EXPLAINING TRAINING - UPDATES TO QCPP TRAINING REQUIREMENTS
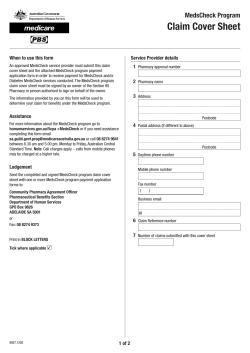
Supporting Excellence in Pharmacy January - February 2014 EXPLAINING TRAINING - UPDATES TO QCPP TRAINING REQUIREMENTS QCPP REQUIREMENTS MANUAL UPDATE #4 ARE YOU QCPP READY? MY FIRST TIME: REACCREDITATION Nick Panayiaris — new Chair of Quality Assurance and Standards Committee Nick Panayiaris Chair, Quality Assurance and Standards Committee National Councillor The Pharmacy Guild of Australia I am delighted to accept the responsibility of Chair of the Quality Assurance and Standards Committee. I see a challenging future ahead for community pharmacy but one that must be supported by quality standards that drive professionalism and support community pharmacy as a healthcare destination. The Quality Assurance and Standards (QAS) Committee is the governing committee that provides strategic guidance over the Quality Care Pharmacy Program and other Pharmacy Guild accreditation and standards matters. After celebrating QCPP’s 15 year birthday in 2013, I am keen to ensure the ongoing development of QCPP to ensure the program’s success for another 15 years and beyond! I believe that the model of community pharmacy for the future is one that reflects the changing focus of pharmacy practice from one of product supply (dispensing of medicines) to a more comprehensive ‘whole of health’ approach incorporating more extensive professional services. There is no doubt that the 5th Community Pharmacy Agreement (5CPA) and the success of the Pharmacy Practice Incentives supported by QCPP has helped drive this change. A great example of the wealth of resources and information published by QCPP to help support pharmacies comply with PPI and QCPP requirements is at www.qcpp.com/incentives/ppi-resources-and-tools As we move into negotiating the 6CPA, the Guild knows community pharmacy needs to make an even greater contribution to primary health care across Australia. We have the network, with over 5300 pharmacies broadly distributed in metropolitan, rural and remote locations. But we need to focus on strengthening, expanding and transforming community pharmacy so it can do more, and be better integrated with other health services so care is seamless. We must do this by building on community pharmacy’s long held core values, skills and professionalism, and quality underpinned by QCPP. I am a great supporter of the Quality Care Pharmacy Program in my pharmacies and I am responsible for QCPP and PPI management within my pharmacy group. However, my mantra for QCPP is that it must have a direct customer impact and have benefit to the customer experience. Regardless of whether QCPP is supporting the smooth and successful operation of a pharmacy or guiding implementation of a new professional service, there needs to be relevance to how QCPP benefits the consumer. I was involved in some of the strategic development of the QAS division and QCPP in 2013. I was very keen to ensure that QCPP stays relevant to improving practice, supporting customer service, and making pharmacies better business operations. I also believe we need to offer a better QCPP value proposition to members and ensure that QCPP is easier to implement and maintain, whilst still driving high standards and compliance with quality requirements. I look forward to hearing your thoughts about the Quality Care Pharmacy Program in my new role as Chair of the Quality Assurance and Standards Committee. I am based in South Australia, and am Vice President of the SA Branch of the Guild. FROM THE DIRECTOR Andrew Matthews National Director Quality Assurance and Standards I’d like to welcome Nick Panayiaris as the new Chair of the Quality Assurance and Standards Committee. I have known Nick for sometime now; he knows community pharmacy and what it needs to be successful in future. He is bright, passionate and is committed to QCPP and the benefits it provides to pharmacy businesses and to community pharmacy overall. I’d also like to acknowledge the contribution of Paul Sinclair, NSW Guild Branch President and former QAS Committee Chair. Paul provided great oversight of the Quality Care Pharmacy Program in Quality Care Pharmacy Program his time as Chair. I thank Paul for the support he personally provided to me and the QAS team. This edition we’re focusing on ‘…are you QCPP ready?’ I loved reading of the two WA pharmacies that came up for first time re-accreditation in 2013. They both acknowledged the great support from their WA QCPP state team to help them maintain their quality management system. Speaking of support from QCPP experts, remember if you are going to APP 2014, don’t forget to visit the QCPP Knowledge Centre and talk to a QCPP Expert. Get ready…get set…get reading: Excellence. 