project is conducted as part of HEDIS Quality Project. The participation of First+Plus providers is important for the recollection of medical information that is crucial to this Project. The process established by First+Plus is the following: 1. Coordination of Appointments • First+Plus sends an introductory letter of HEDIS Project and then contact the provider to coordinate the appointment for the recollection of the necessary medical information. Once coordinated the appointment, the representative of First+Plus visits the facility according to the date and time established. A list per indicator is send with the names of patient’s clinical record needed. All revisions and recollection of health information for HEDIS Project is performed in compliance with HIPAA requirements. Provider Manual 2014 60 2. Medical Records Abstraction First + Plus representative visits the facility or medical office at the coordinated time and date, proceed with the digitization of medical records according to the necessary medical information. 3. Information by Fax Providers may choose the option to send the requested information via fax by completing the established format for this purpose. The Medical Record Review process identifies the compliance of members of First+Plus with the quality indicators under evaluation. The provider participation of First+Plus in this process is crucial to achieve the expected results in HEDIS project. The Role of the Provider to impact the First+Plus HEDIS metrics: 1. All progress notes must be legible and complete with date and time of the encounter. 2. Document the results of diagnostic tests ordered and make annotation of recommendations in the member progress notes such as: changes in the list of medications, education about advance directives, medication adherence, among others. 3. Reconcile members’ medications with medications ordered at discharge after hospitalization, documenting changes such as elimination of drugs, increased dosage, and route change, among others. 4. Motivating patients to meet their annual checkups. 5. Make follow-up calls to members who do not comply with their treatment. Following is the information that must be found in the progress notes of the clinical record of the members for compliance with HEDIS quality measures: MEASURE Adult BMI Assessment (ABA) INFORMATION FROM THE MEDICAL RECORD FOR POSITIVE EVENT (HIT) Measurement Year and Prior Year Progress Notes, Flow Sheets, Growth Chart from Pediatric Provider, Consult Reports from Nutritionists or other Specialists Colorectal Cancer (COL) Report of Colonoscopy since 2002, Report of flexible Sigmoidoscopy since 2007 Hem occult, Guaiac, gFOBT, iFOBT note or lab result negative/positive in measurement year Note or medical history showing procedure (above) Controlling High Blood Problem List Pressure (CBP) Notes from event that got member into the measure or an earlier visit as long as it shows HTN or High Blood Provider Manual 2014 61 EXCLUSION Pregnancy during MY Note showing history of colon or rectal cancer Note showing history of total colectomy Full chart copy to rebut assumption member has HBP (minimum MY, ideally 2nd half Cholesterol Management (CMC) Comprehensive Diabetes Care (CDC) Eyes (DRE) Care for Older Adults (COA) Pressure Notes from last visit in measurement year with a BP reading Vitals Flow sheet Lab Results showing all Lipid tests in measurement year Measurement Year Lab Reports showing: Last HbA1c Last LDL-C or LDL-D OR Last Lipid panel showing (Total Chol, HDL, Triglycerides) All labs in measurement year showing urine specimen results Any Measurement year consult reports from Nephrologist Medication List Problem List showing renal or kidney disease Any note showing Dx of renal insufficiency or failure Any notes/ scripts for ACE Inhibitor/ ARB therapy Last Blood Pressure Listing from measurement year from Progress notes or flow sheets Any consults or hospital documents in measurement year All measurement year and prior reports from Eye Care professional Any mention of eye care or retinopathy in chart Any referral for eye exam Measurement Year Progress Notes: • Any Advanced Directives, Living Wills or signed documentation noting patient has reviewed Advanced Care Materials • Any medication list during measurement year with evidence of review by prescriber or clinical pharmacist • Any measurement year Functional Status Worksheets, Checklists or Evaluation Scales or notation of performance or inability to perform – Activities of Daily Living (ADL’s)/ Instrumental Activities of Daily Living (IADL’s); any evaluation of thinking, gait/ambulation, hearing/vision, and living situation/independence. • Pain Assessment Worksheets, Numeric Rating Scale, Visual Assessment Scale, any notation of Provider Manual 2014 62 PY+MY) Medication list Notation of Pregnancy Full chart to rebut assumption member had AMI, CABG or PTCA or evidence IVD in PY / MY OPTIONAL EXCLUSIONS: Notes showing member has gestational, steroid-induced diabetes Notes showing polycystic ovary disease (females only) Med List, labs and any notes that rebut DX of Diabetes none none comprehensive pain management, pain treatment plan, or notation of absence of pain Medication Reconciliation PostDischarge (MRP) All measurement year discharge summaries (from the outpatient record), Progress Notes, or dated medication records within 30 days of discharge that display evidence that discharge medications were reviewed none Supplemental Data First Plus uses additional data sources other than claims to collect data on health services offered to its members. This additional information is used to identify additional health services which are provided to First Plus members and to confirm the health information provided thru claims submitted by physicians. The supplemental data can be used when the information can be found in the medical record through forms with medical or demographic information, information in medical history forms, diagnoses, laboratories results, test measurements, among others, or when the provider documents in the medical record all the discussed information provided verbally to the member at the time of the medical evaluation. This information is collected by medical records audit, request of the medical information by fax, postal office or by quality initiatives activities performed. Some additional sources of information are: • Information questionnaires, such as Health Initial Assessments • Medical Referrals • Vaccination Record • Laboratory Results • Demographic Records • Estimated Functional Assessments Other sources such as CPT codes II are used to capture diagnostic test results for quality purpose and are also used as supplemental data: 1. These codes can be reported in the claim, after discussing the results of laboratory, and or diagnostic tests with the member; 2. The regular CPT must be included along with these CPT codes II in the claims; 3. The use of these codes can reduce the need for Medical Record Review in the physicians’ offices. Provider Manual 2014 63 Use the following reference list with CPT II codes that can be used to impact HEDIS measures: Description CPT CPT II The most recent Hba1c test during the year 83036, 83037 3044F=most recent Hba1c level less than 7.0% 3045F=most recent Hba1c level between 7.0-9.0% 3046F=most recent Hba1c level greater than 9.0% The most recent LDL-C test during the year 80061,83700,83701,83704,83721 3048F=most recent LDL-C less that 100mg/dl 3049F=most recent LDL-C 100-129mg/dl 3050F=most recent LDL greater than or equal to 130mg/dl Eye Exam=a retinal or dilated eye exam by an eye care professional (optometrist or ophthalmologist) is completed every year or a negative retinal exam (no evidence of retinopathy) by an eye care professional in the prior year. 67028, 67030, 67031, 67036, 67039-67043, 67101, 67105, 67107, 67108, 67110, 67112, 67113, 67121, 67141, 67145, 67208, 67210, 67218, 67220, 67221, 67227, 67228, 92002, 92004, 92012, 92014, 92018, 92019, 92134, 92225-92228, 92230, 92235, 92240, 92250, 92260, 99203-99205, 9921399215, 99242-99245 3072F-low risk if retinopathy in the previous year (no evidence of retinopathy in the previous year) 2022F=Dilated retinal eye exam with interpretation by the ophthalmologist or optometrist documented and review 2024F=7 standard field stereoscopic photos with interpretation by an ophthalmologist or optometrist documented and reviewed 2026F=Eye imaging validated to match diagnosis from 7 standard field sterestopic photos results documented and reviewed COA(Care of Older Adults) 1157F=Advance Care Plan or similar legal document present in the medical record Evidence of Advance Care Planning during the year Provider Manual 2014 64 1158F=Advance Care planning discussion documented in the medical record COA 1159F=Medication list documented in the medical record Medication Review 90862, 99605, 99606 COA 1160F=Review of all medications by a prescribing practitioner or clinical pharmacist documented in the medical record 1170F=Functional Status Assessed Functional Status Assessment COA 0521F=Plan of Care to address pain documented Pain Screening 1125F=Pain Severity Quantified: pain present 1126F=no pain present Comprehensive Diabetes Care(CDC) Nephropathy Screening Test is performed at least once a year. A member in ACE\ARB or has nephropathy is compliant for this submeasure Urine Macroalbumin Evidence of Nephropathy Treatment Provider Manual 2014 82042,82043,82044,84156 81000-81003, 81005 36147, 36800, 36810, 36815, 36818, 36819-36821, 3683136833, 50300, 50320, 50340, 50360, 50365, 50370, 50380, 90935, 90937, 90940, 90945, 90947, 90957-90962, 90965, 90966, 90969, 90970, 90989, 90993, 90997, 90999, 99512 65 3060F=Positive Microalbuminaria Test result documented and reviewed 3061F=Negative microalbuminaria test result documented and reviewed 3062F=Positive Macroalbumina test result documented and reviewed 3066F=Documentation of treatment of nephropathy 4010F=Angiotensin Converting Enzyme (ACE) Inhibitor or Angiotensin Receptor Blocker (ARB) therapy prescribed or currently being taken ACE inhibitor/ARB therapy Diabetic Blood Pressure Control 3074F=Systolic blood pressure less than 130 mm/Hg The most recent BP reading during the year. 3078F=Diastolic blood pressure less than 80 mm/Hg Control 139/89 3075F=Systolic blood pressure 130-139 mm/hg 3079F=Diastolic blood pressure 80-89 mm/hg 3077F=Systolic blood pressure greater than or equal to 140 mm/hg 3080F=Diastolic blood pressure greater than or equal to 90 mm/hg Medication Reconciliation conducted by a prescribing practitioner, clinical pharmacist or registered nurse on or within 30 days of discharge Provider Manual 2014 1111F=Discharge medications reconciled with the current medication list in outpatient medical record 66 Quality Improvement Project (QIP) CMS requires annually implementing a Quality Improvement Project. This year, CMS required to Medicare Advantage organizations to implement a Quality Improvement Project focused on reducing hospital re-admissions. First Plus has developed a Transition Care Management Program to comply with the goal to reduce the hospital re-admissions of its members. There are several interventions being implemented to achieve this goal, such as: alert the Primary Physicians of the admission and discharge of First+Plus members under their care to promote the post-discharge care visit, initiatives of case management, among other interventions. The Role of the Provider in the Quality Improvement Project to reduce hospital readmissions of First+Plus members: 1-Promote the post-discharge visit of the members under your care when First+Plus notified a recent admission/discharge. 2- Educate the member who has had a recent admission to comply with their drugs therapy and self-care strategies to avoid a readmission. 3- Collaborate in Case Management initiatives and First+Plus Post-Discharge Program. 4- Reconcile the medications of First+Plus members after hospital admission. Chronic Care Improvement Program of First+Plus (CCIP) As required by CMS, each Medicare Advantage organization must have established a program to improve chronic care with a defined criteria to identify the members that are going to participate in the Program. This year, CMS required developing a program focused to population with cardiovascular problems. First+Plus has identified an area of opportunity for its members diabetics with hypertension and its CCIP Program is directed to improve the health status of these members with the goal of controlling their blood pressure. To achieve this goal, First+Plus are implementing various strategies such as: sending educational material to all the members under the Program, educational sessions and group activities, individual case management, among others. The Role of the Provider in Chronic Care Improvement Program of First+Plus: 1- Educate your patient who is participating in the Program on strategies for controlling his/her blood pressure and manage their diabetes. 2- Use clinical guidelines of Hypertension and Diabetes published by First+Plus that can be accessed through http://www.firstpluspr.com/es/ in the Section of Provider’s Communication. 3- Promote your patient participation in the CCIP Program, to complete their records of blood pressure, cholesterol, triglycerides and glycosylated hemoglobin. 4- Encourage females participating in the CCIP Program to access the Million Hearts Heart Truth Program by accessing the following e-mail address: Provider Manual 2014 67 http://www.nhlbi.nih.gov/educational/hearttruth/espanol/index.htm 5- Support the Case Management Program activities for First+Plus members under your care. 6- Identify barriers that prevent members under the Program to comply with the goal of controlling their blood pressure and establish strategies to eliminate them. Special Needs Plans, Model of Care and Compliance Tool for Providers First+Plus Special Needs Plans Special Needs Plans (SNPs) are Medicare Advantage plans specialized for individuals with special needs. In the Medicare Modernization Act of 2003, United State Congress identified special needs individuals as: institutionalized beneficiaries or eligible for nursing home care, dual eligible (Medicare and Medicaid) and/or individuals with severe or disabling chronic conditions. First+Plus currently offers the following Special Needs Plans: • • First+Plus Complete- A Special Needs Plan available to people with Diabetes and Medicare. First+Plus Platino- A Special Needs Plan available to anyone who has both medical assistance: Medicare and Medicaid. Special Needs Plan Model of Care Centers for Medicare and Medicaid Services (CMS) require that Special Needs Plans provide a Model of Care through which they deliver healthcare services and manage care for members in a Medicare Advantage organization. The Model of Care consists of eleven (11) elements: 1. Description of Special Needs Plan specific Target Population- Special Needs Plans must provide a description of the population being served. 2. Measurable goals- Special Needs Plans must describe the specific care management goal(s) in measurable terms (e.g., benchmarks, timeframes), how they expected to achieve the goals and the criteria to determine whether goals are achieved. 3. Staff structure and care management roles- Special Needs Plans must provide a description that identifies all staff, both employed and contracted, who performs administrative, clinical and oversight functions for the Model of Care. 4. Interdisciplinary Care Team (ICT) - All Special Needs Plans must have an Interdisciplinary Care Team (ICT) to coordinate the delivery of services and benefits for members. 5. Provider network having special expertise and use of clinical practice guidelines and protocols- Special Needs Plans should describe the specialized expertise in the organization’s provider network to treat the special needs members and how is determined that its providers are actively licensed and competent. 6. Model of Care Training (personnel and provider network)- Special Needs Plans must describe how they conduct the initial and annual MOC training including: content and Provider Manual 2014 68 strategies to assure completion, actions to be taken for those who do not complete the training and the personnel responsible for oversight these activities. 7. Health Risk Assessment (HRA)-The Health Risk Assessment includes a medical, psychosocial, cognitive, and functional assessment that guides care management and accounts for health status changes in the member. All Medicare Advantage organization (MAO) must conduct HRAs when the member enrolls in the plan and within 12 months of the last risk assessment, or as often as the health of the enrollee requires. 8. Individualized Care Plan (ICP)- The Interdisciplinary Care Team must consult with the member to develop a comprehensive Individualized Care Plan that addresses the member’s particular needs. 9. Communication Network- Special Needs Plan must coordinate the delivery of services and benefits through integrated systems of communication among plan personnel, providers, and beneficiaries. 10. Care Management for the most vulnerable subpopulation- Special Needs Plans must describe how most vulnerable members are identify and describe the delivery of add-on services and benefits. 11. Performance and health outcome measurements- Special Needs Plan must describe how and who collect, analyze, report and evaluate the Model of Care and how and to whom it reports the results of the evaluation. Model of Care Goals First+Plus has adopted the following care management goals in which the First+Plus Provider support is essential: • • • • • • • Improve member access to medical, mental health, and social services Improve member access to affordable care Improve coordination of care through an identified point of contact Improve seamless transitions of care across healthcare settings, providers, and health services Improve member access to preventive health services Assure appropriate utilization of services Improve member health outcomes Case Management Program- Please refers to the corresponding Section under Medical Affairs. Compliance Tool for Providers The provider role in the First+Plus Quality Projects is crucial because of his/her direct contact with the member as the “health gatekeeper”. First+Plus Quality staff provides the following Checklist as a Compliance Tool with the Elements of the Special Needs Plan Model of Care. Provider Manual 2014 69 First+Plus Special Needs Plan Model of Care Compliance Tool Element: Interdisciplinary Care Team (ICT) Call and ask to participate directly in the ICT, forum to discuss the case of your patient with the purpose to identify alternatives available to meet the special needs of the members and improves their health outcomes Element: Provider network having special expertise and use of clinical practice guidelines and protocols Complete the First+Plus credentialing and re-credentialing process Keep updated credentials Notify credential changes and status to First+Plus Comply with the Clinical Practice Guidelines and Protocols shared by First+Plus. Electronic copy can be access on www.firstpluspr.com Element: Model of Care Training Complete the First+Plus MOC training Complete the MOC Training Acknowledgement Receipt Form Keep the MOC training as reference source. Electronic copy can be access on www.firstpluspr.com, under Provider Section/Providers Communication Element: Health Risk Assessment (HRA) Complete the Annual Medical Assessment Form (AMAF) for each First+Plus patient Submit the completed AMAFs to First+Plus Continue and encourage the care plan established in the AMAF Re-assessed the member to identify health status changes Element: Individualized Care Plan Review and discuss the Individualized Care Plan sent by First+Plus with the member Encourage the member to continue the treatment established in the care plan Provider Manual 2014 Update the individualized care plan as member health status change Discuss the updated Individualized Care Plan in response to changes in the health status with the member 70 Element: Network Communication Communicate your availability to participate in meetings and conference call with the ICT by calling 787-620-1290 Access on regular basis the First+Plus website to obtain communications and recent events Submit to First+Plus the corresponding Acknowledgment of Receipts Check on regular basis your mail and e-mail to validate if you have received important communication from First+Plus Keep continue communication with personnel of First+Plus Case Management Program Element: Care Management for the most vulnerable subpopulation Maintain related with the benefits that the First+Plus Special Needs Plans provide Refer to the marketing materials available through the First+Plus website www.firstpluspr.com Check in the Individualized Care Plan the risk stratification that First+Plus has adjudicated to your patients to establish health strategies according to their risks Refer the member to the several First+Plus Clinical Programs that meet the eligible criteria using the Referral Form Element: Performance and health outcome measurements Analyze the several health reports of your patients communicated by First+Plus Keep the proper communication in the member record to support the data recollection process, as HEDIS Participate and support First+Plus quality initiatives Participate in First+Plus satisfaction surveys Timely respond to request of information from First+Plus. Provider Manual 2014 71 First+Plus Special Needs Plan Structure and Process Project The Centers for Medicare and Medicaid have contracted the National Committee for Quality Assurance (NCQA) to develop a strategy to evaluate the quality of care that Special Needs Plans provide. The strategy is divided in phases lasting several years starting with the definition and evaluation of the desirable structural characteristics, followed by the evaluation of the processes and ultimately, results. The assessment approach includes two types of assessment: HEDIS measures and measures that assess the structure and process requirements by submitting documentation from the health plan to NCQA. During the evaluation process, First + Plus submits documentation to support the services offered to its members, its Case Management Program, the Transition Care Program, Post-Discharge Management Program, among other documentation. The First+Plus Provider represents an important role as a gatekeeper of the more vulnerable members and as a liaison between the member and the case manager. First+Plus invites all its Providers to encourage First+Plus patients to benefit from Case Management Program and from the First+ Plus Quality Projects and Programs. CAHPS & HOS Satisfaction Surveys A. Medicare Health Outcomes Survey The Health Outcomes Survey by Medicare (HOS) provides a general indication of how well a Medicare Advantage organization manages the Physical and Mental health of its members. Each year, a sample of members of First + Plus are selected to answer the satisfaction questionnaire. The first year of participation is called the Base Questionnaire and two years later, to the same group of members, are repeated the same questionnaire and is called the Follow Up Questionnaire. Here are some of the main components of the questionnaire of this Satisfaction Survey: 1. Physical Health Component · 2. Mental Health Component · 3. If the member has received education related to Urinary Incontinence Physical activity in older adults · 5. Questions related to mood, problems with concentration, etc. Management of urinary incontinence in older adults or urine leakage problems · 4. Questions related to activities of daily living Limitation in physical activities or the execution of some physical activity such as walking Fall Prevention Management · If the member has received a falls prevention education Provider Manual 2013 72 6. Osteoporosis Testing in Older Women 7. Role of Physicians · Explanation of medical conditions (s) and laboratory results by the physician · Waiting time for treatment at medical office The Role of First + Plus Providers in HOS Satisfaction Survey: 1. Communicate and educate your patients on how to improve their physical and mental condition. 2. Explain the treatment plan, so the member can understand his/her laboratory results, plan and changes in his/her treatment and complications of the health condition(s). 3. Encourage your patient to perform physical activity according to their medical condition. 4. Provide written information on how to improve physical and mental health. 5. Encourage your patient to contact their health plan to know about quality initiatives. 6. Provide verbal and written education for the HOS components such as: prevention of falls, urinary incontinence, influenza vaccine, among others. 7. Monitor and provide tracking to the progress of physical and mental health of your patients and their families at each visit. B. Consumer Assessment of Healthcare Providers and System (CAHPS) The Consumer Assessment of Healthcare Providers and Systems (CAHPS) is an annual satisfaction survey administered by CMS. The regulatory agency choose a sample of unaffiliated and affiliated members to get their opinion and experience in relation to clinical and administrative services offered by both the health plan and its contracted providers. CAHPS includes the following domains that are composed of a set of questions that are made to members: 1. Your health care in the last 6 months 2. Your personal doctor 3. Receiving health services from a specialist 4. Your health plan 5. Your Medicare rights 6. Your drug plan and you Provider Manual 2013 73 Of these domains, specific indicators impact the Stars metrics such as: 1. Receiving needed health services · 2. · In the past six months, how easy it was to get an appointment with a specialist? Receiving timely care and appointments In the past six months, when needed services as soon as possible, how fast you received these services? 3. Customer Service 4. Overall rating of the quality of health care · Using the numbers from 0 (terrible) to 10 (being the best) what would be the score of health care in the last 6 months? 5. Overall health plan 6. Coordination of Care · Did you receive follow up from the medical office for the diagnostic tests ordered? 7. Drug Plan Information 8. Drug Plan Rating 9. Receiving necessary prescribed medications The Role of First + Plus Provider in CAHPS Satisfaction Survey: 1. Educate your staff to receive First+Plus members with courtesy and respect. 2. Provide appointments to members in a timely manner according to the medical necessity presented. 3. Promote accessibility of health services needed by the member including referral to specialists. 4. If the member is referred to a specialist, makes sure the member understands the steps to take and what to expect with that referral. 5. Maintain direct communication with consulting specialists to clarify any doubts or questions about the member. 6. Conduct follow-up calls to members with outstanding diagnostic tests performed. 7. Keep all documentation in the medical record and accessible to the member, if requested. Provider Manual 2013 74 First+Plus Star Rating Project – Star Rating Methodology for Classification The Center of Medicare and Medicaid Services (CMS) has developed a methodology for organizations with a Medicare Advantage contract aligned with the following three main objectives: provide better care, maintain healthier people and communities, and reduce health system costs through continuous improvements. This classification is built on the granting of stars based on the performance of the Medicare Advantage organizations related to quality standards identified annually by CMS. Also, this Star rating serves as a tool to inform and support the Medicare beneficiaries to make decisions concerning of their health plan through the comparison of their performance based on the classification obtained. The classification is given from one (1) to five (5) stars: Stars 1 2 3 4 5 Classification Poor Under Average Average Above Average Excellent The Classification is awarded based on the health plan’s performance of the 36 measures managing Medicare Part C and 15 measures for Medicare Part D. These quality measures are included under the following categories: • Outcomes: provision of services to enhance improvements in the members health status through the services provided; • Intermediate outcomes: specificity in the results of health services rendered; • Experience: members perception about his/her experience during the received services; • Access: issues or barriers to receive the necessary health care services; • Process: processes and actions completed in the delivery of health care services. The results of the quality measures using for the Stars Rating Classification are obtained from the following data sources: Data Source HEDIS CAHPS HOS PDE (Prescription Drug Event Data) Administrative Information Provider Manual 2013 Type Health Effective Data Information System based on the utilization of health care services Satisfaction survey focused in the clinical care, experience and results of the health care services rendered and care coordination Satisfaction survey focus in the experience and health outcomes Data of the pharmacy benefits utilization Administrative data reported to CMS, audits results, data concerning complaints and appeals, health plan operational information 75 The Providers Role in First+Plus’ Stars Program: CMS updates annually the quality measures under Stars Rating Classification. First+Plus communicates these changes through the Provider Manual and/or related written communications to support in the coordination of the appropriate health care services to First+Plus’ members and comply with the requirements. First+Plus providers take an active and leading role in the provision of essential and appropriate health care services for the First+Plus members in order that they can maintain and improve their health status. Some of the measures that are taken into consideration under Star Rating Classification that require specific interventions from First+Plus providers are: Measure Breast Cancer Screening Colorectal Cancer Screening Cardiovascular Care - Cholesterol Screening Diabetes Care - Cholesterol Screening Glaucoma Testing Annual Flu Vaccine Improving or Maintaining Physical Health Improving or Maintaining Mental Health Monitoring Physical Activity Adult BMI Assessment Care for Older Adults - Medication Review Care of Older Adults - Functional Status Assessment Care for Older Adults - Pain Screening Osteoporosis Management in Women who had a Fracture Diabetes Care - Eye Exam Diabetes Care - Kidney Disease Monitoring Diabetes Care - Blood Sugar Controlled Diabetes Care - Cholesterol Controlled Controlling Blood Pressure Rheumatoid Arthritis Management Improving Bladder Control Reducing the Risk of Falling Plan All-Cause Readmissions Getting Needed Care Getting Appointments and Care Quickly Care Coordination Getting Needed Prescription Drugs High Risk MedicationUtilization Diabetes Treatment who also have high blood pressure Provider Manual 2013 Data Source HEDIS HEDIS HEDIS HEDIS HEDIS CAHPS HOS HOS HOS HEDIS HEDIS HEDIS HEDIS HEDIS HEDIS HEDIS HEDIS HEDIS HEDIS HEDIS HOS HOS HEDIS CAHPS CAHPS CAHPS CAHPS PDE PDE 76 Medication Adherence for Oral Diabetes Medications Medication Adherence for Hypertension (ACEI or ARB) Medication Adherence for Cholesterol (Statins) PDE PDE PDE Through a continuous monitoring processes of the performance of these quality standards, First+Plus ensures the provision of an excellent health care services to its members. These monitoring procedures are carried out through population trends and individualized analysis for providers. These analyses help First+Plus to create a provider network profile based on their performance and quality of health services rendered. Based on these results, First+Plus develops and implements various quality initiatives to improve the performance and achievement of national, regional and/or organizational standards. These initiatives are supported by First+Plus members and Providers’ network. First+Plus encourages its contracted providers to review all the information included related to quality initiatives, projects, programs and indicators, and complete the relevant interventions aligned to them. Together, we can improve and maintain a good health status of First+Plus members. For more information or questions related to First+Plus’ Quality Programs and Projects, you may contact the Provider Call Center at 1-866-505-5885 or (787) 620-1649. Monday to Friday 8:00am to 5:00pm or send an email to the Quality Department at the following address: [email protected]. We appreciate your constantly support and your active participation in the Quality Projects and Programs to improve our member’s health. We are Quality! Provider Manual 2013 77 Provider Manual 2013 78 ANNUAL MEDICAL ASSESMENT FORM (AMAF) As required by the Centers for Medicare and Medicaid Services (CMS), First+Plus is responsible of ensuring all new beneficiaries receive a comprehensive evaluation within 90 days from the date of enrollment and once a year for already established beneficiaries. The AMAF is the tool designed for physicians to document the annual face to face encounter. The AMAF also facilitates with compliance and medical purposes such as: • Obtaining current clinical profiles of our population in order to design better medical management programs for our beneficiaries, in accordance with our Primary Care Physicians. • Promoting activities focused on preventive measures and other quality initiatives compliance. • Obtaining beneficiaries’ diagnoses updated in a timely manner in order to reflect the most current health status of our population, as required by CMS. For additional information or questions related to coding or Annual Medical Assessment Forms (AMAF), please contact our Coding Department at (787) 622-0726 extension 302/294 or send us an e-mail at [email protected] Provider Manual 2013 79 Provider Manual 2013 80 Provider Manual 2013 81 Provider Manual 2013 82 Provider Manual 2013 83 Provider Manual 2013 84 Provider Manual 2013 85 Provider Manual 2013 86 BILLING AND CLAIMS Provider agrees to safeguard beneficiary privacy and confidentiality and assure accuracy of beneficiary health records and encounter data. Submission of electronic claims/encounter data must be done through the standard HIPAA formats 837P and 837I with the new 5010 HIPAA compliance layout. Those providers that submit paper claims must use the standard format CMS-1500 for professional services, UB-04 for Institutional claims and J-400 ADA for dental services. The providers must comply with prompt payment law requirements for timely claims submissions. All required supporting documentation must also be submitted with a claim. Each form type has its own require fields, depending on provider type. The required fields must be completed on all form types in order for First Plus to evaluate and process your claim. Below please find billing instructions for each form type (CMS-1450-UB-04/CMS-1500/ADA). In order to process a claim adequately and promptly the provider must submit a clean claim to First Plus. Our contract with Medicare requires that First Medical comply with all, Medicare laws, regulations and CMS instructions applicable to the Medicare Advantage Program. Therefore, our Claim Adjudication System applies all regulatory payment rules, according to the provider type, and corresponding contract. The Centers for Medicare and Medicaid Services (CMS) implemented several initiatives to prevent improper payment before a claim is processed, and to identify and recoup improper payments after the claim has been processed. These initiatives have been on place for many years and commonly used and reported to providers by the Medicare contractors, and Medicare Advantage Organizations such as First Medical. These initiatives have the purpose of reducing payment error by identifying and addressing billing errors related to coverage and coding made by providers. The National Correct Coding Initiatives (NCCI) Edits and the MUEs (Medicare Unlikely Edits) are programs that apply the coding policies as defined by the American Medical Association (AMA) Current Procedural Terminology (CPT) Manual, HealthCare Common Procedure Coding System (HCPCS) Manual, National and local Medicare Policies and edits, coding guidelines developed by national societies, standard medical and surgical practices and current coding practice. The NCCI edits are updated quarterly. These edits are used to process physician services under the Medicare Physician Fee Schedule. It is important to understand, however, that the NCCI does not include all possible combinations of correct coding edits or types of unbundling that exist. Providers are obligated to code correctly even if edits do not exist to prevent use of an inappropriate code combination. Should providers determine that claims have been coded incorrectly, they are responsible to contact First Medical to submit a correct bill for the corresponding adjustment. There are other payment rules which may be applicable to the different methodologies according to the provider type and contract that the provider might have with First Medical. The OCE edits Provider Manual 2013 87 (Outpatient Code Editor) payment rules applies to hospital outpatient services that are contracted under an APC payment methodology. In the variety of provider contracts there might be other type of providers that are contracted under DRG, APC, ASC, DME Fee Schedule, Anesthesia payment rules, Part B Drugs, Home Health Services, etc. Different payment rules may apply for all of these payment methodologies. It is important that the provider takes into consideration the importance of submitting a clean claim with the correct coding information in all the required and correspondent fields. You can obtain more information visiting the following Web Pages: http://www.cms.gov/Medicare/Coding/NationalCorrectCodInitEd http://www.cms.gov/Outreach-and-Education/Medicare-Learning-NetworkMLN/MLNProducts/Downloads/How-To-Use-NCCI-Tools.pdf We are enclosing the billing instructions for submission of paper claims. Remember that it is important to submit a timely and complete claim to expedite the processing of your claim. TIMELY SUBMISSION OF CLAIMS All claims from contracted providers must be submitted according to the Prompt Payment Law Regulations of Puerto Rico, as amended from time to time. As of July 28th, 2011 the Prompt Payment Law established the following time frame for claims submission: Original ClaimOriginal Claim- inpatient services Coordination of Benefits Non-Processable Claims Denials/partial payments (Adjustments) 90 days from service day 90 days from discharge date 90 days from the EOP date of the other payer 20 days from non processable letter 20 days from EOP DATE For Non-Participating Providers, servicing First+Plus members, the CMS -Medicare regulations related to timely submission of claims will be applied. Provider Manual 2013 88 BILLING INSTRUCCIONS FOR STANDARD PAPER CLAIM FORMS We are enclosing the billing instructions for submission of paper claims. Remember that it is important to submit a timely and complete claim to expedite the processing of your claim. CMS- 1500 The following definitions apply to the provider terms used on the 1500 Claim Form. Referring Provider The Referring Provider is the individual who directed the patient for care to the provider rendering the services being reported. Examples include, but are not limited to, primary care provider referring to a specialist; orthodontist referring to an oral and maxillofacial surgeon; physician referring to a physical therapist; provider referring to a home health agency. Enter the referring physician NPI number on field 17b of the CMS 1500 when applicable. Ordering Provider The Ordering Provider is the individual who requested the services or items being reported on A service line. Examples include, but are not limited to, provider ordering diagnostic tests and medical equipment or supplies. Rendering Provider The Rendering Provider is the individual who provided the care. In the case where a substitute provider (locum tenens) was used, that individual is considered the Rendering Provider. The Rendering Provider does not include individuals performing services in support roles, such as lab technicians or radiology technicians. Supervising Provider The Supervising Provider is the individual who provided oversight of the Rendering Provider and the care being reported. An example includes, but is not limited to, supervision of a resident physician. Purchased Service Provider A Purchased Service Provider is an individual or entity that performs a service on a contractual or reassignment basis for a separate provider who is billing for the service. Examples of services include, but are not limited to: (a) processing a laboratory specimen; (b) grinding eyeglass lenses to the specifications of the Rendering Provider; or (c) performing diagnostic testing services (excluding clinical laboratory testing) subject to Medicare’s antimarkup rule. In the case where a substitute provider (a locum tenens physician) is used, that individual is not considered a Purchased Service Provider. Provider Manual 2013 89 The following fields are required 1500 Health Insurance Claim Form: Provider Manual 2013 90 FIELD SPECIFIC INSTRUCTIONS –FIRST+PLUS CARRIER BLOCK The carrier block is located in the upper right margin of the form. Instructions: Enter in the white, open carrier area the name and address of the payer to whom this claim is being sent. Enter the name and address information in the following format: 1st Line – Name 2nd Line – First line of address 3rd Line – Second line of address 4th Line – City State (2 characters) and ZIP Code Line Descriptor Type Bytes Columns 4 Payer Name A/N 41 38-78 5 Payer Address 1 A/N 41 38-78 6 Payer Address 2 A/N 41 38-78 7 Payer City State and ZIP A/N 41 38-78 For an address with three lines, enter it in the following format: 1st Line – Name 2nd Line – Line of address 3rd Line – Leave blank 4th Line – City State (2 characters) and ZIP Code ITEMS 1–13: PATIENT AND INSURED INFORMATION Item Number 1 Title: Medicare, Medicaid, TRICARE CHAMPUS, CHAMPVA, Group Health Plan, FECA, Black Lung, Other Instructions: Indicate the type of health insurance coverage applicable to this claim by placing an X in the appropriate box. Only one box can be marked. Description: “Medicare, Medicaid, TRICARE CHAMPUS, CHAMPVA, Group Health Plan, FECA, Black Lung, or Other” means the insurance type to whom the claim is being submitted. Other indicates health insurance including HMOs, commercial insurance, automobile accident, Provider Manual 2013 91 liability, or workers’ compensation. This information directs the claim to the correct program and may establish primary liability. Field Specifications: This field allows for entry of 1 character in any box within the field. Situational Field Item Number 1a Title: Insured’s ID Number Instructions: Enter “Insured’s ID Number” as shown on First+Plus insured’s ID card of the member. Description: The “Insured’s ID Number” is the identification number of the insured. This information identifies the insured to the payer. Field Specification: This field allows for entry of 29 characters. REQUIRED FIELD Note: Claims with invalid, missing or incorrect member id number will be rejected as nonprocessable claims. Providers must correct and return the corrected claim form along with the non- processable letter within the time frame establish by the Prompt Payment Law of Puerto Rico. Item Number 2 Title: Patient’s Name Instructions: Enter the patient’s full last name, first name, and middle initial. If the patient uses a last name suffix (e.g., Jr, Sr) enter it after the last name, and before the first name. Titles (e.g., Sister, Capt, Dr) and professional suffixes (e.g., PhD, MD, Esq) should not be included with the name. Use commas to separate the last name, first name, and middle initial. A hyphen can be used for hyphenated names. Do not use periods within the name. Provider Manual 2013 92 Description: The “Patient’s Name” is the name of the person who received the treatment or supplies. Field Specification: This field allows for the entry of 28 characters. REQUIRED FIELD Note: Provider must ensure that the Patient ID and the name matches the member ID card from First+Plus. Item Number 3 Title: Patient’s Birth Date, Sex Instructions: Enter the patient’s 8-digit birth date (MM | DD | CCYY). Enter an X in the correct box to indicate sex of the patient. Only one box can be marked. If gender is unknown, leave blank. Description: The “Patient’s Birth Date, Sex” (gender) is information that will identify the patient and it distinguishes persons with similar names. Field Specification: This field allows for the entry of the following: 2 characters under MM, 2 characters under DD, 4 characters under YY, and 1 character in either box. REQUIRED FIELD Item Number 4 Title: Insured’s Name Instructions: Enter the insured’s full last name, first name, and middle initial. If the insured uses a last name suffix (e.g., Jr, Sr) enter it after the last name, and before the first name. Titles (e.g., Sister, Capt, Dr) and professional suffixes (e.g., PhD, MD, Esq) should not be included with the name. Use commas to separate the last name, first name, and middle initial. A hyphen can be used for hyphenated names. Do not use periods within the name. Description: The “Insured’s Name” identifies the person who holds the policy, which would be the employee for employer-provided health insurance. Field Specification: This field allows for the entry of 29 characters. SITUATIONAL FIELD Provider Manual 2013 93 Item Number 5 Title: Patient’s Address (multiple fields) Instructions: Enter the patient’s mailing address and telephone number. The first line is for the street address; the second line, the city and state; the third line, the ZIP code and phone number. Do not use punctuation (i.e., commas, periods) or other symbols in the address. When entering a 9digit ZIP code, include the hyphen. If reporting a foreign address, contact payer for specific reporting instructions. If the patient’s address is the same as the insured’s address, then it is not necessary to report the patient’s address. “Patient’s Telephone” does not exist in 4010A1 or 5010A1. The NUCC recommends that the phone number not be reported. For Workers’ Compensation and Other Property and Casualty Claims: If required by a payer to report a telephone number, do not use a hyphen or space as a separator within the telephone number. Description: The “Patient’s Address” refers to the patient’s permanent residence. A temporary address should not be used. Field Specification: This field allows for the entry of the following: 28 characters for street address, 24 characters for city, 3 characters for state, 12 characters for ZIP code, 3 characters for area code, and 10 characters for phone number. REQUIRED FIELD Item Number 6 Title: Patient Relationship to Insured Instructions: Enter an X in the correct box to indicate the patient’s relationship to insured when Item Number 4 is completed. Only one box can be marked. Provider Manual 2013 94 Description: The “Patient Relationship to Insured” refers to how the patient is related to the insured. “Self” would indicate that the insured is the patient. “Spouse” would indicate that the patient is the husband or wife or qualified partner as defined by the insured’s plan. “Child” would indicate that the patient is the minor dependent as defined by the insured’s plan. “Other” would indicate that the patient is other than the self, spouse, or child, which may include employee, ward, or dependent as defined by the insured’s plan. Field Specification: This field allows for entry of 1 character in any box within the field. REQUIRED FIELD Item Number 7 Title: Insured’s Address (multiple fields) Instructions: Enter the insured’s address and telephone number. If Item Number 4 is completed then this field should be completed. The first line is for the street address; the second line, the city and state; the third line, the ZIP code and phone number. Do not use punctuation (i.e., commas, periods) or other symbols, in the address. When entering a 9-digit ZIP code, include the hyphen. If reporting a foreign address, contact payer for specific reporting instructions. “Insured’s Telephone” does not exist in 4010A1 or 5010A1. The NUCC recommends that the phone number not be reported. For Workers Compensation Claims: Enter the address of the employer. For Other Property & Casualty Claims: Enter the address of the insured noted in Item Number 4. For Workers’ Compensation and Other Property and Casualty Claims: If required by a payer to report a telephone number, do not use a hyphen or space as a separator within the telephone number. Description: The “Insured’s Address” refers to the insured’s permanent residence, which may be different from the patient’s address in Item Number 5. Field Specification: This field allows for the entry of the following: 29 characters for street address, 23 characters for city, 4 characters for state, 12 characters for ZIP code, 3 characters for area code, and 10 characters for phone number. SITUATIONAL FIELD Provider Manual 2013 95 Item Number 8 Title: Patient Status Instructions: “Patient Status” does not exist in 4010A1 or 5010A1. The NUCC recommends that this field not be used. If required by a payer to report, enter an X in the box for the patient’s marital status, and for the patient’s employment or student status. Only one box on each line can be marked. Description: The “Patient Status” indicates the patient’s marital and employment status. “Employed” would indicate that the patient has a job. Field Specification: This field allows for entry of 1 character in any box within the field. SITUATIONAL FIELD Item Number 9 Title: Other Insured’s Name Instructions: If Item Number 11d is marked, complete fields 9 and 9a-d, otherwise leave blank. When additional group health coverage exists, enter other insured’s full last name, first name, and middle initial of the enrollee in another health plan if it is different from that shown in Item Number 2. If the insured uses a last name suffix (e.g., Jr, Sr) enter it after the last name, and before the first name. Titles (e.g., Sister, Capt, Dr) and professional suffixes (e.g., PhD, MD, Esq) should not be included with the name. Use commas to separate the last name, first name, and middle initial. A hyphen can be used for hyphenated names. Do not use periods within the name. Description: The “Other Insured’s Name” indicates that there is a holder of another policy that may cover the patient. Field Specification: This field allows for the entry of 28 characters. SITUATIONAL FIELD Provider Manual 2013 96 Item Number 9a Title: Other Insured’s Policy or Group Number Instructions: Enter the policy or group number of the other insured. Do not use a hyphen or space as a separator within the policy or group number. Description: The “Other Insured’s Policy or Group Number” identifies the policy or group number for coverage of the insured as indicated in Item Number 9. Field Specification: This field allows for the entry of 28 characters. SITUATIONAL FIELD Item Number 9b Title: Other Insured’s Date of Birth, Sex Instructions: “Other Insured’s Date of Birth, Sex” does not exist in 4010A1 or 5010A1. The NUCC recommends that this field not be used. If required by payer to report, enter the 8-digit date of birth (MM│DD│CCYY) of the other insured and an X to indicate the sex of the other insured. Only one box can be marked. If gender is unknown, leave blank. Description: The “Other Insured’s Date of Birth, Sex” (gender) identifies the birth date and gender of the insured as indicated in Item Number 9. Field Specification: This field allows for the entry of the following: 2 characters under MM, 2 characters under DD, 4 characters under YY, and 1 character in either box. SITUATIONAL FIELD Provider Manual 2013 97 Item Number 9c Title: Employer’s Name or School Name Instructions: “Employer’s Name or School Name” does not exist in 4010A1 or 5010A1. The NUCC recommends that this field not be used. If required by a payer to report, enter the name of the other insured’s employer or school. Description: The “Employer’s Name or School Name” identifies the name of the employer or school attended by the other insured as indicated in Item Number 9. Field Specification: This field allows for the entry of 28 characters. SITUATIONAL FIELD. Item Number 9d Title: Insurance Plan Name or Program Name Instructions: Enter the other insured’s insurance plan or program name. Description: The “Insurance Plan Name or Program Name” identifies the name of the plan or program of the other insured as indicated in Item Number 9. Field Specification: This field allows for the entry of 28 characters. SITUATIONAL FIELD. Provider Manual 2013 98 Item Numbers 10a–10c Title: Is Patient’s Condition Related To: Instructions: When appropriate, enter an X in the correct box to indicate whether one or more of the services described in Item Number 24 are for a condition or injury that occurred on the job or as a result of an automobile or other accident. Only one box on each line can be marked. The state postal code where the accident occurred must be reported, if “YES” is marked in 10b for “Auto Accident.” Any item marked “YES” indicates there may be other applicable insurance coverage that would be primary, such as automobile liability insurance. Primary insurance information must then be shown in Item Number 11. Description: This information indicates whether the patient’s illness or injury is related to employment, auto accident, or other accident. “Employment” (current or previous) would indicate that the condition is related to the patient’s job or workplace. “Auto Accident” would