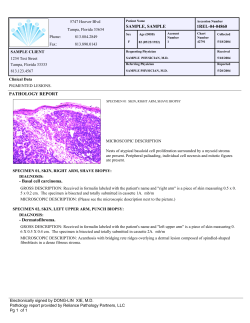
Guide to Laboratory Services Updated August 2014 Lawrence + Memorial Hospital
Guide to Laboratory Services Updated August 2014 Lawrence + Memorial Hospital New London, Connecticut CT License Numbers Lawrence + Memorial Hospital Lab HP-0227 Pequot Health Center Lab HP-0263 Cancer Center Lab HP-0352 Table of Contents PREFACE .................................................................................................... 20 Pathologists: ..................................................................................................................21 Pathologist Assistant: ....................................................................................................21 Administrative Director: ...............................................................................................21 Administrative Consultant: ...........................................................................................21 Section Managers: .........................................................................................................22 Test Priorities ................................................................................................................23 Home Blood Drawing ...................................................................................................24 STAT Laboratory Work ................................................................................................25 Laboratory Critical Results (Panic Values): .................................................................27 L+M Cancer Center Critical Results (Panic Values): ...................................................28 ANATOMIC PATHOLOGY:.................................................................... 29 Slides for Outside Consultation ....................................................................................29 Critical Results ..............................................................................................................29 Specimen Labeling ........................................................................................................29 Specimen Submission/Handling ...................................................................................30 Special Test Request/Submission .................................................................................32 Autopsy (Adult): ...........................................................................................................37 Stillbirth/Fetal Death .....................................................................................................39 BLOOD BANK ........................................................................................... 40 ABO and Rh Typing .....................................................................................................41 ABS see Antibody Screen .............................................................................................42 Albumin.........................................................................................................................43 Ante Partum RhIG, see Rh(D) Immune Globulin Antepartum .....................................44 Antibody Screen ............................................................................................................45 Antibody Titer see Titer ................................................................................................46 Autologous Donors .......................................................................................................47 Autologous Donations are no longer collected at Lawrence + Memorial Hospital.....47 For information on donating Autologous blood, please contact the American Red Cross, CT region at: 860-678-2805 ..............................................................................47 Blood Typing see ABO and Rh Typing ........................................................................48 Compatibility Testing see Red Blood Cells - Crossmatch ............................................49 Cord Blood ....................................................................................................................50 Cryoprecipitate ..............................................................................................................51 Reference Range: Usual dose is 10 units (2 pools of 5)Cryoprecipitated Antihemophitic Factor, Cryoprecipitated AHF, CRYO see CryoprecipitateDirect Antiglobulin Test ..........................................................................................................51 Cryoprecipitated Antihemophitic Factor, Cryoprecipitated AHF, CRYO see CryoprecipitateDirect Antiglobulin Test .......................................................................52 Direct Antiglobulin Test ...............................................................................................53 DAT see Direct Antiglobulin Test ................................................................................54 Deglyced Red Cells see Red Blood Cells Deglycerolized - Crossmatch......................55 Direct Coombs, see Direct Antiglobulin Test ...............................................................56 FFP see Fresh Frozen Plasma .......................................................................................57 Fresh Frozen Plasma .....................................................................................................58 Frozen Red Cells see Red Blood Cells Deglycerolized - Crossmatch ..........................59 Group & Rh, see ABO and Rh Typing .........................................................................60 HLA-ABC .....................................................................................................................61 HLA-DRDQ ..................................................................................................................62 Indirect Antiglobulin Test, see Antibody Screen ..........................................................63 Indirect Coombs see Antibody screen ...........................................................................64 Packed Red Cells, see Red Blood Cells – Crossmatch Panel, see Antibody Identification .................................................................................................................65 Pediatric Packed Cells ...................................................................................................66 Phlebotomy see Therapeutic PhlebotomyPlatelet Concentrate .....................................67 Platelet Concentrate ......................................................................................................68 Platelet Packs see Platelet Concentrate .........................................................................69 Pooled Platelets, see PrePooled Platelets .....................................................................70 Prenatal Rhogam see Rh (D) Immune Globulin Antepartum .......................................71 PrePooled Platelets ........................................................................................................72 Random Donor Platelets see Pre-pooled platelets Red Blood Cells - Crossmatch .......73 Red Blood Cells - Crossmatch ......................................................................................74 Red Blood Cells Deglycerolized - Crossmatch .............................................................75 Red Blood Cells Leukocyte Reduced - Crossmatch .....................................................76 Rh Titer, Antibody Titer, Antibody Quantitation, Atypical Antibody Titer see Titers 77 Rh(D) Immune Globulin ...............................................................................................78 Rh(D) Immune Globulin Antepartum ...........................................................................79 RhIG see Rh(D) Immune Globulin ...............................................................................80 RhoGam see Rh(D) Immune Globulin .........................................................................81 Salt Poor Albumin, Normal Serum Albumin, 25% Serum Albumin, 5% Albumin see Albumin Product ...........................................................................................................82 Therapeutic Bleeding see Therapeutic Phlebotomy ......................................................83 Therapeutic Phlebotomy ...............................................................................................84 Titer ...............................................................................................................................85 Transfusion Reaction Review .......................................................................................86 Type & Screen ...............................................................................................................87 Washed Cells see Red Blood Cells Deglycerolized - Crossmatch ...............................88 Reference Lab.............................................................................................. 89 1st Trimester Risk Screen .............................................................................................90 5-Hydroxyindolacetic Acid, Quantitative, 24 hour Urine .............................................91 5' Nucleotidase, Blood ..................................................................................................92 17-Hydroxyprogesterone ...............................................................................................93 17-Ketosteroids, Total, 24 hour Urine ..........................................................................94 Acetylcholine Receptor Antibody .................................................................................95 Adenovirus Titer ...........................................................................................................96 Adrenocorticotrophic Hormone ....................................................................................97 Aldolase, Blood .............................................................................................................99 Aldosterone, 24 hour Urine .........................................................................................100 Aldosterone, Serum .....................................................................................................101 Alkaline Phosphatase Isoenzymes, Blood ...................................................................102 Alkaline Phosphatase, Bone Specific ..........................................................................103 Alpha - 1 - Antitrypsin, Blood ....................................................................................104 Alpha feto protein, maternal .......................................................................................105 Alprazolam ..................................................................................................................106 Aluminum, Blood ........................................................................................................107 Amino Acids - Quantitative Plasma ............................................................................108 Amino Acids - Quantitative Urine ..............................................................................109 Amino Levulinic Acid, 24 hour Urine ........................................................................110 Amiodarone .................................................................................................................111 Amitriptyline ...............................................................................................................112 Amniotic Fluid L/S Ratio ............................................................................................113 Amphetamines, Urine .................................................................................................114 Amylase Isoenzymes ...................................................................................................115 Anaplasma phagocytophilum Antibody ......................................................................116 Androstenedione .........................................................................................................117 Angioedema Panel, Acquired......................................................................................118 Angiotensin Converting Enzyme ................................................................................119 Anti-Cardiolipin Antibody ..........................................................................................120 Antidiuretic Hormone .................................................................................................121 Anti-DNA, Single Stranded ........................................................................................122 Anti Strep DNase-B ....................................................................................................123 Anti-Epidermal Antibody............................................................................................124 Anti-Glomerular Basement Membrane .......................................................................125 Anti-Mitochondrial Antibody .....................................................................................126 Anti-Neutrophil Cytoplasmic Antibody ......................................................................127 Antinuclear Antibody ..................................................................................................128 Reference Range: < 1:40. ANA pattern reported with positive results.......................128 Antiplatelet Antibody ..................................................................................................129 Anti-Streptolysin O Titer ............................................................................................130 Apolipoprotein A1 ......................................................................................................131 Apolipoprotein B .........................................................................................................132 Apolipoproteins A1&B ...............................................................................................133 Acetylcholine Blocking Antibody...............................................................................134 Arsenic, 24 hour urine .................................................................................................135 Arsenic, Blood.............................................................................................................136 ASCA (Saccharomyces Cerevisiae) IgA ....................................................................137 ASCA (Saccjaromyces Cerevisiae) IgG .....................................................................138 Aspergillus fumigatus IgG ..........................................................................................139 Aspergillus, Serology ..................................................................................................140 Babesia Serology .........................................................................................................141 Barbiturates, Total, Blood ...........................................................................................142 Beta-2-Glycoprotein (IgG, IgA, IgM) .........................................................................143 Beta-2-Microglobulin ..................................................................................................144 Blastomyces, Serology ................................................................................................145 Blood Chromosome Analysis .....................................................................................146 Chromosomes, Bone Marrow or Peripheral Blood .....................................................147 Bordetella Pertussis Antibodies ..................................................................................148 C1 Esterase, Functional ...............................................................................................149 C1 Esterase Inhibitor ...................................................................................................150 C3d Circulating Immune Complexes ..........................................................................151 CA15-3 ........................................................................................................................152 CA19-9 ........................................................................................................................153 CA27.29 ......................................................................................................................154 Caffeine .......................................................................................................................155 Calcitonin ....................................................................................................................156 Candida albicans Antibodies .......................................................................................157 Carbamazepine 10, 11 Epoxide...................................................................................158 Carotene ......................................................................................................................159 Cat Scratch Fever Serology .........................................................................................160 Catecholamines, 24 hour Urine ...................................................................................161 Catecholamines, plasma ..............................................................................................162 Celiac DNA Genotyping .............................................................................................163 Ceruloplasmin .............................................................................................................164 Cholinesterase, Blood .................................................................................................165 Chromium, Plasma ......................................................................................................166 Chromogranin A..........................................................................................................167 Chromosome Analysis, Tissue ....................................................................................168 Citrate, 24 hour urine ..................................................................................................169 Clonazepam .................................................................................................................172 Clozapine.....................................................................................................................173 CMV Antigenemia ......................................................................................................174 Cocaine Metabolites, Urine .........................................................................................176 Coccidioides Antibody ................................................................................................177 Coenzyme Q10 ............................................................................................................178 Cold Agglutinins .........................................................................................................179 Collagen Type I C-Telopeptide (CTx) ........................................................................180 Collagen Cross-Linked N-Telopeptide, Urine ............................................................181 Complement, C2 .........................................................................................................182 Complement, C5 .........................................................................................................183 Complement, C6 .........................................................................................................184 Complement, Total (CH5O)........................................................................................185 Copper, 24 hour urine .................................................................................................186 Copper, Blood .............................................................................................................187 Cortisol, Free 24 hour urine ........................................................................................188 Coxsackie B Virus Titer ..............................................................................................189 C-Peptide .....................................................................................................................190 Creatine Kinase Isoenzyme Panel ...............................................................................191 Cryoglobulins ..............................................................................................................192 Cryptococcus Antibody ...............................................................................................193 CSF IgG ......................................................................................................................194 Cyclic Citrulline Peptide, IgG .....................................................................................195 Cyclosporine ...............................................................................................................197 Cystic Fibrosis Screen .................................................................................................198 Cystine, 24 hour urine .................................................................................................199 Cytomegalovirus Antibodies .......................................................................................200 Desipramine ................................................................................................................202 DHEA Sulfate .............................................................................................................203 Diphtheria Antitoxoid Antibody .................................................................................204 DISOPYRAMIDE.......................................................................................................205 Drug Screen, Serum Only ...........................................................................................207 Echinococcus Serology ...............................................................................................208 Endomysial IgA Antibody ..........................................................................................209 Epstein-Barr Virus DNA, Quantitative PCR ..............................................................212 Erythropoietin .............................................................................................................213 Estrone, serum .............................................................................................................214 Extractable Nuclear Antigen Antibodies ....................................................................215 Factor V Leiden Mutation Analysis ............................................................................216 Factor VIII Multimers .................................................................................................217 Factor VIII Related Antigen ........................................................................................218 Fecal Fat, Random ......................................................................................................219 Fecal Fat, Timed specimen .........................................................................................220 Flecainide ....................................................................................................................221 Flow Cytometry, Bone Marrow or Peripheral Blood..................................................222 Folate, RBC .................................................................................................................223 Fragile-X .....................................................................................................................224 Free T3 ........................................................................................................................225 Free Testosterone ........................................................................................................226 Fructosamine ...............................................................................................................227 FTA-CSF .....................................................................................................................228 FTA Profile .................................................................................................................229 Fungal Serology Panel ................................................................................................230 Gabapentin ..................................................................................................................231 Ganglioside GM-1 Antibodies ....................................................................................232 Gastric Parietal Cell Antibody ....................................................................................233 Gastrin .........................................................................................................................234 Glucagon .....................................................................................................................235 Glucose-6-Phosphate Dehydrogenase .........................................................................236 Glutamic Acid Decarboxylase-65 Antibody ...............................................................237 Growth Hormone (HGH), Human ..............................................................................238 Haptoglobin .................................................................................................................239 Heavy Metal Screen, blood .........................................................................................240 Helicobacter Antibodies ..............................................................................................241 Hemoglobin Electrophoresis .......................................................................................242 Heparin Anti-Xa LMWH Assay .................................................................................243 Heparin Induced Platelet Antibody .............................................................................244 Hepatitis A Antibody, Total with Reflex to IgM ........................................................245 Hepatitis B E Antibody ...............................................................................................246 Hepatitis B E Antigen .................................................................................................247 Hepatitis B Surface Antigen, Neutralization ...............................................................248 Hepatitis B Viral (HBV) DNA Quantitative by PCR .................................................249 Hepatitis C Genotype ..................................................................................................250 Hepatitis C RNA .........................................................................................................251 Hereditary Hemochromatosis, DNA, Mutation Analysis ...........................................252 Herpes Simplex Virus Antibodies ...............................................................................253 Herpes Simplex Virus (HSV) IgM Antibody with Reflex to Titer .............................256 Histamine, blood .........................................................................................................261 Histone Antibodies ......................................................................................................262 Histoplasma Antibody .................................................................................................263 HIV, RNA by PCR (Ultra) ..........................................................................................266 HIV Genotype .............................................................................................................267 HIV-1 Phenotype ........................................................................................................268 HLA - B27...................................................................................................................269 HTLV ABS I & II .......................................................................................................270 Hypersensitivity Pneumonitis Evaluation ...................................................................271 Hypersensitivity Pneumonitis Screen .........................................................................272 IDPH see Immune Deficiency Panel IGF (Insulin-like growth factor) Binding Protein2 ...................................................................................................................................273 IGF (Insulin-like growth factor) Binding Protein-2 ....................................................274 IGF (Insulin-like growth factor) Binding Protein-3 ....................................................275 IgG (Immunoglobulin G) Subclass 4 ..........................................................................276 IgG Subclass Fractionation .........................................................................................277 Imipramine ..................................................................................................................278 Immune Complex, C1 Q .............................................................................................279 Immune Complex Panel ..............................................................................................280 Immune Deficiency Panel ...........................................................................................281 Immunoelectrophoresis, Serum...................................................................................282 Immunoglobulin D ......................................................................................................283 Influenza Antibody Panel ............................................................................................284 Insulin Antibody (Insulin Auto-antibody) ..................................................................285 Insulin Growth Factor-1 ..............................................................................................286 Intrinsic factor Antibody .............................................................................................287 Islet Cell Antibody ......................................................................................................288 JAK2 Mutation ............................................................................................................289 Jo-1 Antibody ..............................................................................................................290 Keppra .........................................................................................................................291 Lamictal.......................................................................................................................292 Lead, Blood .................................................................................................................293 Legionella Serology ....................................................................................................294 Lipoprotein A ..............................................................................................................295 Lipoprotein Fractionation Panel 2, Ion Mobility ........................................................296 Lipoprotein Electrophoresis ........................................................................................297 Liver-Kidney Microsomal Antibody (IgG) .................................................................298 Lorazepam ...................................................................................................................299 Lyme Disease Antibody with Reflex to CSF ratio ......................................................300 Lyme Titer, CSF..........................................................................................................301 Lyme Titer, Misc Fluid ...............................................................................................302 Lyme - Western blot....................................................................................................303 Lymphocyte Enumeration Panel .................................................................................304 Lymphocytic Choriomeningitis Virus Antibody ........................................................305 Lysozyme ....................................................................................................................306 Magnesium, RBC ........................................................................................................307 Magnesium, Urine 24 hour .........................................................................................308 Magnesium, Urine Random ........................................................................................309 Mephobarital Level .....................................................................................................310 MecSTAT 7 panel .......................................................................................................311 MecSTAT 9 panel .......................................................................................................312 Mercury, blood ............................................................................................................313 Metanephrines, Plasma ...............................................................................................314 Metanephrines, Total, 24 hour Urine ..........................................................................315 Methadone, urine.........................................................................................................316 Methotrexate Level .....................................................................................................317 Methylenetetrahydrofolate Reductase .........................................................................318 Methylmalonic Acid....................................................................................................319 MTHFR see Methylenetetrahydrofolate Reductase ....................................................320 Mumps Antibodies ......................................................................................................323 Myasthenia Gravis Panel.............................................................................................324 Mycoplasma Serology .................................................................................................325 Myelin Basic Protein ...................................................................................................326 Myoglobin ...................................................................................................................327 Myoglobin, Urine ........................................................................................................328 Mysoline, Level...........................................................................................................329 Niemann-Pick Disease Mutation Analysis ..................................................................332 Nortriptyline ................................................................................................................333 Organic Acids, urine ...................................................................................................334 Oxalate, Urine .............................................................................................................336 Paraneoplastic AB Evaluation.....................................................................................337 Parvovirus titers ..........................................................................................................338 Pentobarbital ...............................................................................................................339 Phencyclidine ..............................................................................................................340 Phenylalanine, PKU ....................................................................................................341 Phenytoin, Free ...........................................................................................................342 Phosphatidylserine Antibodies (IgG, IgM) .................................................................343 Phospholipids ..............................................................................................................344 PNH with FLAER (High Sensitivity) .........................................................................345 Poliovirus Antibody, Neutralization ...........................................................................346 Porphobilinogen, 24 hour urine...................................................................................347 Porphyrins, Fractionated, Quantitative and Porphobilinogen, 24-Hour Urine ...........348 Porphyrins, Fractionated, Quantitative, Random Urine ..............................................349 Primadone ...................................................................................................................350 Prograf .........................................................................................................................351 Pro-Predict Metabolites ...............................................................................................352 Protein Electrophoresis, Serum ...................................................................................353 Protein Immunoelectrophoresis, Urine .......................................................................354 Prothrombin Gene Mutation .......................................................................................355 PTH, C Terminal .........................................................................................................356 PSA, Free and Total ....................................................................................................357 Pyruvic Acid................................................................................................................358 Q Fever, Titer ..............................................................................................................359 Quinidine, Blood .........................................................................................................360 Rapamycin ...................................................................................................................361 Renin Activity .............................................................................................................362 Reticulin Antibody, IgA ..............................................................................................365 Ristocetin Co-Factor ...................................................................................................366 Rubella Antibodies ......................................................................................................367 Rubeola Antibodies .....................................................................................................368 Schistosoma Serology .................................................................................................369 Scleroderma Antibody ................................................................................................370 Sex Hormone Binding Globulin..................................................................................371 Serotonin, Blood .........................................................................................................372 Sjogrens Antibodies ....................................................................................................373 Smooth Muscle Antibody ...........................................................................................374 Somatostatin ................................................................................................................375 Stone Analysis .............................................................................................................376 Striated Muscle Antibodies .........................................................................................377 Rickettsia Antibodies ..................................................................................................378 Stool Osmolality, 24 hour ...........................................................................................379 Stool Potassium, 24 hour.............................................................................................380 Stool Sodium, 24 hour.................................................................................................381 Streptococcus pneumoniae IgG (23 Serotypes) ..........................................................382 Streptozyme.................................................................................................................383 Tay-Sachs Detection ...................................................................................................384 Tay-Sachs Gene Mutation Analysis -Tay Sachs Mutation .........................................385 Tetanus Antitoxoid Antibody ......................................................................................386 THC Confirmation, Urine ...........................................................................................387 ThinPrep Pap and HR HPV DNA ...............................................................................388 ThinPrep Pap with reflex to HR HPV DNA ...............................................................389 ThinPrep Imaging Pap .................................................................................................390 Thrombin Time ...........................................................................................................391 Thyroglobulin ..............................................................................................................392 Thyroglobulin Antibodies ...........................................................................................393 Thyroid Auto-Antibodies ............................................................................................394 Thyroid Peroxidase Ab ...............................................................................................395 Thyroid Stimulating Immunoglobulin ........................................................................396 Thyroxine Binding Globulin .......................................................................................397 Tissue Transglutaminase Antibody, IgG .....................................................................398 Topamax ......................................................................................................................399 Torch Panel .................................................................................................................400 Toxicology Profile, Blood (Tox. Screen, Blood) ........................................................401 Toxocara ......................................................................................................................402 Toxoplasmosis Antibodies ..........................................................................................403 Toxoplasmosis, Status .................................................................................................404 TPMT ..........................................................................................................................405 TPMT (Thiopurine S-Methyltransferase) Genotype ...................................................406 Transferrin ...................................................................................................................407 Trileptal Level .............................................................................................................408 Tryptase .......................................................................................................................409 TT see Thrombin Time ...............................................................................................410 Urine Myoglobin .........................................................................................................411 Vanillylmandelic Acid, 24 Hour Urine .......................................................................412 VAP ™ Cholesterol panel ...........................................................................................413 Varicella Status ...........................................................................................................414 Varicella-Zoster, Antibodies .......................................................................................415 Vasoactive Intestinal Peptide ......................................................................................416 VDRL-CSF .................................................................................................................417 Viscosity, Serum .........................................................................................................419 Vitamin A, Blood ........................................................................................................420 Vitamin B1 ..................................................................................................................421 Vitamin B2 ..................................................................................................................422 Vitamin B6 ..................................................................................................................423 Vitamin B12 Binding Capacity, Unsaturated..............................................................424 Vitamin C ....................................................................................................................425 Vitamin D1, 25-Dihydroxy .........................................................................................426 Vitamin D, 25 Hydroxy fractionation .........................................................................427 Vitamin E ....................................................................................................................428 Vitamin K ....................................................................................................................429 Zinc, Blood ..................................................................................................................430 CHEMISTRY ............................................................................................ 