3 NEW PROCESS FOR T1A DECLARATIONS QCPP continuously monitors all administration processes for improvements and has transitioned to a new database system which will help facilitate more streamlined administration processes resulting in more effective and efficient service to our members. As part of our review and system upgrade we have been able to identify some areas for improvement including some changes to the T1A Legal and Professional Obligations Declaration process. The T1A Legal and Professional Obligations Declaration form is no longer required to be sent to QCPP. However, the T1A declaration is still required as evidence and will be sighted by your QCPP assessor at your assessment. Please ensure you keep all copies of the T1A Legal and Professional Obligations Declaration for your assessment. T1A LEGAL AND PROFESSIONAL OBLIGATIONS DECLARATION You cannot modify this template. Legal and professional obligations declaration by a proprietor or manager I, (name) being the proprietor/manager of (pharmacy name) located at (pharmacy address) of PBS Approval Number and QCPP ID Number declare that: I have confirmed all pharmacists employed or contracted to work in my pharmacy have current registration with the Pharmacy Board of Australia. I have confirmed all pharmacists employed or contracted to work in my pharmacy have undertaken a self assessment against the PSA Professional Practice Standards within the past 12 months and I am satisfied with the results of the self assessments. I have confirmed all pharmacists employed or contracted to work in my pharmacy have current individual professional indemnity insurance. I have confirmed this pharmacy complies with all legislative requirements relating to the operation of the pharmacy. I have confirmed this pharmacy has no contracts (excluding tenancy leases) that restrict our ability to stock products or provide services that meet the therapeutic needs of our consumers. I declare that the information provided on this declaration is true and accurate. I declare that I have the authority to make this declaration on behalf of this pharmacy. Date: Signed: Pharmacy proprietor/manager Print name: Please Note: The PPI Annual Payment Eligibility Declaration is still required to be submitted to QCPP annually as detailed in the PPI Program Specific Guidelines. The PPI Annual Payment Eligibility Declaration is available on the QCPP website www.qcpp.com and can be submitted to the QCPP helpdesk via fax on 02 6270 1885, email [email protected] or post to PO Box 7036, Canberra Business Centre ACT 2610. CONTENTS 4 7 8 Explaining training — updates to QCPP training requirements QCPP Requirements Manual update #4 Are you QCPP ready? Important Note: The T1A Legal and Professional Obligations Declaration must be declared each accreditation cycle (2 years) and retained as evidence (at the pharmacy) for each assessment. This Declaration is NOT required to be faxed to QCPP. It is the responsibility of the pharmacy to retain this document as evidence. Pharmacies will be requested to produce this declaration at each assessment and may be requested to provide the previous assessment cycle declaration as evidence during assessment visits. QCPP Version 2.2 ©2014 Pharmacy Guild of Australia 10 12 14 Page 1 of 1 Tips from the experts: maintaining QCPP My first time: Reaccreditation Three reports — one big future for pharmacy Supporting Excellence in Pharmacy Excellence January/February 2014 4 EXPLAINING TRAININg — UPDATES TO QCPP TRAINING REQUIReMENTS Peter Guthrey – Pharmacist Consultant T2C Pharmacy Medicines and Pharmacist Only Medicines Checklist requires staff who supply these medicines to undergo initial training via a recognised course and ongoing refresher training. This requirement supports the appropriate supply of these scheduled medicines to the Australian community. While most pharmacies are aware that these ‘S2/S3’ training requirements exist, what the requirements are and which staff members they apply to, appears to be a common point of confusion for many pharmacies. In response to this, QCPP have clarified the requirements in updates to: T2C Supplying Pharmacy Medicines and Pharmacist Only Medicines Checklist Training Requirements for Pharmacy Medicines and Pharmacist Only Medicines brochure The following pages describe who the requirements apply to and what evidence is needed to meet the annual refresher training requirements. More information is available at www.qcpp.com If you have queries regarding these requirements, and how they apply to your pharmacy, contact your QCPP State Manager or email [email protected]. T2C Supplying Pharmacy Medicines and Pharmacist Only Medicines Checklist Action 2.1 Action to meet the program requirement Evidence required at assessment Ensure all staff who directly supply Pharmacy Medicines or assist the pharmacist with the supply of Pharmacist Only Medicines have received initial training via a Recognised Course and ongoing Refresher Training in supplying Pharmacy Medicines and Pharmacist Only Medicines. Proof of compliance with the ‘Training Requirements for Pharmacy Medicines and Pharmacist Only Medicines’ brochure. For more information go to: www.qcpp.com/resources/training-requirements. Quality Care Pharmacy Program This article summarises training requirements for pharmacy medicines and pharmacist only medicines Version 2.2 5 Who do the training