indicate that the condition is the result of an automobile accident. “Other Accident” would indicate that the condition is the result of any other type of accident. Field Specification: This field allows for the entry of the following: 1 character in either box per each line and 2 characters in the Place/State field SITUATIONAL FIELD. Item Number 10d Title: Reserved for Local Use Instructions: Please refer to the most current instructions from the applicable public or private payer regarding the use of this field. When required by payers to provide a sub-set of Condition Provider Manual 2013 99 Codes approved by the NUCC, enter the Condition Code in this field. The Condition Codes approved for use on the 1500 Claim Form are available at www.nucc.org under Code Sets. For Workers Compensation Claims: Condition Codes are required when submitting a bill that is a duplicate or an appeal. (Original Reference Number must be entered in Box 22 for these conditions). Note: Do not use Condition Codes when submitting a revised or corrected bill. Field Specification: This field allows for the entry of 19 characters. SITUATIONAL FIELD. Item Number 11 Title: Insured’s Policy, Group, or FECA Number Instructions: Enter the insured’s policy or group number as it appears on the insured’s health care identification card. If Item Number 4 is completed, then this field should be completed. Do not use a hyphen or space as a separator within the policy or group number. For Workers Compensation and Other Property & Casualty Claims: Required if known. Enter Workers’ Compensation or Property & Casualty Claim Number assigned by the payer. Description: The “Insured’s Policy, Group, or FECA Number” refers to the alphanumeric identifier for the health, auto, or other insurance plan coverage. For worker’s compensation claims the workers compensation carrier’s alphanumeric identifier would be used. The FECA number is the 9-digit alphanumeric identifier assigned to a patient claiming work-related condition(s) under the Federal Employees Compensation Act 5 USC 8101. Field Specification: This field allows for the entry of 29 characters. SITUATIONAL FIELD. Item Number 11a Title: Insured’s Date of Birth, Sex Instructions: Enter the 8-digit date of birth (MM | DD | CCYY) of the insured and an X to indicate the sex of the insured. Only one box can be marked. If gender is unknown, leave blank. Provider Manual 2013 100 Description: The “Insured’s Date of Birth, Sex” (gender) refers to the birth date and gender of the insured as indicated in Item Number 1a. Field Specification: This field allows for the entry of the following: 2 characters under MM, 2 characters under DD, 4 characters under YY, and 1 character in either box. REQUIRED FIELD. Item Number 11b Title: Employer’s Name or School Name Instructions: “Employer’s Name or School Name” does not exist in 4010A1 or 5010A1. The NUCC recommends that this field not be used. If required by payer to report, enter the name of the insured’s employer or school. Description: The insured’s “Employer’s Name or School Name” refers to the name of the employer or school attended by the insured as indicated in Item Number 1a. Field Specification: This field allows for the entry of 29 characters. SITUATIONAL FIELD Item Number 11c Title: Insurance Plan Name or Program Name Instructions: Enter the “Insurance Plan or Program Name” of the insured. Some payers require an identification number of the primary insurer rather than the name in this field. Description: The “Insurance Plan Name or Program Name” refers to the name of the plan or program of the insured as indicated in Item Number 1a. Field Specification: This field allows for the entry of 29 characters. SITUATIONAL FIELD Provider Manual 2013 101 Item Number 11d Title: Is there another Health Benefit Plan? Instructions: When appropriate, enter an X in the correct box. If marked "YES", complete 9 and 9a–d. Only one box can be marked. Description: "Is there another health benefit plan" indicates that the patient has insurance coverage other than the plan indicated in Item Number 1. Field Specification: This field allows for the entry of 1 character in either box. SITUATIONAL FIELD Item Number 12 Title: Patient’s or Authorized Person’s Signature Instructions: Enter “Signature on File,” “SOF,” or legal signature. When legal signature, enter date signed in 6-digit format (MMDDYY) or 8-digit format (MMDDCCYY Description: The “Patient’s or Authorized Person’s Signature” indicates there is an authorization on file for the release of any medical or other information necessary to process and/or adjudicate the claim. Field Specification: Use the space available to enter signature/information and date. REQUIRED FIELD NOTE: Claims with missing information on this field will be returned to the provider as non processable claim. The provider must submit the corrected claim along with the nonprocessable letter within the time frame establishes by the Prompt Payment Law of Puerto Rico. Provider Manual 2013 102 Item Number 13 Title: Insured’s or Authorized Person’s Signature Instructions: Enter “Signature on File,” “SOF,” or legal signature. Description: The “Insured’s or Authorized Person’s Signature” indicates that there is a signature on file authorizing payment of medical benefits. Field Specification: Use the space available to enter signature/information. REQUIRED FIELD NOTE: Claims with missing information on this field will be returned to the provider as non processable claim. The provider must submit the corrected claim along with the nonprocessable letter within the time frame establishes by the Prompt Payment Law of Puerto Rico. ITEMS 14–33: PROVIDER OR SUPPLIER INFORMATION Item Number 14 Title: Date of Current Illness, Injury, Pregnancy Instructions: Enter the 6-digit (MM | DD | YY) or 8-digit (MM | DD | CCYY) date of the first date of the present illness, injury, or pregnancy. For pregnancy, use the date of the last menstrual period (LMP) as the first date. Description: The “Date of Current Illness, Injury and Pregnancy” refers to the first date of onset of illness, the actual date of injury, or the LMP for pregnancy. Field Specification: This field allows for the entry of the following: 2 characters under MM, 2 characters under DD, and 4 characters under YY. SITUATIONAL FIELD Provider Manual 2013 103 Item Number 15 Title: If Patient Has Had Same or Similar Illness Instructions: Enter the first date the patient had the same or a similar illness. Enter the date in the 6-digit format (MM | DD | YY) or 8-digit format (MM | DD | CCYY). Previous pregnancies are not a similar illness. If required by payer to report, enter the first date the patient had the same or a similar illness. Enter the date in the 6-digit format (MM | DD | YY) or 8-digit format (MM | DD | CCYY). Previous pregnancies are not a similar illness. Description: A patient having had same or similar illness would indicate that the patient had a previously related condition. If a post stabilization service the provider should indicate the date of the previous emergency services provided to the patient. Field Specification: This field allows for the entry of the following: 2 characters under MM, 2 characters under DD, and 4 characters under YY. SITUATIONAL FIELD Item Number 16 Title: Dates Patient Unable to Work in Current Occupation Instructions: If the patient is employed and is unable to work in current occupation, a 6-digit (MM | DD | YY) or 8-digit (MM | DD | CCYY) date must be shown for the "from–to" dates that the patient is unable to work. An entry in this field may indicate employment-related insurance coverage. Description: “Dates Patient Unable to Work in Current Occupation” refers to the time span the patient is or was unable to work. Field Specification: This field allows for the entry of the following in each of the date fields: 2 characters under MM, 2 characters under DD, and 4 characters under YY. SITUATIONAL FIELD Provider Manual 2013 104 Item Number 17 Title: Name of Referring Provider or Other Source Instructions: Enter the name (First Name, Middle Initial, and Last Name) and credentials of the professional who referred, ordered, or supervised the service(s) or supply (ies) on the claim. If multiple providers are involved, enter one provider using the following priority order: 1. Referring Provider 2. Ordering Provider 3. Supervising Provider Do not use periods or commas within the name. A hyphen can be used for hyphenated names. Description: The name is the referring provider, ordering provider, or supervising provider who referred, ordered, or supervised the service(s) or supply (ies) on the claim. Field Specification: This field allows for the entry of 26 characters. SITUATIONAL FIELD Item Number 17a and 17b (split field) Title 17a: Other ID# Instructions 17a: The Other ID number of the referring, ordering, or supervising provider is reported in 17a in the shaded area. The qualifier indicating what the number represents is reported in the qualifier field to the immediate right of 17a. Description: The non-NPI ID number of the referring, ordering, or supervising provider refers to the unique identifier of the professional or to the provider designated taxonomy code. Field Specification: This field allows for the entry of 2 characters in the qualifier field and 17 characters in the Other ID# field. SITUATIONAL FIELD Provider Manual 2013 105 Title 17b: NPI # Instructions 17b: Enter the NPI number of the referring, ordering, or supervising provider in Item Number 17b. Description: The NPI number refers to the HIPAA National Provider Identifier number. Field Specification: This field allows for the entry of a 10-digit NPI number SITUATIONAL FIELD. NOTE: If field # 17 is completed, then field #17b must be completed also. Item Number 18 Title: Hospitalization Dates Related to Current Services Instructions: Enter the inpatient 6-digit (MM | DD | YY) or 8-digit (MM | DD | CCYY) hospital admission date followed by the discharge date (if discharge has occurred). If not discharged, leave discharge date blank. This date is when a medical service is furnished as a result of, or subsequent to, a related hospitalization. Description: The “Hospitalization Dates Related to Current Services” refers to an inpatient stay and indicates the admission and discharge dates associated with the service(s) on the claim. Field Specification: This field allows for the entry of the following in each of the date fields: 2 characters under MM, 2 characters under DD, and 4 characters under YY. SITUATIONAL FIELD Provider Manual 2013 106 Item Number 19 Title: Reserved for local use Instructions: Please refer to the most current instructions from the applicable public or private payer regarding the use of this field. Some payers ask for certain identifiers in this field. If identifiers are reported in this field, enter the appropriate qualifiers describing the identifier. Do not enter a space, hyphen, or other separator between the qualifier code and the number. This field is used to supply any additional supporting information related to the Claim. First+Plus will advise provider for the use of this field when deem necessary. Item Number 20 Title: Outside Lab? $Charges Instructions: Complete this field when billing for purchased services by entering an X in “YES.” A “YES” mark indicates that the reported service was provided by an entity other than the billing provider (for example, services subject to Medicare’s anti-markup rule). A “NO” mark or blank indicates that no purchased services are included on the claim. If “Yes” is annotated, enter the purchase price under “$Charges” and complete Item Number 32. Each purchased service must be reported on a separate claim form as only one charge can be entered. When entering the charge amount, enter the amount in the field to the left of the vertical line. Enter number right justified to the left of the vertical line. Enter 00 for cents if the amount is a whole number. Do not use dollar signs, commas, or a decimal point when reporting amounts. Negative dollar amounts are not allowed. Leave the right-hand field blank. Description: “Outside lab? $Charges” reports the costs related to services rendered by an independent provider as indicated in Item Number 32. Field Specification: This field allows for the entry of the following: 1 character in either box in the Outside Lab area and 8 characters to the left of the vertical line in the $Charges area. SITUATIONAL FIELD Provider Manual 2013 107 Item Number 21 Title: Diagnosis or Nature of Illness or Injury (relate items 1, 2, 3, or 4 to 24E by line) Instructions: Enter the patient’s diagnosis/condition. Relate lines 1, 2, 3, 4 to the lines of service in 24E by line number (Diagnosis Pointer). Use the highest level of specificity. Do not provide narrative description in this field. Description: The “Diagnosis or Nature of Illness or Injury” refers to the sign, symptom, complaint, or condition of the patient relating to the service(s) on the claim. Field Specification: This field allows for the entry of 3 characters prior to the period, 1 character above the period, and 4 characters after the period in each of the four line areas. REQUIRED FIELD. At least a principal diagnosis must be reported on field #1. NOTE: Claims with missing, invalid or incomplete information on this field will be returned to the provider as non processable claim. The provider must submit the corrected claim along with the non-processable letter within the time frame establishes by the Prompt Payment Law of Puerto Rico. Note 1: We encourage the reporting of any additional diagnosis beyond the four spaces allow on the CMS 1500 Claim form. In order to comply with this, please specify the diagnosis order number such as 5, 6, 7, 8, etc., and enter the appropriate additional diagnosis code. Please be aware that you must code the diagnosis to the highest level of specificity. The ICD-9CM coding book has the information related to diagnosis that requires a four or fifth digit, as well as the identification of diagnosis that cannot be used as principal diagnosis. Please refer to the symbols and description use on the ICD-9-CM coding books. Note 2: The Centers for Medicare and Medicaid Services along with the Uniform Billing Committee has approved a new CMS 1500 Claim Form that will be release in a near future. The new CMS 1500 claim form will allow the reporting of more than four diagnoses on field #21. This field has been expanded to accommodate the ICD-10 diagnoses codes which are in schedule for implementation on October 1st, 2014. Providers must start getting ready for this major change on coding of diagnosis. Note 3: When the new CMS 1500 become available, FIRST+PLUS will inform the providers of the changes on billing requirements according with the new parameters determine by CMS and the UNIFORM BILLING COMMITTEE. Provider Manual 2013 108 Item Number 22 Title: Medicaid Resubmission and/or Original Reference Number Instructions: List the original reference number for resubmitted claims. Please refer to the most current instructions from the applicable public or private payer regarding the use of this field (e.g., code). Description: Medicaid resubmission means the code and original reference number assigned by the destination payer or receiver to indicate a previously submitted claim or encounter. Field Specification: This field allows for the entry of 11 characters in the Code area and 18 characters in the Original Ref. No. area. SITUATIONAL FIELD. Note: If the provider is submitting an adjustment request/appeal the field ORIGINAL REF NO must be filled with the unique Claim Number assigned by the Plan for each specific claim, which can be found on the Explanation of Payment. Item Number 23 Title: Prior Authorization Number Instructions: Enter any of the following: prior authorization number or referral number, mammography pre-certification number, or Clinical Laboratory Improvement Amendments (CLIA) number, as assigned by the payer for the current service. Do not enter hyphens or spaces within the number. For Workers Compensation and Other Property & Casualty Claims: Required when prior authorization, referral, concurrent review, or voluntary certification was received. Description: The “Prior Authorization Number” refers to the payer assigned number authorizing the service(s). Provider Manual 2013 109 Field Specification: This field allows for the entry of 29 characters. Note 1: The pre-authorization of a service does not guarantee the payment. The payment is subject to the member’s eligibility, and his/her benefit package at the time the service is rendered. Remember that the authorized services are subject to the application of payment rules, coding guidelines according to CMS, AMA regulations as well as any rules established by FIRST+PLUS. Note 2: If service requires an authorization the number must be included with the claim. SITUATIONAL FIELD. SECTION 24 Shaded area Title: Shaded section for supplemental information Instructions: Supplemental information can only be entered with a corresponding, completed service line. The six service lines in section 24 have been divided horizontally to accommodate submission of both the NPI and another/proprietary identifier and to accommodate the submission of supplemental information to support the billed service. The top area of the six service lines is shaded and is the location for reporting supplemental information. It is not intended to allow the billing of 12 lines of service. The supplemental information is to be placed in the shaded section of 24A through 24G as defined in each Item Number. Providers must verify requirements for this supplemental information with the payer. Field Specifications: The shaded area of lines 1 through 6 allow for the entry of 61 characters from the beginning of 24A to the end of 24G. Situational Field Provider Manual 2013 110 Item Number 24A Title: Date(s) of Service [lines 1–6] Instructions: Enter date(s) of service, both the “From” and “To” dates. If there is only one date of service, enter that date under “From” and also on the “To” field. Note: The provider must enter both “from” and “through “dates, regardless if both are the same date. Claims with missing “through” service dates will be returned to the providers as non-processable claims. The number of days must correspond to the number of units in 24G. Description: “Date(s) of Service” indicate the actual month, day, and year the service(s) was provided. Field Specification: This field allows for the entry of the following in each of the unshaved date fields: 2 characters under MM, 2 characters under DD, and 2 characters under YY. REQUIRED FIELD Item Number 24B Title: Place of Service [lines 1–6] Instructions: In 24B, enter the appropriate two-digit code from the Place of Service Code list for each item used or service performed. The Place of Service Codes are available at: www.cms.gov/physicianfeesched/downloads/Websit e_POS_database.pdf Description: The “Place of Service” Code identifies the location where the service was rendered. Field Specification: This field allows for the entry of 2 characters in the unshaved area. Note: Only one Place of Service code is allowed on the CMS 1500. If you have rendered services for the same patient on different places of services, you must bill the services on separate CMS 1500 by the place of services code. (e.i you rendered services to a patient on both POS 11 (OFFICE) and 21 (inpatient), please send separate bills by place of service code for the same patient. REQUIRED FIELD Provider Manual 2013 111 Item Number 24C Title: EMG [lines 1–6] Instructions: Check with payer to determine if this element (emergency indicator) is necessary. If required, enter Y for "YES" or leave blank if "NO" in the bottom, unshaved area of the field. The definition of emergency would be either defined by federal or state regulations or programs, payer contracts. Field Specification: This field allows for the entry of 2 characters in the unshaved area. REQUIRED FIELD Item Number 24D Title: Procedures, Services, or Supplies [lines 1–6] Instructions: Enter the CPT or HCPCS code(s) and modifier(s) (if applicable) from the appropriate code set on effect for the date of service submitted on the claim. This field accommodates the entry of procedure code(s) must be shown without a narrative description. Invalid, deleted code for the service date, incomplete, missing or illegible codes will be denied to the provider. Provider must made the corrections and submit the same to First+Plus Claims Department within the time frame establish by Prompt Payment Law of Puerto Rico. Description: The “Procedures, Services or Supplies” refer to a listing of identifying codes for reporting medical services and procedures. Field Specification: This field allows for the entry of the following: 6 characters in the un-shaded area of the Provider Manual 2013 112 CPT/HCPCS field and four sets of 2 characters in the Modifier area. Note : CPT Category II Codes CPT Category II or CPT Codes that are developed through the CPT Editorial Panel for use in performance measurement serve to encode the quality action(s) described in a measure’s numerator. CPT II codes consist of five alphanumeric characters in a string, ending with the letter “F”. We encourage the reporting of these quality measure CPT codes. REQUIRED FIELD Item Number 24E Title: Diagnosis Pointer [lines 1–6] Instructions: In 24E, enter the diagnosis code reference number (pointer) as shown in Item Number 21 to relate the date of service and the procedures performed to the correspondent diagnosis. When multiple diagnoses are related to one service, the reference number for the primary diagnosis should be listed first, other applicable diagnosis reference numbers should follow. The reference number(s) should be a 1, or a 2, or a 3, or a 4; or multiple numbers as explained. (ICD-9-CM diagnosis codes must be entered in Item Number 21 only. Do not enter them in 24E.) Enter numbers left justified in the field. Do not use commas between the numbers. Description: The “Diagnosis Pointer” refers to the line number from Item Number 21 that relates to the reason the service(s) was performed. There are services that are related to specific conditions in order to be reimbursable. Therefore, the provider must be aware that any related diagnosis indicated on field number 21 to a service code on field number 24d must contain the pointer associated to the service. Field Specification: This field allows for the entry of 4 characters in the unshaded area. Provider Manual 2013 113 REQUIRED FIELD NOTES: Common errors usually observed are the following: -Providers indicates a pointer number that Should be associated to a diagnosis code on field 21, but there is not diagnosis code on that Position number of field 21 (e.i- provider Indicates a pointer 4 when there is not a Diagnosis code on position 4 of field #21) -Provider enters the ICD-9-cm code on this field Instead of the pointer -Providers leave the field blank Failure to complete this field will result on a nonProcessable claim which will be returned to the provider for correction. Item Number 24F Title: $ Charges [lines 1–6] Instructions: Enter the charge for each listed service. Enter number right justified in the dollar area of the field. Do not use commas when reporting dollar amounts. Negative dollar amounts are not allowed. Dollar signs should not be entered. Enter 00 in the cents area if the amount is a whole number. Description: “$Charges” refers to the total billed amount for each service line. Field Specification: This field allows for the entry of 6 characters to the left of the vertical line and 2 characters to the right of the vertical line in the unshaved area. REQUIRED FIELD Item Number 24G Title: Days or Units [lines 1–6] Instructions: Enter the number of days or units. This field is most commonly used for multiple visits, units of supplies, anesthesia minutes, or oxygen volume. If only one service is performed, the numeral 1 must be entered. Enter numbers right justified in the field. No leading zeros are required. If reporting a fraction of a unit, use the decimal point. Provider Manual 2013 114 Anesthesia services must be reported as minutes. Description: “Days or Units” refers to the number of days corresponding to the dates entered in 24A or units as defined in CPT or HCPCS coding manual(s). Field Specification: This field allows for the entry of 3 characters in the un-shaded area. REQUIRED FIELD Item Number 24H Title: EPSDT/Family Plan [lines 1–6] Instructions: For Early & Periodic Screening, Diagnosis, and Treatment related services, enters the response in the shaded portion of the field as follows: If there is no requirement (e.g., state requirement) to report a reason code for EPDST, enter Y for “YES” or N for “NO” only. Description: The “EPSDT/Family Plan” identifies certain services that may be covered under some state plans. Field Specification: This field allows for the entry of 1 character in the un-shaded area and 2 characters in the shaded area. SITUATIONAL FIELD Item Number 24I Title: ID Qualifier [lines 1–6] Instructions: Enter in the shaded area of 24I the qualifier identifying if the number is a non-NPI. The shaded area. Other ID# of the rendering provider is reported in 24J Description: Enter the non NPI number on this field Field Specification: This field allows for the entry of a 2 character qualifier in the shaded area. SITUATIONAL FIELD Provider Manual 2013 115 Item Number 24J Title: Rendering Provider ID # [lines 1–6] Instructions: The individual rendering the service is reported in 24J. Enter the NPI number in the unshaved area of the field. The Rendering Provider is the person or company who rendered or supervised the care. Report the Identification Number in 24J ONLY when it is different from data recorded in items 33a. Enter numbers left justified in the field. Remember you only report this field when the rendering and billing providers NPI are different. Otherwise do not report when the rendering and billing NPI are the same. Description: The NPI ID number of the rendering provider refers to the unique identifier of the provider. Field Specification: This field allows for the entry of a 10 digit NPI number of the unshaved area. REQUIRED FIELD NOTES: COMMON BILLING ERRORS - - Provider Manual 2013 Scenario #1 Combination of rendering provider and billing provider does not match the contracting arrangement on file. This usually occurs when the billing provider is a group/corporation and there are either one or others providers under that group. Under this specific set-up the rendering provider must be specify on field 24J. That rendering provider should be included under the group contract. If a claim is returned as non processable or deny for this issue you should contact Providers Department Credentialing Unit to verify the contracting arrangement on file Scenario #2 Providers has a contract arrangement as a group/corporation and bills as individual provider. You should contact providers Department Credentialing Unit to verify your contracting arrangements. 116 Item Number 25 Title: Federal Tax ID Number Instructions: Enter the “Federal Tax ID Number” (employer identification number or Social Security number) of the Billing Provider identified in Item Number 33/33a. This is the tax ID number intended to be used for 1099 reporting purposes. Enter an X in appropriate box to indicate which number is being reported. Only one box can be marked. Description: The “Federal Tax ID Number” refers to the unique identifier assigned by a federal or state agency. Field Specification: This field allows for the entry of 15 characters for the “Federal Tax ID Number” and 1 character in either box. REQUIRED FIELD Item Number 26 Title: Patient’s Account No. Instructions: Enter the patient’s account number assigned by the provider of service’s or supplier’s accounting system. Description: The “Patient’s Account No.” refers to the identifier assigned by the provider. Field Specification: This field allows for the entry of 14 characters. If you report this number on your claim form the same will be reported on the EOP (Explanation of payment) for the identification purposes of your account. REQUIRED FIELD Item Number 27 Title: Accept Assignment? Provider Manual 2013 117 Instructions: Enter an X in the correct box. Only one box can be marked. Description: The accept assignment indicates that the provider agrees to accept assignment under the terms of the payer’s program. Field Specification: This field allows for the entry of 1 character in either box. REQUIRED FIELD Item Number 28 Title: Total Charge Instructions: Enter total charges for the services (i.e., total of all charges in 24F). Enter number right justified in the dollar area of the field. Do not use commas when reporting dollar amounts. Negative dollar amounts are not allowed. Dollar signs should not be entered. Enter 00 in the cents area if the amount is a whole number. Description: The “Total Charge” indicates the total billed amount for all services entered in 24F (lines 1–6). Field Specification: This field allows for the entry of 7 characters to the left of the vertical line and 2 characters to the right of the vertical line. REQUIRED FIELD Item Number 29 Title: Amount Paid Instructions: Enter total amount the patient and/or other payers paid on the covered services only. Enter number right justified in the dollar area of the field. Do not use commas when reporting dollar amounts. Negative dollar amounts are not allowed. Dollar signs should not be entered. Enter 00 in the cents area if the amount is a whole number. Description: The “Amount Paid” refers to the payment received from the patient or other payers. Provider Manual 2013 118 Field Specification: This field allows for the entry of 6 characters to the left of the vertical line and 2 characters to the right of the vertical line. REQUIRED FIELD Item Number 30 Title: Balance Due Instructions: If required by a payer to report, enter total amount due. Enter number right justified in the dollar area of the field. Do not use commas when reporting dollar amounts. Negative dollar amounts are not allowed. Dollar signs should not be entered. Enter 00 in the cents area if the amount is a whole number. Field Specification: This field allows for the entry of 6 characters to the left of the vertical line and 2 characters to the right of the vertical line. SITUATIONAL FIELD Item Number 31 Title: Signature of Physician or Supplier Including Degrees or Credentials Instructions: Enter the legal signature of the practitioner or supplier, signature of the practitioner or supplier representative, “Signature on File,” or “SOF.” Enter either the 6-digit date (MM | DD | YY), 8-digit date (MM | DD |CCYY), or alphanumeric date (e.g., January 1, 2003) the form was signed. Description: The “Signature of the Physician or Supplier Including Degrees or Credentials” refers to the authorized or accountable person and the degree, credentials, or title. Provider Manual 2013 119 Field Specification: Use the space available to enter signature and date. REQUIRED FIELD NOTE: Claims with incomplete, no legible or blank field will be returned as non-processable. You must return the corrected claim along with the non-processable letter within the time frame establish by the Prompt Payment Law of Puerto Rico. Item Number 32, 32a, and 32b Title 32: Service Facility Location Information Instructions: Enter the name, address, city, state, and zip code of the location where the services were rendered. Providers of service (namely physicians) must identify the supplier’s name, address, zip code, and NPI number when billing for purchased diagnostic tests. When more than one supplier is used, a separate 1500 Claim Form should be used to bill for each supplier. Enter the name and address information in the following format: 1st Line – Name 2nd Line – Address 3rd Line – City State and ZIP Code Do not use punctuation (i.e., commas, periods) or other symbols in the address (e.g., 123 N Main Street 101 instead of 123 N. Main Street, #101). Enter a space between town name and state code; do not include a comma. When entering a 9-digit ZIP code, include the hyphen. Field Specification: This field allows for the entry of three lines of 26 characters each in the Service Facility Location Information area. REQUIRED FIELD Provider Manual 2013 120 Item Number 32a Title 32a: NPI# Instructions: Enter the NPI number of the service facility location in 32a. Description: The NPI number refers to the HIPAA National Provider Identifier number. Field Specification: This field allows for the entry of 10 characters. REQUIRED FIELD Item Number 32b Title 32b: Other ID# Instructions: Enter the two digit qualifier identifying the non-NPI number followed by the ID number. Do not enter a space, hyphen, or other separator between the qualifier and number. Description: The non-NPI number of the service facility refers to the unique identifier of the professional or to the provider designated taxonomy code. Field Specification: This field allows for the entry of 14 characters in 32b. SITUATIONAL FIELD Provider Manual 2013 121 Item Number 33 Title 33: Billing Provider Info & Ph. # Instructions: Enter the provider’s or supplier’s billing name, address, zip code, and phone number. The phone number is to be entered in the area to the right of the field title. Enter the name and address information in the following format: 1st Line – Name 2nd Line – Address 3rd Line – City State and ZIP Code Item 33 identifies the provider that is requesting to be paid for the services rendered and should always be completed. Description: The billing provider’s or supplier’s billing name, address, zip code, and phone number refers to the billing office location and telephone number of the provider or supplier. Field Specification: This field allows for the entry of the following: 3 characters for area code, 9 characters for phone number, and three lines of 29 characters each in the Billing Provider Info area. REQUIRED FIELD Item Number 33a Title 33a: NPI# Instructions: Enter the NPI number of the BILLING PROVIDER in 33a. This field must be always entered. Provider Manual 2013 122 Description: The NPI number refers to the HIPAA National Provider Identifier number. Field Specification: This field allows for the entry of 10 characters. REQUIRED FIELD NOTES: Common errors: -Providers submit other identifiers such as Tax ID/SSI instead of the Billing Provider NPI -Providers submit incorrect combination of billing and rendering providers Claims with errors on this field will be rejected as non-processable claim. Provider must submit a corrected claim along with the non- processable letter within the timeframe establish by The Prompt Payment Law of Puerto Rico. If questions arise due to nonprocessable or denied claims contact Providers Department Services at the telephone number specified on this manual. Item Number 33b Title 33b: Other ID# Instructions: Enter the two digit qualifier identifying the non-NPI number followed by the ID number. Do not enter a space, hyphen, or other separator between the qualifier and number. Description: The non-NPI number of the billing provider refers to the unique identifier of the provider or to the provider designated taxonomy code. Field Specification: This field allows for the entry of 17 characters in 33b. SITUATIONAL FIELD Provider Manual 2013 123 UB-04 (CMS-1450) The CMS-1450- (UB-04) is used for the submission of institutional services such as: Hospital Inpatient Services Hospital Outpatient Services Home Health Services Skilled Nursing Services Ambulatory Surgical Centers among others The National Uniform Billing Committee (nubc.org) was appointed by HIPAA as Designated Standards Maintenance Organization (DSMO) for the Uniform Bill The NUBC is responsible for the maintenance of the Official UB-04 Data Specifications Manual. UB-04 was developed and approved for use beginning in 2007 With the implementation of UB-04 on 2007 some of the fields and codes were changed. The Uniform Billing was developed with the purpose of assist the providers on produce a clean, accurate, and complete claim. Provider Manual 2013 124 The following fields are required UB-04 Health Insurance Claim Form: Provider Manual 2013 125 UB-04 FIELDS DESCRIPTION FL 1- Billing Provider Name, address and Telephone Number The minimum entry is the provider name, city, State, and Zip Code. The post office box number or street name, and number may be included. The State may be abbreviated using standard post office abbreviations. Five or nine digits Zip Codes are acceptable. 1 REQUIRED FL-2 Billing Provider’s Designated Pay-to-Name, Address, and Secondary Identification Fields It should be completed if the provider designated to receive the payment is different that the provider specified on Field Locator 1. 2 SITUATIONAL FL-3ªPatient Control Number The patient’s unique alpha-numeric number assigned by the provider to facilitate retrieval of individual financial records and posting payments. Will be posted on the EOP/Remittance Advice, ANSI 835 if providers submit the same on the claim. 3a.Pt control number REQUIRED. Provider Manual 2013 126 FL-3bMedical/Health Record Number The number assigned to the patient’s medical/health record by the provider. 3b Medical/Health Record Number REQUIRED FL-4 Type of Bill This is a four-digit alphanumeric code which include three specific pieces of information. Indicates the facility where the service were rendered This is a four digit number which must be submitted by the provider accord- ing to the type of service performed. Code Structure: First Digit Second Digit Third Digit Fourth Digit - Leading Zero Type of facility Bill Classification Bill Frequency Codes are available from the NUBC (National Uniform Billing Committee) at www.nubc.org via the NUBC’s Official UB-04 Data Specifications Manual. 4 TYPE REQUIRED OF BILL Examples: First Digit: The first digit will always be zero. (0). Second Digit (Type of Facility) 1. Hospital 2. Skilled Nursing Facility 3. Home Health Facility Provider Manual 2013 127 4. Religious Nonmedical Health Care Institutions (RNHCI)-Hospital Inpatient 5. Reserved for Assignment by the NUBC 6. Intermediate Care 7. Clinic (requires special reporting information for the third digit) 8. Special Facility or ASC surgery (requires special reporting for the third digit) 9. Reserved for Assignment by the NUBC Third Digit (Bill Classification - (except Clinics and Special Facilities) 1. Inpatient Including Medicare Part A 2. Inpatient Medicare Part B Only (Includes HHA Visits Under A Part B Plan Of Treatment) 3. Outpatient – (Includes HHA Visits Under A Part A Plan Of Treatment Includ- ing DME Under Part A) 4. Laboratory Services Provided To Non-Patients, Or Home Health Not Under A Plan Of Treatment 5. Intermediate Care Level I 6. Intermediate Care Level II 7. Reserved For Assignment By The NUBC 8. Swing Beds 9. Reserved For Assignment By The NUBC Third Digit – Clinics Only 071X- Rural health Clinic (RHC) 072X- Clinic -Hospital Based or Independent Renal Dialysis Center 073X- Free-standing 074X-ORF –Outpatient Rehabilitation Facility 075 X-CORF-Comprehensive Outpatient Rehabilitation Facilities 076X-CMHC-Comprehensive mental Health Centers (partial hospitalizations program Service) Provider Manual 2013 128 077X- Federally Qualified Health Center (FQHC) 078X- Reserved for assignment by the NUBC 079X-Clinic –Other Third Digit (Classification for Other Facility Only) This coding structure can be used only when the second digit of the TOB indicates another facility (8). 081X - Hospice (Non-Hospital Based) 082X - Hospice (Hospital-Based) 083X - Ambulatory Surgery Center (ASC) Note: TOB code 083X does not apply to Hospital Outpatient claims. Instead, hospitals use TOB codes 013X, 014X or 012X as Appropriate to report outpatient services. 084X - Freestanding Birthing Center 085X – Critical Access Hospital 086X- Residential Facility (not used) 087X-088X- Reserved for Assignment by the NUBC 089X- Special Facility- Other (not used for Medicare) Fourth Digit (Bill Frequency) CODE STRUCTURE: 0XX0 Nonpayment/Zero Claim -This fourth digit is used to report non payment claims. - Is used to report to the payer a nonreimbursable period of Confinement or termination of care - Use this code when the provider does not expect a payment as a Provider Manual 2013 129 Result of submitting this bill -Use this code when the hospitalization is covered by worker’s Compensation (WC), automobile medical, no-fault insurance or Liability insurance or an employer group health plan (EGHP) 0XX1 Admit-Through –Discharge Claim -This frequency code represent an admit though discharge claim and is used to report the entire inpatient admission or outpatient course of treatment 0XX2 Interim-First Claim (Not Valid for PPS Claims) - This frequency code is used to indicate the first in a series of Claims to the same third-party payer for the same confinement or course of treatment 0XX3 Interim-continuing Claim (Not Valid for PPS Claims -This bill frequency code is used to indicate that a bill is one of a series of claims for the same confinement or course of treatment. In other words, the bill has been submitted previously and further bills are expected. 0XX4 Interim –Last Claim (Not valid for PPS Claims) -This is used to indicate that a bill is the last of a series of claims For the same confinement or course of treatment. 0XX5 Late Charges Only Claim -This code indicates that the provider is submitting charges after An admit-through discharge claim or last interim claim has been Submitted. This code is not intended to be used in lieu of an Provider Manual 2013 130 Adjustment or replacement claim. 0XX6 Reserved for Assignment by the NUBC 0XX7 Replacement of Prior Claim -This TOB code is used when a specific claim needs to be Restated in its entirety, except for the identifying information. The original claim is considered null and void, an Information on this bill completely replaces the previos Claim. 0XX8Void/Cancel of Prior Claim -This code indicates that this claim eliminates and cancels a Previously submitted claim. -A code OXX7 claim must be submitted to show the Corrected information. -In other words, this frequency code cannot be used Unless you have also submitted a 0XX7 claim 0XX9 Final Claim for a Home health PPS Episode -This code indicates the home health bill should be processed as A debit or credit adjustment to the initial HHPS bill. -This code is specific to home health and does not replace Frequency codes 7 or 8. -A claim for an episode billed with TOB code 0329 will be Processed as an adjustment to the RAP, and will trigger a full Or final episode payment under HHPPS. Provider Manual 2013 131 Example: -Admit through Discharge Claim (0XX1) -Interim (First Claim) (0XX2) -Interim (Continuing Claim –Not valid for PPS-DRG Claims) (0XX3) -Interim Last Claim (Not valid for PPS-DRG claims) (0XX4) -Late Charges Only Claim (0XX5) -Reserved for Assignment by the NUBC – (0XX6) -Replacement of Prior Claim – (0XX7) -Void/Cancel of a Prior Claim (0XX8) -Final Claim for a Home Health PPS Episode (0XX9) FOURTH DIGIT- Frequency of the Bill-FOR HOSPICE ONLY 0XXA-Admission/Election Notice 0XXB-Hospice/Termination/Revocation Notice 0XXC-Hospice Change of Provider Notice 0XXD-Hospice/Void/Cancel 0XXE-Hospice Change of Ownership Bill Type Code Samples: A) Claim with bill type (0111) 0 1 1 1 Leading 0, 2nd digit= hospital Third digit= Inpatient Part A Third Digit = Adm thru Discharge B) Claim with bill type (0131) 0 1 3 1 Leading 0, 2nd digit= hospital Third digit= Outpatient, Third Digit = Adm thru Discharge Provider Manual 2013 132 C) Claim with bill type (0322) 0 3 2 2 Leading 0, 2nd digit= Home Health, Third digit= Outpatient, Third Digit = 2 (First RAP claim) D) Claim with bill type (0329) 0 3 2 9 Leading 0, 2nd digit= Home Health, Third digit= Outpatient, Third Digit = 9 Final claim for a Home Health Treatment Episode OTHER BILL TYPES SAMPLES: 011X Hospital Inpatient (Part A) 012XHospital Inpatient Part B only. (Use this TOB to bill for covered ancillary services when the patient has Part B entitlement only or when Part A benefits are not payable or are exhausted) 013 X Hospital Outpatient- uses to bill outpatient services rendered in the emergency or other outpatient department. Single line item date of service for each revenue code is required) 014X Hospital Non Patient Laboratory Services - Single line item date of service for each revenue code is required) 021X SNF Inpatient 022X SNF Inpatient Part B only Provider Manual 2013 133 023X SNF Outpatient 032X Home Health inpatient (Part B Only) - It is used as a request for anticipated Payment (RAP) - Plan of treatment when the patient has both Part A and Part B entitlement 033X Home Health-outpatient /DME under Part A (Single line item date of service for Each revenue code is required) 034X Home Health not under a Plan of Treatment (Single line item date of service for Each revenue code is required) 071X Clinical Rural health 072X Hospital Based or Independent Renal Dialysis Center 073X Clinic-Freestanding (Effective April 1, 2010) 074X Clinic- Outpatient Rehabilitation Facility 075X Clinic- Comprehensive Outpatient Rehabilitation Facility 081X Non Hospital based hospice 082X Hospital Based Hospice 083X Special Facility- Ambulatory surgery Center (ASC) 085X Critical Access Hospital FL- 5 Federal Tax Number The format is NN-NNNNNNN. REQUIRED Provider Manual 2013 134 FL-6 Statement Covers Period From /Through The provider enters the beginning and ending dates of the period included on this bill in numeric fields (MMDDYY). 6 FROM through REQUIRED FL-7 Not used. FL-8 Patient’s Name/Patient ID a. Patient Contract Number b. Patient Name a b 3 REQUIRED FL-9 Patient’s Address The provider enters the patient’s last name, first name, and, if any, middle initial, along with patient ID (if different than the subscriber/insured’s ID) c. d. e. f. Street Name and Number Post Office Box Number City State g. ZIP code 9. Patient Address b a R c REQUIRED Provider Manual 2013 135 d e FL-10 Patient’s Birth Date The provider enters the month, day, and year of birth (MMDDCCYY) of patient. 10. BIRTHDATE REQUIRED FL-11 Patient’s Sex The provider enters an “M” (male) or an “F” (female). The patient’s sex is recorded at admission, outpatient Service, or start of care. 11. SEX REQUIRED FL-12 Admission/Start of Care Date Required For Inpatient and Home Health. The hospital enters the date the patient was admitted for inpatient care (MMDDYY). The HHA enters the same date of admission that was submitted on the RAP for the episode. 12. Date REQUIRED FL-13 Admission Hour For inpatient services indicate the hour in which the patient was admitted. 13. Admission Hour REQUIRED FOR INPATIENT only Provider Manual 2013 136 Code Structure: 01 02 03 04 05 06 07 08 09 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 12:00 (midnight)-12:59am 01:00-01:59 02:00-02:59 03:00-03:59 04:00-04:59 05:00-05:59 06:00-06:59 07:00-07:59 08:00-08:59 09:00-09:59 10:00-10:59 11:00-11:59 12:00 (noon)-12:59p.m. 01:00-01:59 02:00-02:59 03:00-03:59 04:00-04:59 05:00-05:59 06:00-06:59 07:00-07:59 08:00-08:59 09:00-09:59 10:00-10:59 11:00-11:59 FL-14 Type of Admission This field is required. This is the code indicating priority of this admission. 14. TYPE REQUIRED Coding Structure: 1. 2. 3. 4. 5. Emergency Urgent Elective Newborn Trauma Provider Manual 2013 137 6. 7. 8. 9. Reserved for Assignment by the NUBC Reserved for Assignment by the NUBC Reserved for Assignment by the NUBC Information Not available- This code should be used rarely, since the provider must indicate de type of admission of the patient FL-15 Point for Origin for Admission or Visit The provider enters the code indicating the source of the referral for this Admission or visit. 15. SRC REQUIRED This is a required field for inpatient and outpatient hospital, home health, inpatient SNF Coding Structure (for Emergency, Elective or other type of Admission): 123456789ABCDEFG- No healthcare Facility Point of Origin Clinic or Physician’s Office Reserved for assignment by the NUBC Transfer from a Hospital (Different Facility) Transfer from a Skilled Nursing Facility (SNF) or Intermediate Care Facility (ICF)or Assisted Living Facility (ALF) Transfer from Another HealthCare Facility Discontinued effective July 1, 2010 Court/Law Enforcement Information Not Available Reserved for assignment by the NUBC Discontinued effective July 1, 2010 Discontinued effective July 1, 2010 Transfer from One Distinct Unit of the Hospital to Another Distinct Unit of the same hospital resulting in a separate Claim to the Payer Transfer from Ambulatory Surgery Center Transfer from Hospice Facility Z Reserved for Assignment by the NUBC Coding Structure: NEWBORN 1. Discontinued 2. Discontinued 3. Discontinued 4. Discontinued 5- Born inside this hospital Provider Manual 2013 138 6- Born outside of this Hospital 7- 9 Reserved for Assignment by the NUBC FL-16 Discharge Hour 16 DHR SITUATIONAL First Plus requires that this information is provided only when there is a revenue code 0450 on form locator 42, on inpatient claims. FL-17 Patient Discharge Status 17 Stat REQUIRED The provider must submit the patient status code for all TYPE of claims CODING STRUCTURE 01- Discharge to Home or Self-Care (Routine Discharge) 02- Discharged/Transferred to a Short-Term General Hospital for Inpatient Care 03- Discharged/Transferred to SNF WITH Medicare Certification in Anticipation of Skilled Care 04- Discharged/Transferred to a Facility that Provides Custodial or Supportive Care 05- Discharged/Transferred to a Designated Cancer Center or Children’s Hospital 06- Discharged/Transferred to Home Under Care of Organized Home Health Service organization in anticipation of covered Skilled Care 07- Left against medical advice or discontinued care 08- Reserved for Assignment by the NUBC 09- Admitted as an inpatient to this hospital (if a patient is admitted before midnight of the third day following the day of an outpatient diagnostic service or service related to the reason for admission, the outpatient services are considered inpatient. Code 09 applies only to services that begin more than three days prior to the admission or were unrelated to the reason for admission) Provider Manual 2013 139 10- 19 Reserved for assignment by the NUBC 20- Expired 21- Discharged/transferred to Court/Law Enforcement 22-29 Reserved for Assignment by the NUBC 30- Still a patient (used on RAP bills for Home Health bill type 032X or 033X) 31-39 Reserved for Assignment by the NUBC 40- Expired at home 41- Expired in a Medical Facility - Hospice (valid only for Medicare and TRICARE hospice claims only-TOB (FL-4) 081x and 082X) 42- Expired, Place Unknown 43- Discharged/transferred to a Federal Health Care Facility 44-49 Reserved for Assignment by the NUBC 50-Discharged to Hospice-Home (in home hospice services) 51- Discharged to Hospice-Medical Facility (certified) Providing Hospice Level of Care 52-60 Reserved for Assignment by the NUBC 61- Discharged/Transferred within this institution to a Hospital Based Medicare approved Swing Bed 62- Discharged/Transferred to an Inpatient Rehabilitation Facility (IRF) including Rehabilitation Distinct Part Units of a Hospital 63- Discharged/Transferred to a Medicare Certified Long Term Care Hospital (LTCH) 64- Discharged/transferred to a Nursing Facility Certified under Medicaid but not certified under Medicare 65-Discharged/transferred to a Psychiatric Hospital or Psychiatric Distinct Part Unit of a Hospital 66- Discharged/transfers to a Critical Access Hospital 67-69 Reserved for Assignment by the NUBC 70- Discharged/transferred to another type of Healthcare Institution not defined elsewhere in this code list 71-99 Reserved for Assignment by the NUBC Provider Manual 2013 140 FLs 18 – 28 – Condition Codes 18 19 20 21 22 23 24 25 26 27 28 SITUATIONAL This field is required if any condition code is applicable to a claim. These fields contain codes identifying conditions that may affect payer processing of this bill. INSURANCE CODES: 01-Military Service Related 02-Condition is Employment Related 03-Patient covered by Insurance Not Reflected Here 04-Information Only Bill 05-Lien has been filed (This code indicates that the provider has filed a legal claim to recover funds potentially due the patient as a result of legal action initiated by or on behalf of the patient) 06- ESRD Patient in First 30 months of entitlement covered by Employer Group Health Insurance 07-Treatment of non-terminal Condition for Hospice Patient 08- Beneficiary would not provide information concerning other insurance coverage 09-Neither Patient or Spouse is employed 10- Patient and/or spouse is employed but no EGHP coverage exists 11- Disabled beneficiary, but no Large Group Health Plan (LGHP) coverage 12- Use this code when the services were rendered by a Provider in US. This code is being assigned by FIRSTPLUS for this use only 13- Use this code for COB claims. This code is being assigned by FIRSTPLUS as an indicator of a COB claim. It is intended for this use only. It is required that the provider submit (electronically or paper) the correspondent additional condition codes related to the coordination of benefits, as well as the occurrence codes and dates applicable). The provider must submit in the electronic X-12 (837i) all the related fields related to the other insurer payment. 