Provincial Physician Assessment Program Sponsor Manual Practice Readiness Assessments
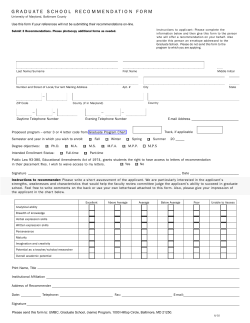
Provincial Physician Assessment Program Practice Readiness Assessments Sponsor Manual 1.0 Description and Purpose 2.0 Applicants 3.0 Clinical Objectives 4.0 Responsibilities of Applicants 5.0 Responsibilities of Assessors and Practice Supervisors 6.0 Responsibilities of Sponsors 7.0 Qualities of Assessors and Practice Supervisors 8.0 Practice Readiness Assessment Agreements 9.0 Provincial Payment Rates 10.0 Assessor Training Schedule A: Sample Sponsorship Form Schedule B: Sample Preliminary Clinical Assessment Report (CBAS-CPSA) Schedule C: Sample Supervised Practice Assessment Report Schedule D: Sample Chart Review & Chart Stimulated Recall Worksheet and instructions Practice Readiness Assessments: Sponsor Manual Updated July 15, 2014 Page 1 1.0 DESCRIPTION & PURPOSE To qualify for an assessment, applicants must first apply through Registration for a practice permit. Physicians who do not meet the full requirements of the General Register must undergo and successfully pass a practice readiness assessment prior to obtaining a practice permit on the Provisional Register. There are two unique components to a practice readiness assessment, and most, but not all, physicians (see below for exceptions) must undergo and successfully pass both components: 1. Preliminary Clinical Assessment: The applicant (candidate) is placed in the practice setting of an approved assessor, who assesses the applicant’s clinical competence through direct observation. The College determines the duration of the preliminary clinical assessment based on the applicant’s qualifications. The typical duration of this assessment is three (3) months. *In some cases, the College may elect to waive the preliminary clinical assessment (e.g. some U.S. applicants, applicants with previous practice experience in a Canadian setting, distinguished applicants appointed to full-time academic positions, Canadian-trained applicants who have not passed the national certification exams, etc.). 2. Supervised Practice Assessment: For a supervised practice assessment, the applicant acts as the most responsible physician in his or her own practice and bills for services provided. An approved assessor visits on a regular basis and assesses the applicant’s clinical competence by reviewing charts, having case-based discussions with the applicant and providing multi-source feedback. The duration of a supervised practice assessment is typically three months. All applicants who do not meet the full requirements of the General Register must complete this assessment component. Capacity within Alberta’s two medical schools does not often support the performance of competency-based assessments on behalf of the College for physicians seeking a practice permit to practice independently. Consequently, community physicians, ideally with experience evaluating student physicians in a medicine practice settings, help conduct practice readiness assessments. The assessments are based on defined objectives, explicit performance standards and clear statements as to the competence achieved. A practice readiness assessment is only part of the information the College uses to reach a decision about an applicant's eligibility for registration. The mere completion of any assessment required by the College does not guarantee a practice permit will be issued. The possible outcomes of an assessment range from eligibility for registration, to registration with conditions, to denial of registration. A practice readiness assessment is not intended to be a training experience. Its purpose is to give applicants opportunities to demonstrate their core knowledge and proficiency in clinical skills, patient management and resource utilization in the family and specialty practice setting. The College's goal is to register only competent and effective practitioners. These and other standards set by the College help ensure Albertan's receive the best care our profession can offer. Practice Readiness Assessments: Sponsor Manual Updated July 15, 2014 Page 2 2.0 APPLICANTS Applicants for College-approved practice readiness assessments may be: 1. Graduates of foreign medical schools who have successfully completed a postgraduate program of medical training of at least 24 months duration outside of Canada containing four months of community-based primary care and a minimum of eight weeks each in three of the following: Pediatrics, Obstetrics and Gynecology, Surgery, and Internal Medicine. 2. Graduates of Canadian medical schools who have not successfully completed the national certification exam. 3. Physicians who seek to return to family or specialty medicine practice after three or more years away from clinical or family medicine. 4. Other physicians who are required by the College to demonstrate their fitness to practice medicine in this setting. 