rEquirements apply to? Action 2.1 applies to all pharmacy assistants who are directly involved in the supply or support the supply of Pharmacy Medicines and/or Pharmacist Only Medicines. Exception: Where all these products are out of reach of customers, only staff who work in the area where Pharmacy Medicines and/or Pharmacist Only Medicines are supplied require the training. The exception applies to pharmacies who comply with T2C Action 6.3 (non-mandatory) where all Pharmacy Medicines are stored out of reach of customers. All Queensland and Western Australian pharmacies should be compliant with this requirement as keeping Pharmacy Medicines out of reach is a legal requirement in these states. The addition of the word ‘directly’ to Action 2.1, and the removal of the ‘50% rule’ is intended to add clarity to which staff members are subject to the requirement. The examples illustrated below provide guidance on how the requirement and ruling apply. Example Pharmacy A Scheduled Medicines out of customer reach Sarah DISPENSARY/ PROFESSIONAL AREA Sarah is a pharmacy assistant who works in the professional services area. She supplies Pharmacy Medicines as a core part of her role. training? COUNTER Brad packs shelves in the general merchandise area of the pharmacy. During busy periods he helps serve in the professional services area. training? James works at the checkout in the pharmacy processing sales. He never works in the professional services area. training? POS James Brad YES YES NO pharmacy Medicines within customer reach Example Pharmacy B Mark DISPENSARY/ PROFESSIONAL AREA COUNTER training? Sam is a pharmacy assistant who works on weekends in a small pharmacy. She helps with all customer enquiries and processes sales. training? Sam Sally works in the cosmetics department of a large pharmacy. Her main role is to sell cosmetics. Sometimes she helps process general sales at the checkout when it gets busy. Karen Karen is a weight loss consultant who conducts weight loss consultations and promotes meal replacement products. She never processes sales at a checkout and she never assists in requests for non-prescription medicines. POS Sally Mark is a first year pharmacy student who works in the dispensary on weekends. YES YES training? YES training? NO all pharmacies Amanda is employed as a delivery driver part-time. She only delivers medicines (including Pharmacy Medicines) and other pharmacy goods to customers at home each morning. training? NO* * Pharmacy must comply with P11F Excellence January/February 2014 6 refresher training Pharmacy staff need to complete at least three hours of refresher training each year. Following a review, the evidence requirements for In-Pharmacy Training have been better aligned with the evidence required for both accredited training and QCPP Approved Refresher Training. The evidence requirements for different avenues for completion of Refresher Training are summarised in the table below: refresher TRAINING Evidence Required at Assessment Accredited Training A statement of attainment or transcript of results issued by the Registered Training Organisation (RTO) and recorded on the staff training record. In-Pharmacy Training [new requirements] Evidence of the training activity and recorded on the staff training record. Examples of evidence could include, but are not limited to: • • • • QCPP Approved Refresher Training Presentation materials Staff meeting record/minutes Session outline Signed attendance list The certificate of completion/attendance and recorded on the staff training record. The revised In-Pharmacy Training evidence requirement is not intended to be a burden to pharmacies who deliver in-pharmacy training as this evidence is likely already being generated by conducting the training activity. Evidence could include handouts, signed attendance lists, session outlines or staff meeting minutes. Any other reasonable evidence that the training has occurred will be accepted as evidence for this requirement. Once the training has been run, it is recommended the activity be placed in the pharmacy’s Evidence Folder. How do I maintain Refresher Training evidence? ACCREDITED TRAINING IN-PHARMACY TRAINING QCPP APPROVED REFRESHER TRAINING Complete accredited module Place transcript or Statement of Attainment in training record Deliver / attend training Place evidence in Evidence Folder Complete QCPP Approved Refresher Training Receive certificate and place in training record Record on T15B training record Refresher Training remedial actions How are remedials treated when a staff member has not completed the minimum 3 hours per year refresher training requirement? If a staff member has not completed the minimum 3 hours refresher training for each year, the assessor will raise a remedial action. The remedial action will be closed out when the pharmacy provides the assessor with evidence the staff member has completed 3 hours refresher training for the last year. The evidence required is outlined in the ‘Training Requirements for Pharmacy Medicines and Pharmacist Only Medicines’ brochure, available at www.qcpp.com. Excerpt from Implementation and Rulings Guide, Version 18 Quality Care Pharmacy Program 7 QCPP REQUIREMENTS MANUAL UPDATE #4 Natalie Smith – National Manager, Practice and Performance Manual updates are released as needed to ensure QCPP remains in line with contemporary pharmacy practice. The table below summarises the fourth round of updates to the QCPP Requirements Manual including the actions required from each update. The updated documents will be distributed to pharmacies at the end of January 2014. Pharmacies will be assessed against these updates at their next assessment. On receipt, please ensure old versions of the documents are removed from the pharmacy’s QCPP Requirements Manual and replaced with the new versions as provided in the update pack. If the pack has not arrived by midFebruary, your pharmacy can access the same documents electronically by visiting www.qcpp.com/qcpp-standard/ qcpp-requirements. The impact or action required column in the table outlines the key revisions to the manual that a pharmacy will need to consider when reviewing their operations manual to align with QCPP requirements. Please remember to revise your customised pharmacy policy and procedures to incorporate the required changes. Table 1. Outline of Manual Updates #4 Action, Procedure or Template Change Impact or action required Table of Contents – PROCEDURES Updated to reflect new versions of procedures listed in this table. Replace previous table of contents behind green Procedures tab in Requirements Manual with version 2.4. Table of Contents – TEMPLATES Updated to reflect new versions of templates listed in this table. Replace previous table of contents behind red Templates tab in Requirements Manual with version 2.4. Element 1 – Compliance with legal and professional obligations T1A Legal and Professional Obligations Declaration Revised Declaration This is now a one page document. Sign and retain as evidence for your assessment. Replace the previous T1A template with the new T1A template version 2.2. Element 2 – Supply of medicines, medical devices and poisons P2G Supplying Poisons Revised Procedure Complies with the new National Code of Practice for Chemicals of Security Concern. Replace procedure in the Requirements Manual, review your customised pharmacy procedure and amend as relevant. T2C Supplying Pharmacy Medicines and Pharmacist Only Medicines Checklist Revised Checklist Clarification of pharmacy assistants requiring initial training, refresher training and supporting guidelines. Replace the previous T2C template with the new T2C template version 2.2. Element 3 – Delivery of health programs and services T3B Dose Administration Aids Revised Checklist Checklist consistent with Guidelines on specialised supply arrangements, Pharmacy Board of Australia. Replace the previous T3B template with the new T3B template version 2.2. Element 12 – Recruiting staff Element 12 Action 5 (page 31) Updated All staff require completed offer of employment stored in their personnel file. Replace page 31 of the Elements (blue section) in Requirements Manual with version 2.1. Excellence January/February 2014 8 ARE YOU QCPP READY? Tess Jones – QCPP Marketing Manager Welcome to 2014 — a new year full of patient support, professional services and health care Resources/Tools A year of collaboration with peers, customer service, dispensing, health promotion and clinical interventions. The future is bright for your pharmacy and the professional services you provide; but are your procedures and policies up to date? Are your staff members trained and informed? Have you reviewed your operations manual since your last assessment? When was that last big ‘spring clean’ of the pharmacy’s important documents? QCPP is here to help. With a suite of tools and resources available, including one-on-one support from state QCPP teams, there is no need to get in a panic leading up to the end of your accreditation period. Quality Care Pharmacy Program QCPP has developed a range of checklists to assist your pharmacy stay on track and ready for assessment. Whether you are after an example of what your assessment will be like with the comprehensive Assessment Guide or a quick reminder of your requirements with the Maintenance Checklist; QCPP has the tool to help you. We have even developed a Professional Services Guide which features all the actions needed to meet Elements 2 and 3 and the PPI Expansion Checklist for pharmacies registered for the Pharmacy Practice Incentives. Download your copy of the checklists from www.qcpp.com/ resources/tools/qcpp-checklists or contact your QCPP state team for a hard copy. 9 Folders The suite of qcpp folders helps your pharmacy meet the requirements of accreditation. This year QCPP added to our suite of folders with the newly developed Evidence for Professional Services folder. This folder can be used to store any resources relating to professional services your pharmacy offers, including procedures, fact sheets or evidence for assessment (i.e. calibration records). It is also a handy tool for