14- 16 Codes are for Payer Use only Provider Manual 2013 141 17-Patient is homeless 18. Maiden Name retained 19. Child retains mother’s name 20. Beneficiary requested billing (This code indicates that the provider realizes that the services are not covered or excluded from coverage, but the beneficiary requested a formal determination of coverage from Medicare or other party) 21. Billing for Denial Notice 22. Patient on multiple drug regimens 23. Home care giver available 24. Home IV patient also receiving Home Health Agency services 25. Patient is a non-U.S. resident 26. VA-Eligible patient chooses to receives services in Medicare-certified facility 27- Patient Referred to a sole community hospital for a diagnostic laboratory test 28-Patient and/or spouse EGHP is Secondary to Medicare 29- Disabled beneficiary and/or family member’s LGHP is Secondary to Medicare 30. Non-research services provided to patients enrolled in a qualified clinical trial STUDENT STATUS 31- Patient is Student (full-time day) 32- Patient is student (cooperative/work study program) 33- Patient is student (full time night) 34- Patient is student (Part-time) 35- Reserved for assignment by the NUBC ACCOMODATIONS 36- General care patient in a specific unit 37- Ward accommodation at patient’s request 38- Semiprivate room not available 39- Private room medically necessary 40- same-day transfer Provider Manual 2013 142 41- Partial hospitalization (This code indicates that the claim is for partial hospitalization services. This condition code is required on all hospital outpatient and community access hospital (CAH) claims for partial hospitalization services (TOB codes 013X and 085X [FL 4] to distinguish partial hospitalization program services from routine outpatient psychiatric services 42- Continuing Care not related to inpatient admission 43- Continuing care not provided within prescribed Post-discharge window 44- Inpatient admission changed to outpatient 45- Ambiguous Gender category TRICARE INFORMATION 46- Non-availability statement on file 47- Transfer from another Home Health Agency (effective July 1, 2010) 48- Psychiatric residential treatment center (RTCs) for children and adolescents 49- Product replacement within product lifecycle 50- Product replacement for known recall of a product 51- Attestation of unrelated outpatient non diagnostic services (effective April 1, 2011)This hospital attests that the outpatient non diagnostic service that was provide within three calendar days (one calendar day for non- subsection (d) hospitals) of the inpatient admission are not related to the inpatient stay 52-54 Reserved for Assignment by the NUBC 55- SNF bed not available 56- Medical appropriateness 57- SNF readmission 58- Terminated Medicare Advantage Enrollee 59- Non-primary ESRD facility PROSPECTIVE PAYMENT 60- Day outlier 61- Cost Outlier 62- Payer code (Not used for FIRSTPLUS providers) 63- Payer code (This code is only for payer) Provider Manual 2013 143 64- Payer code (This code is only for payer) 65- Payer code (This code is only for payer) 66- Provider does not wish cost outlier payment 67- Beneficiary elects not to use Lifetime Reserve (LTR) days 68- Beneficiary elects to use LTR days 69- IME/DGME/N&AH Payment only (this code indicates that the claim is being submitted to request a supplemental payment for indirect medical education (IME), direct graduate medical education (DGME), and nursing and allied health (N&AH) 70- Self-administered Anemia management drug 71- Full care in unit 72- Self-care in unit 73- Self-care training 74- Home 75- Home- 100 percent reimbursement 76- Backup in facility dialysis OTHER CODES 77- Provider accepts or is obligated/required due to a contractual arrangement or Law to accept payment by a primary payer as Payment in full 78- New coverage not implemented by Managed care plan 79- CORF Services provided off-site 80- Home dialysis-nursing facility 81-99 Reserved for assignment by the NUBC SPECIAL PROGRAM INDICATOR CODES RAO- TRICARE external partnership program A1- EPSDT/CHAP (indicates this code is related to early and periodic screening diagnosis and treatment) A2- Physically handicapped children’s program A3- Special Federal funding A4- Family planning A5- Disability Provider Manual 2013 144 A6- Vaccines/Medicare 100% payment A7- Reserved for assignment by the NUBC A8- Reserved for assignment by the NUBC A9- Second Opinion Surgery AA-Abortion performed due to rape AB- Abortion performed due to Incest AC-Abortion performed due to serious fetal genetic defect, deformity, or abnormality AD-Abortion performed due to a life endangering physical condition AE- Abortion performed due to physical health of mother that is not life endangering AF- Abortion performed due to emotional/psychological health of the mother AG-Abortion performed due to social or economic reasons AH- Elective abortion AI- Sterilization AJ- Payer responsible for copayment AK- Air ambulance required AL- Specialized treatment/bed unavailable-alternate facility transport AM- Non-emergency medically necessary stretcher transport required AN- Preadmission screening not required AO- AZ Reserved for assignment by the NUBC BO- Medicare coordinated care demonstration claim B1- Beneficiary ineligible for demonstration program B2- Critical Access Hospital ambulance attestation B3- Pregnancy indicator B4- Admission unrelated to discharge on same day B5-CO- Reserved for assignment by the NUBC Q10 APPROVAL INDICATOR SERVICES CO- Reserved for assignment by the NUBC C1- Approved as billed C2- Automatic approval as billed based on focused review Provider Manual 2013 145 C3-Partial approval C4- Admission/Services denied C5-Post payment review applicable C6- Admission Pre-authorization C7-Extended authorization C8-CZReserved for assignment by the NUBC CLAIM CHANGE REASONS DO-Changes to Services Dates D1-Changes to charges D2-Changes in revenue codes/HCPCS/HIPPS Rate codes D3-Second or subsequent interim PPS bill D4-Change in clinical codes (ICD) for diagnosis and/or Procedure codes D5-Cancel to correct insured or provider ID D6-Cancel only to repay a duplicate or OIG Overpayment D7-Change to make Medicare the Secondary Payer D8-Change to make Medicare the Primary Payer D9- Any other change DA-DQ Reserved for Assignment by the NUBC DR- Disaster Related DS-DZ Change in Patient Status E1-FZ Reserved for Assignment by the NUBC G0- Distinct Medical Visit G1-GZ- Reserved for Assignment by the NUBC H0-Delayed filing, Statement of Intent Submitted (use only when there is the Existence of another third-party liability situation) H1- Reserved for assignment by the NUBC H2-Discharge by a Hospice Provider by Cause (Discharges for cause include Situations where patient safety or hospice staff safety is compromised) H3-H5- ESRD PPS Reoccurrence indicators (effective January 1 2011) Provider Manual 2013 146 H3-Reoccurrence of GI Bleed (MA) Category H4- Reoccurrence of Pneumonia (MB) Category H5 -Reoccurrence of Pericarditis (MC) Category H6-LZ- Reserved for assignment by the NUBC MO-All inclusive rate for outpatient services (Payer only code) MI-M9-Reserved for Payer Assignment MG-MV-Reserved for Payer Assignment MX-Wrong Surgery on Patient (Payer only code) MY-Surgery on Wrong Body Part (Payer only code) MZ-Surgery on Wrong Patient (Payer only code) NO-OZ-Reserved for Assignment by the NUBC PO-Reserved for Public Health Reporting Only P1-Do not Resuscitate Order (DNR) for Public Health Reporting Only P2-P6 -Reserved for Public Health Reporting Only P7-Direct Inpatient Admission from the Public Health Reporting Only P8-PZ -Reserved for Public Health Reporting Only Q0-VZ-Reserved for Assignment by the NUBC W0-United mine Workers of America (UMWA) Demonstration Indicator W1-Reserved for Assignment by the NUBC W2- Duplicate of Original Bill W3 -Level 1 Appeal W4 -Level II Appeal W5-Level III Appeal W6-ZZ-Reserved for Assignment by the NUBC Provider Manual 2013 147 FL- 29 Accident State This data element is required when the services reported are related to an auto accident. 29 ACDT STATE SITUATIONAL This data element is required when the services reported are related to an auto accident. FL-30 Reserved for assignment by the NUBC FLs 31-34 Occurrence Codes and Dates OCURRENCE CODE Date _____________________________ SITUATIONAL The occurrence code and associated date fields define a significant event relating to this bill that may affect processing. Report in alphanumeric sequence. Report occurrence codes in the following order: 31ª, 32ª, 33ª, 34ª, 31b, 32b, 33b, and 34b. If additional codes are need to be reported and there are no occurrence span codes to report, then the additional codes may be reported in 35ª, 36ª, 35b, 35b, with the date in the “from” date. ACCIDENT RELATED CODES 01-Accident/Medical Coverage (Provide date of accident or injury) 02 - No-Fault Insurance Involved- Including Auto Accident/Other 03- Accident/Tort Liability 04- Accident-Employment Related 05- Accident/No Medical or Liability Coverage 06- Crime Victim 07-08 Reserved for Assignment by the NUBC Provider Manual 2013 148 MEDICAL CONDITION CODES 09-Start of Infertility Treatment Cycle 10- Last Menstrual Period 11- Onset of Symptoms/Illness 12- Date of Onset for a chronically dependent individual (CDI) 13- 15 Reserved for Assignment by the NUBC INSURANCE RELATED CODES 16- Date of Last Therapy 17- Date Outpatient Occupational Therapy Plan Established or Last Reviewed 18- Date of Retirement of Patient/Beneficiary 19- Date of Retirement of Spouse 20- Guarantee of Payment Began 21- UR Notice Related 22- Date Active Care Ended 23- Date of Cancellation of Hospice Election Period 24- Date Insurance Denied (This code and corresponding date indicate the date the Health Care Facility received the coverage denial from an insurer) 25- Date benefits terminated by Primary Payer (This code and corresponding date i indicate the date when insurance coverage (including workers compensation or no-fault coverage) is no longer available to the patient. 26. Date SNF Bed became available 27- Date of Hospice Certification or Recertification 28- Date Comprehensive Outpatient Rehabilitation Plan Established or Last Reviewed Date outpatient Physical Therapy Plan Established or Last Reviewed 30- Date Outpatient Speech-Language Pathology Plan established or Last Reviewed 31- Date Beneficiary Notified of intent to Bill (Accommodations) this code and corresponding date indicate the date the patient was notified by the hospital that a covered level of inpatient care was no longer required. Provider Manual 2013 149 32- Date Beneficiary Notified of Intent to Bill (Procedures and Treatment). This code and corresponding date indicate the date the patient was notified by the hospital that the requested care (diagnostic procedures or treatments) may not be considered reasonable or necessary 33- First Day of the Coordination Period for ESRD Beneficiaries covered by an EGHP 34- Date of Election of Extended Care Services- applies only to religious nonmedical health care institutions (RNHCIs) 35- Date treatment started for Physical Therapy 36- Date of Inpatient Hospital Discharge for Covered Transplant Patient 37- Date of Inpatient Hospital Discharge for Non-covered Transplant Patient 38- Date Treatment Started for Home IV Therapy 39- Date Discharged on a Continuous Course of IV Therapy 40- Scheduled Date of Admission 41. Date of First Test for Preadmission Testing 42- Date of Discharge 43- Scheduled date of cancelled surgery 44- Date Treatment Started for Occupational Therapy 45- Date Treatment Started for Speech-Language Therapy 46- Date Treatment Started for Cardiac Rehabilitation 47- Date Cost Outlier Status Begins 48-49 Payer codes (These codes are reserved for third-party payer use only and should not be reported by providers) 50-Assessment date (Effective January 1, 2011)51- Date of Last Kt/V Reading (effective July 1, 2010) 52- Medical Certification/recertification date (Effective January 1, 2011)- This code is used to report the most recent non-hospice medical certification or recertification of a patient) 53- Reserved for assignment by the NUBC 54- Physician Follow-up date (Effective January 1, 2011) 55-69-Reserved for Assignment by the NUBC 70-99 Reserved for Occurrence Span Code A0- Reserved for assignment by the NUBC A1-Birth date-Insured A Provider Manual 2013 150 A2-Effective date-Insured A Policy A3-Benefits Exhausted A4-Split bill date A5-AZ- Reserved for Assignment by the NUBC B0- Reserved for assignment by the NUBC B1- Birth date-Insured B B2- Effective Date- Insured B Policy B3- Benefits Exhausted B4-BZ- Reserved for assignment by the NUBC CO- Reserved for assignment by the NUBC C1- Birth date-Insured C C2- Effective date- Insured C Policy C3- Benefits Exhausted The following Occurrence Codes are reserved for assignment by the NUBC C4-CZ, D0-DQ, DR- Reserved for Disaster Related Occurrence Code DS-DZ, EO -EZ, FO-FZ, GO-GZ, HO-IZ, JO-LZ MO-ZZ –See Definitions under Occurrence Span Codes FLs-35-36 OCCURRENCE SPAN CODES AND DATES OCURRENCE SPAN CODE CODE From Throught _____________________________ SITUATIONAL Occurrence span codes and dates identify an event that relates to payment of the claim. The provider enters codes and associated beginning and ending dates defining a specific event relating to this billing period. The valid occurrence span codes are 70-99 and MO-Z9 Provider Manual 2013 151 CODING STRUCTURE 70- Qualifying Stay dates for SNF use only. This code and corresponding dates indicate the form and through dates of at least a three day hospital stay (excluding the day of discharge or death) that qualifies the patient for Medicare payment of the SNF services billed on this claim. 71- Prior Stay dates- This code and corresponding dates indicate the form and through dates provided by the patient for any hospital stay that ended within 60 days of the current hospital or SNF admission. 72-First/Last Visit (for outpatient services) 73- Benefit Eligibility Period (period during which TRICARE medical benefits are available to a sponsor’s beneficiary) 74- Non covered level of care/Leave of Absence dates 75- SNF Level of care 76- Patient Liability (indicate the from and through dates for a period of non- covered care for which the hospital is allowed to charge the Medicare Beneficiary) 77- Provider Liability period (Indicate the from and through dates for a period of non- covered care for which the provider is liable) 78- SNF Prior Stay Dates 79- Payer Code- This code is not for provider reporting. 80- Prior same SNF Stay dates payment Ban Purposes 81-99 Reserved for assignment by the NUBC MO- QIO/UR approved stay dates M1- Provider Liability-No utilization M2- Dates of Inpatient Respite Care M3- ICF Level of Care M4- Residential Level of Care M5-MQ- Reserved for assignment by the NUBC MR- Reserved for Disaster-Related Occurrence Span Code MS-WZ- Reserved for assignment by the NUBC XO-ZZ- Reserved for assignment by the NUBC Provider Manual 2013 152 FL- 37 Reserved for assignment by the NUBC FL-38 RESPONSIBLE PARTY NAME AND ADDRESS REQUIRED FIELD The name and address of the party responsible for the bill are entered in this field. FLs 39-41 VALUE CODES AND AMOUNTS 39 Value code code Amount a b c d SITUATIONAL These fields contain codes and the related dollar amounts or values that identify data elements that are necessary to process this claim as qualified by the payer organization. Home Health agencies must report this field always. Home Health episode payments must be based on the site at which the beneficiary is served. RAP’s (Request for Anticipated Payments) as well as final claim will not be processed without code 61, and the correspondent CBSA code. Home Health Claims that do not include information on this field will be rejected to the provider. This field is used to report the point of pick up for ambulance services. The point of pick up is reported using the five digit ZIP code with value code A0. Provider Manual 2013 153 CODING STRUCTURE 01-Most Common Semiprivate Room Rate 02-Hospital has no semiprivate rooms 03-Reserved for assignment by the NUBC 04- Inpatient Professional Component charges which are combined billed 05- Professional Component included in charges and also billed separately to Carrier 06- Medicare Blood Deductible 07- Reserved for Assignment by the NUBC 08- Medicare Lifetime Reserve Amount in the First Calendar Year 09- Medicare Coinsurance amount in the First Calendar Year in billing period 10-Lifetime Reserve Amount in the Second Calendar Year 11- Coinsurance amount for second calendar year 12-Working aged beneficiary/spouse with EGHP This code and corresponding amount reflect the EGHP payment made on behalf of an aged beneficiary that the provider is applying to the covered services on this bill. 13-ESRD Beneficiary in a Medicare Coordination period with an EGHP 14-No-Fault, including Auto/other –Reflect the higher priority no-fault (including auto or other) insurance payment made on behalf of the patient or insured. 15-Worker’s compensation- Reflect the WC insurance payment made on behalf of the patient or insured. 16- Public Health service (PHS) or other federal agency 17- Operating Outlier amount- Providers do not report this code. It is use for the Payer only. 18- Operating Disproportionate Share Amount- This code is for payer only. Provider does not report this code. 19-Operating Indirect Medical Education Amount- This code is for payer use only. Providers not report this code. 20- Payer Only Code- This code is not reported by the providers. 21- Catastrophic 22- Surplus 23-Recurring monthly income 24-Medicaid rate code Provider Manual 2013 154 25-Offset to the patient-payment amount-prescription drug 26-Offset to the patient payment amount-hearing and ear services 27- Offset to the patient payment amount-vision and eye services 28- Offset to the patient payment amount-dental services 29-Offset to the patient payment amount- chiropractic services 30- Preadmission testing 31-Patient Liability amount 32-Multiple patient ambulance transport 33- Offset to the patient payment amount-podiatric services 34-Offset to the patient payment amount-other medical services 35-Offset to the patient amount-health insurance premiums 36- Reserved for assignment by the NUBC 37- Units of Blood Furnished 38-Blood deductible units 39-Units of Blood Replaced 40-New coverage not implemented by HMO (for inpatient claims only) 41- Black lung 42- Veterans affairs 43- Disabled beneficiary under age 65 with LGHP 44- Amount provider agreed to accept from the primary insurer when this amount is less than total charges, but higher than payment received 45-Accident hour 46- Number of grace days 47- Any liability insurance 48-Hemoglobin Reading 49-Hematocrit Reading 50-Physical therapy visits 51-Occupational Therapy Visits 52-Speech-Language Therapy Visits 53-Cardiac Rehabilitation Visits Provider Manual 2013 155 54- Newborn Birth weight in grams 55- Eligibility threshold for charity care HOME HEALTH SPECIFIC 56- Skilled nurse-Home visits hours (HHA only) This code and corresponding amount indicate the number of hours of skilled nursing provided during the billing period. The time includes the hours spent in the home and excluded travel time. Use this code to report the time in whole hours (rounded to the nearest whole hour), right-justified to the left of the dollar and cents delimiter. 57-Home Health Aid-Home visit hours (HHA only) This code and corresponding amount indicate the number of hours of home health services provided during this billing period. Use this value to report the time in whole hours. 58- Arterial Blood Gas (PO2/PA2) This code and corresponding amount reflect the arterial blood gas value at the beginning of each reporting period for oxygen therapy. 59- Oxygen Saturation (O2SAT/Oximetry) This code and corresponding amount reflect the oxygen saturation the beginning of each reporting period for oxygen therapy. 60- HHA Branch MSA This code indicates the metropolitan statistical area (MSA) in which the HHA is located. Reports the MSA when the branch locating is different than the HHA’s location. Report the number of the MSA in the dollar portion of the form locator, right-justified to the left of the dollar and cents delimiter. 61- Place of Residence where service is furnished (HHA and Hospice) This code indicates de CBSA number of the place residence where the home health or hospice service is delivered). This code is required for First+Plus. Example: The CBSA for San Juan, Puerto Rico (41980) is entered as 004198000. Enter the CBSA NUMBER WHERE CARE IS BEING RENDERED, NOT THE AGENCY LOCATION. 62- HHA Visits- Part A- This code is for payer use only. Providers do not report this code. 63- HHA Visits-Part B- This code is for payer use only. Providers do not report this code. Provider Manual 2013 156 64- HHA Reimbursement- Part A. This code is for payer use only. Providers do not report this code. 65- HHA Reimbursement Part B- This code is for payer use only. Providers do not report this code. 66- Medicaid Spend Down Amount 67- Peritoneal dialysis- Reflect the number of hours of peritoneal dialysis provided during the billing period. 68- EPO-Drug- Reflects the number of EPO units administered or supplied for self administration 69- State Charity Care Percent 70-75- Payer codes 76- Provider’s interim rate ( Payer code) 77- Medicare New Technology Add-On Payment (Payer code) 78-79- Payer codes 80- Covered days – The number of days covered by the primary payer. 81- Non covered days -The number of days non covered by the primary payer. 82- Co-insurance days –The number of Medicare coinsurance days used during this stay. 83- Lifetime Reserve days- The provider must notify the number of lifetime reserve days used during this stay. Each beneficiary has a lifetime reserve of 60 additional days of inpatient hospital services after using 90 days of inpatient hospital services during a spell of illness. The beneficiary should be notified by the UR, admissions or insurance verification department of his or her right to elect not to use lifetime reserve days before billing for services furnished after the 90 days in this spell of illness. If lifetime reserve days are reported, there must be an entry of 08 Medicare lifetime reserve amount in the first calendar year, or 10 Medicare lifetime reserve amount in the second calendar year, in the value code and amount fields 84-99 Reserved for assignment by the NUBC A0- Special ZIP code reporting- This code is used to report the ZIP code of the location from which the beneficiary is initially placed on board the ambulance. A1- Deductible Payer A A2- Coinsurance Payer A A3- Estimated responsibility Payer A A4- Covered Self-Administrable Drugs-Emergency Provider Manual 2013 157 A5- Covered Self-Administrable Drugs-Not self-administrable in form and situation A6- Covered Self-Administrable Drugs- Diagnostic Study and other A7- Co-Payment Payer A A8- Patient Weight A9- Patient height AA- Regulatory Surcharges, Assessments, Allowances or Health Care Related Taxes Payer A AB-Other Assessments or Allowances (e.g. medical education) Payer A AC-AZ- Reserved for Assignment by the NUBC BO- Reserved for assignment by the NUBC B1- Deductible Payer B B2- Coinsurance Payer B B3- Estimated Responsibility Payer B B4-B6- Reserved for assignment by the NUBC B7- Co-Payment Payer B B8-B9 Reserved for assignment by the NUBC BA-Regulatory surcharges, assessments, allowances or health care related taxes Payer B BB- Other assessments or allowances (e.g. medical education) Payer B BC-CO- Reserved for assignment by the NUBC C1- Deductible Payer C C2- Coinsurance Payer C C3- Estimated Responsibility Payer C C4-C6 Reserved for assignment by the NUBC C7- Co-Payment Payer C C8-C9 Reserved for Assignment by the NUBC CA- Regulatory surcharges, assessments, allowances or health care related Taxes Payer CB- Other assessments or Allowances (e.g. medical education) Payer C CC-CZ- Reserved for assignment by the NUBC DO-D2- Reserved for Assignment by the NUBC D3- Estimated Responsibility Patient Provider Manual 2013 158 D4- Clinical Trial number assigned by the NLM/NIH (National Library of Medicine/National Institutes of Health) D5- Last KT/V Reading D6-DQ- Reserved for assignment by the NUBC DR- Reserved for Disaster Related Value DS-DZ- Reserved for Assignment by the NUBC EO-EZ- Reserved for assignment by the NUBC FO-FB-Reserved for assignment by the NUBC FC- Patient Paid amount FD- Credit received from the manufacturer for a replaced medical device FE-FZ- Reserved for Assignment by the NUBC GO-G7- Reserved for assignment by the NUBC G8- Facility where inpatient hospice service is delivered G9-GZ- Reserved for assignment by the NUBC HO-OZ- Reserved for assignment by the NUBC PO-PZ- Reserved for Assignment by the NUBC QO-YO- Reserved for assignment by the NUBC Y1- Part A demonstration Payment Y2- Part B demonstration Payment Y3- Part B Coinsurance Y4- Conventional Provider Payment for Non-demonstration Claims Y5-ZZ- Reserved for Assignment by the NUBC FL 42- REVENUE CODE Field #42 allows for a four-digit revenue code that represents the specific accommodation, ancillary services or billing calculation. Use this field to report the appropriate numeric code corresponding to each narrative description or standard abbreviation that identifies a specific accommodation and/or ancillary service that is contracted with the provider. Remember that you should refer to your contract with FirstPlus to report the correspondent revenue codes contracted with your facility. For Non-contracted provider you should report the correspondent revenue code for the services provided to the patient. Provider Manual 2013 159 42 REV CD REQUIRED The revenue codes are available from the NUBC (www.nubc.org) via the NUBC’s official UB-04 Specifications Manual. Below please find some of the most common revenue codes use by the providers: ACCOMMODATION REVENUE CODES 0001-Total Charges 0022-Skilled Nursing Health Prospective Payment System 0023- Home Health Prospective Payment System (for First Plus) -This revenue code should appear on both requests for anticipated payment (RAP) (TOB code [FL 4] 0322), and claims (TOB 0329). -This code indicates that the claim is being paid under the HHPPS. -Under HHPPS, the unit of payment is a 60-day episode of care. Each episode Split into two bills. A RAP is sent at the beginning of the episode using Type Of bill 0322 and one claim is billed at the end of the episode using TOB code 0329. -Only one revenue code line is required on the RAP. This line is used to report A single HIPPS code, which is the basis of the anticipated payment -Line item detail reporting should appear only on the claim TOB 0329 -The HHPPS claim will be edited to ensure that the service date (FL 45) Reported with revenue code 0023, the admission date (FL 12), and the first Revenue code date, other than revenue code 0023, all match on an initial Episode of continuous care -New HIPPS code for home health resource groups (HHRG) are required in FL 44 (HCPCS/Rates/HIPPS), adjacent to this revenue code Provider Manual 2013 160 0024- Inpatient Rehabilitation Facility prospective payment system (for First+Plus) -Inpatient Rehabilitation facility (IRF) claims must be billed with TOB code 011X (FL 4) -This code indicates that the claim is being paid under the IRF PPS. It is used in Conjunction with a HIPPS rate code (FL 44) to identify the case-mix group (CMG) into which the beneficiary is classified. It may appears only once on a Claim -Service units (FL 46) must contain the number of covered days for the HIPPS Rate code and must be equal to or greater than 1. -A five-digit HIPPS rate/CMG code is required in FL 44 HCPCS/Rates/HIPPS, Adjacent to this revenue code 0100- All-inclusive room and board plus ancillary This revenue code can be billed with the following TOB codes (FL 4): 011X, 018X, 012X, and 028X 0110- Private room-(One Bed) 0120- Semi- private room (Two beds) general 0121- Semi-private room medical/surgical/GYN 0122- Semi-private room OB 0123- Semi-private room Pediatric 0124- Semi-private room Psychiatric 0125- Semi-private room Hospice 0126- Semi-private room Detoxification 0127- Semi-private room Oncology 0128- Semi-private room Rehabilitation 0129- Semi-private room other 0130- Semi-private Three and four beds general 0140- Deluxe Private- General Provider Manual 2013 161 0150- Room and Board Ward- general 0160 Other room and board-general 0169- Other room and board- Other 0170- Nursery general 0190- Sub acute care-general Level I 0200- Intensive care- general 0201- Intensive care surgical 0202- Intensive care medical 0203- Intensive care pediatric 0204- Intensive care Psychiatric 0206- Intermediate intensive care unit (ICU) 0207- Intensive care- Burn care 0208- Intensive care-Trauma 0209- Other intensive care 0210- Coronary Care- general 0211- Coronary Care- Myocardial Infarction 0212- Coronary Care- Pulmonary 0213- Coronary Care- Heart Transplant 0214- Intermediary Coronary Care unit (CCU) 0219- Other Coronary Care ANCILLARY SERVICES REVENUE CODES 0220- Special Charges- general 0240- All inclusive Ancillary- general 0250- Pharmacy general (also see 063X, an extension of 025X) Provider Manual 2013 162 0251- Generic Drugs 0252- Non generic Drugs 0253- Take home drugs 0254- Drugs incident to other diagnostic services 0255- Drugs incident to radiology 0256- Experimental Drugs 0258- IV solutions 0259- Other Pharmacy 0260- IV Therapy general 0261- Infusion Pump 0270- Medical/Surgical supplies and devices general (see also 062X) 0272- Sterile Supply 0274- Prosthetic/orthotic devices 0275- Pacemaker 0276- Intraocular Lens 0278- Other implants 0279- Other supplies/devices 0280- Oncology General 0290- DME (other than renal)- general 0291- DME Rental 0292- Purchase of new DME 0293- Purchase of used DME 0294- Supplies/drugs for DME effectiveness (HHAs Only) Provider Manual 2013 163 0299- Other Equipment 0300- Laboratory general 0301- Laboratory Chemistry 0302- Laboratory- Immunology 0303- Renal Patient (home) 0304- Nonroutine dialysis 0305- Hematology 0306- Bacteriology and microbiology 0307- Urology 0309- Other laboratory 0310 Laboratory Pathological general 0311 Cytology 0312 Histology 0314 Biopsy 0320- Radiology –Diagnostic-general 0321- Angiocardiography 0322- Arthrography 0323- Arteriography 0324- Chest x ray 0329- Other radiology 0330- Radiology Therapeutic and/or chemotherapy administration- general 0331- Chemotherapy administration- Injected 0332- Chemotherapy administration-oral Provider Manual 2013 164 0333- Radiation therapy 0335- Chemotherapy Administration-IV 0340- Nuclear Medicine- general 0341- Diagnostic procedure 0342- Therapeutic procedures 0343- Diagnostic radiopharmaceuticals 0344- Therapeutic radiopharmaceuticals 0350- Scans (computed tomography CT scans 0351- Head Scan 0352- Body Scan 0359- Other CT scans 0360- Operating room services-general This revenue code must be reported by acute care hospitals for all inpatient surgery admission (emergency or schedule). This is a requirement to comply with CMS HEDIS Reporting mandate statistics. 0361- Minor Surgery 0362- Organ transplant- other than kidney 0367- Kidney transplant 0369- Other OR services 0370- Anesthesia- general 0371- Anesthesia incident to radiology 0372- Anesthesia incident to other diagnostic Services 0374-Acupuncture 0379- Other Anesthesia Provider Manual 2013 165 0380- Blood and Blood components- general 0381- Packed red cells 0382- Whole Blood 0383- Plasma 0384- Platelets 0385- Leukocytes 0386- Other components 0387- Other derivatives (cryoprecipitate) 0389-Other blood 0390- Administration, Processing and Storage for Blood and Blood ComponentsGeneral 0391- Administration (e.g. transfusions) 0392- Processing and storage 0399- Other processing and storage 0400- Other imaging services-general 0401- Diagnostic mammography 0402- Ultrasound 0403- Screening mammography 0404- Positron emission tomography (PET) 0410- Respiratory services- treatments general 0412- Inhalation services 0413- Hyperbaric oxygen therapy 0420- Treatments- Physical Therapy general 0421- Visit charge Provider Manual 2013 166 0422- Hourly charge 0423- Group rate 0424- Evaluation of re-evaluation 0429- Other Physical Therapy 0430- Treatments-Occupational Therapy 0431- Visit Charge 0432- Hourly charge 0433- Group rate 0434- Evaluation of re-evaluation 0439- Other occupational therapy (may include restorative therapy) 0440- Treatments- Speech-Language Therapy Pathology-general 0441- Visit charge 0442- Hourly charge 0443- Group rate 0444- Evaluation of re-evaluation 0449- Other Speech-language pathology 0450- Visits- EMERGENCY ROOM 0451- EMTALA emergency medical screening services 0452- ER beyond EMTALA screening 0456- URGENT CARE 0459- Other Emergency Services 0460- Pulmonary Function general 0469- Other pulmonary function Provider Manual 2013 167 0470- Audiology general 0471- Audiology Diagnostic 0472- Audiology Treatment 0480- Cardiology general 0481- Cardiac Cath Lab 0482- Stress Test 0483- Echocardiology 0489- Other cardiology 0490- AMBULATORY SURGICAL CARE 0500- OUTPATIENT SERVICES (This code indicates outpatient charges for Services rendered to an outpatient who is admitted as an inpatient Before midnight of the day following the date of services. 0510- VISITS CLINIC- general 0511- Chronic pain center 0512- Dental Clinic 0513- Psychiatric Clinic 0514- OB/GYN clinic 0515- Pediatric Clinic 0516- Urgent Care Clinic 0517- Family Practice Clinic 0519- Other Clinic 0520- Freestanding Clinic visits 0530- Osteopathic Services-general 0540- Ambulance- general. Provider must report this revenue code for all Ambulance services. Provider Manual 2013 168 0541- Supplies 0542- Medical Transport 0543- Heart Mobile 0544- Oxygen 0545- Air Ambulance 0546- Neonatal ambulance services 0547- Pharmacy 0549- Other ambulance 0550- Visits Skilled Nursing- general 0551- Visit charge 0552- Hourly charge 0559- Other skilled nursing 0560- Home Health- Medical Social Services 0570- Home Health Aide 0580- Home Health-Other visits 0590- Home Health, Units of Service 0600- Rental Months- Home Health Oxygen 0610- Magnetic Resonance Technology (MRT) tests 0611- MRI- Brain/brain stem 0612- MRI- Spinal Cord/spine 0614- MRI other 0615- MRA Head and Neck 0616- MRA Lower extremities Provider Manual 2013 169 0618- MRA- Other 0619- Other MRT 0621- Medical/surgical supplies extension of 027X revenue code (supplies incident to radiology) 0623- Surgical dressing 0624- FDA investigational devices 0631- Pharmacy extension of 025X revenue codes (Single Source drug) 0633- Restrictive prescription 0634- Erythropoietin (EPO) less than 10,000 units 0635- Erythropoietin (EPO) 10,000 or more units 0636- Drugs requiring detailed coding 0640- Home IV Therapy Services general 0650- Hospice services general 0657- Hospice Physician services 0700- Cast Room general 0720- Labor room/delivery general 0730- EKG/ECG (electrocardiogram)- general 0731- Holter monitor 0732- Telemetry 0739- Other EKG/ECG 0740- EEG (Electroencephalogram)- general 0750- Gastrointestinal Services general 0769- Observation services on outpatient claims Provider Manual 2013 170 0770- Preventive Care Services (general) 0780- Telemedicine- general 0790- Extra Corporeal Shock Wave Therapy 0800- Inpatient renal dialysis sessions- general 0801- Inpatient hemodialysis 0802- Inpatient peritoneal (non-CAPD) 0803- Inpatient continuous ambulatory peritoneal dialysis (CAPD) 0804- Inpatient continuous cycling peritoneal dialysis (CCPD) 0809- Other inpatient dialysis 0810- Acquisition of Body Components 0811- Living Donor 0812- Cadaver donor 0813- Unknown donor 0814- Unsuccessful organ search-donor bank charges 0819- other donor 0820- Hemodialysis sessions-outpatient or Home-general 0821- Hemodialysis/composite or other rate 0822- Home supplies 0823- Home equipment 0824- Maintenance/100 percent 0825- Support Services 0829- Other outpatient hemodialysis 0830- Peritoneal dialysis outpatient or Home sessions- general Provider Manual 2013 171 0831- Peritoneal/composite or other rate 0832- Home supplies 0833- Home equipment 0834- Maintenance/100 percent 0835- Support Services 0840- CAPD outpatient or home - general 0841- CAPD/composite or other rate 0842- Home supplies 0843- Home equipment 0844- Maintenance/100 percent 0845- Support Services 0850- CCPD- outpatient or home days- general 0851- CCPD/composite or other rate 0852- Home supplies 0853- Home equipment 0854- Maintenance/100 percent 0855- Support Services 0859- Other outpatient CCPD 0860- Magneto encephalography (MEG)- general classification 0880- Miscellaneous dialysis 0900- Behavioral Health Treatments/services (also see 091X an extension of 090X) 0901- Electroshock treatment (ECT) Provider Manual 2013 172 0902- Milieu therapy 0903- Play therapy 0904- Activity therapy 0905- Intensive outpatient services-psychiatric 0906- Intensive outpatient services-chemical dependency 0911- Rehabilitation (Behavioral Health Treatments/services-extension of 090X) 0912- Partial hospitalization- less intensive 0913- Partial hospitalization- intensive 0914- Individual Therapy 0915- Group Therapy 0916- Family Therapy 0920- Other diagnostic services-general 0921- Peripheral vascular lab 0922- Electromyelogram 0923- Pap smear 0924- Allergy test 0925- Pregnancy test 0929- Other diagnostic service 0940- Other therapeutic services (see also 095X, an extension of 094X)-general 0941- Recreational therapy 0942- Education/Training 0943- Cardiac Rehabilitation 0944- Drug Rehabilitation Provider Manual 2013 173 0945- Alcohol Rehabilitation 0948- Pulmonary Rehabilitation 0949- Other therapeutic services 0960- Professional Fees (see also 097X abd 098X)-general 0963- Anesthesiologist (MD) 0964- Anesthetist (CRNA) FL 43 Revenue Descriptions This field contains a narrative description or standard abbreviation for each revenue code Category reports don this claim. (FL 42). 43 Description REQUIRED FL 44 –HCPCS/CPT/RATES/HIPPS RATES CODES The provider must submit the correspondent RATE, HCPCS, CPT, or HIPPS code that is associated to the Revenue Code on FL 42 when applicable. This field contains the Healthcare Common Procedure Coding System (HCPCS) code, CPT code applicable to ancillary services, outpatient services, and/or over perdiems. Also, the HIPPS code is also required depending on the bill type submitted and the type of facility; i.e. home health services, Inpatient Rehabilitation facilities. 44 HCPCS/ RATE/HIPPS CODE REQUIRED depending on the revenue code submitted on the bill and or contracting arrangements with the provider. For some inpatient services the provider must submit the daily accommodation rate on the correspondent revenue codes. For Home Health claims the provider must submit the HIPPS code. Also, the Inpatient Rehabilitation facilities must submit the correspondent HIPPS code. Provider Manual 2013 174 FL-45 Service Date This field contains the date on which the indicated service was provided. 45 SERV DATE REQUIRED First Plus requires that the service date be reported for all ancillaries and over perdiem services on an inpatient stay. It is require that every revenue code have an associated line-item date of service or dates of service range for bill types 012X, 013X, 014X,022X, 023X, 032X, 033X, 034X, 071X, 072X, 073X, 074X, 075X, 076X, 081X, 082X, 083X, and 085X Under HHPPS, RC 0023 must include the date of the first billable services provided under the HIPPS code reported on that line. FL- 46 Units of Service This field contains a quantitative measure of services rendered, by revenue, category, to or for the patient, including items such as the number of accommodation days, visits, miles, pints of blood, units or treatments. 46 Service Units REQUIRED Zero or negative values are not allowed for inpatient or outpatient claims. FL- 47 Total Charges This field contains the total charges pertaining to the related revenue code for the current billing period as entered in the Statement Covers Period field (FL 6). 47 Total Charges REQUIRED Provider Manual 2013 175 Under HHPPS, on the RAP and the claim, zero charges must be reported with RC 0023. Under the IRF PPS, the covered charges reported with RC 0024 (FL 42) should be zero. FL-48 Non covered Charges This field contains the total non- covered charges for the destination payer pertaining to a particular revenue code. 48 Non-Covered Charges SITUATIONAL FL- 49 (Untitled) RESERVED for assignment by the NUBC. FL-50 A-C Payer Name This field contains the name of the health plan from which the provider might expect some Payment for the bill for each correspondent line from a through c. A 50 Payer Name B C REQUIRED FL- 51 A - C Health Plan National Identification Number 51 Health Plan ID A B C SITUATIONAL Report the HIPAA National Plan Identifier when it is mandated for use. Until that Provider Manual 2013 176 Occurs, report the legacy or proprietary number as defined in trading partner agreements. FIRSTPLUS has determined that until this field becomes HIPAA Mandatory the provider must leave this field blank for UB-04 paper claims. FL-52 A-C Release of Information Certification Indicator The provider must indicate a Y (yes) in this field. A “Y” indicates that the provider has a signed statement permitting release of medical billing data related to a claim] 52 REL INF A B C REQUIRED FL-53 A, B, C.- Assignment of Benefits Certification Indicator This field shows whether the provider has a signed form authorizing the third-party insurer to pay the provider directly for the services. This indicator applies to the payers listed in FL 50 lines A, B, and C. 53 ASSN BEN A B C SITUATIONAL Provider Manual 2013 177 FL- 54 A, B, C. Prior Payments The amount in this field represents the amount the hospital has received to date toward payment of this bill for the payer indicated in FL 50 on lines A, B, and C 54 Prior payments A B C SITUATIONAL FL-55 A, B, AND C- Estimated amount due-Payer The amount in this field represents an estimate by the hospital of the amount due from The indicated payer in FL 50 on lines A, B, and C. 55 EST AMOUNT DUE A B C SITUATIONAL FL-56 National Provider Identifier-Billing Provider (NPI) This field contains the unique identification number assigned to the provider submitting the bill. 56 NPI REQUIRED Provider Manual 2013 178 FL- 57 Other (Billing) Provider Identifiers Providers contracted under PPS as well as HHA must submit the number assigned by Medicare (Six digits Medicare Provider Number) on this field. 57 A PROV ID C OTHER B SITUATIONAL FL-58 A, B, AND C - Insured Name This field contains the name of the patient or insured individual in whose name the insurance is issued as qualified by the payer organization listed in FL 50 on lines A, B, and C. 58 INSURED NAME A B C Form Locator 58 A is required. Form Locator 58 B is situational Form Locator 58C is situational FL-59 A, B, AND C – Patient’s relationship to Insured This field contains the code that indicates the relationship of the patient to the insured individuals identified in FL 58 on lines A, B, and C. 59 P REL REQUIRED Provider Manual 2013 179 CODING STRUCTURE for UB-04 ONLY: 01-Spouse 18-Self 19-Child 20-Employee 21-Unknown 39-Organ Donor 40-Cadaver Donor 53-LIfe Partner G8-Other Relationship FL-60 A, B, AND C Insured’s Unique Identifier This field contains the insured’s unique identification number assigned by the payer organization. Please refer to the FIRSTPLUS Insurance Card. The provider must enter the complete number. 60 INSURED UNIQUE ID 60 A is a required field. 60B- is situational 60C- is situational FL-61 A, B, AND C Insurance Group Name This field contains the name of the group or plan through which the health insurance coverage is provided to the insured. If the group name is available enter the information in the correspondent line (A, B, or C) 61 GROUP NAME Provider Manual 2013 180 61 A is situational. 61 B is situational. 61C is situational FL-62 A, B, AND C – Insurance Group Number This field contains the identification number, the control number or the code that is assigned by the insurance company or claims administrator to identify the group under which the individual is covered. 62 INSURANCE GROUP NUMBER A B C FL 62 A Required if the insured’s identification card shows a group number. FL 62 B is a situational field. FL 62 C is a situational field. FL- 63 Treatment Authorization Code This field identifies a number or other indicator that designates that the treatment is covered by this bill has been authorized by the payer indicated in FL 50 on lines A, B, and C. 63. TREATMENT AUTHORIZATION CODES A B C REQUIRED FOR HOME HEALTH This is a situational field. The provider must complete the field when applicable (when an authorization or referral number is assigned by the payer.) For Home Health Agencies under First Plus this is a required field. The Home Health Agency must complete this field. Under HHPPS, on the RAP and on the HHA claim, the Provider Manual 2013 181 home health agencies must enter the treatment authorization code from the OASIS software. This data element links the RAP record to the specific OASIS assessment used to produce the HIPPS code reported on FL 44. The treatment authorization is an 18position code. Note: Claims with missing, invalid or incomplete treatment authorization codes will be rejected back to the provider as a non-processable claim. The provider must correct and returned the claim along with the non procesable form letter within the time frame establish by the Prompt Payment Law of Puerto Rico, FL- 64 Document Control Number (DCN) This is the internal control number (ICN) or document control number (DCN) assigned to the original bill by the health plan. This number appears on the Explanation of Payment to the provider (EOP-paper /835-electronic) 64. DOCUMENT CONTROL NUMBER This is a required field when the providers resubmit a claim for adjustment or a reconciliation process to FIRSTPLUS. Please refer to the CLAIM ID number in the EOP. FL- 65 Employer Name (of the Insured) This field contains the name of the employer that provides (or may provide) health care coverage for the insured individual identified in FL 58 on lines A, B, and C. 65. EMPLOYEER NAME This is a situational field, and applies when there is a WC (Workers Compensation) or a EGHP (Employer Group Health Plan). The provider enters the name of the employer that provider the health coverage for the individual identifies on the same lines in FL 58. This information is required when that payer is either primary or secondary and the MA is the secondary or tertiary insurer. Provider Manual 2013 182 FL-66 Diagnosis and Procedure Code Qualifier (ICD version) This code identifies the version of the International Classification of Diseases (ICD) being reported. 66 DX This is a required field. Code Structure: 9-Ninth Edition 0-Tenth Edition Note: When ICD-10 is implemented on October 1st 2014, the provider must ensure that the correct qualifier is selected based on service or (discharge) date. FL- 67 Principal Diagnosis Code This field contains the full ICD-9-CM diagnosis code, including the fourth and fifth digits, if applicable, that describes the principal diagnosis (the condition established after study to be chiefly responsible for causing the hospitalization or use of other hospital services). All diagnosis code must be a valid code. FIRSTPLUS will not accept truncated codes. 67 Principal Diagnoses REQUIRED To prevent claim errors, ICD-9-CM codes should be used at the highest level of specificity. You are required to assign the most precise ICD-9-CM code that most fully explains the narrative description in the chart of symptoms or diagnosis. Vague or nonspecific diagnosis codes may cause you claim to edit for medical necessity. Also, claims submitted with three-or four-digit codes, where four-or five-digit are available will be rejected. Note: Claims with missing, invalid or incomplete principal diagnosis code will be rejected as non-processable claims. The provider must correct and returned the claim along with the non procesable form letter within the time frame establish by the Prompt Payment Law of Puerto Rico. Provider Manual 2013 183 Under the Home Health prospective payment System (HHPPS) on the request for anticipated payment (RAP) and on the final claims, or any other claim submitted, home health agencies must enter the ICD-9-CM code for the principal diagnosis. For inpatients, the condition established after study to be chiefly responsible for the admission of the patient for care should be listed as the principal diagnosis, even though another diagnosis may be more severe. The Medicare code editors as well as the Outpatient Code Editor are applications that are used to identify data inconsistencies on inpatient hospital and outpatient claims. Claims are edited to check each diagnosis code on the claim against a table of valid ICD-9-CM. Invalid codes will be rejected. Edits such as invalid diagnosis code, admitting diagnosis, procedure code will be validated. Invalid fourth or fifth digit of an ICD-9-CM diagnosis code or procedure code will be rejected. E codes use as the principal diagnosis when the E codes describe the circumstances that caused an injury rather than the nature of the injury. Also, age conflicts, sex conflicts, or unacceptable principal diagnosis will be edited and rejected back to the provider. Certain trauma diagnosis codes are used to identify claims involving patients who may be covered under automobile insurance, no-fault, worker’s compensation or other liability insurance for which we should be the secondary payer. Claims with trauma-related diagnosis codes may be delayed or rejected due to missing or incomplete information. We can also due post payment review to investigate any trauma code report don the claim whether the claim is listed as primary, secondary or other diagnosis. There might also be what we consider questionable admissions but that may be covered depending upon the medical circumstances. The following table lists questionable ICD-9CM codes for which First Plus may request additional documentation. Manifestation code as principal diagnosis Manifestation codes describe the manifestation of an underlying dis-ease, not the disease itself, and therefore should not be used as a principal diagnosis. The following list contains some samples of ICD-9-CM diagnoses with corresponding descriptions identified as manifestation codes. Manifestations not allowed as principal diagnosis 2842 28952 28983 29410 29411 Myelophthisis Splenic sequestration Myelofibrosis Dementia w/o behav dist Dementia w behavior dist Provider Manual 2013 184 3207 3210 3211 36642 36643 36644 37044 37105 37215 37231 4211 4220 42491 4257 4258 44381 45620 60491 60881 61611 61651 6281 71110 Mening in oth bact dis Cryptococcal meningitis Mening in oth fungal dis Tetanic cataract Myotonic cataract Cataract w syndrome NEC Keratitis in exanthema Phthisical cornea Parasitic conjunctivitis Rosacea conjunctivitis Ac endocardit in oth dis Ac myocardit in oth dis Endocarditis in oth dis Metabolic cardiomyopathy Cardiomyopath in oth dis Angiopathy in other dis Bleed esoph var oth dis Orchitis in oth disease Male gen dis in oth dis Vaginitis in oth disease Vulvar ulcer in oth dis Infertil-pituitary orig Reiter arthritis-unspec Questionable admission Some diagnoses are not usually sufficient justification for admission to an acute care hospital. For example, if a patient is given code 4011 for benign hypertension, then the patient would have a questionable admission, since benign hypertension is not normally sufficient justification for admission to a hospital. The following list contains some diagnosis codes with corresponding descriptions identified as questionable admission when used as a principal diagnosis. Questionable admissions - principal diagnosis only 25000 27800 3804 4011 4262 4263 4264 79093 7962 9999 V08 DMII wo cmp nt st uncntr Obesity NOS Impacted cerumen Benign hypertension Left bb hemiblock Left bb block NEC Rt bundle branch block Elvtd prstate spcf antgn Elev bl pres w/o hypertn Complic med care NEC/NOS Asymp hiv infectn status Provider Manual 2013 185 V5331 V5332 V5339 Ftng cardiac pacemaker Ftng autmtc dfibrillator Ftng oth cardiac device Unacceptable principal diagnosis There are selected codes that describe a circumstance which influences an individual’s health status but not a current illness or injury, or codes that are not specific manifestations but may be due to an under-lying cause. These codes are considered unacceptable as a principal diagnosis. There are a few usually unacceptable principal diagnosis codes that are considered “acceptable” when a secondary diagnosis is also coded on the record. If no secondary diagnosis is present for this subset of codes, the message REQUIRES SECONDARY DX will appear. The following list contain a some samples of codes with corresponding descriptions identified as unacceptable when entered as principal diagnosis. ➤ Note: Codes that require a secondary diagnosis are indicated with an asterisk (*). Unacceptable principal diagnoses 1992 23877 27950 27951 27952 27953 3051 3533 35831 36570 36571 36572 36573 36574 3708 4142 4143 4144 41512 4233 4404 449 51282 5735 6113 69550 Malig neopl-transp organ Post tp lymphprolif dis Graft-versus-host NOS Ac graft-versus-host dis Chronc graft-vs-host dis Ac on chrn grft-vs-host Tobacco use disorder Thoracic root lesion NEC Lambert-Eaton synd neopl Glaucoma stage NOS Mild stage glaucoma Moderate stage glaucoma Severe stage glaucoma Indeterm stage glaucoma Keratitis NEC Chr tot occlus cor artry Cor ath d/t lpd rch plaq Cor ath d/t calc cor lsn Septic pulmonary embolsm Cardiac tamponade Chr tot occl art extrem Septic arterial embolism Sec spont pneumothorax Hepatopulmonary syndrome Fat necrosis of breast Exfol d/t eryth <10% bdy Provider Manual 2013 186 69551 69552 69553 78951 7981 7982 7989 99802 V010 V011 V012 V013 V014 V015 V016 V0181 V0189 V019 V020 V021 V0252 V0253 V0254 V0259 V0260 V0261 V0262 V0269 V027 V028 V029 V030 V031 V032 V037 V0381 V0382 V0389 V039 V040 V041 V047 V0481 V0482 V0489 V050 Exfl d/t eryth 10-19 bdy Exfl d/t eryth 20-29 bdy Exfl d/t eryth 30-39 bdy Malignant ascites Instantaneous death Death within 24 hr sympt Unattended death Postop shock, septic Cholera contact Tuberculosis contact Poliomyelitis contact Smallpox contact Rubella contact Rabies contact Venereal dis contact Contact/exposure-anthrax Communic dis contact NEC Communic dis contact NOS Cholera carrier Typhoid carrier Streptococus carrier NEC Meth susc Staph carrier Meth resis Staph carrier Bacteria dis carrier NEC Viral hep carrier NOS Hepatitis B carrier Hepatitis C carrier Viral hep carrier NEC Gonorrhea carrier Venereal dis carrier NEC Carrier NEC Vaccin for cholera Vacc-typhoid-paratyphoid Vaccin for tuberculosis Tetanus toxoid inoculat Nd vac hmophlus inflnz b Nd vac strptcs pneumni b Nd other specf vacnation Vaccin for bact dis NOS Vaccin for poliomyelitis Vaccin for smallpox Vaccin for common cold Vaccin for influenza Vaccination for RSV Vaccn/inoc viral dis NEC Arbovirus enceph vaccin Provider Manual 2013 187 V051 V052 V053 V054 V058 V059 V060 V061 V062 V063 V064 V065 V066 V068 V069 V071 V072 V0731 V074 V0751 V0752 V0759 V079 V090 V091 V092 V0990 V0991 V1000 V1001 V1002 V1003 V1004 * V571 * V5721 * V5722 * V573 V574 V5781 *V5789 * V579 Vacc arboviral dis NEC Vaccin for leishmaniasis Need prphyl vc vrl hepat Need prphyl vc varicella Vaccin for disease NEC Vaccin for singl dis NOS Vaccin for cholera + tab Vaccination for DTP-DTaP Vaccin for dtp + tab Vaccin for dtp + polio Vac-measle-mumps-rubella Vaccination for Td-DT Nd vac strp pnumn/inflnz Vac-dis combinations NEC Vac-dis combinations NOS Desensitiza to allergens Prophylact immunotherapy Prophylac fluoride admin Hormone replaces postmeno Use of SERMs Use aromatase inhibitors Use oth agnt af estrogen Prophyl or tx meas NOS Inf mcrg rstn pncllins Inf mcrg rstn b-lactam Inf mcrg rstn macrolides Infc mcrg drgrst mult Infc mcrg drgrst mult Hx of GI malignancy NOS Hx of tongue malignancy Hx-oral/pharynx malign NEC Hx-esophageal malignancy Hx of gastric malignancy Physical therapy NEC Encntr occupatnal therapy Encntr vocational therapy Speech-language therapy Orthotic training Orthotic training Rehabilitation proc NEC Rehabilitation proc NOS Provider Manual 2013 188 FL-67A-67Q Other Diagnosis Codes This field contains the full ICD-9-CM diagnosis codes (including the fourth and fifth digits, if applicable) corresponding to all conditions that coexist at the time of admission, that develop subsequently, or that affect the treatment received and/or the length of stay. Diagnoses that relate to an earlier episode, which have no bearing on the current hospital stay, should be excluded. Other diagnosis code fields I A J B K C D L M E N F O G P H Q This is a required field when there are conditions that result as secondary diagnosis. NOTE: Present on Admission Indicator The present on admission indicator (POA) applies to diagnosis codes (i.e., principal, secondary and E codes) for inpatient claims to general acute-care hospitals or other facilities as required by law or regulation for public health reporting. It is the eighth digit attached to the corresponding diagnosis code. Effective January 1, 2011 the Deficit Reduction Act of 2005 will require all claims that include an inpatient admission to general acute care hospitals or other facilities to contain POA information. Any hospital that is currently contracted under First Plus -DRG methodology of payment must report the POA indicator. All hospital inpatient services rendered by Non-contracted providers must also submit the POA indicator in all the diagnosis related fields. As a general rule, all hospital inpatient admission to general acute care hospitals must report the POA indicator on their claims. We encourage providers to submit the POA indicator on their inpatient acute care admissions regardless their contracted reimbursement methodology. Additional information related to POA guidelines can be obtained from ICD-9-CM Official Guidelines for Coding and Reporting that are available on the NCHS website at http://www.cdc.gov/nchs/datawh/ftpserv/ftpicd9/ftpicd9.htm FL-68 Reserved-Not in used currently. FL-69 Admitting Diagnosis This field is for reporting the complete ICD-9-CM code describing the patient’s diagnosis at the time of admission, including fourth and fifth digits when appropriate. Provider Manual 2013 189 69. ADM DX This is a required field for inpatient admission claims and encounters, and Part B only claims (TOB’s 012X, and 022X in FL 4). Enter the patient’s admitting diagnosis using a complete and accurate ICD-9-CM code. The ICD-9-CMN admitting diagnosis code describes a significant finding representing patient distress, an abnormal finding on an examination, a possible diagnosis base on significant findings, a diagnosis established from a previous encounter or admission, an injury, a poisoning, or a reason or condition (not an illness or injury) such as follow up or pregnancy in labor. FL-70 A-C Patient’s reason for visit This field is for reporting the complete ICD-9-CM code describing the patient’s reason for the visit at the time of admission or outpatient registration, including fourth and fifth digits when appropriate. 