3.0 CLINICAL OBJECTIVES FOR A PRACTICE READINESS ASSESSMENT The clinical objectives identified in the assessment evaluation tools represent the College’s minimum expectation for independent practice. The objectives for a specific applicant may be modified after consultation between the applicant, the assessor and a Co llege designate who is familiar with the candidate's background and intended practice location. Where specific objectives cannot be met within the assessor's practice, the College may need to make other arrangements in consultation with the assessor. The applicant and the assessor/supervisor should review the objectives for the assessment at their first meeting. Assessment should be a dynamic activity, and objectives should be met and recorded throughout the assessment by 1-2 daily notes on e-CBAS. The assessor/supervisor is required to submit formal evaluation reports of the applicant's performance to the College at prescribed intervals (see 5.0 Responsibilities of Assessors/Supervisors). A copy of the final evaluation reports for the Preliminary Clinical Assessment and the Supervised Practice Assessment are included as Schedule A, Schedule B, Schedule C and Schedule D (respectively). Objectives must be observed to have been met or, in the case of the current tool for the preliminary clinical assessment, achieved through inference. Achieving an objective through inference means the assessor is highly confident of the candidate's competence as the result of discussion or observation of related objectives. Both the applicant and the assessor/supervisor should review and sign the evaluation reports before submitting them to the College. Signature by the applicant does not necessarily mean agreement with the findings but does mean he or she agrees the evaluation has been discussed with him or her. Practice Readiness Assessments: Sponsor Manual Updated July 15, 2014 Page 3 4.0 RESPONSIBILITIES OF APPLICANTS Preliminary Clinical Assessment: 1. The primary responsibility for demonstrating proficiency in patient care rests with the applicant. The applicant must be fully aware of the objectives of the preliminary clinical assessment and take the initiative to achieve them. 2. The applicant must respect the final authority of the assessor, whose primary responsibility is to his or her patient. The degree of independence afforded the applicant is decided by the assessor after consideration of the applicant's proficiency with the consent of the patient. The applicant is not registered for independent practice and must be under the supervision of the assessor at all times. 3. The applicant must integrate into the assessor's practice and function in accordance with the custom of the practice in matters such as hours of work, on-call responsibility and relationships with office staff and consultants. 4. The applicant must provide quality patient care commensurate with his or her level of training and recent experience. Applicants must ask for supervision in novel or complex cases, and in order to be observed achieving an objective. 5. The applicant must review all clinical work with the assessor at regular intervals, and seek and attend to feedback and any recommendations of the assessor. 6. The applicant is expected to discuss any difficulty in meeting any requirements or objectives of the preliminary clinical assessment with the assessor. In the event of disagreement between the applicant and the assessor with respect to the purpose or conduct of the preliminary clinical assessment, the applicant is expected to discuss the problem with the appropriate Assistant Registrar at the College. 7. The applicant must respect the assessor's evaluation of the applicant's performance and discuss any outstanding difference of opinion with the Assistant Registrar. The assessor's evaluation report is only part of the information used in reaching a decision about eligibility for registration. 8. The applicant must remain in good standing on the Provisional Register - Physician Undergoing Assessment at the College of Physicians & Surgeons of Alberta and carry adequate professional liability insurance throughout the assessment. Supervised Practice Assessment: 1. The primary responsibility for demonstrating proficiency in patient care rests with the applicant. The applicant must be fully aware of the objectives of the supervised practice assessment and take the initiative to achieve them. 2. The applicant is the most responsible physician whose primary responsibility is to his or her patient. The applicant must remain in good standing on the Provisional Register – Conditional Practice at the College of Physicians & Surgeons of Alberta and carry adequate professional liability insurance throughout the assessment. 3. The applicant will be visited in his or her office by the practice supervisor, initially on a weekly basis, to review charts, hold case-based discussions and provide advice on issues as they arise. The case reviews should include a broad cross section of medical conditions including chronic disease management and common presenting complaints. The practice supervisor will review Practice Readiness Assessments: Sponsor Manual Updated July 15, 2014 Page 4 and discuss between five and 10 charts per visit. Each visit is expected to take approximately two hours. 4. The applicant is expected to discuss any difficulty in meeting any requirements or objectives of the supervised practice assessment with the practice supervisor. In the event of disagreement between the applicant and the supervisor with respect to the purpose or conduct of the supervised practice assessment, the applicant is expected to discuss the problem with the appropriate Assistant Registrar at the College. 5. The applicant must respect the practice supervisor's evaluation of the applicant's performance and discuss any outstanding difference of opinion with the Assistant Registrar. The practice supervisor's evaluation reports, which will be submitted to the College, are only part of the information used in reaching a decision as to eligibility for registration. 