keeping track of your Pharmacy Practice Incentives evidence. An operations manual can ensure there is a single source for policies and procedures in a pharmacy and help the collation of these documents for implementation of QCPP requirements. The Evidence folder is an ideal location to store your pharmacy appearance checklists, hire equipment forms, incident reports etc. and if used regularly it will contain much of the evidence needed at your assessment. The Pharmacy Operations manual has been created to provide pharmacies with a folder that can be easily customised to store your pharmacy’s tailored QCPP policies and procedures. To receive your free copy of the QCPP folders, contact your QCPP state team today. Fast Track QCPP State Teams Implementing the QCPP Standard in your pharmacy is not as daunting as first thought. QCPP has provided electronic copies of all the templates and procedures you see in the Requirements Manual, ready for customisation. We have also included many example documents such as position descriptions to make running your business a little easier. Your QCPP State Team, led by a Quality Care State Manager, has intimate knowledge of the QCPP Standard. They can provide hands on knowledge and experience to assist your pharmacy and staff to implement QCPP. From time to time, new Fast Track documents will be developed to support QCPP requirement changes and are released in line with the Requirements Manual updates. For more information visit www.qcpp. com/resources/tools/fast-track to download new Fast Track documents. The teams can arrange initial and follow-up visits and phone calls on all QCPP matters. The majority of our teams have been in your position, implemented QCPP within a pharmacy, and are now ready to provide their advice and learnings to their peers. For more information visit www.qcpp. com/about-qcpp/qcpp-branch-staff for the contact information of your nearest QCPP Expert. APP KNOWLEDGE CENTRE Visit the QCPP Knowledge Centre at APP2014 from 14-16 March, to get valuable assistance and expert advice to help you meet the QCPP Requirements. QCPP State Managers and experts will be available to provide hands on advice for all things QCPP and PPI. Visit the QCPP Knowledge Centre at stand 42 from Friday 14 March to secure your one-on-one session. These resources are provided free to members and are some of the many ways the program is working to help make implementation of the Standard easier for all pharmacies. For more information on any of the above, please contact your QCPP State Team. www.qcpp.com Excellence January/February 2014 10 tips from the experts: maintaining qcpp Your QCPP State Teams are a valuable resource to pharmacies implementing and maintaining their QCPP accreditation Our QCPP Experts are there to answer your questions and provide in-pharmacy assistance when required. Don’t delay in getting new staff We asked them to provide their top tips in assessment preparation as a handy resource for your next accreditation period. Schedule a short professional services meeting for staff — make sure all staff have a basic understanding of the services the pharmacy is PPI registered for, make sure all staff read related policies and procedures, and this is recorded on their T15B Training Record. Visit www.qcpp.com to meet your QCPP State Managers and for your State Team contact information. Keep training record cards up to date, log all training staff undertake as soon as it is complete on the T15B Training Record. trained — it will benefit the pharmacy with increased sales and service. And make refresher training interesting – try implementing a reward system. When inducting a new staff member, think about the training that individual staff member will need specific to their role. Even an experienced dispensary assistant or dose administration packer that is new to your pharmacy, may not be familiar with your pharmacy systems. For example by recording a brief detail of the ‘Webster Care Guidelines’ if using Webster Care system or your ‘Nursing Home Procedure’ if packing for a facility on the T15B Training Record, your evidence will be ready when your assessment comes around. Inform your pharmacy staff of the QCPP requirement of undertaking and recording at least three hours per year of approved refresher Pharmacy Medicine and Pharmacist Only Medicine training. This could be a simple file for each staff member that is easily accessed that consists of a T15B Training Record placed at the front which they fill out whenever they complete or attend a training followed by any certificates or statements of participation that they received from the training. Quality Care Pharmacy Program Have staff take responsibility for their own training record. Create a system where staff can easily access their T15B Training Record, fill in their own records and file their certificates. Regularly reviewing these records will also ensure all Refresher Training requirements are met. Ensure all of the Human Resource documents are in place and up to date. Get in touch with the IR person available to