BEHAVIORAL HEALTH SERVICES
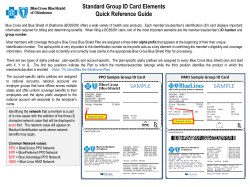
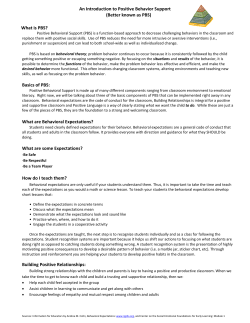
BEHAVIORAL HEALTH SERVICES TABLE OF CONTENTS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 461 OVERVIEW ...... . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .461 Exceptions ........ . . . . . . . . . . .Patients Referring . . . . . . . . .for . . . Behavioral . . . . . . . . . . . .Health . . . . . . . Services . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .461 ........ . . . . . . . . . . . . . with Contracting . . . . . .ValueOptions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .462 ........ . . . . . . . . . . .BEHAVIORAL EMBLEM . . . . . . . . . . . . . . .HEALTH . . . . . . . . . SERVICES . . . . . . . . . . . PROGRAM . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 462 ...... . . . . . . . . . . . . of Continuity . . .Care . . . . . During . . . . . . . . Program . . . . . . . . . .Implementation . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .463 ........ . . . . . . . . . . . . . . . .MANAGEMENT BEHAVIORAL . . . . . . . . . . . . . . . . . PROGRAM . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 464 ...... . . . . . . . .APPROVAL PRIOR . . . . . . . . . . . . REQUIREMENTS . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 464 ...... . . . . . . . . . Outpatient Routine . . . . . . . . . . . . Services . . . . . . . . . -. .No . . . Prior . . . . . . Approval . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .464 ........ . . . . . . . . . .Requiring Services . . . . . . . . . . .Prior . . . . . Approval . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .464 ........ . . . . . . . . . . . .Prior Obtaining . . . . . Approval . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .465 ........ . . . . . . .MANAGEMENT CASE . . . . . . . . . . . . . . . . . PROGRAM . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 465 ...... . . . . . . . . . . . . . . . CARE DEPRESSION . . . . . . .PATH . . . . . . DISEASE . . . . . . . . . . MANAGEMENT . . . . . . . . . . . . . . . . . .PROGRAM . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 465 ...... . . . . . . . . . . . . . . . .PRIMARY TEENSCREEN . . . . . . . . . . .CARE: . . . . . . .MENTAL . . . . . . . . . .HEALTH . . . . . . . . . CHECKUPS . . . . . . . . . . . . . FOR . . . . . TEENS . . . . . . . . . . . . . . . . . . . . . . . 466 ...... . . . . .Mental The . . . . . . . .Health . . . . . . . Checkup . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .466 ........ . . . . . .Primary Why . . . . . . . . .Care . . . . . Practitioners . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .466 ........ . . . . . .to How . . Get . . . . .Started . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .466 ........ . . . . . . . . . . HEALTH MENTAL . . . . . . . . . .PARITY . . . . . . . . AND . . . . . .ADDICTION . . . . . . . . . . . . . .EQUITY . . . . . . . . .ACT . . . . .OF . . . .2008 . . . . . .(MHPAEA) . . . . . . . . . . . . . . . . . . . . . . 468 ...... Back to Table of Contents EmblemHealth Provider Manual Last Updated: 09/03/2014 460 BEHAVIORAL HEALTH SERVICES In this chapter, you'll find our policies and procedures for mental health and substance abuse services, including: Prior approval procedures Post-discharge protocols Mental Health Parity Law OVERVIEW EmblemHealth has engaged ValueOptions® to administer behavioral health services for most of its members under two programs. Members of plans underwritten by GHI HMO, HIP and HIPIC, and administered by VHMS have their behavioral health services administered by ValueOptions under the Emblem Behavioral Health Services Program (EBHSP). Members of EPO/PPO plans underwritten by GHI have their behavioral health services administered by ValueOptions under the EmblemHealth Behavioral Management Program (BMP). Under EBHSP, ValueOptions administers all covered inpatient, outpatient and ambulatory behavioral health services and is responsible for provider network and care management services such as credentialing, claims processing, claims payment, utilization management, case management, grievances and appeals (except for Medicare plans), and all other provider service issues related to behavioral health. Under BMP, ValueOptions manages all covered inpatient, outpatient and ambulatory behavioral health services, including provider network and care management services such as utilization management and case management. All provider claims should be submitted to EmblemHealth, except those for Medicare