5.0 RESPONSIBILITIES OF ASSESSORS/SUPERVISORS Preliminary Clinical Assessment: 1. Concerns or inquiries regarding the applicant's progress in the preliminary clinical assessment should be directed to the appropriate Assistant Registrar of the College. 2. The assessor shall immediately report any issues of significant concern (i.e. patient safety) to the appropriate Assistant Registrar or Senior Medical Advisor. 3. Although the primary responsibility for meeting the objectives of the preliminary clinical assessment rests with the applicant, the assessor is expected to facilitate the applicant’s completion by providing opportunities to manage patients in the practice setting in accordance with the objectives of the preliminary clinical assessment and the applicant's level of proficiency. 4. At the start of the preliminary clinical assessment, the assessor and the applicant are expected to establish an assessment agreement based on the objectives. 5. Assessors should always be available for interaction with the applicant, both for advice and for evaluation of proficiency. The applicant is not registered for independent practice and must be under the supervision of the assessor at all times. 6. Assessors must review the applicant's clinical work at regular intervals and provide immediate feedback and recommendations. Feedback is most useful when it consists of what observed behaviors were effective and what behaviors need improvement. Expectations to enter 1-2 assessment notes a day in e-CBAS. 7. Assessors or their office staff are expected to inform patients of the applicant's status within the practice and seek their consent to be seen by the applicant. 8. Any difficulties encountered in completing the evaluation reports should be reported to the appropriate Assistant Registrar or Senior Medical Advisor immediately. 9. Assessors are required to complete and submit eCBAS evaluation reports to the College at the following prescribed intervals: • Three (3) -Month Preliminary Clinical Assessment: o Interim Evaluation Report must be completed and submitted to the College six (6) weeks after the assessment has commenced, and Practice Readiness Assessments: Sponsor Manual Updated July 15, 2014 Page 5 o Final Evaluation Report must be completed and submitted to the College within one (1) week following conclusion of the assessment. Supervised Practice Assessments: 1. Concerns or inquiries regarding the applicant's progress in the supervised practice assessment should be directed to the appropriate Assistant Registrar of the College. 2. The practice supervisor shall report any issues of significant concern (i.e. patient safety) immediately to the appropriate Assistant Registrar or Senior Medical Advisor. 3. The practice supervisor shall conduct regular office visits to the applicant to review between five and 10 charts, hold case-based discussions, obtain feedback on the applicant from staff and colleagues, and provide advice on issues. It is anticipated that each office visit could take approximately two hours of time. 4. The case reviews should include a broad cross section of medical conditions including chronic disease management and common presenting complaints. Assessment of the charts will be documented on a “Chart Review & Chart Stimulated Recall Worksheet” 10-15 CSRW must be submitted to the College before the 6 week mark. (see Appendix D for instructions and template). 5. Following sufficient interaction between the supervisor and the applicant of no less than one month, the practice supervisor may, at his or her discretion, reassess the frequency of the office visits. Completion of any further Chart Review & Chart Stimulated Recall Worksheets is also at the discretion of the assessor in the case where the records have been found to be satisfactory after the review of a minimum of 15 charts. 6. Practice supervisors are required to complete and submit evaluation reports to the College as well as all completed Chart Review & Chart Stimulated Recall Worksheets at the following prescribed intervals: • Interim Evaluation Report and Worksheets (10-15) must be completed and submitted to the College six (6) weeks after the assessment has commenced, and • Final Evaluation Report and Worksheets must be completed and submitted to the College within one (1) week following conclusion of the assessment. 6.0 RESPONSIBILITIES OF SPONSORS • • The Sponsor will complete the Sponsorship form (See Schedule A) confirming direct sponsorship for the Applicant to go through a practice-readiness assessment by the College for consideration for registration; In the event that the Sponsor is not Alberta Health Services, shall obtain and provide to the College a letter of support from Alberta Health Services for the registration of the Practice Readiness Assessments: Sponsor Manual Updated July 15, 2014 Page 6 • • Applicant on the Provisional Register for the purpose of providing professional services to the benefit of the Sponsor; and Shall render payment for any invoices related to their direct sponsorship of the Applicant in the practice-readiness assessment by the College within 90 days of receipt of such invoice or will be required to pay the current charge for late payments in place at the College. The Sponsor will keep the College informed of any changes in the Applicants status. This includes changes to potential start dates, visa status changes or delays and any other information that will affect the start or completion on an assessment. 