432 Acetaminophen, Blood ................................................................................................433 Acetone, Quantitative, Blood ......................................................................................434 Albumin, Blood ...........................................................................................................435 Albumin, Fluid ............................................................................................................436 Alcohol, Blood ............................................................................................................437 Alcohol, Urine .............................................................................................................438 Alkaline Phosphatase, Blood ......................................................................................439 Alpha feto protein, tumor marker ................................................................................440 Ammonia, Blood .........................................................................................................441 Amniotic Fluid L/S Ratio ............................................................................................442 Amylase, Blood ...........................................................................................................443 Amylase, Body Fluids .................................................................................................444 Amylase, Urine random ..............................................................................................445 Anti-Centromere Antibody .........................................................................................446 Anti-Gliadin Antibodies, IgA and IgG ........................................................................447 Arterial Blood Gas ......................................................................................................448 Arterial pH ..................................................................................................................449 Basic Metabolic Panel .................................................................................................450 Bilirubin, Direct ..........................................................................................................451 Bilirubin, Total (Neonatal) ..........................................................................................452 Bilirubin, Total and Direct, Blood ..............................................................................453 Blood Oxygen Saturation ............................................................................................454 BNP .............................................................................................................................455 C3 Complement ..........................................................................................................456 C4 Complement ..........................................................................................................457 CA-125 ........................................................................................................................458 Calcium, Blood ...........................................................................................................459 Calcium, Serum, Ionized .............................................................................................460 Calcium, Urine ............................................................................................................461 Carbon Dioxide, Total .................................................................................................462 Carboxyhemoglobin ....................................................................................................463 Carcinoembryonic Antigen .........................................................................................464 CCU Profile .................................................................................................................465 Celiac Profile ...............................................................................................................466 Childhood Allergy Panel .............................................................................................467 Chloride, Blood ...........................................................................................................468 Chloride, CSF ..............................................................................................................469 Chloride, Urine ............................................................................................................470 Cholesterol, Total ........................................................................................................471 Cholesterol, Fluid ........................................................................................................472 Cholesterol Fractionation ............................................................................................473 CKMB (Creatine Kinase, MB Fraction) .....................................................................474 Comprehensive Inhalant Panel ....................................................................................475 Comprehensive Metabolic Panel.................................................................................476 Cortisol ........................................................................................................................477 CPK .............................................................................................................................478 C-Reactive Protein ......................................................................................................479 C-Reactive Protein, Cardiac ........................................................................................480 Creatinine, Blood ........................................................................................................481 Creatinine Clearance ...................................................................................................482 Creatinine, 24 hour Timed or Random Urine .............................................................483 Dilantin, Blood ............................................................................................................485 Drugs of Abuse, Urine ................................................................................................486 Electrolytes, Blood ......................................................................................................487 Electrolytes, Urine.......................................................................................................488 Estradiol ......................................................................................................................489 Ferritin, serum .............................................................................................................490 Folate, serum ...............................................................................................................491 Follicle Stimulating Hormone .....................................................................................492 General Food Screen ...................................................................................................494 GGT.............................................................................................................................495 Gentamicin ..................................................................................................................496 Glucose, Blood ............................................................................................................497 Glucose, Fluid .............................................................................................................498 Glucose, OB screen .....................................................................................................499 Glucose, Spinal Fluid ..................................................................................................500 Glucose Tolerance OB Patients ..................................................................................501 Glucose Tolerance Test 2 Hours .................................................................................502 Glycosylated Hemoglobin ...........................................................................................503 HCG, male...................................................................................................................504 HCG, Quantitative, Beta Subunit ................................................................................505 Heart Profile ................................................................................................................506 Hemoglobin, Total ......................................................................................................507 Hepatitis A Antibody (IgM) ........................................................................................508 Hepatitis B Core Antibody (IgM) ...............................................................................509 Hepatitis B Surface Antibody .....................................................................................510 Hepatitis B Surface Antigen ........................................................................................511 Hepatitis C Virus Antibody .........................................................................................512 Hepatitis Panel ............................................................................................................513 HIV-1 Antibody ..........................................................................................................514 Homocysteine ..............................................................................................................515 IgE ...............................................................................................................................516 Immunoglobulin Panel ................................................................................................517 Infectious Mononucleosis Test ...................................................................................518 Insulin Glucose Tolerance, 2 or 3 Hours ....................................................................519 Insulin, Random ..........................................................................................................520 Iron Profile ..................................................................................................................521 Lactic Acid, Blood ......................................................................................................522 Lactic Acid, CSF .........................................................................................................523 Lactic Dehydrogenase, Blood .....................................................................................524 Lactic Dehydrogenas, Fluid ........................................................................................525 Lactose Tolerance Test ...............................................................................................526 Latex Allergen .............................................................................................................527 LDL cholesterol ..........................................................................................................528 Lipase, Serum ..............................................................................................................529 Lithium, Blood ............................................................................................................530 Liver Profile ................................................................................................................531 Luteinizing Hormone ..................................................................................................532 Lyme Disease Serology, Serum ..................................................................................533 Magnesium, Blood ......................................................................................................534 Measles Immunity Panel .............................................................................................535 Methemoglobin ...........................................................................................................536 Microalbumin, Urine ...................................................................................................537 New England Regional Inhalant Panel .......................................................................538 Nut Panel .....................................................................................................................539 Osmolality, Serum.......................................................................................................540 Osmolality, Urine ........................................................................................................541 PG - FLM Test ............................................................................................................542 pH, Body Fluid ............................................................................................................543 Phenobarbital, Blood ...................................................................................................544 Phosphate, Urine .........................................................................................................545 Phosphorus, Blood ......................................................................................................546 Potassium, Blood.........................................................................................................547 Potassium, Urine .........................................................................................................548 Prealbumin ..................................................................................................................549 Pregnancy Test, Serum................................................................................................550 Pregnancy Test, Urine .................................................................................................551 Prenatal Profile ............................................................................................................552 Procalcitonin ...............................................................................................................553 Progesterone ................................................................................................................554 Prolactin ......................................................................................................................555 Prostate Specific Antigen ............................................................................................556 Protein, Body Fluid .....................................................................................................557 Protein, CSF ................................................................................................................558 Protein, Total, Blood ...................................................................................................559 Protein, Urine ..............................................................................................................560 PTH, intact panel .........................................................................................................561 RAST testing – miscellaneous tests ............................................................................562 Rheumatoid Factor ......................................................................................................563 Rheumatoid Profile .....................................................................................................564 Rubella, Status.............................................................................................................565 Rubeola, Status ............................................................................................................566 Salicylate, Blood .........................................................................................................567 SGOT/AST ..................................................................................................................568 SGPT/ALT ..................................................................................................................569 Shellfish Panel .............................................................................................................570 Sodium, Blood.............................................................................................................571 Sodium, Urine .............................................................................................................572 Stinging Insect Panel ...................................................................................................573 Syphyllis Antibodies, Blood .......................................................................................574 T-3, Total.....................................................................................................................576 T4, Free .......................................................................................................................577 Tegretol .......................................................................................................................578 Testosterone, Total ......................................................................................................579 Theophylline ...............................................................................................................580 Thyroid Profile ............................................................................................................581 Thyroid Stimulating Hormone, Ultra sensitive ...........................................................582 Tissue Transglutaminase IgA ......................................................................................583 Triglycerides, Blood ....................................................................................................586 Triglycerides – Fluid ...................................................................................................587 Troponin I....................................................................................................................588 Urea Nitrogen, Blood ..................................................................................................589 Urea, Urine ..................................................................................................................590 Uric Acid, Blood .........................................................................................................591 Uric Acid, Fluid ..........................................................................................................592 Uric Acid, Urine ..........................................................................................................593 Valproic Acid ..............................................................................................................594 Vitamin B12 ................................................................................................................596 Vitamin D 25-Hydroxy ...............................................................................................597 COAGULATION ...................................................................................... 598 Activated Partial Thromboplastin Time ......................................................................599 Antithrombin III ..........................................................................................................600 APTT see Activated Partial Thromboplastin Time .....................................................601 C.A.C. Circulating Anticoagulant see: Mixing Studies ..............................................602 Coagulation Factor Assays see Factor VIII Assay ......................................................603 Coagulation Profile .....................................................................................................604 D-Dimer Quantative ....................................................................................................605 D-Dimer ......................................................................................................................606 DIC Profile ..................................................................................................................607 Factor II Mutation see Prothrombin Gene Mutation ...................................................608 Factor VIII Assay ........................................................................................................609 Fibrinogen Level .........................................................................................................610 HCOAG see Hypercoagulable profile ........................................................................611 Hemorrhagic Screen see Coagulation Profile .............................................................612 Hypercoagulable Profile ..............................................................................................613 LUPA see Lupus Anticoagulant..................................................................................614 Lupus Anticoagulant ...................................................................................................615 Mixing Studies ............................................................................................................616 PFA see Platelet Function Assay ................................................................................617 Platelet Function Assay ...............................................................................................618 Protein C......................................................................................................................619 Protein S ......................................................................................................................620 Prothrombin Time/INR ...............................................................................................621 PT/INR see Prothrombin Time/INR ...........................................................................622 CYTOLOGY ............................................................................................. 623 Ascitic Fluid Cytology see Cytology, Body Fluids: Pleural, Ascitic and Pericardial .624 Breast Cyst Fluid Cytology see Cytology, Spinal and Cyst Fluid: Renal, Ovarian, Breast, Etc. ..................................................................................................................625 Bronchial Brushings, Cytology see Cytology, Brushings: Bronchial, Esophageal, Gastric, Small Bowel, Colonic, Etc. ...........................................................................626 Bronchial Washings, Cytology see Cytology, Bronchial, Esophageal Washings and Tracheal Aspirations ...................................................................................................627 Cyst Fluid Cytology see Cytology, Spinal and Cyst Fluid: Renal, Ovarian, Breast, Etc. ..................................................................................................................628 Cytology, Body Fluids: Pleural, Ascitic and Pericardial ............................................629 Cytology, Bronchial, Esophageal Washings and Tracheal Aspirations ......................630 Cytology, Brushings: Bronchial, Esophageal, Gastric, Small Bowel, Colonic, Etc. ..631 Cytology, Cervical – Vaginal Smears .........................................................................632 Cytology, Nipple Discharge ........................................................................................633 Cytology, Spinal and Cyst Fluid: Renal, Ovarian, Breast, Etc. ..................................634 Cytology, Sputum .......................................................................................................635 Cytology, Urine ...........................................................................................................636 Cytology: Viral Study: Cytomegalic Virus on Urine ..................................................637 Cytomegalic Inclusion Bodies see Cytology: Viral Study: Cytomegalic Virus on Urine ............................................................................................................................638 Cytomegalic Inclusion Disease (CID) see Cytology: Viral Study: Cytomegalic Virus on Urine .......................................................................................................................639 Esophageal Washings, Tracheal Aspiration Cytology see Cytology, Bronchial, Esophageal Washings and Tracheal Aspirations ........................................................640 Fine Needle Aspiration ...............................................................................................641 Nipple Discharge Cytology, see Cytology, Nipple Discharge ....................................642 Ovarian Cyst Fluid Cytology see Cytology, Spinal and Cyst Fluid: Renal, Ovarian, Breast, Etc. ..................................................................................................................643 Pap Smear see Cytology, Cervical - Vaginal Smears .................................................644 Papanicolaou Smear see Cytology, Cervical - Vaginal Smears ..................................645 Paracentesis Cytology see Cytology, Body Fluids: Pleural, Ascitic and Pericardial ..646 Pericardial Fluid Cytology see Cytology, Body Fluids: Pleural, Ascitic and Pericardial ...................................................................................................................647 Pericardiocentesis Cytology see Cytology, Body Fluids: Pleural, Ascitic and Pericardial ...................................................................................................................648 Pleural Fluid Cytology see Cytology, Body Fluids: Pleural, Ascitic and Pericardial .649 Renal Cyst Fluid Cytology see Cytology, Spinal and Cyst Fluid: Renal, Ovarian, Breast, Etc. ..................................................................................................................650 Spinal Fluid Cytology see Cytology, Spinal and Cyst Fluid: Renal, Ovarian, Breast, Etc. ..............................................................................................................................651 Sputum Cytology see Cytology, Sputum ....................................................................652 Sputum Series Cytology see Cytology, Sputum .........................................................653 Thoracentesis Cytology see Cytology, Body Fluids: Pleural, Ascitic and Pericardial654 Tzanck Preparation......................................................................................................655 HEMATOLOGY ...................................................................................... 656 Babesia Smear .............................................................................................................657 Body Fluid Analysis ....................................................................................................658 Body Fluid ...................................................................................................................659 Bone Marrow ..............................................................................................................660 CBC see Complete Blood Count.................................................................................661 Chronic Leukemia/Lymphoma Immunophenotyping .................................................662 Cerebrospinal Fluid Analysis ......................................................................................663 Complete Blood Count ................................................................................................664 Complete Blood Count with Manual Differential .......................................................665 CSFCT see Cerebrospinal Fluid Analysis...................................................................666 Ehrlichia Smear ...........................................................................................................667 Eosinophil Smear ........................................................................................................668 Erythrocyte Sedimentation Rate see Sedimentation Rate ...........................................669 ESR see Sedimentation Rate .......................................................................................670 FCEL see Body Fluid Analysis ...................................................................................671 Fetal Hemoglobin Stain...............................................................................................672 FHCT see Hematocrit - Body Fluid ............................................................................673 Fluid Crystals ..............................................................................................................674 Fluid Hematocrit .........................................................................................................675 Hemogram see Complete Blood Count.......................................................................676 Hematocrit - Peripheral Blood ....................................................................................677 Hemoglobin-Peripheral Blood ....................................................................................678 Hemogram see Complete Blood Count.......................................................................679 Iron Stain, Bone Marrow - see Bone Marrow ............................................................680 Kleihauer-Betke Fetal Hgb Stain - see Fetal Hemoglobin Stain................................681 Malaria Smear .............................................................................................................682 Manual Differential see Differential White Blood Cell Count ...................................683 Nasal Smear for Eosinophils see Eosinophil Smear ...................................................684 Platelet Count ..............................................................................................................685 Retic Count see Reticulocyte Count ...........................................................................686 Reticulocyte Count ......................................................................................................687 RTC see Reticulocyte Count .......................................................................................688 Sedimentation Rate .....................................................................................................689 Sed Rate see Sedimentation Rate ................................................................................690 Sickle see Sickle Cell Preparation ...............................................................................691 Sickle Cell see Sickle Cell Preparation .......................................................................692 Sickle Cell Preparation ................................................................................................693 Spinal Fluid Cell Count see Cerebrospinal Fluid Analysis .........................................694 Sputum for Eosinophils see Eosinophil Smear ...........................................................695 Synovial Fluid Analysis ..............................................................................................696 WBC see White Blood Cell Count..............................................................................697 White Blood Cell Count ..............................................................................................698 HOME BLOOD DRAWING ................................................................... 699 MICROBIOLOGY ................................................................................... 700 MICROBIOLOGY COVERAGE ...............................................................................700 MICROBIOLOGY REQUISITIONING ....................................................................700 COLLECTION AND TRANSPORT OF MICROBIOLOGY SPECIMENS ............700 REJECTION OF SPECIMENS ..................................................................................702 SPECIMEN COLLECTION .......................................................................................703 Stool Collection/Transport Guide...........................................................................708 Recommendation for O&P evaluation ........................................................................708 AFB Blood Culture see Culture, Mycobacteria, Blood ..............................................710 AFB Smear and Culture, MAV Culture, TB Culture see Culture, Mycobacteria.......711 Beta Strep Group A (Rapid Test) ...............................................................................712 Beta Strep Screen (24 hour) see Culture, Throat, for Beta Strep Group A .................713 Blood Culture for MAV see Culture, Mycobacteria, Blood .......................................714 Blood Culture, Fungus see Culture, Blood .................................................................715 Blood Culture, Routine see Culture, Blood ................................................................716 C. Difficile Toxin ........................................................................................................717 Candida Antigen ..........................................................................................................718 Chlamydia PCR ...........................................................................................................719 Clostridium Difficile Toxin, Stool for C.Diff see C. Difficile Toxin .........................720 Cryptococcal Antigen, Blood ......................................................................................721 Cryptococcal Antigen, CSF ........................................................................................722 Cryptococcus Stain see India Ink Prep ........................................................................723 Cryptosporidum Antigen .............................................................................................724 Culture, Anaerobic ......................................................................................................725 Culture, Candida .........................................................................................................726 Culture, Anal/Rectal for GC .......................................................................................727 Culture, Blood – Bacterial...........................................................................................728 Culture, Body Fluid .....................................................................................................729 Culture, Bone ..............................................................................................................730 Culture, Bone Marrow ................................................................................................731 Culture, Bone Marrow for AFB see Culture, Mycobacteria, Bone Marrow ...............732 Culture, Bronchial Washing ........................................................................................733 Culture, Catheter Tip ...................................................................................................734 Culture, CMV ..............................................................................................................735 Culture, CSF for AFB see Culture, Mycobacteria, CSF .............................................736 Culture, CSF & Gram Stain ........................................................................................737 Culture, Cytomegalovirus see Culture, CMV .............................................................738 Culture, Ear .................................................................................................................739 Culture, Eye.................................................................................................................740 Culture, Fungus ...........................................................................................................741 Culture, Fungus, Bone Marrow ...................................................................................742 Culture, Fungus, Skin ..................................................................................................743 Culture, Genital Sites ..................................................................................................744 Culture, Legionella ......................................................................................................745 Culture, Mycobacteria .................................................................................................746 Culture, Mycobacteria, Blood .....................................................................................747 Culture, Mycobacteria, Bone Marrow ........................................................................748 Culture, Mycobacteria, CSF ........................................................................................749 Culture, Mycoplasma Pnemoniae ...............................................................................750 Culture, Mycoplasma/Ureaplasma ..............................................................................751 Culture, Nose...............................................................................................................752 Culture, Pertussis.........................................................................................................753 Culture, Skin ...............................................................................................................754 Culture, Sputum and Gram Stain ................................................................................755 Culture, Stool ..............................................................................................................756 Culture, Throat (Comprehensive) ...............................................................................757 Culture, Throat Beta Strep Group A ...........................................................................758 Culture, Throat, for C. Diphtheria ...............................................................................759 Culture, Throat, for Neisseria Gonorrhoeae ................................................................760 Culture, Tissue ............................................................................................................761 Culture, Urine, Catheterized .......................................................................................762 Culture, Urine Midvoid Specimen ..............................................................................763 Culture, Urine, Suprapubic Puncture ..........................................................................764 Culture, Wound, Miscellaneous Sites .........................................................................765 Cyclospora Stain .........................................................................................................766 PCR for Neisseria Gonorrhoeae .................................................................................767 Enterovirus PCR (CSF) ...............................................................................................768 Fetal Fibronectin Test .................................................................................................769 Fungal Wet Prep see KOH Prep..................................................................................770 GBS Screen see Group B Strep Screen .......................................................................771 G.C. Culture, Throat see Culture, Throat, for Neisseria Gonorrhoeae .......................772 GC DNA Probe see DNA Probe for Neisseria Gonorrhoeae ......................................773 Giardia Antigen ...........................................................................................................774 Gram Stain ..................................................................................................................775 Group B Strep Screen (Culture/PCR) .........................................................................776 India Ink Prep ..............................................................................................................777 Influenza PCR .............................................................................................................778 KOH Prep ....................................................................................................................779 Legionella Culture see Culture, Legionella ................................................................780 Legionella DFA ...........................................................................................................781 Legionella Urine Antigen ............................................................................................782 MAV Blood Culture see Culture, Mycobacteria, Blood .............................................783 Maximum Bactericidal Dilution (MBD) .....................................................................784 MBC see Minimum Bactericidal Concentration .........................................................785 MBD see Maximum Bactericidal Dilution (MBD) ....................................................786 MIC see Minimum Inhibitory Concentration (Send Out Test) ...................................787 Minimum Bactericidal Concentration .........................................................................788 Minimum Inhibitory Concentration (Special request Send Out Test) ........................789 MRSA Screen PCR .....................................................................................................790 MRSA/SA Screen PCR (soft tissue) ..........................................................................791 O& P, Stool for Amoeba, Worm Identification see Ova and Parasites ......................792 Occult Blood, Guaiac Method.....................................................................................793 Pinworm Exam ............................................................................................................794 Pinworm Prep see Pinworm Exam ..............................................................................795 Pneumocystis DFA......................................................................................................796 Respiratory Syncytial Virus ........................................................................................797 Rotavirus Exam ...........................................................................................................798 RSV Exam see Respiratory Syncytial Virus ...............................................................799 Schlicter Test see Maximum Bactericidal Dilution (MBD)........................................800 Scotch tape prep see Pinworm Exam ..........................................................................801 Semen Analysis ...........................................................................................................802 Serum Cidal Test see Maximum Bactericidal Dilution (MBD) ..................................803 Skin scrapings for fungus see Culture, Fungus, Skin..................................................804 Sperm Post Vasectomy ...............................................................................................805 Sputum for PCP see Pneumocystis DFA ....................................................................806 Staph aureus/MRSA Nasal Screen PCR .....................................................................807 Stool for Blood see Occult Blood, Guaiac Method .....................................................808 Stool for Enteric Pathogens see Culture, Stool ...........................................................809 Stool for Guaiac see Occult Blood, Guaiac Method ...................................................810 Trichomonas Rapid Test .............................................................................................811 Urine for G.C. see Culture, Urine for Neisseria Gonorrhoeae ....................................812 VRE PCR ....................................................................................................................813 Wet prep for Trichomonas see Trichomonas Prep ......................................................814 Whooping Cough see Culture, Pertussis .....................................................................815 URINALYSIS ............................................................................................ 816 Clinitest .......................................................................................................................817 Eosinophils in Urine ....................................................................................................818 EOUR see Eosinophils in Urine ..................................................................................819 Hemosiderin, Urine .....................................................................................................820 Routine Urine see Urinalysis - Routine ......................................................................821 Urinalysis – Routine ....................................................................................................822 Urine Bilirubin ............................................................................................................823 Urine Blood .................................................................................................................824 Urine Glucose..............................................................................................................825 Urine Iron see Hemosiderin, Urine .............................................................................826 Urine Ketones..............................................................................................................827 Urine Leukocyte Esterase ...........................................................................................828 Urine Nitrites ...............................................................................................................829 Urine pH ......................................................................................................................830 Urine Protein ...............................................................................................................831 Urine Specific Gravity ................................................................................................832 Urine Urobilinogen .....................................................................................................833 PREFACE This manual is dedicated to continued excellence in service by the laboratory staff of the Lawrence + Memorial Hospital. It is designed to improve communication between laboratory personnel and staff physicians, nurses, health unit coordinators and medical assistants who utilize the services of the laboratory. An attempt was made to list pertinent details regarding each test: the type of specimen required; section performing test; turn-around time and reference values. The availability of each test is also indicated under the specific test listing. The test listings are arranged alphabetically by department and alphabetically in the index of this manual. A STAT LIST is included for quick reference (See pages 25- 26). For the purposes of this manual, the department is divided into nine sections including Anatomic Pathology, Blood Bank, Reference Lab, Chemistry, Coagulation, Cytology, Hematology, Microbiology, and Urinalysis. Support is supplied by the Information Services, Phlebotomy, Secretarial, Central Receiving Center and Call Center sections. The laboratory is inspected and approved by the College of American Pathologists, Joint Commission, and CLIA. Extensive quality control programs include proficiency surveys of the American Society of Clinical Pathologists and College of American Pathologists. A repeat laboratory test will be performed at no extra charge whenever a physician has any question as to the validity of a test result. Staff consultation will be available if needed to resolve such questions. Pathologists: Victoria G. Reyes-D'Arcy, M.D., D.A.B. Director of Laboratories Joseph C. Benedict, M.D., D.A.B. Associate Pathologist Nicole E. Muscato, M.D., D.A.B. Associate Pathologist Kevin B. Green, M.D., D.A.B. Associate Pathologist Anica Antic, M.D., D.A.B. Associate Pathologist Asim Ejaz, M.D., D.A.B. Associate Pathologist Elise L. Krejci, M.D., D.A.B. Associate Pathologist Pathologist Assistant: Michelle Zaremba, MHS, PA (ASCP) Administrative Director: Nicole Gomes, BS, MT (ASCP) Administrative Director of Laboratory Administrative Consultant: Judith Portelance, MS, BS, DLM (ASCP) Administrative Consultant Section Managers: Joan Blessing, BA - Pathology Office Manager Kimberly Brown, MBA , BS, HTL (ASCP) –Histology Darleen Chretien, BS, MT (ASCP) - Pequot Laboratory Elizabeth DeRosa, BS, MT (ASCP) SBB - Blood Bank Sarah Glennon, MAT, BS M, MLT (ASCP) – Phlebotomy Melissa Grandolfi, MS, CT (ASCP) - Cytology Barbara Naillis, BS, MT (ASCP) - Chemistry/Serology/Point of Care Testing Reference Lab Peter Speciale, MHS, PHD, M (ASCP) sm – Microbiology Audrey Turner, AS, PBT (ASCP) – Outreach/Call Center/Central Receiving Center Pedro Ugarelli, MS, BS, MT (ASCP) - Coagulation/Hematology/Urinalysis, Cancer Center Laboratory Laboratory Main Number: x5101 Test Priorities The following test priorities are available: ROUTINE: These specimens are collected beginning at 4:00 AM the morning after receiving the order. STAT: Includes selected tests (see STAT List Page 26), which can be ordered 24 hours per day, 7 days per week. These tests will be collected and processed immediately. (Average turn-around time: one (1) hour after receipt). URGENT: These tests can be ordered any time with telephone notice and followed by an order. It should be noted that collection of the specimen is immediate. The specimen will be processed with the next regularly scheduled run. Inpatients vs Outpatients Inpatients Tests for inpatients are available as ROUTINE, STAT, and URGENT. Outpatients Tests for outpatients are handled as ROUTINE whenever possible. In certain circumstances (arrival of specimen after last regularly scheduled run or specialized test which is not run on a daily basis), test requests may receive STAT handling. STAT tests are available for emergency department patients. Outpatients requiring laboratory services are registered by the outpatient registration staff. They are then directed to the outpatient laboratory where the specimen(s) is obtained. Outpatient laboratory areas and hours of operation include: ACC Building: Monday through Friday 6:30 AM to 6:00 PM, Saturday 7:00 AM to 12 noon Pequot Treatment Center: Monday through Sunday 6:30 AM to 7:00 PM Flanders Health Center: Monday through Friday 6:30 AM to 5:00 PM; Saturday 7:00 AM to 12 Noon. Shaw's Cove Patient Facility: Monday through Friday 8:30 AM to 5:00 PM. Home Blood Drawing As a convenience for our homebound patients, we offer a home blood drawing service. To provide this service we must receive a L&M HOME DRAW REQUEST FORM that has been filled out completely, signed and dated by the ordering physican specifying the date of service to start as well as the frequency of draw for the ordered test(s). We prefer at least one day's notice for all home draw requests. To request a blank home draw requisition, please call 860-444-5101. STAT Laboratory Work Only the following tests are available as STAT procedures. Others can occasionally be performed by arrangement with the Pathologist on call. HEMATOLOGY: CBC Platelet Count Hemoglobin (Hgb) Hematocrit (Hct) White Blood Count (WBC) Spinal Fluid Counts (CSFCT) IMMUNOLOGY/SEROLOGY: Pregnancy test Monospot BhCg. QuantEstradiol and Progesterone Mon-Fri 7-11 PM Sat & Sun 7-3 PM Amniotic Fluid - PG Slide test only. *L/S Ratio must be approved by Pathologist on call COAGULATION: Fibrinogen Level Prothrombin Time INR Activated Partial Thromboplastin Time (APTT) D-Dimer BLOOD BANK: Emergency release of group O packed cells ABO/Rh Antibody screen Transfusion Reaction Workup Crossmatch Direct Antiglobulin Test CHEMISTRY: Acetone Alcohol (Medical reasons only; not MEDICAL LEGAL) Amylase Bilirubin BUN Calcium Creatinine Lithium Drugs of Abuse Screen Electrolytes (Na, K, Cl, CO2) Therapeutic Drugs Enzymes (Alk Phos, CPK, LDH, SGOT, SGPT) Glucose Ionized Calcium Lactic Acid Salicylate Spinal Fluid protein and sugar TP-A/G Uric Acid Lithium Theophylline Therapeutic Drugs Heart Profile (Troponin & CPK-MB) Carboxyhemoglobin Methemoglobin MICROBIOLOGY: Blood Culture Drawn Spinal Fluid Culture Planted Gram Stain of spinal fluid or sputum FFN (Fetal Fibronectin) Rapid (10 minute) Beta Strep Screen URINALYSIS: Complete urinalysis Any culture after 11:00 PM considered 'STAT' by the attending M.D. can be processed on request. Routine cultures received after 11:00 PM are placed in the night specimen refrigerator and processed the next morning. Laboratory Critical Results (Panic Values): The following is a list of