you from your state Branch office. If you are a Guild Member, you will have access to complementary support and advice. QCPP should be a team effort. The saying many hands make light work can be true if you let it. Many pharmacy assistants thrive on being given extra responsibility and it makes them feel like a valued member of the pharmacy team. There are many little tasks that other members of the pharmacy team could take on as part of their regular routine such as the daily fridge checking, or the pharmacy appearance checklist. These are simple but important tasks that will take little training. Stay informed with the updates sent to you from QCPP. Don’t just delete the Branch communications that are sent to your inbox. These are great sources of information, tips and upcoming events which may be beneficial. Split the program into different areas and match those to the interests/skills of your staff. Areas may include the PPI, Staff Inductions, Staff Training, Hiring of Equipment, Customer Service, etc. These responsibilities can involve reviewing related policies and procedures, managing records or equipment maintenance - with the QCPP Coordinator overseeing it all. 11 Check what PPI services your pharmacy is registered for on the 5CPA website at www.5cpa.com.au. Some of the services you are offering may have changed over the past two years. It’s also a good idea to make sure you are registered for the appropriate amount of services in Primary Health Care and Community Services Support to maintain those PPI payments. Plan regular reviews — It’s easy to keep things on track if you give QCPP a little attention often. Use the resources you have available to you such as Fast Track, the QCPP website and your State QCPP Team. Your Implementation Officer is always willing to visit, answer emails and offer advice over the phone. Use an intranet if you are part of a group. Keep an eye on your document control — update both the Requirements Manual and operations manual as soon as your updates are received. Hang a copy of the contents page from your Evidence Folder on the wall to remind when and what to do — such as daily fridge temperature recording and completing the T17D Loss Prevention Checklist every three months. Record, record, record — ensure all of the evidence is available for your assessor. Be consistent and utilise the complementary folders provided by your State QCPP Team. Complete a mini self-assessment every year and check that everything is on track. Discuss with your staff your pharmacy’s procedures when a customer requests a blood pressure check and to make sure it is recorded according to your procedure. By educating your staff on how they can distinguish the difference between a T3C Screening and Risk Assessment or a T3I Disease State Management service it will assist them in knowing what procedure to follow and how to record. Excellence January/February 2014 12 MY FIRST TIME: REACCREDITATION Tess Jones – QCPP Marketing Manager Over 670 pharmacies joined the Quality Care Pharmacy Program in 2011 with the purpose of registering for the Pharmacy Practice Incentive Program. Today, these pharmacies are QCPP converts, dedicated to providing quality services and health care to their customers. While the accreditation and assessment process may seem daunting to some pharmacies, there are those that take it all in their stride. QCPP spoke to two pharmacies who recently underwent their first reaccreditation with the program and can see the positive outcomes of implementing a quality program in their pharmacy. Springs Chemmart Pharmacy in outer Perth was prepared going into their first reaccreditation. They had followed the advice of their QCPP Implementation Officer Joanne Arbuckle and were confident in their well-structured review process. Pharmacy Assistant and QCPP Coordinator Michelle Croymann admits the positive attitude was not always present, especially while undergoing initial accreditation in 2011. ‘QCPP was really daunting to me in the beginning. I took over coordination from another colleague and I had to start the process again. But starting from scratch turned out to be a blessing in disguise,’ Michelle said. Quality Care Pharmacy Program 13 Michelle credits the positive advice from the QCPP team to giving her the confidence to restart the process again. With in-pharmacy visits, emails and a stream of phone calls, Michelle was able to implement QCPP in the pharmacy, and establish a thorough maintenance program. ‘Undergoing reaccreditation was a breeze in comparison because of the wellstructured plan we had set up. ‘We were encouraged to set up a review plan and follow it month by month, something simple that in hindsight makes great sense.’ Michelle developed the plan based on the advice from Joanne, who advocated for regular maintenance of QCPP procedures and policies – not only to make the accreditation process smoother, but also to keep the pharmacy business running well. ‘Looking back implementing QCPP was kind of simple. There was no need to stress with all the templates and procedures provided for us,’ Michelle said. ‘But one thing we did learn and apply was – record, record, record.’ ‘Quality Care is not a chore. It is part of every day and doing it consistently takes the stress out of your upcoming assessment.’ It was a similar story for Leschenault Pharmacy in regional WA. Pharmacist Manager Mary Rose credits their successful reaccreditation to regular maintenance and staying on top of policies and processes. ‘When you have all the processes and policies in place and follow them, it makes your assessment preparation easier.’ ‘Develop the policy, stick to it and make sure you complete all requirements and record where necessary,’ Mary said. The regional pharmacy employs only one pharmacist which does restrict the level of professional services that can be deployed to patients. But this hasn’t held the pharmacy back on their implementation of Pharmacy Practice Incentive Program services. Are you QCPP ready? ‘I am most proud of our responsiveness to implementing new PPI processes. Each time we get a new info pack or manual updates we are onto them and ensure they are integrated straight away. It doesn’t make sense for us to just leave the pack unopened and to sit on them until assessment time.’ While Mary wasn’t involved in the initial implementation of QCPP at Leschenault Pharmacy, she has been involved with implementation at other pharmacies. A task which Mary says is very daunting when you first open the Requirements Manual, but if compiled into its individual components, or Elements, is not as bad as first thought. And there are some barriers to being a regional pharmacy, but the dedication of Mary and the WA QCPP Team overcame those obstacles. ‘The implementation officer came and went through our evidence and pointed out what needed to be updated. Just something as simple as sticking notes on documents we needed to look at really helped. Remembering to use version control really helped too,’ Mary said. ‘But being able to get things electronically and by email really helped us. There is so much on the web now days to help with our services.’ Visit the QCPP Knowledge Centre at APP2014 from 14-16 March, to get valuable assistance to help you meet QCPP requirements to become eligible to access PPIs. QCPP State Managers and experts will be available to provide hands on advice for all things QCPP and PPI. Visit the QCPP Knowledge Centre at stand 42 from Friday 14 March to secure your one-on-one session. Excellence January/February 2014 14 THREE REPORTS — ONE BIG FUTURE FOR PHARMACY Andrew Matthews – National Director, Quality Assurance and Standards Every now and then, it’s a good idea to polish up the crystal ball and look into the future. The recent release of three important reports has made the future for QCPP and the pharmacy profession a little clearer. It’s exciting — but only if we are prepared to make necessary changes. Our network of over 5300 community pharmacies in metropolitan, regional and rural/ remote areas of Australia ensures the delivery of medicines and other vital health services to all Australians. Yet compared to some other countries, our role in delivering primary care has been limited. Community pharmacy has the capacity to do more, and can do more. The Royal Pharmaceutical Society ‘Now or Never — shaping pharmacy for the future’ 1 report highlights that pharmacists and community pharmacy can offer far more than just medicines. i A high street presence and long opening hours mean that community pharmacy has the potential to play a crucial role in new models of out-of-hours primary and urgent care. The report discusses models of care which put pharmacy at the forefront of keeping people healthy and meeting common health needs. In England, like Australia, such models of care have already been pioneered and proven. Some pharmacies such as our Pharmacy of the Year winners are important examples of good practice, and demonstrate that pharmacy can help the health and social care system achieve more for less. The independent Chair of the Commission on future models of care delivered through pharmacy which led to the report was Dr Judith Smith, Director of Policy at the Nuffield Trust. Dr Smith is a guest speaker at the 2014 APP Conference. i Quality Care Pharmacy Program 15 But recent Guild surveys show that whilst we are offering a broad range of ‘ad-hoc’ services in response to population needs, these services are delivered in an uncoordinated approach across the community pharmacy network. QCPP as a quality management tool drives pharmacy to deliver services to a quality standard. But we need to do better to build consistency, quality and coordination to ensure a case for consistent fee for service funding. Pharmacy also needs to ensure services are integrated with other health professionals - so care is seamless. A key recommendation for pharmacists from the report is that pharmacists and their employers must recognise the imperative to shift their focus away from dispensing and supply of medicines towards providing a broader range of services. better utilise pharmacists’ skills. With the agreement of GPs and patients, pharmacists should be able to provide repeat prescriptions to people with simple, stable conditions. They should also be able to provide vaccinations and to work with GPs to help patients manage chronic conditions. The proposals in the report apply specifically to seven rural areas with the worst shortages of GP services. Whilst the report doesn’t focus on just expanded roles of pharmacy only, it demonstrates changes could be in place within five years. If adopted in 2011–12, the proposals would have resolved the worst shortages for just $30 million. The costs would mostly have been offset by fewer, or less costly, hospitalisations as a result of better population health. A lesson for all health services and accreditation bodies is the public enquiry into the Mid-Staffordshire NHS Foundation Trust by Robert Francis QC3 . It was an enquiry into the The report comments that in England, there is insufficient public awareness of the range of services pharmacists can offer. There is a pressing need to de-mystify pharmacy so that patients, the public and the rest of the health service understand the extent of the role that pharmacists do and can have in providing direct care. This is probably true for Australia too. That’s why one of the Pharmacy Guild priorities is focusing on enhancing and marketing the value of community pharmacy. Stafford Hospital in Staffordshire, a county in the West Midlands region of England. It tells the appalling story of unnecessary suffering of hundreds of people, failed by a system which ignored the warning signs and put corporate self-interest and cost control ahead of patients and their safety. Whilst an accredited health service, the misguided focus was on reaching targets, achieving financial balance and seeking foundation trust status at the cost of delivering acceptable standards of care. The Trust Board did not listen sufficiently to its patients and staff or ensure the correction of deficiencies brought to the Trust’s attention. It did not tackle the tolerance of poor standards and the disengagement of senior clinical staff from managerial and leadership responsibilities. Another important publication has been the Grattan Institute It brings out the importance that healthcare accreditation ‘Access all areas — new solutions for GP shortages in rural Australia’ 2 report . It recognises that pharmacists are highly trained, have expertise in medicines, and that the community pharmacy network means we are located broadly in communities throughout Australia. The report acknowledges that the Australian health system, especially in rural areas, can standards are ultimately in place to adequately test the quality of care being provided to patients. Standards and methods of ensuring compliance need to be focused on the effect of service deficiencies on patients and poor standards should not be tolerated because of the consequent risk to patients. References 1 Royal Pharmaceutical Society. Now or Never: Shaping pharmacy for the future. Available at: www.rpharms.com/models-of-care/report.asp Grattan Institute. Access all areas: new solutions for GP shortages in rural Australia. Sept 2013. Available at: http://grattan.edu.au/publications/reports/post/access-all-areas-new-solutions-for-gp-shortages-in-rural-australia/ 2 3 Robert Francis QC. Mid Staffordshire NHS Foundation Trust Public Inquiry final report. Available at: www.midstaffspublicinquiry.com/report Excellence January/February 2014 16 REFRESHER TRAINING The following courses have been approved for Refresher Training since the November/December edition of Excellence. This approved list is correct at Thursday 5 December 2013. To see the complete list of currently approved activities go to www.qcpp.com/resources/training-requirements. Approved Duration Training Approval Period Format 30 mins 20/9/1319/9/15 Online Albalon Red Eye Allergy Learning Module 30 mins 22/10/1321/10/15 Online Zantac Learning Module 30 mins 12/11/1311/11/15 Online Gastro-Stop Learning Module Training Provider Contact Details and Notes Pharmacy Club (iLearning Group) www.pharmacyclub.com Contacting QCPP Phone 1300 363 340 Website www.qcpp.com QCPP STATE MANAGERS ACT Lisa Gibbons 02 6270 8900 NT Kylie Clark 08 8944 6900 SA Gillian Starr 08 8304 8300 VIC Natalie Law 03 9810 9999 NSW Belinda Nankivell 02 9467 7100 QLD Nicole Floyd 07 3831 3788 TAS Sally Davis 03 6220 2955 WA Cathie Marshall 08 9429 4154 Supporting Excellence in Pharmacy Thank you to Craven’s Pharmacy, Perth, WA; Gerald Burns Pharmacy, Bicton, WA; Lim’s Pharmacy, Springvale, VIC; for their participation in the photography. QCPP is committed to adopting environmentally friendly practices and chooses to print Excellence on 100% recycled paper. Thank you to Chemmart® Pharmacy Superstore Eaton, WA; Cape York Guardian Pharmacy, QLD; Martin’s Chemist, NSW; and Orana Mall Pharmacy, NSW for their participation in the photography. QCPP is committed to adopting environmentally friendly practices and chooses to print Excellence on 100% recycled paper.
© Copyright 2026