70. PATIENT REASON A B C DX Patient’s Reason for Visit is required for all un-scheduled outpatient visits. Unscheduled outpatient visits are defined as TOB 013X or 085X with a priority or type of admission (FL 14) of 1, 2, or 5 and revenue codes of 045X, 0516, 0526, or 0762. FL-71 Prospective Payment System (PPS) code Required Field. The hospital must report the correspondent DRG code related to an acute care admission on this field. This code it is usually available from the medical records coding system of the hospital. This code might identify those emergency or schedule admissions related to Surgeries. CMS requires that surgery admissions be identified properly. Note: For those providers that submit electronic claims (837 I) please report the DRG CODE on LOOP 2300 –Claim Information/Segment HI Diagnosis Related Group (DRG) Information. 71. PPS CODE REQUIRED FIELD Provider Manual 2013 190 FL-72 a-c External Cause of Injury (ECI)-E Code This field contains up to three full ICD-9-CM codes, including the fourth and fifth digits if applicable, pertaining to the external cause of injury, poisoning or adverse effect. Health Care facilities are encouraged to report an E code whenever there is a diagnosis of an injury, poisoning or other adverse effect. 72. ECI CODE This is a Situational field. FL-73 Reserved. FL-74 Principal Procedure Code and Date This field contains the ICD-9CM code for the inpatient principal procedure performed at the claim level during the period covered by this bill and the corresponding date on which the principal procedure was performed. HIPAA code set requirements do not allow the use of ICD-9-CM procedure codes on outpatient claims. 74. PRINCIPAL PROCEDURE CODE DATE This is a situational field. Note: All inpatient surgery admissions must be reported with the correspondent ICD-9CM procedure codes. Remember CMS requires that all surgery admissions be reported accordingly. 74A-74E Other Procedure Codes and Dates This field allows reporting of up to five ICD-9-CM codes to identify the significant procedures performed during the billing period, other than the principal procedure, and the corresponding dates on which the procedures were performed. Report those that are most important for the episode of care and specifically any therapeutic procedures closely related to the principal diagnosis. Provider Manual 2013 191 HIPAA code set requirements do not allow the use of ICD-9-CM procedure codes on outpatient claims. CODE DATE Completion of this field is required for inpatient Part A claims only. Inpatient hospital claims require reporting the principal procedure if a significant procedure occurred during the hospitalization. The principal procedure is the procedure performed for definitive treatment rather than for diagnostic or exploratory purposes, or which was necessary to take care of complication. It is also the procedure most closely related to the principal diagnosis. Enter the full ICD-9-CM code, including the fourth digit when applicable, and the date of the principal procedure. This is a situational field. Note: All inpatient surgery admissions must be reported with the correspondent ICD-9-CM procedure codes. Remember CMS requires that all surgery admissions be reported accordingly. FL- 75 Reserved FL-76 Attending Provider Name and Identifiers (including NPI) This field identifies the name and identifying number of the attending provider. The attending provider is the individual who has overall responsibility for the patient’s medical care and treatment reported on this claim. 76. ATTENDING NPI This is a required field Note: Effective January 1st, 2012 CMS requires that field 76 be completed. FL-77 Operating Physician Name and Identifiers This field identifies the name and identification number of the individual with the primary responsibility for performing the surgical procedure(s). 77. OPERATING NPI This is a situational field. Provider Manual 2013 192 FL-78 and 79 Other Provider Names and Identifiers These fields contain the name and identification number of the provider that corresponds to the indicated provider type on this claim. 78. OTHER NPI This is a situational field. FL-80 Remarks This field is used to capture additional information necessary to adjudicate the claim. Provide any additional information that is necessary to adjudicate the claim or otherwise fulfill the payer’s reporting requirements. Enter any information that is not reported elsewhere on the bill but that may be necessary for reimbursement. 80. Remarks This is a situational field. FL-81 Code-Code field This field is used to report overflow or additional codes related to field locators or to report externally maintained codes approved by the NUBC for inclusion in the institutional data set. 81 CC A B C D This is a situational field Provider Manual 2013 193 ADA DENTAL CLAIM FORM The following fields are required ADA Dental Health Insurance Claim Form: Provider Manual 2013 194 HEADER INFORMATION Box 1 Type of Transaction Required Field Indicate whether Actual Service or Request for Predetermination/Preauthorization Box 2 Predetermination/Preauthorization Number Situational Field Enter Prior Authorization Number, if applicable Box 3 Insurance Company/Dental Plan Benefit Information Required Field Indicate Insurance Company claim submission address • Refer to your provider billing manuals for information on the mailing address for claims submission OTHER COVERAGE Box 4 Other Dental or Medical Coverage? Situational Field- Complete if there is another coverage Check Yes or No • If yes, please complete box 5-11 Box 5 Name of Policy Holder/Subscriber in box 4 Situational Field If box 4 is completed, then this field must be completed Provider Manual 2013 195 Box 6 Date of Birth Situational Field If box 4 is completed, then this field must be completed Box 7 Gender Situational Field If box 4 is completed, then this field must be completed Box 8 Policyholder/Subscriber ID (SSN or ID#) Situational Field If box 4 is completed, then this field must be completed Box 9 Plan/Group Number Situational Field If box 4 is completed, then this field must be completed Box 10 Patient’s Relationship to Person Named in Box 5 Situational Field If box 4 is completed, then this field must be completed Box 11 Other Company/Dental Benefit Plan Name, Address, City, State, Zip Code Situational Field Indicate the “other insurance plan(s)” Name and address Provider Manual 2013 196 POLICYHOLDER/SUBSCRIBER INFORMATION Box 12 Policy Holder/Subscriber Name Required Field Indicate subscriber’s name and Address Box 13 Date of Birth Required Field Enter patient’s date of birth Box 14 Gender Required Field Check the correspondent box Box 15 Policyholder/Subscriber ID Required Field Enter patient’s contract number as appear on the First+Plus Insurance Card Must have 9 characters Note: claim with missing, incorrect, or incomplete contract number will be rejected as nonprocessable. The provider must correct the claim and return it to First+Plus along with the non-processable form letter within the timeframe establish by the Prompt Payment Law of Puerto Rico. Box 16 Plan/Group Number Situational Enter the group number as appears on the member insurance card Provider Manual 2013 197 Box 17 Employer Name Situational Field If applicable enter the employer name PATIENT INFORMATION Box 18 Relationship to Policyholder/Subscriber in #12 Above Situational Field Check the correspondent box as appropriate Box 19 Student Status Not use by First+Plus Box 20 Name, Address, City, State, Zip Code Required field Enter the name, address, city, State, Zip Code of the patient. Box 21 Date of Birth Required Field Enter the patient Date of Birthday Box 22 Gender Required Field Enter the patient gender Provider Manual 2013 198 Box 23 Patient ID/Account # Required field If you enter the patient’s account number, we will report it back to you on your remittance advice (RA)/Explanation of payment (EOP) Up to 12 characters, any combination of alpha characters or numbers RECORD OF SERVICES PROVIDED Box 24 through 31 Required Fields ( unless otherwise noted) Repeat Boxes 24-31 for any additional services/procedures rendered, up to a total of 10 lines per claim form Box 24 Procedure Date Required Field Enter the date of the service Must be in mmddccyy format, e.g., 08152012 Note: claim with missing, incorrect, or incomplete procedure date will be rejected as nonprocessable. The provider must correct the claim and return it to First+Plus along with the non-processable form letter within the timeframe establish by the Prompt Payment Law of Puerto Rico. Box 25 Area of Oral Cavity Situational Field Report when restoration procedures are involved Box 26 Tooth System Situational Indicate the tooth system if service require the notification of the system Provider Manual 2013 199 Box 27 Tooth Number(s) or Letter(s) Required Field, except for preventive services Enter number of tooth , as applicable Must be no more than two (2) characters (1-32) Note: claim with missing, incorrect or incomplete Tooth number, if required, will be rejected as non-processable. The provider must correct the claim and return it to First+Plus along with the non-processable form letter within the timeframe establish by the Prompt Payment Law of Puerto Rico. Box 28 Tooth Surface Required Field, when the procedure requires submission of the tooth number Enter tooth surface, as applicable Up to five (5)surfaces, one character each Surface o M-Mesial o 0- Oclusal o I- Incisal o B- Bucal o D-Distal o F- Facial o L- Lingual Note: claim with missing, incorrect or incomplete tooth surface, if required, will be rejected as non-processable. The provider must correct the claim and return it to First+Plus along with the non-processable form letter within the timeframe establish by the Prompt Payment Law of Puerto Rico. Box 29 Procedure Code Required Field Enter the applicable CDT procedure code Must be five (5) characters beginning with a “D” Note: claim with missing, incorrect, or incomplete procedure code will be rejected as nonprocessable. The provider must correct the claim and return it to First+Plus along with the Provider Manual 2013 200 non-processable form letter within the timeframe establish by the Prompt Payment Law of Puerto Rico. Box 30 Description Required Field Enter description of procedure according to CDT guidelines Box 31 Fee Required Field Note: claim with missing, incorrect, or incomplete information will be rejected as nonprocessable. The provider must correct the claim and return it to First+Plus along with the non-processable form letter within the timeframe establish by the Prompt Payment Law of Puerto Rico. Enter fee charged for procedure Must be in a valid currency format: dd.cc, e.g., 24.00 Box 32 Other Fee(s) Not used by First+Plus Box 33 Total fee Required Field Enter your total charge (per page) Must equal the total of all fees entered in Box 31 Up to nine (9) digits Must be in a valid currency format, dd.cc, e.g., 24.00 Provider Manual 2013 201 MISSING TEETH INFORMATION Box 34 Situational Field Check appropriate number when the procedure requires that the missing tooth be reported Box 35 Remarks Use this field to report any other relevant information needed for the Payer to make a determination on the claim, such as emergency services justification, etc. Situational Field AUTHORIZATIONS Box 36 Patient/Guardian Signature Required Field By signing this field the Patient acknowledge notification of the treatment plan and associated fees. The patient agrees to be responsible for all charges for dental services and materials not paid by the dental benefit plan. Note: claim with missing, incorrect, or incomplete patient/guardian signature will be rejected as non-processable. The provider must correct the claim and return it to First+Plus along with the non-processable form letter within the timeframe establish by the Prompt Payment Law of Puerto Rico. Box 37 Subscriber Signature/Date Required Field The Subscriber must sign the Claim Form or “Signature on File” can be provided. By given a statement of “Signature on File” the provider is attesting that there is an authorization on file for the release of any medical or other information necessary to process and/or adjudicate the claim, and that the subscriber is authorizing payment of the dental services to the dentist or dental entity included on the Claim Form Note: claim with missing, incorrect, or incomplete Subscriber signature will be rejected as non-processable. The provider must correct the claim and return it to First+Plus along with the non-processable form letter within the timeframe establish by the Prompt First+Plus payment law of Puerto Rico. Provider Manual 2013 202 ANCILLARY CLAIM/TREATMENT INFORMATION Box 38 Place of Treatment Required Field Check the applicable box • Must have one box checked Box 39 Number of enclosures Situational Field Check appropriate box DO NOT send radiographs to First+Plus for claims processing, except when root canal procedures are performed, or if a request is generated by First+Plus for claim processing and medical necessity review Box 40 Is the treatment for orthodontics? Not used by First+Plus Box 41 Date Appliance Placed Not used by First+Plus Box 42 Months of Treatment Remaining Not used by First+Plus Box 43 Replacement of Prosthesis Situational Field Check Yes or No • Must have one box checked • If No, do not complete fields 41 and 42 Provider Manual 2013 203 Box 44 Date Prior Placement Situational Field, if box 43 is checked Yes Enter date of prior placement in mmddccyy format, e.g.,08152013 Box 45 Treatment Resulting from Situational Field If the treatment is the result of an occupational illness/injury, auto accident, or other accident Check appropriate box If Box is checked, enter date of occupational illness/injury, auto or other accident in mmddccyy format, e.g.,08152013 Box 46 Situational Field, if any box in 45 is checked must enter date Enter date of occupational illness/injury, auto or other accident in mmddccyy format, e.g., 08152013 Box 47 Auto Accident State Situational Field Indicate the state in which the auto accident took place BILLING DENTIST OR DENTAL ENTITY Box 48 Name, Address, City State, Zip Code of the billing Dentist Required Field Enter the name of the billing dentist or group • The provider name entered in this field is the provider name that services will be reimbursed to and under which the monies will be reported to the Internal Revenue Service • The provider name must be entered the same way the provider is enrolled in First+Plus ; either Provider Manual 2013 204 • Individual providers billing and seeking reimbursement under their individual provider name; or • Group practices billing and seeking reimbursement under a group provider name Note: claim with missing, incorrect, or incomplete billing dentist name and address, will be rejected as non-processable. The provider must correct the claim and return it to First+Plus along with the non-processable form letter within the timeframe establish by the Prompt Payment Law of Puerto Rico. Enter the address of the billing dentist or group Box 49 NPI Required Field Enter the 10-digit billing provider’s NPI ( National Provider Identifier) Note: claim with missing, incorrect, or incomplete billing provider NPI number will be rejected as non-processable. The provider must correct the claim and return it to First+Plus along with the non-processable form letter within the timeframe establish by the Prompt Payment Law of Puerto Rico. Box 50 License number Required Field Note: claim with missing, incorrect, or incomplete license number will be rejected as nonprocessable. The provider must correct the claim and return it to First+Plus along with the non-processable form letter within the timeframe establish by the Prompt Payment Law of Puerto Rico. Box 51 Social Security Number (SSN) or Tax Identification Number (TIN) Required Field Enter the Billing Dentist or Dental Entity TIN or SSN • This number must match what First+Plus has in your contract file Note: claim with missing, incorrect, or incomplete SSN will be rejected as non-processable. The provider must correct the claim and return it to First+Plus along with the nonprocessable form letter within the timeframe establish by the Prompt Payment Law of Puerto Rico. Provider Manual 2013 205 Box 52 Phone Number Required Field Enter phone number for billing provider, in the event that First+Plus might need to contact you for further information Box 52a Additional Provider ID Situational Field Treating Dentist And Treatment Location Information Box 53 Signature or name of treating dentist and date Required field Enter the performing provider’s full name Enter date • Must be in mmddccyy format, e.g., 08152013 • Must be on or after the date of service Note: claim with missing, or incomplete signature will be rejected as non-processable. The provider must correct the claim and return it to First+Plus along with the non-processable form letter within the timeframe establish by the Prompt Payment Law of Puerto Rico. Box 54 Treating dentist NPI Required Field Enter the 10-digit performing provider’s NPI ( National Provider Identifier) Note: claim with missing, incorrect, or incomplete treating dentist NPI number will be rejected as non-processable. The provider must correct the claim and return it to First+Plus along with the non-processable form letter within the timeframe establish by the Prompt Payment Law of Puerto Rico. Box 55 License Number (of treating dentist) Required Field Provider Manual 2013 206 Box 56 Treating dentist Address, City, State, Zip Code Required Field Enter address for the treating provider Box 56a Provide specialty code Situational Field If an NPI is in Box 54 • Enter the corresponding 10 digit taxonomy code • Strongly suggested that a taxonomy code be provided when an NPI is in box 54 • The NPI number and corresponding taxonomy code must be on file with First+Plus Box 57 Phone Number Required Field The number First+Plus can use to contact you if there are questions re: your claim Box 58 Additional Provider ID Situational Field Other Relevant Information: Dental Services does not require pre-authorization. However, the provider must verify eligibility and confirm that the services and/or benefit have not been exhausted by the patient. Provider Manual 2013 207 ADJUSTMENT REASON CODES Adjustment Reason Codes are codes that describe the reason of the action taken on a claim line, or entire claim during the adjudication process. This allows the provider to review the payment or denial of a service for the required corrective action, if needed. The Adjustment Reason Codes are standard HIPAA CODES that are reviewed from time to time. A list of REMARK CODES associated with the Adjustment Reason Codes is included. Also, a list of User Defined Adj. Reason Codes is included for your reference. These codes are included on your EOP (Explanation of Payments). ADJUSTMENT REASON CODES USER DEFINED-CLAIMS DEPARTMENT ADJ REASON CODE DESCRIPTION U02 U06 U07 U08 U09 U11 U13 U17 U18 U19 U20 U21 U23 U24 U25 U26 AMAF Balance billing does not apply Original Medicare limiting charge Foreign Hospital -Member Reimbursement COB Information not received Settlement Claim Provider settlement -no payment Re-Coding HH Services No Legible claim Complete mouth x-rays limited to 3 yrs intervals Report does not justify emergency exam Non processable through CMS-1500 and/or 837P. Submit AMAF HHPPS RAP Claim Adjustment HHPPS Final Bill Payment Original payment void Full payment on final bill U28 Negative amount represents collection against receivable created in prior overpayment U29 U30 U31 U32 U34 U35 U36 U37 U38 Adjustment as result of MPFS fee update COB Claim Payment based on a contractual amount or agreement LUPA Payment For reporting purposes-No reimbursement to member applies Member has PDP coverage only OIG Exclusion List Provider Hospice Covered Service Claim-Bill Original MEDICARE Bill original MEDICARE for non-Hospice Services Provider Manual 2013 208 U39 U40 U41 U42 U44 U45 U46 U47 U48 U49 U50 U51 U52 U53 U54 U55 U56 U57 U58 U59 U60 U61 U62 U63 U64 U65 U66 U67 Hospice Claim----Submit correspondent Modifier No Cost-Sharing Hospice Payment Applies Hospice Claim-Submit correspondent Condition Code Service covered by Hospice Provider Revenue code submitted does not correspondent to the hospital review document VA Copayments not covered per MEDICARE Regulation Previous interest payment adjustment Service not contracted by provider Service not authorized Level of service not authorized by Medical Review Adjustment due to incorrect member ID Adjustment due to payment to incorrect provider Adjustment due to fee amounts Adjustment due to service code changes from the provider Adjustment due to changes in number of units Adjustment due to changes on dates Adjustment due to changes on level of service Adjustment due to combination of revenue codes and CPT Adjustment due to incorrect place of service Adjustment due to service date Adjustment due for corrections on Pointer Adjustment due to payment rules Adjustment due for duplicate payment Information submitted does not justify payment of this claim Service does not covered Benefit limit COB does not proceed Claim paid in full U68 No claim level adjustment U69 U70 U72 U73 U74 U76 U77 U78 U79 Medicare Secondary Payer Adjusted amount Procedure postponed, cancelled or delayed Missing invoice- Claim cannot be adjusted Level of care change per hospital review Level of care not approved by hospital review Denial days as per Hospital review determination claim denied -No supporting documentation submitted for review Incorrect revenue code submitted for service-see Contract Revenue code change- according to service provided and Contract U81 U86 Coverage not in effect at the time the service was provided Adjustment request received outside time limit Provider Manual 2013 209 U87 U88 U89 U91 U95 U96 U97 Hospital Review revenue code change-payment process on another line Same level of service but different revenue code as per hospital review Supplemental information for line of service is required Re-process due to original claim lines incomplete processing Claim line service dates are in conflict with related procedure code date of services Informative-Additional Day(s) -contracted surgery package Informative-Approved hospital days included on the contracted surgery package U104 Additional adjustment done on claim No payments proceed. Patient is responsible for payment of deductibles, co-payment and/or co-insurance according to the benefit coverage Charge(s) exceed the fee of the dental service code billed The procedure service code performed is required in addition to the billed code Please specify place of service Service previously processed and/or paid for the same tooth and/or surface under another dental procedure code Supplementary (Suppletory) prior to transplant Service not covered, usually use for orthodoncy services or major facial surgery Adjustment or repairs only proceed after six (6) months of insertion of denture or prosthesis Case was evaluated by dental consultant Not paid under OPPS AMAF Balance billing does not apply Original Medicare limiting charge Foreign hospital-member reimbursement COB information not received Settlement claim Provider settlement-no payment Re-coding HH services No legible claim Complete mouth x-rays limited to 3 yrs. intervals report does not justify emergency exam Non processable through cms-1500 and/or 837p. submit AMAF HHPPS rap claim adjustment HHPPS final bill payment Original payment void Full payment on final bill Negative amount represents collection against receivable created in prior overpayment Adjustment as result of MPFS fee update COB claim Payment based on a contractual amount or agreement U105 U106 U107 U109 U110 U111 U112 U113 U114 U115 U02 U06 U07 U08 U09 U11 U13 U17 U18 U19 U20 U21 U23 U24 U25 U26 U28 U29 U30 U31 Provider Manual 2013 210 U32 U34 U35 U36 U37 U38 U39 U40 U41 U42 U44 U45 U46 U47 U48 U49 U50 U51 U52 U53 U54 U55 U56 U57 U58 U59 U60 U61 U62 U63 U64 U65 U66 U67 Lupa payment For reporting purposes-no reimbursement to member applies Member has PDP coverage only OIG exclusion list provider Hospice covered service claim-bill original Medicare Bill original Medicare for non-hospice services Hospice claim submit correspondent modifier No cost-sharing hospice payment applies Hospice claim submit correspondent condition code Service covered by hospice provider Revenue code submitted is not correct according with audit Copayments not covered per Medicare regulation Previous interest payment adjustment Service not contracted by provider Service not authorized Level of service not authorized by medical review Adjustment incorrect affiliate number Adjustment payment to the provider wrong Adjustment for differences in rates Adjustment for changes in codes by the providers Adjustment for difference in number of units Adjustment for change in dates Adjustment for change in level of service Adjustment by combination of revenue code with CPT Adjustment wrong place of services Adjustment in date of services Adjustment pointer corrección Adjustment payment rule Adjustment duplicated payment Information submitted does not justify the payment of this claim Service not covered Benefit Limit COB does not proceed Claim paid in full U68 No claim level adjustment U69 U70 U72 U73 U74 U76 Medicare secondary payer adjustment amount Procedure postponed, canceled or delayed Missing invoice- claims cannot be adjusted Level of care change per hospital review Level of care not approved by hospital review Denial days as per Hospital review determination Provider Manual 2013 211 U77 U78 U79 Claim denied -No supporting documentation submitted for review Incorrect revenue code submitted for service-see Contract Revenue code change- according to service provided and Contract U81 U86 U87 U88 U89 U91 U95 U96 U97 U104 Coverage not in effect at the time the service was provided Adjustment Request received out the stipulated time Hospital Review revenue code change-payment process on another line Same level of service but different revenue code as per hospital review Supplemental information for line of service is required Re-process due to original claim lines incomplete processing Claim line service dates are in conflict with related procedure code date of services Informativo-Día(s) adicional(es)-paquete de cirugía contratado Informativo-Días de estadía aprobados incluidos en paquete de cirugía contratado Additional adjustment done on claim Not applicable payment. Patient is responsible for payment, deductibles, copayments and / or coinsurance according with benefits covered Charges exceed dental code rate Code is required procedure performed service in addition to code billed Please specify place of service U105 U106 U107 U109 Provider Manual 2013 212 CLAIM ADJUSTMENT REASON CODES 1 Deductible Amount Start: 01/01/1995 2 Coinsurance Amount Start: 01/01/1995 3 Co-payment Amount Start: 01/01/1995 4 The procedure code is inconsistent with the modifier used or a required modifier is missing. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 5 The procedure code/bill type is inconsistent with the place of service. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 6 The procedure/revenue code is inconsistent with the patient's age. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 7 The procedure/revenue code is inconsistent with the patient's gender. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 8 The procedure code is inconsistent with the provider type/specialty (taxonomy). Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 9 The diagnosis is inconsistent with the patient's age. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 10 The diagnosis is inconsistent with the patient's gender. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 11 The diagnosis is inconsistent with the procedure. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 12 The diagnosis is inconsistent with the provider type. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 13 The date of death precedes the date of service. Start: 01/01/1995 14 The date of birth follows the date of service. Start: 01/01/1995 15 The authorization number is missing, invalid, or does not apply to the billed services or provider. Start: 01/01/1995 | Last Modified: 09/30/2007 16 Claim/service lacks information which is needed for adjudication. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) This change effective 11/1/2013: Claim/service lacks information or has submission/billing error(s) which is needed for adjudication. Do not use this code for claims attachment(s). At least one Remark Code must be provided (may be comprised of ei- Provider Manual 2013 213 ther the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 01/20/2013 17 Requested information was not provided or was insufficient/incomplete. At least one Remark Code must be provided (may be comprised of either the Remittance Advice Remark Code or NCPDP Reject Reason Code.) Start: 01/01/1995 | Last Modified: 09/21/2008 | Stop: 07/01/2009 18 Exact duplicate claim/service (Use only with Group Code OA) Start: 01/01/1995 | Last Modified: 01/20/2013 19 This is a work-related injury/illness and thus the liability of the Worker's Compensation Carrier. Start: 01/01/1995 | Last Modified: 09/30/2007 20 This injury/illness is covered by the liability carrier. Start: 01/01/1995 | Last Modified: 09/30/2007 21 This injury/illness is the liability of the no-fault carrier. Start: 01/01/1995 | Last Modified: 09/30/2007 22 This care may be covered by another payer per coordination of benefits. Start: 01/01/1995 | Last Modified: 09/30/2007 23 The impact of prior payer(s) adjudication including payments and/or adjustments. (Use only with Group Code OA) Start: 01/01/1995 | Last Modified: 09/30/2012 24 Charges are covered under a capitation agreement/managed care plan. Start: 01/01/1995 | Last Modified: 09/30/2007 25 Payment denied. Your Stop loss deductible has not been met. Start: 01/01/1995 | Stop: 04/01/2008 26 Expenses incurred prior to coverage. Start: 01/01/1995 27 Expenses incurred after coverage terminated. Start: 01/01/1995 28 Coverage not in effect at the time the service was provided. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Redundant to codes 26&27. 29 The time limit for filing has expired. Start: 01/01/1995 30 Payment adjusted because the patient has not met the required eligibility, spend down, waiting, or residency requirements. Start: 01/01/1995 | Stop: 02/01/2006 31 Patient cannot be identified as our insured. Start: 01/01/1995 | Last Modified: 09/30/2007 32 Our records indicate that this dependent is not an eligible dependent as defined. Start: 01/01/1995 33 Insured has no dependent coverage. Start: 01/01/1995 | Last Modified: 09/30/2007 34 Insured has no coverage for newborns. Provider Manual 2013 214 Start: 01/01/1995 | Last Modified: 09/30/2007 35 Lifetime benefit maximum has been reached. Start: 01/01/1995 | Last Modified: 10/31/2002 36 Balance does not exceed co-payment amount. Start: 01/01/1995 | Stop: 10/16/2003 37 Balance does not exceed deductible. Start: 01/01/1995 | Stop: 10/16/2003 38 Services not provided or authorized by designated (network/primary care) providers. Start: 01/01/1995 | Last Modified: 06/30/2003 | Stop: 01/01/2013 39 Services denied at the time authorization/pre-certification was requested. Start: 01/01/1995 40 Charges do not meet qualifications for emergent/urgent care. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 41 Discount agreed to in Preferred Provider contract. Start: 01/01/1995 | Stop: 10/16/2003 42 Charges exceed our fee schedule or maximum allowable amount. (Use CARC 45) Start: 01/01/1995 | Last Modified: 10/31/2006 | Stop: 06/01/2007 43 Gramm-Rudman reduction. Start: 01/01/1995 | Stop: 07/01/2006 44 Prompt-pay discount. Start: 01/01/1995 45 Charge exceeds fee schedule/maximum allowable or contracted/legislated fee arrangement. (Use Group Codes PR or CO depending upon liability). This change effective 7/1/2013: Charge exceeds fee schedule/maximum allowable or contracted/legislated fee arrangement. (Use only with Group Codes PR or CO depending upon liability) Start: 01/01/1995 | Last Modified: 09/30/2012 46 This (these) service(s) is (are) not covered. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 96. 47 This (these) diagnosis(es) is (are) not covered, missing, or are invalid. Start: 01/01/1995 | Stop: 02/01/2006 48 This (these) procedure(s) is (are) not covered. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 96. 49 These are non-covered services because this is a routine exam or screening procedure done in conjunction with a routine exam. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. This change effective 11/1/2013: This is a non-covered service because it is a routine/preventive exam or a diagnostic/screening procedure done in conjunction with a routine/preventive exam. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 01/20/2013 50 These are non-covered services because this is not deemed a 'medical necessity' by the payer. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 Provider Manual 2013 215 51 These are non-covered services because this is a pre-existing condition. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 52 The referring/prescribing/rendering provider is not eligible to refer/prescribe/order/perform the service billed. Start: 01/01/1995 | Stop: 02/01/2006 53 Services by an immediate relative or a member of the same household are not covered. Start: 01/01/1995 54 Multiple physicians/assistants are not covered in this case. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 55 Procedure/treatment is deemed experimental/investigational by the payer. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 56 Procedure/treatment has not been deemed 'proven to be effective' by the payer. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 57 Payment denied/reduced because the payer deems the information submitted does not support this level of service, this many services, this length of service, this dosage, or this day's supply. Start: 01/01/1995 | Stop: 06/30/2007 Notes: Split into codes 150, 151, 152, 153 and 154. 58 Treatment was deemed by the payer to have been rendered in an inappropriate or invalid place of service. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 59 Processed based on multiple or concurrent procedure rules. (For example multiple surgery or diagnostic imaging, concurrent anesthesia.) Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 60 Charges for outpatient services are not covered when performed within a period of time prior to or after inpatient services. Start: 01/01/1995 | Last Modified: 06/01/2008 61 Penalty for failure to obtain second surgical opinion. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 62 Payment denied/reduced for absence of, or exceeded, pre-certification/authorization. Start: 01/01/1995 | Last Modified: 10/31/2006 | Stop: 04/01/2007 63 Correction to a prior claim. Start: 01/01/1995 | Stop: 10/16/2003 64 Denial reversed per Medical Review. Start: 01/01/1995 | Stop: 10/16/2003 65 Procedure code was incorrect. This payment reflects the correct code. Start: 01/01/1995 | Stop: 10/16/2003 66 Blood Deductible. Start: 01/01/1995 67 Lifetime reserve days. (Handled in QTY, QTY01=LA) Provider Manual 2013 216 Start: 01/01/1995 | Stop: 10/16/2003 68 DRG weight. (Handled in CLP12) Start: 01/01/1995 | Stop: 10/16/2003 69 Day outlier amount. Start: 01/01/1995 70 Cost outlier - Adjustment to compensate for additional costs. Start: 01/01/1995 | Last Modified: 06/30/2001 71 Primary Payer amount. Start: 01/01/1995 | Stop: 06/30/2000 Notes: Use code 23. 72 Coinsurance day. (Handled in QTY, QTY01=CD) Start: 01/01/1995 | Stop: 10/16/2003 73 Administrative days. Start: 01/01/1995 | Stop: 10/16/2003 74 Indirect Medical Education Adjustment. Start: 01/01/1995 75 Direct Medical Education Adjustment. Start: 01/01/1995 76 Disproportionate Share Adjustment. Start: 01/01/1995 77 Covered days. (Handled in QTY, QTY01=CA) Start: 01/01/1995 | Stop: 10/16/2003 78 Non-Covered days/Room charge adjustment. Start: 01/01/1995 79 Cost Report days. (Handled in MIA15) Start: 01/01/1995 | Stop: 10/16/2003 80 Outlier days. (Handled in QTY, QTY01=OU) Start: 01/01/1995 | Stop: 10/16/2003 81 Discharges. Start: 01/01/1995 | Stop: 10/16/2003 82 PIP days. Start: 01/01/1995 | Stop: 10/16/2003 83 Total visits. Start: 01/01/1995 | Stop: 10/16/2003 84 Capital Adjustment. (Handled in MIA) Start: 01/01/1995 | Stop: 10/16/2003 85 Patient Interest Adjustment (Use Only Group code PR) Start: 01/01/1995 | Last Modified: 07/09/2007 Notes: Only use when the payment of interest is the responsibility of the patient. 86 Statutory Adjustment. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Duplicative of code 45. Provider Manual 2013 217 87 Transfer amount. Start: 01/01/1995 | Last Modified: 09/20/2009 | Stop: 01/01/2012 88 Adjustment amount represents collection against receivable created in prior overpayment. Start: 01/01/1995 | Stop: 06/30/2007 89 Professional fees removed from charges. Start: 01/01/1995 90 Ingredient cost adjustment. Note: To be used for pharmaceuticals only. Start: 01/01/1995 | Last Modified: 07/01/2009 91 Dispensing fee adjustment. Start: 01/01/1995 92 Claim Paid in full. Start: 01/01/1995 | Stop: 10/16/2003 93 No Claim level Adjustments. Start: 01/01/1995 | Stop: 10/16/2003 Notes: As of 004010, CAS at the claim level is optional. 94 Processed in Excess of charges. Start: 01/01/1995 95 Plan procedures not followed. Start: 01/01/1995 | Last Modified: 09/30/2007 96 Non-covered charge(s). At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 97 The benefit for this service is included in the payment/allowance for another service/procedure that has already been adjudicated. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 98 The hospital must file the Medicare claim for this inpatient non-physician service. Start: 01/01/1995 | Stop: 10/16/2003 99 Medicare Secondary Payer Adjustment Amount. Start: 01/01/1995 | Stop: 10/16/2003 100 Payment made to patient/insured/responsible party/employer. Start: 01/01/1995 | Last Modified: 01/27/2008 101 Predetermination: anticipated payment upon completion of services or claim adjudication. Start: 01/01/1995 | Last Modified: 02/28/1999 102 Major Medical Adjustment. Start: 01/01/1995 103 Provider promotional discount (e.g., Senior citizen discount). Start: 01/01/1995 | Last Modified: 06/30/2001 104 Managed care withholding. Start: 01/01/1995 105 Tax withholding. Start: 01/01/1995 106 Patient payment option/election not in effect. Start: 01/01/1995 Provider Manual 2013 218 107 The related or qualifying claim/service was not identified on this claim. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 108 Rent/purchase guidelines were not met. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 109 Claim/service not covered by this payer/contractor. You must send the claim/service to the correct payer/contractor. Start: 01/01/1995 | Last Modified: 01/29/2012 110 Billing date predates service date. Start: 01/01/1995 111 Not covered unless the provider accepts assignment. Start: 01/01/1995 112 Service not furnished directly to the patient and/or not documented. Start: 01/01/1995 | Last Modified: 09/30/2007 113 Payment denied because service/procedure was provided outside the United States or as a result of war. Start: 01/01/1995 | Last Modified: 02/28/2001 | Stop: 06/30/2007 Notes: Use Codes 157, 158 or 159. 114 Procedure/product not approved by the Food and Drug Administration. Start: 01/01/1995 115 Procedure postponed, canceled, or delayed. Start: 01/01/1995 | Last Modified: 09/30/2007 116 The advance indemnification notice signed by the patient did not comply with requirements. Start: 01/01/1995 | Last Modified: 09/30/2007 117 Transportation is only covered to the closest facility that can provide the necessary care. Start: 01/01/1995 | Last Modified: 09/30/2007 118 ESRD network support adjustment. Start: 01/01/1995 | Last Modified: 09/30/2007 119 Benefit maximum for this time period or occurrence has been reached. Start: 01/01/1995 | Last Modified: 02/29/2004 120 Patient is covered by a managed care plan. Start: 01/01/1995 | Stop: 06/30/2007 Notes: Use code 24. 121 Indemnification adjustment - compensation for outstanding member responsibility. Start: 01/01/1995 | Last Modified: 09/30/2007 122 Psychiatric reduction. Start: 01/01/1995 123 Payer refund due to overpayment. Start: 01/01/1995 | Stop: 06/30/2007 Notes: Refer to implementation guide for proper handling of reversals. 124 Payer refund amount - not our patient. Start: 01/01/1995 | Last Modified: 06/30/1999 | Stop: 06/30/2007 Notes: Refer to implementation guide for proper handling of reversals. Provider Manual 2013 219 125 Submission/billing error(s). At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 01/01/1995 | Last Modified: 09/20/2009 | Stop: 11/01/2013 126 Deductible -- Major Medical Start: 02/28/1997 | Last Modified: 09/30/2007 | Stop: 04/01/2008 Notes: Use Group Code PR and code 1. 127 Coinsurance -- Major Medical Start: 02/28/1997 | Last Modified: 09/30/2007 | Stop: 04/01/2008 Notes: Use Group Code PR and code 2. 128 Newborn's services are covered in the mother's Allowance. Start: 02/28/1997 129 Prior processing information appears incorrect. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 02/28/1997 | Last Modified: 01/30/2011 130 Claim submission fee. Start: 02/28/1997 | Last Modified: 06/30/2001 131 Claim specific negotiated discount. Start: 02/28/1997 132 Prearranged demonstration project adjustment. Start: 02/28/1997 133 The disposition of the claim/service is pending further review. (Use only with Group Code OA) Start: 02/28/1997 | Last Modified: 01/20/2013 134 Technical fees removed from charges. Start: 10/31/1998 135 Interim bills cannot be processed. Start: 10/31/1998 | Last Modified: 09/30/2007 136 Failure to follow prior payer's coverage rules. (Use Group Code OA). This change effective 7/1/2013: Failure to follow prior payer's coverage rules. (Use only with Group Code OA) Start: 10/31/1998 | Last Modified: 09/30/2012 137 Regulatory Surcharges, Assessments, Allowances or Health Related Taxes. Start: 02/28/1999 | Last Modified: 09/30/2007 138 Appeal procedures not followed or time limits not met. Start: 06/30/1999 | Last Modified: 09/30/2007 139 Contracted funding agreement - Subscriber is employed by the provider of services. Start: 06/30/1999 140 Patient/Insured health identification number and name do not match. Start: 06/30/1999 141 Claim spans eligible and ineligible periods of coverage. Start: 06/30/1999 | Last Modified: 09/30/2007 | Stop: 07/01/2012 142 Monthly Medicaid patient liability amount. Start: 06/30/2000 | Last Modified: 09/30/2007 143 Portion of payment deferred. Start: 02/28/2001 Provider Manual 2013 220 144 Incentive adjustment, e.g. preferred product/service. Start: 06/30/2001 145 Premium payment withholding Start: 06/30/2002 | Last Modified: 09/30/2007 | Stop: 04/01/2008 Notes: Use Group Code CO and code 45. 146 Diagnosis was invalid for the date(s) of service reported. Start: 06/30/2002 | Last Modified: 09/30/2007 147 Provider contracted/negotiated rate expired or not on file. Start: 06/30/2002 148 Information from another provider was not provided or was insufficient/incomplete. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 06/30/2002 | Last Modified: 09/20/2009 149 Lifetime benefit maximum has been reached for this service/benefit category. Start: 10/31/2002 150 Payer deems the information submitted does not support this level of service. Start: 10/31/2002 | Last Modified: 09/30/2007 151 Payment adjusted because the payer deems the information submitted does not support this many/frequency of services. Start: 10/31/2002 | Last Modified: 01/27/2008 152 Payer deems the information submitted does not support this length of service. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 10/31/2002 | Last Modified: 09/20/2009 153 Payer deems the information submitted does not support this dosage. Start: 10/31/2002 | Last Modified: 09/30/2007 154 Payer deems the information submitted does not support this day's supply. Start: 10/31/2002 | Last Modified: 09/30/2007 155 Patient refused the service/procedure. Start: 06/30/2003 | Last Modified: 09/30/2007 156 Flexible spending account payments. Note: Use code 187. Start: 09/30/2003 | Last Modified: 01/25/2009 | Stop: 10/01/2009 157 Service/procedure was provided as a result of an act of war. Start: 09/30/2003 | Last Modified: 09/30/2007 158 Service/procedure was provided outside of the United States. Start: 09/30/2003 | Last Modified: 09/30/2007 159 Service/procedure was provided as a result of terrorism. Start: 09/30/2003 | Last Modified: 09/30/2007 160 Injury/illness was the result of an activity that is benefit exclusion. Start: 09/30/2003 | Last Modified: 09/30/2007 161 Provider performance bonus Start: 02/29/2004 162 State-mandated Requirement for Property and Casualty, see Claim Payment Remarks Code for specific explanation. Start: 02/29/2004 Provider Manual 2013 221 163 Attachment referenced on the claim was not received. Start: 06/30/2004 | Last Modified: 09/30/2007 164 Attachment referenced on the claim was not received in a timely fashion. Start: 06/30/2004 | Last Modified: 09/30/2007 165 Referral absent or exceeded. Start: 10/31/2004 | Last Modified: 09/30/2007 166 These services were submitted after this payers responsibility for processing claims under this plan ended. Start: 02/28/2005 167 This (these) diagnosis(es) is (are) not covered. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/30/2005 | Last Modified: 09/20/2009 168 Service(s) have been considered under the patient's medical plan. Benefits are not available under this dental plan. Start: 06/30/2005 | Last Modified: 09/30/2007 169 Alternate benefit has been provided. Start: 06/30/2005 | Last Modified: 09/30/2007 170 Payment is denied when performed/billed by this type of provider. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/30/2005 | Last Modified: 09/20/2009 171 Payment is denied when performed/billed by this type of provider in this type of facility. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/30/2005 | Last Modified: 09/20/2009 172 Payment is adjusted when performed/billed by a provider of this specialty. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/30/2005 | Last Modified: 09/20/2009 173 Service was not prescribed by a physician. This change effective 7/1/2013: Service/equipment was not prescribed by a physician. Start: 06/30/2005 | Last Modified: 09/30/2012 174 Service was not prescribed prior to delivery. Start: 06/30/2005 | Last Modified: 09/30/2007 175 Prescription is incomplete. Start: 06/30/2005 | Last Modified: 09/30/2007 176 Prescription is not current. Start: 06/30/2005 | Last Modified: 09/30/2007 177 Patient has not met the required eligibility requirements. Start: 06/30/2005 | Last Modified: 09/30/2007 178 Patient has not met the required spend down requirements. Start: 06/30/2005 | Last Modified: 09/30/2007 179 Patient has not met the required waiting requirements. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/30/2005 | Last Modified: 09/20/2009 180 Patient has not met the required residency requirements. Start: 06/30/2005 | Last Modified: 09/30/2007 181 Procedure code was invalid on the date of service. Start: 06/30/2005 | Last Modified: 09/30/2007 Provider Manual 2013 222 182 Procedure modifier was invalid on the date of service. Start: 06/30/2005 | Last Modified: 09/30/2007 183 The referring provider is not eligible to refer the service billed. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/30/2005 | Last Modified: 09/20/2009 184 The prescribing/ordering provider is not eligible to prescribe/order the service billed. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/30/2005 | Last Modified: 09/20/2009 185 The rendering provider is not eligible to perform the service billed. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/30/2005 | Last Modified: 09/20/2009 186 Level of care change adjustment. Start: 06/30/2005 | Last Modified: 09/30/2007 187 Consumer Spending Account payments (includes but is not limited to Flexible Spending Account, Health Savings Account, Health Reimbursement Account, etc.) Start: 06/30/2005 | Last Modified: 01/25/2009 188 This product/procedure is only covered when used according to FDA recommendations. Start: 06/30/2005 189 'Not otherwise classified' or 'unlisted' procedure code (CPT/HCPCS) was billed when there is a specific procedure code for this procedure/service Start: 06/30/2005 190 Payment is included in the allowance for a Skilled Nursing Facility (SNF) qualified stay. Start: 10/31/2005 191 Not a work related injury/illness and thus not the liability of the workers' compensation carrier Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segments (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF) Start: 10/31/2005 | Last Modified: 10/17/2010 192 Nonstandard adjustment code from paper remittance. Note: This code is to be used by providers/payers providing Coordination of Benefits information to another payer in the 837 transaction only. This code is only used when the non-standard code cannot be reasonably mapped to an existing Claims Adjustment Reason Code, specifically Deductible, Coinsurance and Co-payment. Start: 10/31/2005 | Last Modified: 09/30/2007 193 Original payment decision is being maintained. Upon review, it was determined that this claim was processed properly. Start: 02/28/2006 | Last Modified: 01/27/2008 194 Anesthesia performed by the operating physician, the assistant surgeon or the attending physician. Start: 02/28/2006 | Last Modified: 09/30/2007 195 Refund issued to an erroneous priority payer for this claim/service. Start: 02/28/2006 | Last Modified: 09/30/2007 196 Claim/service denied based on prior payer's coverage determination. Start: 06/30/2006 | Stop: 02/01/2007 Notes: Use code 136. 