those life-threatening values, which must be telephoned to the physician or representative: White Blood Count Absolute neutrophils Blasts Babesia, Malaria, Ehrlichia Hemoglobin Hematocrit Platelet Count INR PTT Fibrinogen Bilirubin, newborn (0-30 d) Bilirubin, cord blood Serum Calcium Glucose Potassium Sodium CO2 Creatinine Troponin Blood Culture CSF Gram Stain and Culture Isolation of Presumed E coli 0157 Culture Gram Stain, Sterile Body Site AFB Smear, Inpatient Direct Coombs, Cord Blood Arterial/Venous Blood Gas Arterial/Venous Blood Gas Arterial Blood Gas Acetaminophen Digoxin Dilantin (Phenytoin) Gentamicin Lithium Phenobarbital Salicylate Tegretol (Carbamazepine) Theophylline Tobramycin Valproic Acid Vancomycin ≤ 2,000 OR ≥ 35,000 white cells/dl ≤ 1,000 neutrophils/dl Present Present ≤ 7.0 gm/dl ≤ 20% Newborn (0-60 days) ≤ 30% OR ≥ 65% Child (2 months to 6 years) ≤25% ≤ 50,000 platelets/dl ≥ 5.0 ≥ 100 seconds Newborn (0-30 days) ≥ 60 seconds > 1000 mg/dl > 15 mg/dl > 4 mg/dl ≤ 6.5 mg/dl OR ≥ 13 mg/dl ≤ 50 mg/dl OR ≥ 400 mg/dl Newborn (0-30 days) ≤ 40 mg/dl OR ≥ 200 mg/dl ≤ 3.0 mmol/L OR ≥ 6.0 mmol/L Newborn (0-30 days) ≤ 3.0 mmol/L OR ≥ 6.5 mmol/L ≤ 120 mmol/L OR ≥ 155 mmol/L (adult: 17 yrs or older) Newborn/child (0 days – 16 yrs) ≤ 125 mmol/L OR ≥ 155 mmol/L ≤ 10 mmol/L ≥7.0 mg/dl Newborn (0-30 days) >1.5 mg/dl ≥1.00 ng/ml Positive Positive In stool Positive for organism associated with bioterrorism Positive Positive Positive PCO2 >50 mm Hg and pH <7.30 PCO2 <30 mm Hg and pH >7.50 PO2<55 mm Hg >150 ug/ml >2.0 ng/ml >30 ug/ml >10 ug/ml >1.5 mmol/L >50 ug/ml >30 mg/dl >15 ug/ml >20 ug/ml >10 ug/ml >120 ug/ml >60 ug/ml L+M Cancer Center Critical Results (Panic Values): The following is a set of results explicitly for use with lab results originating within the Cancer Center. For those labs, items on Cancer Center-specific list of critical laboratory results supersede the general critical results list. If the result is not on the Cancer-Center specific list, then the parameters on the general list stand. White Blood Count Blasts Hemoglobin Hematocrit Platelet Count INR Serum Calcium ≤ 500 OR ≥ 100,000 white cells/dl Forward only to pathologist for review. Do not call oncologist. ≤ 7.0 gm/dl ≤ 20% OR ≥55% ≤ 10,000 OR ≥ 1,000,000 platelets/dl ≥ 5.0 ≤ 6.0 OR ≥ 12.0 mg/dl Chloride ≤ 70 mmol/L OR ≥ 140 mmol/L CO2 ≤ 15 mmol/L OR ≥ 40 mmol/L Creatinine Glucose Magnesium Potassium Sodium AST ALT Uric Acid ≥2.0 mg/dl (If patient < 2.0 mg/dL previously) ≤ 50 mg/dL OR ≥ 350 mg/dl ≤ 1.1 mg/dL OR ≥ 3.6 mg/dl ≤ 3.0 mmol/L OR ≥ 5.5 mmol/L ≤ 125 mmol/L OR ≥ 155 mmol/L ≥ 500 U/L ≥ 500 U/L ≥ 12.0 mg/dl Critical results which indicate a possible life-threatening situation (i.e., Panic Values) are called to the floor or ordering/covering/on-call physician within 60 minutes after a critical result is obtained. The message is not given to clerical personnel in-house. Individuals may be designated by the physician to receive such critical results in the outpatient setting. The first and last name of the physician/office designee or nurse notified is recorded on the patient report. After hours and on weekends, critical values are also faxed to the outpatient office. Please refer to the policy Critical Tests and Critical Values in the L+M Hospital Policy Manual. ANATOMIC PATHOLOGY: The Pathology Department is chaired by Victoria Reyes MD. Histology and Autopsy are under the immediate direction of Kevin Green MD. The Dept is staffed at all times with AP/CP board certified pathologists. The Pathologist Assistant (PA) has been formally trained in laboratory and gross room safety, specimen accessioning in CoPath, and all grossing and tissue processing aspects, including touch preparations, frozen sections, and handling of different tissue specimens. All tissue removed in Lawrence + Memorial Hospital's Main Campus or satellite facilities must be processed by a pathologist or PA, and examined by a pathologist at the gross and/or microscopic level. Exempt specimens are approved by the Medical Executive Committee although ultimate discretion is left to the attending surgeon. Surgical Pathology reports on routine biopsy specimens are available within 48 hours following accession of the specimen. Slides for microscopic evaluation of routine cases are generally not available prior to 11:00 AM. Every effort will be made to expedite cases where early discharge of the patient is contingent upon the Surgical Pathology report. Large specimens requiring prolonged fixation, decalcification, ancillary testing, extra-departmental consultation, and sentinel lymph node cases may delay the Surgical Pathology report. Tissue is held for 2 weeks after the case is signed out. Slides and blocks are held for 10 years. The Pathology Dept. is located on the third floor of the Hospital on 3.3, and is open M-F for receipt of routine specimens from 8:00 AM until 4:00 PM and 8:00 AM to 12:00 noon on Saturday. An on-call pathologist is available 24/7/52. Slides for Outside Consultation: If a patient at Lawrence + Memorial Hospital is referred to an outside institution or if a clinician desires a second opinion from an outside institution, the Pathology Dept. must be notified such that slides and a copy of the surgical pathology report are forwarded to the outside institution in a timely manner. Ideally, twenty-four hours advance notice is given for such requests. Clinicians may also send outside slides and corresponding reports to the Pathology Department for review and documentation at L+M Hospital. Note that patients may not hand carry slides given risk of breakage or loss in transit. Slides and/or paraffin blocks sent in consultation to referral institutions are tracked by internal notation in CoPath. Critical Results: Defined critical results are relayed to the clinician in a timely manner. Every attempt will be made to record date and time of notification in the permanent record. Critical results include all new and/or unexpected malignancies (except skin), significant and unexpected findings, vasculitides, the presence of fat in endometrial or endoscopic biopsies, absence of chorionic villi in POC, and invasive fungal infections, among others. Critical results are reviewed from time to time by the Dept. Any changes are made at the level of Dept. Chair after discussion and notification within the Dept. Specimen Labeling: In accordance with the Lab’s accreditation agencies (CAP, JC) and its internal Specimen Labeling and Irreplaceable Specimen policy (available on the hospital intranet under Lab), all submitted specimens must be accompanied by a properly completed specimen label and Surgical Pathology Request Form. Specimen Container/Label: The specimen label must include at two patient identifiers (patient’s full name and date of birth). The specimen label must include the specimen source. Appropriate containers with fixative may be obtained from Surgical Pathology (x 5100) Surgical Pathology Request Form (Requisition): The Surgical Pathology Request Form must be completed by the physician /LIP or designee, and must include (but is not limited to): patient’s full name, date of birth, specimen source, ordering physician information, all relevant history and/or clinical impression, and any special orders/additional information (eg, orientation) to facilitate appropriate triage and diagnosis. Un/Mislabeled Specimens: Because an unlabeled or mislabeled specimen usually cannot be recollected, an Irreplaceable Specimen Form (ISF) will be sent to the MD/LIP for completion in the outpatient setting. If such a mislabeled or unlabeled specimen is received in-house (e.g., operating room, endoscopy suite, patient floor), it may be identified in Histology by a designated person. All events are documented and presented at Lab Quality Committee. Quality Referrals may be submitted, if appropriate.. Specimen Submission/Handling: Surgical specimens submitted from in-house patients are first ordered within the corresponding HIS under Pathology > Histology. Those specimens submitted from private offices do not enter the HIS. All specimens received should be accompanied by a paper Surgical Pathology Request Form (Requisition) that is retained on-site for a minimum of two years. Appropriate containers with fixative/preservative may be obtained from Surgical Pathology (x 5100). Routine Specimens: Test Availability: M-F 8a-4p; Sat. 8a-12p Prior Notification to Pathology: No Meditech Exam Requested: Routine/Permanent Paperwork Required: Surgical Pathology Request Form Specimen Handling: Formalin, Fresh/Saline (refrigerated) Specimen Submission: Routine Specimens are submitted in formalin for standard histology processing. Results are reported by a pathologist within 48 hours of receipt. Specimen may also be submitted fresh to the Histology Department with subsequent fixation in formalin. If specimens are submitted fresh or in saline (especially after hours), then every effort must be made to keep the specimens refrigerated and delivered to the Laboratory as soon as possible to preserve tissue integrity and decrease risk of compromised processing and interpretation. Fresh Specimens: Test Availability: M-F 8a-4p; Sat. 8a-12p Prior Notification to Pathology: No Meditech Exam Requested: Fresh Paperwork Required: Surgical Pathology Request Form (indicating FRESH specimen) Specimen Handling: Fresh, Immediate delivery Specimen Submission: Many ancillary tests (see Special Test Request/Submission section below) require fresh tissue specimens. These special tests cannot be performed on formalin fixed tissue. Therefore, clinicians may submit specimens fresh or in minimal saline (to keep the tissue moist) to ensure all potential appropriate testing may be performed. In such cases, specimens must be delivered immediately to the Laboratory and labeled “FRESH” for appropriate triage and processing, and to avoid compromise of specimen integrity. If the specimen is obtained after hours, specimens must be kept refrigerated. Consult a pathologist if questions arise. Intra-Operative Consultation Specimens: Test Availability: 24 hours Prior Notification to Pathology: Yes Meditech Exam Requested: Intra-Operative Consultation Paperwork Required: Surgical Pathology Request Form Intra-Operative Consultation Form Specimen Handling: Fresh, Immediate delivery Specimen Submission: Intra-Operative Consultation Specimens require immediate gross and/or microsopic evaluation by a pathologist during an operative procedure. Surgeons generally request intra-operative consultations to direct the immediate next step in surgery or to inform treatment. These specimens must be sent fresh to the Histology Department immediately for triage and interpretation, along with the Surgical Pathology Request Form and the Intra-Operative Consultation Form. The PA/Pathologist will perform either a Gross Consult, Touch Preparation, or Frozen Section on the submitted tissue. The Pathologist will render an interpretation and verbally communicate his/her findings to the requesting surgeon by phone or intercom. If additional fresh tissue is needed, then the pathologist will inform the submitting physician. Discussion between the pathologist and surgeon may occur during intraoperative consultations to obtain additional information (eg, other intra-op findings, diagnostic imaging results, previous patient history).Rarely the requesting physician may not be available to receive the result. In this situation, the pathologist will make every effort to speak directly with the surgeon and verbally communicate the intraoperative consultation findings. After the Intra-Operative Consult is performed, it is recorded on the Intra-Operative Consultation Form with the Pathologist's signed diagnosis. This Intra-Op Consult Form becomes part of the patient's record and is placed in the paper medical chart. If multiple specimens are sent for Intra-Operative Consult, EACH specimen must be accompanied by a complete label, Surgical Pathology Request Form, and Intra-Operative Consultation Form. Pathologists are made aware of scheduled intra-operative consults the day before the operation or when the O.R. schedule is delivered to the Laboratory. *If a non-scheduled consult is requested during an operation occurring between 8:00 AM and 5:00 PM, notify the Path Dept. at x5100 before sending tissue to Histology. *If an Intra-Operative Consultation is required on Sunday, a holiday, after 12:00 Noon on Saturday or after 5:00 PM on a weekday, the attending surgeon must contact the pathologist on-call by telephone to discuss, in advance, the pertinent clinical information and concerns to be addressed by the consult (margins, presence of tumor, specimen adequacy, etc). Stand-by or add-on cases that require intra-operative consult must be communicated to the Pathology office (x5100). Lymph Node Exam Specimens: Test Availability: 24 hours Prior Notification to Pathology: Yes Meditech Exam Requested: Lymph Node Exam Paperwork Required: Surgical Pathology Request Form Microbiology Orders Lymph Node Exam Form Specimen Handling: Fresh, Immediate delivery Specimen Submission: A Lymph Node Exam is typically reserved for cases to R/O Lymphoma and/or R/O Infection. Specimens are immediately sent sterile and fresh to Histology with a Surgical Pathology Request Form, a Lymph Node Exam Form, and Microbiology Orders. The specimen is triaged immediately in the fresh state and samples taken for all appropriate testing, at the discretion of the attending Pathologist, who may or may not consult with the surgical attending. Bone Marrow Specimens: Bone Marrow specimens involve multiple specimens that are handled in Hematology, Histology, and Pathology. For a step-by-step complete guide, please reference the Hematology Section: Bone Marrow. Consult a Pathologist with any questions. Special Test Request/Submission: Special, often ancillary and/or esoteric, tests may be requested by the submitting clinician and/or Pathologist. These tests may require specific handling, submission, preparation and additional paperwork. Any questions regarding special testing should be directed to the Pathology Department (x5100) prior to specimen collection to ensure appropriate and adequate tissue is obtained and submitted. Muscle Biopsy: Test Availability: M-Th 8a-12p Prior Notification to Pathology: Yes, 24 hours Meditech Exam Requested: Fresh Paperwork Required: Surgical Pathology Request Form Reference Lab Requisition Specimen Handling: Fresh, Immediate delivery Specimen Submission: The test is available M-Th prior to 12:00 Noon. Surgical Pathology (x5100) is to be notified 24 hours in advance and all appropriate paperwork completed (Reference Lab Requisition). Three portions of skeletal muscle will be obtained and submitted in two Price clamps. Specimens with attached Price clamps must be delivered immediately by the OR staff on saline-moistened gauze to Histology with a Surgical Pathology Request Form. The lab will process the specimen and properly package/ship the specimen to the reference laboratory according to protocol. Clamps will be returned to the O.R Cytogenetics/Chromosome Analysis/Karyotyping: Test Availability: M-F 8a-3p Prior Notification to Pathology: Yes Meditech Exam Requested: NA Paperwork Required: Reference Lab Cytogenetics Requisition Specimen Handling: Fresh/RPMI Specimen Submission: All cytogenetic testing (chromosome analysis, karyotyping, etc.) must be done on fresh tissue submitted in RPMI fluid. DO NOT PLACE IN FIXATIVE! Test orders are not placed in the HIS. For efficient testing, samples are to be submitted to Histology M-F, prior to 3pm. If a clinician plans to obtain the tissue sample: - Obtain necessary RPMI fluid and a Cytogenetics Requisition (for the reference lab) from Histology, prior to the scheduled procedure. - Place tissue sample (2-3mm pieces) in RPMI. - Return RPMI sample and requisition to Histology as soon as possible. If immediate submission is not feasible, keep RPMI refrigerated. - If an additional tissue sample is desired for routine histology, submit the specimen separately according to the Routine Specimen Submission/Handling guidelines (above) For Lab/Histology triage and submission: - Send a fresh specimen with the Surgical Pathology Request Form to Histology immediately, indicating specimen is for cytogenetics. Flow Cytometry (R/O Lymphoma): Test Availability: M-F 8a-3p Prior Notification to Pathology: Yes Meditech Exam Requested: NA Paperwork Required: Reference Lab Flow Cytometry Requisition Specimen Handling: Fresh/RPMI Specimen Submission: All flow cytometry testing (testing for lymphoma) must be done on fresh tissue submitted in RPMI fluid. DO NOT PLACE IN FIXATIVE! Test orders are not placed in the HIS. For efficient testing, samples are to be submitted to Histology M-F, prior to 3pm. If a clinician plans to obtain the tissue sample: - Obtain necessary RPMI fluid from Histology, prior to the scheduled procedure. - Place tissue sample (2-3mm pieces) in RPMI. - Return RPMI sample to Histology during working hours (M-F, 8-3pm), as soon as possible. If immediate submission is not feasible, keep RPMI refrigerated. **NOTE: A Pathologist will complete the Reference Lab Requisition; therefore the specimen must always be delivered directly to Histology staff to ensure proper communication of testing! - If an additional tissue sample is desired for routine histology, submit the specimen separately according to the Routine Specimen Submission/Handling guidelines (above) For Lab/Histology triage and submission: - Send a fresh specimen with the Surgical Pathology Request Form to Histology immediately, indicating specimen is for flow cytometry. Histology + Microbiology (Shared Specimen): Test Availability: 24 hours Prior Notification to Pathology: No Meditech Exam Requested: Microbiology (as desired); Histology > Fresh Paperwork Required: Surgical Pathology Request Form Microbiology Orders Specimen Handling: Fresh, Immediate delivery Specimen Submission: Separate and distinct specimens for histology and microbiology are preferred for lab submission. In the event only a single specimen is obtained and a clinician would like both histology and microbiology performed: - The specimen must be submitted sterile/fresh with a pink "Shared Specimen" sticker. - Histology and Microbiology orders and requisitions are completed and delivered with the one specimen. - Specimen and paperwork are submitted to the following department for triage M-F 7a-5p = Deliver to Histology M-F 5p-11p = Deliver to Central Receiving Center (CRC) M-F 11p-7a = Deliver to Microbiology Saturday 7a-12p = Deliver to Histology Saturday 12p-11p = Deliver to Central Receiving Center (CRC) Saturday 11p-7a = Deliver to Microbiology Sunday 7a-11p = Deliver to Central Receiving Center (CRC) Sunday 11p-7a = Deliver to Microbiology Foreign Bodies/Implants (Gross Only): Test Availability: M-F 8a-4p Prior Notification to Pathology: No Meditech Exam Requested: Routine/Permanent; Fresh Paperwork Required: Surgical Pathology Request Form Specimen Handling: Fresh; Formalin Specimen Submission: Foreign bodies, etc. are handled as tissue specimens and sent to the lab. If the surgeon wants a specimen, he/she must sign a release form AFTER it is described (and preferably signed out) by the pathologist. Some specimens (e.g. teeth, gallstones) are given gross descriptions only as no tissue is available to process. Stone Analysis(Gross Only): Test Availability: M-F 8a-4p Prior Notification to Pathology: No Meditech Exam Requested: Routine/Permanent; Fresh Paperwork Required: Surgical Pathology Request Form Specimen Handling: Fresh; Formalin Specimen Submission: Stones can be handled as tissue specimens and sent to the lab. If the surgeon wants a specimen, he/she must sign a release form AFTER it is described (and preferably signed out) by the pathologist. In the event component analysis is desired, stones can be sent to Specimen Processing. For detailed submission instructions, see CHEMISTRY: Stone Analysis Kidney Biopsy (Medical): Test Availability: M-F 8a-3p Prior Notification to Pathology: Yes Meditech Exam Requested: Routine; Fresh Paperwork Required: Surgical Pathology Request Form Specimen Handling: Fresh in labeled/oriented Petri Dish, Immediate delivery Specimen Submission: All non-neoplastic kidney biopsy testing must be done on fresh tissue. DO NOT PLACE IN FIXATIVE! Testing includes light, electron, and immunofluorescence microscopy For efficient testing, samples are to be submitted to Histology M-F, prior to 3pm., with a 24 hour notification. - Send tissue fresh on normal saline-moistened Telfa gauze in a sealed, labeled Petri dish. - Identify the cortical and medullary ends of the biopsies (preferably on the specimen label sticker). - Deliver to the Histology Lab immediately, with the Surgical Pathology Request Form, and notify a Histotechnologist, PA or a Pathologist. ** DO NOT leave the specimen without notifying Histology/Lab staff** Direct Immunofluorescence (IF): Test Availability: M-F 8a-3p Prior Notification to Pathology: Yes Meditech Exam Requested: Routine; Fresh Paperwork Required: Surgical Pathology Request Form Specimen Handling: Fresh; Michel's Transport Media Specimen Submission: All immunofluorescence testing for antibodies/autoimmune diseases, must be done on fresh tissue placed in Michel's Transport Media. DO NOT PLACE IN FIXATIVE! For efficient testing, samples are to be submitted to Histology M-F, prior to 3pm., with a 24 hour notification. If a clinician plans to obtain the tissue sample: - Obtain necessary Michel's Transport Media fluid from Histology, prior to the scheduled procedure. - Place tissue sample in Michel's Transport Media. - Return sample to Histology during working hours (M-F, 8-3pm) with Surgical Pathology Request Form, indicating immunofluorescence testing (IF) testing is requested. - If an additional tissue sample is desired for routine histology, submit the specimen separately according to the Routine Specimen Submission/Handling guidelines (above) For Lab/Histology triage and submission: - Send a fresh specimen with the Surgical Pathology Request Form to Histology immediately, indicating specimen is for immunofluorescence testing (IF). **Indicate if entire specimen is for IF, or to be split for both IF and routine histology** Quantitative Iron/Copper: Test Availability: M-F 8a-3p Prior Notification to Pathology: No Meditech Exam Requested: Routine/Permanent Paperwork Required: Surgical Pathology Request Form Specimen Handling: Formalin Specimen Submission: Liver biopsies can be submitted for Iron/Copper testing in the same manner as Routine Specimens. An indication should be made on the Surgical Pathology Request Form of either Iron or Copper test request. Transmission Electron Microscopy: Test Availability: M-F 8a-3p Prior Notification to Pathology: Yes Meditech Exam Requested: Routine; Fresh Paperwork Required: Surgical Pathology Request Form Specimen Handling: Fresh; Glutaraldehyde Specimen Submission: All transmission electron microscopy (TEM; EM) testing for cellular ultra-structure must be done on glutaraldehyde fixed tissue. DO NOT PLACE IN FORMALIN! For efficient testing, samples are to be submitted to Histology M-F, prior to 3pm., with a 24 hour notification. If a clinician plans to obtain the tissue sample: - Obtain necessary glutaraldehyde fixative from Histology, prior to the scheduled procedure. - Place tissue sample in glutaraldehyde fixative. - Return sample to Histology during working hours (M-F, 8-3pm) with Surgical Pathology Request Form indicating specimen is for transmission electron microscopy (TEM; EM). - If an additional tissue sample is desired for routine histology, submit the specimen separately according to the Routine Specimen Submission/Handling guidelines (above) For Lab/Histology triage and submission: - Send a fresh specimen with the Surgical Pathology Request Form to Histology immediately, indicating specimen is for transmission electron microscopy (TEM; EM). **Indicate if entire specimen is for EM, or to be split for both EM and routine histology** Autopsy (Adult): The autopsy suite is located on the second floor of the 100 building room #2.120B. The Medical Staff is encouraged to obtain a post-mortem examination in all cases of unusual deaths and of medicolegal and educational interest. The Post-mortem Examination Permission and Consultation Request, which can be found on the hospital intranet (i.e., autopsy permit), is obtained through the efforts of the attending physicians in cooperation with the Admitting Coordinator. The full policy/procedure for requesting an adult autopsy is located in Patient Care Services. When a valid permit for autopsy is obtained, the Laboratory is notified. The autopsy permit must be completed by the person assuming responsibility for burial of the deceased and witnessed by the attending physician or other individual obtaining permission. Under no circumstances should a funeral director be notified to remove a body on whom an autopsy permit has been obtained prior to release by the laboratory. Please note all autopsies are performed by a pathologist with the assistance of a Diener Service and/or of the Pathologists' Assistant (PA). Private post mortem examinations are available upon request and incur a charge for pathology services and hospital facilities. An autopsy will not be performed until the pathologist has, in-hand, a properly signed authorization. A valid permit is defined in Section 10-143 of the Connecticut State Public Health Codes: Section 19-143 Section 19a-286 (formerly Sec. 19-143). Autopsies, consent for. Performance or attendance by nonaffiliated physician. (a) Whenever any person dies and no postmortem examination or autopsy has been ordered pursuant to subsection (b) of section 19a-406, no physician shall conduct or assist in conducting any postmortem examination or autopsy upon the body of such deceased person without first obtaining the consent of whichever one of the following persons, eighteen years of age or older, assumes custody of the body for the purposes of burial; Father, mother, husband, wife, child, guardian, next of kin, friend or any person charged by law with the responsibility for burial. If two or more persons assume custody of the body, consent of one of them shall be deemed sufficient. Any such consent may be in writing or may be given by telephone provided a record of any such consent by telephone shall be kept by such physician for not less than three years. An autopsy may be performed at another facility or attended by a physician who is not affiliated with Lawrence + Memorial, but any resultant fees or expenses (including but not limited to costs of transfer of the deceased to another facility) will be borne by the person requesting those actions. Permission for autopsy may be obtained by telephone. The permission must be overheard by two witnesses to the conversation. When the family wishes to limit the extent of the examination, the restriction must be recorded on the autopsy permit form. In possible medicolegal cases, the Medical Examiner (ME) must be contacted at (860) 679-3980 before any suggestion regarding autopsy permission is made to the family of the deceased. Indications for Medical Examiner input include, but are not limited to: - Suspected toxin - Sudden or unexpected death - Death due to disease which might constitute a threat to the public health - Death at or related to the workplace - Death occurring under suspicious circumstances (e.g., child abuse) Note: ME Autopsies are performed on all homicide victims and gunshot victims. In addition, the vast majority of pedestrian deaths, Sudden Death syndrome, overdoses, industrial accidents, sudden and otherwise unexplained deaths under the age of 45, and a variety of other types of cases are subject to autopsy examination. Autopsies not falling under the jurisdiction of a Medical Examiner are limited to the bodies of individuals whose death is pronounced while in Lawrence + Memorial Hospital as an inpatient. These autopsies are performed as a service without charge to the family of the deceased. Arrangements for an autopsy on the body of deceased individuals not admitted to Lawrence + Memorial Hospital, including deaths occurring in the Emergency Department, may be made by the family on a fee-for-service basis, with the hospital and pathologist. Clinicians and pathologist may discuss the case before autopsy is performed to clarify any outstanding clinical concerns or questions. Clinicians are notified when the autopsy will be performed. Final anatomic diagnoses on post-mortem examinations will be sent to the attending of record for inpatient autopsy cases. Post-mortem examinations are performed in the hospital in the autopsy suite. Attending clinicians my request to be present the autopsy; however, performance of the post-mortem examination will not be delayed to accommodate such a request. Brain cutting is scheduled as needed. The Pathology Department has a consultant Neuropathologist, Dr. Solitaire, who provides comprehensive neuropathology services. Stillbirth/Fetal Death: If a fetus is born at a period of gestation of twenty weeks or greater and weighs 350gms or greater, and there is no attempt at respiration, no action of the heart and no movement of voluntary muscle, then such instances are recorded by the state as a fetal death, and a fetal death certificate must be filed. Any live birth (i.e., spontaneous respiration) will be treated as an adult death regardless of gestational age, and a death certificate must be completed. If a postmortem examination is requested for these cases, an autopsy permit must be completed by the attending physician and the laboratory notified. The fetus is taken to the morgue and security is also notified of a pending autopsy. If examination of the placenta is desired, the placenta should be sent to the laboratory as a Routine Specimen and accompanied by a completed Request for Placental Examination form. For a stillbirth prior to twenty weeks of gestation or less than 350 gms., a fetal death certificate is not filed. If a postmortem examination is desired, the fetus is sent to Histology for examination as a Routine Specimen. It is not necessary to obtain an autopsy permit. If an autopsy permit has been completed for a, then the submitting physician will be notified that the fetus will be examined in Surgical Pathology and an autopsy permit is not necessary. BLOOD BANK The Blood Bank is located on 3.3 at extension 5110. It is under the direction of Nicole Muscato, M.D. and is managed by Elizabeth DeRosa, BS, MT (ASCP)SBB. This section is accredited by the College of American Pathologists (CAP), and is registered with the Food and Drug Administration (FDA) and the State Department of Health. Blood Bank. Orders are entered directly into the Hospital Information system (HIS). In case of computer down time, a Universal Requisition is required for all orders. The requisitions are obtained from the stockroom and are to be filled out at the nurse's station with the following information: 1. Patient's demographic data 2. Check off necessary tests and indicate number of units 3. Priority - routine, STAT, today, outpatient date of transfusion or Preop Packed Cell units that are crossmatched are held a maximum of 4 days from the time the type and screen specimen was obtained (the only exception is for PAT specimens, see below). Definite transfusion order must include a Doctors Oders: Adult Blood Transfusion. Outpatient transfusions must also be scheduled through the Outpatient Infusion department or the Cancer Center. A completed and signed transfusion order from is faxed to 860-444-5163. Pre-Admission Testing Requisitions are required for preop orders. If the patient has not been pregnant or transfused in the last 3 months, then this specimen can be used for compatibility testing up to 21 days. The hospital obtains blood and blood components from the American Red Cross Blood Services in Farmington, CT. All donations are from volunteer donors and are tested with licensed screening tests for viral markers as required by the FDA. Besides blood and blood components, the Blood Bank also dispenses plasma derivatives such as Factor VIII, Factor IX, Novoseven and Rh Immune Globulin. Refer to the package inserts of specific products for more information. Therapeutic phlebotomy appointments are scheduled and drawn by personnel in the Outpatient Clinic (x2184). Blood obtained from therapeutic phlebotomies are labeled "Not For Transfusion" and are appropriately discarded in the Blood Bank. ABO and Rh Typing Synonyms: Group & Rh, Blood Typing, Blood Grouping. Type & Rh, ABO/Rh General Use: Identify blood type Test Mnemonic: ABRH (forward & reverse typing) ABRHF (forward typing only for neonates <4 months of age) Test Includes: ABO and Rh Blood Types Lab Performing Test: Blood Bank Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Positive patient identification Specimen Required: K2EDTA Blood Container Required: 6 ml K2EDTA Plasma Pink Top Volume of Specimen: 6 ml Minimum Volume of Specimen: 2 ml Causes for Rejection: Improper sample, improper labeling, excessive hemolysis Availability: 24 hours daily Time Required Routinely for Processing: 4-8 hours, STAT -1/2 hour ABS see Antibody Screen Albumin Contact the pharmacy Ante Partum RhIG, see Rh(D) Immune Globulin Antepartum Antibody Screen Synonyms: Indirect Antiglobulin Test, IAT, Indirect Coombs, Indirect AHG, Antibody Detection, Atypical Antibody Screening; ABS General Use: Detects atypical antibody(ies) in patient's serum Test Mnemonic: ABSR Test Includes: Antibody screen for Atypical Antibodies. Lab Performing Test: Blood Bank Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Positive patient identification Specimen Required: K2EDTA Blood Container Required: 6 ml K2EDTA Plasma Pink Top Volume of Specimen: 6 ml Minimum Volume of Specimen: 5 ml Causes for Rejection: Improper labeling, excessive hemolysis, insufficient volume, specimen more than 24 hrs old. Availability: 24 hours daily Time Required Routinely for Processing: 4-8 hours; STAT -3/4 hour Additional Information: If antibody screen is positive, antibody identification work up is performed. Reference Range: Negative Antibody Titer see Titer Autologous Donors Autologous Donations are no longer collected at Lawrence + Memorial Hospital. For information on donating Autologous blood, please contact the American Red Cross, CT region at: 860-678-2805 Blood Typing see ABO and Rh Typing Compatibility Testing see Red Blood Cells - Crossmatch Cord Blood General Use: To evaluate newborn for hemolytic disease of the newborn (HDN) and to determine mother's candidacy for Rh Immune Globulin. Test Mnemonic: CDEV Test Includes: ABO and Rh Typing and DAT Lab Performing Test: Blood Bank Request Form: Cord Blood (ABO/RH & Direct Coombs) - Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood Container Required: 10 ml red top tube, no separator Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml Routinely: CDEV is done on cord samples from group O mothers, Rh Negative mothers and mothers with clinically significant atypical antibodies. Otherwise the cord sample is held in the blood bank for 14 days. Causes for Rejection: Improper labeling - must have patient name, hospital number, date, mother's name and mother's hospital number Availability: 24 hours daily Time Required Routinely for Processing: 8 hours if routine; STAT - 1 hr Cryoprecipitate Synonyms: Cryoprecipitated Antihemophilic Factor, Cryoprecipitated AHF, CRYO General Use: Treatment of fibrinogen or factor XIII deficiency, or dysfibrinogenemia. Test Mnemonic: TCRY Testing required: ABO and Rh Type, if not known Lab Performing Test: Blood Bank Request Form: A transfusion order faxed to the blood bank is required (860-4445163). Signed order by physician/Health Professional Affiliate(HPA) specify # of units. Patient Preparation: Proper patient identification. Must sign Informed Consent for Transfusion Special Instructions: Can be used for only 6 hours (after thawing the pool of 5). Specimen Required: 2 independently collected ABO typings on file at L+M, or 1 pink top tube. Container Required: 6 ml K2EDTA Plasma Pink Top Volume of Specimen: 6 ml Minimum Volume of Specimen: 2 ml Availability: 24 hours daily Time Required Routinely for Processing: 1/2 hour Additional Information: Cryoprecipitate is supplied as a pool of 5 products. If 10 cryo units are ordered, 2 pools will be issued. They bags of 5 will not be pooled together. Product contains factor VIII, factor XIII, von Willebrand's factor and fibrinogen. Each unit contains approximately 10 ml of plasma. Reference Range: Usual dose is 10 units (2 pools of 5) Cryoprecipitated Antihemophitic Factor, Cryoprecipitated AHF, CRYO see Cryoprecipitate Direct Antiglobulin Test Synonyms: Direct Coombs, DAT, Direct AHG Test General Use: Detect antibody bound to patient's red cells Test Mnemonic: DAT Test Includes: Direct anti-human globulin test with polyspeciflc anti-human globulin serum. It may include use of monospecific reagents (anti-IgG, and anti C3d, C3b) when indicated. Lab Performing Test: Blood Bank Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Proper patient identification Specimen Required: Whole blood (EDTA). In case of a newborn a cord blood is used (see Cord Blood) Container Required: 6 ml pink top tube or cord blood. Volume of Specimen: 6 ml Minimum Volume of Specimen: 6 ml Causes for Rejection: Improper labeling, specimen greater than 24 hrs. old. Availability: 24 hours daily Time Required Routinely for Processing: 4-8 hours; STAT- 1/2 hr Additional Information: If the test with anti-IgG is positive, an eluate will be performed to identify the antibody coating the cells Reference Range: Negative DAT see Direct Antiglobulin Test Deglyced Red Cells see Red Blood Cells Deglycerolized - Crossmatch Direct Coombs, see Direct Antiglobulin Test FFP see Fresh Frozen Plasma Fresh Frozen Plasma Synonyms: FFP, 24 hr plasma General Use: Treatment of coagulation factor deficiencies. NOT indicated for condition responsive to volume replacements or when specific corrective factors (factor VIII and/or IX) are available Test Mnemonic: TFFP Test Includes: ABO and Rh Type, if not known. Thawing frozen plasma Lab Performing Test: Blood Bank Request Form: A transfusion order faxed to the blood bank is required (860-4445163). Signed order by physician/Health Professional Affiliate(HPA) specify # of units. Patient Preparation: Proper patient identification. Must sign Informed Consent for Transfusion Special Instructions: Must be used within 24 hours after thawing Specimen Required: 2 independently collected ABO typings on file at L+M or 1 pink top tube. Container Required: 6 ml K2EDTA Pink Top Volume of Specimen: 6 ml pink top tube Minimum Volume of Specimen: 2 ml Availability: 24 hours daily Time Required Routinely for Processing: 1/2 hour Additional Information: FFP contains plasma proteins including all coagulation factors. Frozen Red Cells see Red Blood Cells Deglycerolized - Crossmatch Group & Rh, see ABO and Rh Typing HLA-ABC Synonyms: ABC typing for HLA General Use: For Bone Marrow, Stem Cell or Platelet matching Test Mnemonic: HLAABC Lab Performing Test: American Red Cross, Connecticut Region, HLA lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood (EDTA) Container Required: Lavender Top Tube (EDTA) Volume of Specimen: 12ml - draw 3 EDTA tubes Minimum Volume of Specimen: 10ml Availability: Draw any day of week; Sent Mon-Thursday Time Required Routinely for Processing: 1 week HLA-DRDQ Synonym: DR typing for HLA General Use: For Bone Marrow, Stem Cell or Platelet matching Test Mnemonic: HLADRQ Lab Performing Test: American Red Cross, Connecticut Region, HLA lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood (EDTA) Container Required: Lavender Top Tube (EDTA) Volume of Specimen: 12ml - draw 3 EDTA tubes Indirect Antiglobulin Test, see Antibody Screen Indirect Coombs see Antibody screen Packed Red Cells, see Red Blood Cells – Crossmatch Panel, see Antibody Identification Pediatric Packed Cells General Use: Packed cell aliquot infusions should not exceed 4 hours. Mother’s K2EDTA specimen may be used for antibody screen and crossmatch if unable to obtain a clotted specimen from infants under 1 week of age. Test Mnemonic: XM Test Includes: Type and screen, if not already determined on current admission Lab Performing Test: Blood Bank Request Form: Signed order by physician/Health Professional Affiliate(HPA) and a transfusion order form faxed to 860-444-5163. Patient Preparation: Positive patient identification Special Instructions: This is only for neonates <4 months of age. After 4 months order PC (Packed Cells) Specimen Required: K2EDTA Blood Container Required: 3 ml K2EDTA lavender top Minimum Volume of Specimen: 1 ml Causes for Rejection: Improper labeling, excessive hemolysis Availability: 24 hours daily Time Required Routinely for Processing: 1 hour Additional Information: Unless there is an extreme emergency, pedi units are CMV negative, irradiated and negative for HgBs and issued in a syringe. Phlebotomy see Therapeutic Phlebotomy Platelet Concentrate Synonyms: Platelet Packs; Platelets; Random Donor Platelets; Platelet Transfusions, Pooled Platelets. See also – Pre-Pooled platelets General Use: To treat bleeding due to thrombocytopenia or platelet function abnormality Test Mnemonic: TPPL or TPPH (pheresis) Test Includes: ABO and Rh Type, if not known Lab Performing Test: Blood Bank Request Form: Request must be phoned to the Blood Bank when the order is initiated. Transfusion order faxed to the blood bank is required (860- 444-5163). Signed order by physician/Health Professional Affiliate(HPA) specify number of units requested. Patient Preparation: Proper patient identification. Must sign Informed Consent for Transfusion Special Instructions: Platelets are no longer supplied by individual platelet concentrates. Platelets are supplied and issued in pools of 5. They have a 5 day expiration period. One pool of 5 is considered one dose. Specimen Required: 2 independently collected ABO typings on file at L+M, or 1 pink top tube. Container Required: 6 ml K2EDTA Pink Top Volume of Specimen: 6 ml Minimum Volume of Specimen: 2 ml Causes for Rejection: Normal platelet count improper labeling of specimen Additional Information: One dose of pooled platelets is expected to increase the platelet count of an adult with a blood volume of 5000 ml about 35,000 to 50,000/mm3. Reference Range: Usual adult dose 5 units pooled. Platelet Packs see Platelet Concentrate Pooled Platelets, see PrePooled Platelets Prenatal Rhogam see Rh (D) Immune Globulin Antepartum PrePooled Platelets Synonyms: Platelet Packs; Platelets; Random Donor Platelets; Platelet Transfusions, Pooled Platelets. General Use: To treat bleeding due to thrombocytopenia or platelet function abnormality. PrePooled Platelets contain 5 random donor platelets pooled together in a closed system that maintains the 5 day expiration. The platelets are pooled and tested for bacterial contamination by the blood supplier. Test Mnemonic: TPPL Test Includes: ABO and Rh Type, if not known Lab Performing Test: Blood Bank Request Form: Request must be phoned to the Blood Bank when the order is initiated. A transfusion order faxed to the blood bank is also required (860-4445163). Signed order by physician/Health Professional Affiliate(HPA), specify number of units. Patient Preparation: Proper patient identification. Must sign Informed Consent for Transfusion Special Instructions: PrePooled Platelets have a 5 day expiration period. Specimen Required: 2 independently collected ABO typings on file at L+M, or 1 pink top tube. Container Required: 6 ml K2EDTA Pink Top Volume of Specimen: 6 ml Minimum Volume of Specimen: 2 ml Causes for Rejection: Normal platelet count, improper labeling of specimen Additional Information: One dose of prepooled platelets is expected to increase the platelet count of an adult with a blood volume of 5000 ml about 35,000 to 50,000/mm3. Reference Range: One dose = 5 random platelets Random Donor Platelets see Pre-pooled platelets Red Blood Cells - Crossmatch Synonyms: Packed Red Cells, Compatibility Testing, Type and Crossmatch. General Use: Transfusion of patients with symptomatic anemia for restoration of oxygen - carrying capacity. Infusion should not exceed 4 hours per unit Test Mnemonic: XM Test Includes: ABO and Rh Type, antibody screen and crossmatch Lab Performing Test: Blood Bank Request Form: A transfusion order faxed to the blood bank is required (860-4445163). Signed order by physician/Health Professional Affiliate(HPA), specify number of units. Patient Preparation: Positive patient identification. Must sign Informed Consent for Transfusion Special Instructions: Crossmatched blood held for a maximum of 3 days. Specimen Required: K2EDTA Blood Container Required: 6 ml K2EDTA Pink Top Volume of Specimen: 6 ml Minimum Volume of Specimen: 5 ml Causes for Rejection: Improper labeling, excessive hemolysis, insufficient volume, specimen more than 24 hrs. old. Availability: 24 hours daily Time Required Routinely for Processing: 10 minutes with completed Type and Screen, otherwise 45 minutes Additional Information: Blood available uncrossmatched in emergency per physicians order. Release form for uncrossmatched blood is initiated by Blood Bank and must be signed by the physician. Red Blood Cells Deglycerolized - Crossmatch Synonyms: Frozen Red Cells; Deglyced Red Cells; Washed Cells General Use: Only used for patients with difficult compatibility problems or severe reactions to plasma proteins Test Mnemonic: XM Test Includes: Group, Rh, antibody screen & compatibility testing Lab Performing Test: Blood Bank and Connecticut Red Cross Blood Services Lab Request Form: A transfusion order faxed to the blood bank is required (860-444-5163). Signed order by physician/Health Professional Affiliate(HPA). Patient Preparation: Proper patient identification. Must sign Informed Consent for Transfusion Specimen Required: K2EDTA Blood Container Required: 6 ml K2EDTA Pink Top Volume of Specimen: 6 ml Minimum Volume of Specimen: 5 ml Causes for Rejection: Improper labeling, excessive hemolysis, insufficient volume, specimen more than 24 hrs old. Availability: Not STAT, weekdays. Product must be obtained on special order from American Red Cross Blood Services. Special transportation needed. Time Required Routinely for Processing: 24 hours Additional Information: Product when thawed has a 24-hour shelf life. Red Blood Cells Leukocyte Reduced - Crossmatch Synonyms: Buffy Coat Poor Blood, White Cell Poor Blood General Use: To prevent recurrent febrile, non-hemolytic transfusion reactions or HLA alloimmunization. Test Mnemonic: XM Test Includes: ABO and Rh Type, Antibody screen and crossmatch Lab Performing Test: Blood Bank Request Form: A transfusion order faxed to the blood bank is required (860-4445163). Signed order by physician/Health Professional Affiliate(HPA). Patient Preparation: Proper patient identification Special Instructions: Must sign Informed Consent for Transfusion Specimen Required: K2EDTA Blood Container Required: 6 ml K2EDTA Pink Top Volume of Specimen: 6 ml Minimum Volume of Specimen: 5 ml Causes for Rejection: improper labeling, excessive hemolysis, insufficient volume, specimen more than 24 hrs old. Availability: 24 hours daily Time Required Routinely for Processing: 10 minutes with completed TYSC; otherwise 45 minutes Additional Information: Red Cells are filtered pre-storage at the American Red Cross through blood filters that remove >99% of the White Cells. Rh Titer, Antibody Titer, Antibody Quantitation, Atypical Antibody Titer see Titers Rh(D) Immune Globulin Synonyms: RhoGam; RhIG General Use: Given to D-negative women to prevent development of Anti-D and hemolytic disease of newborn in subsequent pregnancies Test Mnemonic: TRHG RHEV (full work up, including antibody screen) Test Includes: Fetal screen to detect fetal-maternal hemorrhage greater than 30 ml Lab Performing Test: Blood Bank Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Proper patient identification Special Instructions: Blood required from both mother and baby Specimen Required: Clotted blood from infant; EDTA tube from mother Container Required: 10 ml red top tube (no separator) from the cord, and a 6 ml Pink Top for mother or capillary tube for newborn Volume of Specimen: 10 ml red top tube, cord sample(no separator) and a 6 ml Pink Top from mother. If cord is unavailable, capillary tubes from heel stick Minimum Volume of Specimen: 3 ml for mother, 1 ml for newborn Causes for Rejection: Baby Rh-negative, mother D-positive, or active anti-D present in maternal serum Availability: Routine days Time Required Routinely for Processing: Up to 4 hours Additional Information: Dosage of Rh(D) immune globulin is determined by a fetal screen done by Blood Bank on postpartum maternal blood. If fetal screen is positive, a quantative test is done by the Hematology. Rh(D) Immune Globulin Antepartum Synonyms: Antepartum RhIG, Prenatal Rhogam General Use: Given to Rh-negative women to prevent the development of anti-D and hemolytic disease of newborn in subsequent pregnancies Test Mnemonic: TRHG Test Includes: Antibody Screen as ordered Lab Performing Test: Blood Bank Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Proper patient identification Special instructions: Given to D-negative mothers during the 26th - 28th week of pregnancy, who have not previously produced anti-D Specimen Required: K2EDTA Blood Container Required: 6 ml Pink Top Volume of Specimen: 6 ml from patient Minimum Volume of Specimen: 5 ml Collection: Collect specimen before dose of RH(D) Immune Globulin is given Causes for Rejection: If patient is D-positive, or an active, immune anti D is detected in the mother’s plasma. Availability: Routine Contraindications: If mother known D-Positive, or has produced Anti-D RhIG see Rh(D) Immune Globulin RhoGam see Rh(D) Immune Globulin Salt Poor Albumin, Normal Serum Albumin, 25% Serum Albumin, 5% Albumin see Albumin Product Contact the pharmacy Therapeutic Bleeding see Therapeutic Phlebotomy Therapeutic Phlebotomy Synonyms: Therapeutic Bleeding; Phlebotomy Test Mnemonic: PHLEB Test Includes: Drawing up to 450 ml of blood from patient Lab Performing Test: Blood Bank or Outpatient Clinic (by appointment) phone # Ext 2184 Request Form: Patient must have a physician order. New standing orders are required every 12 months. Signed order by physician/Health Professional Affiliate(HPA). Patient Preparation: Hemoglobin or hematocrit determination on chart less than 48 hours old. Must sign consent for the procedure. Vital signs must be documented immediately prior. Special Instructions: Outpatient appointments made with Outpatient Clinic 4420711 Ext #2184. Container Required: Blood donor bag Volume of Specimen: Up to 500 mL Causes for Rejection: Discretion of pathologist Availability: Weekdays only 8:00AM -4:30PM; emergency therapeutic Phlebotomies cleared through a pathologist Time Required Routinely for Processing: 1 hour Titer Synonyms: Rh Titer, Antibody titer, Antibody Quantitation, Atypical Antibody Titer General Use: To quantitate antibody Test Mnemonic: ATIT (only orderable by blood bank staff.) Order ABSR or PREN1 Test Includes: Antibody screen (detection), identification and antibody titer Lab Performing Test: Blood Bank Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Positive patient identification Specimen Required: K2EDTA Blood Container Required: 6 ml Pink Top Volume of Specimen: 6 ml Minimum Volume of Specimen: 4 ml Causes for Rejection: Improper labeling, excessive hemolysis, insufficient volume, specimen more than 24 hrs old. Availability: Routine weekdays Time Required Routinely for Processing: Up to 8 hours Additional Information: Titers are only be done if antibody is present in patient's plasma and is considered clinically significant and the patient is pregnant. Transfusion Reaction Review General Use: Investigate transfusion problems Test Mnemonic: TRXRX Test Includes: DAT, Compatibility Studies, Urine for Blood and Chemistry Studies as necessary. Workup may be modified by Blood Bank in accordance with AABB/FDA/CAP guidelines. Lab Performing Test: Blood Bank Request Form: Lawrence + Memorial Hospital Suspected Transfusion Reaction Report (L+M- 278 Lab) Patient Preparation: Positive patient identification Special Instructions: Follow instructions on back of the product. Attending physician must be notified prior to calling Blood Bank Container Required: 6 ml K2EDTA Pink Top Volume of Specimen: 6 ml K2EDTA Minimum Volume of Specimen: 6 ml pink top Availability: STAT, 24 hours daily Time Required Routinely for Processing: Varies with type of reaction reported Specimen Required: Post transfusion pink top tube. Additional Information: Blood container must be sent to Blood Bank with the Transfusion Record, include tubing and saline bag. Reference Range: N/A Type & Screen Synonyms: Cells and Serum, Gr, Rh & Scr General Use: Required for Pre-transfusion testing. Determination of ABO/Rh and possible presence of an atypical antibody. Test Mnemonic: TYSC Test Includes: ABO and Rh Type and antibody screen Lab Performing Test: Blood Bank Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Positive patient identification Specimen Required: K2EDTA specimen Container Required: 6 ml K2EDTA Pink Top Volume of Specimen: 6 ml Minimum Volume of Specimen: 5 ml Causes for Rejection: Improper labeling, excessive hemolysis, insufficient volume, specimen more than 24 hrs old. Availability: 24 hours daily Time Required Routinely for Processing: 4-8 hours; STAT - hour Additional Information: Decreases crossmatch time should transfusion become necessary. If antibody screen is positive, antibody identification will be done. For npatients with antibodies, 2 units will be made available until the specimen expires. Washed Cells see Red Blood Cells Deglycerolized - Crossmatch Reference Lab The Reference Lab section is directed by Victoria G. Reyes-D'Arcy, M.D. and supervised by Barbara Naillis. The Section is staffed Monday through Friday from 6:30 am to 11 pm. Limited services are available on weekends and holidays from 7 am to 3 pm. For Reference Lab services call ext 4153. The Supervisor can be reached at ext 3780. 