7.0 QUALITIES OF PRACTICE READINESS ASSESSORS/SUPERVISORS Practice readiness assessors and supervisors must: • • • • • • • 8.0 be a respected clinician, have an appreciation of the privilege of self-regulation and all that entails, have broad knowledge of Canadian health care and experience in a variety of health care settings, Have a minimum of three years of active registration in Alberta be a member in good standing with the College, possess common sense, the ability to be objective and make firm decisions Previous experience teaching and assessing residents and other medical learners is an asset. PRACTICE READINESS ASSESSMENT AGREEMENTS Agreement(s) between the College and the preliminary clinical assessor and/or practice supervisor will be put in place to formalize the assessor/supervisor’s engagement in the completion of a practice readiness assessment. These Agreements help clarify the respective relationship between the physician assessors and the College, and identify related expectations and payment rates. In general, the agreement(s) will accomplish the following: • • • • Establish a clear reporting relationship between the College and the assessor/supervisor, Outline provincial compensation rates for practice readiness assessors (preliminary clinical assessors and/or practice supervisors), Outline indemnification for practice readiness assessment work undertaken on behalf of the College by the assessor, and Encompass a conflict of interest and confidentiality agreement signed by the assessor/supervisor. In order for the College to indemnify and pay the Assessor a signed agreement must returned to the College. Practice Readiness Assessments: Sponsor Manual Updated July 15, 2014 Page 7 9.0 PROVINCIAL PAYMENT RATES (subject to change) A. Preliminary Clinical Assessor: • One thousand six hundred fifty dollars ($1,650) per week for the duration of the assessment: o Three-month Assessment = $19,800 total B. Supervised Practice Assessor: • Hourly rate based on the current College policy around per diem compensation ($125/hour) to a maximum of 15 hours over the duration of the full three-month assessment The sponsor is required to reimburse the College for the total costs of the practice readiness assessor fees and for the College’s applicant PPAP administrative fee. (The 2014 PPAP administrative fee is $3,500+GST/applicant; check the College’s website for updated payment rates and administrative fees at http://www.cpsa.ab.ca/Services/ace/practicereadiness/requirements.aspx) 10.0 PRACTICE READINESS ASSESSOR SUPPORT Each year the College provides new assessors with formal training that focuses on introducing them to the assessment tools, expectations of the assessor role, etc. After initial training, the Senior Medical Advisor, Assessment & Competency Enhancement, or delegate provides assessors with ongoing support for advice and assistance as the need arises. In addition, annual educational workshops are also held to enhance skills, and to gather feedback from the assessors/supervisors on the assessment tools and related processes associated with practice readiness assessment in Alberta. Practice Readiness Assessments: Sponsor Manual Updated July 15, 2014 Page 8 SCHEDULE A Physician Sponsorship SPONSOR INSTRUCTIONS: SA M PL E 1. Please fully read and complete this form 2. Review the Applicant’s Eligibility Letter issued by the College of Physicians & Surgeons of Alberta (CPSA) 3. Forward the completed form to both: • The CPSA Registration Department to identify your Sponsorship ([email protected]) • Alberta Health Services (if the Sponsor is NOT Alberta Health Services), Zone Medical Director’s office in your zone, to request their support APPLICANT DETAILS: Applicant’s Last Name: ______________________ Applicant’s Given Name(s): ______________________ CPSA tracking number: ______________________ Discipline the applicant is being sponsored to practice in: ______________________ Does the applicant’s intended practice match what is outlined in the CPSA Eligibility Letter? Yes No The applicant requires (as outlined in the applicant’s CPSA Eligibility Letter): Preliminary Clinical Assessment of approximately 3 months and a Supervised Practice Assessment of approximately 3 months Supervised Practice Assessment of approximately 3 months only Specific location where applicant will practice following a successful assessment (e.g., Clinic name and address, solo or group practice): Type(s) of practice the applicant will work in: (check all that apply) Clinic/Office Walk-In Clinic setting Long Term Care In-Patient Setting Update July 9, 2014 Acute Care In-Patient Setting Emergency Department Other:________________________ Supporting Documents / Physician Sponsorship SPONSOR DETAILS: Sponsors are required to sign an agreement with the CPSA identifying both parties' responsibilities as well as the Provincial Physician Assessment Program (PPAP) fees that the sponsor is responsible for paying Applicant is being sponsored by (check only one): Alberta Health Services: Zone: ____________________________ E Covenant Health Corporate Clinic in Alberta Private clinic in Alberta SA M PL A currently registered physician in Alberta with active independent license Other (specify): __________________________________________ Sponsor’s full contact information (if not AHS): Address: _______________________________________________ Phone: _________________________________________________ Fax: ___________________________________________________ Email: _________________________________________________ Signing Authorities: ______________________________________ Sponsor’s CPSA registration number (if applicable): ____________________________ Anticipated start date applicant is able to commence the assessment: ______________________ (Note: This is not a guaranteed start date) (dd/mmm/yyyy) Sponsor’s Last Name: ______________________ Sponsor’s Given Name(s): ______________________ Sponsor’s signature: ______________________________________ Update July 9, 2014 Date signed: ___________________ Supporting Documents / Physician Sponsorship SA M PL E SCHEDULE B SCHEDULE C Provincial Physician Assessment Program FINAL - Supervised Practice Assessment CPSA: Number Consider all competency components under each Primary Competency Category (PCC) before assigning overall assessment rating. Process ID: Number Check appropriate assessment rating below (Double Click to type) PCC: HISTORY TAKING Provide documentation to support those competency components that need improvement. 1. Key historical features of the presenting complaint are documented. SATISFACTORY UNSATISFACTORY 2. Problem labels or diagnoses are documented and those with ongoing implications for future care are readily identifiable at future visits. 3. Significant past medical history (e.g. major diseases, major surgical procedures, results of significant investigations) is available. 4. Allergies are readily identifiable. 5. A list of active medications is available. 6. Relevant prevention and health promotion issues are documented. SA O M N P O L T E U SE GENERAL COMMENTS: Consider all competency components under each Primary Competency Category (PCC) before assigning overall assessment rating. Check appropriate assessment rating below (Double Click to type) PCC: PHYSICAL EXAMINATION & TECHNIQUES Provide documentation to support those competency components that need improvement. 1. Physical findings are documented. SATISFACTORY UNSATISFACTORY 2. Evidence of examining patients in a manner which is focused on determining the presence or absence of relevant clinical signs, and which is appropriate to the context of the visit. GENERAL COMMENTS: Consider all competency components under each Primary Competency Category (PCC) before assigning overall assessment rating. Check appropriate assessment rating below (Double Click to type) PCC: DIAGNOSTIC AND PROBLEM DEFINITION Provide documentation to support those competency components that need improvement. SATISFACTORY UNSATISFACTORY 1. Evidence is documented of a search for the root cause. 2. Evidence of appropriate clinical reasoning. D 3. Evidence of a differential diagnosis that is based on an interpretation and prioritization of related history, physical examination and investigation. 4. Considerations of relevant psychological, social and lifestyle issues are evident. GENERAL COMMENTS: Version 2 - March 28, 2011 Document Name: Assessment - Supervised Practice Interim Report 1 of 3 Provincial Physician Assessment Program FINAL - Supervised Practice Assessment CPSA: Number Consider all competency components under each Primary Competency Category (PCC) before assigning overall assessment rating. Process ID: Number Check appropriate assessment rating below (Double Click to type) PCC: COMMUNICATION/RELATIONSHIP SKILLS Provide documentation to support those competency components that need improvement. SATISFACTORY UNSATISFACTORY 1. Communicates clearly and is easily understood by patients and their families, office staff and colleagues. 2. Demonstrates respect for patients and their families, office staff and colleagues. 3. Demonstrates an understanding of the key components of patient/family communication. 4. Interacts collaboratively with other physicians. GENERAL COMMENTS: Consider all competency components under each Primary Competency Category (PCC) before assigning overall assessment rating. Check appropriate assessment rating below (Double Click to type) SA O M N P O L T E U SE PCC: INVESTIGATION AND MANAGEMENT Provide documentation to support those competency components that need improvement. SATISFACTORY UNSATISFACTORY 1. Investigations, referrals and treatment (including name, dosage and quantity of prescriptions) are documented. 2. Uses diagnostic and treatment resources appropriately. 3. Advises on/prescribes medications appropriately. 4. Makes appropriate use of consultants and allied personnel. 5. Evidence of providing education to patients and families, and of enlisting their participation in the management plan. GENERAL COMMENTS: Consider all competency components under each Primary Competency Category (PCC) before assigning overall assessment rating. Check appropriate assessment rating below (Double Click to type) PCC: MEDICAL KNOWLEDGE Provide documentation to support those competency components that need improvement. SATISFACTORY UNSATISFACTORY 1. Management choices adhere to practice standards or variance is explained. D 2. Ongoing and preventative care can be referenced to specific sources of information (e.g. evidence-based literature) when asked. GENERAL COMMENTS: Consider all competency components under each Primary Competency Category (PCC) before assigning overall assessment rating. Check appropriate assessment rating below (Double Click to type) PCC: PUBLIC HEALTH, MEDICO-LEGAL, ETHICAL Provide documentation to support those competency components that need improvement. 