197 Precertification/authorization/notification absent. Start: 10/31/2006 | Last Modified: 09/30/2007 Provider Manual 2013 223 198 Precertification/authorization exceeded. Start: 10/31/2006 | Last Modified: 09/30/2007 199 Revenue code and Procedure code do not match. Start: 10/31/2006 200 Expenses incurred during lapse in coverage Start: 10/31/2006 201 Workers' Compensation case settled. Patient is responsible for amount of this claim/service through WC 'Medicare set aside arrangement' or other agreement. (Use group code PR). This change effective 7/1/2013: Workers Compensation case settled. Patient is responsible for amount of this claim/service through WC 'Medicare set aside arrangement' or other agreement. (Use only with Group Code PR) Start: 10/31/2006 | Last Modified: 09/30/2012 202 Non-covered personal comfort or convenience services. Start: 02/28/2007 | Last Modified: 09/30/2007 203 Discontinued or reduced service. Start: 02/28/2007 | Last Modified: 09/30/2007 204 This service/equipment/drug is not covered under the patient’s current benefit plan Start: 02/28/2007 205 Pharmacy discount card processing fee Start: 07/09/2007 206 National Provider Identifier - missing. Start: 07/09/2007 | Last Modified: 09/30/2007 207 National Provider identifier - Invalid format Start: 07/09/2007 | Last Modified: 06/01/2008 208 National Provider Identifier - Not matched. Start: 07/09/2007 | Last Modified: 09/30/2007 209 Per regulatory or other agreement. The provider cannot collect this amount from the patient. However, this amount may be billed to subsequent payer. Refund to patient if collected. (Use Group code OA) This change effective 7/1/2013: Per regulatory or other agreement. The provider cannot collect this amount from the patient. However, this amount may be billed to subsequent payer. Refund to patient if collected. (Use only with Group code OA) Start: 07/09/2007 | Last Modified: 09/30/2012 210 Payment adjusted because pre-certification/authorization not received in a timely fashion Start: 07/09/2007 211 National Drug Codes (NDC) not eligible for rebate, are not covered. Start: 07/09/2007 212 Administrative surcharges are not covered Start: 11/05/2007 213 Non-compliance with the physician self-referral prohibition legislation or payer policy. Start: 01/27/2008 214 Workers' Compensation claim adjudicated as non-compensable. This Payer not liable for claim or service/treatment. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segment (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). To be used for Workers' Compensation only Start: 01/27/2008 | Last Modified: 10/17/2010 Provider Manual 2013 224 215 Based on subrogation of a third party settlement Start: 01/27/2008 216 Based on the findings of a review organization Start: 01/27/2008 217 Based on payer reasonable and customary fees. No maximum allowable defined by legislated fee arrangement. (Note: To be used for Property and Casualty only) Start: 01/27/2008 | Last Modified: 09/30/2012 218 Based on entitlement to benefits. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segment (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). To be used for Workers' Compensation only Start: 01/27/2008 | Last Modified: 10/17/2010 219 Based on extent of injury. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segment (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). Start: 01/27/2008 | Last Modified: 10/17/2010 220 The applicable fee schedule/fee database does not contain the billed code. Please resubmit a bill with the appropriate fee schedule/fee database code(s) that best describe the service(s) provided and supporting documentation if required. (Note: To be used for Property and Casualty only) Start: 01/27/2008 | Last Modified: 09/30/2012 221 Workers' Compensation claim is under investigation. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segment (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). This change effective 7/1/2013: Claim is under investigation. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segment (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). (Note: To be used by Property & Casualty only) Start: 01/27/2008 | Last Modified: 09/30/2012 222 Exceeds the contracted maximum number of hours/days/units by this provider for this period. This is not patient specific. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/01/2008 | Last Modified: 09/20/2009 223 Adjustment code for mandated federal, state or local law/regulation that is not already covered by another code and is mandated before a new code can be created. Start: 06/01/2008 SEQUESTRATION ONLY - IS DONE BY THE EZCAP SYSTEM AUTOMATICALLY 224 Patient identification compromised by identity theft. Identity verification required for processing this and future claims. Start: 06/01/2008 225 Penalty or Interest Payment by Payer (Only used for plan to plan encounter reporting within the 837) Start: 06/01/2008 226 Information requested from the Billing/Rendering Provider was not provided or was insufficient/incomplete. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) This change effective 7/1/2013: Information requested from the Billing/Rendering Provider was not provided or not provided timely or was insufficient/incomplete. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 09/21/2008 | Last Modified: 09/30/2012 Provider Manual 2013 225 227 Information requested from the patient/insured/responsible party was not provided or was insufficient/incomplete. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 09/21/2008 | Last Modified: 09/20/2009 228 Denied for failure of this provider, another provider or the subscriber to supply requested information to a previous payer for their adjudication Start: 09/21/2008 229 Partial charge amount not considered by Medicare due to the initial claim Type of Bill being 12X. Note: This code can only be used in the 837 transaction to convey Coordination of Benefits information when the secondary payer's cost avoidance policy allows providers to bypass claim submission to a prior payer. Use Group Code PR. This change effective 7/1/2013: Partial charge amount not considered by Medicare due to the initial claim Type of Bill being 12X. Note: This code can only be used in the 837 transaction to convey Coordination of Benefits information when the secondary payer's cost avoidance policy allows providers to bypass claim submission to a prior payer. (Use only with Group Code PR) Start: 01/25/2009 | Last Modified: 09/30/2012 230 No available or correlating CPT/HCPCS code to describe this service. Note: Used only by Property and Casualty. Start: 01/25/2009 231 Mutually exclusive procedures cannot be done in the same day/setting. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 07/01/2009 | Last Modified: 09/20/2009 232 Institutional Transfer Amount. Note - Applies to institutional claims only and explains the DRG amount difference when the patient care crosses multiple institutions. Start: 11/01/2009 233 Services/charges related to the treatment of a hospital-acquired condition or preventable medical error. Start: 01/24/2010 234 This procedure is not paid separately. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 01/24/2010 235 Sales Tax Start: 06/06/2010 236 This procedure or procedure/modifier combination is not compatible with another procedure or procedure/modifier combination provided on the same day according to the National Correct Coding Initiative. This change effective 7/1/2013: This procedure or procedure/modifier combination is not compatible with another procedure or procedure/modifier combination provided on the same day according to the National Correct Coding Initiative or workers compensation state regulations/ fee schedule requirements. Start: 01/30/2011 | Last Modified: 09/30/2012 237 Legislated/Regulatory Penalty. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 06/05/2011 238 Claim spans eligible and ineligible periods of coverage, this is the reduction for the ineligible period (use Group Code PR). This change effective 7/1/2013: Claim spans eligible and ineligible periods of coverage, this is the reduction for the ineligible period. (Use only with Group Code PR) Start: 03/01/2012 | Last Modified: 09/30/2012 239 Claim spans eligible and ineligible periods of coverage. Rebill separate claims. Start: 03/01/2012 | Last Modified: 01/29/2012 240 The diagnosis is inconsistent with the patient's birth weight. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Provider Manual 2013 226 Start: 06/03/2012 241 Low Income Subsidy (LIS) Co-payment Amount Start: 06/03/2012 242 Services not provided by network/primary care providers. Start: 06/03/2012 243 Services not authorized by network/primary care providers. Start: 06/03/2012 244 Payment reduced to zero due to litigation. Additional information will be sent following the conclusion of litigation. To be used for Property & Casualty only. Start: 09/30/2012 245 Provider performance program withhold. Start: 09/30/2012 246 This non-payable code is for required reporting only. Start: 09/30/2012 247 248 249 Deductible for Professional service rendered in an Institutional setting and billed on an Institutional claim. Start: 09/30/2012 Notes: For Medicare Bundled Payment use only, under the Patient Protection and Affordable Care Act (PPACA). Coinsurance for Professional service rendered in an Institutional setting and billed on an Institutional claim. Start: 09/30/2012 Notes: For Medicare Bundled Payment use only, under the Patient Protection and Affordable Care Act (PPACA). This claim has been identified as a readmission. (Use only with Group Code CO) Start: 09/30/2012 250 The attachment content received is inconsistent with the expected content. Start: 09/30/2012 251 The attachment content received did not contain the content required to process this claim or service. Start: 09/30/2012 252 An attachment is required to adjudicate this claim/service. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). Start: 09/30/2012 A0 Patient refund amount. Start: 01/01/1995 A1 Claim/Service denied. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 01/01/1995 | Last Modified: 09/20/2009 A2 Contractual adjustment. Start: 01/01/1995 | Last Modified: 02/28/2007 | Stop: 01/01/2008 Notes: Use Code 45 with Group Code 'CO' or use another appropriate specific adjustment code. A3 Medicare Secondary Payer liability met. Start: 01/01/1995 | Stop: 10/16/2003 A4 Medicare Claim PPS Capital Day Outlier Amount. Start: 01/01/1995 | Last Modified: 09/30/2007 | Stop: 04/01/2008 Provider Manual 2013 227 A5 Medicare Claim PPS Capital Cost Outlier Amount. Start: 01/01/1995 A6 Prior hospitalization or 30 day transfer requirement not met. Start: 01/01/1995 A7 Presumptive Payment Adjustment Start: 01/01/1995 A8 Ungroupable DRG. Start: 01/01/1995 | Last Modified: 09/30/2007 B1 Non-covered visits. Start: 01/01/1995 B2 Covered visits. Start: 01/01/1995 | Stop: 10/16/2003 B3 Covered charges. Start: 01/01/1995 | Stop: 10/16/2003 B4 Late filing penalty. Start: 01/01/1995 B5 Coverage/program guidelines were not met or were exceeded. Start: 01/01/1995 | Last Modified: 09/30/2007 B6 This payment is adjusted when performed/billed by this type of provider, by this type of provider in this type of facility, or by a provider of this specialty. Start: 01/01/1995 | Stop: 02/01/2006 B7 This provider was not certified/eligible to be paid for this procedure/service on this date of service. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 B8 Alternative services were available, and should have been utilized. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 B9 Patient is enrolled in a Hospice. Start: 01/01/1995 | Last Modified: 09/30/2007 B10 Allowed amount has been reduced because a component of the basic procedure/test was paid. The beneficiary is not liable for more than the charge limit for the basic procedure/test. Start: 01/01/1995 B11 The claim/service has been transferred to the proper payer/processor for processing. Claim/service not covered by this payer/processor. Start: 01/01/1995 B12 Services not documented in patients' medical records. Start: 01/01/1995 B13 Previously paid. Payment for this claim/service may have been provided in a previous payment. Start: 01/01/1995 B14 Only one visit or consultation per physician per day is covered. Start: 01/01/1995 | Last Modified: 09/30/2007 B15 This service/procedure requires that a qualifying service/procedure be received and covered. The qualifying other service/procedure has not been received/adjudicated. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 Provider Manual 2013 228 B16 'New Patient' qualifications were not met. Start: 01/01/1995 | Last Modified: 09/30/2007 B17 Payment adjusted because this service was not prescribed by a physician, not prescribed prior to delivery, the prescription is incomplete, or the prescription is not current. Start: 01/01/1995 | Stop: 02/01/2006 B18 This procedure code and modifier were invalid on the date of service. Start: 01/01/1995 | Last Modified: 09/21/2008 | Stop: 03/01/2009 B19 Claim/service adjusted because of the finding of a Review Organization. Start: 01/01/1995 | Stop: 10/16/2003 B20 Procedure/service was partially or fully furnished by another provider. Start: 01/01/1995 | Last Modified: 09/30/2007 B21 The charges were reduced because the service/care was partially furnished by another physician. Start: 01/01/1995 | Stop: 10/16/2003 B22 This payment is adjusted based on the diagnosis. Start: 01/01/1995 | Last Modified: 02/28/2001 B23 Procedure billed is not authorized per your Clinical Laboratory Improvement Amendment (CLIA) proficiency test. Start: 01/01/1995 | Last Modified: 09/30/2007 D1 Claim/service denied. Level of subluxation is missing or inadequate. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D2 Claim lacks the name, strength, or dosage of the drug furnished. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D3 Claim/service denied because information to indicate if the patient owns the equipment that requires the part or supply was missing. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D4 Claim/service does not indicate the period of time for which this will be needed. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D5 Claim/service denied. Claim lacks individual lab codes included in the test. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D6 Claim/service denied. Claim did not include patient's medical record for the service. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D7 Claim/service denied. Claim lacks date of patient's most recent physician visit. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D8 Claim/service denied. Claim lacks indicator that 'x-ray is available for review.' Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D9 Claim/service denied. Claim lacks invoice or statement certifying the actual cost of the lens, less discounts or the type of intraocular lens used. Provider Manual 2013 229 Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D10 Claim/service denied. Completed physician financial relationship form not on file. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 17. D11 Claim lacks completed pacemaker registration form. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 17. D12 Claim/service denied. Claim does not identify who performed the purchased diagnostic test or the amount you were charged for the test. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 17. D13 Claim/service denied. Performed by a facility/supplier in which the ordering/referring physician has a financial interest. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 17. D14 Claim lacks indication that plan of treatment is on file. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 17. D15 Claim lacks indication that service was supervised or evaluated by a physician. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 17. D16 Claim lacks prior payer payment information. Start: 01/01/1995 | Stop: 06/30/2007 Notes: Use code 16 with appropriate claim payment remark code [N4]. D17 Claim/Service has invalid non-covered days. Start: 01/01/1995 | Stop: 06/30/2007 Notes: Use code 16 with appropriate claim payment remark code. D18 Claim/Service has missing diagnosis information. Start: 01/01/1995 | Stop: 06/30/2007 Notes: Use code 16 with appropriate claim payment remark code. D19 Claim/Service lacks Physician/Operative or other supporting documentation Start: 01/01/1995 | Stop: 06/30/2007 Notes: Use code 16 with appropriate claim payment remark code. D20 Claim/Service missing service/product information. Start: 01/01/1995 | Stop: 06/30/2007 Notes: Use code 16 with appropriate claim payment remark code. D21 This (these) diagnosis(es) is (are) missing or are invalid Start: 01/01/1995 | Stop: 06/30/2007 D22 Reimbursement was adjusted for the reasons to be provided in separate correspondence. (Note: To be used for Workers' Compensation only) - Temporary code to be added for timeframe only until 01/01/2009. Another code to be established and/or for 06/2008 meeting for a revised code to replace or strategy to use another existing code. Start: 01/27/2008 | Stop: 01/01/2009 Provider Manual 2013 230 D23 This dual eligible patient is covered by Medicare Part D per Medicare Retro-Eligibility. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 11/01/2009 | Stop: 01/01/2012 W1 Workers' compensation jurisdictional fee schedule adjustment. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Class of Contract Code Identification Segment (Loop 2100 Other Claim Related Information REF). If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). Start: 02/29/2000 | Last Modified: 10/17/2010 W2 Payment reduced or denied based on workers' compensation jurisdictional regulations or payment policies, use only if no other code is applicable. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segment (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). To be used for Workers' Compensation only. Start: 10/17/2010 W3 The Benefit for this Service is included in the payment/allowance for another service/procedure that has been performed on the same day. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. For use by Property and Casualty only. Start: 09/30/2012 W4 Workers' Compensation Medical Treatment Guideline Adjustment. Start: 09/30/2012 Y1 Payment denied based on Medical Payments Coverage (MPC) or Personal Injury Protection (PIP) Benefits jurisdictional regulations or payment policies, use only if no other code is applicable. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segment (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). To be used for P&C Auto only. Start: 09/30/2012 Y2 Payment adjusted based on Medical Payments Coverage (MPC) or Personal Injury Protection (PIP) Benefits jurisdictional regulations or payment policies, use only if no other code is applicable. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segment (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). To be used for P&C Auto only. Start: 09/30/2012 Y3 Medical Payments Coverage (MPC) or Personal Injury Protection (PIP) Benefits jurisdictional fee schedule adjustment. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Class of Contract Code Identification Segment (Loop 2100 Other Claim Related Information REF). If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). To be used for P&C Auto only. Start: 09/30/2012 Provider Manual 2013 231 The Remittance Advice Remark Code List M1 X-ray not taken within the past 12 months or near enough to the start of treatment. Start: 01/01/1997 M2 Not paid separately when the patient is an inpatient. Start: 01/01/1997 M3 Equipment is the same or similar to equipment already being used. Start: 01/01/1997 M4 Alert: This is the last monthly installment payment for this durable medical equipment. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) M5 Monthly rental payments can continue until the earlier of the 15th month from the first rental month, or the month when the equipment is no longer needed. Start: 01/01/1997 M6 Alert: You must furnish and service this item for any period of medical need for the remainder of the reasonable useful lifetime of the equipment. Start: 01/01/1997 | Last Modified: 03/01/2009 Notes: (Modified 4/1/07, 3/1/2009) M7 No rental payment after the item is purchased, or after the total of issued rental payments equals the purchase price. Start: 01/01/1997 M8 We do not accept blood gas tests results when the test was conducted by a medical supplier or taken while the patient is on oxygen. Start: 01/01/1997 M9 Alert: This is the tenth rental month. You must offer the patient the choice of changing the rental to a purchase agreement. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) M10 Equipment purchases are limited to the first or the tenth month of medical necessity. Start: 01/01/1997 M11 DME, orthotics and prosthetics must be billed to the DME carrier who services the patient's zip code. Start: 01/01/1997 M12 Diagnostic tests performed by a physician must indicate whether purchased services are included on the claim. Start: 01/01/1997 M13 Only one initial visit is covered per specialty per medical group. Start: 01/01/1997 | Last Modified: 06/30/2007 Notes: (Modified 6/30/03) M14 No separate payment for an injection administered during an office visit, and no payment for a full office visit if the patient only received an injection. Start: 01/01/1997 M15 Separately billed services/tests have been bundled as they are considered components of the same procedure. Separate payment is not allowed. Start: 01/01/1997 Provider Manual 2013 232 M16 Alert: Please see our web site, mailings, or bulletins for more details concerning this policy/procedure/decision. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Reactivated 4/1/04, Modified 11/18/05, 4/1/07) M17 Alert: Payment approved as you did not know, and could not reasonably have been expected to know, that this would not normally have been covered for this patient. In the future, you will be liable for charges for the same service(s) under the same or similar conditions. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) M18 Certain services may be approved for home use. Neither a hospital nor a Skilled Nursing Facility (SNF) is considered to be a patient's home. Start: 01/01/1997 | Last Modified: 06/30/2003 Notes: (Modified 6/30/03) M19 Missing oxygen certification/re-certification. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) Related to N234 M20 Missing/incomplete/invalid HCPCS. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M21 Missing/incomplete/invalid place of residence for this service/item provided in a home. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M22 Missing/incomplete/invalid number of miles traveled. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M23 Missing invoice. Start: 01/01/1997 | Last Modified: 08/01/2005 Notes: (Modified 8/1/05) M24 Missing/incomplete/invalid number of doses per vial. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M25 The information furnished does not substantiate the need for this level of service. If you believe the service should have been fully covered as billed, or if you did not know and could not reasonably have been expected to know that we would not pay for this level of service, or if you notified the patient in writing in advance that we would not pay for this level of service and he/she agreed in writing to pay, ask us to review your claim within 120 days of the date of this notice. If you do not request an appeal, we will, upon application from the patient, reimburse him/her for the amount you have collected from him/her in excess of any deductible and coinsurance amounts. We will recover the reimbursement from you as an overpayment. Start: 01/01/1997 | Last Modified: 11/01/2010 Notes: (Modified 10/1/02, 6/30/03, 8/1/05, 11/5/07, 11/1/10) Provider Manual 2013 233 M26 The information furnished does not substantiate the need for this level of service. If you have collected any amount from the patient for this level of service /any amount that exceeds the limiting charge for the less extensive service, the law requires you to refund that amount to the patient within 30 days of receiving this notice. The requirements for refund are in 1824(I) of the Social Security Act and 42CFR411.408. The section specifies that physicians who knowingly and willfully fail to make appropriate refunds may be subject to civil monetary penalties and/or exclusion from the program. If you have any questions about this notice, please contact this office. Start: 01/01/1997 | Last Modified: 11/05/2007 Notes: (Modified 10/1/02, 6/30/03, 8/1/05, 11/5/07. Also refer to N356) M27 Alert: The patient has been relieved of liability of payment of these items and services under the limitation of liability provision of the law. The provider is ultimately liable for the patient's waived charges, including any charges for coinsurance, since the items or services were not reasonable and necessary or constituted custodial care, and you knew or could reasonably have been expected to know, that they were not covered. You may appeal this determination. You may ask for an appeal regarding both the coverage determination and the issue of whether you exercised due care. The appeal request must be filed within 120 days of the date you receive this notice. You must make the request through this office. Start: 01/01/1997 | Last Modified: 08/01/2007 Notes: (Modified 10/1/02, 8/1/05, 4/1/07, 8/1/07) M28 This does not qualify for payment under Part B when Part A coverage is exhausted or not otherwise available. Start: 01/01/1997 M29 Missing operative note/report. Start: 01/01/1997 | Last Modified: 07/01/2008 Notes: (Modified 2/28/03, 7/1/2008) Related to N233 M30 Missing pathology report. Start: 01/01/1997 | Last Modified: 08/01/2004 Notes: (Modified 8/1/04, 2/28/03) Related to N236 M31 Missing radiology report. Start: 01/01/1997 | Last Modified: 08/01/2004 Notes: (Modified 8/1/04, 2/28/03) Related to N240 M32 Alert: This is a conditional payment made pending a decision on this service by the patient's primary payer. This payment may be subject to refund upon your receipt of any additional payment for this service from another payer. You must contact this office immediately upon receipt of an additional payment for this service. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) M33 Missing/incomplete/invalid UPIN for the ordering/referring/performing provider. Start: 01/01/1997 | Stop: 08/01/2004 Notes: Consider using M68 M34 Claim lacks the CLIA certification number. Start: 01/01/1997 | Stop: 08/01/2004 Notes: Consider using MA120 Provider Manual 2013 234 M35 Missing/incomplete/invalid pre-operative photos or visual field results. Start: 01/01/1997 | Stop: 02/05/2005 Notes: Consider using N178 M36 This is the 11th rental month. We cannot pay for this until you indicate that the patient has been given the option of changing the rental to a purchase. Start: 01/01/1997 M37 Not covered when the patient is under age 35. Start: 01/01/1997 | Last Modified: 03/08/2011 Notes: (Modified 3/8/11) M38 The patient is liable for the charges for this service as you informed the patient in writing before the service was furnished that we would not pay for it, and the patient agreed to pay. Start: 01/01/1997 M39 The patient is not liable for payment for this service as the advance notice of noncoverage you provided the patient did not comply with program requirements. Start: 01/01/1997 | Last Modified: 11/01/2012 Notes: (Modified 2/1/04, 4/1/07, 11/1/09, 11/1/12) Related to N563 M40 Claim must be assigned and must be filed by the practitioner's employer. Start: 01/01/1997 M41 We do not pay for this as the patient has no legal obligation to pay for this. Start: 01/01/1997 M42 The medical necessity form must be personally signed by the attending physician. Start: 01/01/1997 M43 Payment for this service previously issued to you or another provider by another carrier/intermediary. Start: 01/01/1997 | Stop: 01/31/2004 Notes: Consider using Reason Code 23 M44 Missing/incomplete/invalid condition code. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M45 Missing/incomplete/invalid occurrence code(s). Start: 01/01/1997 | Last Modified: 12/02/2004 Notes: (Modified 12/2/04) Related to N299 M46 Missing/incomplete/invalid occurrence span code(s). Start: 01/01/1997 | Last Modified: 12/02/2004 Notes: (Modified 12/2/04) Related to N300 M47 Missing/incomplete/invalid internal or document control number. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M48 Payment for services furnished to hospital inpatients (other than professional services of physicians) can only be made to the hospital. You must request payment from the hospital rather than the patient for this service. Start: 01/01/1997 | Stop: 01/31/2004 Notes: Consider using M97 Provider Manual 2013 235 M49 Missing/incomplete/invalid value code(s) or amount(s). Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M50 Missing/incomplete/invalid revenue code(s). Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M51 Missing/incomplete/invalid procedure code(s). Start: 01/01/1997 | Last Modified: 12/02/2004 Notes: (Modified 12/2/04) Related to N301 M52 Missing/incomplete/invalid “from” date(s) of service. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M53 Missing/incomplete/invalid days or units of service. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M54 Missing/incomplete/invalid total charges. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M55 We do not pay for self-administered anti-emetic drugs that are not administered with a covered oral anti-cancer drug. Start: 01/01/1997 M56 Missing/incomplete/invalid payer identifier. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M57 Missing/incomplete/invalid provider identifier. Start: 01/01/1997 | Stop: 06/02/2005 M58 Missing/incomplete/invalid claim information. Resubmit claim after corrections. Start: 01/01/1997 | Stop: 02/05/2005 M59 Missing/incomplete/invalid “to” date(s) of service. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M60 Missing Certificate of Medical Necessity. Start: 01/01/1997 | Last Modified: 08/01/2004 Notes: (Modified 8/1/04, 6/30/03) Related to N227 M61 We cannot pay for this as the approval period for the FDA clinical trial has expired. Start: 01/01/1997 M62 Missing/incomplete/invalid treatment authorization code. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M63 We do not pay for more than one of these on the same day. Start: 01/01/1997 | Stop: 01/31/2004 Notes: Consider using M86 Provider Manual 2013 236 M64 Missing/incomplete/invalid other diagnosis. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M65 One interpreting physician charge can be submitted per claim when a purchased diagnostic test is indicated. Please submit a separate claim for each interpreting physician. Start: 01/01/1997 M66 Our records indicate that you billed diagnostic tests subject to price limitations and the procedure code submitted includes a professional component. Only the technical component is subject to price limitations. Please submit the technical and professional components of this service as separate line items. Start: 01/01/1997 M67 Missing/incomplete/invalid other procedure code(s). Start: 01/01/1997 | Last Modified: 12/02/2004 Notes: (Modified 12/2/04) Related to N302 M68 Missing/incomplete/invalid attending, ordering, rendering, supervising or referring physician identification. Start: 01/01/1997 | Stop: 06/02/2005 M69 Paid at the regular rate as you did not submit documentation to justify the modified procedure code. Start: 01/01/1997 | Last Modified: 02/01/2004 Notes: (Modified 2/1/04) M70 Alert: The NDC code submitted for this service was translated to a HCPCS code for processing, but please continue to submit the NDC on future claims for this item. Start: 01/01/1997 | Last Modified: 08/01/2007 Notes: (Modified 4/1/2007, 8/1/07) M71 Total payment reduced due to overlap of tests billed. Start: 01/01/1997 M72 Did not enter full 8-digit date (MM/DD/CCYY). Start: 01/01/1997 | Stop: 10/16/2003 Notes: Consider using MA52 M73 The HPSA/Physician Scarcity bonus can only be paid on the professional component of this service. Rebill as separate professional and technical components. Start: 01/01/1997 | Last Modified: 08/01/2004 Notes: (Modified 8/1/04) M74 This service does not qualify for a HPSA/Physician Scarcity bonus payment. Start: 01/01/1997 | Last Modified: 12/02/2004 Notes: (Modified 12/2/04) M75 Multiple automated multichannel tests performed on the same day combined for payment. Start: 01/01/1997 | Last Modified: 11/05/2007 Notes: (Modified 11/5/07) M76 Missing/incomplete/invalid diagnosis or condition. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) Provider Manual 2013 237 M77 Missing/incomplete/invalid place of service. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M78 Missing/incomplete/invalid HCPCS modifier. Start: 01/01/1997 | Stop: 05/18/2006 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03,) Consider using Reason Code 4 M79 Missing/incomplete/invalid charge. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M80 Not covered when performed during the same session/date as a previously processed service for the patient. Start: 01/01/1997 | Last Modified: 10/31/2002 Notes: (Modified 10/31/02) M81 You are required to code to the highest level of specificity. Start: 01/01/1997 | Last Modified: 02/01/2004 Notes: (Modified 2/1/04) M82 Service is not covered when patient is under age 50. Start: 01/01/1997 M83 Service is not covered unless the patient is classified as at high risk. Start: 01/01/1997 M84 Medical code sets used must be the codes in effect at the time of service Start: 01/01/1997 | Last Modified: 02/01/2004 Notes: (Modified 2/1/04) M85 Subjected to review of physician evaluation and management services. Start: 01/01/1997 M86 Service denied because payment already made for same/similar procedure within set time frame. Start: 01/01/1997 | Last Modified: 06/30/2003 Notes: (Modified 6/30/03) M87 Claim/service(s) subjected to CFO-CAP prepayment review. Start: 01/01/1997 M88 We cannot pay for laboratory tests unless billed by the laboratory that did the work. Start: 01/01/1997 | Stop: 08/01/2004 Notes: Consider using Reason Code B20 M89 Not covered more than once under age 40. Start: 01/01/1997 M90 Not covered more than once in a 12 month period. Start: 01/01/1997 M91 Lab procedures with different CLIA certification numbers must be billed on separate claims. Start: 01/01/1997 M92 Services subjected to review under the Home Health Medical Review Initiative. Provider Manual 2013 238 Start: 01/01/1997 | Stop: 08/01/2004 M93 Information supplied supports a break in therapy. A new capped rental period began with delivery of this equipment. Start: 01/01/1997 M94 Information supplied does not support a break in therapy. A new capped rental period will not begin. Start: 01/01/1997 M95 Services subjected to Home Health Initiative medical review/cost report audit. Start: 01/01/1997 M96 The technical component of a service furnished to an inpatient may only be billed by that inpatient facility. You must contact the inpatient facility for technical component reimbursement. If not already billed, you should bill us for the professional component only. Start: 01/01/1997 M97 Not paid to practitioner when provided to patient in this place of service. Payment included in the reimbursement issued the facility. Start: 01/01/1997 M98 Begin to report the Universal Product Number on claims for items of this type. We will soon begin to deny payment for items of this type if billed without the correct UPN. Start: 01/01/1997 | Stop: 01/31/2004 Notes: Consider using M99 M99 Missing/incomplete/invalid Universal Product Number/Serial Number. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M100 We do not pay for an oral anti-emetic drug that is not administered for use immediately before, at, or within 48 hours of administration of a covered chemotherapy drug. Start: 01/01/1997 M101 Begin to report a G1-G5 modifier with this HCPCS. We will soon begin to deny payment for this service if billed without a G1-G5 modifier. Start: 01/01/1997 | Stop: 01/31/2004 Notes: Consider using M78 M102 Service not performed on equipment approved by the FDA for this purpose. Start: 01/01/1997 M103 Information supplied supports a break in therapy. However, the medical information we have for this patient does not support the need for this item as billed. We have approved payment for this item at a reduced level, and a new capped rental period will begin with the delivery of this equipment. Start: 01/01/1997 M104 Information supplied supports a break in therapy. A new capped rental period will begin with delivery of the equipment. This is the maximum approved under the fee schedule for this item or service. Start: 01/01/1997 M105 Information supplied does not support a break in therapy. The medical information we have for this patient does not support the need for this item as billed. We have approved payment for this item at a reduced level, and a new capped rental period will not begin. Start: 01/01/1997 Provider Manual 2013 239 M106 Information supplied does not support a break in therapy. A new capped rental period will not begin. This is the maximum approved under the fee schedule for this item or service. Start: 01/01/1997 | Stop: 01/31/2004 Notes: Consider using MA 31 M107 Payment reduced as 90-day rolling average hematocrit for ESRD patient exceeded 36.5%. Start: 01/01/1997 M108 Missing/incomplete/invalid provider identifier for the provider who interpreted the diagnostic test. Start: 01/01/1997 | Stop: 06/02/2005 M109 We have provided you with a bundled payment for a tele-consultation. You must send 25 percent of the tele-consultation payment to the referring practitioner. Start: 01/01/1997 M110 Missing/incomplete/invalid provider identifier for the provider from whom you purchased interpretation services. Start: 01/01/1997 | Stop: 06/02/2005 M111 We do not pay for chiropractic manipulative treatment when the patient refuses to have an x-ray taken. Start: 01/01/1997 M112 Reimbursement for this item is based on the single payment amount required under the DMEPOS Competitive Bidding Program for the area where the patient resides. Start: 01/01/1997 | Last Modified: 11/05/2007 Notes: (Modified 11/5/07) M113 Our records indicate that this patient began using this item/service prior to the current contract period for the DMEPOS Competitive Bidding Program. Start: 01/01/1997 | Last Modified: 11/05/2007 Notes: (Modified 11/5/07) M114 This service was processed in accordance with rules and guidelines under the DMEPOS Competitive Bidding Program or a Demonstration Project. For more information regarding these projects, contact your local contractor. Start: 01/01/1997 | Last Modified: 11/05/2007 Notes: (Modified 8/1/06, 11/5/07) M115 This item is denied when provided to this patient by a non-contract or nondemonstration supplier. Start: 01/01/1997 | Last Modified: 11/05/2007 Notes: (Modified 11/5/2007) M116 Processed under a demonstration project or program. Project or program is ending and additional services may not be paid under this project or program. Start: 01/01/1997 | Last Modified: 03/08/2011 Notes: (Modified 2/1/04, 3/15/11) M117 Not covered unless submitted via electronic claim. Start: 01/01/1997 | Last Modified: 06/30/2003 Notes: (Modified 6/30/03) M118 Letter to follow containing further information. Start: 01/01/1997 | Stop: 01/01/2011 | Last Modified: 11/01/2009 Provider Manual 2013 240 Notes: Consider using N202 M119 Missing/incomplete/invalid/ deactivated/withdrawn National Drug Code (NDC). Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 2/28/03, 4/1/04) M120 Missing/incomplete/invalid provider identifier for the substituting physician who furnished the service(s) under a reciprocal billing or locum tenens arrangement. Start: 01/01/1997 | Stop: 06/02/2005 M121 We pay for this service only when performed with a covered cryosurgical ablation. Start: 01/01/1997 M122 Missing/incomplete/invalid level of subluxation. Start: 01/01/1997 | Last Modified: 02/28/2006 Notes: (Modified 2/28/03) M123 Missing/incomplete/invalid name, strength, or dosage of the drug furnished. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M124 Missing indication of whether the patient owns the equipment that requires the part or supply. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) Related to N230 M125 Missing/incomplete/invalid information on the period of time for which the service/supply/equipment will be needed. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M126 Missing/incomplete/invalid individual lab codes included in the test. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M127 Missing patient medical record for this service. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) Related to N237 M128 Missing/incomplete/invalid date of the patient’s last physician visit. Start: 01/01/1997 | Stop: 06/02/2005 M129 Missing/incomplete/invalid indicator of x-ray availability for review. Start: 01/01/1997 | Last Modified: 06/30/2003 Notes: (Modified 2/28/03, 6/30/03) M130 Missing invoice or statement certifying the actual cost of the lens, less discounts, and/or the type of intraocular lens used. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) Related to N231 M131 Missing physician financial relationship form. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) Related to N239 M132 Missing pacemaker registration form. Start: 01/01/1997 | Last Modified: 02/28/2003 Provider Manual 2013 241 Notes: (Modified 2/28/03) Related to N235 M133 Claim did not identify who performed the purchased diagnostic test or the amount you were charged for the test. Start: 01/01/1997 M134 Performed by a facility/supplier in which the provider has a financial interest. Start: 01/01/1997 | Last Modified: 06/30/2003 Notes: (Modified 6/30/03) M135 Missing/incomplete/invalid plan of treatment. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M136 Missing/incomplete/invalid indication that the service was supervised or evaluated by a physician. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) M137 Part B coinsurance under a demonstration project or pilot program. Start: 01/01/1997 | Last Modified: 11/01/2012 Notes: (Modified 11/1/12) M138 Patient identified as a demonstration participant but the patient was not enrolled in the demonstration at the time services were rendered. Coverage is limited to demonstration participants. Start: 01/01/1997 M139 Denied services exceed the coverage limit for the demonstration. Start: 01/01/1997 M140 Service not covered until after the patient’s 50th birthday, i.e., no coverage prior to the day after the 50th birthday Start: 01/01/1997 | Stop: 01/30/2004 Notes: Consider using M82 M141 Missing physician certified plan of care. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) Related to N238 M142 Missing American Diabetes Association Certificate of Recognition. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) Related to N226 M143 The provider must update license information with the payer. Start: 01/01/1997 | Last Modified: 12/01/2006 Notes: (Modified 12/1/06) M144 Pre-/post-operative care payment is included in the allowance for the surgery/procedure. Start: 01/01/1997 MA01 Alert: If you do not agree with what we approved for these services, you may appeal our decision. To make sure that we are fair to you, we require another individual that did not process your initial claim to conduct the appeal. However, in order to be eligible for an appeal, you must write to us within 120 days of the date you received this notice, unless you have a good reason for being late. Provider Manual 2013 242 Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 10/31/02, 6/30/03, 8/1/05, 4/1/07) MA02 Alert: If you do not agree with this determination, you have the right to appeal. You must file a written request for an appeal within 180 days of the date you receive this notice. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 10/31/02, 6/30/03, 8/1/05, 12/29/05, 8/1/06, 4/1/07) MA03 If you do not agree with the approved amounts and $100 or more is in dispute (less deductible and coinsurance), you may ask for a hearing within six months of the date of this notice. To meet the $100, you may combine amounts on other claims that have been denied, including reopened appeals if you received a revised decision. You must appeal each claim on time. Start: 01/01/1997 | Stop: 10/01/2006 | Last Modified: 11/18/2005 Notes: Consider using MA02 (Modified 10/31/02, 6/30/03, 8/1/05, 11/18/05) MA04 Secondary payment cannot be considered without the identity of or payment information from the primary payer. The information was either not reported or was illegible. Start: 01/01/1997 MA05 Incorrect admission date patient status or type of bill entry on claim. Start: 01/01/1997 | Stop: 10/16/2003 Notes: Consider using MA30, MA40 or MA43 MA06 Missing/incomplete/invalid beginning and/or ending date(s). Start: 01/01/1997 | Stop: 08/01/2004 Notes: Consider using MA31 MA07 Alert: The claim information has also been forwarded to Medicaid for review. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) MA08 Alert: Claim information was not forwarded because the supplemental coverage is not with a Medigap plan, or you do not participate in Medicare. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) MA09 Claim submitted as unassigned but processed as assigned. You agreed to accept assignment for all claims. Start: 01/01/1997 MA10 Alert: The patient's payment was in excess of the amount owed. You must refund the overpayment to the patient. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) MA11 Payment is being issued on a conditional basis. If no-fault insurance, liability insurance, Workers' Compensation, Department of Veterans Affairs, or a group health plan for employees and dependents also covers this claim, a refund may be due us. Please contact us if the patient is covered by any of these sources. Start: 01/01/1997 | Stop: 01/31/2004 Notes: Consider using M32 MA12 You have not established that you have the right under the law to bill for services furnished by the person(s) that furnished this (these) service(s). Start: 01/01/1997 Provider Manual 2013 243 MA13 Alert: You may be subject to penalties if you bill the patient for amounts not reported with the PR (patient responsibility) group code. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) MA14 Alert: The patient is a member of an employer-sponsored prepaid health plan. Services from outside that health plan are not covered. However, as you were not previously notified of this, we are paying this time. In the future, we will not pay you for non-plan services. Start: 01/01/1997 | Last Modified: 08/01/2007 Notes: (Modified 4/1/07, 8/1/07) MA15 Alert: Your claim has been separated to expedite handling. You will receive a separate notice for the other services reported. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) MA16 The patient is covered by the Black Lung Program. Send this claim to the Department of Labor, Federal Black Lung Program, P.O. Box 828, Lanham-Seabrook MD 20703. Start: 01/01/1997 MA17 We are the primary payer and have paid at the primary rate. You must contact the patient's other insurer to refund any excess it may have paid due to its erroneous primary payment. Start: 01/01/1997 MA18 Alert: The claim information is also being forwarded to the patient's supplemental insurer. Send any questions regarding supplemental benefits to them. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) MA19 Alert: Information was not sent to the Medigap insurer due to incorrect/invalid information you submitted concerning that insurer. Please verify your information and submit your secondary claim directly to that insurer. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) MA20 Skilled Nursing Facility (SNF) stay not covered when care is primarily related to the use of an urethral catheter for convenience or the control of incontinence. Start: 01/01/1997 | Last Modified: 06/30/2003 Notes: (Modified 6/30/03) MA21 SSA records indicate mismatch with name and sex. Start: 01/01/1997 MA22 Payment of less than $1.00 suppressed. Start: 01/01/1997 MA23 Demand bill approved as result of medical review. Start: 01/01/1997 MA24 Christian Science Sanitarium/ Skilled Nursing Facility (SNF) bill in the same benefit period. Start: 01/01/1997 | Last Modified: 06/30/2003 Notes: (Modified 6/30/03) MA25 A patient may not elect to change a hospice provider more than once in a benefit period. Start: 01/01/1997 Provider Manual 2013 244 MA26 Alert: Our records indicate that you were previously informed of this rule. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) MA27 Missing/incomplete/invalid entitlement number or name shown on the claim. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA28 Alert: Receipt of this notice by a physician or supplier who did not accept assignment is for information only and does not make the physician or supplier a party to the determination. No additional rights to appeal this decision, above those rights already provided for by regulation/instruction, are conferred by receipt of this notice. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) MA29 Missing/incomplete/invalid provider name, city, state, or zip code. Start: 01/01/1997 | Stop: 06/02/2005 MA30 Missing/incomplete/invalid type of bill. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA31 Missing/incomplete/invalid beginning and ending dates of the period billed. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA32 Missing/incomplete/invalid number of covered days during the billing period. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA33 Missing/incomplete/invalid noncovered days during the billing period. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA34 Missing/incomplete/invalid number of coinsurance days during the billing period. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA35 Missing/incomplete/invalid number of lifetime reserve days. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA36 Missing/incomplete/invalid patient name. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA37 Missing/incomplete/invalid patient's address. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA38 Missing/incomplete/invalid birth date. Start: 01/01/1997 | Stop: 06/02/2005 MA39 Missing/incomplete/invalid gender. Start: 01/01/1997 | Last Modified: 02/28/2003 Provider Manual 2013 245 Notes: (Modified 2/28/03) MA40 Missing/incomplete/invalid admission date. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA41 Missing/incomplete/invalid admission type. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA42 Missing/incomplete/invalid admission source. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA43 Missing/incomplete/invalid patient status. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA44 Alert: No appeal rights. Adjudicative decision based on law. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) MA45 Alert: As previously advised, a portion or all of your payment is being held in a special account. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) MA46 The new information was considered but additional payment will not be issued. Start: 01/01/1997 | Last Modified: 03/01/2009 Notes: (Modified 3/1/2009) MA47 Our records show you have opted out of Medicare, agreeing with the patient not to bill Medicare for services/tests/supplies furnished. As result, we cannot pay this claim. The patient is responsible for payment. Start: 01/01/1997 MA48 Missing/incomplete/invalid name or address of responsible party or primary payer. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA49 Missing/incomplete/invalid six-digit provider identifier for home health agency or hospice for physician(s) performing care plan oversight services. Start: 01/01/1997 | Stop: 08/01/2004 Notes: Consider using MA76 MA50 Missing/incomplete/invalid Investigational Device Exemption number for FDA-approved clinical trial services. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA51 Missing/incomplete/invalid CLIA certification number for laboratory services billed by physician office laboratory. Start: 01/01/1997 | Stop: 02/05/2005 Notes: Consider using MA120 MA52 Missing/incomplete/invalid date. Provider Manual 2013 246 Start: 01/01/1997 | Stop: 06/02/2005 MA53 Missing/incomplete/invalid Competitive Bidding Demonstration Project identification. Start: 01/01/1997 | Last Modified: 02/01/2004 Notes: (Modified 2/1/04) MA54 Physician certification or election consent for hospice care not received timely. Start: 01/01/1997 MA55 Not covered as patient received medical health care services, automatically revoking his/her election to receive religious non-medical health care services. Start: 01/01/1997 MA56 Our records show you have opted out of Medicare, agreeing with the patient not to bill Medicare for services/tests/supplies furnished. As result, we cannot pay this claim. The patient is responsible for payment, but under Federal law, you cannot charge the patient more than the limiting charge amount. Start: 01/01/1997 MA57 Patient submitted written request to revoke his/her election for religious non-medical health care services. Start: 01/01/1997 MA58 Missing/incomplete/invalid release of information indicator. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA59 Alert: The patient overpaid you for these services. You must issue the patient a refund within 30 days for the difference between his/her payment and the total amount shown as patient responsibility on this notice. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) MA60 Missing/incomplete/invalid patient relationship to insured. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA61 Missing/incomplete/invalid social security number or health insurance claim number. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA62 Alert: This is a telephone review decision. Start: 01/01/1997 | Last Modified: 08/01/2007 Notes: (Modified 4/1/07, 8/1/07) MA63 Missing/incomplete/invalid principal diagnosis. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA64 Our records indicate that we should be the third payer for this claim. We cannot process this claim until we have received payment information from the primary and secondary payers. Start: 01/01/1997 MA65 Missing/incomplete/invalid admitting diagnosis. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) Provider Manual 2013 247 MA66 Missing/incomplete/invalid principal procedure code. Start: 01/01/1997 | Last Modified: 12/02/2004 Notes: (Modified 12/2/04) Related to N303 MA67 Correction to a prior claim. Start: 01/01/1997 MA68 Alert: We did not crossover this claim because the secondary insurance information on the claim was incomplete. Please supply complete information or use the PLANID of the insurer to assure correct and timely routing of the claim. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) MA69 Missing/incomplete/invalid remarks. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA70 Missing/incomplete/invalid provider representative signature. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA71 Missing/incomplete/invalid provider representative signature date. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA72 Alert: The patient overpaid you for these assigned services. You must issue the patient a refund within 30 days for the difference between his/her payment to you and the total of the amount shown as patient responsibility and as paid to the patient on this notice. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) MA73 Informational remittance associated with a Medicare demonstration. No payment issued under fee-for-service Medicare as patient has elected managed care. Start: 01/01/1997 MA74 This payment replaces an earlier payment for this claim that was either lost, damaged or returned. Start: 01/01/1997 MA75 Missing/incomplete/invalid patient or authorized representative signature. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA76 Missing/incomplete/invalid provider identifier for home health agency or hospice when physician is performing care plan oversight services. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03, 2/1/04) MA77 Alert: The patient overpaid you. You must issue the patient a refund within 30 days for the difference between the patient’s payment less the total of our and other payer payments and the amount shown as patient responsibility on this notice. Start: 01/01/1997 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) MA78 The patient overpaid you. You must issue the patient a refund within 30 days for the difference between our allowed amount total and the amount paid by the patient. Start: 01/01/1997 | Stop: 01/31/2004 Provider Manual 2013 248 Notes: Consider using MA59 MA79 Billed in excess of interim rate. Start: 01/01/1997 MA80 Informational notice. No payment issued for this claim with this notice. Payment issued to the hospital by its intermediary for all services for this encounter under a demonstration project. Start: 01/01/1997 MA81 Missing/incomplete/invalid provider/supplier signature. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA82 Missing/incomplete/invalid provider/supplier billing number/identifier or billing name, address, city, state, zip code, or phone number. Start: 01/01/1997 | Stop: 06/02/2005 MA83 Did not indicate whether we are the primary or secondary payer. Start: 01/01/1997 | Last Modified: 08/01/2005 Notes: (Modified 8/1/05) MA84 Patient identified as participating in the National Emphysema Treatment Trial but our records indicate that this patient is either not a participant, or has not yet been approved for this phase of the study. Contact Johns Hopkins University, the study coordinator, to resolve if there was a discrepancy. Start: 01/01/1997 MA85 Our records indicate that a primary payer exists (other than ourselves); however, you did not complete or enter accurately the insurance plan/group/program name or identification number. Enter the PlanID when effective. Start: 01/01/1997 | Stop: 08/01/2004 Notes: Consider using MA92 MA86 Missing/incomplete/invalid group or policy number of the insured for the primary coverage. Start: 01/01/1997 | Stop: 08/01/2004 Notes: Consider using MA92 MA87 Missing/incomplete/invalid insured's name for the primary payer. Start: 01/01/1997 | Stop: 08/01/2004 Notes: Consider using MA92 MA88 Missing/incomplete/invalid insured's address and/or telephone number for the primary payer. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA89 Missing/incomplete/invalid patient's relationship to the insured for the primary payer. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA90 Missing/incomplete/invalid employment status code for the primary insured. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03). MA91 This determination is the result of the appeal you filed. Provider Manual 2013 249 Start: 01/01/1997 MA92 Missing plan information for other insurance. Start: 01/01/1997 | Last Modified: 02/01/2004 Notes: (Modified 2/1/04) Related to N245 MA93 Non-PIP (Periodic Interim Payment) claim. Start: 01/01/1997 | Last Modified: 06/30/2003 Notes: (Modified 6/30/03) MA94 Did not enter the statement “Attending physician not hospice employee” on the claim form to certify that the rendering physician is not an employee of the hospice. Start: 01/01/1997 | Last Modified: 08/01/2005 Notes: (Reactivated 4/1/04, Modified 8/1/05) MA95 A not otherwise classified or unlisted procedure code(s) was billed but a narrative description of the procedure was not entered on the claim. Refer to item 19 on the HCFA1500. Start: 01/01/1997 | Stop: 01/01/2004 | Last Modified: 02/28/2003 Notes: (Deactivated 2/28/2003) (Erroneous description corrected 9/2/2008) Consider using M51 MA96 Claim rejected. Coded as a Medicare Managed Care Demonstration but patient is not enrolled in a Medicare managed care plan. Start: 01/01/1997 MA97 Missing/incomplete/invalid Medicare Managed Care Demonstration contract number or clinical trial registry number. Start: 01/01/1997 | Last Modified: 02/29/2008 Notes: (Modified 2/29/08) MA98 Claim Rejected. Does not contain the correct Medicare Managed Care Demonstration contract number for this beneficiary. Start: 01/01/1997 | Stop: 10/16/2003 Notes: Consider using MA97 MA99 Missing/incomplete/invalid Medigap information. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA100 Missing/incomplete/invalid date of current illness or symptoms Start: 01/01/1997 | Last Modified: 03/30/2005 Notes: (Modified 2/28/03, 3/30/05) MA101 A Skilled Nursing Facility (SNF) is responsible for payment of outside providers who furnish these services/supplies to residents. Start: 01/01/1997 | Stop: 01/01/2011 | Last Modified: 06/30/2003 Notes: Consider using N538 MA102 Missing/incomplete/invalid name or provider identifier for the rendering/referring/ ordering/ supervising provider. Start: 01/01/1997 | Stop: 08/01/2004 Notes: Consider using M68 MA103 Hemophilia Add On. Start: 01/01/1997 Provider Manual 2013 250 MA104 Missing/incomplete/invalid date the patient was last seen or the provider identifier of the attending physician. Start: 01/01/1997 | Stop: 01/31/2004 Notes: Consider using M128 or M57 MA105 Missing/incomplete/invalid provider number for this place of service. Start: 01/01/1997 | Stop: 06/02/2005 MA106 PIP (Periodic Interim Payment) claim. Start: 01/01/1997 | Last Modified: 06/30/2003 Notes: (Modified 6/30/03) MA107 Paper claim contains more than three separate data items in field 19. Start: 01/01/1997 MA108 Paper claim contains more than one data item in field 23. Start: 01/01/1997 MA109 Claim processed in accordance with ambulatory surgical guidelines. Start: 01/01/1997 MA110 Missing/incomplete/invalid information on whether the diagnostic test(s) were performed by an outside entity or if no purchased tests are included on the claim. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA111 Missing/incomplete/invalid purchase price of the test(s) and/or the performing laboratory's name and address. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA112 Missing/incomplete/invalid group practice information. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA113 Incomplete/invalid taxpayer identification number (TIN) submitted by you per the Internal Revenue Service. Your claims cannot be processed without your correct TIN, and you may not bill the patient pending correction of your TIN. There are no appeal rights for unprocessable claims, but you may resubmit this claim after you have notified this office of your correct TIN. Start: 01/01/1997 MA114 Missing/incomplete/invalid information on where the services were furnished. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA115 Missing/incomplete/invalid physical location (name and address, or PIN) where the service(s) were rendered in a Health Professional Shortage Area (HPSA). Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA116 Did not complete the statement 'Homebound' on the claim to validate whether laboratory services were performed at home or in an institution. Start: 01/01/1997 Notes: (Reactivated 4/1/04) MA117 This claim has been assessed a $1.00 user fee. Provider Manual 2013 251 Start: 01/01/1997 MA118 Coinsurance and/or deductible amounts apply to a claim for services or supplies furnished to a Medicare-eligible veteran through a facility of the Department of Veterans Affairs. No Medicare payment issued. Start: 01/01/1997 MA119 Provider level adjustment for late claim filing applies to this claim. Start: 01/01/1997 | Stop: 05/01/2008 | Last Modified: 11/05/2007 Notes: Consider using Reason Code B4 MA120 Missing/incomplete/invalid CLIA certification number. Start: 01/01/1997 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) MA121 Missing/incomplete/invalid x-ray date. Start: 01/01/1997 | Last Modified: 12/02/2004 Notes: (Modified 12/2/04) MA122 Missing/incomplete/invalid initial treatment date. Start: 01/01/1997 | Last Modified: 12/02/2004 Notes: (Modified 12/2/04) MA123 Your center was not selected to participate in this study, therefore, we cannot pay for these services. Start: 01/01/1997 MA124 Processed for IME only. Start: 01/01/1997 | Stop: 01/31/2004 Notes: Consider using Reason Code 74 MA125 Per legislation governing this program, payment constitutes payment in full. Start: 01/01/1997 MA126 Pancreas transplant not covered unless kidney transplant performed. Start: 10/12/2001 MA127 Reserved for future use. Start: 10/12/2001 | Stop: 06/02/2005 MA128 Missing/incomplete/invalid FDA approval number. Start: 10/12/2001 | Last Modified: 03/30/2005 Notes: (Modified 2/28/03, 3/30/05) MA129 This provider was not certified for this procedure on this date of service. Start: 10/12/2001 | Stop: 01/31/2004 | Last Modified: 01/31/2004 Notes: Consider using MA120 and Reason Code B7 MA130 Your claim contains incomplete and/or invalid information, and no appeal rights are afforded because the claim is un-processable. Please submit a new claim with the complete/correct information. Start: 10/12/2001 MA131 Physician already paid for services in conjunction with this demonstration claim. You must have the physician withdraw that claim and refund the payment before we can process your claim. Start: 10/12/2001 Provider Manual 2013 252 MA132 Adjustment to the pre-demonstration rate. Start: 10/12/2001 MA133 Claim overlaps inpatient stay. Rebill only those services rendered outside the inpatient stay. Start: 10/12/2001 MA134 Missing/incomplete/invalid provider number of the facility where the patient resides. Start: 10/12/2001 N1 Alert: You may appeal this decision in writing within the required time limits following receipt of this notice by following the instructions included in your contract or plan benefit documents. Start: 01/01/2000 | Last Modified: 04/01/2007 Notes: (Modified 2/28/03, 4/1/07) N2 This allowance has been made in accordance with the most appropriate course of treatment provision of the plan. Start: 01/01/2000 N3 Missing consent form. Start: 01/01/2000 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) Related to N228 N4 Missing/Incomplete/Invalid prior Insurance Carrier(s) EOB. Start: 01/01/2000 | Last Modified: 03/06/2012 Notes: (Modified 2/28/03, 3/6/2012) N5 EOB received from previous payer. Claim not on file. Start: 01/01/2000 N6 Under FEHB law (U.S.C. 8904(b)), we cannot pay more for covered care than the amount Medicare would have allowed if the patient were enrolled in Medicare Part A and/or Medicare Part B. Start: 01/01/2000 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) N7 Processing of this claim/service has included consideration under Major Medical provisions. Start: 01/01/2000 N8 Crossover claim denied by previous payer and complete claim data not forwarded. Resubmit this claim to this payer to provide adequate data for adjudication. Start: 01/01/2000 N9 Adjustment represents the estimated amount a previous payer may pay. Start: 01/01/2000 | Last Modified: 11/18/2005 Notes: (Modified 11/18/05) N10 Payment based on the findings of a review organization/professional consult/manual adjudication/medical or dental advisor. Start: 01/01/2000 | Last Modified: 07/01/2008 Notes: (Modified 10/31/02, 7/1/08) N11 Denial reversed because of medical review. Start: 01/01/2000 Provider Manual 2013 253 N12 Policy provides coverage supplemental to Medicare. As the member does not appear to be enrolled in the applicable part of Medicare, the member is responsible for payment of the portion of the charge that would have been covered by Medicare. Start: 01/01/2000 | Last Modified: 08/01/2007 Notes: (Modified 8/1/07) N13 Payment based on professional/technical component modifier(s). Start: 01/01/2000 N14 Payment based on a contractual amount or agreement, fee schedule, or maximum allowable amount. Start: 01/01/2000 | Stop: 10/01/2007 Notes: Consider using Reason Code 45 N15 Services for a newborn must be billed separately. Start: 01/01/2000 N16 Family/member Out-of-Pocket maximum has been met. Payment based on a higher percentage. Start: 01/01/2000 N17 Per admission deductible. Start: 01/01/2000 | Stop: 08/01/2004 Notes: Consider using Reason Code 1 N18 Payment based on the Medicare allowed amount. Start: 01/01/2000 | Stop: 01/31/2004 Notes: Consider using N14 N19 Procedure code incidental to primary procedure. Start: 01/01/2000 N20 Service not payable with other service rendered on the same date. Start: 01/01/2000 N21 Alert: Your line item has been separated into multiple lines to expedite handling. Start: 01/01/2000 | Last Modified: 04/01/2007 Notes: (Modified 8/1/05, 4/1/07) N22 This procedure code was added/changed because it more accurately describes the services rendered. Start: 01/01/2000 | Last Modified: 02/28/2003 Notes: (Modified 10/31/02, 2/28/03) N23 Alert: Patient liability may be affected due to coordination of benefits with other carriers and/or maximum benefit provisions. Start: 01/01/2000 | Last Modified: 04/01/2007 Notes: (Modified 8/13/01, 4/1/07) N24 Missing/incomplete/invalid Electronic Funds Transfer (EFT) banking information. Start: 01/01/2000 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) N25 This company has been contracted by your benefit plan to provide administrative claims payment services only. This company does not assume financial risk or obligation with respect to claims processed on behalf of your benefit plan. Start: 01/01/2000 Provider Manual 2013 254 N26 Missing itemized bill/statement. Start: 01/01/2000 | Last Modified: 07/01/2008 Notes: (Modified 2/28/03, 7/1/2008) Related to N232 N27 Missing/incomplete/invalid treatment number. Start: 01/01/2000 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) N28 Consent form requirements not fulfilled. Start: 01/01/2000 N29 Missing documentation/orders/notes/summary/report/chart. Start: 01/01/2000 | Last Modified: 08/01/2005 Notes: (Modified 2/28/03, 8/1/05) Related to N225 N30 Patient ineligible for this service. Start: 01/01/2000 | Last Modified: 06/30/2003 Notes: (Modified 6/30/03) N31 Missing/incomplete/invalid prescribing provider identifier. Start: 01/01/2000 | Last Modified: 12/02/2004 Notes: (Modified 12/2/04) N32 Claim must be submitted by the provider who rendered the service. Start: 01/01/2000 | Last Modified: 06/30/2003 Notes: (Modified 6/30/03) N33 No record of health check prior to initiation of treatment. Start: 01/01/2000 N34 Incorrect claim form/format for this service. Start: 01/01/2000 | Last Modified: 11/18/2005 Notes: (Modified 11/18/05) N35 Program integrity/utilization review decision. Start: 01/01/2000 N36 Claim must meet primary payer’s processing requirements before we can consider payment. Start: 01/01/2000 N37 Missing/incomplete/invalid tooth number/letter. Start: 01/01/2000 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) N38 Missing/incomplete/invalid place of service. Start: 01/01/2000 | Stop: 02/05/2005 Notes: Consider using M77 N39 Procedure code is not compatible with tooth number/letter. Start: 01/01/2000 N40 Missing radiology film(s)/image(s). Start: 01/01/2000 | Last Modified: 07/01/2008 Notes: (Modified 2/1/04, 7/1/08) Related to N242 N41 Authorization request denied. Provider Manual 2013 255 Start: 01/01/2000 | Stop: 10/16/2003 Notes: Consider using Reason Code 39 N42 No record of mental health assessment. Start: 01/01/2000 N43 Bed hold or leave days exceeded. Start: 01/01/2000 N44 Payer’s share of regulatory surcharges, assessments, allowances or health care-related taxes paid directly to the regulatory authority. Start: 01/01/2000 | Stop: 10/16/2003 Notes: Consider using Reason Code 137 N45 Payment based on authorized amount. Start: 01/01/2000 N46 Missing/incomplete/invalid admission hour. Start: 01/01/2000 N47 Claim conflicts with another inpatient stay. Start: 01/01/2000 N48 Claim information does not agree with information received from other insurance carrier. Start: 01/01/2000 N49 Court ordered coverage information needs validation. Start: 01/01/2000 N50 Missing/incomplete/invalid discharge information. Start: 01/01/2000 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) N51 Electronic interchange agreement not on file for provider/submitter. Start: 01/01/2000 N52 Patient not enrolled in the billing provider's managed care plan on the date of service. Start: 01/01/2000 N53 Missing/incomplete/invalid point of pick-up address. Start: 01/01/2000 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) N54 Claim information is inconsistent with pre-certified/authorized services. Start: 01/01/2000 N55 Procedures for billing with group/referring/performing providers were not followed. Start: 01/01/2000 N56 Procedure code billed is not correct/valid for the services billed or the date of service billed. Start: 01/01/2000 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) N57 Missing/incomplete/invalid prescribing date. Start: 01/01/2000 | Last Modified: 12/02/2004 Notes: (Modified 12/2/04) Related to N304 Provider Manual 2013 256 N58 Missing/incomplete/invalid patient liability amount. Start: 01/01/2000 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) N59 Please refer to your provider manual for additional program and provider information. Start: 01/01/2000 | Last Modified: 11/01/2009 Notes: (Modified 4/1/07, 11/1/09) N60 A valid NDC is required for payment of drug claims effective October 02. Start: 01/01/2000 | Stop: 01/31/2004 Notes: Consider using M119 N61 Rebill services on separate claims. Start: 01/01/2000 N62 Dates of service span multiple rate periods. Resubmit separate claims. Start: 01/01/2000 | Last Modified: 03/08/2011 Notes: (Modified 3/8/11) N63 Rebill services on separate claim lines. Start: 01/01/2000 N64 The “from” and “to” dates must be different. Start: 01/01/2000 N65 Procedure code or procedure rate count cannot be determined, or was not on file, for the date of service/provider. Start: 01/01/2000 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) N66 Missing/incomplete/invalid documentation. Start: 01/01/2000 | Stop: 02/05/2005 Notes: Consider using N29 or N225. N67 Professional provider services not paid separately. Included in facility payment under a demonstration project. Apply to that facility for payment, or resubmit your claim if: the facility notifies you the patient was excluded from this demonstration; or if you furnished these services in another location on the date of the patient’s admission or discharge from a demonstration hospital. If services were furnished in a facility not involved in the demonstration on the same date the patient was discharged from or admitted to a demonstration facility, you must report the provider ID number for the nondemonstration facility on the new claim. Start: 01/01/2000 N68 Prior payment being cancelled as we were subsequently notified this patient was covered by a demonstration project in this site of service. Professional services were included in the payment made to the facility. You must contact the facility for your payment. Prior payment made to you by the patient or another insurer for this claim must be refunded to the payer within 30 days. Start: 01/01/2000 N69 PPS (Prospective Payment System) code changed by claims processing system. Start: 01/01/2000 | Last Modified: 07/01/2012 Notes: (Modified 6/30/03, 7/1/12) N70 Consolidated billing and payment applies. Provider Manual 2013 257 Start: 01/01/2000 | Last Modified: 11/05/2007 Notes: (Modified 2/28/02, 11/5/07) N71 Your unassigned claim for a drug or biological, clinical diagnostic laboratory services or ambulance service was processed as an assigned claim. You are required by law to accept assignment for these types of claims. Start: 01/01/2000 | Last Modified: 06/30/2003 Notes: (Modified 2/21/02, 6/30/03) N72 PPS (Prospective Payment System) code changed by medical reviewers. Not supported by clinical records. Start: 01/01/2000 | Last Modified: 06/30/2003 Notes: (Modified 6/30/03) N73 A Skilled Nursing Facility is responsible for payment of outside providers who furnish these services/supplies under arrangement to its residents. Start: 01/01/2000 | Stop: 01/31/2004 Notes: Consider using MA101 or N200 N74 Resubmit with multiple claims, each claim covering services provided in only one calendar month. Start: 01/01/2000 N75 Missing/incomplete/invalid tooth surface information. Start: 01/01/2000 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) N76 Missing/incomplete/invalid number of riders. Start: 01/01/2000 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) N77 Missing/incomplete/invalid designated provider number. Start: 01/01/2000 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) N78 The necessary components of the child and teen checkup (EPSDT) were not completed. Start: 01/01/2000 N79 Service billed is not compatible with patient location information. Start: 01/01/2000 N80 Missing/incomplete/invalid prenatal screening information. Start: 01/01/2000 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) N81 Procedure billed is not compatible with tooth surface code. Start: 01/01/2000 N82 Provider must accept insurance payment as payment in full when a third party payer contract specifies full reimbursement. Start: 01/01/2000 N83 No appeal rights. Adjudicative decision based on the provisions of a demonstration project. Start: 01/01/2000 N84 Alert: Further installment payments are forthcoming. Start: 01/01/2000 | Last Modified: 04/01/2007 Provider Manual 2013 258 Notes: (Modified 4/1/07, 8/1/07) N85 Alert: This is the final installment payment. Start: 01/01/2000 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07, 8/1/07) N86 A failed trial of pelvic muscle exercise training is required in order for biofeedback training for the treatment of urinary incontinence to be covered. Start: 01/01/2000 N87 Home use of biofeedback therapy is not covered. Start: 01/01/2000 N88 Alert: This payment is being made conditionally. An HHA episode of care notice has been filed for this patient. When a patient is treated under a HHA episode of care, consolidated billing requires that certain therapy services and supplies, such as this, be included in the HHA's payment. This payment will need to be recouped from you if we establish that the patient is concurrently receiving treatment under a HHA episode of care. Start: 01/01/2000 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N89 Alert: Payment information for this claim has been forwarded to more than one other payer, but format limitations permit only one of the secondary payers to be identified in this remittance advice. Start: 01/01/2000 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N90 Covered only when performed by the attending physician. Start: 01/01/2000 N91 Services not included in the appeal review. Start: 01/01/2000 N92 This facility is not certified for digital mammography. Start: 01/01/2000 N93 A separate claim must be submitted for each place of service. Services furnished at multiple sites may not be billed in the same claim. Start: 01/01/2000 N94 Claim/Service denied because a more specific taxonomy code is required for adjudication. Start: 01/01/2000 N95 This provider type/provider specialty may not bill this service. Start: 07/31/2001 | Last Modified: 02/28/2003 Notes: (Modified 2/28/03) N96 Patient must be refractory to conventional therapy (documented behavioral, pharmacologic and/or surgical corrective therapy) and be an appropriate surgical candidate such that implantation with anesthesia can occur. Start: 08/24/2001 N97 Patients with stress incontinence, urinary obstruction, and specific neurologic diseases (e.g., diabetes with peripheral nerve involvement) which are associated with secondary manifestations of the above three indications are excluded. Start: 08/24/2001 Provider Manual 2013 259 N98 Patient must have had a successful test stimulation in order to support subsequent implantation. Before a patient is eligible for permanent implantation, he/she must demonstrate a 50 percent or greater improvement through test stimulation. Improvement is measured through voiding diaries. Start: 08/24/2001 N99 Patient must be able to demonstrate adequate ability to record voiding diary data such that clinical results of the implant procedure can be properly evaluated. Start: 08/24/2001 N100 PPS (Prospect Payment System) code corrected during adjudication. Start: 09/14/2001 | Last Modified: 06/30/2003 Notes: (Modified 6/30/03) N101 Additional information is needed in order to process this claim. Please resubmit the claim with the identification number of the provider where this service took place. The Medicare number of the site of service provider should be preceded with the letters 'HSP' and entered into item #32 on the claim form. You may bill only one site of service provider number per claim. Start: 10/31/2001 | Stop: 01/31/2004 Notes: Consider uisng MA105 N102 This claim has been denied without reviewing the medical record because the requested records were not received or were not received timely. Start: 10/31/2001 N103 Social Security records indicate that this patient was a prisoner when the service was rendered. This payer does not cover items and services furnished to an individual while he or she is in a Federal facility, or while he or she is in State or local custody under a penal authority, unless under State or local law, the individual is personally liable for the cost of his or her health care while incarcerated and the State or local government pursues such debt in the same way and with the same vigor as any other debt. Start: 10/31/2001 | Last Modified: 07/01/2012 Notes: (Modified 6/30/03, 7/1/12) N104 This claim/service is not payable under our claims jurisdiction area. You can identify the correct Medicare contractor to process this claim/service through the CMS website at www.cms.gov. Start: 01/29/2002 | Last Modified: 07/01/2010 Notes: (Modified 10/31/02, 7/1/10) N105 This is a misdirected claim/service for an RRB beneficiary. Submit paper claims to the RRB carrier: Palmetto GBA, P.O. Box 10066, Augusta, GA 30999. Call 866-749-4301 for RRB EDI information for electronic claims processing. Start: 01/29/2002 N106 Payment for services furnished to Skilled Nursing Facility (SNF) inpatients (except for excluded services) can only be made to the SNF. You must request payment from the SNF rather than the patient for this service. Start: 01/31/2002 N107 Services furnished to Skilled Nursing Facility (SNF) inpatients must be billed on the inpatient claim. They cannot be billed separately as outpatient services. Start: 01/31/2002 N108 Missing/incomplete/invalid upgrade information. Start: 01/31/2002 | Last Modified: 02/28/2003 Provider Manual 2013 260 Notes: (Modified 2/28/03) N109 This claim/service was chosen for complex review and was denied after reviewing the medical records. Start: 02/28/2002 | Last Modified: 03/01/2009 Notes: (Modified 3/1/2009) N110 This facility is not certified for film mammography. Start: 02/28/2002 N111 No appeal right except duplicate claim/service issue. This service was included in a claim that has been previously billed and adjudicated. Start: 02/28/2002 N112 This claim is excluded from your electronic remittance advice. Start: 02/28/2002 N113 Only one initial visit is covered per physician, group practice or provider. Start: 04/16/2002 | Last Modified: 06/30/2003 Notes: (Modified 6/30/03) N114 During the transition to the Ambulance Fee Schedule, payment is based on the lesser of a blended amount calculated using a percentage of the reasonable charge/cost and fee schedule amounts, or the submitted charge for the service. You will be notified yearly what the percentages for the blended payment calculation will be. Start: 05/30/2002 N115 This decision was based on a Local Coverage Determination (LCD). An LCD provides a guide to assist in determining whether a particular item or service is covered. A copy of this policy is available at www.cms.gov/mcd, or if you do not have web access, you may contact the contractor to request a copy of the LCD. Start: 05/30/2002 | Last Modified: 07/01/2010 Notes: (Modified 4/1/04, 7/1/10) N116 This payment is being made conditionally because the service was provided in the home, and it is possible that the patient is under a home health episode of care. When a patient is treated under a home health episode of care, consolidated billing requires that certain therapy services and supplies, such as this, be included in the home health agency’s (HHA’s) payment. This payment will need to be recouped from you if we establish that the patient is concurrently receiving treatment under an HHA episode of care. Start: 06/30/2002 N117 This service is paid only once in a patient’s lifetime. Start: 07/30/2002 | Last Modified: 06/30/2003 Notes: (Modified 6/30/03) N118 This service is not paid if billed more than once every 28 days. Start: 07/30/2002 N119 This service is not paid if billed once every 28 days, and the patient has spent 5 or more consecutive days in any inpatient or Skilled /nursing Facility (SNF) within those 28 days. Start: 07/30/2002 | Last Modified: 06/30/2003 Notes: (Modified 6/30/03) N120 Payment is subject to home health prospective payment system partial episode payment adjustment. Patient was transferred/discharged/readmitted during payment episode. Provider Manual 2013 261 Start: 08/09/2002 | Last Modified: 06/30/2003 Notes: (Modified 6/30/03) N121 Medicare Part B does not pay for items or services provided by this type of practitioner for beneficiaries in a Medicare Part A covered Skilled Nursing Facility (SNF) stay. Start: 09/09/2002 | Last Modified: 08/01/2004 Notes: (Modified 8/1/04, 6/30/03) N122 Add-on code cannot be billed by itself. Start: 09/12/2002 | Last Modified: 08/01/2005 Notes: (Modified 8/1/05) N123 This is a split service and represents a portion of the units from the originally submitted service. Start: 09/24/2002 N124 Payment has been denied for the/made only for a less extensive service/item because the information furnished does not substantiate the need for the (more extensive) service/item. The patient is liable for the charges for this service/item as you informed the patient in writing before the service/item was furnished that we would not pay for it, and the patient agreed to pay. Start: 09/26/2002 N125 Payment has been (denied for the/made only for a less extensive) service/item because the information furnished does not substantiate the need for the (more extensive) service/item. If you have collected any amount from the patient, you must refund that amount to the patient within 30 days of receiving this notice. The requirements for a refund are in §1834(a)(18) of the Social Security Act (and in §§1834(j)(4) and 1879(h) by cross-reference to §1834(a)(18)). Section 1834(a)(18)(B) specifies that suppliers which knowingly and willfully fail to make appropriate refunds may be subject to civil money penalties and/or exclusion from the Medicare program. If you have any questions about this notice, please contact this office. Start: 09/26/2002 | Last Modified: 08/01/2005 Notes: (Modified 8/1/05. Also refer to N356) N126 Social Security Records indicate that this individual has been deported. This payer does not cover items and services furnished to individuals who have been deported. Start: 10/17/2002 N127 This is a misdirected claim/service for a United Mine Workers of America (UMWA) beneficiary. Please submit claims to them. Start: 10/31/2007 | Last Modified: 08/01/2004 Notes: (Modified 8/1/04 N128 This amount represents the prior to coverage portion of the allowance. Start: 10/31/2002 N129 Not eligible due to the patient's age. Start: 10/31/2002 | Last Modified: 08/01/2007 Notes: (Modified 8/1/07) N130 Consult plan benefit documents/guidelines for information about restrictions for this service. Start: 10/31/2002 | Last Modified: 11/01/2009 Notes: (Modified 4/1/07, 7/1/08, 11/1/09) Provider Manual 2013 262 N131 Total payments under multiple contracts cannot exceed the allowance for this service. Start: 10/31/2002 N132 Alert: Payments will cease for services rendered by this US Government debarred or excluded provider after the 30 day grace period as previously notified. Start: 10/31/2002 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N133 Alert: Services for predetermination and services requesting payment are being processed separately. Start: 10/31/2002 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N134 Alert: This represents your scheduled payment for this service. If treatment has been discontinued, please contact Customer Service. Start: 10/31/2002 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N135 Record fees are the patient's responsibility and limited to the specified co-payment. Start: 10/31/2002 N136 Alert: To obtain information on the process to file an appeal in Arizona, call the Department's Consumer Assistance Office at (602) 912-8444 or (800) 325-2548. Start: 10/31/2002 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N137 Alert: The provider acting on the Member's behalf, may file an appeal with the Payer. The provider, acting on the Member's behalf, may file a complaint with the State Insurance Regulatory Authority without first filing an appeal, if the coverage decision involves an urgent condition for which care has not been rendered. The address may be obtained from the State Insurance Regulatory Authority. Start: 10/31/2002 | Last Modified: 04/01/2007 Notes: (Modified 8/1/04, 2/28/03, 4/1/07) N138 Alert: In the event you disagree with the Dental Advisor's opinion and have additional information relative to the case, you may submit radiographs to the Dental Advisor Unit at the subscriber's dental insurance carrier for a second Independent Dental Advisor Review. Start: 10/31/2002 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N139 Alert: Under the Code of Federal Regulations, Chapter 32, Section 199.13 a nonparticipating provider is not an appropriate appealing party. Therefore, if you disagree with the Dental Advisor's opinion, you may appeal the determination if appointed in writing, by the beneficiary, to act as his/her representative. Should you be appointed as a representative, submit a copy of this letter, a signed statement explaining the matter in which you disagree, and any radiographs and relevant information to the subscriber's Dental insurance carrier within 90 days from the date of this letter. Start: 10/31/2002 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) Provider Manual 2013 263 N140 Alert: You have not been designated as an authorized OCONUS provider therefore are not considered an appropriate appealing party. If the beneficiary has appointed you, in writing, to act as his/her representative and you disagree with the Dental Advisor's opinion, you may appeal by submitting a copy of this letter, a signed statement explaining the matter in which you disagree, and any relevant information to the subscriber's Dental insurance carrier within 90 days from the date of this letter. Start: 10/31/2002 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N141 The patient was not residing in a long-term care facility during all or part of the service dates billed. Start: 10/31/2002 N142 The original claim was denied. Resubmit a new claim, not a replacement claim. Start: 10/31/2002 N143 The patient was not in a hospice program during all or part of the service dates billed. Start: 10/31/2002 N144 The rate changed during the dates of service billed. Start: 10/31/2002 N145 Missing/incomplete/invalid provider identifier for this place of service. Start: 10/31/2002 | Stop: 06/02/2005 N146 Missing screening document. Start: 10/31/2002 | Last Modified: 08/01/2004 Notes: (Modified 8/1/04) Related to N243 N147 Long term care case mix or per diem rate cannot be determined because the patient ID number is missing, incomplete, or invalid on the assignment request. Start: 10/31/2002 N148 Missing/incomplete/invalid date of last menstrual period. Start: 10/31/2002 N149 Rebill all applicable services on a single claim. Start: 10/31/2002 N150 Missing/incomplete/invalid model number. Start: 10/31/2002 N151 Telephone contact services will not be paid until the face-to-face contact requirement has been met. Start: 10/31/2002 N152 Missing/incomplete/invalid replacement claim information. Start: 10/31/2002 N153 Missing/incomplete/invalid room and board rate. Start: 10/31/2002 N154 Alert: This payment was delayed for correction of provider's mailing address. Start: 10/31/2002 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N155 Alert: Our records do not indicate that other insurance is on file. Please submit other insurance information for our records. Start: 10/31/2002 | Last Modified: 04/01/2007 Provider Manual 2013 264 Notes: (Modified 4/1/07) N156 Alert: The patient is responsible for the difference between the approved treatment and the elective treatment. Start: 10/31/2002 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N157 Transportation to/from this destination is not covered. Start: 02/28/2003 | Last Modified: 02/01/2004 Notes: (Modified 2/1/04) N158 Transportation in a vehicle other than an ambulance is not covered. Start: 02/28/2003 N159 Payment denied/reduced because mileage is not covered when the patient is not in the ambulance. Start: 02/28/2003 N160 The patient must choose an option before a payment can be made for this procedure/ equipment/ supply/ service. Start: 02/28/2003 | Last Modified: 02/01/2004 Notes: (Modified 2/1/04) N161 This drug/service/supply is covered only when the associated service is covered. Start: 02/28/2003 N162 Alert: Although your claim was paid, you have billed for a test/specialty not included in your Laboratory Certification. Your failure to correct the laboratory certification information will result in a denial of payment in the near future. Start: 02/28/2003 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N163 Medical record does not support code billed per the code definition. Start: 02/28/2003 N164 Transportation to/from this destination is not covered. Start: 02/28/2003 | Stop: 01/31/2004 Notes: Consider using N157 N165 Transportation in a vehicle other than an ambulance is not covered. Start: 02/28/2003 | Stop: 01/31/2004 Notes: Consider using N158) N166 Payment denied/reduced because mileage is not covered when the patient is not in the ambulance. Start: 02/28/2003 | Stop: 01/31/2004 Notes: Consider using N159 N167 Charges exceed the post-transplant coverage limit. Start: 02/28/2003 N168 The patient must choose an option before a payment can be made for this procedure/ equipment/ supply/ service. Start: 02/28/2003 | Stop: 01/31/2004 Notes: Consider using N160 N169 This drug/service/supply is covered only when the associated service is covered. Start: 02/28/2003 | Stop: 01/31/2004 Provider Manual 2013 265 Notes: Consider using N161 N170 A new/revised/renewed certificate of medical necessity is needed. Start: 02/28/2003 N171 Payment for repair or replacement is not covered or has exceeded the purchase price. Start: 02/28/2003 N172 The patient is not liable for the denied/adjusted charge(s) for receiving any updated service/item. Start: 02/28/2003 N173 No qualifying hospital stay dates were provided for this episode of care. Start: 02/28/2003 N174 This is not a covered service/procedure/ equipment/bed, however patient liability is limited to amounts shown in the adjustments under group 'PR'. Start: 02/28/2003 N175 Missing review organization approval. Start: 02/28/2003 | Last Modified: 02/29/2008 Notes: (Modified 8/1/04, 2/29/08) Related to N241 N176 Services provided aboard a ship are covered only when the ship is of United States registry and is in United States waters. In addition, a doctor licensed to practice in the United States must provide the service. Start: 02/28/2003 N177 Alert: We did not send this claim to patient’s other insurer. They have indicated no additional payment can be made. Start: 02/28/2003 | Last Modified: 04/01/2007 Notes: (Modified 6/30/03, 4/1/07) N178 Missing pre-operative photos or visual field results. Start: 02/28/2003 | Last Modified: 08/01/2004 Notes: (Modified 8/1/04) Related to N244 N179 Additional information has been requested from the member. The charges will be reconsidered upon receipt of that information. Start: 02/28/2003 N180 This item or service does not meet the criteria for the category under which it was billed. Start: 02/28/2003 N181 Additional information is required from another provider involved in this service. Start: 02/28/2003 | Last Modified: 12/01/2006 Notes: (Modified 12/1/06) N182 This claim/service must be billed according to the schedule for this plan. Start: 02/28/2003 N183 Alert: This is a predetermination advisory message, when this service is submitted for payment additional documentation as specified in plan documents will be required to process benefits. Start: 02/28/2003 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N184 Rebill technical and professional components separately. Start: 02/28/2003 Provider Manual 2013 266 N185 Alert: Do not resubmit this claim/service. Start: 02/28/2003 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N186 Non-Availability Statement (NAS) required for this service. Contact the nearest Military Treatment Facility (MTF) for assistance. Start: 02/28/2003 N187 Alert: You may request a review in writing within the required time limits following receipt of this notice by following the instructions included in your contract or plan benefit documents. Start: 02/28/2003 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N188 The approved level of care does not match the procedure code submitted. Start: 02/28/2003 N189 Alert: This service has been paid as a one-time exception to the plan's benefit restrictions. Start: 02/28/2003 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N190 Missing contract indicator. Start: 02/28/2003 | Last Modified: 08/01/2004 Notes: (Modified 8/1/04) Related to N229 N191 The provider must update insurance information directly with payer. Start: 02/28/2003 N192 Patient is a Medicaid/Qualified Medicare Beneficiary. Start: 02/28/2003 N193 Specific federal/state/local program may cover this service through another payer. Start: 02/28/2003 N194 Technical component not paid if provider does not own the equipment used. Start: 02/25/2003 N195 The technical component must be billed separately. Start: 02/25/2003 N196 Alert: Patient eligible to apply for other coverage which may be primary. Start: 02/25/2003 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N197 The subscriber must update insurance information directly with payer. Start: 02/25/2003 N198 Rendering provider must be affiliated with the pay-to provider. Start: 02/25/2003 N199 Additional payment/recoupment approved based on payer-initiated review/audit. Start: 02/25/2003 | Last Modified: 08/01/2006 Notes: (Modified 8/1/06) N200 The professional component must be billed separately. Start: 02/25/2003 Provider Manual 2013 267 N201 A mental health facility is responsible for payment of outside providers who furnish these services/supplies to residents. Start: 02/25/2003 | Stop: 01/01/2011 Notes: Consider using N538 N202 Additional information/explanation will be sent separately Start: 06/30/2003 | Last Modified: 11/01/2009 Notes: (Modified 4/1/07, 11/1/09) N203 Missing/incomplete/invalid anesthesia time/units Start: 06/30/2003 N204 Services under review for possible pre-existing condition. Send medical records for prior 12 months Start: 06/30/2003 N205 Information provided was illegible Start: 06/30/2003 N206 The supporting documentation does not match the information sent on the claim. Start: 06/30/2003 | Last Modified: 03/06/2012 Notes: (Modified 3/6/12) N207 Missing/incomplete/invalid weight. Start: 06/30/2003 | Last Modified: 11/18/2005 Notes: (Modified 11/18/05) N208 Missing/incomplete/invalid DRG code Start: 06/30/2003 N209 Missing/incomplete/invalid taxpayer identification number (TIN). Start: 06/30/2003 | Last Modified: 07/01/2008 Notes: (Modified 7/1/08) N210 Alert: You may appeal this decision Start: 06/30/2003 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N211 Alert: You may not appeal this decision Start: 06/30/2003 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N212 Charges processed under a Point of Service benefit Start: 02/01/2004 N213 Missing/incomplete/invalid facility/discrete unit DRG/DRG exempt status information Start: 04/01/2004 N214 Missing/incomplete/invalid history of the related initial surgical procedure(s) Start: 04/01/2004 N215 Alert: A payer providing supplemental or secondary coverage shall not require a claims determination for this service from a primary payer as a condition of making its own claims determination. Start: 04/01/2004 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) Provider Manual 2013 268 N216 We do not offer coverage for this type of service or the patient is not enrolled in this portion of our benefit package Start: 04/01/2004 | Last Modified: 03/01/2010 Notes: (modified 3/1/2010) N217 We pay only one site of service per provider per claim N218 You must furnish and service this item for as long as the patient continues to need it. We can pay for maintenance and/or servicing for the time period specified in the contract or coverage manual. Start: 08/01/2004 N219 Payment based on previous payer's allowed amount. Start: 08/01/2004 N220 Alert: See the payer's web site or contact the payer's Customer Service department to obtain forms and instructions for filing a provider dispute. Start: 08/01/2004 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N221 Missing Admitting History and Physical report. Start: 08/01/2004 N222 Incomplete/invalid Admitting History and Physical report. Start: 08/01/2004 N223 Missing documentation of benefit to the patient during initial treatment period. Start: 08/01/2004 N224 Incomplete/invalid documentation of benefit to the patient during initial treatment period. Start: 08/01/2004 N225 Incomplete/invalid documentation/orders/notes/summary/report/chart. Start: 08/01/2004 | Last Modified: 08/01/2005 Notes: (Modified 8/1/05) N226 Incomplete/invalid American Diabetes Association Certificate of Recognition. Start: 08/01/2004 N227 Incomplete/invalid Certificate of Medical Necessity. Start: 08/01/2004 N228 Incomplete/invalid consent form. Start: 08/01/2004 N229 Incomplete/invalid contract indicator. Start: 08/01/2004 N230 Incomplete/invalid indication of whether the patient owns the equipment that requires the part or supply. Start: 08/01/2004 N231 Incomplete/invalid invoice or statement certifying the actual cost of the lens, less discounts, and/or the type of intraocular lens used. Start: 08/01/2004 N232 Incomplete/invalid itemized bill/statement. Start: 08/01/2004 | Last Modified: 07/01/2008 Notes: (Modified 7/1/08) Provider Manual 2013 269 N233 Incomplete/invalid operative note/report. Start: 08/01/2004 | Last Modified: 07/01/2008 Notes: (Modified 7/1/08) N234 Incomplete/invalid oxygen certification/re-certification. Start: 08/01/2004 N235 Incomplete/invalid pacemaker registration form. Start: 08/01/2004 N236 Incomplete/invalid pathology report. Start: 08/01/2004 N237 Incomplete/invalid patient medical record for this service. Start: 08/01/2004 N238 Incomplete/invalid physician certified plan of care Start: 08/01/2004 N239 Incomplete/invalid physician financial relationship form. Start: 08/01/2004 N240 Incomplete/invalid radiology report. Start: 08/01/2004 N241 Incomplete/invalid review organization approval. Start: 08/01/2004 | Last Modified: 02/29/2008 Notes: (Modified 2/29/08) N242 Incomplete/invalid radiology film(s)/image(s). Start: 08/01/2004 | Last Modified: 07/01/2008 Notes: (Modified 7/1/08) N243 Incomplete/invalid/not approved screening document. Start: 08/01/2004 N244 Incomplete/invalid pre-operative photos/visual field results. Start: 08/01/2004 N245 Incomplete/invalid plan information for other insurance Start: 08/01/2004 N246 State regulated patient payment limitations apply to this service. Start: 12/02/2004 N247 Missing/incomplete/invalid assistant surgeon taxonomy. Start: 12/02/2004 N248 Missing/incomplete/invalid assistant surgeon name. Start: 12/02/2004 N249 Missing/incomplete/invalid assistant surgeon primary identifier. Start: 12/02/2004 N250 Missing/incomplete/invalid assistant surgeon secondary identifier. Start: 12/02/2004 N251 Missing/incomplete/invalid attending provider taxonomy. Start: 12/02/2004 Provider Manual 2013 270 N252 Missing/incomplete/invalid attending provider name. Start: 12/02/2004 N253 Missing/incomplete/invalid attending provider primary identifier. Start: 12/02/2004 N254 Missing/incomplete/invalid attending provider secondary identifier. Start: 12/02/2004 N255 Missing/incomplete/invalid billing provider taxonomy. Start: 12/02/2004 N256 Missing/incomplete/invalid billing provider/supplier name. Start: 12/02/2004 N257 Missing/incomplete/invalid billing provider/supplier primary identifier. Start: 12/02/2004 N258 Missing/incomplete/invalid billing provider/supplier address. Start: 12/02/2004 N259 Missing/incomplete/invalid billing provider/supplier secondary identifier. Start: 12/02/2004 N260 Missing/incomplete/invalid billing provider/supplier contact information. Start: 12/02/2004 N261 Missing/incomplete/invalid operating provider name. Start: 12/02/2004 N262 Missing/incomplete/invalid operating provider primary identifier. Start: 12/02/2004 N263 Missing/incomplete/invalid operating provider secondary identifier. Start: 12/02/2004 N264 Missing/incomplete/invalid ordering provider name. Start: 12/02/2004 N265 Missing/incomplete/invalid ordering provider primary identifier. Start: 12/02/2004 N266 Missing/incomplete/invalid ordering provider address. Start: 12/02/2004 N267 Missing/incomplete/invalid ordering provider secondary identifier. Start: 12/02/2004 N268 Missing/incomplete/invalid ordering provider contact information. Start: 12/02/2004 N269 Missing/incomplete/invalid other provider name. Start: 12/02/2004 N270 Missing/incomplete/invalid other provider primary identifier. Start: 12/02/2004 N271 Missing/incomplete/invalid other provider secondary identifier. Start: 12/02/2004 N272 Missing/incomplete/invalid other payer attending provider identifier. Provider Manual 2013 271 Start: 12/02/2004 N273 Missing/incomplete/invalid other payer operating provider identifier. Start: 12/02/2004 N274 Missing/incomplete/invalid other payer other provider identifier. Start: 12/02/2004 N275 Missing/incomplete/invalid other payer purchased service provider identifier. Start: 12/02/2004 N276 Missing/incomplete/invalid other payer referring provider identifier. Start: 12/02/2004 N277 Missing/incomplete/invalid other payer rendering provider identifier. Start: 12/02/2004 N278 Missing/incomplete/invalid other payer service facility provider identifier. Start: 12/02/2004 N279 Missing/incomplete/invalid pay-to provider name. Start: 12/02/2004 N280 Missing/incomplete/invalid pay-to provider primary identifier. Start: 12/02/2004 N281 Missing/incomplete/invalid pay-to provider address. Start: 12/02/2004 N282 Missing/incomplete/invalid pay-to provider secondary identifier. Start: 12/02/2004 N283 Missing/incomplete/invalid purchased service provider identifier. Start: 12/02/2004 N284 Missing/incomplete/invalid referring provider taxonomy. Start: 12/02/2004 N285 Missing/incomplete/invalid referring provider name. Start: 12/02/2004 N286 Missing/incomplete/invalid referring provider primary identifier. Start: 12/02/2004 N287 Missing/incomplete/invalid referring provider secondary identifier. Start: 12/02/2004 N288 Missing/incomplete/invalid rendering provider taxonomy. Start: 12/02/2004 N289 Missing/incomplete/invalid rendering provider name. Start: 12/02/2004 N290 Missing/incomplete/invalid