members; these claims should be submitted to ValueOptions. All appeals and grievances should be submitted to ValueOptions, except for those of Medicare members; these appeals and grievances should be submitted to EmblemHealth. Exceptions Members who have the Montefiore logo in the lower left corner of their ID card These members access behavioral health providers in the Montefiore network. They also may use the ValueOptions network if they choose. For providers who are not Montefiore network participants, claims for members who have the Montefiore logo on their ID card must be submitted to ValueOptions. Utilization management functions for behavioral health services for these members, including prior approvals, are performed by Montefiore. (Please refer to the Your Plan Members chapter for examples of ID cards with the Montefiore logo.) EmblemHealth administers disease management, including the Depression Disease Management program, for all members. Referring Patients for Behavioral Health Services Providers must be contracted in the ValueOptions network(s) to provide covered behavioral health care to members served by BMP and EBHSP. Back to Table of Contents EmblemHealth Provider Manual Last Updated: 09/03/2014 461 BEHAVIORAL HEALTH SERVICES You and your patients are able to find EBHSP and BMP practitioners and facilities by going to the Find a Doctor tool of www.emblemhealth.com and entering the patient's ID number at the beginning of the search. Since some of our benefit plans use different networks, entering the patient's ID number will ensure that the search locates a provider that participates in the patient's benefit plan. Contracting with ValueOptions EBHSP To care for all members served by the EBHSP, providers are required to participate in both of the ValueOptions practitioner networks and must have both a ValueOptions practitioner agreement and a CHCS IPA agreement (collectively referred to as "ValueOptions Agreements"). Providers who only have a CHCS IPA agreement will only be permitted to provide in-network care to members of HIP HMO (including commercial, HIP Medicaid, HIP Family Health Plus, HIP Child Health Plus, and EmblemHealth Medicare HMO) and GHI HMO lines of business. Providers who only have a ValueOptions practitioner agreement will only be permitted to provide in-network care to members of HIPIC's EPO and PPO plans and VHMS ASO accounts. BMP To care for members served by the BMP, providers are only required to have a ValueOptions practitioner agreement. For more information about contracting with ValueOptions, please call their Provider Line at 1-800-397-1630 and ask to speak with the Credentialing department. EMBLEM BEHAVIORAL HEALTH SERVICES PROGRAM As of January 1, 2012, behavioral health services for members in plans underwritten by GHI HMO and HIP or in ASO plans administered by VHMS (as previously described in the "Overview") are administered by ValueOptions under the Emblem Behavioral Health Services Program. Benefit plans served by EBHSP include: EmblemHealth: EmblemHealth CompreHealth EPO EmblemHealth Medicare HMO plans (which includes Dual Eligible Group HMO SNP, Dual Eligible HMO SNP, VIP Essential HMO, VIP High Option HMO, VIP HMO, VIP Premier Group HMO and VIP Rx Carveout HMO) GHI HMO: GHI HMO GHI HMO Direct Access HMO GHI HMO Value Plan HIP: Direct Pay HMO/POS HIPaccess® I Back to Table of Contents EmblemHealth Provider Manual Last Updated: 09/03/2014 462 BEHAVIORAL HEALTH SERVICES HIPaccess® II HIP Prime® EPO/HMO/POS/PPO HIP Select® EPO/PPO Medicaid Managed Care Family Health Plus Child Health Plus FEHB Vytra HMO VHMS: ASO accounts Continuity of Care During Program Implementation For Patients in an Active Course of Treatment Prior to January 1, 2012 For dates of service prior to January 1, 2012, EmblemHealth was responsible for behavioral health services provided to HIP and VHMS members and Magellan Health Services was responsible for behavioral health services provided to GHI HMO members. Patients who are in an active course of treatment with a provider who has declined network participation in the EBHSP or has not completed the necessary application, credentialing and contracting processes with ValueOptions as of January 1, 2012 may elect to continue treatment with the provider for a period up to 90 days, so long as the provider accepts the applicable current fee schedule and follows the existing policies and procedures. This will support continuity of care until the member can find a new provider who can meet their needs. Routine Outpatient