1. Evidence of compliance with the CMA Code of Ethics. SATISFACTORY UNSATISFACTORY 2. Documented awareness of, and attention to public health and social issues. 3. Evidence of informed consent obtained where appropriate. 4. Demonstrates evidence of “duty to report” in circumstances that present a danger to others (communicable diseases, child abuse, etc.). GENERAL COMMENTS: Version 2 - March 28, 2011 Document Name: Assessment - Supervised Practice Interim Report 2 of 3 Provincial Physician Assessment Program FINAL - Supervised Practice Assessment CPSA: Number Process ID: Number Consider all competency components under each Primary Competency Category (PCC) before assigning overall assessment rating. Check appropriate assessment rating below (Double Click to type) PCC: FOLLOW-UP Provide documentation to support those competency components that need improvement. SATISFACTORY UNSATISFACTORY 1. Arrangements for follow-up are documented (for all chronic problems and for acute problems, when necessary). 2. A system is in place to ensure follow-up of critical issues, results and/or reports. GENERAL COMMENTS: Consider all competency components under each Primary Competency Category (PCC) before assigning overall assessment rating. Check appropriate assessment rating below (Double Click to type) PCC: PROFESSIONALISM Provide documentation to support those competency components that need improvement. SATISFACTORY UNSATISFACTORY Sources of information include: _________ Chart Audit _________ Formal Discussion _________ Direct Observation SA O M N P O L T E U SE 1. Demonstrates the ability to recognize own limitations and gaps and seek out appropriate resources-reading, electronic, consultation. 2. Demonstrates responsibility for continuing care of patients and, when appropriate, for transfer of care of patients to another physician. GENERAL COMMENTS: _________ Interviews with Peers _________ Interviews with Non-Physician Coworkers _________ Other:____________________________________________________________ The following signatures acknowledge that this evaluation report, which has been completed by Dr. Practice Supervisor for Dr. Applicant, has been reviewed prior to submission to the College of Physicians & Surgeons of Alberta by the following individuals: APPLICANT Signature D Print Name Date PRACTICE SUPERVISOR Signature Print Name Date Please submit signed and completed evaluation report to: Provincial Physician Assessment Program College of Physicians & Surgeons of Alberta 2700, 10020 – 100 Street NW Edmonton, AB T5J 0N3 Fax: (780) 420-0651 Email: [email protected] Version 2 - March 28, 2011 Document Name: Assessment - Supervised Practice Interim Report 3 of 3 SCHEDULE D Supervised Practice Assessment Chart Review and Chart Stimulated Recall Introduction Applicants have already demonstrated that they have the requisite medical knowledge, skills and attributes to practice as the most responsible physician on the Provisional Register as a result of successfully completing the preliminary clinical assessment component of a practice readiness assessment. Alternatively, the College may have waived the requirement for the preliminary clinical assessment as it is believed that the applicant already possess sufficient training and/or experience such that these conditions have been met. In either situation, the purpose of the supervised practice assessment is to assess whether an applicant is continuing to demonstrate good medical practice in his/her own practice setting in the role of the most responsible physician. As opposed to the preliminary clinical assessment, direct observation is not the method of assessment for the supervised practice component. Assessment in this component is achieved through chart review, chart stimulated recall and through interviews with an applicant’s colleagues or staff. The Interim and Final assessment reports for the supervised practice assessment have already been provided for reference (see Appendix B in the PPAP Information Manual – Section 1). The College has also prepared the following additional tools for use while the supervisor performs each supervised practice visit; Chart Review Guide, Chart Stimulated Recall Interview Guide and the Chart Review and Chart Stimulated Recall Worksheet (attached). The Chart Review Guide is intended to assist the supervisor to evaluate the applicant’s competence as evidenced in the charts, while the Chart Stimulated Recall Interview Guide is intended to assist the supervisor formulate questions to ask the applicant in order to gain information not readily apparent in the chart. The Chart Review and Chart Stimulated Recall Worksheet acts as a means to document the supervisor’s findings following the chart review and the subsequent discussions with the applicant. The supervisor is asked to judge the quality and organization of the chart notes, and in doing so, to look for internal consistency (for example, are historical problems followed through with appropriate examinations and investigations?) and for discordances (for example, does the assessment align with the history and physical findings?). Finally, the supervisor is asked to engage in case-based discussions that probe the