rendering provider primary identifier. Start: 12/02/2004 N291 Missing/incomplete/invalid rendering provider secondary identifier. Start: 12/02/2004 | Last Modified: 11/01/2010 N292 Missing/incomplete/invalid service facility name. Start: 12/02/2004 Provider Manual 2013 272 N293 Missing/incomplete/invalid service facility primary identifier. Start: 12/02/2004 N294 Missing/incomplete/invalid service facility primary address. Start: 12/02/2004 N295 Missing/incomplete/invalid service facility secondary identifier. Start: 12/02/2004 N296 Missing/incomplete/invalid supervising provider name. Start: 12/02/2004 N297 Missing/incomplete/invalid supervising provider primary identifier. Start: 12/02/2004 N298 Missing/incomplete/invalid supervising provider secondary identifier. Start: 12/02/2004 N299 Missing/incomplete/invalid occurrence date(s). Start: 12/02/2004 N300 Missing/incomplete/invalid occurrence span date(s). Start: 12/02/2004 N301 Missing/incomplete/invalid procedure date(s). Start: 12/02/2004 N302 Missing/incomplete/invalid other procedure date(s). Start: 12/02/2004 N303 Missing/incomplete/invalid principal procedure date. Start: 12/02/2004 N304 Missing/incomplete/invalid dispensed date. Start: 12/02/2004 N305 Missing/incomplete/invalid accident date. Start: 12/02/2004 N306 Missing/incomplete/invalid acute manifestation date. Start: 12/02/2004 N307 Missing/incomplete/invalid adjudication or payment date. Start: 12/02/2004 N308 Missing/incomplete/invalid appliance placement date. Start: 12/02/2004 N309 Missing/incomplete/invalid assessment date. Start: 12/02/2004 N310 Missing/incomplete/invalid assumed or relinquished care date. Start: 12/02/2004 N311 Missing/incomplete/invalid authorized to return to work date. Start: 12/02/2004 N312 Missing/incomplete/invalid begin therapy date. Start: 12/02/2004 N313 Missing/incomplete/invalid certification revision date. Provider Manual 2013 273 Start: 12/02/2004 N314 Missing/incomplete/invalid diagnosis date. Start: 12/02/2004 N315 Missing/incomplete/invalid disability from date. Start: 12/02/2004 N316 Missing/incomplete/invalid disability to date. Start: 12/02/2004 N317 Missing/incomplete/invalid discharge hour. Start: 12/02/2004 N318 Missing/incomplete/invalid discharge or end of care date. Start: 12/02/2004 N319 Missing/incomplete/invalid hearing or vision prescription date. Start: 12/02/2004 N320 Missing/incomplete/invalid Home Health Certification Period. Start: 12/02/2004 N321 Missing/incomplete/invalid last admission period. Start: 12/02/2004 N322 Missing/incomplete/invalid last certification date. Start: 12/02/2004 N323 Missing/incomplete/invalid last contact date. Start: 12/02/2004 N324 Missing/incomplete/invalid last seen/visit date. Start: 12/02/2004 N325 Missing/incomplete/invalid last worked date. Start: 12/02/2004 N326 Missing/incomplete/invalid last x-ray date. Start: 12/02/2004 N327 Missing/incomplete/invalid other insured birth date. Start: 12/02/2004 N328 Missing/incomplete/invalid Oxygen Saturation Test date. Start: 12/02/2004 N329 Missing/incomplete/invalid patient birth date. Start: 12/02/2004 N330 Missing/incomplete/invalid patient death date. Start: 12/02/2004 N331 Missing/incomplete/invalid physician order date. Start: 12/02/2004 N332 Missing/incomplete/invalid prior hospital discharge date. Start: 12/02/2004 N333 Missing/incomplete/invalid prior placement date. Start: 12/02/2004 Provider Manual 2013 274 N334 Missing/incomplete/invalid re-evaluation date Start: 12/02/2004 N335 Missing/incomplete/invalid referral date. Start: 12/02/2004 N336 Missing/incomplete/invalid replacement date. Start: 12/02/2004 N337 Missing/incomplete/invalid secondary diagnosis date. Start: 12/02/2004 N338 Missing/incomplete/invalid shipped date. Start: 12/02/2004 N339 Missing/incomplete/invalid similar illness or symptom date. Start: 12/02/2004 N340 Missing/incomplete/invalid subscriber birth date. Start: 12/02/2004 N341 Missing/incomplete/invalid surgery date. Start: 12/02/2004 N342 Missing/incomplete/invalid test performed date. Start: 12/02/2004 N343 Missing/incomplete/invalid Transcutaneous Electrical Nerve Stimulator (TENS) trial start date. Start: 12/02/2004 N344 Missing/incomplete/invalid Transcutaneous Electrical Nerve Stimulator (TENS) trial end date. Start: 12/02/2004 N345 Date range not valid with units submitted. Start: 03/30/2005 N346 Missing/incomplete/invalid oral cavity designation code. Start: 03/30/2005 N347 Your claim for a referred or purchased service cannot be paid because payment has already been made for this same service to another provider by a payment contractor representing the payer. Start: 03/30/2005 N348 You chose that this service/supply/drug would be rendered/supplied and billed by a different practitioner/supplier. Start: 08/01/2005 N349 The administration method and drug must be reported to adjudicate this service. Start: 08/01/2005 N350 Missing/incomplete/invalid description of service for a Not Otherwise Classified (NOC) code or for an Unlisted/By Report procedure. Start: 08/01/2005 | Last Modified: 07/01/2008 Notes: (Modified 7/1/08) N351 Service date outside of the approved treatment plan service dates. Start: 08/01/2005 Provider Manual 2013 275 N352 Alert: There are no scheduled payments for this service. Submit a claim for each patient visit. Start: 08/01/2005 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N353 Alert: Benefits have been estimated, when the actual services have been rendered, additional payment will be considered based on the submitted claim. Start: 08/01/2005 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N354 Incomplete/invalid invoice Start: 08/01/2005 N355 Alert: The law permits exceptions to the refund requirement in two cases: - If you did not know, and could not have reasonably been expected to know, that we would not pay for this service; or - If you notified the patient in writing before providing the service that you believed that we were likely to deny the service, and the patient signed a statement agreeing to pay for the service. If you come within either exception, or if you believe the carrier was wrong in its determination that we do not pay for this service, you should request appeal of this determination within 30 days of the date of this notice. Your request for review should include any additional information necessary to support your position. If you request an appeal within 30 days of receiving this notice, you may delay refunding the amount to the patient until you receive the results of the review. If the review decision is favorable to you, you do not need to make any refund. If, however, the review is unfavorable, the law specifies that you must make the refund within 15 days of receiving the unfavorable review decision. The law also permits you to request an appeal at any time within 120 days of the date you receive this notice. However, an appeal request that is received more than 30 days after the date of this notice, does not permit you to delay making the refund. Regardless of when a review is requested, the patient will be notified that you have requested one, and will receive a copy of the determination. The patient has received a separate notice of this denial decision. The notice advises that he/she may be entitled to a refund of any amounts paid, if you should have known that we would not pay and did not tell him/her. It also instructs the patient to contact our office if he/she does not hear anything about a refund within 30 days Start: 08/01/2005 | Last Modified: 04/01/2007 Notes: (Modified 11/18/05, Modified 4/1/07) N356 Not covered when performed with, or subsequent to, a non-covered service. Start: 08/01/2005 | Last Modified: 03/08/2011 Notes: (Modified 3/8/11) N357 Time frame requirements between this service/procedure/supply and a related service/procedure/supply have not been met. Start: 11/18/2005 N358 Alert: This decision may be reviewed if additional documentation as described in the contract or plan benefit documents is submitted. Start: 11/18/2005 | Last Modified: 04/01/2007 Provider Manual 2013 276 Notes: (Modified 4/1/07) N359 Missing/incomplete/invalid height. Start: 11/18/2005 N360 Alert: Coordination of benefits has not been calculated when estimating benefits for this pre-determination. Submit payment information from the primary payer with the secondary claim. Start: 11/18/2005 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N361 Payment adjusted based on multiple diagnostic imaging procedure rules Start: 11/18/2005 | Stop: 10/01/2007 | Last Modified: 12/01/2006 Notes: (Modified 12/1/06) Consider using Reason Code 59 N362 The number of Days or Units of Service exceeds our acceptable maximum. Start: 11/18/2005 N363 Alert: in the near future we are implementing new policies/procedures that would affect this determination. Start: 11/18/2005 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N364 Alert: According to our agreement, you must waive the deductible and/or coinsurance amounts. Start: 11/18/2005 | Last Modified: 04/01/2007 Notes: (Modified 4/1/07) N365 This procedure code is not payable. It is for reporting/information purposes only. Start: 04/01/2006 N366 Requested information not provided. The claim will be reopened if the information previously requested is submitted within one year after the date of this denial notice. Start: 04/01/2006 N367 Alert: The claim information has been forwarded to a Consumer Spending Account processor for review; for example, flexible spending account or health savings account. Start: 04/01/2006 | Last Modified: 07/01/2008 Notes: (Modified 4/1/07, 11/5/07, 7/1/08) N368 You must appeal the determination of the previously adjudicated claim. Start: 04/01/2006 N369 Alert: Although this claim has been processed, it is deficient according to state legislation/regulation. Start: 04/01/2006 N370 Billing exceeds the rental months covered/approved by the payer. Start: 08/01/2006 N371 Alert: title of this equipment must be transferred to the patient. Start: 08/01/2006 N372 Only reasonable and necessary maintenance/service charges are covered. Start: 08/01/2006 N373 It has been determined that another payer paid the services as primary when they were not the primary payer. Therefore, we are refunding to the payer that paid as primary on your behalf. Provider Manual 2013 277 Start: 12/01/2006 N374 Primary Medicare Part A insurance has been exhausted and a Part B Remittance Advice is required. Start: 12/01/2006 N375 Missing/incomplete/invalid questionnaire/information required to determine dependent eligibility. Start: 12/01/2006 N376 Subscriber/patient is assigned to active military duty, therefore primary coverage may be TRICARE. Start: 12/01/2006 N377 Payment based on a processed replacement claim. Start: 12/01/2006 | Last Modified: 11/05/2007 Notes: (Modified 11/5/07) N378 Missing/incomplete/invalid prescription quantity. Start: 12/01/2006 N379 Claim level information does not match line level information. Start: 12/01/2006 N380 The original claim has been processed, submit a corrected claim. Start: 04/01/2007 N381 Consult our contractual agreement for restrictions/billing/payment information related to these charges. Start: 04/01/2007 N382 Missing/incomplete/invalid patient identifier. Start: 04/01/2007 N383 Not covered when deemed cosmetic. Start: 04/01/2007 | Last Modified: 03/08/2011 Notes: (Modified 3/8/11) N384 Records indicate that the referenced body part/tooth has been removed in a previous procedure. Start: 04/01/2007 N385 Notification of admission was not timely according to published plan procedures. Start: 04/01/2007 | Last Modified: 11/05/2007 Notes: (Modified 11/5/07) N386 This decision was based on a National Coverage Determination (NCD). An NCD provides a coverage determination as to whether a particular item or service is covered. A copy of this policy is available at www.cms.gov/mcd/search.asp. If you do not have web access, you may contact the contractor to request a copy of the NCD. Start: 04/01/2007 | Last Modified: 07/01/2010 Notes: (Modified 7/1/2010) N387 Alert: Submit this claim to the patient's other insurer for potential payment of supplemental benefits. We did not forward the claim information. Start: 04/01/2007 | Last Modified: 03/01/2009 Notes: (Modified 3/1/2009) N388 Missing/incomplete/invalid prescription number Provider Manual 2013 278 Start: 08/01/2007 N389 Duplicate prescription number submitted. Start: 08/01/2007 N390 This service/report cannot be billed separately. Start: 08/01/2007 | Last Modified: 07/01/2008 Notes: (Modified 7/1/08) N391 Missing emergency department records. Start: 08/01/2007 N392 Incomplete/invalid emergency department records. Start: 08/01/2007 N393 Missing progress notes/report. Start: 08/01/2007 | Last Modified: 07/01/2008 Notes: (Modified 7/1/08) N394 Incomplete/invalid progress notes/report. Start: 08/01/2007 | Last Modified: 07/01/2008 Notes: (Modified 7/1/08) N395 Missing laboratory report. Start: 08/01/2007 N396 Incomplete/invalid laboratory report. Start: 08/01/2007 N397 Benefits are not available for incomplete service(s)/undelivered item(s). Start: 08/01/2007 N398 Missing elective consent form. Start: 08/01/2007 N399 Incomplete/invalid elective consent form. Start: 08/01/2007 N400 Alert: Electronically enabled providers should submit claims electronically. Start: 08/01/2007 N401 Missing periodontal charting. Start: 08/01/2007 N402 Incomplete/invalid periodontal charting. Start: 08/01/2007 N403 Missing facility certification. Start: 08/01/2007 N404 Incomplete/invalid facility certification. Start: 08/01/2007 N405 This service is only covered when the donor's insurer(s) do not provide coverage for the service. Start: 08/01/2007 N406 This service is only covered when the recipient's insurer(s) do not provide coverage for the service. Start: 08/01/2007 Provider Manual 2013 279 N407 You are not an approved submitter for this transmission format. Start: 08/01/2007 N408 This payer does not cover deductibles assessed by a previous payer. Start: 08/01/2007 N409 This service is related to an accidental injury and is not covered unless provided within a specific time frame from the date of the accident. Start: 08/01/2007 N410 Not covered unless the prescription changes. Start: 08/01/2007 | Last Modified: 03/08/2011 Notes: (Modified 3/8/11) N411 This service is allowed one time in a 6-month period. (This temporary code will be deactivated on 2/1/09. Must be used with Reason Code 119.) Start: 08/01/2007 | Stop: 02/01/2009 N412 This service is allowed 2 times in a 12-month period. (This temporary code will be deactivated on 2/1/09. Must be used with Reason Code 119.) Start: 08/01/2007 | Stop: 02/01/2009 N413 This service is allowed 2 times in a benefit year. (This temporary code will be deactivated on 2/1/09. Must be used with Reason Code 119.) Start: 08/01/2007 | Stop: 02/01/2009 N414 This service is allowed 4 times in a 12-month period. (This temporary code will be deactivated on 2/1/09. Must be used with Reason Code 119.) Start: 08/01/2007 | Stop: 02/01/2009 N415 This service is allowed 1 time in an 18-month period. (This temporary code will be deactivated on 2/1/09. Must be used with Reason Code 119.) Start: 08/01/2007 | Stop: 02/01/2009 N416 This service is allowed 1 time in a 3-year period. (This temporary code will be deactivated on 2/1/09. Must be used with Reason Code 119.) Start: 08/01/2007 | Stop: 02/01/2009 N417 This service is allowed 1 time in a 5-year period. (This temporary code will be deactivated on 2/1/09. Must be used with Reason Code 119.) Start: 08/01/2007 | Stop: 02/01/2009 N418 Misrouted claim. See the payer's claim submission instructions. Start: 08/01/2007 N419 Claim payment was the result of a payer's retroactive adjustment due to a retroactive rate change. Start: 08/01/2007 N420 Claim payment was the result of a payer's retroactive adjustment due to a Coordination of Benefits or Third Party Liability Recovery. Start: 08/01/2007 N421 Claim payment was the result of a payer's retroactive adjustment due to a review organization decision. Start: 08/01/2007 | Last Modified: 05/08/2008 Notes: (Modified 2/29/08, typo fixed 5/8/08) N422 Claim payment was the result of a payer's retroactive adjustment due to a payer's contract incentive program. Start: 08/01/2007 | Last Modified: 05/08/2008 Provider Manual 2013 280 Notes: (Typo fixed 5/8/08) N423 Claim payment was the result of a payer's retroactive adjustment due to a non standard program. Start: 08/01/2007 N424 Patient does not reside in the geographic area required for this type of payment. Start: 08/01/2007 N425 Statutorily excluded service(s). Start: 08/01/2007 N426 No coverage when self-administered. Start: 08/01/2007 N427 Payment for eyeglasses or contact lenses can be made only after cataract surgery. Start: 08/01/2007 N428 Not covered when performed in this place of service. Start: 08/01/2007 | Last Modified: 03/08/2011 Notes: (Modified 3/8/11) N429 Not covered when considered routine. Start: 08/01/2007 | Last Modified: 03/08/2011 Notes: (Modified 3/8/11) N430 Procedure code is inconsistent with the units billed. Start: 11/05/2007 N431 Not covered with this procedure. Start: 11/05/2007 | Last Modified: 03/08/2011 Notes: (Modified 3/8/11) N432 Adjustment based on a Recovery Audit. Start: 11/05/2007 N433 Resubmit this claim using only your National Provider Identifier (NPI) Start: 02/29/2008 N434 Missing/Incomplete/Invalid Present on Admission indicator. Start: 07/01/2008 N435 Exceeds number/frequency approved /allowed within time period without support documentation. Start: 07/01/2008 N436 The injury claim has not been accepted and a mandatory medical reimbursement has been made. Start: 07/01/2008 N437 Alert: If the injury claim is accepted, these charges will be reconsidered. Start: 07/01/2008 N438 This jurisdiction only accepts paper claims Start: 07/01/2008 N439 Missing anesthesia physical status report/indicators. Start: 07/01/2008 N440 Incomplete/invalid anesthesia physical status report/indicators. Provider Manual 2013 281 Start: 07/01/2008 N441 This missed appointment is not covered. Start: 07/01/2008 N442 Payment based on an alternate fee schedule. Start: 07/01/2008 N443 Missing/incomplete/invalid total time or begin/end time. Start: 07/01/2008 N444 Alert: This facility has not filed the Election for High Cost Outlier form with the Division of Workers' Compensation. Start: 07/01/2008 N445 Missing document for actual cost or paid amount. Start: 07/01/2008 N446 Incomplete/invalid document for actual cost or paid amount. Start: 07/01/2008 N447 Payment is based on a generic equivalent as required documentation was not provided. Start: 07/01/2008 N448 This drug/service/supply is not included in the fee schedule or contracted/legislated fee arrangement Start: 07/01/2008 N449 Payment based on a comparable drug/service/supply. Start: 07/01/2008 N450 Covered only when performed by the primary treating physician or the designee. Start: 07/01/2008 N451 Missing Admission Summary Report. Start: 07/01/2008 N452 Incomplete/invalid Admission Summary Report. Start: 07/01/2008 N453 Missing Consultation Report. Start: 07/01/2008 N454 Incomplete/invalid Consultation Report. Start: 07/01/2008 N455 Missing Physician Order. Start: 07/01/2008 N456 Incomplete/invalid Physician Order. Start: 07/01/2008 N457 Missing Diagnostic Report. Start: 07/01/2008 N458 Incomplete/invalid Diagnostic Report. Start: 07/01/2008 N459 Missing Discharge Summary. Start: 07/01/2008 N460 Incomplete/invalid Discharge Summary. Provider Manual 2013 282 Start: 07/01/2008 N461 Missing Nursing Notes. Start: 07/01/2008 N462 Incomplete/invalid Nursing Notes. Start: 07/01/2008 N463 Missing support data for claim. Start: 07/01/2008 N464 Incomplete/invalid support data for claim. Start: 07/01/2008 N465 Missing Physical Therapy Notes/Report. Start: 07/01/2008 N466 Incomplete/invalid Physical Therapy Notes/Report. Start: 07/01/2008 N467 Missing Report of Tests and Analysis Report. Start: 07/01/2008 N468 Incomplete/invalid Report of Tests and Analysis Report. Start: 07/01/2008 N469 Alert: Claim/Service(s) subject to appeal process, see section 935 of Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (MMA). Start: 07/01/2008 N470 This payment will complete the mandatory medical reimbursement limit. Start: 07/01/2008 N471 Missing/incomplete/invalid HIPPS Rate Code. Start: 07/01/2008 N472 Payment for this service has been issued to another provider. Start: 07/01/2008 N473 Missing certification. Start: 07/01/2008 N474 Incomplete/invalid certification Start: 07/01/2008 N475 Missing completed referral form. Start: 07/01/2008 N476 Incomplete/invalid completed referral form Start: 07/01/2008 N477 Missing Dental Models. Start: 07/01/2008 N478 Incomplete/invalid Dental Models Start: 07/01/2008 N479 Missing Explanation of Benefits (Coordination of Benefits or Medicare Secondary Payer). Start: 07/01/2008 N480 Incomplete/invalid Explanation of Benefits (Coordination of Benefits or Medicare Secondary Payer). Provider Manual 2013 283 Start: 07/01/2008 N481 Missing Models. Start: 07/01/2008 N482 Incomplete/invalid Models Start: 07/01/2008 N483 Missing Periodontal Charts. Start: 07/01/2008 N484 Incomplete/invalid Periodontal Charts Start: 07/01/2008 N485 Missing Physical Therapy Certification. Start: 07/01/2008 N486 Incomplete/invalid Physical Therapy Certification. Start: 07/01/2008 N487 Missing Prosthetics or Orthotics Certification. Start: 07/01/2008 N488 Incomplete/invalid Prosthetics or Orthotics Certification Start: 07/01/2008 N489 Missing referral form. Start: 07/01/2008 N490 Incomplete/invalid referral form Start: 07/01/2008 N491 Missing/Incomplete/Invalid Exclusionary Rider Condition. Start: 07/01/2008 N492 Alert: A network provider may bill the member for this service if the member requested the service and agreed in writing, prior to receiving the service, to be financially responsible for the billed charge. Start: 07/01/2008 N493 Missing Doctor First Report of Injury. Start: 07/01/2008 N494 Incomplete/invalid Doctor First Report of Injury. Start: 07/01/2008 N495 Missing Supplemental Medical Report. Start: 07/01/2008 N496 Incomplete/invalid Supplemental Medical Report. Start: 07/01/2008 N497 Missing Medical Permanent Impairment or Disability Report. Start: 07/01/2008 N498 Incomplete/invalid Medical Permanent Impairment or Disability Report. Start: 07/01/2008 N499 Missing Medical Legal Report. Start: 07/01/2008 N500 Incomplete/invalid Medical Legal Report. Provider Manual 2013 284 Start: 07/01/2008 N501 Missing Vocational Report. Start: 07/01/2008 N502 Incomplete/invalid Vocational Report. Start: 07/01/2008 N503 Missing Work Status Report. Start: 07/01/2008 N504 Incomplete/invalid Work Status Report. Start: 07/01/2008 N505 Alert: This response includes only services that could be estimated in real time. No estimate will be provided for the services that could not be estimated in real time. Start: 11/01/2008 N506 Alert: This is an estimate of the member’s liability based on the information available at the time the estimate was processed. Actual coverage and member liability amounts will be determined when the claim is processed. This is not a pre-authorization or a guarantee of payment. Start: 11/01/2008 N507 Plan distance requirements have not been met. Start: 11/01/2008 N508 Alert: This real time claim adjudication response represents the member responsibility to the provider for services reported. The member will receive an Explanation of Benefits electronically or in the mail. Contact the insurer if there are any questions. Start: 11/01/2008 N509 Alert: A current inquiry shows the member’s Consumer Spending Account contains sufficient funds to cover the member liability for this claim/service. Actual payment from the Consumer Spending Account will depend on the availability of funds and determination of eligible services at the time of payment processing. Start: 11/01/2008 N510 Alert: A current inquiry shows the member’s Consumer Spending Account does not contain sufficient funds to cover the member's liability for this claim/service. Actual payment from the Consumer Spending Account will depend on the availability of funds and determination of eligible services at the time of payment processing. Start: 11/01/2008 N511 Alert: Information on the availability of Consumer Spending Account funds to cover the member liability on this claim/service is not available at this time. Start: 11/01/2008 N512 Alert: This is the initial remit of a non-NCPDP claim originally submitted real-time without change to the adjudication. Start: 11/01/2008 N513 Alert: This is the initial remit of a non-NCPDP claim originally submitted real-time with a change to the adjudication. Start: 11/01/2008 N514 Consult plan benefit documents/guidelines for information about restrictions for this service. Start: 11/01/2008 | Stop: 01/01/2011 Notes: Consider using N130 Provider Manual 2013 285 N515 Alert: Submit this claim to the patient's other insurer for potential payment of supplemental benefits. We did not forward the claim information. (use N387 instead) Start: 11/01/2008 | Stop: 10/01/2009 N516 Records indicate a mismatch between the submitted NPI and EIN. Start: 03/01/2009 N517 Resubmit a new claim with the requested information. Start: 03/01/2009 N518 No separate payment for accessories when furnished for use with oxygen equipment. Start: 03/01/2009 N519 Invalid combination of HCPCS modifiers. Start: 07/01/2009 N520 Alert: Payment made from a Consumer Spending Account. Start: 07/01/2009 N521 Mismatch between the submitted provider information and the provider information stored in our system. Start: 11/01/2009 N522 Duplicate of a claim processed, or to be processed, as a crossover claim. Start: 11/01/2009 | Last Modified: 03/01/2010 N523 The limitation on outlier payments defined by this payer for this service period has been met. The outlier payment otherwise applicable to this claim has not been paid. Start: 03/01/2010 N524 Based on policy this payment constitutes payment in full. Start: 03/01/2010 N525 These services are not covered when performed within the global period of another service. Start: 03/01/2010 N526 Not qualified for recovery based on employer size. Start: 03/01/2010 N527 We processed this claim as the primary payer prior to receiving the recovery demand. Start: 03/01/2010 N528 Patient is entitled to benefits for Institutional Services only. Start: 03/01/2010 | Last Modified: 07/01/2010 Notes: (Modified 7/1/10) N529 Patient is entitled to benefits for Professional Services only. Start: 03/01/2010 | Last Modified: 07/01/2010 Notes: (Modified 7/1/10) N530 Not Qualified for Recovery based on enrollment information. Start: 03/01/2010 | Last Modified: 07/01/2010 Notes: (Modified 7/1/10) N531 Not qualified for recovery based on direct payment of premium. Start: 03/01/2010 N532 Not qualified for recovery based on disability and working status. Start: 03/01/2010 Provider Manual 2013 286 N533 Services performed in an Indian Health Services facility under a self-insured tribal Group Health Plan. Start: 07/01/2010 N534 This is an individual policy, the employer does not participate in plan sponsorship. Start: 07/01/2010 N535 Payment is adjusted when procedure is performed in this place of service based on the submitted procedure code and place of service. Start: 07/01/2010 N536 We are not changing the prior payer's determination of patient responsibility, which you may collect, as this service is not covered by us. Start: 07/01/2010 N537 We have examined claims history and no records of the services have been found. Start: 07/01/2010 N538 A facility is responsible for payment to outside providers who furnish these services/supplies/drugs to its patients/residents. Start: 07/01/2010 N539 Alert: We processed appeals/waiver requests on your behalf and that request has been denied. Start: 07/01/2010 N540 Payment adjusted based on the interrupted stay policy. Start: 11/01/2010 N541 Mismatch between the submitted insurance type code and the information stored in our system. Start: 11/01/2010 N542 Missing income verification. Start: 03/08/2011 N543 Incomplete/invalid income verification Start: 03/08/2011 N544 Alert: Although this was paid, you have billed with a referring/ordering provider that does not match our system record. Unless, corrected, this will not be paid in the future. Start: 07/01/2011 N545 Payment reduced based on status as an unsuccessful prescriber per the Electronic Prescribing (eRx) Incentive Program. Start: 07/01/2011 N546 Payment represents a previous reduction based on the Electronic Prescribing (eRx) Incentive Program. Start: 07/01/2011 N547 A refund request (Frequency Type Code 8) was processed previously. Start: 03/06/2012 N548 Alert: Patient's calendar year deductible has been met. Start: 03/06/2012 N549 Alert: Patient's calendar year out-of-pocket maximum has been met. Start: 03/06/2012 Provider Manual 2013 287 N550 Alert: You have not responded to requests to revalidate your provider/supplier enrollment information. Your failure to revalidate your enrollment information will result in a payment hold in the near future. Start: 03/06/2012 N551 Payment adjusted based on the Ambulatory Surgical Center (ASC) Quality Reporting Program. Start: 03/06/2012 N552 Payment adjusted to reverse a previous withhold/bonus amount. Start: 03/06/2012 N553 Payment adjusted based on a Low Income Subsidy (LIS) retroactive coverage or status change. Start: 03/06/2012 | Stop: 11/01/2012 N554 Missing/Incomplete/Invalid Family Planning Indicator Start: 07/01/2012 N555 Missing medication list. Start: 07/01/2012 N556 Incomplete/invalid medication list. Start: 07/01/2012 N557 This claim/service is not payable under our service area. The claim must be filed to the Payer/Plan in whose service area the specimen was collected. Start: 07/01/2012 N558 This claim/service is not payable under our service area. The claim must be filed to the Payer/Plan in whose service area the equipment was received. Start: 07/01/2012 N559 This claim/service is not payable under our service area. The claim must be filed to the Payer/Plan in whose service area the Ordering Physician is located. Start: 07/01/2012 N560 The pilot program requires an interim or final claim within 60 days of the Notice of Admission. A claim was not received. Start: 11/01/2012 N561 The bundled claim originally submitted for this episode of care includes related readmissions. You may resubmit the original claim to receive a corrected payment based on this readmission. Start: 11/01/2012 N562 The provider number of your incoming claim does not match the provider number on the processed Notice of Admission (NOA) for this bundled payment. Start: 11/01/2012 N563 Missing required provider/supplier issuance of advance patient notice of non-coverage. The patient is not liable for payment for this service. Start: 11/01/2012 Notes: Related to M39 N564 Patient did not meet the inclusion criteria for the demonstration project or pilot program. Start: 11/01/2012 N565 Alert: This non-payable reporting code requires a modifier. Future claims containing this non-payable reporting code must include an appropriate modifier for the claim to be processed. Provider Manual 2013 288 Start: 11/01/2012 | Last Modified: 03/01/2013 Notes: (Modified 3/1/13) N566 Alert: This procedure code requires functional reporting. Future claims containing this procedure code must include an applicable non-payable code and appropriate modifiers for the claim to be processed. Start: 11/01/2012 N567 Not covered when considered preventative. Start: 03/01/2013 N568 Alert: Initial payment based on the Notice of Admission (NOA) under the Bundled Payment Model IV initiative. Start: 03/01/2013 N569 Not covered when performed for the reported diagnosis. Start: 03/01/2013 N570 Missing/incomplete/invalid credentialing data Start: 03/01/2013 N571 Alert: Payment will be issued quarterly by another payer/contractor. Start: 03/01/2013 N572 This procedure is not payable unless non-payable reporting codes and appropriate modifiers are submitted. Start: 03/01/2013 N573 Alert: You have been overpaid and must refund the overpayment. The refund will be requested separately by another payer/contractor. Start: 03/01/2013 Provider Manual 2013 289 CLAIM ADJUSTMENT REASON CODES 1 Deductible Amount Start: 01/01/1995 2 Coinsurance Amount Start: 01/01/1995 3 Co-payment Amount Start: 01/01/1995 4 The procedure code is inconsistent with the modifier used or a required modifier is missing. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 5 The procedure code/bill type is inconsistent with the place of service. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 6 The procedure/revenue code is inconsistent with the patient's age. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 7 The procedure/revenue code is inconsistent with the patient's gender. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 8 The procedure code is inconsistent with the provider type/specialty (taxonomy). Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 9 The diagnosis is inconsistent with the patient's age. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 10 The diagnosis is inconsistent with the patient's gender. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 11 The diagnosis is inconsistent with the procedure. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 12 The diagnosis is inconsistent with the provider type. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 13 The date of death precedes the date of service. Start: 01/01/1995 14 The date of birth follows the date of service. Start: 01/01/1995 15 The authorization number is missing, invalid, or does not apply to the billed services or provider. Start: 01/01/1995 | Last Modified: 09/30/2007 16 Claim/service lacks information which is needed for adjudication. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) This change effective 11/1/2013: Claim/service lacks information or has submission/billing error(s) which is needed for adjudication. Do not use this code for claims attachment(s). At least one Remark Code must be provided (may be comprised of ei- Provider Manual 2013 290 ther the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 01/20/2013 17 Requested information was not provided or was insufficient/incomplete. At least one Remark Code must be provided (may be comprised of either the Remittance Advice Remark Code or NCPDP Reject Reason Code.) Start: 01/01/1995 | Last Modified: 09/21/2008 | Stop: 07/01/2009 18 Exact duplicate claim/service (Use only with Group Code OA) Start: 01/01/1995 | Last Modified: 01/20/2013 19 This is a work-related injury/illness and thus the liability of the Worker's Compensation Carrier. Start: 01/01/1995 | Last Modified: 09/30/2007 20 This injury/illness is covered by the liability carrier. Start: 01/01/1995 | Last Modified: 09/30/2007 21 This injury/illness is the liability of the no-fault carrier. Start: 01/01/1995 | Last Modified: 09/30/2007 22 This care may be covered by another payer per coordination of benefits. Start: 01/01/1995 | Last Modified: 09/30/2007 23 The impact of prior payer(s) adjudication including payments and/or adjustments. (Use only with Group Code OA) Start: 01/01/1995 | Last Modified: 09/30/2012 24 Charges are covered under a capitation agreement/managed care plan. Start: 01/01/1995 | Last Modified: 09/30/2007 25 Payment denied. Your Stop loss deductible has not been met. Start: 01/01/1995 | Stop: 04/01/2008 26 Expenses incurred prior to coverage. Start: 01/01/1995 27 Expenses incurred after coverage terminated. Start: 01/01/1995 28 Coverage not in effect at the time the service was provided. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Redundant to codes 26&27. 29 The time limit for filing has expired. Start: 01/01/1995 30 Payment adjusted because the patient has not met the required eligibility, spend down, waiting, or residency requirements. Start: 01/01/1995 | Stop: 02/01/2006 31 Patient cannot be identified as our insured. Start: 01/01/1995 | Last Modified: 09/30/2007 32 Our records indicate that this dependent is not an eligible dependent as defined. Start: 01/01/1995 33 Insured has no dependent coverage. Start: 01/01/1995 | Last Modified: 09/30/2007 34 Insured has no coverage for newborns. Provider Manual 2013 291 Start: 01/01/1995 | Last Modified: 09/30/2007 35 Lifetime benefit maximum has been reached. Start: 01/01/1995 | Last Modified: 10/31/2002 36 Balance does not exceed co-payment amount. Start: 01/01/1995 | Stop: 10/16/2003 37 Balance does not exceed deductible. Start: 01/01/1995 | Stop: 10/16/2003 38 Services not provided or authorized by designated (network/primary care) providers. Start: 01/01/1995 | Last Modified: 06/30/2003 | Stop: 01/01/2013 39 Services denied at the time authorization/pre-certification was requested. Start: 01/01/1995 40 Charges do not meet qualifications for emergent/urgent care. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 41 Discount agreed to in Preferred Provider contract. Start: 01/01/1995 | Stop: 10/16/2003 42 Charges exceed our fee schedule or maximum allowable amount. (Use CARC 45) Start: 01/01/1995 | Last Modified: 10/31/2006 | Stop: 06/01/2007 43 Gramm-Rudman reduction. Start: 01/01/1995 | Stop: 07/01/2006 44 Prompt-pay discount. Start: 01/01/1995 45 Charge exceeds fee schedule/maximum allowable or contracted/legislated fee arrangement. (Use Group Codes PR or CO depending upon liability). This change effective 7/1/2013: Charge exceeds fee schedule/maximum allowable or contracted/legislated fee arrangement. (Use only with Group Codes PR or CO depending upon liability) Start: 01/01/1995 | Last Modified: 09/30/2012 46 This (these) service(s) is (are) not covered. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 96. 47 This (these) diagnosis(es) is (are) not covered, missing, or are invalid. Start: 01/01/1995 | Stop: 02/01/2006 48 This (these) procedure(s) is (are) not covered. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 96. 49 These are non-covered services because this is a routine exam or screening procedure done in conjunction with a routine exam. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. This change effective 11/1/2013: This is a non-covered service because it is a routine/preventive exam or a diagnostic/screening procedure done in conjunction with a routine/preventive exam. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 01/20/2013 50 These are non-covered services because this is not deemed a 'medical necessity' by the payer. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 Provider Manual 2013 292 51 These are non-covered services because this is a pre-existing condition. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 52 The referring/prescribing/rendering provider is not eligible to refer/prescribe/order/perform the service billed. Start: 01/01/1995 | Stop: 02/01/2006 53 Services by an immediate relative or a member of the same household are not covered. Start: 01/01/1995 54 Multiple physicians/assistants are not covered in this case. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 55 Procedure/treatment is deemed experimental/investigational by the payer. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 56 Procedure/treatment has not been deemed 'proven to be effective' by the payer. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 57 Payment denied/reduced because the payer deems the information submitted does not support this level of service, this many services, this length of service, this dosage, or this day's supply. Start: 01/01/1995 | Stop: 06/30/2007 Notes: Split into codes 150, 151, 152, 153 and 154. 58 Treatment was deemed by the payer to have been rendered in an inappropriate or invalid place of service. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 59 Processed based on multiple or concurrent procedure rules. (For example multiple surgery or diagnostic imaging, concurrent anesthesia.) Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 60 Charges for outpatient services are not covered when performed within a period of time prior to or after inpatient services. Start: 01/01/1995 | Last Modified: 06/01/2008 61 Penalty for failure to obtain second surgical opinion. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 62 Payment denied/reduced for absence of, or exceeded, pre-certification/authorization. Start: 01/01/1995 | Last Modified: 10/31/2006 | Stop: 04/01/2007 63 Correction to a prior claim. Start: 01/01/1995 | Stop: 10/16/2003 64 Denial reversed per Medical Review. Start: 01/01/1995 | Stop: 10/16/2003 65 Procedure code was incorrect. This payment reflects the correct code. Start: 01/01/1995 | Stop: 10/16/2003 66 Blood Deductible. Start: 01/01/1995 67 Lifetime reserve days. (Handled in QTY, QTY01=LA) Provider Manual 2013 293 Start: 01/01/1995 | Stop: 10/16/2003 68 DRG weight. (Handled in CLP12) Start: 01/01/1995 | Stop: 10/16/2003 69 Day outlier amount. Start: 01/01/1995 70 Cost outlier - Adjustment to compensate for additional costs. Start: 01/01/1995 | Last Modified: 06/30/2001 71 Primary Payer amount. Start: 01/01/1995 | Stop: 06/30/2000 Notes: Use code 23. 72 Coinsurance day. (Handled in QTY, QTY01=CD) Start: 01/01/1995 | Stop: 10/16/2003 73 Administrative days. Start: 01/01/1995 | Stop: 10/16/2003 74 Indirect Medical Education Adjustment. Start: 01/01/1995 75 Direct Medical Education Adjustment. Start: 01/01/1995 76 Disproportionate Share Adjustment. Start: 01/01/1995 77 Covered days. (Handled in QTY, QTY01=CA) Start: 01/01/1995 | Stop: 10/16/2003 78 Non-Covered days/Room charge adjustment. Start: 01/01/1995 79 Cost Report days. (Handled in MIA15) Start: 01/01/1995 | Stop: 10/16/2003 80 Outlier days. (Handled in QTY, QTY01=OU) Start: 01/01/1995 | Stop: 10/16/2003 81 Discharges. Start: 01/01/1995 | Stop: 10/16/2003 82 PIP days. Start: 01/01/1995 | Stop: 10/16/2003 83 Total visits. Start: 01/01/1995 | Stop: 10/16/2003 84 Capital Adjustment. (Handled in MIA) Start: 01/01/1995 | Stop: 10/16/2003 85 Patient Interest Adjustment (Use Only Group code PR) Start: 01/01/1995 | Last Modified: 07/09/2007 Notes: Only use when the payment of interest is the responsibility of the patient. 86 Statutory Adjustment. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Duplicative of code 45. Provider Manual 2013 294 87 Transfer amount. Start: 01/01/1995 | Last Modified: 09/20/2009 | Stop: 01/01/2012 88 Adjustment amount represents collection against receivable created in prior overpayment. Start: 01/01/1995 | Stop: 06/30/2007 89 Professional fees removed from charges. Start: 01/01/1995 90 Ingredient cost adjustment. Note: To be used for pharmaceuticals only. Start: 01/01/1995 | Last Modified: 07/01/2009 91 Dispensing fee adjustment. Start: 01/01/1995 92 Claim Paid in full. Start: 01/01/1995 | Stop: 10/16/2003 93 No Claim level Adjustments. Start: 01/01/1995 | Stop: 10/16/2003 Notes: As of 004010, CAS at the claim level is optional. 94 Processed in Excess of charges. Start: 01/01/1995 95 Plan procedures not followed. Start: 01/01/1995 | Last Modified: 09/30/2007 96 Non-covered charge(s). At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 97 The benefit for this service is included in the payment/allowance for another service/procedure that has already been adjudicated. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 98 The hospital must file the Medicare claim for this inpatient non-physician service. Start: 01/01/1995 | Stop: 10/16/2003 99 Medicare Secondary Payer Adjustment Amount. Start: 01/01/1995 | Stop: 10/16/2003 100 Payment made to patient/insured/responsible party/employer. Start: 01/01/1995 | Last Modified: 01/27/2008 101 Predetermination: anticipated payment upon completion of services or claim adjudication. Start: 01/01/1995 | Last Modified: 02/28/1999 102 Major Medical Adjustment. Start: 01/01/1995 103 Provider promotional discount (e.g., Senior citizen discount). Start: 01/01/1995 | Last Modified: 06/30/2001 104 Managed care withholding. Start: 01/01/1995 105 Tax withholding. Start: 01/01/1995 106 Patient payment option/election not in effect. Provider Manual 2013 295 Start: 01/01/1995 107 The related or qualifying claim/service was not identified on this claim. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 108 Rent/purchase guidelines were not met. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 109 Claim/service not covered by this payer/contractor. You must send the claim/service to the correct payer/contractor. Start: 01/01/1995 | Last Modified: 01/29/2012 110 Billing date predates service date. Start: 01/01/1995 111 Not covered unless the provider accepts assignment. Start: 01/01/1995 112 Service not furnished directly to the patient and/or not documented. Start: 01/01/1995 | Last Modified: 09/30/2007 113 Payment denied because service/procedure was provided outside the United States or as a result of war. Start: 01/01/1995 | Last Modified: 02/28/2001 | Stop: 06/30/2007 Notes: Use Codes 157, 158 or 159. 114 Procedure/product not approved by the Food and Drug Administration. Start: 01/01/1995 115 Procedure postponed, canceled, or delayed. Start: 01/01/1995 | Last Modified: 09/30/2007 116 The advance indemnification notice signed by the patient did not comply with requirements. Start: 01/01/1995 | Last Modified: 09/30/2007 117 Transportation is only covered to the closest facility that can provide the necessary care. Start: 01/01/1995 | Last Modified: 09/30/2007 118 ESRD network support adjustment. Start: 01/01/1995 | Last Modified: 09/30/2007 119 Benefit maximum for this time period or occurrence has been reached. Start: 01/01/1995 | Last Modified: 02/29/2004 120 Patient is covered by a managed care plan. Start: 01/01/1995 | Stop: 06/30/2007 Notes: Use code 24. 121 Indemnification adjustment - compensation for outstanding member responsibility. Start: 01/01/1995 | Last Modified: 09/30/2007 122 Psychiatric reduction. Start: 01/01/1995 123 Payer refund due to overpayment. Start: 01/01/1995 | Stop: 06/30/2007 Notes: Refer to implementation guide for proper handling of reversals. 124 Payer refund amount - not our patient. Start: 01/01/1995 | Last Modified: 06/30/1999 | Stop: 06/30/2007 Provider Manual 2013 296 Notes: Refer to implementation guide for proper handling of reversals. 125 Submission/billing error(s). At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 01/01/1995 | Last Modified: 09/20/2009 | Stop: 11/01/2013 126 Deductible -- Major Medical Start: 02/28/1997 | Last Modified: 09/30/2007 | Stop: 04/01/2008 Notes: Use Group Code PR and code 1. 127 Coinsurance -- Major Medical Start: 02/28/1997 | Last Modified: 09/30/2007 | Stop: 04/01/2008 Notes: Use Group Code PR and code 2. 128 Newborn's services are covered in the mother's Allowance. Start: 02/28/1997 129 Prior processing information appears incorrect. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 02/28/1997 | Last Modified: 01/30/2011 130 Claim submission fee. Start: 02/28/1997 | Last Modified: 06/30/2001 131 Claim specific negotiated discount. Start: 02/28/1997 132 Prearranged demonstration project adjustment. Start: 02/28/1997 133 The disposition of the claim/service is pending further review. (Use only with Group Code OA) Start: 02/28/1997 | Last Modified: 01/20/2013 134 Technical fees removed from charges. Start: 10/31/1998 135 Interim bills cannot be processed. Start: 10/31/1998 | Last Modified: 09/30/2007 136 Failure to follow prior payer's coverage rules. (Use Group Code OA). This change effective 7/1/2013: Failure to follow prior payer's coverage rules. (Use only with Group Code OA) Start: 10/31/1998 | Last Modified: 09/30/2012 137 Regulatory Surcharges, Assessments, Allowances or Health Related Taxes. Start: 02/28/1999 | Last Modified: 09/30/2007 138 Appeal procedures not followed or time limits not met. Start: 06/30/1999 | Last Modified: 09/30/2007 139 Contracted funding agreement - Subscriber is employed by the provider of services. Start: 06/30/1999 140 Patient/Insured health identification number and name do not match. Start: 06/30/1999 141 Claim spans eligible and ineligible periods of coverage. Start: 06/30/1999 | Last Modified: 09/30/2007 | Stop: 07/01/2012 142 Monthly Medicaid patient liability amount. Start: 06/30/2000 | Last Modified: 09/30/2007 143 Portion of payment deferred. Provider Manual 2013 297 Start: 02/28/2001 144 Incentive adjustment, e.g. preferred product/service. Start: 06/30/2001 145 Premium payment withholding Start: 06/30/2002 | Last Modified: 09/30/2007 | Stop: 04/01/2008 Notes: Use Group Code CO and code 45. 146 Diagnosis was invalid for the date(s) of service reported. Start: 06/30/2002 | Last Modified: 09/30/2007 147 Provider contracted/negotiated rate expired or not on file. Start: 06/30/2002 148 Information from another provider was not provided or was insufficient/incomplete. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 06/30/2002 | Last Modified: 09/20/2009 149 Lifetime benefit maximum has been reached for this service/benefit category. Start: 10/31/2002 150 Payer deems the information submitted does not support this level of service. Start: 10/31/2002 | Last Modified: 09/30/2007 151 Payment adjusted because the payer deems the information submitted does not support this many/frequency of services. Start: 10/31/2002 | Last Modified: 01/27/2008 152 Payer deems the information submitted does not support this length of service. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 10/31/2002 | Last Modified: 09/20/2009 153 Payer deems the information submitted does not support this dosage. Start: 10/31/2002 | Last Modified: 09/30/2007 154 Payer deems the information submitted does not support this day's supply. Start: 10/31/2002 | Last Modified: 09/30/2007 155 Patient refused the service/procedure. Start: 06/30/2003 | Last Modified: 09/30/2007 156 Flexible spending account payments. Note: Use code 187. Start: 09/30/2003 | Last Modified: 01/25/2009 | Stop: 10/01/2009 157 Service/procedure was provided as a result of an act of war. Start: 09/30/2003 | Last Modified: 09/30/2007 158 Service/procedure was provided outside of the United States. Start: 09/30/2003 | Last Modified: 09/30/2007 159 Service/procedure was provided as a result of terrorism. Start: 09/30/2003 | Last Modified: 09/30/2007 160 Injury/illness was the result of an activity that is benefit exclusion. Start: 09/30/2003 | Last Modified: 09/30/2007 161 Provider performance bonus Start: 02/29/2004 162 State-mandated Requirement for Property and Casualty, see Claim Payment Remarks Code for specific explanation. Provider Manual 2013 298 Start: 02/29/2004 163 Attachment referenced on the claim was not received. Start: 06/30/2004 | Last Modified: 09/30/2007 164 Attachment referenced on the claim was not received in a timely fashion. Start: 06/30/2004 | Last Modified: 09/30/2007 165 Referral absent or exceeded. Start: 10/31/2004 | Last Modified: 09/30/2007 166 These services were submitted after this payers responsibility for processing claims under this plan ended. Start: 02/28/2005 167 This (these) diagnosis(es) is (are) not covered. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/30/2005 | Last Modified: 09/20/2009 168 Service(s) have been considered under the patient's medical plan. Benefits are not available under this dental plan. Start: 06/30/2005 | Last Modified: 09/30/2007 169 Alternate benefit has been provided. Start: 06/30/2005 | Last Modified: 09/30/2007 170 Payment is denied when performed/billed by this type of provider. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/30/2005 | Last Modified: 09/20/2009 171 Payment is denied when performed/billed by this type of provider in this type of facility. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/30/2005 | Last Modified: 09/20/2009 172 Payment is adjusted when performed/billed by a provider of this specialty. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/30/2005 | Last Modified: 09/20/2009 173 Service was not prescribed by a physician. This change effective 7/1/2013: Service/equipment was not prescribed by a physician. Start: 06/30/2005 | Last Modified: 09/30/2012 174 Service was not prescribed prior to delivery. Start: 06/30/2005 | Last Modified: 09/30/2007 175 Prescription is incomplete. Start: 06/30/2005 | Last Modified: 09/30/2007 176 Prescription is not current. Start: 06/30/2005 | Last Modified: 09/30/2007 177 Patient has not met the required eligibility requirements. Start: 06/30/2005 | Last Modified: 09/30/2007 178 Patient has not met the required spend down requirements. Start: 06/30/2005 | Last Modified: 09/30/2007 179 Patient has not met the required waiting requirements. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/30/2005 | Last Modified: 09/20/2009 180 Patient has not met the required residency requirements. Start: 06/30/2005 | Last Modified: 09/30/2007 Provider Manual 2013 299 181 Procedure code was invalid on the date of service. Start: 06/30/2005 | Last Modified: 09/30/2007 182 Procedure modifier was invalid on the date of service. Start: 06/30/2005 | Last Modified: 09/30/2007 183 The referring provider is not eligible to refer the service billed. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/30/2005 | Last Modified: 09/20/2009 184 The prescribing/ordering provider is not eligible to prescribe/order the service billed. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/30/2005 | Last Modified: 09/20/2009 185 The rendering provider is not eligible to perform the service billed. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/30/2005 | Last Modified: 09/20/2009 186 Level of care change adjustment. Start: 06/30/2005 | Last Modified: 09/30/2007 187 Consumer Spending Account payments (includes but is not limited to Flexible Spending Account, Health Savings Account, Health Reimbursement Account, etc.) Start: 06/30/2005 | Last Modified: 01/25/2009 188 This product/procedure is only covered when used according to FDA recommendations. Start: 06/30/2005 189 'Not otherwise classified' or 'unlisted' procedure code (CPT/HCPCS) was billed when there is a specific procedure code for this procedure/service Start: 06/30/2005 190 Payment is included in the allowance for a Skilled Nursing Facility (SNF) qualified stay. Start: 10/31/2005 191 Not a work related injury/illness and thus not the liability of the workers' compensation carrier Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segments (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF) Start: 10/31/2005 | Last Modified: 10/17/2010 192 Nonstandard adjustment code from paper remittance. Note: This code is to be used by providers/payers providing Coordination of Benefits information to another payer in the 837 transaction only. This code is only used when the non-standard code cannot be reasonably mapped to an existing Claims Adjustment Reason Code, specifically Deductible, Coinsurance and Co-payment. Start: 10/31/2005 | Last Modified: 09/30/2007 193 Original payment decision is being maintained. Upon review, it was determined that this claim was processed properly. Start: 02/28/2006 | Last Modified: 01/27/2008 194 Anesthesia performed by the operating physician, the assistant surgeon or the attending physician. Start: 02/28/2006 | Last Modified: 09/30/2007 195 Refund issued to an erroneous priority payer for this claim/service. Start: 02/28/2006 | Last Modified: 09/30/2007 196 Claim/service denied based on prior payer's coverage determination. Start: 06/30/2006 | Stop: 02/01/2007 Notes: Use code 136. Provider Manual 2013 300 197 Precertification/authorization/notification absent. Start: 10/31/2006 | Last Modified: 09/30/2007 198 Precertification/authorization exceeded. Start: 10/31/2006 | Last Modified: 09/30/2007 199 Revenue code and Procedure code do not match. Start: 10/31/2006 200 Expenses incurred during lapse in coverage Start: 10/31/2006 201 Workers' Compensation case settled. Patient is responsible for amount of this claim/service through WC 'Medicare set aside arrangement' or other agreement. (Use group code PR). This change effective 7/1/2013: Workers Compensation case settled. Patient is responsible for amount of this claim/service through WC 'Medicare set aside arrangement' or other agreement. (Use only with Group Code PR) Start: 10/31/2006 | Last Modified: 09/30/2012 202 Non-covered personal comfort or convenience services. Start: 02/28/2007 | Last Modified: 09/30/2007 203 Discontinued or reduced service. Start: 02/28/2007 | Last Modified: 09/30/2007 204 This service/equipment/drug is not covered under the patient’s current benefit plan Start: 02/28/2007 205 Pharmacy discount card processing fee Start: 07/09/2007 206 National Provider Identifier - missing. Start: 07/09/2007 | Last Modified: 09/30/2007 207 National Provider identifier - Invalid format Start: 07/09/2007 | Last Modified: 06/01/2008 208 National Provider Identifier - Not matched. Start: 07/09/2007 | Last Modified: 09/30/2007 209 Per regulatory or other agreement. The provider cannot collect this amount from the patient. However, this amount may be billed to subsequent payer. Refund to patient if collected. (Use Group code OA) This change effective 7/1/2013: Per regulatory or other agreement. The provider cannot collect this amount from the patient. However, this amount may be billed to subsequent payer. Refund to patient if collected. (Use only with Group code OA) Start: 07/09/2007 | Last Modified: 09/30/2012 210 Payment adjusted because pre-certification/authorization not received in a timely fashion Start: 07/09/2007 211 National Drug Codes (NDC) not eligible for rebate, are not covered. Start: 07/09/2007 212 Administrative surcharges are not covered Start: 11/05/2007 213 Non-compliance with the physician self-referral prohibition legislation or payer policy. Start: 01/27/2008 214 Workers' Compensation claim adjudicated as non-compensable. This Payer not liable for claim or service/treatment. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segment (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Seg- Provider Manual 2013 301 ment (loop 2110 Service Payment information REF). To be used for Workers' Compensation only Start: 01/27/2008 | Last Modified: 10/17/2010 215 Based on subrogation of a third party settlement Start: 01/27/2008 216 Based on the findings of a review organization Start: 01/27/2008 217 Based on payer reasonable and customary fees. No maximum allowable defined by legislated fee arrangement. (Note: To be used for Property and Casualty only) Start: 01/27/2008 | Last Modified: 09/30/2012 218 Based on entitlement to benefits. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segment (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). To be used for Workers' Compensation only Start: 01/27/2008 | Last Modified: 10/17/2010 219 Based on extent of injury. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segment (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). Start: 01/27/2008 | Last Modified: 10/17/2010 220 The applicable fee schedule/fee database does not contain the billed code. Please resubmit a bill with the appropriate fee schedule/fee database code(s) that best describe the service(s) provided and supporting documentation if required. (Note: To be used for Property and Casualty only) Start: 01/27/2008 | Last Modified: 09/30/2012 221 Workers' Compensation claim is under investigation. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segment (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). This change effective 7/1/2013: Claim is under investigation. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segment (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). (Note: To be used by Property & Casualty only) Start: 01/27/2008 | Last Modified: 09/30/2012 222 Exceeds the contracted maximum number of hours/days/units by this provider for this period. This is not patient specific. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/01/2008 | Last Modified: 09/20/2009 223 Adjustment code for mandated federal, state or local law/regulation that is not already covered by another code and is mandated before a new code can be created. Start: 06/01/2008 SEQUESTRATION ONLY - IS DONE BY THE EZCAP SYSTEM AUTOMATICALLY 224 Patient identification compromised by identity theft. Identity verification required for processing this and future claims. Start: 06/01/2008 225 Penalty or Interest Payment by Payer (Only used for plan to plan encounter reporting within the 837) Start: 06/01/2008 Provider Manual 2013 302 226 Information requested from the Billing/Rendering Provider was not provided or was insufficient/incomplete. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) This change effective 7/1/2013: Information requested from the Billing/Rendering Provider was not provided or not provided timely or was insufficient/incomplete. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 09/21/2008 | Last Modified: 09/30/2012 227 Information requested from the patient/insured/responsible party was not provided or was insufficient/incomplete. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 09/21/2008 | Last Modified: 09/20/2009 228 Denied for failure of this provider, another provider or the subscriber to supply requested information to a previous payer for their adjudication Start: 09/21/2008 229 Partial charge amount not considered by Medicare due to the initial claim Type of Bill being 12X. Note: This code can only be used in the 837 transaction to convey Coordination of Benefits information when the secondary payer's cost avoidance policy allows providers to bypass claim submission to a prior payer. Use Group Code PR. This change effective 7/1/2013: Partial charge amount not considered by Medicare due to the initial claim Type of Bill being 12X. Note: This code can only be used in the 837 transaction to convey Coordination of Benefits information when the secondary payer's cost avoidance policy allows providers to bypass claim submission to a prior payer. (Use only with Group Code PR) Start: 01/25/2009 | Last Modified: 09/30/2012 230 No available or correlating CPT/HCPCS code to describe this service. Note: Used only by Property and Casualty. Start: 01/25/2009 231 Mutually exclusive procedures cannot be done in the same day/setting. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 07/01/2009 | Last Modified: 09/20/2009 232 Institutional Transfer Amount. Note - Applies to institutional claims only and explains the DRG amount difference when the patient care crosses multiple institutions. Start: 11/01/2009 233 Services/charges related to the treatment of a hospital-acquired condition or preventable medical error. Start: 01/24/2010 234 This procedure is not paid separately. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 01/24/2010 235 Sales Tax Start: 06/06/2010 236 This procedure or procedure/modifier combination is not compatible with another procedure or procedure/modifier combination provided on the same day according to the National Correct Coding Initiative. This change effective 7/1/2013: This procedure or procedure/modifier combination is not compatible with another procedure or procedure/modifier combination provided on the same day according to the National Correct Coding Initiative or workers compensation state regulations/ fee schedule requirements. Start: 01/30/2011 | Last Modified: 09/30/2012 237 Legislated/Regulatory Penalty. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 06/05/2011 238 Claim spans eligible and ineligible periods of coverage, this is the reduction for the ineligible period (use Group Code PR). This change effective 7/1/2013: Claim spans eligible and ineligible pe- Provider Manual 2013 303 riods of coverage, this is the reduction for the ineligible period. (Use only with Group Code PR) Start: 03/01/2012 | Last Modified: 09/30/2012 239 Claim spans eligible and ineligible periods of coverage. Rebill separate claims. Start: 03/01/2012 | Last Modified: 01/29/2012 240 The diagnosis is inconsistent with the patient's birth weight. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 06/03/2012 241 Low Income Subsidy (LIS) Co-payment Amount Start: 06/03/2012 242 Services not provided by network/primary care providers. Start: 06/03/2012 243 Services not authorized by network/primary care providers. Start: 06/03/2012 244 Payment reduced to zero due to litigation. Additional information will be sent following the conclusion of litigation. To be used for Property & Casualty only. Start: 09/30/2012 245 Provider performance program withhold. Start: 09/30/2012 246 This non-payable code is for required reporting only. Start: 09/30/2012 247 Deductible for Professional service rendered in an Institutional setting and billed on an Institutional claim. Start: 09/30/2012 Notes: For Medicare Bundled Payment use only, under the Patient Protection and Affordable Care Act (PPACA). 248 Coinsurance for Professional service rendered in an Institutional setting and billed on an Institutional claim. Start: 09/30/2012 Notes: For Medicare Bundled Payment use only, under the Patient Protection and Affordable Care Act (PPACA). 249 This claim has been identified as a readmission. (Use only with Group Code CO) Start: 09/30/2012 250 The attachment content received is inconsistent with the expected content. Start: 09/30/2012 251 The attachment content received did not contain the content required to process this claim or service. Start: 09/30/2012 252 An attachment is required to adjudicate this claim/service. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). Start: 09/30/2012 A0 Patient refund amount. Start: 01/01/1995 A1 Claim/Service denied. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 01/01/1995 | Last Modified: 09/20/2009 A2 Contractual adjustment. Start: 01/01/1995 | Last Modified: 02/28/2007 | Stop: 01/01/2008 Provider Manual 2013 304 Notes: Use Code 45 with Group Code 'CO' or use another appropriate specific adjustment code. A3 Medicare Secondary Payer liability met. Start: 01/01/1995 | Stop: 10/16/2003 A4 Medicare Claim PPS Capital Day Outlier Amount. Start: 01/01/1995 | Last Modified: 09/30/2007 | Stop: 04/01/2008 A5 Medicare Claim PPS Capital Cost Outlier Amount. Start: 01/01/1995 A6 Prior hospitalization or 30 day transfer requirement not met. Start: 01/01/1995 A7 Presumptive Payment Adjustment Start: 01/01/1995 A8 Ungroupable DRG. Start: 01/01/1995 | Last Modified: 09/30/2007 B1 Non-covered visits. Start: 01/01/1995 B2 Covered visits. Start: 01/01/1995 | Stop: 10/16/2003 B3 Covered charges. Start: 01/01/1995 | Stop: 10/16/2003 B4 Late filing penalty. Start: 01/01/1995 B5 Coverage/program guidelines were not met or were exceeded. Start: 01/01/1995 | Last Modified: 09/30/2007 B6 This payment is adjusted when performed/billed by this type of provider, by this type of provider in this type of facility, or by a provider of this specialty. Start: 01/01/1995 | Stop: 02/01/2006 B7 This provider was not certified/eligible to be paid for this procedure/service on this date of service. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 B8 Alternative services were available, and should have been utilized. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 B9 Patient is enrolled in a Hospice. Start: 01/01/1995 | Last Modified: 09/30/2007 B10 Allowed amount has been reduced because a component of the basic procedure/test was paid. The beneficiary is not liable for more than the charge limit for the basic procedure/test. Start: 01/01/1995 B11 The claim/service has been transferred to the proper payer/processor for processing. Claim/service not covered by this payer/processor. Start: 01/01/1995 B12 Services not documented in patients' medical records. Start: 01/01/1995 B13 Previously paid. Payment for this claim/service may have been provided in a previous payment. Start: 01/01/1995 Provider Manual 2013 305 B14 Only one visit or consultation per physician per day is covered. Start: 01/01/1995 | Last Modified: 09/30/2007 B15 This service/procedure requires that a qualifying service/procedure be received and covered. The qualifying other service/procedure has not been received/adjudicated. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. Start: 01/01/1995 | Last Modified: 09/20/2009 B16 'New Patient' qualifications were not met. Start: 01/01/1995 | Last Modified: 09/30/2007 B17 Payment adjusted because this service was not prescribed by a physician, not prescribed prior to delivery, the prescription is incomplete, or the prescription is not current. Start: 01/01/1995 | Stop: 02/01/2006 B18 This procedure code and modifier were invalid on the date of service. Start: 01/01/1995 | Last Modified: 09/21/2008 | Stop: 03/01/2009 B19 Claim/service adjusted because of the finding of a Review Organization. Start: 01/01/1995 | Stop: 10/16/2003 B20 Procedure/service was partially or fully furnished by another provider. Start: 01/01/1995 | Last Modified: 09/30/2007 B21 The charges were reduced because the service/care was partially furnished by another physician. Start: 01/01/1995 | Stop: 10/16/2003 B22 This payment is adjusted based on the diagnosis. Start: 01/01/1995 | Last Modified: 02/28/2001 B23 Procedure billed is not authorized per your Clinical Laboratory Improvement Amendment (CLIA) proficiency test. Start: 01/01/1995 | Last Modified: 09/30/2007 D1 Claim/service denied. Level of subluxation is missing or inadequate. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D2 Claim lacks the name, strength, or dosage of the drug furnished. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D3 Claim/service denied because information to indicate if the patient owns the equipment that requires the part or supply was missing. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D4 Claim/service does not indicate the period of time for which this will be needed. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D5 Claim/service denied. Claim lacks individual lab codes included in the test. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D6 Claim/service denied. Claim did not include patient's medical record for the service. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D7 Claim/service denied. Claim lacks date of patient's most recent physician visit. Provider Manual 2013 306 Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D8 Claim/service denied. Claim lacks indicator that 'x-ray is available for review.' Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D9 Claim/service denied. Claim lacks invoice or statement certifying the actual cost of the lens, less discounts or the type of intraocular lens used. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 16 and remark codes if necessary. D10 Claim/service denied. Completed physician financial relationship form not on file. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 17. D11 Claim lacks completed pacemaker registration form. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 17. D12 Claim/service denied. Claim does not identify who performed the purchased diagnostic test or the amount you were charged for the test. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 17. D13 Claim/service denied. Performed by a facility/supplier in which the ordering/referring physician has a financial interest. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 17. D14 Claim lacks indication that plan of treatment is on file. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 17. D15 Claim lacks indication that service was supervised or evaluated by a physician. Start: 01/01/1995 | Stop: 10/16/2003 Notes: Use code 17. D16 Claim lacks prior payer payment information. Start: 01/01/1995 | Stop: 06/30/2007 Notes: Use code 16 with appropriate claim payment remark code [N4]. D17 Claim/Service has invalid non-covered days. Start: 01/01/1995 | Stop: 06/30/2007 Notes: Use code 16 with appropriate claim payment remark code. D18 Claim/Service has missing diagnosis information. Start: 01/01/1995 | Stop: 06/30/2007 Notes: Use code 16 with appropriate claim payment remark code. D19 Claim/Service lacks Physician/Operative or other supporting documentation Start: 01/01/1995 | Stop: 06/30/2007 Notes: Use code 16 with appropriate claim payment remark code. D20 Claim/Service missing service/product information. Start: 01/01/1995 | Stop: 06/30/2007 Notes: Use code 16 with appropriate claim payment remark code. Provider Manual 2013 307 D21 This (these) diagnosis(es) is (are) missing or are invalid Start: 01/01/1995 | Stop: 06/30/2007 D22 Reimbursement was adjusted for the reasons to be provided in separate correspondence. (Note: To be used for Workers' Compensation only) - Temporary code to be added for timeframe only until 01/01/2009. Another code to be established and/or for 06/2008 meeting for a revised code to replace or strategy to use another existing code Start: 01/27/2008 | Stop: 01/01/2009 D23 This dual eligible patient is covered by Medicare Part D per Medicare Retro-Eligibility. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT.) Start: 11/01/2009 | Stop: 01/01/2012 W1 Workers' compensation jurisdictional fee schedule adjustment. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Class of Contract Code Identification Segment (Loop 2100 Other Claim Related Information REF). If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). Start: 02/29/2000 | Last Modified: 10/17/2010 W2 Payment reduced or denied based on workers' compensation jurisdictional regulations or payment policies, use only if no other code is applicable. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segment (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). To be used for Workers' Compensation only. Start: 10/17/2010 W3 The Benefit for this Service is included in the payment/allowance for another service/procedure that has been performed on the same day. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. For use by Property and Casualty only. Start: 09/30/2012 W4 Workers' Compensation Medical Treatment Guideline Adjustment. Start: 09/30/2012 Y1 Payment denied based on Medical Payments Coverage (MPC) or Personal Injury Protection (PIP) Benefits jurisdictional regulations or payment policies, use only if no other code is applicable. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segment (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). To be used for P&C Auto only. Start: 09/30/2012 Y2 Payment adjusted based on Medical Payments Coverage (MPC) or Personal Injury Protection (PIP) Benefits jurisdictional regulations or payment policies, use only if no other code is applicable. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Insurance Policy Number Segment (Loop 2100 Other Claim Related Information REF qualifier 'IG') for the jurisdictional regulation. If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). To be used for P&C Auto only. Start: 09/30/2012 Y3 Medical Payments Coverage (MPC) or Personal Injury Protection (PIP) Benefits jurisdictional fee schedule adjustment. Note: If adjustment is at the Claim Level, the payer must send and the provider should refer to the 835 Class of Contract Code Identification Segment (Loop 2100 Other Claim Related Information REF). If adjustment is at the Line Level, the payer must send and the provider should refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment information REF). To be used for P&C Auto only. Start: 09/30/2012 Provider Manual 2013 308 VE CODE V1 V10 V100 V101 V102 V103 V104 V105 V106 V107 V108 V109 V11 V110 V111 V112 V113 V114 V115 V116 V117 V118 V119 V12 V120 V121 V122 V123 V124 V125 V126 V127 V128 V129 V13 V130 V131 V132 V133 V134 Provider Manual 2013 VE CODE DESCRIPTION Compound with comprehensive Mutually exclusive Dos integrity Endoscopy Endoscopy 51 Reduced services Reduced services Reduced services Repeat surgery Unlisted Unusual procedure Reduced services Included in E&M Discontinued procedure Separate procedure Separate procedure Global ER Mod 26 review Psych UROLOGY(catheter) Included in E&M Application of cast Casting & strapping Included in E&M Diagnostic laparoscopy CMS bundled Bundled/excluded CMS Injections / misc Reserved Included in E&M Cast/ splint/ strap E&M counseling E&M w/psych E&M neonatal #1 Quantitative and qualitative E&M neonatal #2 E&M critical care Separate procedure User denied Delivery 309 V135 V136 V137 V138 V139 V14 V140 V141 V142 V143 V144 V145 V146 V147 V148 V149 V15 V150 V151 V152 V153 V154 V155 V156 V157 V158 V159 V16 V160 V161 V162 V163 V164 V165 V166 V167 V168 V169 V17 V170 V171 Provider Manual 2013 Sex conflict Modifier 51 Modifier 50 Copay check Lab/x-ray read Mutually exclusive Global already billed Repeat global procedure No auth Non-facility setting Anesthesia up code Billed less than paid Not valid mod New patient visit Ob visits Global ob Global orthopedic Office visit w/ ob care Office visit w/delivery Decision for surgery Invalid 26/tc modifier Incident to Pt service 25 mod Distinct procedure Prolonged E&M service Prolonged service Global procedure E&m with bat Sleep study Lab panel Critical care qty Timely filing Cob/tpl Benefit check Add-on procedure Add-on procedure Invalid facility Incidental procedure Cosmetic (never payable) Cosmetic/reconstructive 310 V172 V173 V174 V175 V176 V177 V178 V18 V180 V181 V182 V183 V184 V185 V19 V190 V191 V192 V196 V197 V198 V199 V2 V20 V21 V22 V23 V24 V25 V26 V27 V271 V272 V273 V274 V275 V28 V29 V3 V30 V301 Provider Manual 2013 Cosmetic/reconstructive Cosmetic/reconstructive Cosmetic/reconstructive Cosmetic/reconstructive Chiropractic rad Chiropractor acute treatment Add-on Blood collection Professional / technical Surgical modifier Radiology modifier Pathology modifier E&M modifier CMS non-covered Exploration included Return to surgery(major) Return to surgery(minor) Drug administration The diagnosis for this service cannot be primary Medically unlikely edit Never events No consults Lab unbundling Separate procedure Separate procedure Global procedure Separate procedure Anesthesia included Surgery w/ specimen handling Global procedure Global procedure Decision for minor surgery Global decision Global period Global period Global period Unbundled Unbundled Global anesthesia With vs. Without conflict CCI Edits 311 V31 V32 V33 V34 V340 V35 V36 V37 V38 V39 V4 V40 V400 V401 V402 V403 V404 V41 V410 V411 V412 V413 V42 V43 V44 V45 V46 V47 V48 V49 V5 V50 V51 V52 V53 V54 V55 V56 V57 V58 V59 Provider Manual 2013 Compound with comprehensive Compound with comprehensive Compound with comprehensive Compound with comprehensive Null Compound with comprehensive Compound with comprehensive Compound with comprehensive Compound with comprehensive Compound with comprehensive Mutually exclusive Compound with comprehensive Transfers Not physician svc Non billable code Non-covered Invalid admit Laboratory panels Esrd (ov) Esrd (monthly) Esrd (day) Esrd (medical) Medicare fee Quantity check All inclusive Incident to Incident to Asst on self Duplicate procedure Duplicate procedure Sigmoidoscopy precedence Multiple 1 day visits Invalid sex Invalid place of service Invalid member age Day mismatch with billed qty Included in E&M Compound with comprehensive Compound with comprehensive Global anesthesia Global anesthesia 312 V6 V60 V61 V62 V63 V64 V65 V66 V67 V68 V69 V7 V70 V701 V702 V71 V72 V73 V74 V75 V76 V77 V78 V8 V80 V81 V82 V83 V84 V85 V86 V87 V88 V89 V9 V90 V91 V92 V93 V94 V95 Provider Manual 2013 Basically same procedure Ob conflict Once in lifetime Global emergency Endoscopic Colonoscopy Signoidoscopy Compound with comprehensive Dialysis quantity Compound with comprehensive Asst/cosrg mismatch Excision includes wound repair Invalid modifier Invalid CPT Invalid dx Decision for minor surgery Global decision Global period Global period Global period Sos rule Srg tray Global procedure Global endoscopic Case rate Dx detail Rad reduction Null Bilateral Up code Assistant surgeon Assistant surgeon Invalid co-surgeon Invalid co-surgeon Incidental procedure No team surgeon No team surgeon Bad date of service Terminated code Terminated code Ineligible 313 V96 V97 V98 V99 VEX XX1 ZZZ V420 Provider Manual 2013 Surgical qty Invalid dx Unauthorized Duplicate procedure Plan override of VE edit Invalid eob Automatic adjustment MPFS Functional G-Code 314 ELECTRONIC BILLING (EDI) First+Plus will accept electronic claims in the Standard HIPAA transactions. First+Plus accepts electronics claims from all active Clearing House’s in Puerto Rico, therefore providers should coordinate with their respective contracted Clearing House in order to submit electronic claims to First Plus. Contracted providers could also submit electronic claims directly with First Plus, but before submitting them, the provider has to complete the configuration process. We encourage providers to submit their claims electronically for more efficiency and effective payment process. X12 and HIPAA Compliance Checking, and Business Edits First Plus returns a 999 Functional Acknowledgment to the submitter for every inbound 837 transaction received. Each transaction passes through edits to ensure that it is X12 compliant. If it successfully passes X12 syntax edits, a 999 Functional Acknowledgement is returned indicating acceptance of the transaction. If the transaction fails X12 syntax compliance, the 999Functional Acknowledgement will also report the Level 1 errors in the AK segments and, depending on where the error occurred, will indicate that the entire interchange, functional group or transaction set has been rejected. Claim Status Report (277CA Transaction) First Plus returns a Claim Status Report (277CA) for each received file detailing the acceptance or rejection of each claim within the transaction. This report is sent to the transmitter of the X12 file. For example, if First Plus receives a file from a Clearinghouse the claim status report is sent to the Clearinghouse. It is responsibility of the provider to request that report from its Clearinghouse. In the Claim Status Report the claim status category code A1 means claim acceptance and A3 means claim rejection by First Plus. Usually the claim status category code is followed by the claim status code that describes the error. These codes are standardized through the industry and your system should interpret them. A complete list of the claim status codes as well as Claim Adjustment Reason Codes (CARC), and Remittance Advice Remark Codes (RARC) can be found at: http://www.wpc-edi.com/reference/ Provider Manual 2013 315 Claims Status Category-277CA A0 Acknowledgement/Forwarded-The claim/encounter has been forwarded to another entity. Start: 01/01/1995 A1 Acknowledgement/Receipt-The claim/encounter has been received. This does not mean that the claim has been accepted for adjudication. Start: 01/01/1995 A2 Acknowledgement/Acceptance into adjudication system-The claim/encounter has been accepted into the adjudication system. Start: 01/01/1995 A3 Acknowledgement/Returned as unprocessable claim-The claim/encounter has been rejected and has not been entered into the adjudication system. A4 Start: 01/01/1995 Acknowledgement/Not Found-The claim/encounter can not be found in the adjudication system. A5 Start: 01/01/1995 Acknowledgement/Split Claim-The claim/encounter has been split upon acceptance into the adjudication system. A6 A7 Start: 02/28/2002 Acknowledgement/Rejected for Missing Information - The claim/encounter is missing the information specified in the Status details and has been rejected. Start: 10/31/2002 Acknowledgement/Rejected for Invalid Information - The claim/encounter has invalid information as specified in the Status details and has been rejected. Start: 10/31/2002 A8 P0 Acknowledgement / Rejected for relational field in error. Start: 10/31/2004 Pending: Adjudication/Details-This is a generic message about a pended claim. A pended claim is one for which no remittance advice has been issued, or only part of the claim has been paid. Start: 01/01/1995 P1 Pending/In Process-The claim or encounter is in the adjudication system. Start: 01/01/1995 P2 P3 P4 Pending/Payer Review-The claim/encounter is suspended and is pending review (e.g. medical review, repricing, Third Party Administrator processing). Start: 01/01/1995 | Last Modified: 01/27/2008 Pending/Provider Requested Information - The claim or encounter is waiting for information that has already been requested from the provider. (Note: A Claim Status Code identifying the type of information requested, must be reported) Start: 01/01/1995 | Last Modified: 01/27/2008 Pending/Patient Requested Information - The claim or encounter is waiting for information that has already been requested from the patient. (Note: A status code identifying the type of information requested must be sent) Start: 01/01/1995 | Last Modified: 01/27/2008 P5 Provider Manual 2013 Pending/Payer Administrative/System hold Start: 10/31/2006 316 F0 Finalized-The claim/encounter has completed the adjudication cycle and no more action will be taken. Start: 01/01/1995 F1 Finalized/Payment-The claim/line has been paid. Start: 01/01/1995 F2 Finalized/Denial-The claim/line has been denied. Start: 01/01/1995 F3 F3F F3N F4 Finalized/Revised - Adjudication information has been changed Start: 02/28/2001 Finalized/Forwarded-The claim/encounter processing has been completed. Any applicable payment has been made and the claim/encounter has been forwarded to a subsequent entity as identified on the original claim or in this payer's records. Start: 01/01/1995 Finalized/Not Forwarded-The claim/encounter processing has been completed. Any applicable payment has been made. The claim/encounter has NOT been forwarded to any subsequent entity identified on the original claim. Start: 01/01/1995 Finalized/Adjudication Complete - No payment forthcoming-The claim/encounter has been adjudicated and no further payment is forthcoming. Start: 01/01/1995 F5 Finalized/Cannot Process R0 Start: 01/01/1995 | Stop: 10/16/2003 Requests for additional Information/General Requests-Requests that don't fall into other R-type categories. Start: 01/01/1995 R1 Requests for additional Information/Entity Requests-Requests for information about specific entities (subscribers, patients, various providers). Start: 01/01/1995 R3 Requests for additional Information/Claim/Line-Requests for information that could normally be submitted on a claim. Start: 01/01/1995 | Last Modified: 02/28/1998 R4 R5 Requests for additional Information/Documentation-Requests for additional supporting documentation. Examples: certification, x-ray, notes. Start: 01/01/1995 | Last Modified: 02/28/1998 Request for additional information/more specific detail-Additional information as a follow up to a previous request is needed. The original information was received but is inadequate. More specific/detailed information is requested. Start: 01/01/1995 | Last Modified: 06/30/1998 R6 Requests for additional information – Regulatory requirements R7 Start: 02/28/2007 Requests for additional information – Confirm care is consistent with Health Plan policy coverage R8 Start: 02/28/2007 Requests for additional information – Confirm care is consistent with health plan coverage exceptions Start: 02/28/2007 Provider Manual 2013 317 R9 Requests for additional information – Determination of medical necessity Start: 02/28/2007 R10 Requests for additional information – Support a filed grievance or appeal Start: 02/28/2007 R11 Requests for additional information – Pre-payment review of claims R12 Start: 02/28/2007 Requests for additional information – Clarification or justification of use for specified procedure code Start: 02/28/2007 R13 Requests for additional information – Original documents submitted are not readable. Used only for subsequent request(s). Start: 02/28/2007 R14 R15 Requests for additional information – Original documents received are not what was requested. Used only for subsequent request(s). Start: 02/28/2007 Requests for additional information – Workers Compensation coverage determination. Start: 02/28/2007 R16 Requests for additional information – Eligibility determination Start: 02/28/2007 R17 RQ Replacement of a Prior Request. Used to indicate that the current attachment request replaces a prior attachment request. Start: 01/20/2013 General Questions (Yes/No Responses)-Questions that may be answered by a simple 'yes' or 'no'. Start: 01/01/1995 | Last Modified: 07/09/2007 | Stop: 01/01/2008 E0 Response not possible - error on submitted request data Start: 01/01/1995 | Last Modified: 02/28/2002 E1 Response not possible - System Status Start: 02/29/2000 E2 Information Holder is not responding; resubmit at a later time. Start: 06/30/2003 E3 E4 Correction required - relational fields in error. Start: 01/24/2010 Trading partner agreement specific requirement not met: Data correction required. (Note: A status code identifying the type of information requested must be sent) Start: 01/30/2011 D0 Data Search Unsuccessful - The payer is unable to return status on the requested claim(s) based on the submitted search criteria. Start: 01/01/1995 | Last Modified: 09/20/2009 Provider Manual 2013 318 FRAUD, WASTE & ABUSE Health care fraud and abuse is a federal offense. First+Plus has a strict zero-tolerance policy toward fraud, waste and abuse. The purpose of investigating these activities is to protect the member, government, and/or First+Plus from paying more for a service than it is obligated to pay. However, First+Plus’ zero-tolerance policy is not limited to cases of fraud or abuse. First+Plus also investigates instances of waste as well as any inappropriate activities. Our policies in this area reflect that First+Plus, its providers, their staff and agents are subject to federal and state laws designed to prevent fraud and abuse in government programs (e.g., Medicare and Medicaid), federally funded contracts and private insurance. First+Plus complies with all applicable laws, including the Federal False Claims Act, applicable whistleblower protection laws, the Deficit Reduction Act of 2005, the American Recovery and Reinvestment Act of 2009, the Patient Protection and Affordable Care Act of 2010 and applicable state and federal billing requirements for state-funded programs, federally funded health care programs (e.g., Medicare Advantage, SCHIP and Medicaid) and other payers. First+Plus expectation is that you fully cooperate and participate in its fraud, waste and abuse programs. This includes, but not limited to, permitting First+Plus access to member records and allowing for on-site audits or reviews. Also, First+Plus may interview Members as part of an investigation, without provider interference. What is Fraud? Fraud means an intentional deception or misrepresentation made by a person with the knowledge that the deception could result in some unauthorized benefit to him / herself for some other person. It includes any act that constitutes fraud under applicable federal or state law. What is Abuse? Abuse means provider practices that are inconsistent with sound fiscal, business, or medical practices, and result in an unnecessary cost to government-sponsored programs, and other health care programs/plans, or in reimbursement for services that are not medically necessary or that fail to meet professionally recognized standards for health care. It also includes recipient practices that result in unnecessary cost to federally and/or state-funded health care programs, and other payers. What is Waste? Waste means over-utilization of services or other practices that result in unnecessary costs. Examples of Fraud, Waste and Abuse include, but are not limited to: • Billing more than once for the same service • Billing for services never performed or provided Provider Manual 2013 319 • • • • • • • Performing inappropriate or unnecessary services Routinely waiving patient deductibles or co-payments Providing lower cost or used equipment and billing for higher cost or new equipment Using someone else’s identity Altering or falsifying pharmacy prescriptions Providing services in a method that conflicts with regulatory requirement Prescribing a medication for 30 days with a refill when it is not known if the medication will be needed. FWA Training: First+Plus providers are responsible for administering the necessary training on Fraud, Waste and Abuse to its new employees within the first 90 days of employment, including managers, directors, contractors, subcontractors, and board members and annually thereafter. The provider must keep a copy of this training and proof of its delivery in case First+Plus and/or any government agency requests it and must acknowledge, annually, that it has complied with this requirement. CMS has developed a web-based training module that can be used to satisfy the FWA training and education requirements. Using CMS’ training and education module is optional. However, this training meets CMS’ FWA training requirements and is accepted by First+Plus as an appropriate training tool. The FWA training and education module is available through the CMS’ Medicare Learning Network (MLN). To take a web-based training course, go to http://www.cms.gov/MLNProducts. There is one exception to the FWA training and education requirement. Regulations effective June 7, 2010 implemented a “deeming” exception which exempts providers who are enrolled in Medicare Parts A or B from annual FWA education and training (42 CFR § 422.503(b)(4)(vi)(C)(2) and 42 CFR§ 423.504(b)(4)(vi)(C)(3)). Therefore, if an entity or an individual is enrolled in Medicare Parts A or B, the FWA training and education requirement has already been satisfied. In the case of chains, such as chain pharmacies, each individual location must be enrolled in Medicare Part A or Part B to be “deemed”. The deeming exception for FWA training and education does not apply to the Medicare Parts C and D compliance training and education requirement. Therefore, even if a health care provider, entity or supplier is deemed for FWA training and education, the requirement for compliance training and education must still be fulfilled. It is important that you keep training logs, demonstrating who was trained, including training dates and certificates of completion. For your convenience, a certificate of completion, which can be filled out by the person completing the FWA training, is included as the last slide of CMS’ FWA training and education module. Provider Manual 2013 320 Reporting Fraud, Waste and Abuse: First+Plus expects providers, their staff and agents to report any suspected cases of fraud, waste or abuse. First+Plus will not retaliate against you if you inform us, the federal government, state government or any other regulatory agency with oversight authority of any suspected cases of fraud, waste or abuse. If a violation of federal law has taken place, the case will be referred to the Centers of Medicare & Medicaid Services (OIG), Department of Health and Human Service Office of Inspector General (OIG), and/or other law enforcement agencies, as appropriate. Overpayments for prescription drugs require immediate corrective action in the form of repayment. All employees, members, and providers shall report all alleged Fraud, Waste, and Abuse cases and other inappropriate activities to the Special Investigations Unit (SIU) Department. All such activities will be subject to investigation and forwarded to the applicable government agency for further investigation, if warranted. Reports of potential or actual compliance issues related to First+Plus Medicare Part C or Part D program must be self-reported to the Centers for Medicare & Medicaid Services (CMS), Office of the Inspector General (OIG), the Medicare Drug Integrity Contractors (MEDICs) and/or the Office of the Commissioner of Insurance for further investigation. An individual who engages in any fraud, waste, and abuse activity, alone or in collaboration with other employees, patients, or providers, are subject to immediate disciplinary action up to and including termination of contract. An employee, member or provider must report any alleged inappropriate activity but may do so voluntarily without disclosing his/her name and information. First+Plus will not tolerate retaliation in any form, and regards any form of retaliatory action toward any reporter of potential fraud, waste or abuse as a very serious regulatory/legal violation. Any questions involving inappropriate activities or clarification should be forwarded to the SIU Department. Reports to the Fraud, Waste and Abuse Hotline may be made 24 hours a day/seven days a week. Callers may choose to remain anonymous. All calls will be investigated and remain confidential. Fraud, Waste and Abuse reports may be made through one of the following: Provider Manual 2013 321 • • Fraud, Waste and Abuse Hotline at (866) 933-9336 Fraud, Waste and Abuse email: [email protected] In writing to: • First+Plus Special Investigations Unit PO Box 191580 San Juan, PR 00918-1580 The informant needs to provide the SIU Department with as much detail as possible on the incident. If available, provide: • • • • • Description of the incident When informant became aware of the incident Date(s) the incident occurred Specific individuals involved in the incident If available, provide documentation/evidence. If not anonymous, the informant should be prepared to provide his/her name and contact phone number in the event additional information and/or follow up is required. The SIU Department creates a file and begins the investigation. Please note, the SIU Department will not update the informant of the status or results of the investigation as such information is confidential. You may also contact the following: U.S. Department of Health and Human Services (HHS) Office of Inspector General (OIG) OIG’s National Hotline: 1-800-323-8603 Fax: 202-254-4292 Email: [email protected] Centers for Medicare & Medicaid Services (CMS) 1-800-633-4227 Website: http://www.cms.gov Important Laws against Health Care Fraud that you must know There are a number of laws that address health care fraud. These laws define fraud and establish the framework for the prosecution of criminal acts and the initiation of civil suits by injured parties. Listed below are a few of the laws that address health care fraud. We encourage you to review Chapter 9 of the Prescription Drug Benefit Manual or Chapter 21 of the Medicare Manage care Manual, specifically Appendix B which includes other laws which you may need to be compliant with. Provider Manual 2013 322 Federal False Claims Act (FCA) – 31 U.S.C. Titles 1347 The False Claims Act addresses any person or entity that does any of the following: • Knowingly presents, or causes to be presented, to an employee of the United States government a false or fraudulent claim for payment or approval • Knowingly makes, uses or causes to be made or used, a false record or statement to get a false or fraudulent claim paid or approved by the government • Conspires to defraud the government by getting a false or fraudulent claim allowed or paid • Knowingly makes, uses or causes to be made or used, a false record or statement to conceal, avoid or decrease an obligation to pay or transmit money to the government • Has actual knowledge of the information • Acts in deliberate ignorance of the truth or falsity of the information • Acts in reckless disregard of the truth or falsity of the information; no proof of specific intent to defraud is required. The False Claims Act imposes two sorts of liability: • The submitter of the false claim or statement is liable for a civil penalty, regardless of whether the submission of a claim actually causes the government any damages and even if the claim is rejected. • The submitter of the claim is liable for damages that the government sustains because of the submission of the false claim. Under the False Claims Act, those who knowingly submit or cause another person to submit false claims for payment by the government, are liable for three times the government’s damages plus civil penalties of $5,000 to $10,000 per false claim. Note: The federal government does not consider an innocent mistake as a legitimate defense for submitting a false claim and the violation could result in a multitude of penalties. Whistleblower (Qui Tam) Protection – 31 United States Code Service (USC) 3730 (h) The whistleblower provision protects employees who assist the federal government in investigation and prosecution of violations of the False Claims Act. Whistleblower protections apply only to actions taken in furtherance of a viable False Claims Act case, which has been, or is about to be, filed. The provision prevents retaliation against employees such as firing them for assisting in the investigation and prosecution. If any retaliation does occur, the employee has a right to obtain legal counsel to defend the actions taken. Note: A whistleblower (Qui Tam) is someone, such as an employee, who reports suspected misconduct that would be considered an action against company policy or federal laws or regulations. In 1994 alone, false claims act litigation resulted in payment to people/plaintiffs of $379 million. Provider Manual 2013 323 Physician Self-Referral Prohibition Statute commonly referred to as the “Stark Law” 1877 of the Social Security Act (42 USC 1395) This statute prohibits physicians from referring Medicare patients for certain designated health services (DHS) to an entity with which the physician or a member of the physician’s immediate family has a financial relationship, unless an exception applies. It also prohibits an entity from presenting or causing to be presented a bill or claim to anyone for a DHS furnished as a result of a prohibited referral. Anti-Kickback Statute Section 1128(b) of the Social Security Act (42 USC 1320a-7b (b)) The federal anti-kickback laws that apply to Medicare and Medicaid prohibit health care professionals, entities and vendors from knowingly offering, paying, soliciting or receiving remuneration of any kind to induce the referral of business under a federal program. In addition, most states have laws that prohibit kickbacks and rebates. Remuneration under the federal antikickback statute includes the transfer of anything of value, directly or indirectly, overtly or covertly, in cash or in kind. Violators are subject to criminal sanctions such as imprisonment, as well as high fines, exclusion from Medicare and Medicaid, very costly civil penalties and possible prosecution under many similar state laws. The anti-kickback law is extremely broad and covers a wider range of activities than just traditional kickbacks. Federal regulations include safe harbors that protect certain technically prohibited activities from prosecution. If you are unsure whether an activity violates the antikickback law, you should seek the advice of a legal professional. Fraud and Abuse, Privacy and Security Provisions of the Health Insurance Portability and Accountability Act, as modified by HITECH Act This act could be considered an extension of HIPAA, as it enabled the U.S. Department of Health and Human Services to promote and expand the adoption of health information technology. It addresses: • Use of electronic health records, including incentives for adopting them and requirements around their disclosure • How to secure protected health information appropriately • When and to whom notifications should made in regard to data breaches of unsecured protected health information (PHI) http://www.healthit.gov/policy-researchers-implementers/final-rules-regulations Antitrust Laws State and federal antitrust laws prohibit monopolistic conduct and agreements that restrain trade. First+Plus is committed to competition and consumer choice in the marketplace. All health care Provider Manual 2013 324 professionals, entities and vendors must adhere to the antitrust laws and must avoid any agreements or understandings with competitors on price, customers, markets or other terms of dealing and avoid trade practices that unfairly or unreasonably restrain competition in dealings with providers or customers. Civil Monetary Penalties Law The OIG may seek civil penalties and sometimes exclusion for a wide variety of conduct and is authorized to seek different amounts of penalties and assessments based on type of violation at issue. Penalties range from $10,000 to $50,000 per violation and include: • Presenting a claim that the person knows or should know is for an item or • Service that was not provided or is false or fraudulent or for which payment may not be made. • Violating Medicare assignment provisions. • Violating the Medicare physician agreement. • Providing false or misleading information expected to influence a decision or discharge. • Making false statements or misrepresentations on application or contracts to participate in Federal Health Care programs. • Violations of the Anti-Kickback statute and/or Stark Law. The Beneficiary Anti-Inducement Statute (42 U.S.C. § 1320a-7a (a) (5) This federal statute declares that any person who gives or offers to give anything of value* to a Medicare or Medicaid beneficiary that the person knows or should know is likely to influence a beneficiary’s choice of a particular health care provider, practitioner, or supplier to buy or rent a Medicare or Medicaid covered item from the provider, practitioner, or supplier may be liable for civil money penalties of up to $10,000 for each wrongful act. http://www.gpo.gov/fdsys/pkg/USCODE-2010-title42/pdf/USCODE-2010-title42-chap7subchapXI-partAsec1320a-7a.pdf * The OIG stated in guidance that there is a “nominal value” exception that allows a health care provider to give: • A gift to a beneficiary as long as the gift has a retail value of $10 or less • Multiple gifts of $10 or less over a 12-month period, as long as the total retail value of the gifts does not exceed $50 Any such gift must not be in cash or cash equivalents, so it should not be a gift card or gift certificate. Types of gifts and their value(s) are detailed in a Special Advisory Bulletin from the OIG: https://oig.hhs.gov/fraud/docs/alertsandbulletins/SABGiftsandInducements.pdf Provider Manual 2013 325 Additional Resources • CMS Prescription Drug Manual – Chapter 9: o http://www.cms.gov/manuals/downloads/Pub100_18.pdf • Code of Federal Register: (see 42 CFR 422.503 and 42 CFR 422.504) • Office of the Inspector General: o http://www.oig.hhs.gov/compliance/compliance-guidance/index.asp • Federal Sentencing Guidelines: o http://ussc.gov/Guidelines • Health Insurance Portability and Accountability Act (HIPAA): o http://aspe.hhs.gov/admnsimp/pl104191.htm • False Claims Act: o http://www.justice.gov/jmd/ls/legislative_histories/pl99-562/pl99-562.html • Anti-Kickback Statute (see section 1128B(b): o http://www.ssa.gov/OP_Home/ssact/title11/1128B.htm#f First+Plus does not knowingly tolerate fraudulent activity by any of its providers, its employees and/or agents and will investigate and report any such known activity to the appropriate regulatory, federal and state agencies for further action and investigation. Provider Manual 2013 326 ADDITIONAL INFORMATION: • First+Plus does not deny, limit or condition the coverage or furnishing of benefits to individuals eligible to enrolling First+Plus on the basis of health status. (ESRD excluded) • No referrals are needed to access care provided by contracting or non-contracting providers under PPO coverage’s. Some services may require precertification or may not be covered when rendered by an out of network provider. • First+Plus members have direct access to mammography and influenza vaccines as well as to women’s specialist for routine and preventive services • No additional co-payment beyond an office visit co-payment if applicable may be charged for influenza vaccines or the pneumococcal vaccine • First+Plus receives federal payments under the Medicare Advantage program. It complies with all laws and regulation applicable to entities receiving federal funds including, but not limited to, Title VI of the Civil Rights Act of 1964, the Age discrimination Act of 1975, the Americans with Disabilities Act and the Rehabilitation Act of 1973 • First+Plus monitors and reports to quality and performance including but not limited to: member satisfaction, disenrollment, and health outcomes. • Provider agrees to provide reasonable continuity of care as required by CMS regulation to beneficiaries eligible for such care. Provider Manual 2013 327
© Copyright 2026