Care Providers who do not participate in the ValueOptions network(s) delivering routine outpatient behavioral health treatment do not need to obtain approval to provide routine outpatient care during the 90 day transition period. Non-routine Outpatient Care Providers must contact ValueOptions to obtain prior approval to deliver continuing non-routine outpatient care for dates of service beginning January 1, 2012. Alternative Level of Care (Partial hospitalization, Intensive Outpatient) If the patient is in an alternative level of care initiated or authorized by EmblemHealth or Magellan Health Services (as applicable) prior to the transition date and needs to continue that level of care after the transition date, the provider should contact EmblemHealth or Magellan Health Services (as applicable) for concurrent approval. Intensive outpatient behavioral health services will require a prior approval from ValueOptions for dates of service beginning January 1, 2012. Inpatient Care EmblemHealth and Magellan Health Services (as applicable) are responsible for medical management and for adjudicating claims for inpatient care initiated prior to the commencement of the EBHSP until the patient is discharged and/or moved to an alternate level Back to Table of Contents EmblemHealth Provider Manual Last Updated: 09/03/2014 463 BEHAVIORAL HEALTH SERVICES of care. At that point, responsibility for utilization and claims management will transition to ValueOptions. BEHAVIORAL MANAGEMENT PROGRAM Members of EPO and PPO plans underwritten by GHI have their behavioral health services (as previously described in the "Overview") administered by ValueOptions under the Behavioral Management Program (BMP). Benefit plans served by BMP include: EmblemHealth: EmblemHealth ConsumerDirect EPO/PPO EmblemHealth EPO/PPO EmblemHealth InBalance EPO/PPO EmblemHealth Medicare PPO plans (which includes Dual Eligible PPO, SNP, Group Access PPO, Group Access RX PPO, Medicare ASO accounts [GuildNet Gold and ArchCare], Medicare PPO I, Medicare PPO II, Medicare PPO III and PPO High Option) GHI: DC37 Med Team Program EPO/PPO Share Federal Employees Health Benefits Program (FEHB) GHI/CUNY Student Health Insurance Program H.E.R.E.I.U. Network Access NYCTA TWU PRIOR APPROVAL REQUIREMENTS In some cases, coverage of behavioral health services to a member served by EBHSP or BMP requires a prior approval before the service can be rendered. Members may be subject to a copay and/or deductible depending on their benefit plan. Routine Outpatient Services - No Prior Approval Prior approval is not required for routine outpatient services. These services include initial consultation and individual, group, family, couple and collateral treatment. ValueOptions will, however, reach out to practitioners when there are questions regarding the member's clinical treatment. Services Requiring Prior Approval Prior approval is always required for the following services: Inpatient behavioral health treatment Ambulatory detoxification treatment Outpatient ECT (electro-convulsive treatment) Partial hospitalization Back to Table of Contents EmblemHealth Provider Manual Last Updated: 09/03/2014 464 BEHAVIORAL HEALTH SERVICES Intensive outpatient treatment Neuropsychological testing Psychological testing Obtaining Prior Approval If you are a behavioral health provider and your patient is served by EBHSP or the BMP you must contact ValueOptions directly to obtain prior approval when necessary. Once ValueOptions approves the service, you must notify your patient of the approval. You must notify ValueOptions if you are unable to reach your patient (or his or her designee). The telephone numbers to contact for prior approval are: EBHSP: 1-888-447-2526 BMP: 1-800-692-2489 CASE MANAGEMENT PROGRAM The Case Management Program is administered by ValueOptions for all members (except for those with the Montefiore logo on their ID card). Patients who have the greatest risk of needing intensive behavioral health services including inpatient care are eligible for case management services. Patients are identified through multiple sources including provider referrals. An enrolled patient is assigned a case manager who will contact them, devise a treatment care plan and will work with their treatment provider(s) to assist with medication adherence and treatment plan compliance. The Case Management Program involves frequent telephonic counseling sessions between the case manager and patient to aid the patient in staying out of the hospital. To refer a patient to the Case