applicant’s medical knowledge, and clinical decision making and judgment. Applicant – Supervisor Practice Visits Supervisors are expected to meet regularly with the applicant over the course of the assessment. Prior to each visit or at the beginning of each visit, the supervisor should request between 5-10 charts be made available for his/her review to provide the basis for the chart stimulated recall. The chart reviews should involve a broad cross section of medical conditions including chronic disease management and common presenting complaints. Once the supervisor has reviewed the cases and completed the associated worksheets, he/she should arrange to meet with the applicant to conduct chart stimulated recall. The supervisor should begin the discussion with open ended questions to reduce bias and to provide insight into the applicants thought processes. The questions should be asked in a nonjudgmental, non biased approach and the supervisor should be prepared to provide advice and feedback to the applicant throughout the supervised practice visit. Questions related to professionalism can be included in the discussion. Notes captured on the worksheets should be kept by the supervisor after each visit to assist with completion of either the Interim or Final Progress Report for submission to the College at the designated intervals. These notes will provide support to substantiate the associated evaluation results through concrete examples gathered from each of the supervised practice visits and can be valuable in the event that an assessment finding is ever challenged by an applicant. Note: Any worksheets or notes completed over the course of the assessment relating to an applicant must be submitted to the College with the assessment reports following completion of the Supervised Practice Assessment. Supervised Practice Assessment – CSR Interview Guide Supervised Practice Assessment – Chart Simulated Recall Interview Guide A. B. Individual Visit Questions 1. General – “Please tell me about this visit.” [Alternative: “Please outline your approach to the presenting complaint and highlight the key points.”] 2. Clinical Assessment – “What specific features led you to this diagnosis or clinical impression?” Were there any other conditions that you ruled out?” 3. Investigations and Referrals - “What specific features led you to the investigations/referrals you chose?” Were there any other investigations/referrals that you thought about, deferred or ruled out? 4. Treatment - “What specific features led you to the management you chose?” “Were there any other treatments that you thought about, deferred or ruled out?” [Alternative: “I note that you ordered ‘XYZ’. What factors influenced your choice?” “Were there any other medications you considered?” 5. Follow-up - “Do you recall if there was a decision about follow-up?” “What were the factors that influenced your decision?” 6. Patient Factors - “Patient characteristics sometimes influence decision-making. Was there anything special about this patient that influenced your decisions regarding management? (e.g. psychosocial issues, compliance, past medical history, current medications, support systems, employment)”. “On reflection, is there anything about this patient you wish you knew more about?” 7. Practice/System Factors - “Is there anything special about your practice setting that influenced your management in this case? (e.g. a nurse educator, lack of access to laboratory or x-ray)”. “On reflection, what changes would improve your ability to deliver care to this patient?” Broader Practice Issue Questions 1. Getting Timely Answers To Clinical Questions Purpose: To determine the physician’s awareness and processes to find reliable/current clinical information. When you don’t know the answer to a clinical question, what do you do to get a timely answer? Do you use the Internet/reference books/journals to search for clinical information? Are those sources serving your needs? Tell me about a particularly challenging patient where you needed urgent knowledge and could not contact a colleague. What additional resources would help you to find timely answers to clinical questions? A strong response will indicate use of multiple sources (web-based; paper resources; colleague support); will indicate openness to new sources and methods; and is willing to adapt to available resources. Page 2 Supervised Practice Assessment – CSR Interview Guide 2. Use Of Optimal Office Systems Purpose: To determine the physician’s awareness of the impact of office processes on patient care and provider satisfaction. What frustrates you about your office practice? Which systems in your office for management of people, paper and patients work well? Which don’t? o How well is intra-office communication working? o How well is inter-office communication working? o How up-to-date and readily available are your medical records? o How are third party requests for reports being handled? How can they be handled better? o How are phone calls managed (to front desk/ to physician)? What works and what isn’t? o How is follow-up of lab results/ notification of patients handled? How well is that working? What are the barriers to improving office functioning? What problems/barriers are office issues versus health system issues? A strong response will indicate awareness of the strengths and weakness in the office; will acknowledge responsibility for it; and will have processes to adjust as problems are identified. 