Management Program, please call the Mental Health number on the back of the member's ID card. DEPRESSION CARE PATH DISEASE MANAGEMENT PROGRAM Any plan member who is receiving antidepressant medication and/or has a major depression diagnosis is eligible to participate in the Depression Care PATH (Positive Actions Toward Health) program, which is administered by EmblemHealth. The Depression Care PATH program provides educational resources and phone outreach to help your patient self-manage depression. Health coaches, who are licensed social workers, provide members with: Access to educational materials about depression Answers to frequently asked questions and concerns about depression Back to Table of Contents EmblemHealth Provider Manual Last Updated: 09/03/2014 465 BEHAVIORAL HEALTH SERVICES Assistance making appointments with mental health professionals Assistance coordinating care Coaching calls, including the importance of medication adherence Assessment of depression severity To refer a patient to the Depression Care PATH Program, call 1-800-447-0769. TEENSCREEN PRIMARY CARE: MENTAL HEALTH CHECKUPS FOR TEENS EmblemHealth participates in TeenScreen® Primary Care, an initiative that offers annual standard mental health checkups to adolescent patients through their primary care practitioners. Patients 11 to 18 years of age with GHI, GHI HMO, HIP or EmblemHealth coverage are eligible to participate in the program. TeenScreen Primary Care in an initiative of the National Center for Mental Health Checkups at Columbia University. The Mental Health Checkup The mental health checkup includes a brief questionnaire that patients complete in the waiting or exam room. The questionnaire can help evaluate if a teen is suffering from depression, anxiety or other condition. When the mental illness is identified early, teens have the best chance to lead healthy lives and reach their full potential. Why Primary Care Practitioners Primary care practitioners are in a unique position to help detect mental health conditions. According to the US Surgeon General, 21 percent of our nation's youth suffers from a diagnosable mental disorder that causes impairment, but 80 percent are not identified and do not receive help. Further, about two million teenagers are affected by depression; however, most of these teens go undiagnosed and untreated. Mental health screening is an effective way to identify at-risk teens and is recommended by the US Preventive Services Task Force the Institute of Medicine, the American Academy of Pediatrics, the American Academy of Family Physicians and the National Association of pediatric Nurse Practitioners. How to Get Started Primary care practitioners who are interested in providing mental health checkups to their teen patients will receive the Pocket Guide for mental health checkups. The guide provides all the information you and your staff needs to participate in the program, including: Evidence-based screening questionnaires and other resource materials Information on obtaining reimbursement for screening Information on accessing immediate referrals from network resources through our mental health partners Ongoing support and technical assistance Back to Table of Contents EmblemHealth Provider Manual Last Updated: 09/03/2014 466 BEHAVIORAL HEALTH SERVICES To request these materials, please e-mail [email protected] or call 1-212-265-4426. Snapshots of the Pocket Guide & Screening Questionnaire Reimbursement Codes for a Mental Health Checkup during a Well-child Exam Back to Table of Contents EmblemHealth Provider Manual Last Updated: 09/03/2014 467 BEHAVIORAL HEALTH SERVICES MENTAL HEALTH PARITY AND ADDICTION EQUITY ACT OF 2008 (MHPAEA) On October 3, 2008 Congress enacted the MHPAEA. The MHPAEA applies to large group, CHIPS and Medicare members whose group enrolled in the plan on or after October 3, 2009. Under the MHPAEA, the expanded coverage for behavioral health services enacted by the New York State legislature under Timothy's Law was further enhanced to include substance abuse treatment and non-biologically based mental health treatment. As a result of the MHPAEA, there is no day or visit limitation for members covered by the act who have a behavioral health benefit and meet medical necessity criteria. Prior approval requirements continue to apply to these services. As of November 1, 2009 there are no limits to behavioral health services for Child Health Plus members. Back to Table of Contents EmblemHealth Provider Manual Last Updated: 09/03/2014 468
© Copyright 2026