3. Utilizing Illness Prevention Strategies Purpose: To determine the physician’s capacity and commitment to health promotion / risk reduction strategies. How do you see your role in promoting healthy lifestyles? What health promotion / risk reduction strategies do you use in your practice? How do you / how often do you encourage lifestyle modification? How do you / how often do you address smoking, weight management, exercise, alcohol and other risk factors in disease management? What screening tests do you recommend for (disease: e.g. diabetes) (age- and sex-specific populations)? A strong response will indicate responsibility for promoting healthy living among patients; will demonstrate (document in the record) a routine implementation of established preventive interventions (preferably in a flow sheet or summary page) and have reminder systems in place; will demonstrate routine questioning about risk factors; will have written material for patients; and will identify frequently used resources in the community to assist patients with these factors. 4. Empowering Patients In Self-Care Purpose: To determine the physician’s commitment to promoting and facilitating patients’ active participation in their care. How do you encourage patients to take responsibility for their care? How do you facilitate their active participation in care plans? What written information do you provide to your patients? Do you help your patients set targets/goals for improvement? Do you use homework assignments for patients? Do you refer patients to community resources to assist in reaching goals? A strong response will indicate commitment to achieving a partnership with the patient in a treatment plan; will provide written material or refer to resources available; will offer treatment choices to patients; will assign homework and will assist the patient to set goals; will measure successes. Page 3 Supervised Practice Assessment – CSR Interview Guide Supervised Practice Assessment - Chart Review Guide (Evidence of Care Provided) ITEMS a) Do the recorded history and physical findings support the problem or diagnosis? Yes, if: there is evidence of any elaboration of the presenting complaint and evidence of examination, when appropriate, of: the offending part, an organ system, including features to distinguish the seriousness of the problem, and vital signs. Yes, if: I, as a colleague, could take over care of this patient safely without having to talk to the doctor. Comment if important history is not evident (e.g. the features of a chest pain; the cause of an injury; suicidal ideation in a case of depression; the features that distinguish among important diagnoses.) b) Are problems or diagnoses recorded in the chart? Yes, if: problem labels (e.g. hip pain) or diagnoses (e.g. osteoarthritis) are recorded. Comment if patients’ undifferentiated complaints are simply restated without evidence of being defined by the physician (e.g. chest pain without history or physical examination or apparent attempt to characterize the pain). Comment if major medical problems are overlooked. c) Do x-rays and laboratory tests support the problem or diagnosis? Yes, if: investigations ordered reflect modern choices for laboratory and imaging studies AND are sufficient in each case to assess a problem or diagnosis. They may or may not be noted in the visit record. d) Are abnormal findings or results properly followed-up? Yes, if: appropriate action is taken on abnormal findings on laboratory and imaging studies (i.e. advice, further investigation, treatment) e) Are the names, dosages and quantities of prescribed medications recorded? Self-explanatory. f) Are treatments, referrals and other interventions recorded and appropriate? Yes, if: advice or management strategy is recorded. g) Are plans for follow-up recorded when follow-up is important? Yes, if: there is evidence of responsibility being taken for monitoring the course of an injury or illness, or the effect of advice or treatment. Page 4 Please copy this form as many times as needed Supervised Practice Assessment – Chart Review & Chart Stimulated Recall Worksheet Applicant Name: __________________________ Applicant CPSA No._______________________ Examples where the clinical record raises questions about: responses to abnormal findings; evidence for diagnoses; choices of investigations or treatments; or diligence of follow-up. Record either chart ID #, or the combination of patient initials and date of birth and recent date of visit. Do not record patients’ names. Chart ID#: OR Patient’s Initials: DOB: Date of Visit: Do the recorded history and physical findings support the problem or diagnosis? Yes No N/A (b) (c) (d) (e) (f) (g) Are problems or diagnoses recorded in the chart? Do x-rays and laboratory tests support the problem or diagnosis? Are abnormal findings or results properly followed-up? Are the names, dosages and quantities of prescribed medications recorded? Are treatments, referrals and other interventions recorded and appropriate? Are plans for follow-up recorded when follow-up is important? Yes Yes Yes Yes Yes Yes No No No No No No N/A N/A N/A N/A N/A N/A SA O M N P O L T E U SE (a) Field Notes & Chart Stimulated Recall (CSR) • • • D Impressions • • • Physician: ___________ Supervisor: ___________ Date: ___________ Monitoring & Compliance / Supervised Practice Assessment – Chart Review
© Copyright 2026