1st Trimester Risk Screen General Use: Screening for fetal chromosome abnormalities. Test Mnemonic: FRSTTM Test Includes: PAPP-A, AFP, HcG, Inhibin, Estriol Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient is drawn in first trimester of pregnancy Special Instructions: Yale “Risk History” form needed at time of specimen collection. Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: No patient History from Availability: Can be drawn Mon-Sunday. Only sent to Yale Mon-Friday (no holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report 5-Hydroxyindolacetic Acid, Quantitative, 24 hour Urine Synonyms: 5HIAA-Quantitative General Use: Evaluate serotonin production as with carcinoid tumors Test Mnemonic: U5HI24 Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient should avoid food high in indoles: avocados, banana, tomato, plum, walnut, pineapple, and eggplant. Patient should also avoid tobacco, tea and coffee three days prior to specimen collection. Specimen Required: 24 hour urine Special Instructions: Keep refrigerated during collection Container Required: 24 hour urine container with preservative obtained from Specimen Processing Laboratory Volume of Specimen: Entire 24 hour collection Minimum Volume of Specimen: Entire collection Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report 5' Nucleotidase, Blood General Use: Parallels the activity of alkaline phosphatase in liver disease but is not elevated in Rickets or Paget's disease. Test Mnemonic: 5NUC Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube, No gel barrier tubes!, Deliver immediately! Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Improper tube type, delay in transport to Lab Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 3-4 days Reference Range: See report 17-Hydroxyprogesterone General Use: 17-Hydroxyprogesterone is useful in detecting patients with congenital adrenal hyperplasia (CAH), monitoring cortisol replacement therapy, evaluating infertility and adrenal and overarian neoplasms. Test Mnemonic: 17HYDR Test Includes: Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Special Instructions: Specimen Required: Clotted blood (serum) Container Required: Red top tube, No gel Volume of Specimen: 1.0 mL serum Minimum Volume of Specimen: 1.0 mL serum Causes for Rejection: SST Tube Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report 17-Ketosteroids, Total, 24 hour Urine Synonyms: 17-KS General Use: Evaluate Androgenic function Test Mnemonic: U17K24 Lab Performing Test: Specimen Processing; sent Reference Lab Request Form: Universal requisition; use as back up to Meditech Specimen Required: 24 hour urine Special Instructions: Keep refrigerated during collection Container Required: 24 hour urine container with preservative supplied by Specimen Processing Laboratory. Volume of Specimen: Entire collection Minimum Volume of Specimen: Entire 24 hr collection Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 3-7 days Reference Range: See report Acetylcholine Receptor Antibody Synonyms: ARA General Use: Useful in the diagnosis of Myasthenia gravis Test Mnemonic: ACTYAB Lab Performing Test: Specimen Processing; Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 5.0 mL Minimum Volume of Specimen: 2 mL Causes for Rejection: Excessive hemolysis Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 5 days Additional Information: May also be ordered as part of a Myasthenia gravis Panel Reference Range: See report Adenovirus Titer General Use: Used to support a diagnosis of viral infection due to Adenovirus Test Mnemonic: ADEN Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml. Minimum Volume of Specimen: 2 ml. serum Causes for Rejection: Gross hemolysis, chylous serum Availability: Sent out Mon-Sat. (not holidays) Time Required Routinely for Processing: 5 days Reference Range: See printed report Adrenocorticotrophic Hormone Synonyms: ACTH; Corticotrophin General Use: Pituitary function test useful in the differential diagnosis of Cushing's syndrome, Addison's disease and also in ectopic ACTH syndrome Test Mnemonic: ACTH Lab Performing Test: Specimen Processing - sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Fasting recommended Special Instructions: Sample should be drawn in am (7-10AM) - Deliver to lab immediately on ice. Commonly collected simultaneously with cortisol level. Specimen Required: Plasma (EDTA) Container Required: Lavender (EDTA) tube. Draw in pre-chilled tube, place on ice, and deliver ASAP! Volume of Specimen: 5 ml Minimum Volume of Specimen: 1 ml plasma Causes for Rejection: Gross hemolysis Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 4 days Additional Information: The ACTH level is affected by stress, which may obscure the normal diurnal change. ACTH level should be correlated with cortisol levels. Reference Range: See report AFFIRM VP DNA Probe Panel Synonym: Bacterial Vaginosis/Vaginitis Panel General Use: Testing for organisms associated with bacterial vaginosis Test Mnemonic: AFFIRM Test Includes: Candida Species, Trichomonas vaginalis, Gardnerella vaginalis Lab Performing Test: Specimen Processing; Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Vaginal swab Container Required: AFFIRM VPIII Ambient Temp Transport System (ATTS) Volume of Specimen: One swab Minimum volume: One swab Causes for Rejection: Specimens > 72 hrs old, frozen specimens or swabs received in transport systems other than AFFIRM Availability: Sent out Monday-Saturday (not holidays) Time Required Routinely for Processing: One week Additional Information: Cervical specimens should be avoided, specimens should not be collected if patient has used vaginal products in the previous 72 hours Reference Range: Not detected Aldolase, Blood Synonym: Fructose-1,6 bisphosphate General Use: Differential diagnosis of cellular necrosis, cartilage disorder, acute hepatitis, progressive muscular dystrophy, myocardial infarction, pancreatitis Test Mnemonic: ALDO Lab Performing Test: Specimen Processing - sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml blood Minimum Volume of Specimen: 3 ml serum Causes for Rejection: Gross hemolysis, icterus, lipemia Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 2 days Reference Range: See report Aldosterone, 24 hour Urine General Use: Determining adrenal cortical function and renal hypertension Test Mnemonic: UALD24 Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Keep refrigerated during and after collection Specimen Required: 24 hour urine collection Container Required: 24 hour urine container with 10gms boric acid, supplied by Specimen Processing lab Volume of Specimen: Entire collection Minimum Volume of Specimen: Entire collection Availability: sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 6 days Reference Range: See report Aldosterone, Serum General Use: Evaluation of adrenal function Test Mnemonic: ALDS Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Draw “upright” samples at least ½ hour after patient sits up Specimen Required: Clotted blood (serum) Container Required: Plain Red top – no gel barrier! Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: SST tube Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See report Alkaline Phosphatase Isoenzymes, Blood Synonyms: Alkaline Phosphatase Fractionation General Use: Differentiate liver disease and bone disease Test Mnemonic: ALKISO Lab Performing Test: Specimen Processing, sent to Reference Lab Patient Preparation: Overnight fasting preferred Special Instructions: Age and sex of patient are necessary for interpretation of results Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum). Spin within 30 min Container Required: Red top tube (SST) Volume of Specimen: 10 ml blood Minimum Volume of Specimen: 3 ml serum Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 2-5 days Reference Range: See report Alkaline Phosphatase, Bone Specific General Use: Provides a general index of bone turnover, formation and a specific index of total osteoblast activity. Test Mnemonic: ALKIBS Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis, icterus, lipemia and non-serum specimens Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report Alpha - 1 - Antitrypsin, Blood General Use: Diagnosis of alpha- antitrypsin deficiency Test Mnemonic: A1AT Lab Performing Test: Specimen Processing - sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Overnight fasting preferred Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Causes for Rejection: Lipemic samples not accepted Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 3 days Reference Range: See report Alpha feto protein, maternal Synonym: Quad screen, AFP, AFETO General Use: Screening for Down’s Syndrome and Neural tube defects Test Mnemonic: AFETO Test Includes: AFP, HcG, Inhibin and Estriol Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Sample must be drawn between 15 weeks 0 days and 22 weeks 6 days. Special Instructions: Prenatal Assay form (History form) must accompany the specimen. Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: No patient history form Availability: Specimen may be drawn Mon-Sunday. Only sent to Yale MonFriday (no holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report Alprazolam Synonym: Xanax General Use: Alprazolam is an anti-anxiety agent of the benzodiazepine class. It is indicated for the management of anxiety disorders and for anxiety associated with depression. Test Mnemonic: ALP Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Protect from light, Deliver ASAP, Keep at Room temperature! Specimen Required: Clotted blood (serum) Container Required: Red top tube – No gel tubes! Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Drawn in tube with gel barrier (SST) or any serum separator (SST). Received not protected from light. Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 6 days Reference Range: See Report Aluminum, Blood General Use: Determining aluminum toxicity Test Mnemonic: ALUM Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient should refrain from taking antacids containing aluminum compounds at least three days prior to sample collection. Specimen Required: Plasma Container Required: Navy top tube (EDTA) Volume of Specimen: 1 Navy (EDTA) tube Minimum Volume of Specimen: 2 ml plasma Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 6 days Reference Range: See Report Amino Acids - Quantitative Plasma General Use: Evaluation of metabolic disorders Test Mnemonic: AAS Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: plasma Container Required: green top tube (Li or Na heparin) Volume of Specimen: 6 or 10 ml of whole blood Minimum Volume of Specimen: 1.0 ml plasma Availability: Sent Monday-Friday (no weekends or holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Amino Acids - Quantitative Urine Synonyms: Amino Acid Screen General Use: Evaluation of metabolic disorders Test Mnemonic: UAA Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Random urine Container Required: Standard urine collection container (urine) Volume of Specimen: Entire collection Minimum Volume: 5 ml random urine Availability: Sent Monday-Friday (no weekends or holidays) Time Required Routinely for Processing: 2 Days Reference Range: See report Amino Levulinic Acid, 24 hour Urine Synonym: ALA General Use: Evaluate porphyrias and lead poisoning Test Mnemonic: UALA24 Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Avoid exposure of specimen to light during & after collection. Refrigerate during and after collection. Specimen Required: 24 hr collection Container Required: Brown urine specimen container from lab (no preservative) Volume of Specimen: Entire specimen collection Minimum Volume of Specimen: 24 hr. entire specimen Availability: Sent Monday- Saturday (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See report Amiodarone General Use: Therapeutic drug monitoring Test Mnemonic: AMIO Test Includes: Amiodarone and Desethylamiodarone (metabolite) Lab Performing Test: Specimen Processing, sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliverer to Lab immediately! Specimen Required: Clotted blood (serum) Container Required: Red top tube – No gel tubes! Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Cause for Rejection: Improper tube, gross hemolysis Availability: Sent Mon. - Saturday (no holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report Amitriptyline Synonyms: Elavil, Lambitrol General Use: Monitor therapeutic drug level Test Mnemonic: AMI Test Includes: Amitriptyline, Nortriptyline, combined total (calculated) Lab Performing Test: Specimen Processing - sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Collect as trough or at least 12 hours after last dose Specimen Required: Clotted blood (Serum) Container Required: Red top with no gel barrier! Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Causes for Rejection: Drawn in tube with gel barrier or any serum separator (SST), Gross hemolysis Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 6 days Reference Range: See report Amniotic Fluid L/S Ratio Test Mnemonic: LS Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Amniotic fluid Minimum Volume of Specimen: 3 ml of fluid Time Required Routinely for Processing: Results ready same day or the following day, depending on time specimen is received in lab. Reference Range: See Report Amphetamines, Urine Test Mnemonic: UAMPH Test Includes: Amphetamine, Methamphetamine Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Random urine Container Required: Urine Cup Volume of Specimen: 20 mL urine Minimum Volume of Specimen: 20 mL urine Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 7 days Reference Range: See Report Amylase Isoenzymes Synonym: Salivary Amylase Test Mnemonic: AMYISO Test Includes: Total Amylase, Pancreatic Isoenzyme, and Salivary Isoenzymes (calculated) Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 6 days Reference Range: See Report Anaplasma phagocytophilum Antibody Synonym: Ehrlichia, HGE General Use: Used to support a diagnosis of Ehrlichiosis Test Mnemonic: ANAPLA Test Includes: Testing for E. chaffeensis and E. equi Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Time Required Routinely for Processing: 5 days Reference Range: Interpretation provided with test results Androstenedione General Use: Androstenedione may be useful in evaluating patients with androgen excess and managing patients with congenital adrenal hyperplasia (CAH). Test Mnemonic: ANDR Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Early morning specimen preferred Specimen Required: Clotted blood (serum) Container Required: Red top tube – No gel tubes! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Drawn in tube with gel barrier or any serum separator (SST) Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 7 days Reference Range: See Report Angioedema Panel, Acquired Test Mnemonic: ANGIOP Test Includes: C1 Inhibitor, Functional; C1 Inhibitor, Protein; C1q Complement Component Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Overnight fasting is preferrd Special Instructions: Early morning specimen preferred Specimen Required: Clotted blood (serum) Container Required: Red top tube – No gel tubes! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Drawn in tube with gel barrier or any serum separator (SST) Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 7 days Reference Range: See Report Angiotensin Converting Enzyme General Use: Useful in diagnosis of sarcoidosis Test Mnemonic: ACE Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 2.0 ml Minimum Volume of Specimen: 1.0 ml serum Causes for Rejection: Gross Hemolysis and EDTA plasma Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 2 days Reference Range: See report Anti-Cardiolipin Antibody Synonyms: Cardiolipin Antibodies General Use: Elevations may be predictive of risk of thrombosis or recurrent spontaneous abortions of early pregnancy. Also present in SLE patients with arterial and venous thrombosis Test Mnemonic: ACARD Test Includes: Anti-cardiolipin IgG, IgM and IgA Lab Performing Test: Specimen Processing; Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Citrated Plasma Container Required: Light blue top Volume of Specimen: 1.0 ml Minimum Volume of Specimen: 1.0 ml Causes for Rejection: Gross hemolysis Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 5 days Reference Range: See report Antidiuretic Hormone Synonym: Arginine Vasopressin (AVP) General Use: Diagnosis of electrolyte imbalances; screening for fluid regulation and renal function Test Mnemonic: ADH Lab Performing Test: Specimen Processing; Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliver immediately to Specimen Processing lab Specimen Required: Whole blood (EDTA) Container Required: Lavender top tube (2) (EDTA) Volume of Specimen: 4 mL EDTA plasma Minimum Volume of Specimen: 2 mL EDTA plasma Causes for Rejection: Delay in receipt of sample Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 9 days Reference Range: See report Anti-DNA, Single Stranded Synonyms: ssDNA General Use: Abs to single stranded DNA may be present in patients with SLE and other autoimmune diseases Test Mnemonic: SSDNA Test Includes: ssDNA IgG Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliver ASAP! Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST), deliver to Lab immediately! Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Delay in receipt of sample Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Anti Strep DNase-B Synonyms: Anti-deoxyribonuclease B General Use: Diagnostic of recent or previous infection with Beta hemolytic streptococci Test Mnemonic: ADNB Lab Performing Test: Specimen Processing; Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4-7 days Reference Range: Varies according to age of patient reference ranges provided with results Anti-Epidermal Antibody Synonyms: Anti-skin (dermal-epidermal) Antibody General Use: Present in 80% of patients with bullous pemphigoid. Test Mnemonic: AEAB Test Includes: Differentiation of Abs to intercellular substance and basement membrane zone Lab Performing Test: Specimen Processing; Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, icterus, or lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: Negative Anti-Glomerular Basement Membrane Synonyms: Anti-GBM General Use: High titers suggestive of Goodpasture's disease or Anti-GBM nephritis Test Mnemonic: AGBM Lab Performing Test: Specimen Processing; Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 3 days Reference Range: Negative Anti-Mitochondrial Antibody General Use: Diagnostic for primary biliary cirrhosis Test Mnemonic: AMA Lab Performing Test: Specimen Processing; Sent to Reference Laboratory Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See report Anti-Neutrophil Cytoplasmic Antibody Synonyms: ANCA General Use: To support the diagnosis of Wegener's granulomatosis, Good Pasture's disease Test Mnemonic: ANCA Lab Performing Test: Specimen Processing;Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Antinuclear Antibody General Use: Screening test for Autoimmune diseases, connective tissue diseases Test Mnemonic: ANASR Lab Performing Test Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml. serum Causes for Rejection: Gross hemolysis, chylous serum Availability: Mon. - Fri, 7:00 AM-3:00PM ; Not Stat Time Required Routinely for Processing: 2-3 days Reference Range: < 1:40. ANA pattern reported with positive results Antiplatelet Antibody General Use: Determine presence of antibody to platelets Test Mnemonic: ANTPLT Test Includes: IgG Indirect Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Wrong collection tube, mislabeled or unlabeled specimen. Availability: Sent out Mon – Sat (not holidays) Reference Range: See printed report Anti-Streptolysin O Titer Synonyms: Streptolysin-O Antibody, ASO, Strep A, Streptococcus, Group A, Strep General Use: To detect presence of antibodies to Streptolysin-O Test Mnemonic: ASOAB Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, lipemic Availability: Sent out Mon - Sat (not holidays) Time Required Routinely for Processing: 3 days Reference Range: See report Apolipoprotein A1 General Use: Apolipoprotein A1, has been reported to be a better predictor of CAD than HDL and Triglycerides Test Mnemonic: APOA1 Lab Performing Test: Specimen Processing – Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Fasting for at least 12 hours is required Specimen Required: Clotted blood (serum) Container Required: Red top (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross Lipemia, Plasma Availability: Sent Monday – Saturday (no holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report Apolipoprotein B General Use: Indication of CAD. In some patients APOB is elevated even in the presence of normal LDL Test Mnemonic: APOB Lab Performing Test: Specimen Processing- Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient must be fasting Specimen Required: Clotted blood (serum) Container Required: Red top tube (No gel) Volume of Specimen: 10ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis or lipemia, Plasma Availability: Sent Monday-Saturday (no holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report Apolipoproteins A1&B General Use: Apolipoprotein A1 is the primary protein associated with HDL cholesterol. Like HDL cholesterol, increased concentrations are associated with reduced risk of cardiovascular disease. Apolipoprotein B-100 is the primary protein associated with LDL cholesterol and other lipid particles. Like LDL cholesterol, increased concentrations are associated with increased risk of cardiovascular disease. The ratio of these two apolipoproteins correlates with risk of cardiovascular disease. Test Mnemonic: APO Test Includes: Apolipoprotein A1, Apolipoprotein B, Apolipoprotein B/A1 ratio (Calculated) Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Fasting required – 12-16 hours Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis and lipemia, Plasma Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 3 days Additional Information: Apolipoprotein A1 & Apolipoprotein B can each be ordered separately (Mnemonics: APOA1 & APOB) Reference Range: See Report Acetylcholine Blocking Antibody General Use: Useful in the diagnosis and management of Myastenia Gravis Test Mnemonic: ACYBAB Lab Performing Test: Specimen Processing; Sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (No gel) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 5 days Reference Range: Reference range and interpretation is provided with test results Arsenic, 24 hour urine Synonyms: As General Use: Arsenic poisoning, arsenic toxicity Test Mnemonic: UARS24 Lab Performing Test: Specimen Processing; sent to reference laboratory Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Specimen must not be voided into a metal container! Patient should refrain from eating shellfish, shrimp, crab, lobster and bottomfeeders such as flounder at least three days prior to specimen collection. Special Instructions: Keep refrigerated during collection Specimen Required: Entire 24 hour urine collection Container Required: 24 hr acid washed container obtained from Specimen Processing Lab Volume of Specimen: Entire 24 hour collection Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Arsenic, Blood General Use: Arsenic toxicity Test Mnemonic: ARS Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Pt should refrain from seafood and herbal supplements for three days prior to blood collection. Special Instructions: Do not spin tube!!! Specimen Required: Whole blood Container Required: Navy top (EDTA) Volume of Specimen: 7 ml Minimum Volume of Specimen: entire collection Causes for Rejection: Improper tube type, centrifuged tube, gross hemolysis Availability: Sent Mon-Saturday (no holidays) Time Required Routinely for Processing: 3 days Additional Information: Arsenic may only be present in blood for 4-6 hours. This test is most accurate in acute poisoning. Reference Range: See Report ASCA (Saccharomyces Cerevisiae) IgA Synonym: anti-Saccharomyces cerevisiae antibodies (ASCA) of the IgA class General Use: The presence of ASCA (S. cerevisiae) IgA antibodies, used in conjunction with clinical findings and other laboratory tests, may aid in the diagnosis of patients with Crohn's disease. ASCA (S. cerevisiae) IgA ELISA should be used to complement, but not to replace or to substitute for ASCA IgG antibody testing. Test Mnemonic: ASCAIA Test Includes: Semi-quantitative detection of anti-Saccharomyces cerevisiae antibodies (ASCA) of the IgA class Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 6 days Reference Range: See Report ASCA (Saccjaromyces Cerevisiae) IgG Synonym: anti-Saccharomyces cerevisiae antibodies (ASCA) of the IgG class General Use: This test is intended to aid in the diagnosis of patients with Crohn's disease. Test Mnemonic: ASCAIG Test Includes: enzyme-linked immunosorbent assay (ELISA) for the semiquantitative detection of S. Cerevisiae (ASCA) IgG Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 6 days Reference Range: See Report Aspergillus fumigatus IgG General Use: Useful to confirm exposure to or infection by Aspergillus fumigatus Test Mnemonic: ASPIGG Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10ml Minimum Volume of Specimen: 0.5 ml serum Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 4-5 days Reference Range: See Report Aspergillus, Serology General Use: Aid in the diagnosis and prognosis of infections due to Aspergillus sp. and in the planning of a fungus culture schedule Test Mnemonic: ASPERP Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 6 days Additional Information: This test is also available in the Fungal Serology Panel Reference Range: Negative Babesia Serology Synonym: Babesia microti General Use: To aid in the diagnosis of infection with Babesia Microti Test Mnemonic: BABS Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: Negative Barbiturates, Total, Blood General Use: Barbiturate toxicity Test Mnemonic: BARB Test Includes: Amobarbital, Butabarbital, Butalbital, Pentobarbital, Phenobarbital, Secobarbital Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: 2 Red top tubes; No gel barrier tube! Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Improper tube type Availability: Monday-Saturday (not holidays) Time Required Routinely for Processing: 7 days Reference Range: See report Beta-2-Glycoprotein (IgG, IgA, IgM) General Use: Beta-2-Glycoprotein 1, apolipoprotein H, is a cofactor in antiphospholipid antibody binding and is the critical antigen in the antiphospholipid antibody syndrome. Beta-2-Glycoprotein 1 Antibody is more specific than Cardiolipin Antibody that may express reactivity in patients with syphilis and other infectious diseases. Test Mnemonic: B2GLY Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Plasma Container Required: 2 blue top (Sodium Citrate) tubes Volume of Specimen: 2 blue top (Sodium Citrate) tubes Minimum Volume of Specimen: 3 ml plasma Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 7 days Reference Range: See Report Beta-2-Microglobulin General Use: Used as an indicator of glomerular function Elevated levels also noted in neoplasms. Test Mnemonic: B2M Lab Performing Test: Specimen Processing- Sent to referring lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1.0 ml serum Causes for Rejection: Improper tube, gross hemolysis, lipemia Availability: Sent Mon-Saturday (no holidays) Reference Range: See report Blastomyces, Serology General Use: Aid in the diagnosis and prognosis of infections due to Blastomyces Dermatitidis and in the planning of a fungus culture schedule Test Mnemonic: BLAS Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: This test is also available in the Fungal Serology Panel. Specimen Required: Clotted blood (serum) Container Required: Red Top Tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: Negative Blood Chromosome Analysis Synonym: Karyotype General Use: Physician interpretation Test Mnemonic: BLCR Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Diagnosis required – ICD.9 Specimen Required: Whole blood Container Required: Green top tube (sodium heparin) Volume of Specimen: 10.0 ml of blood (green top tube) Minimum Volume of Specimen: 3.0 ml Causes for Rejection: Clotted specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Daily Mon-Fri: not STAT, not available on weekends Time Required Routinely for Processing: 2-3 weeks Reference Range: Interpreted by physician Chromosomes, Bone Marrow or Peripheral Blood Synonyms: Bone Marrow Karyotype General Use: Interpreted by physician Test Mnemonic: KARYO Lab Performing Test: Specimen Processing, sent to Reference lab Request Form: Bone Marrow Request form (filled out in entirely by physician) Patient Preparation: Performed by physician Special Instructions: Call Hematology for bone marrow tray Specimen Required: Bone marrow aspirate or peripheral blood Container Required: Green top tube (sodium heparin) or EDTA Lavender top Volume of Specimen: 3.0 ml Minimum Volume of Specimen: 2.0 ml Causes for Rejection: Clotted specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Daily Mon-Fri. Time Required for Processing: 21 days Reference Range: See charted report Bordetella Pertussis Antibodies Synonym: Bordetella Antibodies General Use: Used to establish evidence of infection/exposure to Bordetella pertussis, the causative agent of whooping cough. Test Mnemonic: BORDPAB Test Includes: Pertussis toxin IgG, Pertussis toxin IgA, Filamentous Hemagglutinin Antigen IgG, Filamentous Hemagglutinin Antigen IgA Lab Performing Test: Specimen Processing, sent to Reference lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: none Special Instructions: none Specimen Required: clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Excessive hemolysis Availability: Sent out Monday thru Saturday (no holidays) Time Required Routinely for Processing: 1 week Reference Range: See report C1 Esterase, Functional General Use: Functional C1-Inhibitor, C1 Esterase Test Mnemonic: C1FUNC Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliver to lab immediately! Specimen Required: Clotted blood (serum) Container Required: Red top tube- No gel tube! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Improper tube type, gross hemolysis and lipemia Availability: Sent Mon-Saturday (no holidays) Time Required Routinely for Processing: 6 days Reference Range: See Report C1 Esterase Inhibitor General Use: A deficiency of this protein is characteristic of hereditary angioedema Test Mnemonic: C1EST Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Overnight fasting is preferred Special Instructions: Collect on ice. Deliver immediately to Specimen Processing Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, delay in delivery to Lab Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 5 days Reference Range: See report C3d Circulating Immune Complexes General Use: Circulating immune complexes (CIC) are present in many individuals with systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA), especially with any of the vasculitides complications. Levels of CICs have been reported to show correlation with disease activity in that higher levels are reported during active phases of the disease. Test Mnemonic: C3DIGG Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (No Gel) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: SST tube, delay in delivery to Lab Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 7 days Reference Range: See report CA15-3 General Use: Useful for monitoring therapy and confirming biopsy of certain carcinomas Test Mnemonic: CA153 Lab Performing Test: Specimen Processing, sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume Required: 2 ml Causes For Rejection: Gross hemolysis or lipemia Availability: Sent out Monday through Saturday (not holidays) Reference Range: See patient report CA19-9 Synonym: Carbohydrate Antigen 19-9 General Use: Useful for monitoring therapy and confirming biopsy of certain carcinomas Test Mnemonic: CA19 Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report CA27.29 General Use: Useful in monitoring therapy and confirming biopsy of certain carcinomas Test Mnemonic: CA27 Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Improper tube type, Gross hemolysis Availability: Sent out Mon - Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Caffeine General Use: Therapeutic drug monitoring Test Mnemonic: CAF Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube- SST Volume of Specimen: 10 ml Minimum Volume of Specimen: 0.5 ml serum Availability: Sent Mon-Saturday * Stats only on Sat. Time Required Routinely for Processing: 2-3 days for routine Reference Range: See Report Calcitonin Synonyms: Thyrocalcitonin General Use: Early detection of medullary carcinoma of the thyroid gland; evaluation of calcium metabolism Test Mnemonic: CALC Lab Performing Test: Specimen Processing; sent to reference laboratory Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Overnight fasting preferred Special Instructions: Deliver immediately to Laboratory! Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Delay in receipt of specimen, Gross hemolysis Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 3 days Reference Range: See report Candida albicans Antibodies General Use: Aid in the diagnosis and prognosis of Candida fungal infections and in the planning of a fungus culture schedule Test Mnemonic: CANALB Test Includes: IgG, IgM, IgA Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red Top Tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 5 days Reference Range: See Report Carbamazepine 10, 11 Epoxide General Use: Carbamazepine and its metabolite (10, 11-Carbamazepine epoxide) are widely used for control of generalized tonic-clonic, partial-onset, complex and mixed seizure disorders. Test Mnemonic: CARBEP Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube – No gel tubes! Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: SST tube Time Required Routinely for Processing: 5 days Reference Range: See Report Carotene General Use: Diagnosis of malabsorption syndromes Test Mnemonic: CARO Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Protect specimen from light by wrapping in aluminum foil Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Causes for Rejection: Refrigerated specimens, exposure of specimen to light Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 5 Days Reference Range: See report Cat Scratch Fever Serology Synonyms: Bartonella Abs General Use: To aid in the diagnosis of Cat Scratch disease Test Mnemonic: BARTAB Test Includes: Bartonella henselae IgG, IgM; Bartonella quintana IgG, IgM. Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: Negative Catecholamines, 24 hour Urine General Use: Evaluation of catecholamine production Test Mnemonic: UCAT24 Test Includes: Urine Dopamine, Epinephrine, Norepinephrine, and total catecholamine (calculated) Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: It is preferable for the patient to be off medications for three days prior to collection. However, common antihypertensives (diuretics, ACE inhibitors, calcium channel blockers, alpha and beta blockers) cause minimal or no interference. Patient should avoid alcohol, coffee, tea, tobacco (including use of nicotine patch), bananas, citrus fruits and strenuous exercise prior to collection. Special Instructions: Refrigerate during collection Specimen Required: 24 hr urine Container Required: 24 hour urine container with 25ml 6N HCL obtained from Specimen Processing laboratory. Volume of Specimen: Entire 24 hr collection Minimum Volume of Specimen: Entire 24 hr collection Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 4-5 Days Reference Range: See report Catecholamines, plasma General Use: Differential diagnosis of pheochromocytoma Test Mnemonic: CATP Test Includes: Dopamine, Epinephrine, Norepinephrine, and total catecholamines (calculated) Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Overnight fasting is required. Patient should avoid alcohol, coffee, tea, tobacco and strenuous exercise prior to collection. Special Instructions: Draw in pre-chilled tube. Place on ice; deliver to lab immediately! Specimen Required: Whole blood (plasma) Container Required: 2 green top tubes (Na heparin) Draw in pre-chilled tubes, place on ice and deliver ASAP. Volume of Specimen: 10 ml Minimum Volume of Specimen: 2.5 ml plasma Causes for Rejection: Improper tube type, specimen storage or delay in transport Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report Celiac DNA Genotyping Synonyms: Celiac Disease HLA Typing Test Mnemonic: CELDNA Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Do not spin! Specimen Required: Whole blood (ACD-A or ACD-B) Container Required: Yellow top ACD tube - obtain from Specimen Processing Lab Volume of Specimen: 10 ml Minimum Volume of Specimen: 5 ml Availability: Sent Monday-Saturday (not holidays) Reference Range: See report Ceruloplasmin General Use: Diagnostic test for Wilson's disease Test Mnemonic: CERU Lab Performing Test: Specimen Processing; sent to reference laboratory Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Overnight fasting is preferred Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Cholinesterase, Blood Synonyms: Pseudo-Cholinesterase; Serum Cholinesterase General Use: Evaluate prolonged anesthetic effect post surgery, nerve gas poisoning or insecticide poisoning Test Mnemonic: PSCHOL Lab Performing Test: Specimen Processing; sent to reference laboratory Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole Blood (EDTA) Container Required: Lavender top tube with (EDTA) Volume of Specimen: 4 ml Minimum Volume of Specimen: 2 ml Plasma Reasons for Rejection: Hemolysis Availability: Sent Monday - Saturday (not holidays) Time Required Routinely for Processing: 3 days Reference Range: See report Chromium, Plasma General Use: Occupational exposure and exposure to environmental contamination of chromium may lead to toxicity. Test Mnemonic: CHR Lab Performing Test: Specimen Processing; sent to reference laboratory Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient should refrain from taking vitamins, mineral or herbal supplements at least one week prior to specimen collection Specimen Required: Navy EDTA Plasma Container Required: Navy EDTA tube Volume of Specimen: 4 ml Minimum Volume of Specimen: 2 ml Plasma Causes for Rejection: Clotted, grossly hemolyzed Availability: Sent Monday - Saturday (not holidays) Time Required Routinely for Processing: 1 Week Reference Range: See report Chromogranin A Synonyms: CgA General Use: Serum Chromogranin A is used to assess peptide-secreting endocrine neoplasms and multiple endocrine neoplasia. Test Mnemonic: CHROMA Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis, lipemia, icterus Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report Chromosome Analysis, Tissue Synonyms: Karyotype General Use: Autosomal or sex chromosome mosaicism not detected in lymphocytes may be determined in fibroblasts obtained from a tissue biopsy. Test Mnemonic: TISCHR Lab Performing Test: Specimen Processing, sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Tissue sample Container Required: Transport Media Volume of Specimen: 2x3 mm tissue sample Minimum Volume of Specimen: 2x3 mm tissue sample Causes for Rejection: Formalin Fixed Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 21 days Reference Range: See individual reports Citrate, 24 hour urine Synonym: Citric Acid General Use: Urine levels of Citrate are increased in metabolic and respiratory alkalosis Test Mnemonic: UCIT24 Test Includes: Creatinine, Citric acid Lab Performing Test: Specimen Processing, sent to Reference Lab Request form : Signed order by physician/Health Professional Affiliate(HPA Patient Preparation: Call Specimen Processing lab for special collection container Special Instructions: Keep specimen refrigerated during entire collection Specimen Required: 24 hr urine Container Required: 24 hr urine container with no preservative, obtained from Lab. Call ext 4153 Volume of Specimen: Entire collection Minimum Volume of Specimen: Entire collection Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 6 days Reference Range: See Report Chlamydia trachomatis DNA,SDA Synonyms : CT, ProbeTec General Use : For detection of C. Trachomatis Test Mnemonic: CT Lab Performing Test: Specimen processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Urine or endocervical,urethral or vaginal swab Conatiner Required: BD Transport or BD Urine Preservative Transport kit Volume Of Specimen: One swab or 15-60 ml of urine Minimum Volume of Specimen: One swab or 15 ml of urine Causes for Rejection: Swabs received in any other transport kit. Overfilled or underfilled urine transport container. Cleansing swab received. Availability: Sent out Monday –Saturday (not holidays) Time Routinely Required for Processing: 4 days Reference Range: Not detected Clamydia trachomatis/Neisseria gonorrhoeae DNA, SDA Synonym: CT/GC General Use: For Detection of sexually transmitted diseases Test Mnemonic: GCCAMP Test Includes: Clamydia trachomatis, Neisseria gonorrhoeae Lab Performing test: Specimen Processing; Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate (HPA) Specimen Required: Urine or endocervical,urethral or vaginal swab Container required: BD transport kit for swab or BD urine preservative transport for urine Volume of Specimen: One swab or 15-60 ml of urine Minimum Volume of Specimen: One swab or 15 ml of urine Causes for Rejection: Only BD collection kits allowed. Overfilled or underfilled urine transport container. Collection kit received with cleansing swab. Availability: Sent out Monday-Saturday (not holidays) Time Required Routinely for Processing: 4 days Additional Information: Pink swab for vaginal specimens, blue swab for urethral specimens Reference Range: Not detected Clonazepam Synonym: Klonopin General Use: Clonazepam is a benzodiazepine used as a tranquilizer. Clonazepam is used in treating patients with seizures and in reducing tardive dyskinesia. Test Mnemonic: CLO Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Optimum time to collect sample: 4 hours post oral dose Special Instructions: Deliver ASAP! Specimen Required: Clotted blood (serum) Container Required: Red top tube – No gel tubes! Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gel barrier tube received Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report Clozapine Synonym: Clozaril General Use: Clozapine is used selectively in the treatment of patients with schizophrenia. Therapeutic drug monitoring is useful to optimize dose and to avoid toxicity. Test Mnemonic: CLOZ Test Includes: Clozapine, Norclozapine Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliver ASAP! Specimen Required: EDTA plasma Container Required: Purple top EDTA Volume of Specimen: 4 mL Minimum Volume of Specimen: 2 mL plasma Causes for Rejection: Gross hemolysis, lipemia, received room temperature, gel barrier tube received Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report CMV Antigenemia Synonym: Cytomegalovirus Antigenemia Test Mnemonic: CMVAG Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliver Immediately to Lab! Specimen Required: Whole blood Container Required: 2 Lavender (EDTA) top tubes Volume of Specimen: 2 Lavender (EDTA) top tubes Minimum Volume of Specimen: 2 Lavender (EDTA) top tubes Causes for Rejection: Received room temperature Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report Coagulation Factor Assays II,V,VII,IX,X,XI,XII Synonyms: Factor Assays II,V,VII,IX,X,XI,XII General Use: Detecting specific coagulation factor deficiencies Test Mnemonic: FII; FV; FVII; FX; FXI; FXII Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient must not be on anticoagulants Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Collection Instuctions: Centrifuge light blue-top tube for 15 minutes at approximately 1500 g within 60 minutes of collection. Using a plastic pipette, remove plasma, taking care to avoid the WBC/platelet buffy layer and place into a plastic vial. Centrifuge a second time and transfer platelet poor plasma into a new plastic vial. Plasma must be free of platelets (<10,000/mcl). Freeze immediately and ship on dry ice. Specimen Required: Plasma Container Required: Blue top tube (sodium citrate) – 2 for each test ordered Volume of Specimen: 3 ml plasma for each test Minimum Volume of Specimen: 1 ml plasma for each test Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See printed report Cocaine Metabolites, Urine Test Mnemonic: UCOCCO Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Urine Container Required: Urine cup Volume of Specimen: 20 mL Minimum Volume of Specimen: 20 mL Availability: Sent out Mon-Sat (not holidays) Reference Range: See printed report Coccidioides Antibody General Use: Aid in the diagnosis and prognosis of Coccidioides immitis infections and in the planning of a fungus culture schedule Test Mnemonic: COCC Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red Top Tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Additional Information: This test is also available in the Fungal Serology Panel Reference Range: Negative Coenzyme Q10 Test Mnemonic: COEQ10 Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient should fast 10-12 hours prior to collection. Patient may have water. It is not necessary to discontinue nutritional supplements prior to this test. Special Instructions: Protect from light; Deliver ASAP! Specimen Required: Clotted blood (serum) Container Required: Red top tube – No gel tubes! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Received room temperature, not protected from light Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 6 days Reference Range: See Report Cold Agglutinins Synonyms: Cold Hemagglutinins General Use: To aid in diagnosis of primary atypical pneumoniae and certain hemolytic anemias Test Mnemonic: CAG Lab Performing Test: Specimen Processing – sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Blood, after being drawn, must be kept at room temperature Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, chylous serum. Blood > 1 hour old. Specimen received frozen. Availability: Sent Mon – Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See report Collagen Type I C-Telopeptide (CTx) Synonyms: C-Telopeptide, Serum, CTX, Beta-Crosslaps General Use: CTx is useful to asses bone resorption in patients with metabolic bone disease. The test is also useful in monitoring therapy to slow or halt osteoporotic bone loss. Test Mnemonic: CTELO Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Fasting required. Fasting morning collection 8-10 a.m. (diurnal variations cause elevated levels at night). Special Instructions: Allow blood to clot 10-15 minutes at room temperature. Then centrifuge and separate serum from cells. Deliver to CP immediately! Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Moderate/gross hemolysis, Grossly lipemic or icteric, Non-fasting specimens Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report Collagen Cross-Linked N-Telopeptide, Urine Synonyms: N-Telopeptide, Osteomark, NTx General Use: Screen and monitor osteoporosis Test Mnemonic: UNTX Test Includes: N-telopeptide, creatinine Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Random urine specimen should be the second void of the morning Specimen Required: Second morning urine void Volume of Specimen: 25 ml urine Minimum Volume of Specimen: 2 ml urine Time Required Routinely for Processing: 5 days Reference Range: See report Complement, C2 Synonyms: C2 General Use: Complement levels aid in the diagnosis of certain inflammatory conditions, autoimmune disease states, and some genetic disorders. Test Mnemonic: COMPC2 Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Separate serum within one hour of time draw and refrigerate Specimen Required: Clotted blood (serum) Container Required: Red top tube (No Gel!) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 8 days Reference Range: See report Complement, C5 Synonyms: C5 General Use: Complement levels aid in the diagnosis of certain inflammatory conditions, autoimmune disease states, and some genetic disorders. Test Mnemonic: COMPC5 Lab Performing Test: Specimen Processing; Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Complement, C6 Synonyms: C6 General Use: Complement levels aid in the diagnosis of certain inflammatory conditions, autoimmune disease states, and some genetic disorders Test Mnemonic: COMPC6 Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 9 days Reference Range: See report Complement, Total (CH5O) Synonyms: Total hemolytic complement General Use: To follow SLE patient's response to therapeutic regime; to evaluate for complement component deficiency Test Mnemonic: CH5O Lab Performing Test: Specimen Processing; Sent to Reference lab. Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Special Instructions: Deliver to the lab immediately! Container Required: Red top tube, no gel barrier! Volume of Specimen: 10 ml blood Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, lipemia, received room temperature, delay in delivery to Lab Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Copper, 24 hour urine Synonyms: Urine Cu General Use: Evaluate disorders of copper metabolism, copper poisoning Test Mnemonic: UCU24 Test Includes: Quantitative urine copper Lab Performing Test: Specimen Processing; sent to reference laboratory Request Form: Signed order by physician/Health Professional Affiliate(HPA). Patient Preparation: Patient should refrain from taking vitamins, minerals or herbal supplements at least 1 week prior to specimen collection Special Instructions: Specimen must be voided into metal free container. Refrigerate during collection Specimen Required: 24 hour urine Container Required: Acid washed 24 hour urine container supplied by Specimen Processing Laboratory Volume of Specimen: Entire collection Availability: Sent Monday -Saturday (not holidays) Time Required Routinely for Processing: 6 days Reference Range: See report Copper, Blood Synonyms: Cu General Use: Evaluate abnormal copper metabolism; i.e., Wilson's Disease; copper poisoning Test Mnemonic: CU Lab Performing Test: Specimen Processing; sent to reference laboratory Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood Container Required: Navy blue top, (No additive) Volume of Specimen: 7 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Hemolysis Availability: Sent Monday - Saturday (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See report Cortisol, Free 24 hour urine General Use: The measurement of free cortisol in urine is a valuable tool for diagnosis of Cushing’s Disease Test Mnemonic: UCOR24 Test Includes: free cortisol and urine creatinine Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: 24 hour urine container supplied by Specimen Processing Laboratory Specimen Required: 24 hr urine Container Required: 24 hr urine container Volume of Specimen: Entire collection Minimum Volume of Specimen: Entire collection Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 4-5 days Reference Range: See Report Coxsackie B Virus Titer Synonyms: Coxsackie B 1-6 General Use: Used to support a diagnosis of Coxsackie virus infection Test Mnemonic: COX Test Includes: Coxsackie B Types 1, 2, 3, 4, 5, 6 Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Additional Information: Throat & rectal swabs will yield better viral recovery. It is suggested that these accompany the serum sample. Reference Range: Less than a four fold increase in titer C-Peptide Synonym: C-Terminal Insulin General Use: Marker for endogenous insulin production Test Mnemonic: CPEP Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient should be fasting Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Room temperature specimens received more than 24 hous after collection Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 2-3 days Reference Range: See report Creatine Kinase Isoenzyme Panel Synonyms: CPK Isoenzymes Test Mnemonic: CPKISO Lab Performing Test: Specimen Processing, sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliver ASAP! Specimen Required: Clotted blood (serum) Container Required: Red Top Tube (SST) Volume of Specimen: 10 mL Minimum Volume of Specimen: 2 mL serum Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1-3 days Additional Information: Use if presence of CKBB is needed for evaluation; otherwise order "Heart" to obtain total CPK and CKMB Reference Range: See report Cryoglobulins General Use: Detection of cold precipitating macroglobulins Test Mnemonic: CRYOG Lab Performing Test: Specimen Processing, sent to reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Draw in heated tube. Place tube in 37 degree heating block immediately after specimen draw. After 1 hour in heating block, spin. Do not refrigerate tube! Specimen Required: Blood clotted at 37 degrees Container Required: Heated plain red top tube (No Gel!) - 2 Volume of Specimen: 10 ml Minimum Volume of Specimen: 2.5 ml serum Causes for Rejection: Improper temperature storage Availability: Sent Mon-Saturday (not holidays) Time Required Routinely for Processing: 5 days. Reference range: Negative Cryptococcus Antibody General Use: Aid in the diagnosis and prognosis of Cryptococcal infections and in the planning of a fungus culture schedule Test Mnemonic: CRY Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Additional Information: This test is also available in the Fungal Serology Panel. Reference Range: Negative CSF IgG Synonym: Immunoglobulin G, CSF Test Mnemonic: CSFIGG Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Cerebrospinal fluid (CSF) Container Required: Sterile plastic tube Volume of Specimen: 2 ml CSF Minimum Volume of Specimen: 1 ml CSF Causes for Rejection: Hemolysis, lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 5 days Reference Range: See Report Cyclic Citrulline Peptide, IgG Synonyms: Citrullinated Peptide (CCP) IgG, CCP, Anti-Cyclic Citrullinated Peptide (CCP) Antibody IgG General Use: This test has been proven to be better for use in the diagnosis of Rheumatoid arthritis than conventional testing. Test Mnemonic: CYCPE Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report Cyclospora and Isospora Examination General Use: Cyclospora cayetanensis and Isospora belli are parasites that cause malaise, low grade fever and diarrhea. Test mnemonic: CYCLSP Test Includes: Cyclospora and Isospora Examination, Concentration Lab Performing Test: Speciemn Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate (HPA) Specimen Required: Stool Container Required: Volume of Specimen: Minimum Volume of Specimen: Causes for Rejection: Unpreserved stool. Frozen specimens Availability: Sent out Monday-Saturday (not holidays) Time Required Routinely for Processing: 5 days Reference Range: See Report Cyclosporine General Use: Immunosuppressant Therapy Test Mnemonic: CYA Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood Container Required: Lavender top tube (EDTA) Volume of Specimen: 5 mL Minimum Volume of Specimen: 2 mL Causes for Rejection: Improper tube type Availability: Sent Mon-Saturday (no holidays) Time Required Routinely for Processing: 1 week Reference Range: See Report Cystic Fibrosis Screen Synonym: Cystic Fibrosis Gene Mutation General Use: Screening for relevant gene mutations Test Mnemonic: CYSMUT Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood Container Required: Lavender top tube (ETDA) - 2 Volume of Specimen: 2 lavender top tubes Minimum Volume of Specimen: Entire collection Causes for Rejection: Insufficient quantity Availability: Sent Mon-Saturday (no holidays) Time Required Routinely for Processing: 1 week Reference Range: See Report Cystine, 24 hour urine Test Mnemonic: UCYS24 Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Keep refrigerated during collection. Deliver ASAP! Specimen Required: 24 hour urine collection Container Required: 24 hour urine container with no preservative Volume of Specimen: Entire collection Minimum Volume of Specimen: Entire collection Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See Report Cytomegalovirus Antibodies Synonyms: CMV General Use: Used to support a diagnosis of Cytomegalovirus infection Test Mnemonic: CMVAB Test Includes: CMV IgG and IgM Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross Hemolysis Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Cytomegalovirus Detection by PCR General Use: Detection of CMV Test Mnemonic: CMVPCR Test Includes: Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Stool, urine, CSF, BAL, fluids or Tissue biopsy Container Required: Fluids in sterile container. Tissue in viral transport media. Volume Of Specimen: Minimum Volume of Specimen: Availability: Time Required Routinely for Processing: Additional Information: Reference Range: See Report Desipramine Synonyms: Norpramin General Use: Therapeutic drug monitoring Test Mnemonic: DESI Lab Performing Test: Specimen Processing - sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Collect as a trough or at least 12 hours after last dose Special Instructions: Separate from cells as soon as possible Specimen Required: Clotted blood (serum) Container Required: Red top tube with NO gel barrier! Volume of Specimen: 10 ml serum Minimum Volume of Specimen: 3 ml serum Causes for Rejection: Drawn in tube with serum separator (SST), gross hemolysis Availability: Sent Monday - Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report DHEA Sulfate General Use: DHEA-S is the sulfated form of DHEA and is the major androgen produced by the adrenal glands. This test is used in the differential diagnosis of hirsute or virilized female patients and for the diagnosis of isolated premature adrenarche and adrenal tumors. Test Mnemonic: DHEAS Lab Performing Test: Specimen Processing - sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top SST tube Volume of Specimen: 10 ml serum Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis Availability: Sent Monday - Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Diphtheria Antitoxoid Antibody Synonym: Diphtheria Antibody IgG General Use: Used to evaluate Diphtheria immunization efficacy. Test Mnemonic: DIPAB Lab Performing Test: Specimen Processing, sent to Reference lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis Availability: Sent out Monday thru Saturday (no holidays) Time Required Routinely for Processing: 1 week Reference Range: See report DISOPYRAMIDE Synonym: Norpace General Use: Monitor therapeutic drug level Test Mnemonic: NORPA Test Includes: Disopyramide Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (No gel barrier) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Drawn in tube with gel barrier Availability: Sent Monday - Saturday (not holidays) Time Required Routinely for Processing: 5-6 days Reference Range: See report DNA (ds) Antibody Synonyms: dsDNA, Double-Stranded DNA Antibody, Native DNA, Anti-DNA, (dsDNA) General Use: For diagnosis and follow up of SLE Test Mnemonic: DSDNAB Lab Performing Test: Specimen Processing; Sent to Reference laboratory Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, icterus, lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Drug Screen, Serum Only Test Mnemonic: DRGS Request Form: Signed order by physician/Health Professional Affiliate(HPA) Lab Performing Test: Specimen Processing - sent to reference lab Specimen Required: Clotted blood (serum) Container Required: Red top tube, No gel! Volume of Specimen: 10 ml Minimum Volume of Specimen: 5 ml serum Causes for Rejection: Improper tube type Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 5 days Reference Range: See report Echinococcus Serology General Use: Used to support a diagnosis of Echinococcosus granulosus Test Mnemonic: ECHIN Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red Top Tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4-8 days Reference Range: Negative Endomysial IgA Antibody General Use: A positive IgA endomysial antibody result supports the diagnosis of celiac disease. Test Mnemonic: ENDMYS Test Includes: If Endomysial Antibody Screen IgA is abnormal, Endomysial Antibody Titer will be performed at an additional charge. Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Sent Mon-Saturday (not holidays) Causes for Rejection: Gross Hemolysis and lipemia Time Required Routinely for Processing: 4 days Reference Range: See Report Enterovirus Detection by PCR General Use: Detection of Enterovirus Test Mnemonic: ENTPCR Test Includes: Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Throat swab, Nasopharyngeal swab or wash, stool and others Container Required: Viral Transport Media Volume of Specimen: Availability: Time Required Routinely for Processing: Additional Information: Reference Range: See Report Epstein-Barr Viral Panel Synonyms: EBV Panel General Use: Diagnosis and confirmation of Epstein-Barr Virus infection Test Mnemonic: EBVP Test Includes: Epstein-Barr Virus VCA Antibody (IgM), Epstein-Barr Virus VCA Antibody (IgG), Epstein-Barr Virus Nuclear Antigen (EBNA) Antibody (IgG) Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, lipemia, icterus Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Epstein-Barr Virus DNA, Quantitative PCR Synonym: EBV Quant DNA General Use: Epstein-Barr Virus DNA, Real-Time PCR is useful in assessing active disease. Central nervous system infections can be diagnosed with CSF specimens. Test Mnemonic: EBVDNA Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole Blood or plasma Container Required: Lavender top (EDTA) tube Volume of Specimen: 1 Lavender top (EDTA) tubes Minimum Volume of Specimen: 1 ml whole blood or plasma Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report Erythropoietin General Use: Diagnosis of kidney disease and anemia Test Mnemonic: ERY Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Cause for Rejection: Gross hemolysis Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 2-3 days Reference Range: See report Estrone, serum General Use: Estrone is primarily derived from metabolism of androstenedione in peripheral tissues, especially adipose tissues. Individuals with obesity have increased conversion of androstenedione to Estrone leading to higher concentrations. In addition, an increase in the ratio of Estrone to Estradiol may be useful in assessing menopause in women. Test Mnemonic: ESTRS Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube – No gel tubes! Tube must be full! Volume of Specimen: 10 ml Minimum Volume of Specimen: 4 ml serum Causes for Rejection: Gross hemolysis, lipemia, SST tube received Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 3 days Additional information: May also be ordered as part of serum estrogen panel, which includes estradiol and estrone (mnemonic ESTROGS) Reference Range: See Report Extractable Nuclear Antigen Antibodies Synonyms: Anti-Ribonucleic Protein Antigen, Anti-ENA Antibody, ENA Antibodies, Anti-Smith Antibody, Ribonuclear Protein Antibody, RNP Antibody General Use: Use to aid in the differentiation or diagnosis of SLE and Mixed Connective Tissue Disease (MCTD) Test Mnemonic: AENA Test Includes: Anti-RNP and Anti-SM/RNP complex Lab Performing Test: Specimen Processing; Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Cause for Rejection: Gross hemolysis, icterus, and/or lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Factor V Leiden Mutation Analysis Synonyms: Factor Five General Use: To determine the presence of a mutation in the Factor V molecule producing a hypercoagulable state Test Mnemonic: FVLEID Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10 ml of blood collected must be discarded. Specimen Required: Whole blood at room temperature Container Required: Lavender top tube (EDTA) - 2 Volume of Specimen: 2 lavender top tubes Minimum Volume of Specimen: 1 lavender top tube Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen Availability: Sent out Mon–Sat (not holidays) Time Required Routinely for Processing: 5 days Reference Range: See printed report Factor VIII Multimers Synonym: von Willebrand Factor Antigen, Multimeric General Use: For the analysis of Von Willebrand Antigen multimers for the diagnosis of Von Willebrands Disease. Test Mnemonic: F8MULT Lab Performing Test: Specimen Processing; Sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Fasting for at least 8 hours is preferred Special Instructions: Deliver Immediately to Lab! Specimen Required: Plasma Container Required: Blue top tube (Sodium Citrate) Volume of Specimen: Full blue top tube Minimum Volume of Specimen: 2 ml plasma Causes for Rejection: Gross hemolysis Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 7 days Reference Range: See Report Factor VIII Related Antigen Synonym: von Willebrand Factor Antigen General Use: Interpreted by physician Test Mnemonic: FVIIIA Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Overnight fasting is preferred. Patient must not be on anticoagulants. Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Collection Instructions: Centrifuge light blue-top tube for 15 minutes at approximately 1500 g within 60 minutes of collection. Using a plastic pipette, remove plasma, taking care to avoid the WBC/platelet buffy layer and place into a plastic vial. Centrifuge a second time and transfer platelet poor plasma into a new plastic vial. Plasma must be free of platelets (<10,000/mcl). Freeze immediately and ship on dry ice. Specimen Required: Plasma Container Required: Blue top tube (sodium citrate) – tube must be full Volume of Specimen: 2 ml plasma Minimum Volume of Specimen: 1 ml plasma Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Sent out Mon-Sat (not holidays) Reference Range: See printed report Fecal Fat, Random Synonyms: Qualitative stool for fat, lipids, stool General Use: Screening test for presence of split fat globules and neutral fat globules Test Mnemonic: FFRAN Lab Performing Test: Specimen Processing. Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Fresh random stool, no 24 hr collections or urines. Container Required: Sterile cup, stool cup Minimum Volume of Specimen: 2 grams Causes for Rejection: Insufficient specimen volume, specimen contaminated with urine and/or water, specimen containing interfering substances, eg. castor oil, bismuth, metamucil, barium; no swabs accepted, no 72 hour fecal collection. Availability: Sent Mon-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report Fecal Fat, Timed specimen Synonym: Lipids, Stool, Split Fats, Unesterfied Fatty Acids General Use: Excessive Fat in stool is useful in diagnosing patients with malabsorption and maldigestion, e.g., pancreatic failure. In addition, results may be useful in monitoring patients receiving exogenous enzyme therapy for chronic diarrhea. Test Mnemonic: FF Test Includes: Quantitative fecal fat Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient should be on a diet including 100 grams of fat per day for 3 days prior to collection and during the collection period. Special Instructions: Collect in pre-weighed container, send entire collection. Keep refrigerated during collection. Specimen Required: Collect stool for 24, 48 or 72 hours Container Required: Pre-weighed plastic container with tight lid Volume of Specimen: Entire collection Minimum Volume of Specimen: Entire collection Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 8-10 days Reference Range: See Report Flecainide Synonym: Tambocor ® General Use: Monitoring the flecainide concentration is used to assure compliance and avoid toxicity of this cardiac drug used to treat ventricular tachycardia and premature cardiac contractions. Test Mnemonic: FLE Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Optimum time to collect sample: 1 hour before next dose. Specimen Required: Clotted blood (serum) Container Required: Red top tube – No gel tubes! Volume of Specimen: 10 ml Minimum Volume of Specimen: 4 ml serum Causes for Rejection: SST tube received Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 7 days Reference Range: See Report Flow Cytometry, Bone Marrow or Peripheral Blood Synonyms: Leukemia/Lymphoma Panel, CLLP Test Mnemonic: FLOW Lab Performing Test: Specimen Processing, sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Clinical history required Specimen Required: Whole blood Container Required: 1 Green top tube (sodium heparin) or EDTA Lavender top Volume of Specimen: 4.0 ml of bone marrow or whole blood Minimum Volume of Specimen: 1.0 ml of bone marrow or whole blood Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen Availability: Daily, Mon.-Fri.; not available on weekends; not done STAT Time Required Routinely for Processing: 1-2 days Reference Range: Interpretation made by pathologist Folate, RBC General Use: Detect folate deficiencies and monitor therapy Test Mnemonic: FOLRBC Lab Performing Test: Specimen Processing, sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Keep tube at room temp! Do not refrigerate or freeze. Specimen Required: Whole blood, plasma Container Required: Lavender top (EDTA) - 2 Volume of Specimen: 5 ml Minimum Volume of Specimen: entire collection Causes for Rejection: Improper storage temperature Availability: Sent Mon-Saturday (not holidays) Time Required Routinely for Processing: 2-3 days Reference Range: See Report Fragile-X Synonym: Fragile X with reflex General Use: Routine chromosome analysis Test Mnemonic: FRAGX Test Includes: If Fragile X, PCR result is not Normal, or Gray zone, then Fragile X, Southern Blot will be performed at an additional charge Lab Performing Test: Specimen Processing. Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood - kept at room temp! Container Required: 4 Lavender top tubes (EDTA) Volume of Specimen: 10 ml whole blood Minimum Volume of Specimen: 5.0 ml Causes for Rejection: Improper tube type or specimen not kept at room temp Availability: Sent Mon-Sat, (not holidays) Time Required for Processing: 1 week Reference Range: See report Free T3 Synonym: FT3 General Use: Thyroid testing Test Mnemonic: FT3 Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube-(SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Sent Mon-Saturday (not holidays) Time Required Routinely for Processing: 2-3 days Reference Range: See Report Free Testosterone General Use: This test is helpful in the diagnosis of hypogonadism in males and hirsutism and virilization in females Test Mnemonic: FTEST Test Includes: Testosterone, free, bioavailable, and total Lab Performing Test: Specimen Processing - sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: 2 Red top tubes , No gel barrier tubes! Volume of Specimen: 10 ml (2 tubes) Minimum Volume of Specimen: 4 ml serum Causes for Rejection: SST tube received Availability: Sent Monday - Saturday (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See report Fructosamine General Use: Useful in monitoring the degree of glycemia over short to intermediate time frames (1-3 weeks) Test Mnemonic: FRUC Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Avoid hemolysis of specimen Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml Causes for Rejection: Hemolysis, icterus Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report FTA-CSF Synonym: Treponema pallidum antibody General Use: Test for neurosyphilis, The FTA-CSF test is considered experimental at this time. Test Mnemonic: FTASF Lab Performing Test: Specimen Processing, sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Cerebrospinal fluid Container Required: Clean sterile container, glass tube Volume of Specimen: 2 ml of CSF Minimum Volume of Specimen: 0.5 ml CSF Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: One week Reference Range: Non-reactive FTA Profile General Use: Useful in the diagnosis and treatment of Syphilis Test Mnemonic: FTAP Test Includes: RPR Titer and FTA-ABS Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report Fungal Serology Panel General Use: Aid in the diagnosis and prognosis of fungal infection and in the planning of a fungus culture schedule Test Mnemonic: FUNGP Test Includes: Aspergillus, Blastomyces. Coccidiomycosis, Histoplasmosis and Cryptococcal Serologies Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: These tests may be ordered individually; see specific listing for each fungus Container Required: Red top tube (SST) – 2 Specimen Required: Clotted blood (serum) Volume of Specimen: Two 10 ml tubes Minimum Volume of Specimen: 5 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Gabapentin Synonym: Neurontin General Use: Gabapentin is an anticonvulsant drug commonly used as adjunctive therapy to treat partial seizures. Test Mnemonic: GABAP Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Draw sample 2 hours after last dose at steady state. Special Instructions: Separate plasma from cells ASAP! Specimen Required: Plasma Container Required: Lavender top (EDTA) tube - 2 Volume of Specimen: 3 ml plasma Availability: Sent out Mon-Sat (not holidays) Causes for Rejection: SST tube received, grossly hemolyzed Time Required Routinely for Processing: 6 days Reference Range: See Report Ganglioside GM-1 Antibodies Synonym: GMI Antibodies General Use: Ganglioside GM-1 Antibody IgG is associated with the GuillainBarre syndrome, particularly the acute motor axonal neuropathy variant. Antibody IgM is associated with chronic multifocal motor neuropathy. Test Mnemonic: GANGAB Test Includes: GMI IgG and IgM antibodies Lab Performing Test: Specimen Processing; Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Overnight fasting is preferred Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume Required: 2 ml serum Availability: Sent Monday-Friday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Gastric Parietal Cell Antibody General Use: 80% of patients with pernicious anemia have Anti-parietal cells Ab. Useful in diagnosis of atrophic gastritis Test Mnemonic: GPCAB Lab Performing Test: Specimen Processing; Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Gastrin Synonyms: Serum Gastrin General Use: Diagnosis of Zollinger-Ellison syndrome and of pernicious anemia Test Mnemonic: GASTR Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient fasting overnight or at least 12 hours before specimen is drawn Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST); Deliver immediately to lab Volume of Specimen: 10 ml Minimum Volume of Specimen: 2.0 ml serum Causes for Rejection: Gross hemolysis, lipemia, icterus Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Glucagon General Use: Glucagon measurement is useful primarily when considering a glucagon-secreting tumor of the pancreas. Glucagon is also used to diagnose glucagon deficiency in patients with hypoglycemia. Test Mnemonic: GLUCA Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Overnight fasting is required Specimen Required: plasma Container Required: 2 Lavender top (EDTA) tube Volume of Specimen: 2 Lavender top (EDTA) tubes Minimum Volume of Specimen: 3 ml plasma Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 7 days Reference Range: See Report Glucose-6-Phosphate Dehydrogenase Synonym: G-6-PD General Use: Confirmatory test to determine the cause of hemolysis Test Mnemonic: G6PHD Lab Performing Test: Specimen Processing, sent to Reference lab. Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood Container Required: Lavender top tube (EDTA) Volume of Specimen: 5.0 ml of blood (lavender top tube) Minimum Volume of Specimen: 1.0 ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Sent Mon-Sat, no holidays Time required for Processing: 3-5 days Reference Range: See Report Glutamic Acid Decarboxylase-65 Antibody Synonym: Anti-GAD General Use: Useful in identifying Type 2 diabetic individuals who may progress to Type 1 Test Mnemonic: GGAD65 Lab Performing Test: Specimen Processing; Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume Required: 1 ml serum Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Growth Hormone (HGH), Human Synonyms: Human Growth Hormone (HGH); HGH; General Use: (1) Diagnosis of hypopituitarism (2) Diagnosis of acromegaly Test Mnemonic: HGRH Lab Performing Test: Specimen Processing: Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Random growth hormone collection should be performed on fasting patients who have rested for at least 30 minutes prior to collection Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis, Plasma Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Haptoglobin General Use: Evaluation of intravascular hemolysis and acute or chronic inflammatory response Test Mnemonic: HAP Lab Performing Test: Specimen Processing; Sent to reference lab. Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml serum Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 3-4 days Reference Range: See report Heavy Metal Screen, blood General Use: Useful in the diagnosis of toxicity due to arsenic, cadmium, lead or mercury exposure Test Mnemonic: HEAVY Test Includes: Arsenic, Lead, Cadmium and Mercury Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient should refrain from eating seafood and taking herbal supplements for at least 3 days before specimen collection. Specimen Required: Whole blood Container Required: 3 Navy top (EDTA) tubes and 1 Tan top (K-EDTA or sodium heparin) tube Volume of Specimen: 3 - 10 ml Navy (EDTA) tubes and 1- 5 ml Tan tube Minimum Volume of Specimen: 3 Navy (EDTA) tubes and 1 Tan tube Causes for Rejection: Improper tube types Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report Helicobacter Antibodies General Use: To aid in the diagnosis of infection with Helicobacter sp or as a marker of bacterial eradication following therapy Test Mnemonic: HELI Test Includes: Helicobacter IgG, IgM and IgA Lab Performing Test: Specimen Processing; Sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Hemoglobin Electrophoresis Synonym: Hemoglobinopathy Evaluation General Use: To rule out the presence of abnormal hemoglobin Test Mnemonic: HGBELE Test Includes: Hemoglobin A1, Fetal Hemoglobin, Hemoglobin A2 and any hemoglobin variants, Red Blood Cell Count, Hemoglobin, Hematocrit, MCV, MCH, RDW Lab Performing Test: Specimen Processing; Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood (EDTA) Container Required: Lavender top tube (EDTA) Volume of Specimen: 4 ml whole blood Minimum Volume of Specimen: 3 ml of whole blood Availability: Sent out Monday - Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Heparin Anti-Xa LMWH Assay Synonyms: Anti-Xa Assay General Use: To determine therapeutic levels of low molecular weight heparin Test Mnemonic: XAHEP Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient should be on low molecular weight heparin Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Collection Instructions: Deliver to lab immediately! Specimen Required: Plasma Container Required: Blue top tube (sodium citrate) Volume of Specimen: 2 ml plasma Minimum Volume of Specimen: 1 ml plasma Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See printed report Heparin Induced Platelet Antibody Synonym: Heparin Associated Platlet Antibody General Use: Heparin can induce thrombocytopenia, a decreased platelet count, due to antibody stimulation. False positive results may be due to immune complexes. False negative results may be due to low titer, low avidity antibodies. Test Mnemonic: HIPAB Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Separate serum from cells ASAP! Deliver to lab ASAP Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Availability: Sent out Mon-Sat (not holidays) Reference Range: See Report Hepatitis A Antibody, Total with Reflex to IgM General Use: To confirm acute or convalescent phase of Hepatitis A infection. Test Mnemonic: HEPATO Test Includes: If Hepatitis A Antibody Total is reactive, Hepatitis A IgM Antibody will be performed at an additional charge Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report Hepatitis B E Antibody General Use: Presence of antibody is prognostic for resolution of infection due to Hepatitis B virus Test Mnemonic: HBENAB Lab Performing Test: Specimen Processing; Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, lipemia Availability: Sent out Mon - Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: Reported as positive or negative Hepatitis B E Antigen General Use: Predictor of acute active infection with Hepatitis B virus representing the most infectious period. Test Mnemonic: HBENAG Lab Performing Test: Specimen Processing; Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml Causes for Rejection: Gross hemolysis, lipemia Availability: Sent out Mon - Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: Negative Hepatitis B Surface Antigen, Neutralization General Use: Surface antigen usually appears in the serum after an incubation period of 1 to 6 months following exposure to Hepatitis B virus and peaks shortly after onset of symptoms. It typically disappears within 1 to 3 months. Persistence of Hepatitis B surface antigen for greater than 6 months is a prognostic indicator of chronic Hepatitis B infection. Test Mnemonic: HBSAGN Lab Performing Test: Specimen Processing; Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml Causes for Rejection: Gross hemolysis and lipemia Availability: Sent out Mon - Sat (not holidays) Reference Range: See Report Hepatitis B Viral (HBV) DNA Quantitative by PCR General Use: Chronic carriers will persist in producing detectable HBV. Patients with chronic liver disease of unknown origin most commonly have HBV that is detected by viral DNA testing. Quantitative measurement of HBV viral DNA may be used to monitor progression of disease. Test Mnemonic: HBVDNA Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliver ASAP! Specimen Required: Plasma Container Required: 2 lavender top EDTA tubes Volume of Specimen: 3 mL plasma Minimum Volume of Specimen: 2 ml plasma Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 8 days Reference Range: See Report Hepatitis C Genotype General Use: Genotypes are useful as a predictor of the efficacy of anti-viral therapy and disease management Test Mnemonic: HCGENO Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood (EDTA) Container Required: 2 lavender top EDTA tubes; Deliver blood immediately! Volume of Specimen: 2 ml plasma Minimum Volume of Specimen: 1 ml plasma Cause for Rejection: Improper tube type Availability: Sent Mon.- Sat. (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Hepatitis C RNA General Use: To quantitate viral load in patients with chronic Hepatitis C or to measure response to alpha interferon treatment Test Mnemonic: HCVRNA Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliver tubes immediately! Specimen Required: Whole blood (EDTA) Container Required: 2 lavender top tubes, Deliver immediately! Volume of Specimen: 5 ml Minimum Volume of Specimen: 3 mL plasma Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Hereditary Hemochromatosis, DNA, Mutation Analysis Synonym: Hemochrom HFE Gene Anal, Blood, Hemochromatosis General Use: Hereditary Hemochromatosis (HH) is an inherited disorder wherein the body accumulates excess iron. This test establishes HH diagnosis in individuals with abnormal iron study results and identifies at-risk family members. Test Mnemonic: HEMOCH Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: whole blood Container Required: lavender top (EDTA) Volume of Specimen: 2 lavender top tubes (5ml) Minimum Volume of Specimen: entire collection Availability: Sent Mon-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See Report Herpes Simplex Virus Antibodies Synonyms: Herpes simplex titers General Use: Used to support a diagnosis of Herpes Virus infection Test Mnemonic: HERPE Test Includes: Herpes Abs IgG and IgM, Types I & II Lab Performing Test: Specimen Processing; Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red Top Tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Herpes Simplex Virus Culture with Reflex Typing Synonym: Herpes Simplex Virus Culture, includes Typing General Use: There are two HSV serotypes. HSV 1 is commonly associated with infection of non-genital sites. HSV 2 is most commonly associated with genital tract and neonatal infections. Typing may assist in prognosis for lesion recurrence and epidemiological studies. Test Mnemonic: HERP Test Includes: If culture is positive, typing is performed at additional charge Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Vesicle,fluid, scrapings or swab from lesion,. 2 ml CSF urogenital and respiratory specimens, conjuntival or corneal scrapings or tissues in sterile leak-proof container Container Required: V-C-M medium (green cap) tube Volume of Specimen: One swab or 2ml CSF Minimum Volume of Specimen: One swab or 1ml of CSF Special Instructions: Use only plastic shaft rayon on Dacron swabs Causes for Rejection: Raw stool, dry swabs, gel-based transport systems, tissues in fixatives, sputum, specimens received frozen and wooden shaft swabs Availability: Mon- Fri 7am to 3pm Time Required Routinely for Processing: 2 weeks Reference Range: See Report Herpes Simplex Virus (HSV) IgG 1&2 General Use: This assay is type specific and will differentiate between HSV-1 and HSV-2 infections Test Mnemonic: HSVG Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis, lipemia Availability: Sent out Mon-Sat (not holidays) Additional Information: May also be ordered as part of the panel HERPE, which includes HSV IgG 1&2 and HSV IgM Reference Range: See Report Herpes Simplex Virus (HSV) IgM Antibody with Reflex to Titer General Use: To distinguish a primary from a recurrent HSV infection. However, in case of extensive infection (recurrent), an IgM response may be observed. Test Mnemonic: HERIGM Test Includes: If HSV IgM is positive, a titer will be performed at an additional charge. Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross lipemia Availability: Sent out Mon-Sat (not holidays) Additional Information: May also be ordered as part of the panel HERPE, which includes HSV IgG 1&2 and HSV IgM Reference Range: See Report Herpes Simplex Virus/Varicella-Zoster Virus, Rapid Culture General Use: To distinguish VZV from HSV Test Mnemonic: HSVVZV Test Includes: HSV rapid culture and VZV rapid culture Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Swab of lesion or aspirate from mouth, skin or conjunctiva, respiratory specimens, tissue sections, body fluids or CSF Conatiner Required: V-C-M medium (green cap) tube Volume of Specimen: One swab or 0.3 ml aspirate or body fluid Minimum Volume of Specimen: One swab or 0.3 ml aspirate or body fluid Additional Information: Genital, rectal and peri-rectal specimen should be ordered as HERP Causes for Rejection: Dry swabs, gel-based transport systems,slides, stool, urines or wooden-shaft swabs Availability: Mon – Fri 7am to 3pm Time Required Routinely for Processing: 5 days Reference Range: See Report Herpes Virus Detection by Direct Fluorescent Antibody (DFA) Stain and Culture General Use: For Detection of Herpes virus Test Mnemonic: HERPDFA Test Includes: Lab Performing Test: Specimen Processing; Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Container Required: Viral transport media Volume of Specimen: Minimum Volume of Specimen: Causes for Rejection: Availability: Time Required Routinely for Processing: Reference Range: See Report Herpes Virus Detection by PCR General Use: Detection of Herpes Virus Test Mnemonic: HERPPCR Test Includes: Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: CSF best specimen to test Container Required: Sterile Tube Volume of Specimen: Minimum V olume of Specimen: Additional Information: Newborns are swabbed on 4 sies with one swab (conjunctiva,mouth,NP,rectum) Causes for Rejection: Availability: Time Required Routinely for Processing: Reference Range: See Report Histamine, 24 hour urine General Use: Histamine is a mediator of the allergic response. Histamine release causes itching, flushing, hives, vomiting, syncope, and even shock. In addition, some patients with gastric carcinoids may exhibit high concentrations of histamine. Test Mnemonic: UHIS24 Test Includes: Creatinine Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient should avoid direct sunlight. Patient should avoid taking antihistamines, oral corticosteroids and substances which block H2 receptors for at least 24 hours prior to specimen collection. Specimen Required: 24 hour urine collection Container Required: 24 hour urine container with 10 ml 6N HCl, supplied by Specimen Processing lab Volume of Specimen: Entire collection Minimum Volume of Specimen: Entire collection Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report Histamine, blood General Use: Histamine is a mediator of the allergic response. Histamine release causes itching, flushing, hives, vomiting, syncope, and even shock. In addition, some patients with gastric carcinoids may exhibit high concentrations of histamine. Test Mnemonic: HISTA Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Avoid taking allergy causing drugs, antihistamines, oral corticosteroids and substances which block H2 receptors 24 hours prior to collection. Special Instructions: Deliver ASAP! Specimen Required: Plasma Container Required: Lavender top (EDTA) tube Volume of Specimen: 1 Lavender top (EDTA) tube Minimum Volume of Specimen: 1 mL plasma Causes for Rejection: Hemolysis, lipemia, received room temperature Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report Histone Antibodies Synonyms: Anti-Histone Antibody General Use: Diagnostic for differentiating drug-induced lupus from SLE Test Mnemonic: HISTAB Lab Performing Test: Specimen Processing; Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Overnight fasting is preferred Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: Negative Histoplasma Antibody General Use: Aid in the diagnosis of acute broncho-pulmonary histoplasmosis and in the planning of a fungus culture schedule. Test Mnemonic: HIS Test Includes: Antibodies to Yeast and Mycelial antigens Lab Performing Test: Specimen Processing; Sent to Reference lab. Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: This test is also available in the Fungal Serology Panel Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml blood Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: Negative Histoplasma Galactomannan Antigen, Urine General Use: Frequently detected in urine of patients with disseminated histoplasmosis. Test Mnemonic: HISTUR Lab Performing Test: Specimen Processing; sent to Reference lab Request Form Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: urine in sterile container Container Required: Sterile leak-proof urine cup Volume Of Specimen: 10 ml random urine Minimum Volume of Specimen: 1 ml random urine Availability: Mon –Fri 7am to 3pm Time Required Routinely for Processing: 3-6 days References Range: See Report HIV,DNA by PCR General Use: To aid in the diagnosis of AIDS Test Mnemonic: HIVDNA Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Blood must stay at room temp until reaching Lab! Specimen Required: Whole blood (EDTA) Container Required: Lavender top tube (EDTA) Volume of Specimen: 5 ml Minimum Volume of Specimen: 3 ml whole blood Availability: Sent out Mon - Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: Not detected HIV, RNA by PCR (Ultra) General Use: Viral load testing, quantitative Test Mnemonic: HIVQ Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliver to lab immediately! Specimen Required: Plasma Container Required: Lavender top (EDTA) - 2 Volume of Specimen: 5 ml Minimum Volume of Specimen: 3 mL plasma Causes for Rejection: Delay in transport Availability: Sent Mon-Saturday (no holidays) Time Required Routinely for Processing: 1 week Reference Range: See Report HIV Genotype General Use: Evaluation of HIV drug resistance Test Mnemonic: HIVGEN Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood (EDTA) Special Instructions: Deliver tubes to lab immediately! Container Required: Two Lavender top tubes (EDTA) Volume of Specimen: Two 4 ml tubes Minimum Volume of Specimen: 3 ml plasma Causes for Rejection: Improper tube type, delay in receipt of specimen Availability: Sent Mon.-Sat. (not holidays) Reference Range: See report HIV-1 Phenotype Synonym: HIV Antivirogram General Use: Resistance testing is useful when HIV treatment is initiated for changed. Test Mnemonic: HIVPHE Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood (plasma) Container Required: 2 Lavender top EDTA tubes – deliver to Lab immediately Volume of Specimen: 2- 4ml tubes Minimum Volume of Specimen: 2 ml plasma Causes for Rejection: Delay in transport of specimen, improper tube type Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 10 days Additional Information: Assay is intended for use only for patients with viral loads of ≥500 copies. Reference Range: See Report HLA - B27 Synonyms: HLA - Antigen; B27; Tissue Typing General Use: Differential diagnosis of arthritis, HLA-B27 is a marker for MarieStrumpel Disease and may be associated with other diseases Test Mnemonic: HLAB27 Lab Performing Test: Specimen Processing Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood Container Required: 10 mL green top- Na Hep. Obtain from Specimen Processing Lab Volume of Specimen: 10 ml. Keep at room temp. Deliver Immediately! Minimum Volume of Specimen: 5 ml Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report HTLV ABS I & II Test Mnemonic: HTLVAB Test Includes: If HTLV-I/II Antibody is positive, HTLV-I/II Antibody, Confirmatory Assay will be performed at an additional charge Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Centrifuge specimen ASAP Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Sent out Mon-Sat (not holidays) Reference Range: See Report Hypersensitivity Pneumonitis Evaluation General Use: Aid in diagnosis of hypersensitivity pneumonitis Test Mnemonic: HYPEV Test Includes: Micropolyspora faeni, Saccharomonospora viridis, T. candidus, T. sacchari, T. vulgaris, Aspergillus fumigatus, A. pullulans IgG, Alternaria tenuis IgG, Cladosporium herbarum IgG, Penicillium notatum IgG, Phoma spp IgG, Trichoderma viride IgG, Mixed Feathers IgG, Pigeon Droppings IgG Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 9 days Reference Range: See report Hypersensitivity Pneumonitis Screen Synonyms: Aspergillus precipitans, Hypersensitivity screen General Use: Aid in diagnosis of hypersensitivity pneumonitis Test Mnemonic: HPS Test Includes: Aspergillus fumigatus, Micropolyspora faeni, Pigeon Serum, T. candidus, T. vulgaris, S. viridis Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report IDPH see Immune Deficiency Panel IGF (Insulin-like growth factor) Binding Protein-2 Test Mnemonic: IGFP2 Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliver ASAP! Specimen Required: Clotted blood (serum) Container Required: Red top tube – No gel tubes! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis Availability: Sent out Mon-Sat (not holidays) Reference Range: See Report IGF (Insulin-like growth factor) Binding Protein-3 General Use: Of the six distinct IGF binding proteins structurally characterized at this time, IGFBP-3 has been shown to be the major carrier of the IGFs, transporting approximately 95% of circulating IGF-I and IGF-II. Test Mnemonic: IGFBP3 Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube – No gel tubes! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis, lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report IgG (Immunoglobulin G) Subclass 4 Test Mnemonic: IGGSC4 Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Overnight fasting is preferred Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis; lipemia Availability: Sent out Mon-Sat (not holidays) Reference Range: See Report IgG Subclass Fractionation Synonym: Immunoglobulin IgG subclasses General Use: Aid in diagnosis of primary Immunodeficiencies, AIDS, Recurred infectious Diseases, Parasitic Disease, Allergic Disorders, Autoimmune Disease, Malignancies Test Mnemonic: IGGSUB Test Includes: IgG1, IgG2, IgG3, IgG4, total IgG Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Fasting (overnight) preferred Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis, lipemia Availability: Sent Monday - Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Imipramine Synonyms: Tofranil General Use: Therapeutic drug monitoring. Test Mnemonic: IMIP Test Includes: Desipramine (Metabolite) Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube with NO gel barrier! Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Causes for Rejection: Drawn in tube with serum separator (SST), Gross hemolysis Availability: Sent out Monday-Saturday (not holidays) Time Required Routinely for Processing: 5 days Reference Range: See report Immune Complex, C1 Q General Use: High values are associated with the presence of circulating immunecomplexes (CIC). Test Mnemonic: C1Q Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliver to Lab immediately! Specimen Required: Clotted Blood (serum) No Gel barrier tube! Container Required: Red top tube (no gel barrier!) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Moderate and gross hemolysis, lipemia, plasma Availability: Sent out Mon-Sat (not holidays) Additional Information: May also be ordered as part of an Immune Complex Panel Reference Range: See report Immune Complex Panel General Use: To demonstrate the formation of circulating immune complexes Test Mnemonic: IMCP Test Includes: CIC-C3d IgG (Raji) and Immune Complex C1Q Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (No gel barrier!) Deliver immediately to Lab! Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Immune Deficiency Panel Synonyms: T & B Cells, Lymphocyte Subset Panel 3 General Use: Used in assessment of immune deficiency disease (AIDS) i.e. HIV. Test Includes: Absolute Lymphocytes, Percentage CD3, Absolute CD3, Percentage CD4, Absolute CD4, Percentage CD8, Absolute CD8, CD4/CD8 Ratio (calculated) Test Mnemonic: LYMSP3 Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Must be kept at room temperature - do not refrigerate. If a CBC is also required, a separate EDTA (lavender-top) tube must be submitted. Specimen Required: Whole blood Container Required: Lavender top tube (EDTA) Volume of Specimen: 4.0 ml of blood (lavender top tube) Minimum Volume of Specimen: 4.0 ml Causes for Rejection: Clotted, hemolyzed, or refrigerated specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Monday through Friday (cut off for drawing on Friday is 2 pm, no Sat or Sun draws) Time Required Routinely for Processing: 2 - 3 days Reference Range: See printed report Immunoelectrophoresis, Serum Synonyms: IEP Test Mnemonic: IEPS Test Includes: Immunoglobulins, Immunofixation and Serum Protein Electrophoresis (SPE) Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Causes for Rejection: Hemolysis Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Additional Information: Includes Immunofixation and Protein electrophoresis Reference Range: See report Immunoglobulin D Synonyms: IgD General Use: Useful in the diagnosis of myeloma, chronic infections, and acquired deficiency disorders Test Mnemonic: IGD Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Influenza Antibody Panel General Use: Used to support a diagnosis of influenza virus infection Test Mnemonic: INFLAB Test Includes: Influenzae A and B Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Insulin Antibody (Insulin Auto-antibody) General Use: Present in 50% of newly diagnosed Type I diabetic and individuals with Insulin resistance Test Mnemonic: INSAB Lab Performing Test: Specimen Processing; Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (no gel barrier!) Volume of Specimen: 10 ml Minimum Volume Required: 1 ml Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Insulin Growth Factor-1 Synonym Somatomedin-C, IGF-1 General Use: Diagnosis of acromegaly and pituitary deficiency Test Mnemonic: IGF1C Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red – no gel barrier! Deliver to Lab ASAP! Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, lipemia Availability: Sent Mon-Saturday (not holidays) Time Required Routinely for Processing: 8 days Reference Range: See Report Intrinsic factor Antibody Synonyms: IF-blocking Antibodies General Use: Diagnostic of pernicious anemia. Test Mnemonic: IFAB Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Islet Cell Antibody General Use: Useful as an early marker of beta pancreatic cell destruction Test Mnemonic: ISLET Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report JAK2 Mutation General Use: Diagnose Polycythemia Vera (PV), Essential Thrombocythemia (ET), and Idiopathic Myelofibrosis (MF) Test Mnemonic: JAK2 Test Includes: If the JAK2 V617F result is negative, then Exons 12, 13 will be performed at an additional charge Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Label tube with time and date of draw Specimen Required: Whole Blood (EDTA) Container Required: Lavender top EDTA Volume of Specimen: 6 ml Minimum Volume of Specimen: 4 ml Causes for Rejection: Gross hemolysis, clotted blood Availability: Sent out Mon-Sat (not holidays) Reference Range: See report Jo-1 Antibody General Use: To aid in the diagnosis of polymyositis and dermatomyositis Test Mnemonic: JO1 Lab Performing Test: Specimen Processing; Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: Sent out Mon - Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Keppra Synonym: Levetiracetam General Use: Monitoring for patients on Keppra therapy Test Mnemonic: KEPPRA Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube – No gel tubes! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Received room temperature, incorrect tube Availability: Sent out Mon-Sat (not holidays) Reference Range: See Report Lamictal Synonym: Lamotrigine General Use: Drug monitoring for patients on Lamotrigine therapy Test Mnemonic: LAMIC Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube, No gel barrier! Deliver to Lab immediately! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1.0 ml serum Causes for Rejection: Improper tube type, gross hemolysis, lipemia Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report Lead, Blood Synonyms: Pb, Blood General Use: Lead toxicity, lead poisoning Test Mnemonic: LEADP Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole venous blood Container Required: 1 Lavender top( Must be protected from light) tube and 1 tan top tube Volume of Specimen: Lavender top 5 ml (protect tube from light!), Tan top 3 ml Minimum Volume of Specimen: 3 ml each tube Causes for Rejection: Lavender top tube not protected from light Availability: Sent Monday-Friday (not holidays) Time Required Routinely for Processing: 1 week Additional Information: For STAT Lead testing contact Specimen Processing to make special arrangements. Reference Range: See report Legionella Serology Synonyms: Legionnaires Disease Serology General Use: To support diagnosis of infection with Legionella pneumophila Test Mnemonic: LEGS Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (No Gel) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Lipoprotein A Synonym: Lp(a) General Use: Elevations of Lpa are associated with increased risk of CAD Test Mnemonic: LPA Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient must be fasting Specimen Required: Clotted blood (serum) Container Required: Red top tube- (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross lipemia Availability: Sent Mon-Saturday (no holidays) Time Required Routinely for Processing: 1 week Reference Range: See Report Lipoprotein Fractionation Panel 2, Ion Mobility General Use: Evaluation of hyper or hypolipidemia; phenotyping Test Mnemonic: LIPOSZ Test Includes: LDL, Total; LDL, Medium and Small; LDL, Very Small; HDL, Large; LDL Peak Diameter; LDL Phenotype Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: 12-14 hours fasting required Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Causes for Rejection: Non-fasting sample, gross hemolysis, lipemia Availability: Sent Mon - Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report for interpretation Lipoprotein Electrophoresis Test Mnemonic: LIPOEL General Use: Evaluation of hyper or hypolipidemia; phenotyping Test Includes: Cholesterol, Triglycerides, Chylomicrons, Beta Lipoproteins, PreBeta Lipoproteins, and Alpha Lipoproteins Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: 12-14 hours fasting required Specimen Required: Clotted blood (serum) Container Required: Red top tube (No Gel) Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Causes for Rejection: Non-fasting sample Availability: Sent Mon - Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report for interpretation Liver-Kidney Microsomal Antibody (IgG) Synonyms: Anti -LKM General Use: Anti-LKM Abs are found in a subgroup of patients with autoimmune chronic active hepatitis (CAH) Test Mnemonic: LKM Lab Performing Test: Specimen Processing; Sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Reasons for Rejection: Gross hemolysis, lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Lorazepam Synonym: Ativan Test Mnemonic: LORAZ Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: 2 Red top tubes – No gel tubes! Volume of Specimen: 2 Red top (no gel) tubes Minimum Volume of Specimen: 4 ml serum Causes for Rejection: SST Tube Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 3 days Reference Range: See Report Lyme Disease Antibody with Reflex to CSF ratio General Use: The Borrelia burgdorferi antibody index is used as an aid for the diagnosis of neuroborreliosis. Test Mnemonic: LYMIND Test Includes: Borrelia burgdorferi IgG, IgM Antibodies (CSF and Serum); Total IgG and Total IgM (CSF and Serum); Albumin (CSF and Serum); Borrelia burgdorferi Antibody Index; Albumin Ratio Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Test requires both serum and CSF. Collect serum and CSF samples within 24 hours of each other. Specimen Required: CSF and Clotted blood (serum) Container Required: CSF – sterile tube; Red top tube (SST) Volume of Specimen: 2 ml CSF and 1 Red top tube (SST) Causes for Rejection: For CSF collection, it is important to obtain a clean tap. The presence of red cells invalidates the assay. Xanthrochromic or turbid CSF is not acceptable. Availability: sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 4-8 days Reference Range: See Report Lyme Titer, CSF General Use: To aid in the diagnosis of CNS involvement with Lyme disease Test Mnemonic: LYMESF Test Includes: Lyme IgG and Igm titers Lab Performing Test: Specimen Processing; Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: It is recommended that serum samples be ordered along with CSF tests for valid comparison and interpretation Specimen Required: Cerebrospinal fluid Container Required: Sterile container, glass or plastic tube Volume of Specimen: 1 ml Minimum Volume of Specimen: 1 ml Availability: Sent Mon.-Sat., not holidays Time Required Routinely for Processing: 1 week Reference Range: See report Lyme Titer, Misc Fluid General Use: To aid in diagnosis of Lyme arthritis with joint involvement Test Mnemonic: LYMISC Test Includes: Lyme fluid IgG and IgM Lab Performing Test: Specimen Processing; Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Please specify fluid source Specimen Required: Appropriate fluid (not CSF) Container Required: Sterile glass or plastic tube Volume of Specimen: 2 ml fluid Minimum Volume of Specimen: 1 ml fluid Causes for Rejection: Clotted fluid sample Availability: Sent Mon.-Sat., not holidays Time Required Routinely for Processing: 1 week Reference Range: See report Lyme - Western blot Synonyms: Lyme, Immunoblot, Burrelia burgdorferi General Use: To support a diagnosis of Lyme disease or to rule out "false positive" ELISA tests Test Mnemonic: WESTQ Test Includes: Antibody banding to IgG and IgM Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: No antibody bands present. Interpretation provided with report Lymphocyte Enumeration Panel Synonym: Lymphocyte Subset Panel 1 General Use: Immunophenotypic analysis may assist in evaluating cellular immunocompetency in suspected cases of primary and secondary immunodeficiency states. Test Mnemonic: LENUP Test Includes: Absolute Lymphocytes, Absolute CD3, Percentage CD3, Absolute CD4, Percentage CD4, Absolute CD8, Percentage CD8, CD4/CD8 Ratio (calculated), Absolute CD16/56, Percentage CD16/56, Absolute CD19, Percentage CD19 Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Keep at Room Temperature! If a CBC is also required, a separate EDTA (lavender-top) tube must be submitted. Specimen Required: Whole blood Container Required: 3 Lavender top (EDTA) tubes Minimum Volume of Specimen: 3 Lavender top tubes Availability: Sent out Mon-Sat (not holidays) Reference Range: See Report Lymphocytic Choriomeningitis Virus Antibody Synonyms: LCM Ab General Use: To aid in the diagnosis of infection due to LCV Test Mnemonic: LCV Test Includes: Lymphocytic Choriomeningitis Virus Antibodies IgG and IgM Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: Negative Lysozyme Synonym: Muramidase General Use: Lysozyme plays an important role in a host's defense against microorganisms. Lysozyme concentrations are increased in patients with acute myelocytic leukemia with monocytic differentiation (FAB M4/M5). Concentrations may also be increased in patients with other leukemias, sarcoidosis, and infections such as tuberculosis. With sarcoidosis, lysozyme may be useful in monitoring disease and treatment. Test Mnemonic: LYSO Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Reasons for Rejections: Incorrect tube type Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report Magnesium, RBC General Use: Magnesium is an essential trace element. Deficiency leads to irritability, neuromuscular abnormalities, cardiac and renal damage. Its salts are used as antacids and cathartics. Excessive amount may cause CNS depression, loss of muscle tone, respiratory and cardiac arrest. Test Mnemonic: MAGRBC Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Pateint should refrain from taking vitamins or mineral herbal supplements for at least one week before sample collection Specimen Required: Whole Blood (EDTA) Container Required: Lavender top EDTA tube Volume of Specimen: Entire specimen Minimum Volume of Specimen: 1 mL whole blood Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Magnesium, Urine 24 hour General Use: Evaluate magnesium metabolism Test Mnemonic: UMG24 Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: 24 hour collection or random urines Patient Preparation: Do not include first morning specimen. Collect all sunsequent voiding. The last sample should be the first morning specimen voided the following morning at the same time as the previous morning’s first voiding. Container Required: 24 hour acidified urine container obtained from Specimen Processing Lab Volume of Specimen: Entire specimen Minimum Volume of Specimen: Entire specimen Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Magnesium, Urine Random General Use: Evaluate magnesium metabolism Test Mnemonic: UMG Test Includes: Creatinine Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Random urine Container Required: No preservative! Volume of Specimen: Entire specimen Minimum Volume of Specimen: 1 mL urine Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Mephobarital Level Synonyms: Mebaral General Use: Monitor therapeutic drug level Test Mnemonic: MEPBAR Test Includes: Mephobarbital and Phenobarbital (metabolite) Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube - No gel barrier! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Reasons for Rejection: Collected in SST tube Availability: Sent Mon-Sat. (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report MecSTAT 7 panel General Use: Drug screening for breast milk Test Mnemonic: MEC7 Test Includes: 7 drug panel Lab Performing Test: Specimen Processing, sent to Reference lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Requires “Chain of Custody”. Call Specimen Processing lab for instructions @ ext 4153 Specimen Required: Breast Milk Container Required: special tamper proof container, call Specimen Processing lab for kit. Minimum Volume of Specimen: 10 mLs of breast milk Causes for Rejection: Chain of custody protocol not followed or insufficient sample volume. Availability: Sent Mon-Sunday including holidays Time Required Routinely for Processing: 1-3 days Reference Range: See Report MecSTAT 9 panel General Use: Drug screening for newborns Test Mnemonic: MEC9 Test Includes: 9 drug panel Lab Performing Test: Specimen Processing, sent to Reference lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Requires “Chain of Custody”. Call Specimen Processing lab for instructions @ ext 4153 Specimen Required: Meconium Container Required: Special tamper proof container, call Specimen Processing lab for kit. Minimum Volume of Specimen: 2 gms of meconium Causes for Rejection: Chain of custody protocol not followed or insufficient sample volume. Availability: Sent Mon-Sunday including holidays Time Required Routinely for Processing: 1-3 days Reference Range: See Report Mercury, blood Synonym: Hg Test Mnemonic: MERC Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Plasma Container Required: Navy (EDTA) tube Volume of Specimen: 4 ml plasma Minimum Volume of Specimen: 1 mL of plasma Reasons for Rejection: SST tube Availability: Sent out Mon-Sat (not holidays) Reference Range: See Report Metanephrines, Plasma General Use: Increased levels can be found in patients suffering from pheochromocytoma, ganglioneuroma and neurogenic factors. Test Mnemonic: METNP Test Includes: Metanephrine, Normetanephrine, and total Metanephrine Lab Performing Test: Specimen Processing, sent to Reference lab. Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Specimens must be drawn in “pre-chilled” tubes. Keep the tubes on ice for transport to the lab! Send to lab ASAP! Specimen Required: Plasma Container Required: Two (2) lavender top pre-chilled EDTA tubes kept on ice. Volume of Specimen: Entire collection tubes should be sent to lab Minimum Volume of Specimen: 3-5ml plasma Causes for Rejection: Specimen not drawn in pre-chilled tubes and/or not kept on ice during transport. Availability: Sent out Monday- Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See Report Metanephrines, Total, 24 hour Urine General Use: Evaluate catecholamine disorders Test Mnemonic: UMET24 Test Includes: Metanephrine, Normetanephrine, total metanephrine Lab Performing Test: Specimen Processing: sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: 24 hour urine Special Instructions: Keep refrigerated during collection Container Required: 24 hour urine container with preservative supplied by Specimen Processing Lab Volume of Specimen: Entire collection Minimum Volume of Specimen: Entire collection Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Additional Information: Medications patient is receiving are important in interpretation Methadone, urine General Use: Methadone is used in the detoxification and maintenance programs for physical dependence on narcotics. The analysis for methadone is useful in the determination of compliance with maintenance program prescriptions, and in the determination of dose effectiveness. Test Mnemonic: METHU Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Urine Container Required: Plastic sterile container Volume of Specimen: 15 mL Minimum Volume of Specimen: 5 mL urine Availability: Sent out Mon-Sat (not holidays) Reference Range: See Report Methotrexate Level General Use: Monitor therapeutic drug level Test Mnemonic: MTX Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Collect 24, 48, or 72 hours after dose Specimen Required: Clotted Blood (Serum); protect from light; (wrap with aluminum foil) Container Required: Red top tube; protect from light at time of draw (Do not use SST tubes) No gel barrier! Deliver immediately! Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Specimen not protected from light; gel barrier tube Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Methylenetetrahydrofolate Reductase Synonyms: MTHFR General Use: To assess a mutation in the methylenetetrahydrofolate gene which regulates homocysteine; such a mutation could lead to a prothrombotic condition Test Mnemonic: MTHFR Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10 ml of blood collected must be discarded. Specimen Required: Whole blood Container Required: Lavender top tube (EDTA) Volume of Specimen: One full lavender top tube Minimum Volume of Specimen: One full lavender top tube Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 14 days Reference Range: See Report Methylmalonic Acid General Use: To confirm tissue cobalamin deficency in individuals with low serum cobalamin levels Test Mnemonic: METMAL Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Specimen must be sent to Main Lab within 1 hour of draw time Specimen Required: Clotted blood, serum Container Required: Red Top Tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent Monday-Saturday (not holidays) Time Required Routinely Required for Processing: 1 week Reference Range: See report MTHFR see Methylenetetrahydrofolate Reductase Microsporidia Spore Detection General Use: Detection of Microsporidia infection Test Mnemonic: MSPOR Test Includes: Smear and concentration Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Stool Container Required: Sterile screw-cap container with 10% formalin ; Specimen must be transferred to formalin vial within 30 minutes of collection Volume of Specimen: 5g(5ml) of stool Minimum Volume of Specimen: 5g (5ml) stool Causes for Rejection: Unpreserved or frozen stool Availability: Mon – Fri 7am to 3pm Time Routinely Required for Processing: 5 days Reference Range: None Detected Multiple Sclerosis Panel Synonyms: MSP, MS Panel General Use: Evaluation of CSF for infections, degenerative or neoplastic processes Test Mnemonic: MSP1 Test Includes: Albumin (CSF and Serum), IgG (CSF and Serum), Oligoclonal Bands CSF, and IgG Synthesis Rate/Index, CSF (calculated) Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Blood must be drawn at same time CSF is obtained Specimen Required: Cerebrospinal fluid, clotted blood (serum) Container Required: Clean glass or plastic container (CSF) and Red top (SST) Volume of Specimen: 3 ml CSF and 10 ml blood Minimum Volume of Specimen: 3 ml CSF, 2 ml serum Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Mumps Antibodies General Use: To aid in the diagnosis of infection with mumps virus Test Mnemonic: MUMPS Test Includes: Mumps Ab IgG and IgM Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Reasons for Rejection: Gross hemolyis, lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Myasthenia Gravis Panel General Use: To aid in the diagnosis and management of Myasthenia gravis Test Mnemonic: MYGR Test Includes: Anti-Striated Muscle Antibody Screen with Reflex; Acetylcholine Receptor Binding Antibody. If Anti-Striated Muscle Antibody Screen is positive, Anti-Striated Muscle Antibody Titer will be performed at an additional charge. Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Causes for Rejection: Gross hemolysis Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Mycoplasma Serology Synonyms: Mycoplasma pneumoniae Titer General Use: Used to support a diagnosis of Mycoplasma infection, atypical viral pneumoniae Test Mnemonic: MYCOAB Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Myelin Basic Protein General Use: The pesence of myelin basic protein in the spinal fluid is supportive evidence for the diagnosis of multiple sclerosis and other demyelinating diseases, although it is a non-specific finding and present in other causes of damage to CNS myelin. Test Mnemonic: MBP Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Cerebrospinal Fluid Container Required: Sterile plastic container Volume of Specimen: 1.2 ml CSF Minimum Volume of Specimen: 0.5 mL Causes for Rejection: Hemolysis Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report Myoglobin General Use: The breakdown of skeletal muscle releases myoglobin Test Mnemonic: MYO Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10ml Minimum Volume of Specimen: 0.5 ml serum Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report Myoglobin, Urine General Use: The breakdown of skeletal muscle releases myoglobin Test Mnemonic: UMYOG Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Urine- Deliver ASAP! Container Required: Sterile Cup Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml urine Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report Mysoline, Level Synonyms: Primidone General Use: Monitor therapeutic drug level Test Mnemonic: PRIMA Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube - no gel barrier (SST) tubes Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Drawn in gel barrier tube Availability: Sent Mon. - Sat. (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See report Neisseria gonorrhoeae DNA, SDA Synonym: Gonorrhea,GC General Use: For detection of Gonorrhea Test Mnemonic: GC Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Urine or endocervical, urethral or vaginal swab Container Required: BD Transport or BD Urine Preservative Transport kit Volume of Specimen: One swab or 15-60 ml of urine Minimum Volume of Specimen: One swab or 15 ml of urine Causes for Rejection: Swabs received in any other transport kit. Overfilled or underfilled urine transport container. Cleansing swab received. Availability: Sent out Monday-Saturday (not holidays) Time Required Routinely for Processing: 4 days Additional Information: Pink swab for vaginal specimens, blue swab for urethral specimens Reference Range: Not detected Nickel Test Mnemonic: NI Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Serum Container Required: Royal blue top tube Volume of Specimen: 2 mL Minimum Volume of Specimen: 1 mL Causes for Rejection: SST tube received, grossly hemolyzed Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 7 days Reference Range: See Report Niemann-Pick Disease Mutation Analysis General Use: Niemann-Pick Disease, a debilitating and fatal disease, is caused by an inherited deficiency of the enzyme acid sphingomyelinase. Niemann-Pick Disease is an autosomal recessive disease with a carrier rate of 1 in 90 among Ashkenazi Jews and a much lower carrier rate in other populations. Mutation Analysis detects greater than 95% of mutations described in the Ashkenazi Jewish population. Test Mnemonic: NIEMAN Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Keep at Room Temperature! Specimen Required: Whole blood Container Required: Lavender top tubes (2) Volume of Specimen: 2 Lavender top tubes Minimum Volume of Specimen: 5 ml Whole blood Availability: Sent out Mon-Sat (not holidays) Reference Range: See Report Nortriptyline Synonyms: Aventyl General Use: Monitor therapeutic drug level Test Mnemonic: NORT Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Collect just before next dose or at least 12 hours after last dose. Specimen Required: Clotted blood (serum) Container Required: Red top with NO gel barrier! Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Drawn in tube with gel barrier, gross hemolysis Availability: Sent out Monday-Saturday (not holidays) Time Required Routinely for Processing: 3-4 days Reference Range: See report Organic Acids, urine General Use: Evaluation/Diagnosis of inborn error of metabolism Test Mnemonic: ORGUR Test Include: 78 organic acids. Contact the lab at x4153 for details Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Refrigerate during collection Specimen Required: Random urine Container Required: Urine cup, no preservative Volume of Specimen: Entire collection Minimum Volume of Specimen: Entire collection Availability: Sent out Mon-Thurs only Reference Range: See Report Ova and Parasites, Stool, Concentrate and Permanent Smear Synonym: O and P with Permanent Stain General Use: To aid in correct diagnosis of intestinal parasitic infection Test Mnemonic: OAP Lab Performing test: Specimen Processing; Sent to Reference lab Request Form Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Interfering substances – bismuth,barium (wait 7-10 days) Antimicrobial agents (wait 2 weeks), gallbladder dye (wait 3 weeks after procedure) Specimen Required: Stool Container Required: 10% formalin transport vial and PVA transport medium Volume of Specimen: Add stool to bring liquid level on vials to the “fill to here” line Minimum Volume of Specimen: Add stool to bring liquid level on vials to the “fill to here” line Causes for Rejection: unpreserved stool, specimens containing barium and stools in vials other than 10% formalin and PVA Availability: Mon-Fri 7a to 3p Time Required Routinely for Processing: 4 days Reference Range: See Report Oxalate, Urine General Use: Renal function test; patients who form calcium oxalate kidney stones appear to absorb and excrete a higher portion of their dietary oxalate in urine than do normal subjects Test Mnemonic: UOXA24 Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient should refrain from taking excessive amounts of Ascorbic Acid or Oxalate-rich foods (i.e., spinach, coffee, tea, chocolate, rhubarb) for at least 48 hours prior to the collection period. Special Instructions: Specimen must be kept refrigerated during collection Specimen Required: 24 hour urine Container Required: Use 24 hour acidified urine container obtained from Specimen Processing Lab Volume of Specimen: Entire collection Minimum Volume of Specimen: Entire collection Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 3 days Reference Range: See report Paraneoplastic AB Evaluation General Use: To aid in the diagnosis of paraneoplastic autoimmune sensory/motor disorders Test Mnemonic: PARANO Test Includes: Hu Ab, Yo Ab Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent Mon - Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Parvovirus titers Synonyms: Fifth's Disease titer, Parvovirus B-19 General Use: To rule out exposure to Parvovirus in pregnant females during first trimester or aid in the diagnosis of parvovirus arthritis Test Mnemonic: PARVO Test Includes: Parvovirus IgG and IgM Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Additional Information: Information must include estimated delivery date for pregnant females Reference Range: See report Pentobarbital Synonym: Nembutal Test Mnemonic: PENTO Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Collect just prior to next dose Specimen Required: Clotted blood (serum) Container Required: Red top tube – No gel tube! Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Reasons for Rejection: SST tube Availability: Sent out Mon-Sat (not holidays) Reference Range: See Report Phencyclidine Test Mnemonic: PCP Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tubes (2) – No gel tubes! Volume of Specimen: 2 Red top (no gel) tubes Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Reference Range: See Report Phenylalanine, PKU Synonyms: Phenylketonuria test General Use: PKU screen or monitor of diet Test Mnemonic: PKU Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood (plasma) Container Required: Green top tube (Na Heparin); deliver ASAP! Volume of Specimen: 3 ml whole blood Minimum Volume of Specimen: 2 ml plasma Availability: Sent Monday-Friday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Phenytoin, Free Synonym: Free Dilantin General Use: Free dilantin is a better estimate of the active drug level at the body receptor sites. Test Mnemonic: FDILA Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube, No gel barrier. Deliver to Lab immediately! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 3 days Reference Range: See Report Phosphatidylserine Antibodies (IgG, IgM) Test Mnemonic: PHOSAB Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Plasma, 3.2% sodium citrate Container Required: Light blue top, 3.2% sodium citrate tube Volume of Specimen: 5 mL Minimum Volume of Specimen: 1 ml plasma Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report Phospholipids General Use: Phospholipids are used in diagnosing and treating disorders of lipid metabolism associated with atherosclerosis. Test Mnemonic: PHOSLP Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Fasting required! Specimen must be centrifuged within one hour of collection and poured off into plastic transfer tube Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gel barrier tube Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 5 days Reference Range: See Report PNH with FLAER (High Sensitivity) Synonym: Paroxsysmal Nocturnal Hemoglobinuria, GPI, PI Linked antigen Test Mnemonic: PNHHS Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Keep at Room Temperature! Specimen Required: Whole blood Container Required: 10 mL green top, sodium heparin tube Volume of Specimen: 10 mL Minimum Volume of Specimen: 5 mL Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report Poliovirus Antibody, Neutralization General Use: This sensitive procedure is recommended for vaccine response testing and type-specific serodiagnosis of recent poliovirus infection. Test Mnemonic: POLAB Testing Includes: Poliovirus Types 1, 2, and 3 Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Serum Container Required: Red top, SST tube Volume of Specimen: 10 mL Minimum Volume of Specimen: 2 mL Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 2-8 days Reference Range: See Report Porphobilinogen, 24 hour urine General Use: Urinary Porphobilinogen is the first step in the diagnosis of acute intermittent prophyria (AIP). AIP is an autosomal dominant disorder characterized by deficiency of porphobilinogen deaminase. Acute attacks usually include gastrointestinal disturbance and neuropsychiatric disorders. Test Mnemonic: UPBG24 Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Keep refrigerated during collection. Protect from light, Deliver ASAP! Specimen Required: 24 hour urine collection Container Required: 24 hour urine container, no preservative Volume of Specimen: Entire collection Minimum Volume of Specimen: Entire collection Reasons for Rejection: Not protected from light Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 4 days Reference Range: See Report Porphyrins, Fractionated, Quantitative and Porphobilinogen, 24-Hour Urine General Use: Evaluate porphyrias, lead poisoning Test Mnemonic: UPOR24 Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Do not expose to light; Keep refrigerated; Deliver immediately after collection. Specimen Required: 24 hr urine; refrigerate during collection time; protect from light (wrap in aluminum foil) Container Required: Special urine container supplied by Specimen Processing lab Volume of Specimen: Entire specimen Minimum Volume of Specimen: Entire specimen Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Porphyrins, Fractionated, Quantitative, Random Urine General Use: Evaluate porphyrias, lead poisoning Test Mnemonic: UPORSC Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Do not expose to light; Refrigerated during collection. Deliver immediately after collection. Specimen Required: Random Urine (wrap in aluminum foil) Container Required: Sterile urine cup protected from light Volume of Specimen: Entire specimen Reason for Rejection: Specimen not protected from light Minimum Volume of Specimen: 2 mL Urine Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Primadone Test Mnemonic: PRIMA Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Serum Container Required: Red top no gel tube Volume of Specimen: 2.0 mL Reason for Rejection: SST (Gel) tube received Minimum Volume of Specimen: 1 mL serum Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Prograf Synonym: Tacrolimus General Use: Immunosuppressant drug therapy Test Mnemonic: PROGRA Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Optimal time to draw is 0.5-1 hour before next dose Specimen Required: whole blood plasma Container Required: Lavender top (EDTA) Volume of Specimen: 5 ml Minimum Volume of Specimen: 2 ml whole blood Reasons for Rejection: Clotted, SST tube Availability: Sent Mon-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See Report Pro-Predict Metabolites Synonym: Prometheus metabolites General Use: Useful for monitoring patients on Immuran therapy Test Mnemonic: PROPRE Test Includes: 6-TG and 6-MMP Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood Container Required: 2 Lavender top (EDTA) tubes Volume of Specimen: 5ml whole blood (2 tubes) Minimum Volume of Specimen: 5 ml whole blood Availability: Sent Monday-Friday (not holidays) Time Required Routinely for Processing: 5-7 days Reference Range: See Report Protein Electrophoresis, Serum Synonyms: SPEP General Use: Screening test for serum protein abnormalities Test Mnemonic: EPS Test Includes: Total protein, protein electrophoresis Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Protein Immunoelectrophoresis, Urine Synonyms: Urine Protein Electrophoresis; General Use: This test is used to semi-quantitate Bence Jones proteinuria and to study kidney disorders Test Mnemonic: 24 hr collection: UIEP24; random urine: UIEP Test Includes: Urinary protein fractionation Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: A serum protein electrophoresis should also be ordered for a complete evaluation Specimen Required: Random or 24 hr urine specimen Container Required: Random: routine urine cup, for 24 hr collection obtain container from Specimen Processing Volume of Specimen: Entire collection Availability: Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Prothrombin Gene Mutation Synonyms: Factor II 20210A Mutation General Use: Assess the presence of a gene mutation which has potential to cause thrombosis Test Mnemonic: PTGMUT Lab Performing Test: Specimen Processing, sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Specimen Required: Whole blood Container Required: Lavender top tube (EDTA) - 2 Volume of Specimen: 2 lavender top tubes Minimum Volume of Specimen: 1 lavender top tube Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 8 days Reference Range: See printed report PTH, C Terminal Synonyms: C Terminal Parathyroid hormone General Use: Diagnosis of hypo and hyperparathyroidism Test Mnemonic: PTHC Test Includes: PTH, C Terminal and calcium Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Fasting Special Instructions: Draw specimen between 7:00AM. and 10:00AM. Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST). Deliver to Lab immediately! Volume of Specimen: 10 ml Minimum Volume of Specimen: 5 ml serum Causes for Rejection: Delay in receipt of specimen Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report PSA, Free and Total General Use: To discriminate between prostate Ca and benign prostatic hypertrophy (BPH) Test Mnemonic: FTPSA Test Includes: Total PSA, Free PSA, % Free PSA(calculated) Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST). Deliver to Lab immediately! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Delay in transport of specimen, Gross hemolysis, lipemia, icterus Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report Pyruvic Acid Synonym: Pyruvate Test Mnemonic: PYR Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Call CP lab at ext 4153 before drawing blood! Specimen Required: Whole blood, plasma. Requires special pre-treatment! Container Required: Lavender (EDTA) - 2 Volume of Specimen: 5 ml Minimum Volume of Specimen: 4 ml whole blood Causes for Rejection: Improper specimen treatment prior to transport Availability: Sent Mon-Saturday (not holidays) Time Required Routinely for Processing: 2-3 days Reference Range: See Report Q Fever, Titer Synonym: Coxiella burnetii General Use: Used to support a diagnosis of Q fever due to Coxiella burneti Test Mnemonic: QFEVER Test Includes: Q fever Abs IgG and IgM with reflex to titers Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Quinidine, Blood General Use: Monitor therapeutic drug level Test Mnemonic: QUINI Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube -no gel barrier! Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gel barrier tube (SST) Availability: Mon-Sat. (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See report Rapamycin Synonym: Sirolimus General Use: Monitor therapeutic drug level Test Mnemonic: RAPA Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Optimal time to draw specimen is 0.5 to 1 hour before next oral dose at steady state. Specimen Required: Whole blood Container Required: Lavender top EDTA tube Volume of Specimen: 2 mL Minimum Volume of Specimen: 1 mL whole blood Causes for Rejection: Gel barrier tube (SST), clotted Availability: Mon-Sat. (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See report Renin Activity Synonym: PRA General Use: Useful in evaluating hypertension (renal and renovascular hypertension) Test Mnemonic: REN Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Follow doctor’s instructions since many factors are known to influence plasma renin activity Special Instructions: Deliver tube immediately- keep at room temperature! Specimen Required: EDTA blood, plasma Container Required: 2 Lavender top tube (EDTA) Volume of Specimen: Two tubes (4ml each) whole blood (EDTA) Minimum Volume of Specimen: 4 ml of plasma Causes for Rejection: Improper tube/storage, delay in receipt of specimen; lipemia, received refrigerated. Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report. Respiratory Virus Panel by Direct Fluorescent Antibody Stain General Use: Detection of Respiratory Viruses Test Mnemonic: RESDFA Test Includes: Influenza A,Influenza B, Para-Influenza 1/2/3, Adenovirus, Respiratory Syncitial Virus, Metapneumo virus Lab Performing Test: Specimen Precessing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Nasopharyngeal swab or wash, Bronch wash Container Required: Viral Transport Media Volume of Specimen: Minimum Volume of Specimen: Availability: 7 days per week (fall- winter flu season) Time Required Routinely for Processing: Up to 2 days. Specimens Received by 7pm resulted that day; after 7pm resulted the next day Additional Information: RSV typing for A & B is not performed Reference Range: See Report Respiratory Virus Panel by PCR General Use: For Detection of Respiratory Viruses. PCR detects unique Genetic material from viruses Test Mnemonic: RESPCR Test Includes: Influenza A, Influenza B, Para-Influenza, Adenovirus, Respiratory Syncitial Virus, Rhinovirus, Metapneumo virus Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Nasopharyngeal swab or wash, Bronch wash Container Required: Viral Transport Media Volume of Specimen: Minimum Volume of Specimen: Availability: 7 days (fall-winter flu season) Time Required Routinely for Processing: Up to 2 days. Specimens received by 7pm resulted that day; after 7pm resulted the next day Additional Information: Can be sent to Yale or CT DPH lab. CT DPH Lab tests for more viruses. Reference Range: See Report Reticulin Antibody, IgA General Use: To aid in the diagnosis of Celiac disease Test Mnemonic: RETIGA Includes: If Reticulin antibody IgA screen is positive, Reticulin antibody IgA titer will be performed at an additional charge. Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 0.5 ml serum Reason for Rejection: Gross hemolysis, lipemia Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report Ristocetin Co-Factor General Use: Interpreted by physician Test Mnemonic: RISTO Lab Performing Test: Specimen Processing, sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Fasting for at least 8 hours in preferred. Patient must not be on anticoagulants Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Collection Instruction: Deliver to Lab immediately Specimen Required: Plasma Container Required: Blue top tube (sodium citrate) Volume of Specimen: 1 blue top tube (tube must be full) Minimum Volume of Specimen: 1 full blue top tube Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Sent out Mon-Sat (not holidays) Reference Range: See printed report Rubella Antibodies General Use: To aid in the diagnosis of infection with Rubella (German measles) virus Test Mnemonic: RUBAB Test Includes: Rubella Abs, IgG and IgM Lab Performing Test: Specimen Processing; sent to reference labs Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Rubeola Antibodies Synonyms: Measles titer General Use: Used to support a diagnosis of Rubeola virus infection Test Mnemonic: RUBEA Test Includes: Rubeola IgG and Rubeola IgM Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Schistosoma Serology General Use: To aid in the diagnosis of infection with Schistosoma parasite Test Mnemonic: SCHIS Test Includes: IgG and IgM antibodies Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Scleroderma Antibody Synonyms: Antibody to ScL-70, Topoisomerase I General Use: Useful in the diagnosis of Progressive Systemic Sclerosis (PSS) Test Mnemonic: SCLER Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Reasons for Rejection: Gross hemolysis, lipemia, icterus Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Sex Hormone Binding Globulin Synonyms: Testosterone binding globulin General Use: Useful in the assessment of androgen Status Test Mnemonic: SHBG Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Plasma, gross hemolysis Availability: Sent Mon-Sat (Not holidays) Reference Range: See Report Serotonin, Blood General Use: Evaluation of carcinoid syndromes Test Mnemonic: SERO Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient should avoid food high in indoles. Avoid avocados, bananas, tomatoes, plums, walnuts, pineapple, and eggplant prior to testing. Patient should also avoid tobacco, tea, and coffee three days prior to specimen collection. Specimen Required: Clotted blood (serum), deliver to Lab immediately! Container Required: Red top tube, No gel barrier tubes! Special Instructions: Deliver tube immediately! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Sjogrens Antibodies Synonyms: Antibodies to SS-A/Ro and SS-B/La General Use: To aid in the diagnosis of SLE or Sjogrens Syndrome-Sicca complex Test Mnemonics: SJAB Test Includes: SS-A, SS-B Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, lipemia, icterus Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Smooth Muscle Antibody Synonym: Actin General Use: Diagnostic test for lupoid hepatitis. Useful in the differential diagnosis of primary biliary cirrhosis & chronic active hepatitis. Test Mnemonic: SMA Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Reasons for Rejection: Gross hemolysis, lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Somatostatin General Use: Somatostatin is a neurohormone produced in the brain, hypothalamus and gastrointestinal tract. This test is used to diagnose somatostatin-producing tumors. Elevated levels are observed with somatostatinoma, medullary thyroid carcinoma and pheochromocytoma. Test Mnemonic: SOMAT Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Draw in a pre-chilled lavender top tube. Separate and freeze immediately. Specimen Required: Plasma (EDTA) Container Required: Pre-chilled Lavender top EDTA tube Volume of Specimen: 5 mL Minimum Volume of Specimen: 2 mL plasma Reasons for Rejection: Gross hemolysis, lipemia, icterus Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 3 weeks Reference Range: See report Stone Analysis General Use: Evaluation of stone formation and composition. Test Mnemonic: STONE Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Stones Container Required: Sterile screw top container Volume of Specimen: Send stone specimen only. Do not send stone in urine Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: One week Additional Information: Please indicate site from which stone is removed. Reference Range: See report Striated Muscle Antibodies General Use: Diagnostic test for Myasthenia gravis Test Mnemonic: STRMAB Test Includes: If Striated Muscle Anitbody screen is positive, Striated Muscles Antibody titer will be performed at an additional charge. Lab Performing Test: Specimen Processing; Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: May also be ordered as part of Myasthenia Gravis Panel Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Rickettsia Antibodies Synonyms: Rocky Mountain Spotted Fever Abs, Spotted Fever Typhus, RMSF General Use: Support diagnosis of infection due to Rickettsia in the spotted fever group Test Mnemonic: ROCKY Test Includes: If Rickettsia (RMSF) Antibodies (IgG, IgM) are positive, titers will be performed at an additional charge Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Stool Osmolality, 24 hour Synonym: Osmotic gap, feces Test Mnemonic: STOSM Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliver ASAP! Specimen Required: 24, 48, 72 hour liquid stool Container Required: Plastic leak-proof feces container Volume of Specimen: Entire collection Availability: Sent out Mon-Sat (not holidays) Reference Range: See Report Stool Potassium, 24 hour Synonym: Potassium, feces Test Mnemonic: STOOLK Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Keep refrigerated during collection. Deliver ASAP! Specimen Required: 24, 48, or 72 hour liquid stool Container Required: Plastic leak-proof container Volume of Specimen: Entire collection Availability: Sent out Mon-Sat (not holidays) Reference Range: See Report Stool Sodium, 24 hour Synonym: Sodium, feces Test Mnemonic: STNA Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Keep refrigerated during collection. Deliver ASAP! Specimen Required: 24, 48, or 72 hour liquid stool Container Required: Plastic leak-proof container Volume of Specimen: Entire collection Availability: Sent out Mon-Sat (not holidays) Reference Range: See Report Streptococcus pneumoniae IgG (23 Serotypes) General Use: Responses to pneumococcal vaccines are demonstrated by 2- to 4fold increases in the levels of IgG recognizing approximately 70% of the serotypes contained within a given pneumococcal vaccine. Test Mnemonic: SPNU23 Test Includes: Serotypes 1, 2, 3, 4, 5, 8, 9 (9N), 12 (12F), 17 (17F), 14, 19 (19F), 20, 22 (22F), 23 (23F), 26 (6B), 34 (10A), 43 (11A), 51 (7F), 54 (15B), 56 (18C), 57 (19A), 68 (9V), 70 (33F) Lab Performing Test: Specimen Processing; sent to reference labs Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Streptozyme General Use: To demonstrate the presence of antibodies to a wide variety of Streptococcal enzymes Test Mnemonic: STRZ Test Includes: If Streptozyme Screen is positive, Streptozyme titer will be performed at an additional charge Lab Performing Test: Specimen Processing; sent to reference labs Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Tay-Sachs Detection Synonym: Hexosaminidase A & B General Use: Test for "carrier state" of Tay-Sachs Test Mnemonic: TAYHXA Test Includes: Hexosaminidase A and B Lab Performing Test: Specimen Processing; Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood Container Required: Yellow ACD/2. Deliver ASAP! Volume of Specimen: 20 ml Minimum Volume Required: 20 ml Whole Blood Availability: Sent Monday-Thursday ONLY Time Required Routinely for Processing: 1 week Reference Range: See report Tay-Sachs Gene Mutation Analysis -Tay Sachs Mutation General Use: Genetic Counseling Test Mnemonic: TAYMUT Lab Performing Test: Specimen Processing; Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood (EDTA) Container Required: Lavender top tube - draw 2. Keep room temperature Special Instructions: Deliver tubes immediately to Lab Volume of Specimen: 8 ml whole blood Minimum Volume Required: 8 ml whole blood Causes for rejection: Improper tube type or insufficient quantity Availability: Sent Monday-Saturday (not holidays) Reference Range: See report Tetanus Antitoxoid Antibody Synonym: Tetanus Antibody IgG General Use: Used to evaluate Tetanus immunization efficacy. Test Mnemonic: TETAB Test Includes: Test for Tetanus Antitoxoid IgG Lab Performing Test: Specimen Processing, sent to Reference lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: excessive hemolysis Availability: Sent out Monday thru Saturday (no holidays) Time Required Routinely for Processing: 1 week Reference Range: See report THC Confirmation, Urine Test Mnemonic: UTHCCO Test Includes: Carboxy Acid THC, THC/Creatinine ratio, Creatinine Lab Performing Test: Specimen Processing, sent to Reference lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Random Urine Container Required: Sterile cup Volume of Specimen: 20 mL Minimum Volume of Specimen: 5 mL urine Availability: Sent out Monday thru Saturday (no holidays) Time Required Routinely for Processing: 1 week Reference Range: See report ThinPrep Pap and HR HPV DNA General Use: Liquid-based Pap Testing is intended for use in screening and detection of cervical cancer, pre-cancerous lesions, atypical cells and all other cytologic categories as defined by the Bethesda System for Reporting Results of Cervical Cytology. Test Mnemonic: PAP 15003 Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Gynocological sample Container Required: Pap sample collected in PreservCyt, alcohol-based solution that serves as preservative, transport, and antibacterial medium for samples. Volume of Specimen: Entire collection Minimum Volume of Specimen: Entire collection Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 5-10 days negative, 7-12 days abnormal Reference Range: See report ThinPrep Pap with reflex to HR HPV DNA General Use: Liquid-based Pap Testing is intended for use in screening and detection of cervical cancer, pre-cancerous lesions, atypical cells and all other cytologic categories as defined by the Bethesda System for Reporting Results of Cervical Cytology. Test Mnemonic: PAP 31530 Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Gynocological sample Container Required: Pap sample collected in PreservCyt, alcohol-based solution that serves as preservative, transport, and antibacterial medium for samples. Volume of Specimen: Entire collection Minimum Volume of Specimen: Entire collection Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 5-10 days negative, 7-12 days abnormal Reference Range: See report ThinPrep Imaging Pap Test Mnemonic: PAP 58315 Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Gynocological sample Container Required: Pap sample collected in PreservCyt, alcohol-based solution that serves as preservative, transport, and antibacterial medium for samples. Volume of Specimen: Entire collection Minimum Volume of Specimen: Entire collection Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 5-10 days negative Reference Range: See report Thrombin Time General Use: Determination of severe hypofibrinogenemia or qualitative abnormality of fibrinogen Test Mnemonic: TT Lab Performing Test: Specimen Processing, sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient must not be on anticoagulants Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Collection Instruction: Deliver to Lab immediately! Specimen Required: Plasma Container Required: Blue top tube (sodium citrate) Volume of Specimen: 1 full blue top tube Minimum Volume of Specimen: 1 ml plasma from full blue top tube Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Sent out Mon-Sat (not holidays) Reference Range: See on printed report. Thyroglobulin Synonym: Thyroglobulin Antibodies General Use: Thyroid disease testing Test Mnemonic: THYRO Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Reasons for Rejection: Gross hemolysis Availability: Sent Mon-Saturday (not holidays) Time Required Routinely for Processing: 2-3 days Reference Range: See Report Thyroglobulin Antibodies Synonym: Antithyroglobulin Abs General Use: Useful in the diagnosis and management of Thyroid disorders Test Mnemonic: TGA Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml sreum Reasons for Rejection: Gross hemolysis Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report Thyroid Auto-Antibodies General Use: Diagnostic test for Hashimoto's thyroiditis; thyroid function test Test Mnemonic: THYAA Test Includes: Thyroglobulin Abs and Thyroid Peroxidase Abs Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Reason for Rejection: Gross hemolysis, lipemia Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Thyroid Peroxidase Ab Synonym: Anti-thyroid Micrsomal Antibody, Anti-TPO General Use: Thyroid disease testing Test Mnemonic: TPO Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent Mon-Saturday (not holidays) Reasons for Rejection: Gross Hemolysis Time Required Routinely for Processing: 2-3 days Reference Range: See Report Thyroid Stimulating Immunoglobulin Synonym: Long acting Thyroid stimulator, Thyroid Stimulating Immunoglobulin General Use: Useful in the treatment of Graves Disease Test Mnemonic: THYSIG Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 0.2 ml Reasons for Rejection: Gross hemolysis, lipemia, icterus, incorrect tube type Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report Thyroxine Binding Globulin Synonyms: TBG General Use: Binding capacity for T-4 Test Mnemonic: TBG Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml of serum Reason for Rejection: Gross Hemolysis Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Tissue Transglutaminase Antibody, IgG Synonyms: tTg antibody (IgG) General Use: Tissue Transglutaminase Antibody, IgG, is useful in diagnosing gluten-sensitive enteropathies, such as Celiac Sprue Disease, and an associated skin condition, dermatitis herpetiformis in patients who are IgA-deficient. Test Mnemonic: TTGIGG Lab Performing Test: Specimen Processing, sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis or gross lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 5 days Reference Range: See report Topamax Synonym: Topiramate General Use: Topamax/Topiramate is an antidepressant used as an adjunctive treatment of partial-onset epilepsy and Lennox-Gastaut syndrome in children. Test Mnemonic: TOPA Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Draw at peak (2-4 hours after dose) or trough (0.5-1hour before dose) at steady state. Do not use gel barrier tubes! Special Instructions: Centrifuge tube within 1 hour of draw Specimen Required: Clotted blood (serum) Container Required: Red top tube, No gel barrier tubes! Deliver to Lab immediately; tube must be centrifuged within 1 hour of draw. Volume of Specimen: 10 mL Minimum Volume of Specimen: 0.5 mL serum Causes for Rejection: Improper tube type, delay in specimen processing Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report Torch Panel General Use: To support diagnosis of Torch infections in newborns or pregnant females Test Mnemonic: TORCH Test Includes: Toxoplasmosis IgG and Igm, Rubella IgG and Igm, Cytomegalovirus IgG and Igm, Herpes IgG and Igm. Lab Performing Test: Specimen Processing; Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Two (2) red top tubes (SST) Volume of Specimen: 15 ml Minimum Volume of Specimen: 5 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: Reference ranges provided with results Toxicology Profile, Blood (Tox. Screen, Blood) Synonyms: Toxicology Screen, Blood General Use: Drug toxicity; toxicology screen Test Mnemonic: DRGS Test Includes: Call lab for complete listing of components Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: 2 red top tubes, No gel barrier! Volume of Specimen: 15 ml blood Minimum Volume of Specimen: 10 ml serum Availability: Sent Monday-Saturday (not holidays) Causes for Rejection: Gel barrier tubes Time Required Routinely for Processing: 1 week Reference Range: See report Toxocara Synonyms: VLM Titer; Toxocara Canis, Visceral larva migrans General Use: Used to support a diagnosis of Visceral larva migrans Test Mnemonic: TOXOC Lab Performing Test: Specimen Processing; sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: Negative Toxoplasmosis Antibodies Synonyms: Toxoplasma Serology General Use: Used to support a diagnosis of Toxoplasmosis gondii Test Mnemonic: TOXAB Test Includes: Toxo IgG and Toxo Igm Lab Performing Test: Specimen Processing; Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 mL Causes for Rejection: Gross hemolysis, lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Toxoplasmosis, Status General Use: Used to determine immunity or past exposure to Toxoplasma gondii Test Mnemonic: TOXOIG Test Includes: Toxoplasma IgG Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Reasons for Rejection: Gross hemolysis, lipemia Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: Reported as immune or non-immune TPMT Synonym: Thiopurine Methyltransferase, Myelosuppresion, Myelotoxicity, SoftTPMT General Use: Detection of individuals with low thiopurine methyltransferase activity who are at risk for excessivr myelosuppression or severe hematopoietic toxicity when taking azathioprine (Imuran) or 6-MP (Purinethol). Test Mnemonic: TPMT Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Test should be ordered/drawn Mon – Thurs only Container Required: Green top sodium heparin 10 ml tube Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 mL Availability: Mon – Thurs only Reference Range: See Report TPMT (Thiopurine S-Methyltransferase) Genotype General Use: This test detects common deficiency variants in the TPMT gene and therefore identifies individuals who are at risk of developing serious adverse effects when administered thiopurine drugs Test Mnemonic: TPMTG Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Keep at room temperature. Do not spin. Specimen Required: Whole blood Container Required: Lavender top tube (EDTA) Volume of Specimen: 4 ml of blood (lavender top tube) Minimum Volume of Specimen: 3 ml Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 9-10 days Reference Range: See printed report Transferrin General Use: Differential diagnosis of anemia Test Mnemonic: TRANS Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis, lipemia Availability: Sent Mon-Saturday (not holidays) Time Required Routinely for Processing: 2-3 days Reference Range: See Report Trileptal Level Synonym: Oxcarbazepine, 10-Hydroxycarbazepine General Use: To monitor patient on Oxcarbazepine therapy Test Mnemonic: TRIL Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube, No gel barrier tubes. Deliver to Lab immediately! Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See Report Tryptase General Use: Tryptase concentrations are increased with immediate hypersensitivity (anaphylaxis), acute allergen challenge, and mastocytosis. Test Mnemonic: TRYPT Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliver ASAP! ` Specimen Required: Clotted blood (serum) Container Required: Red top tube – no gel! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis, SST tube Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: Test performed on Tuesdays Reference Range: See Report TT see Thrombin Time Urine Myoglobin General Use: Interpretation by physician Test Mnemonic: UMYO Lab Performing Test: Specimen Processing, sent to Reference lab. Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Send to L&M Lab immediately. Specimen must be frozen for transport to Reference lab. Specimen Required: Fresh urine Container Required: Urine cup Volume of Specimen: 10 ml Minimum Volume of Specimen: 10 ml Causes for Rejection: Incorrect specimen volume, mislabeled or unlabeled specimen Availability: Sent Mon-Sat, no holidays Time Required Routinely for Processing: 3 days Availability: Sent Mon-Sat, no holidays Reference Range: See Report Vanillylmandelic Acid, 24 Hour Urine Synonyms: VMA General Use: Diagnosis of catecholamine-producing tumors Test Mnemonic: UVMA24 Test Includes: Creatinine Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: It is preferable for the patient to be off medications for three days prior to collection. However, common antihypertensives (diuretics, ACE inhibitors, calcium channel blockers, alpha and beta blockers) cause minimal or no interference. Patient should avoid alcohol, coffee, tea, tobacco (including use of nicotine patch), bananas, citrus fruits and strenuous exercise prior to collection. Specimen Required: 24 hour urine Container Required: 24 hour urine container obtained from Specimen Processing Volume of Specimen: Entire specimen Minimum Volume of Specimen: Entire specimen Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report VAP ™ Cholesterol panel Synonym: Lipid Fractionation, Lipid Subparticle, Expanded Lipid Profile, Expanded Lipid Subparticle, LDL Sub Fraction General Use: The VAP ™ Cholesterol tests is a comprehensive test that includes not only the standard lipid measurement but 21 lipid subfractions and emerging risk factors such as Lp(a), IDL-C and LDL pattern size. Test Mnemonic: VAP Test Includes: Total Cholesterol, Direct LDL Cholesterol, HDL Cholesterol, and direct measured Triglycerides, 21 Lipid Subfractions, Lp(a), IDL-C and LDL pattern size, non-HDL cholesterol components: LDL, IDL, Lp(a), and VLDL Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Although 10-12 hour fast (no alcohol for 24 hours) is required for the most accurate triglyceride measurement, all other values of the VAP test are directly measured and fasting does not affect their outcome. Special Instructions: Specimen must be centrifuged within 3 hrs of time of draw. Deliver to Lab ASAP or call for processing instructions! Specimen Required: clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1.5 mL serum Causes for Rejection: Improper specimen processing, Gross hemolysis Availability: Sent Monday-Sat (not holidays) Reference Range: See Report Varicella Status Synonyms: Varicella - immunity, Chicken pox titer, Herpes Zoster General Use: To determine immunity or past infection with Varicella-Zoster virus. Test Mnemonic: VARIG Lab Performing Test: Specimen Processing; sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: Reported as immune or non-immune Varicella-Zoster, Antibodies Synonyms: Chickenpox titer, Varicella zoster General Use: Used to support a diagnosis of Herpes zoster-Varicella infection Test Mnemonic: VARAB Test Includes: Varicella Abs IgG and IgM Lab Performing Test: Specimen Processing; Sent to Reference lab. Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Vasoactive Intestinal Peptide Synonym: VIP General Use: VIP is a neurotransmitter and its excess can cause secretory diarrhea. VIP-secreting tumors are most commonly found in the tail of the pancreas in adults. VIP-producing ganglioneuromas or ganglioneuroblastomas may be found in the adrenal glands in children. Test Mnemonic: VASOP Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliver immediately! Specimen Required: Plasma Container Required: 2 - Lavender top (EDTA) tubes Volume of Specimen: 2 - Lavender top (EDTA) tubes Minimum Volume of Specimen: 3 ml plasma Causes for Rejection: Lipemic samples not acceptable Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 9 days Reference Range: See Report VDRL-CSF General Use: To aid in the diagnosis of latent syphilis Test Mnemonic: VDSF Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Cerebrospinal fluid Container Required: Clean sterile container Volume of Specimen: 1 ml Minimum Volume of Specimen: 0.5 ml CSF Causes for Rejection: Excessive contamination with RBC's Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 1 week Additional Information: The VDRL slide test is still the only test recommended by CDC for use with cerebrospinal fluid Reference Range: Nonreactive Virus Culture General Use: For Detection of Viruses Test Mnemonic: VIRC Test Includes: Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate (HPA) Specimen Required: Skin swabs, biopsies, respiratory specimens, CSF or stool Container Required: Viral Transport Media Volume of Specimen: Minimum Volume of Specimen: Availability: Time Required Routinely for Processing: Additional Information: MD must specify what viruses to test for. Reference Range: See Report Viscosity, Serum Synonyms: Serum Viscosity General Use: Detection of hyperviscosity syndromes associated with myeloma and other dysproteinemias Test Mnemonic: VISCO Lab Performing Test: Specimen Processing; Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 5 days Reference Range: See report Vitamin A, Blood Synonyms: Retinol General Use: Differential diagnosis of malabsorption syndromes; essential for vision and bone growth Test Mnemonic: VITAA Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Overnight fasting is preferred Special Instructions: Protect specimen from light by wraping in foil Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST); protect from light! Volume of Specimen: 10 ml blood Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Not protected from light Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See report. Vitamin B1 Synonym: Thiamine General Use: Thiamine deficiency of toxicity Test Mnemonic: VITAB1 Lab Performing Test: Specimen Processing, Sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliver to lab immediately, protect tube from light! Specimen Required: Whole blood, plasma Container Required: lavender top (EDTA) Volume of Specimen: 5 ml Minimum Volume of Specimen: entire collection Causes for Rejection: Exposure to light, delay in transport, improper tube type Availability: Sent Mon-Saturday (no holidays) Time Required Routinely for Processing: 1 week Reference Range: See Report Vitamin B2 Synonym: Riboflavin General Use: Rule out Riboflavin deficiency Test Mnemonic: VITB2 Lab Performing Test: Specimen Processing; sent to Reference Lab Request form: Universal requisition; use only as a backup to Meditech Specimen Required: Whole blood (plasma) Container Required: Lavender top tube (EDTA); protect from light! Deliver immediately! Volume of Specimen: 4 ml whole blood Minimum Volume of Specimen: 1 ml plasma Causes for Rejection: Improper tube type, not light protected Availability: Sent Mon.-Sat. (not holidays) Time Required Routinely for Processing: 1 week Additional Information: Specimen must be protected from light; Deliver immediately! Reference Range: See report Vitamin B6 Synonym: Pyridoxine, Pyridoxal, B6 General Use: Vitamin b6 deficiency may be observed in patients with metabolic disorders secondary to drug use or alcoholism. Test Mnemonic: VITB6 Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Overnight fasting. Patient must be restricted from alcohol and vitamins for at least 24 hours before sample collection. Specimen Required: Whole blood (plasma) Container Required: Lavender top tube (EDTA). Protect from light and deliver to Lab immediately!! Volume of Specimen: 5 ml whole blood Minimum Volume of Specimen: 0.5 ml plasma Causes for Rejection: Tube not protected from light. Delay in transport to Lab Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 6 days Reference Range: See Report Vitamin B12 Binding Capacity, Unsaturated Synonym: Transcobalamin General Use: Vitamin B 12 Binding Capacity, Unsaturated (Transcobalamin), binds and transports vitamin B 12 in the circulation. Increased concentrations are associated with patients with myeloproliferative disorders. Decreased concentrations are associated with infants with megaloblastic anemia or transcobalamin deficiency. Test Mnemonic: VB12BI Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Cause for Rejection: Plasma Availability: Sent out Mon-Sat (not holidays) Time Required Routinely for Processing: 8 days Reference Range: See Report Vitamin C Synonym: Ascorbic Acid General Use: Evaluation of Vitamin C deficiency, scurvy Test Mnemonic: VITAC Lab Performing Test: Specimen Processing: sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Overnight fasting is preferred. Patient should refrain from taking vitamin C supplements or fruits 24 hours prior to sample collection. Special Instructions: Deliver to lab immediately, protect tube from light! Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST); protect from light! Deliver immediately! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Not light protected Availability: Sent out Mon.-Sat. (not holidays) Time Required Routinely for Processing: 1 week Additional Information: Specimen must be protected from light; Deliver immediately! Reference Range: See report Vitamin D1, 25-Dihydroxy General Use: Deficiencies of 1,25-dihydoxy Vitamin D, the most active form, causes hypocalcemia, osteomalcia and related disorders. Test Mnemonic: VD125 Test Includes: Vitamin D,1,25 (OH)2,Total; Vitamin D3, 1,25 (OH)2; Vitamin D2, 1,25 (OH)2 Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Keep tube refrigerated after drawing! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1.5 ml serum Causes for Rejection: Improper storage temperature. Availability: Sent Monday-Sat (not holidays) Time Required Routinely for Processing: 5 days Reference Range: See Report Vitamin D, 25 Hydroxy fractionation General Use: Measurement of serum 25-OH vitamin D concentrations provide a good index of circulating vitamin D activity in patients not suffering from renal disease. Lower than normal 25-OH vitamin D levels can result from a dietary deficiency, poor absorption of the vitamin or impaired metabolism of the sterol in the liver. Test Mnemonic: VD25FR Test Includes: Vitamin D, 25-OH, Total; Vitamin D, 25-OH, D 3; Vitamin D, 25OH, D2 Lab Performing Test: Specimen Processing, sent to Reference Lab Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Fasting preferred, but not required Specimen Required: Clotted blood (serum) Container Required: Red top tube – No gel tube! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Sent out Mon-Sat (not holidays) Reference Range: See Report Vitamin E Synonym: Alpha-Tocopherol General Use: Useful in evalutation of Vitamin E deficiency in pre-maturity, cystic fibrosis and mal-absorption syndromes Test Mnemonic: VITAE Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Over night fasting is preferred Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST); protect from light and deliver immediately! Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml Causes for Rejection: Not light protected, delay in receipt of specimen Availability: Sent out Mon.-Sat. (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Vitamin K General Use: Vitamin K is a required co-factor for the synthesis of factors 2, 7, 9, and 10 and proteins C and S. Deficiencies of vitamin K lead to bleeding. Coumadin® (warfarin) acts as an anticoagulant because it is a vitamin K antagonist. Test Mnemonic: VITK Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Over night fasting is preferred Specimen Required: Plasma (EDTA) Container Required: Lavender top (EDTA); protect from light and deliver immediately! Volume of Specimen: 5 ml Minimum Volume of Specimen: 2 ml plasma Causes for Rejection: Not light protected, delay in receipt of specimen Availability: Sent out Mon.-Sat. (not holidays) Time Required Routinely for Processing: 1 week Reference Range: See report Zinc, Blood Synonyms: Zn General Use: Zinc toxicity Test Mnemonic: ZI Lab Performing Test: Specimen Processing; sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood (EDTA) Container Required: Navy Blue top with EDTA as preservative; must be spun within 2 hours of collection; Deliver ASAP! Volume of Specimen: 5.0 ml whole blood Minimum Volume of Specimen: 1.0 ml plasma Causes for Rejection: Improper tube type; hemolysis Availability: Sent Monday-Saturday (not holidays) Time Required Routinely for Processing: 3-5 days Reference Range: See report REFERENCES: Quest Diagnostics Test Menu CHEMISTRY The section is directed by Victoria G. Reyes-D'Arcy, M.D. and supervised by Barbara Naillis. Most tests are available on a daily basis Monday through Sunday from 7am to 11 pm. STAT testing, where applicable, is available on a 24 hour basis. For Chemistry services call ext 5144, for Serology services call ext 5119. The Chemistry/Serology supervisor can be reached at ext 3780. Acetaminophen, Blood Synonyms: Tylenol General Use: Acetaminophen toxicity, acetaminophen poisoning Test Mnemonic: TYL Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours, Stat 1 hour Reference Range: Therapeutic range 10-30 ug/ml.; >150 ug/mL is potentially toxic Acetone, Quantitative, Blood Synonyms: Blood ketones General Use: Evaluation of ketonemia Test Mnemonic: ACET Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Do not use alcohol to clean venipuncture site. Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml Serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours, Stat 1 hour Reference Range: Negative Albumin, Blood Synonyms: ALB General Use: Evaluate serum protein, nutritional status, renal and liver function Test Mnemonic: ALB Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours, Stat 1 hour Reference Range: 3.4-5.0 gms/dl Albumin, Fluid Test Mnemonic: FALBU Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Indicate source when ordering Container Required: Sterile glass/plastic tube Volume of Specimen: 1 ml Minimum Volume of Specimen: 0.5ml Causes for Rejection: Viscous or clotted sample Availability: Daily 24 hours daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: Reference ranges not established Alcohol, Blood Synonyms: Blood Ethanol, ETOH General Use: Evaluation of alcohol intoxication Test Mnemonic: ALC Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Do not use alcohol to clean venipuncture site Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Additional information: "Chain of Custody" protocol not followed. Test offered for medical (non-legal) evaluation only. Reference Range: None detected (Legal intoxication > .08 gm/dL) Alcohol, Urine Synonyms: Urine ethanol General Use: Alcohol ingestion Test Mnemonic: UALC Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Urine container, not just lid, must have patient identification Specimen Required: Freshly voided urine Container Required: Clean urine specimen container Volume of Specimen: 30 ml Minimum Volume of Specimen: 10 ml, 30 ml required if confirmation is requested Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours, Stat 1 hour Additional information: "Chain of Custody" protocol not followed; test offered for medical (non-legal) evaluation only. Reference Range: None detected Alkaline Phosphatase, Blood Synonyms: ALP General Use: Liver function; Metabolic bone disorders Test Mnemonic: ALKP Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours, Stat 1 hour Reference Range: 50-136 U/L for Adults Levels in Children are 2-3 times Adult range Alpha feto protein, tumor marker General Use: Useful in the dx and management of germ cell and hepatic carcinomas Test Mnemonic: AFPTM Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis or chylous serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs, Stat 1 hour Reference Range: See report Ammonia, Blood Synonyms: NH3 General Use: Liver function test Test Mnemonic: NH3 Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Vacutainer tube should be placed on ice and brought to laboratory immediately after drawing Specimen Required: Heparinized Blood (Plasma) Container Required: Li Heparin green top vacutainer tube (heparin). Place on ice; deliver to Lab immediately. Volume of Specimen: 4 ml Minimum Volume of Specimen: 1.0 ml plasma Causes for Rejection: Specimen received past 30 minute after collection; specimen not received on ice Availability: daily 24 hrs Time Required Routinely for Processing: 1 hour Reference Range: <32 umol/L Amniotic Fluid L/S Ratio Synonyms: L/S Ratio General Use: Test for fetal maturity Test Mnemonic: LS Test Includes: Lecithin/Sphingomyelin Ratio, fluid creatinine, PG by TLC Lab Performing Test: Chemistry/Serology, sent to Yale Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Amniotic fluid should be placed in a dark container to reduce light effect. Call Chemistry laboratory to schedule test arrangements. Ext 5119 Specimen Required: Amniotic fluid – specimen must be received in lab no later than 10am for same day results! Container Required: Dark brown plastic tube Volume of Specimen: 10 ml Minimum Volume of Specimen: 5 mL Availability: Mon-Sun Time Required Routinely for Processing: 8 hours Additional information: Blood in the specimen may alter the ratio. Bloody taps are questionable. Vaginal pools are not acceptable for L/S ratio testing Reference Range: See Report Amylase, Blood Synonyms: Amy General Use: Pancreatic disease Test Mnemonic: AMYL Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top vacutainer (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1.0 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours, Stat 1 hour Reference Range: 25-115 U/L Amylase, Body Fluids General Use: Pancreatic disease Test Mnemonic: FAMYL Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Specify source when ordering Specimen Required: Fluid (no preservatives) Container Required: Any clean dry container Causes for Rejection: Viscous or clotted sample Volume of Specimen: 1 ml Minimum Volume of Specimen: 0.5 ml Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours. Stat 1 hour Reference Range: Not established Amylase, Urine random General Use: Pancreatic function Test Mnemonic: UAML Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: For 24 hour collections, call the Specimen Processing Lab. Specimen Required: Random urine specimens Container Required: Any clean container (no preservative) Volume of Specimen: 5 mL Minimum Volume of Specimen: 1 mL Availability: 24 hrs daily Time Required Routinely for Processing: 8 hours Reference Range: Not established Anti-Centromere Antibody Synonyms: Anti-Kinetochore Ab General Use: To aid in the diagnosis of patients with CREST syndrome. Also exhibited by one third of patients with Raynaud's disease Test Mnemonic: CENT Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml Causes for Rejection: Gross hemolysis Availability: Mon – Fri 7am – 3pm. Not STAT Time Required Routinely for Processing: 2 days Reference Range: Negative Anti-Gliadin Antibodies, IgA and IgG Test Mnemonic: GLIAB Test Includes: Anti-gliadin antibody IgA and Anti-gliadin antibody IgG Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Mon – Fri 7:00am-3:00pm Time Required Routinely for Processing: 72 hours Reference Range: See Report Arterial Blood Gas Synonyms: Blood Gas, Complete Test Mnemonic: ABG Test Includes: pH, pCO2, HCO3 Lab Performing Test: Respiratory Therapy and Point of Care (Chemistry) Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: On required O2 Special Instructions: Notify lab if on anticoagulants Specimen Required: Arterial Blood Container Required: Heparinized syringe Volume of Specimen: 3 ml Minimum Volume of Specimen: 0.5 ml Availability: 24 hours per day; Stat or routine Time Required Routinely for Processing: 30 minutes Reference Range: See report Arterial pH Synonyms: Blood pH Test Mnemonic: BPH Lab Performing Test: Respiratory Therapy and Point of Care (Chemistry) Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Notify lab if on anticoagulants; Specimen Required: Arterial or venous blood Container Required: Heparinized syringe or green top tube (Heparin) Volume of Specimen: 1 ml Minimum Volume of Specimen: 85uL Availability: Stat: 24 hours per day or routine Time Required Routinely for Processing: 30 minutes Reference Range: Arterial 7.35-7.45 Basic Metabolic Panel General Use: Metabolic Screening Test Mnemonic: BASIC Test Includes: Glucose, BUN, Creatinine with GFR, Calcium, Electrolytes , gap Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Fasting Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Specimen grossly hemolyzed or lipemic Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: See individual test reports Bilirubin, Direct Synonyms: Conjugated bilirubin General Use: Liver function Test Mnemonic: DBIL Lab Performing Test: Chemistry Request Form: : Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: For Neonates Protect from light! Specimen Required: clotted blood (serum) Container Required: 1 pediatric microtainer tube or Red top tube (SST) Minimum Volume of Specimen: 0.1 ml serum for neonates or 1 ml from SST Causes for Rejection: Extreme hemolysis , hemolysis will falsely depress values. Availability: 24 hours daily Time Required Routinely for Processing: Routine: 2 hours; Stat: 1 hour Reference Range: See report Bilirubin, Total (Neonatal) Synonyms: NBIL General Use: Liver function Test Mnemonic: TBIL Test Includes: On newborns (less than 21 days old) If total is >15 mg/dl, a direct bilirubin is performed Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Protect from light Specimen Required: Clotted blood (serum) Container Required: 1 pediatric (microtainer) tube Volume of Specimen: 1 ml Minimum Volume of Specimen: 0.1 ml serum Causes for Rejection: Extreme hemolysis of specimen Availability: 24 hours daily Time Required Routinely for Processing: Routine, 2 hours; Stat, 1 hour Reference Range: See report Bilirubin, Total and Direct, Blood Synonyms: Total and Conjugated Bilirubin; General Use: Liver function Test Mnemonic: BILI Test Includes: Total and direct Bilirubin Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: For Neonates Protect from light! Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml. Minimum Volume of Specimen: 1.0 ml serum Causes for Rejection: Extreme hemolysis of specimen Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: Direct<0.2 mg/dL: Total <1.0 mg/dl Blood Oxygen Saturation Synonyms: Arterial O2 Saturation Test Mnemonic: O2SAT Lab Performing Test: Respiratory Therapy and Point of Care (Chemistry) Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: On required O2 for minimum of 20 minutes Special Instructions: Notify lab if on anticoagulants; specimen must be transported on ice Specimen Required: Arterial blood Container Required: Heparinized syringe Volume of Specimen: 3 ml Minimum Volume of Specimen: 0.5 ml Availability: 24 hours daily Time Required Routinely for Processing: 30 minutes Reference Range: See report BNP Synonym: Brain natriuretic peptide General Use: Aid in the diagnosis of CHF Test Mnemonic: BNP Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top SST tube Volume of Specimen: 10 ml of clotted blood Minimum Volume of Specimen: 1 ml serum Causes for Rejection: gross hemolysis Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours, STAT 1 hour Reference Range: Age dependent; See report C3 Complement Synonyms: C3 General Use: Serum complement evaluation is useful in the diagnosis of several disease states Test Mnemonic: CC3 Lab Performing Test: Chemistry/Serology Request Form: : Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Causes for Rejection: Gross hemolysis, chylous serum Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Reference Range: Age/gender dependent; See report C4 Complement Synonyms: C4 General Use: Serum complement evaluation is useful in the diagnosis of several disease states Test Mnemonic: CC4 Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis; chylous serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Reference Range: Age /gender dependent; See report CA-125 Synonyms: Carbohydrate antigen-125 General Use: Useful for monitoring therapy and confirming biopsy of certain carcinomas Test Mnemonic: CA125 Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis Availability: Mon - Fri 7am-5pm; Sat 7am-3pm Time Required Routinely for Processing: 24 hrs Reference Range: See report Calcium, Blood Synonyms: Ca General Use: Endocrine disorders; metabolic disorders Test Mnemonic: CA Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml. Minimum Volume of Specimen: 1 ml serum Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours, Stat 1 hour Reference Range: 8.5-10.1 mg/dl Calcium, Serum, Ionized Synonyms: Ionized Calcium Test Mnemonic: IONCA Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Special Instructions: Allow specimen to clot at room temperature for 30 minutes. Then spin tube,keep refrigerated and deliver to lab ASAP. Container Required: Red top tube (SST) Volume of Specimen: 10 ml blood Minimum Volume of Specimen: 2 ml Availability: 24 hours daily Additional information: Tube may not be shared with other lab tests Time Required Routinely for Processing: 1 hour Limitations: Total calcium remains the first line test for evaluation of calcium abnormality Reference Range: See report Calcium, Urine Synonyms: Urinary Calcium General Use: Evaluation of calcium metabolism Test Mnemonic: 24 hour collection-UCA24: random specimen-UCA Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: 24 hour urine collection or random specimen Container Required: Yellow top urine tube or Urine cup for random. 24 hr. urine container supplied by Chemistry lab Volume of Specimen: Entire specimen Availability: Daily 7am-11pm for 24 hour collection; 24 hrs daily for random collection Time Required Routinely for Processing: 1 Day for 24 hour collection; Random collection: Routine 8 hrs; Stat 1 hour Reference Range: See Report Carbon Dioxide, Total Synonyms: CO2 General Use: Evaluation of acid - base balance Test Mnemonic: CO2 Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml blood Minimum Volume of Specimen: 1 ml serum Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hrs, Stat 1 hour Reference Range: 21-32 mmol/L Carboxyhemoglobin Synonyms: Blood CO Level Test Mnemonic: COHGB Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Specimen must be transported on ice Specimen Required: Whole blood (heparinized) Container Required: Heparinized syringe, green top tube Volume of Specimen: 3 ml Minimum Volume of Specimen: 85 ul Availability: 24 hrs. daily Time Required Routinely for Processing: 30 minutes Reference Range: Suburban Nonsmoker: <1.5% of tHGB Smokers: 1.5-5.0% of tHGB Heavy Smokers: >5.0-9.0% of tHGB Carcinoembryonic Antigen Synonyms: CEA General Use: For follow up of patients with neoplasm, to evaluate and monitor anti-neoplastic therapy Test Mnemonic: CEA Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Reference Range: See report CCU Profile General Use: Cardiac evaluation for MI Test Mnemonic: CCU Test Includes: CBC, Glucose, Bun, Creatinine with GFR, Electrolytes, gap, Sgot/Ast, Magnesium, Heart (Total CPK and Troponin I) Lab Performing Test: Hematology and Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole Blood (Plasma) and Clotted Blood (Serum) Container Required: Lavender top (EDTA), Red top (SST) and Green top (Li Heparin) Volume of Specimen: 5 ml Whole Blood, 10 ml Clotted Blood Minimum Volume of Specimen: 5 ml Whole Blood and 2 ml Serum Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours, Stat 1 hour Reference Range: See individual test reports Celiac Profile Test Mnemonic: CELIAC Test Includes: Anti-gliadin antibodies, IgA and IgG; total IgA; IgA tTg Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Mon - Fri 7:00AM-3:00PM Time Required Routinely for Processing: 72 hours Reference Range: See Report Childhood Allergy Panel Synonym: Allergy testing General Use: To aid in the diagnosis of atopic allergies Test Mnemonic: CALPAN Test Includes: For a complete listing of the allergens included in the panel, call Serology at 444-5119. Total IgE is included with panel. Lab Performing Test: Chemistry/Serology Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: none Specimen Required: clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 5 ml serum Causes for Rejection: Gross hemolysis Availability: Mon-Fri 7am to 3pm Time Required Routinely for Processing: 48 hrs Reference Range: Interpretation provided with results. Chloride, Blood General Use: Evaluate electrolyte balance Test Mnemonic: CL Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours, Stat 1 hour Reference Range: 98-107 mmol/L Chloride, CSF General Use: CSF chloride may be lowered in tuberculosis Test Mnemonic: CSFCL Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Submit serum sample for chloride determination for proper Interpretation of CSF chloride Specimen Required: Cerebrospinal fluid Container Required: Spinal fluid tube Volume of Specimen: 1.0 ml Minimum Volume of Specimen: 0.5 ml Availability: Stat; 24 hours daily Additional information: Deliver to laboratory immediately! Time Required Routinely for Processing: Routine 8 hours, Stat 1 hour Reference Range: Reference ranges not established. Chloride, Urine Synonyms: CL Urine General Use: Electrolyte balance studies Test Mnemonic: 24 hour collection-UCL24; random specimen-UCL Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Timed or random urine collected by nursing staff Specimen Required: Timed or random urine Container Required: 24 hour urine container supplied by laboratory; Yellow top urine tube or urine cup for random Volume of Specimen: Entire specimen Minimum Volume of Specimen: Entire specimen Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: See Report Cholesterol, Total Synonyms: Serum Cholesterol General Use: Lipid screening Test Mnemonic: CHOL Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: 12-14 hours fasting: should be on stable diet for 3 weeks prior to collection Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Non fasting sample Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: Desirable: <200 mg/dL Borderline High: 200-240 mg/dL High: >or= 240 mg/dL Cholesterol, Fluid Test Mnemonic: FCHOLE Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Indicate source when ordering Container Required: Sterile glass/plastic tube Volume of Specimen: 1 ml Minimum Volume of Specimen: 0.5 ml Causes for Rejection: Viscous or clotted sample Availability: 24 hrs. daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Reference Range: Reference ranges not established Cholesterol Fractionation Synonyms: CHOF General Use: Cholesterol screening Test Mnemonic: LIPFRA Test Includes: Total Cholesterol, Triglylcerides, HDL and calculated LDL Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: 12 - 14 hours fasting: Should be on stable diet for 3 weeks prior to test Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Non fasting sample Availability: 24 hrs. daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: See individual reports CKMB (Creatine Kinase, MB Fraction) Synonyms: MMB, CPK2 General Use: To document myocardial infarction Test Mnemonic: CKMB Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml Availability: 24 hrs Daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hr Reference Range: <3.5 ng/mL Comprehensive Inhalant Panel Synonyms: Allergy testing General Use: To aid in diagnosis of atopic allergies Test Mnemonic: CIP Test Includes: Screening for most common trees, grasses, weeds, mold and animal allergens. Total IgE is included with panel. Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 4 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: Mon-Fri 7AM to 3PM Time Required Routinely for Processing: 48 hours Additional information: A complete listing of the allergens included is available from the lab. Call 444-5119 Reference Range: Interpretation provided with results Comprehensive Metabolic Panel Synonyms: Chem panel General Use: Metabolic Screening Test Mnemonic: COMP Test Includes: Glucose, BUN, Creatinine with GFR, Calcium, Total Protein, Albumin,Globulin, Total Bilirubin Alkaline Phosphatase, SGOT, SGPT, Electrolytes ,gap Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Fasting for optimum results Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml blood Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Specimen grossly hemolyzed or grossly lipemic Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours, Stat 1 hour Reference Range: See individual test reports Cortisol General Use: Diagnosis of adrenocortical insufficiency (Addison's disease) and adrenocortical hypersecretion (Cushing's disease) Test Mnemonic: CORT Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: Mon - Fri 7AM-5PM; Sat 7AM-3PM Time Required Routinely for Processing: 24 hrs Reference Range: Before 10am 4.5-22.7 ug/dL After 5pm 1.7-14.1 ug/dL CPK Synonyms: Creatine Kinase General Use: Cardiac damage, muscle disease, brain damage, acute pulmonary diseases Test Mnemonic: CK Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours, Stat 1 hour Reference Range: Females: 26-192 U/L Males: 39-308 U/L C-Reactive Protein Synonym: CRP General Use: CRP has been detected in the serum or patients with inflammation or necrosis. Test Mnemonic: CRP Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: None Special Instructions: None Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume Required: 1 ml serum Causes for Rejection: Gross hemolysis or chylous serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Additional information: None Reference Range: <0.30 mg/dL C-Reactive Protein, Cardiac Synonym: High sensitivity CRP General Use: Evalution for risk of heart disease Test Mnemonic: HSCRP Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: None Special Instructions: None Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume Required: 1 ml serum Causes for Rejection: Gross hemolysis or chylous serum Availability: 24 hrs daily. Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Reference Range: See patient report Creatinine, Blood General Use: Kidney function Test Mnemonic: CRETP Test Includes: GFR calculation Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: 0.6 – 1.3 mg/dL Creatinine Clearance Synonyms: 24 hr creatinine clearance General Use: Renal function Test Mnemonic: CCLR Test Includes: Serum creatinine, Urine creatinine Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: For best results, no meat, tea, coffee or drugs should be consumed on day of test Special Instructions: Blood creatinine must be drawn within 72 hr of urine collection. Urine container must have collection times on it. ( keep refrigerated during collection) Specimen Required: 24 hr urine collection and 10 ml clotted blood (serum) Container Required: 24 hour urine container obtained from Chemistry and red top tube (SST) Volume of Specimen: Entire timed urine collection and 3 ml serum Minimum Volume of Specimen: Entire collection Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour. Reference Range: See Report Creatinine, 24 hour Timed or Random Urine Test Mnemonic: 24 hr collection - UCR24; random specimen UCREAT General Use: Kidney function Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Observe usual 24 hr urine collection instructions (keep refrigerated during collection) Specimen Required: Random or timed 24 hour urine collection Container Required: 24 urine container obtained from Chemistry. Urine cup or yellow top urine tube for random collection Volume of Specimen: Entire collection for 24 hr and 10 ml for random Minimum Volume of Specimen: Entire specimen for 24 hr and 1 ml for random Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: See Report Digoxin, Blood Synonyms: Lanoxin General Use: Diagnosis of digoxin toxicity Test Mnemonic: DIG Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Specimen should be collected at least 6 hrs after the last oral dose. Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml blood Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs. daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: Therapeutic range : 0.8-2.0 ng/mL Dilantin, Blood Synonyms: Phenytoin General Use: Monitor therapeutic drug levels Test Mnemonic: DILA Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: Therapeutic: 10-20 ug/mL; > 30 ug/mL is potentially toxic Drugs of Abuse, Urine Synonyms: UDS General Use: Drugs of abuse toxicity; drug poisoning Test Mnemonic: DA Test Includes: Urine: Amphetamines, Barbiturates, Benzodiazepines, THC, Cocaine, Opiates and Methadone Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Fresh voided urine Container Required: Clean urine specimen container or yellow top urine tube, urine container and lid must have patient identification Volume of Specimen: 30 mls Minimum Volume of Specimen: 10 mls; 30 mls urine required if confirmation is requested Availability: Daily 24 hrs Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Additional information: 'Chain of Custody' protocol not followed; screen offered for medical (non-legal) purposes only: Confirmation of positive results available by request, call ext 5144 Reference Range: Negative Electrolytes, Blood General Use: Electrolyte balance Test Mnemonic: LYTES Test Includes: Na, K, CI, CO2 and anion gap Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Extreme hemolysis Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: See individual test reports Electrolytes, Urine Synonyms: Lytes, Urine General Use: Renal function Test Includes: Random Urine Sodium, Potassium and Chloride Test Mnemonic: ULYTES Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Random urine collection Specimen Required: Random urine Container Required: Yellow top urine tube or random urine cup Volume of Specimen: 10 ml urine Minimum Volume of Specimen: 1 ml for random Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: See Report Estradiol Synonyms: E2 General Use: Assessment of hypothalamus, pituitary, and ovarian function Test Mnemonic: ESTRA Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Mon - Fri 7AM-5PM. Sat 7am-3pm. May be ordered STAT Time Required Routinely for Processing: 24 hrs Reference Range: See report Ferritin, serum General Use: Screening for iron deficiency anemia Test Mnemonic: FERR Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: None Specimen Required: Clotted Blood (Serum). Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: Mon-Fri 7AM-5PM; Sat 7AM-3PM Time Required Routinely for Processing: 24 hrs Reference Range: See Report Folate, serum Synonyms: Folic Acid (Serum) General Use: Diagnosis of folate deficiency; monitoring folate therapy Test Mnemonic: FOL Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient should be fasting overnight Specimen Required: Clotted Blood (Serum). Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Grossly hemolyzed specimen Availability: Mon-Fri 7AM-5PM; Sat 7AM-3PM Time Required Routinely for Processing: 24 hrs Reference Range: >2.7 ng/mL Follicle Stimulating Hormone Synonyms: FSH General Use: Assessment of pituitary function and to distinguish primary from secondary gonadal failure Test Mnemonic: FSH Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: Mon-Fri 7AM-5PM; Sat 7AM-3PM Time Required Routinely for Processing: 24 hours Reference Range: FSH ranges vary with age and phase of menstrual cycle. Ranges are provided with results. Free and Total Prostate Specific Antigen Synonyms: Free and Total PSA General Use: To aid in the diagnosis and monitoring of Prostatic Ca and BPH Test Mnemonic: FRTPSA Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container required: Red top tube (SST) Volume of Specimen: 10ml Minimum Volume of Specimen: 1ml Causes for Rejection: Gross hemolysis or chylous serum Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours; STAT 1 hour Reference Range: See Report General Food Screen Synonyms: Allergy testing General Use: To aid in diagnosis of atopic allergies Test Mnemonic: GFS Test Includes: Allergy screening for milk, eggs, wheat, peanut, soybean and corn. Total IgE is included with panel. Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: Mon-Fri 7AM to 3PM Time Required Routinely for Processing: 48 hours Reference Range: Interpretation provided with test results GGT Synonyms: SGGT, GGTP General Use: Liver function test which parallels liver alkaline phosphatase Test Mnemonic: GGT Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: Males: 15-85 U/L; Females: 5-55 U/L Gentamicin Synonyms: Garamycin General Use: Monitor therapeutic level Test Mnemonic: Trough: GENT; peak: GENP; random: GENR Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Peak level: draw specimen 30 minutes after end of 30 minute I.V. infusion; Trough level: draw immediately prior to next dose Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 mL serum Availability: Daily 24 hrs Time Required Routinely for Processing: 2 hours Additional information: Specimens should be drawn at steady state, usually after fifth dose, if drug given every 8 hours, or after third dose, if given every 12 hours; Gentamicin has significant nephrotoxicity and ototoxicity Limitations: Toxic levels may be reflective of, rather than predictive of, renal damage. Reference Range: Therapeutic Peak: 4-8 ug/ml, Trough: 0.0-2.0 ug/ml. Glucose, Blood Synonyms: Fasting blood sugar, Non-fasting blood sugar General Use: Diabetes mellitus; Carbohydrate metabolism disorders Test Mnemonic: Fasting: FBS; Non-fasting (Casual): GLUCR Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: FBS - Patient should fast overnight 8-12 hours; NPO after 11pm. Special Instructions: Non-fasting glucose – If order is for "post-prandial" testing instruct patient to eat a meal 1 hr. prior to collection. Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: See Report Glucose, Fluid Test Mnemonic: FGLU Test Includes: Fluid glucose Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Specify source when ordering Specimen Required: Body fluid, specify source Container Required: Sterile glass/plastic tube Volume of Specimen: 2 ml Minimum Volume of Specimen: 1 ml Causes for Rejection: Viscous or clotted specimen Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: Reference ranges not established Glucose, OB screen General Use: For OB patients who do not show diagnostic elevations of fasting or casual glucose Test Mnemonic: GOBS Test Includes: Single blood sample for glucose drawn one hour after 50gm oral dose of glucose Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: This test does not require fasting Specimen Required: Clotted blood (serum) Container Required: Red Top Tube (SST) Volume of Specimen: 10 ml. Minimum Volume of Specimen: 1 ml. serum Cause for Rejection: Grossly hemolyzed blood Availability: Daily Time Required Routinely for Processing: Routine 8 hrs. Reference Range: See report Glucose, Spinal Fluid Synonyms: CSF Glucose General Use: Diagnosis of central nervous system disorders Test Mnemonic: CSFG Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Physicians responsibility Special Instructions: Specimen brought to laboratory immediately by nursing staff. Specimen Required: Spinal fluid Container Required: Clean test tube Volume of Specimen: 1 ml. Minimum Volume of Specimen: 0.3 ml Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Additional information: Suggest simultaneous blood glucose Reference Range: 40-70 mg/dL Glucose Tolerance OB Patients Synonyms: GTOB General Use: Diagnosis of Gestational Diabetes Test Mnemonic: GTOB Test Includes: Fasting, 1 hr, 2 hr, 3 hr glucose Lab Performing Test: Chemistry (Call for instructions) Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient must fast for Minimum 8 hrs - not longer than 14 hrs. Fasting is drawn then a 100gm dose oral glucose is given Special Instructions: Overnight fast. NPO until test completed Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum each timed collection Availability: Daily 7AM-llPM Time Required Routinely for Processing: 8 hours Reference Range: See Report Glucose Tolerance Test 2 Hours Synonyms: GTT General Use: Diabetes Test Mnemonic: 2 hr: GTT2 Test Includes: Glucose determination at fasting and 2 hours. Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient must fast at least 8 hrs and not more than 14 hrs. NPO until test is completed. Fasting is drawn then patient is given a 75 gm dose of oral glucose. Blood specimen is drawn at 2 hours. Specimen Required: Clotted blood (Serum) Container Required: Red top (SST) for each timed collection and FBS Volume of Specimen: 10 ml. Minimum Volume of Specimen: 1 ml serum each collection Availability: Daily Time Required Routinely for Processing: 8 hours Additional information: The standard test is 2 hrs with a 75gm oral glucose dose. Reference Range: See report Glycosylated Hemoglobin Synonyms: Hemoglobin A1c, General Use: To aid in the management of diabetic patients Test Mnemonic: A1C Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood (EDTA) Container Required: Lavender top tube (may be shared with CBC tube) Volume of Specimen: 5 ml blood Minimum Volume of Specimen: 2 ml whole blood Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Contraindications: Not useful more often than at 4-6 week intervals. Not indicated for diagnosis of diabetes. Additional information: Chronic blood loss, hemolytic anemia, or other setting for decrease in RBC life span, results in a decrease in the glycosylated hemoglobin level. Reference Range: 4.2-6.3% Diabetics out of control: greater than 12% HCG, male Synonyms: Human chorionic gonadotropin General Use: This marker may be useful in diagnosis, therapy and prognosis of testicular embryonal carcinoma Test Mnemonic: HCG Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Reference Range: <2.0 mIU/mL HCG, Quantitative, Beta Subunit Synonyms: Quantitative Bhcg General Use: Diagnosis of certain cancers such as choriocarcinoma and certain embryonal cell carcinomas as well as the detection of ectopic pregnancy Test Mnemonic: BHCG Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Not done on urine. Gross hemolysis Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: Reference ranges for normal gestational weeks are provided with test result Heart Profile Synonyms: MI Profile General Use: Cardiac evaluation for MI Test Mnemonic: HEART Test Includes: Total CPK and Troponin I Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen:10 ml Minimum Volume of Specimen: 1 ml serum Availability: Daily 24 hrs Time Required Routinely for Processing: Routine 8 hours; 1 hour Stat Reference Range: See individual reports Hemoglobin, Total Synonyms: tHb Test Mnemonic: THGB Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Notify lab if on anticoagulants Specimen Required: Whole Blood (heparinized) Container Required: Heparinized syringe, green top tube Volume of Specimen: 3 ml Minimum Volume of Specimen: 85 uL Availability: Stat 24 hours per day Time Required Routinely for Processing: 30 minutes Reference Range: See report Hepatitis A Antibody (IgM) General Use: Presence of Hepatitis A Antibody (lgM) indicates recent acute phase infection with Hepatitis A virus Test Mnemonic: HAVABM Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis Availability: Mon – Fri 7:00AM – 5:00PM, Sat 7:00am – 3:00 pm Time Required Routinely for Processing: 24 hrs Additional information: May be ordered as part of Hepatitis Panel (HEPP) Reference Range: Reported as Positive or Negative Hepatitis B Core Antibody (IgM) Synonyms: HBc Ab General Use: This marker is an early indicator of acute infection with Hepatitis B virus Test Mnemonic: HBCIGM Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red Top Tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml Causes for Rejection: Gross hemolysis, chylous serum Availability: Mon – Fri 7:00AM – 5:00PM; Sat 7:00AM – 3:00PM Time Required Routinely for Processing: 24 hours Additional information: May be ordered as part of Hepatitis Panel (HEPP) Reference Range: Reported as positive or negative Hepatitis B Surface Antibody Synonyms: Hepatitis Bs Ab, HBs Ab General Use: Screening test for past infection and subsequent immunity to Hepatitis B Virus Test Mnemonic: HBSAB Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red Top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml Causes for Rejection: Excessive hemolysis, chylous serum Availability: Mon – Fri 7:00AM – 5:00PM; Sat 7AM – 3PM Time Required Routinely for Processing: 24 hours Reference Range: Reported as Positive or Negative Hepatitis B Surface Antigen Synonyms: HBsAg General Use: Presence of HBsAg antigen indicates present infection with Hepatitis B virus or chronic carrier state Test Mnemonic: HBSAG Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis Availability: Mon – Fri 7:00AM – 5:00PM; Sat 7AM-3PM; STAT upon request Time Required Routinely for Processing: 24 hrs Additional information: May be ordered as part of Hepatitis Panel (HEPP) Reference Range: Negative Hepatitis C Virus Antibody General Use: Used to aid in the diagnosis of Hepatitis C infection Test Mnemonic: HEPC Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: Mon – Fri 7:00AM – 5:00PM; Sat 7AM-3PM Time Required Routinely for Processing: 24 hrs Additional information: May be ordered as part of Hepatitis Panel (HEPP) Reference Range: Negative Hepatitis Panel General Use: Screening for infection with Hepatitis A, Hepatitis B, or Hepatitis C virus Test Mnemonic: HEPP Test Includes: HbsAg, HbcAb (IgM), Hepatitis A Antibody (IgM), Hepatitis C Virus Ab. Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red Top Tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 3 ml serum Causes for Rejection: Gross hemolysis Availability: Mon – Fri 7:00AM – 5:00PM; Sat 7AM-3PM Time Required Routinely for Processing: 24 hrs Reference Range: Individual tests reported as positive or negative HIV-1 Antibody Synonyms: Human lmmunodeficiency Virus, AIDS test General Use: Used to support a diagnosis of AIDS or AIDS related complex Test Mnemonic: HIV Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis Availability: Mon – Fri 7:00am-5:00pm; Sat 7:00am-3:00pm, Stat available upon request Time Required Routinely for Processing: Stat 2 hrs/Routine 24 hrs. If positive, the Western Blot test is done for confirmation Additional information: This test is designed to help detect infection by or exposure to the virus which as been implicated as the cause of Acquired Immunodeficiency Syndrome (AIDS) Reference Range: Negative Homocysteine General Use: Elevated levels of homocysteine are observed in patients at risk for coronary heart disease and stroke. Test Mnemonic: HCYS Lab Performing Test: Chemistry Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Fasting for at least 8 hours is preferred Special Instructions: Put specimen on ice immediately after collection. Centrifuge within 1 hour. Keep refrigerated. Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Specimen received at room temperature Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 2 hrs Reference Range: See Report IgE Synonyms: Immunoglobulin E General Use: Management of patients with atopic disease such as asthma, hay fever, eczema, and in patients with respiratory allergies Test Mnemonic: IGE Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis. chylous serum Availability: Mon – Fri 7am-3pm Time Required Routinely for Processing: 48 hrs Reference Range: See report Immunoglobulin Panel General Use: To evaluate humoral immunity or monitor therapy in myeloma patients. Maybe of diagnostic importance in infections and autoimmune diseases Test Mnemonic: IMMGS Test Includes: IgG, IgA and IgM Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis or chylous serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs: Stat 1 hour Reference Range: Reference ranges are age dependent - see report Infectious Mononucleosis Test Synonyms: Monospot Test General Use: For the detection of heterophile antibodies related to infectious mononucleosis Test Mnemonic: MONOS Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hours a day, Mon-Sun.; Stat and routine Time Required Routinely for Processing: Routine 8 hrs; STAT 1 hr Reference Range: Negative Insulin Glucose Tolerance, 2 or 3 Hours Synonyms: IGT General Use: Insulin to Glucose levels have prognostic value in predicting the benefits of insulin therapy and likelihood of progression to insulin-dependence Test Mnemonic: IGT2: 2 hour; IGT3: 3 hour Test Includes: Insulin and Glucose determinations at fasting at 1/2 hour and for each hour of the tolerance ordered Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Overnight fasting. NPO until test is completed Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) for each timed collection and FBS Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum each timed collection Availability: Mon.- Fri 7:00am – 11:00pm;Sat. 7AM-3PM Time Required Routinely for Processing: 8 hrs. Reference Range: See report Insulin, Random General Use: Hypoglycemia, pancreatic function, insulin resistance Test Mnemonic: INS Lab Performing Test: Chemistry; Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Mon –Fri 7:00am-5:00pm; Sat 7AM-3PM Time Required Routinely for Processing: 1 day Reference Range: See report Iron Profile General Use: Evaluation of iron metabolism; differential diagnosis of anemia Test Mnemonic: IRON Test Includes: Serum iron, Total iron binding capacity and % Transferrin Saturation Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Additional information: Indicate whether or not patient is receiving Iron therapy Reference Range: See individual test reports Lactic Acid, Blood Synonyms: Lactate General Use: Evaluate lactic acidosis; metabolic acidosis Test Mnemonic: LACT Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient should be fasting and at rest. Special Instructions: Specimen must be delivered on ice to laboratory immediately after collection. Specimen Required: Whole venous blood Container Required: Gray top tube, place tube on ice! Volume of Specimen: 7 ml Minimum Volume of Specimen: 3 ml Causes for Rejection: Specimen not kept on ice or delay in transport to Lab Availability: 24 hrs daily Time Required Routinely for Processing: Stat - 1 hour Reference Range: 0.4-2.0 mmol/L. Lactic Acid, CSF Synonyms: CSF Lactate General Use: Diagnosis of disorders of the central nervous system Test Mnemonic: CSFLA Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Spinal fluid Container Required: Sterile glass/plastic tube Volume of Specimen: 1.0 ml Minimum Volume of Specimen: 0.5 ml Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours, Stat 1 hour Reference Range: 0.6-2.2 mmol/L Lactic Dehydrogenase, Blood Synonyms: LDH General Use: Cardiac and liver disorder; certain tumors Test Mnemonic: LDH Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml. Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Reference Range: 87-241 U/L Lactic Dehydrogenas, Fluid General Use: Evaluation of hemolytic states Test Mnemonic: FLLDH Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Indicate source when ordering Container Required: Sterile glass/plastic tube Volume of Specimen: 1 ml Minimum Volume of Specimen: 0.5 ml Causes for Rejection: Viscous or clotted specimen Availability: 24 Hrs daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hr Reference Range: Reference range not established Lactose Tolerance Test Synonyms: Lactose consumption test General Use: Lactose intolerance evaluation. Test Mnemonic: LTOL Test Includes: Fasting, 15 min., 30 min., 60 min., and 90 min. lactose Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: NPO after midnight preceding day of test. Special Instructions: A fasting specimen must be drawn before lactose is given to patient. Coordinate lactose administration and specimen collection with Phlebotomy team. Specimens drawn 15, 30, 60 and 90 minutes post Lactose Dose. Specimen Required: Whole venous blood Container Required: Gray top tube Volume of Specimen: 7 ml Minimum Volume of Specimen: 7 ml Availability: Monday-Friday, 7AM to 3PM. Not Stat Time Required Routinely for Processing: 8 hours Additional information: Lactose is obtained from pharmacy by nursing for inpatients; by laboratory for outpatients Reference Range: Interpretation: An increase of blood glucose >20 mg/dL over the fasting level on any of the timed specimens is considered normal (based on a 50gm lactose date) Latex Allergen Synonym: Allergy testing/K82 General Use: To aid in the diagnosis of atopic allergies Test Mnemonic: K82 Test Includes: Allergy screening for latex. Lab Performing Test: Chemistry/Serology Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: none Special Instructions: none Specimen Required: clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis Availability: Mon-Fri 7am to 3pm Time Required Routinely for Processing: 48 hrs Reference Range: Interpretation provided with results. LDL cholesterol Synonyms: LDL, direct General Use: Determination of potential risk for heart disease Test Mnemonic: LDLD Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml. Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours Reference Range: See Report Lipase, Serum Synonyms: Lipase General Use: Pancreatic function Test Mnemonic: LIPS Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: 73-393 u/L Lithium, Blood Synonyms: Li General Use: Therapeutic Drug monitoring Test Mnemonic: LI Lab Performing Test: Chemistry lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours: Stat 1 hour Reference Range: Therapeutic range 0.6-1.2 mmol/L Liver Profile Synonyms: Liver function tests Test Mnemonic: LIV Test Includes: TPRO, TBlL, DBIL, ALKP, ALT, AST,ALB and globulin Lab Performing Test: Chemistry lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Daily 24 hrs Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: See individual test reference ranges Luteinizing Hormone General Use: Assessment of hypothalamic function and pituitary function; to distinguish between primary and secondary gonadal failure Test Mnemonic: LH Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Excessive hemolysis, chylous serum Availability: Mon-Fri 7AM to 5PM; Sat 7AM to 3PM. Time Required Routinely for Processing: 24 hours Reference Range: See report. Ranges are sex and cycle dependent Lyme Disease Serology, Serum Synonyms: Lyme Arthritis Antibodies General Use: To aid in the diagnosis of Lyme disease Test Mnemonic: LYME Test Includes: Lyme Abs IgG and IgM Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Excessive hemolysis Availability: Mon-Fri 7am to 5pm; Sat 7am -3pm Time Required Routinely for Processing: 24 hrs Limitations: Positive or borderline results will be referenced out for Western blot testing Reference Range: Negative Magnesium, Blood Synonyms: Mg General Use: Evaluation of metabolic disorders Test Mnemonic: MG Lab Performing Test: Chemistry Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Rourine 8 hrs; stat 1 hour Reference Range: 1.8 - 2.4 mg/dL Measles Immunity Panel General Use: To determine immunity to Rubella and Rubeola (measles virus) Test Mnemonic: MIMP Test Includes: Rubella immune status, Rubeola immune status Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Mon – Fri 7am-5pm; Sat 7am-3pm Time Required Routinely for Processing: 2-3 days Reference Range: Reported as immune or non-immune Methemoglobin General Use: Evaluation of cyanosis or methemoglobinemia due to drugs or chemicals Test Mnemonic: METHGB Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood (heparinized) * Must be transported on ice Container Required: Heparinized syringe or Green top tube (Na Heparin) Volume of Specimen: 3 ml Minimum Volume of Specimen: 85 uL Causes for Rejection: Specimen not on ice when received Availability: 24 hrs. daily Time Required Routinely for Processing: 1 hour Reference Range: See report Microalbumin, Urine Synonyms: Urinary Albumin General Use: Evaluation of renal function. Diagnosis of diabetic nephropathy Test Mnemonic: Random specimen: UMCALM; 24 hr collection; UMCA24 Test Includes: Microalbumin and urine creatinine Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: 24 hr collection or random urine Container Required: 24 hr urine container obtained from chemistry; yellow top urine tube or random urine cup Volume of Specimen: Entire collection for 24 hour/10 ml for random Minimum Volume of Specimen: Entire collection for 24 hour/2 ml for random Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hrs: Stat 1 hour Reference Range: See Report New England Regional Inhalant Panel Synonyms: Allergy Testing General Use: To aid in the diagnosis of atopic allergies Test Mnemonic: RIPNE Test Includes: Screening test for Northeast regional trees, grasses, molds and animal allergens. Total IgE is included with panel. Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 5 ml serum Availability: Mon-Fri 7AM to 3PM Time Required Routinely for Processing: 48 hrs Additional information: A complete listing of the allergens included is available from the lab. Call 444-5119 Reference Range: Interpretation provided with test results Nut Panel Synonym: Allergy testing General Use: To aid in the diagnosis of atopic allergies Test Mnemonic: NUTP Test Includes: Allergy screening for peanut, hazelnut, brazil nut, almond, pecan, pistachio, cashew and walnut. Total IgE is included with panel. Lab Performing Test: Chemistry/Serology Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: none Specimen Required: clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 5 ml serum Causes for Rejection: Gross hemolysis Availability: Mon-Fri 7am to 3pm Time Required Routinely for Processing: 48 hrs Reference Range: Interpretation provided with results. Osmolality, Serum Synonyms: Serum Osmolality General Use: Dehydration, electrolyte balance Test Mnemonic: OSMO Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 0.5 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: 275-295 mOsm/Kg Osmolality, Urine Test Mnemonic: UOSM Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Random urine Container Required: Yellow top urine tube or urine container routinely used for random collection Volume of Specimen: 5 ml Minimum Volume of Specimen: 0.5 ml Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: 450-750 mOsm/Kg PG - FLM Test Synonyms: Phosphotidyglycerol Slide Test General Use: Fetal lung maturity determination Test Mnemonic: PGFLM Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Amniotic fluid from amniocentesis or vaginal pool Container Required: Dark brown sterile plastic tube Volume of Specimen: 2 ml Minimum Volume of Specimen: 1 ml amniotic fluid Availability: Mon-Fri 7AM to 11PM; Sat 7AM to 3PM; STAT upon request, Call lab 444-5119 Time Required Routinely for Processing: 1 hour Reference Range: Positive indicates maturity pH, Body Fluid Test Mnemonic: FPHP General Use: Determine pH of clinical specimen. Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Indicate source when ordering Specimen Required: Body fluid (urine, gastric, thoracentesis, etc.) Container Required: Sterile glass/plastic tube Volume of Specimen: 2 ml Minimum Volume of Specimen: 1 ml Causes for Rejection: Viscous or clotted specimen Availability: Daily 7AM-11PM Time Required Routinely for Processing: 8 hours Reference Range: Reference range not established Phenobarbital, Blood Synonyms: Phenobarb level General Use: Monitor therapeutic drug level Test Mnemonic: PHEN Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Additional information: Optimal sampling time after dosage is 2-8 hrs. Reference Range: Therapeutic level: 15-40 ug/mL; Toxic level: > 50 ug/mL Phosphate, Urine Synonyms: Urinary Phosphorus General Use: Electrolyte disorders; renal function test Test Mnemonic: Random specimen: UPHOS; 24 hr collection: UPHS24 Test Includes: Phosphorus on random or timed urine specimen Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Urine specimen obtained by nursing staff for Inpatients Specimen Required: Timed or random urine Container Required: 24 hour urine container supplied by laboratory; Yellow top urine tube or urine cup for random testing Volume of Specimen: Entire specimen for 24 hr collection/ 10 ml for random Minimum Volume of Specimen: Entire specimen for 24 hour/1 ml for random Availability: Daily 7AM-11PM Time Required Routinely for Processing: 1 Day Reference Range: 24 hr specimens: 0.3-1.0 g/TV (dependent on dietary intake) Random: Ranges not established, dependent on diurnal variation Phosphorus, Blood Synonyms: P04 General Use: Evaluation of phosphorus metabolism Test Mnemonic: PHOS Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml. Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: 2.5-4.9 mg/dL Potassium, Blood Synonyms: K General Use: Evaluate electrolyte balance Test Mnemonic: K Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml blood Minimum Volume of Specimen: 0.5 ml serum Causes for Rejection: Moderate to gross hemolysis; drawn from an IV infused vein Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: 3.5-5.1 mmol/L Potassium, Urine Synonyms: K, Urine General Use: Renal function Test Mnemonic: 24hr: UK24; Random Urine: UK Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Random or 24 hr urine collection Specimen Required: Random or timed urine (24hr) Container Required: routine urine container or yellow top urine tube; 24 hour urine container obtained from Chemistry Volume of Specimen: Entire collection or 1 ml for random Minimum Volume of Specimen: Entire timed collection Availability: Daily, 7AM-11PM Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: 24 hr specimens: 25-100 mEq/24 hr Random: 30-90 mEq/L (Varies with diet) Prealbumin Synonyms: Transthyretin, Thyroxine-binding prealbumin General Use: Screening for protein-calorie malnutrition and to monitor the effectiveness of nutritional support therapy Test Mnemonic: PAB Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs: Stat 1 hour Reference Range: 20-40 mg/dL Pregnancy Test, Serum Synonyms: Bhcg, Qualitative General Use: Screening test for pregnancy Test Mnemonic: PREGS Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis Availability: 24 hours a day, Mon-Sun. STAT and routine Time Required Routinely for Processing: Routine 8 hours; STAT 1 hour Reference Range: Non-pregnant females: Negative Normal pregnant female: Positive Pregnancy Test, Urine General Use: Screening test for pregnancy Test Mnemonic: UPREG Lab Performing Test: Serology/Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Urine specimen, preferably first morning void Container Required: Clean sterile urine cup or yellow top urine tube Volume of Specimen: 2 ml Minimum Volume of Specimen: 1 ml urine Availability: 24 hrs a day, Mon-Sun. STAT and routine Time Required Routinely for Processing: Routine 8 hours; STAT 1 hour Reference Range: Non-pregnant females: Negative Normal pregnant female: Positive Prenatal Profile General Use: Prenatal screening Test Mnemonic: PRENAT 1 Test Includes: BsAg, Syphab, Rubella, CBC, Ab Screen, ABO/Rh,A1C and HIV Lab Performing Test: Chemistry, Hematology, Blood Bank Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Must be ordered as order set Specimen Required: Clotted blood and whole blood (EDTA) Container Required: Red top tube(SST), Lavendar (EDTA) and K2EDTA Pink Top Volume of Specimen: 10 ml clotted Blood, 4 ml Lavender EDTA and 6 ml K2EDTA Minimum Volume of Specimen: 3 ml Serum, 3 ml Lavender EDTA Blood and 2 ml K2EDTA Blood Availability: 7AM-11PM; Mon-Sun. Not stat Time Required Routinely for Processing: 1-4 days Reference Range: See individual tests for reference ranges Procalcitonin General Use: To aid in the work-up of infectious causes of sepsis. Test Mnemonic: PROCAL Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis Availability: 24 Hrs daily Time Required Routinely for Processing: 1 Hour Reference Range: See text report Progesterone General Use: As an indicator of natural or induced ovulation or in the diagnosis of threatened abortion Test Mnemonic: PROG Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis or chylous serum Availability: Mon - Fri 7AM-5PM; Sat 7am-3pm May be ordered STAT Reference Range: Ranges vary according to sex and cycle of female – See test report. Prolactin General Use: Pituitary function test useful in the detection of prolactin secreting pituitary tumors with or without galactorrhea and in the assessment of pituitary dysfunction Test Mnemonic: PROL Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Excessive hemolysis, chylous serum Availability: Mon-Fri 7AM-5PM; Sat 7AM-3PM Time Required Routinely for Processing: 24 hours Reference Range: see report Prostate Specific Antigen Synonyms: PSA General Use: To aid in the diagnosis and monitoring of Prostatic Ca and BPH Test Mnemonic: PSA Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis or chylous serum Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours; STAT 1 hour Reference Range: <4.0 ng/ml Protein, Body Fluid General Use: Evaluating pathological processes Test Mnemonic: FTOTP Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Body fluid (i.e. ascites fluid, pleural fluid, etc.) Container Required: Clean glass or plastic tube Volume of Specimen: 3 ml Minimum Volume of Specimen: 1 ml Causes for Rejection: Viscous or clotted specimen Availability: 24 Hrs daily Time Required Routinely for Processing: 8 hours Additional information: Identify source of body fluid in comment field Reference Range: Reference ranges not established Protein, CSF General Use: Diagnosis of CSF pathological processes Test Mnemonic: CSFTP Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Physician's responsibility Special Instructions: Specimen must be brought to laboratory Stat Specimen Required: Cerebrospinal fluid Container Required: Any sterile container Volume of Specimen: 1 ml Minimum Volume of Specimen: 0.5 ml Availability: 24 hrs daily Time Required Routinely for Processing: Routine 2 hours; Stat 1 hour Additional information: Fresh blood in the specimen will invalidate the result; xanthochromia or hemolysis may falsely depress results Reference Range: 15-45 mg/dL Protein, Total, Blood Synonyms: TP General Use: Evaluate serum proteins, nutritional status, liver and renal function Test Mnemonic: TPP Test Includes: Total Protein, Albumin, Globulin Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: See individual tests Protein, Urine General Use: Detection of proteinuria Test Mnemonic: Random: UTP and 24 hr: UTP24 Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: 24 hr: instruct the patient to void at 8:00 AM and discard the specimen. Then collect all urine including the final specimen voided at the end of the 24 hour collection period. Specimen Required: Timed or random urine Container Required: Random urine container or yellow top urine tube/ 24 hour urine container obtained from chemistry Volume of Specimen: 24 hr collection: entire specimen; random collection 10 ml Minimum Volume of Specimen: 24 hr collection : entire specimen: random collection : 1 ml Availability: Daily, 7AM-11PM Time Required Routinely for Processing: 24 hours Additional information: Exact hours of specimen collection should be recorded on label supplied with bottle. 24-hour collections are preferable for evaluation of nephrotic states and inflammatory renal disorders Reference Range: 24 hr specimens: 0-0.15 gm/TV Random: 0-14 mg/dL PTH, intact panel Synonym: Intact parathyroid hormone General Use: Aid in the differentiation of hyperparathyroidism from nonparathyroid hypercalcemia Test Mnemonic: PTHP Test Includes: PTH, intact and Calcium Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) and whole blood (plasma) Container Required: Red top (SST) and Lavender top (EDTA) Volume of Specimen: 10 ml clotted blood and 5 ml whole blood Minimum Volume of Specimen: 1 ml serum and 1 ml plasma Causes for Rejection: Improper container, gross hemolysis Availability: Monday – Friday 7 am to 5 pm; Sat 7am-3pm. STAT upon request Time Required Routinely for Processing: Routine 8 hours, STAT 1 hour Reference Range: See report for interpretation RAST testing – miscellaneous tests Synonym: Allergy testing General Use: To aid in the diagnosis of atopic allergies Test Mnemonic: Order as misc test Available misc tests: Tomato, orange, tuna, salmon, apple, casein, kiwi, banana, fusarium proliferatum, cow’s whey, mountain cedar, elm, walnut tree, cottonwood, mulberry, sheep sorrel. Please contact specimen processing for any allergen not listed, ext. 3139. Lab Performing Test: Chemistry/Serology Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: none Specimen Required: clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: Varies depending on number of tests ordered Causes for Rejection: Gross hemolysis Availability: Mon-Fri 7am to 3pm Time Required Routinely for Processing: 48 hrs Additional Information: Latex, New England Regional Inhalant Panel, Comprehensive Inhalant Panel, General Food Screen, Shellfish Panel, Nut Panel, Childhood Allergy Panel, and Stinging Insect Panel are orderable and are listed separately in the lab guide. Reference Range: Interpretation provided with results. Rheumatoid Factor Synonyms: RAF Titer General Use: Diagnostic test for Rheumatoid arthritis Test Mnemonic: RF Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: < 15.0 IU/mL Rheumatoid Profile Synonyms: RA Profile General Use: Screening tests for SLE, Rheumatoid Arthritis, Gout, Lyme, arthritis. Test Mnemonic: RHEU Test Includes: ANA, RA factor, Lyme titer, Uric acid, CBC, Sed rate Lab Performing Test: Hematology & Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (serum) and whole blood (EDTA) Container Required: Red top tube, Lavender (EDTA) tube, Black top VacuTech tube Volume of Specimen: 10 ml clotted blood, 5 ml whole blood Minimum Volume of Specimen: 4 ml serum, 2 ml whole blood Causes for Rejection: Gross hemolysis Availability: 7:00AM-11:00PM; Mon. thru Sun. Not Stat. Time Required Routinely for Processing: 3-5 days Reference Range: see individual assays Rubella, Status Synonyms: German measles immunity titer General Use: To determine immune status to Rubella virus Test Mnemonic: RUBL Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: Mon - Fri 7AM-llPM. Sat 7AM-3PM Time Required Routinely for Processing: 24 hrs Reference Range: Reported as Immune or Non-immune Rubeola, Status Synonyms: Rubeola, immunity General Use: To determine immunity to or past exposure to Rubeola virus Test Mnemonic: RUBE Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood Container Required: Red top tube Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis. chylous serum Availability: Mon - Fri 7AM-11PM. Sat 7AM-3PM Time Required Routinely for Processing: 2-3 days Reference Range: Reported as Immune or Non-immune Salicylate, Blood Synonyms: Aspirin level General Use: Monitor therapy; toxicology Test Mnemonic: SAL Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine: 8 hours; stat, 1 hour Reference Range: Therapeutic: 2.8 – 20.0 mg/dL; >30 mg/dl potentially toxic result SGOT/AST Synonyms: GOT, AST General Use: Liver evaluation Test Mnemonic: AST Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: 15-37 U/L SGPT/ALT Synonyms: GPT, ALT General Use: Liver evaluation Test Mnemonic: ALT Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted serum (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml blood Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: 12-78 U/L Shellfish Panel Synonym: Allergy testing General Use: To aid in the diagnosis of atopic allergies Test Mnemonic: SHELLP Test Includes: Allergy screening for crab, shrimp, blue mussel, lobster, clam, oyster and scallop. Total IgE is included with panel. Lab Performing Test: Chemistry/Serology Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: none Special Instructions: Specimen Required: clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 5 ml serum Causes for Rejection: Gross hemolysis Availability: Mon-Fri 7am to 3pm Time Required Routinely for Processing: 48 hrs Reference Range: Interpretation provided with results. Sodium, Blood Synonyms: Na Test Mnemonic: NA Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml blood Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: 136-145 mmol/L Sodium, Urine Synonyms: Urine Na General Use: Renal function Test Mnemonic: UNA: random; UNA24: 24 hour collection Lab Performing Test: Chemistry Request Form: Universal requisition: used only as back-up to Meditech Specimen Required: Random or 24 hr collection Container Required: 24 hour urine container supplied by laboratory; Yellow top urine tube or urine cup for random Volume of Specimen: Entire collection Minimum Volume of Specimen: 0.5 ml Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: 24 hr specimens: 80-290 mEq/24 hr Random: Ranges not established Stinging Insect Panel Synonyms: Allergy Testing General Use: To aid in the diagnosis of atopic allergies Test Mnemonic: SIP Test Includes: Screening test for honeybee venom, white faced hornet, yellow jacket venom, paper wasp venom and yellow hornet. Total IgE is included with panel. Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Availability: Mon-Fri 7AM to 3PM Time Required Routinely for Processing: 48 hrs Reference Range: Interpretation provided with results Syphyllis Antibodies, Blood Synonyms: Rapid Plasma Reagin test General Use: Screening test for syphilis, Prenatal blood testing Test Mnemonic: SYPHAB Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Excessive hemolysis, chylous serum Availability: Mon-Fri 7am-5pm, Sat 7am – 3pm Time Required Routinely for Processing: 72 hours. Positive and borderline tests are referenced out for RPR confirmatory testing. Reference Range: Nonreactive T-3, Total Synonyms: Triiodothyronine General Use: Thyroid function, specifically used in the diagnosis of T-3 thyrotoxicosis Test Mnemonic: TT3 Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml of serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Additional information: Not to be confused with T3 Uptake which is part of Thyroid Profile Reference Range: See report T4, Free Synonyms: Free Thyroxine, FT4 General Use: Test for thyroid function Test Mnemonic: FT4 Lab Performing Test: Chemistry/Serology Request Form: Universal requisition; use only as a back up to Meditech Specimen Required: Clotted blond (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml blood Minimum Volume of Specimen: 1 ml serum Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Reference Range : See report Tegretol Synonyms: Carbamazepine General Use: Monitor therapeutic drug level Test Mnemonic: TEG Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml blood Minimum Volume of Specimen: 1.0 ml serum Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hr Reference Range: Therapeutic: 8-12 ug/mL ; > 15 ug/mL is potentially toxic Testosterone, Total General Use: This test is useful in the diagnosis of hypogonadism in males and hirsutism and virilization in females Test Mnemonic: TEST Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml blood Minimum Volume of Specimen: 2 ml serum Availability: Mon-Fri 7:00am – 11:00pm; Sat 7:00am-3:00pm Time Required Routinely for Processing: 24 hrs Reference Range: See report Theophylline Synonyms: Aminophylline General Use: Monitor therapeutic drug level Test Mnemonic: THEO Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted Blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1.0 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours, Stat 1 hour Reference Range: Therapeutic: 10-20 ug/ml ; > 20 ug/mL potentially toxic Thyroid Profile General Use: Thyroid function assessment and monitoring Test Mnemonic: THY Test Includes: T3 Uptake, T4, TSH ultra and calculated Free Thyroxine Index Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Reference Range: See report Thyroid Stimulating Hormone, Ultra sensitive Synonyms: TSH Ultra General Use: Differential diagnosis of primary hypothyroidism from secondary hypothyroidism Test Mnemonic: TSH Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Reference Range: See report Tissue Transglutaminase IgA Synonym: IgA tTg Test Mnemonic: TTGIGA Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Mon - Fri 7:00am-3:00pm Time Required Routinely for Processing: 48 hours Reference Range: See Report Tree Nut Panel Synonym: Allergy testing General Use: To aid in the diagnosis of atopic allergies Test Mnemonic: TRNUTP Test Includes: Allergy screening for hazelnut,brazil nut, almond,pecan, pistachio Cashew and walnut. Total IgE is included with panel. Lab Performing Test: Chemistry/Serology Request form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: none Specimen Required: clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 5 ml of serum Causes for Rejection: Gross hemolysis Availability: Mon-Fri 7am to 3pm Time Required Routinely for Processing: 48 hrs Reference Range: Interpretation provided with results Tobramycin Synonyms: Nebcin General Use: Monitor therapeutic level Test Mnemonic: Trough: TOBT; peak: TOBP; random: TOBR Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Peak level: 30 minutes after IV infusion is completed; Trough: immediately before next dose. Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: Daily 24 hrs Time Required Routinely for Processing: 2 hours Additional information: Levels should be drawn at steady state, usually 24-36 hours after starting treatment, depending on dosing schedule. Reference Range: Therapeutic Peak: 4-8 ug/mL; Trough: 0-2 ug/mL Triglycerides, Blood Synonyms: Trig Test Mnemonic: TRIG Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: 12-14 hrs. fasting; should be on stable diet 2 weeks prior to collection of blood Specimen Required: Clotted blood (Serum) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml of serum Container Required: Red top tube (SST) Lab Performing Test: Chemistry Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Causes for Rejection: Nonfasting sample General Use: Evaluate hyper or hypo lipidemia Reference Range: <150 mg/dL Triglycerides – Fluid Test Mnemonic: FTRIGS Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Indicate source when ordering Container Required: Sterile glass/plastic tube Volume of Specimen: 1 ml Minimum Volume of Specimen: 0.5 ml Causes for Rejection: Viscous or clotted specimen Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Reference Range: Reference ranges not established Troponin I Synonym: Cardiac Troponin General Use: Assessment of AMI Test Mnemonic: TROPIP Lab Performing Test: Chemistry Request Form: Universal Requisition; use only as a backup to Meditech Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 0.5 ml serum Causes for Rejection: Improper tube type Availability: 24 hrs. daily Time Required Routinely for Processing: 1 hour STAT; Routine 8 hrs Additional information: May also be ordered as part of MI profile (HEART) Reference Range: See report Urea Nitrogen, Blood Synonyms: BUN; Blood Urea Nitrogen General Use: Kidney function Test Mnemonic: BUN Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1.0 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hr Reference Range: 7-18 mg/dL Urea, Urine Synonyms: Urinary Urea Nitrogen General Use: Kidney function Test Mnemonic: Random: UUN; 24 hr collection UUN24 Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Refrigerate urine during collection Specimen Required: Random or 24 hour urine Container Required: 24 hour urine container obtained from Chemistry; yellow top urine tube or urine cup for random collection Volume of Specimen: 24 hr collection : Entire collection; random collection :10 ml Minimun Volume of Specimen: 24 hr collection: entire collection ; random collection : 1 ml Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hr Reference Range: 24 hr specimens: 6-17 gm/TV Random: Ranges not established Uric Acid, Blood Synonyms: UA General Use: Diagnosis of gout, metabolic disorders, and toxemia of pregnancy Test Mnemonic: URIC Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1.0 ml serum Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hour Reference Range: 2.6-6.0 mg/dL females; 3.5-7.2 mg/dL males Uric Acid, Fluid General Use: Diagnosis of gout and rheumatoid syndromes Test Mnemonic: FURICA Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Indicate source when ordering Container Required: Clean glass/plastic tube Volume of Specimen: 1 ml Minimum Volume of Specimen: 0.5 ml Causes for Rejection: Viscous or clotted specimen Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Reference Range: Reference ranges not established Uric Acid, Urine Synonyms: Urinary UA General Use: Uric acid metabolism Test Mnemonic: Random: UUA; 24 hr collection: UUA24 Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Normal diet 24 hours prior to collection Special Instructions: Refrigerate urine during collection Specimen Required: Random or 24 hr. collection Container Required: 24 hour urine container obtained from chemistry; urine cup for random collection or yellow top urine tube Volume of Specimen: 24 hr collection : entire collection ; random collection : 10 ml Minimum Volume of Specimen: 24 hr collection : entire collection ; random collection : 1 ml Availability: 24 hours daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Reference Range: 24 hr specimens: 0.25 - 0.75 gm/TV Random: Reference ranges not established Valproic Acid Synonyms: Depakene General Use: Monitor therapeutic level Test Mnemonic: VPA Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Trough values drawn just before next dose possibly more useful than peak values drawn 1-3 hours after an oral dose. Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hrs; Stat 1 hour Reference Range: Therapeutic range: 50-100 ug/mL; > 120 ug/mL potentially Toxic Vancomycin General Use: Therapeutic drug monitoring Test Mnemonic: Trough level: VANT; peak level: VANP Lab Performing Test: Chemistry Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml serum Collection: Trough levels are collected 1/2 hr before dose is given. Peak levels are collected 1 hr after infusion is finished Availability: 24 hrs daily Time Required Routinely for Processing: Routine 8 hours; Stat 1 hr Reference Range: Trough: 5-10 ug/mL; Peak levels: 30 min post 1hr infusion: 30-40 ug/mL, 60 min post 1 hr infusion: 25-40 ug/mL, 120 min post 1 hr infusion: 18-26 ug/mL Vitamin B12 Synonyms: Cyanocobalamin, B12 General Use: Screening for B-12 deficiency, malabsorption; pernicious anemia Test Mnemonic: B12 Lab Performing Test: Chemistry/Serology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (Serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml blood Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Gross hemolysis, chylous serum Availability: Mon - Fri 7AM to 11PM; Sat 7AM to 3PM Time Required Routinely for Processing: 24 hrs Reference Range: 239-931 pg/ml Vitamin D 25-Hydroxy General Use: Measurement of serum 25-OH Vitamin D provides a good index of circulating Vitamin D activity. Test Mnemonic: VD25 Lab Performing Test: Chemistry/Serology Request form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clotted blood (serum) Container Required: Red top tube (SST) Volume of Specimen: 10 ml Minimum Volume of Specimen: 1.0 ml serum Availability: Monday – Friday 7:00am-11:00pm,Sat 7:00am-3:00pm Time Required Routinely for Processing: 1 day Reference Range: See Report COAGULATION The Coagulation section of the Laboratory is directed by Victoria G. Reyes-D'Arcy/ Asim Ejaz, M.D., D.A.B. Pathologist, and Pedro Ugarelli, M.S., B.S., M.T., Hematology Manager. For procedures not listed please consult with the Hematology Manager(Ext. 4137) or Pathologist. All specimens must be properly labeled with patient's full name, identification number, time and date of collection, and the test requested. Activated Partial Thromboplastin Time Synonyms: APTT General Use: Measures intrinsic coagulation system; monitor unfractionated heparin therapy Test Mnemonic: APTT Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Container Required: Blue top tube (sodium citrate) Specimen Required: Plasma Volume of Specimen: 2.7ml Minimum Volume of Specimen: 2.7ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Samples must be processed within 4 hours of collection Availability: Routine and Stat 24 hours daily Time Required Routinely for Processing: Routine: 2 hours; Stat: 30 minutes Reference Range: See printed report Antithrombin III General Use: Part of hypercoagulation profile (HCOAG); quantitation of ATIII level. Test Mnemonic: ATIII Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient must not be on anticoagulants Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Specimen Required: Plasma Container Required: Blue top tube (sodium citrate) Volume of Specimen: 2.7 ml Minimum Volume of Specimen: 2.7ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Samples must be processed within 4 hours of collection Availability: Performed once a week Reference Range: See printed report APTT see Activated Partial Thromboplastin Time C.A.C. Circulating Anticoagulant see: Mixing Studies Coagulation Factor Assays see Factor VIII Assay Coagulation Profile Synonyms: Hemorrhagic Screen General Use: Screening for coagulation disorder Test Mnemonic: COAGP Profile Includes: Prothrombin Time, APTT, Fibrinogen, Platelet Count, Platelet Function Assay Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Specimen Required: Plasma and fresh whole blood Container Required: 2 Blue top tubes (sodium citrate) and 1 lavender top tube (EDTA) Volume of Specimen: Two 2.7 ml (blue top tubes) and 4.0 ml of fresh whole blood (lavender top tube) Minimum Volume of Specimen: Two 2.7 ml (blue top tubes) and 4.0 ml whole blood (lavender top tube) Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: 24 hours daily, routine and stat Time Required Routinely for Processing: 2 hours Reference Range: See printed report. D-Dimer Quantative Synonyms: Automated D-Dimer, Quantitative D-Dimer General Use: Rule out DVT/PE in emergency room settings in low-moderate risk patients. Test Mnemonic: DDIMER Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Container Required: Blue top tube (sodium citrate) Specimen Required: Plasma Volume of Specimen: 2.7ml Minimum Volume of Specimen: 2.7ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, specimen more than 2 hours old, mislabeled or unlabeled specimen. Availability: Routine and Stat 24 hours daily Time Required Routinely for Processing: Routine: 1-2 hours; Stat: 30 minutes Reference Range: See printed report D-Dimer Qualitative Synonyms: DDimer Qualitative, DIM General Use: Detection of fibrin degradation Test Mnemonic: DDQUAL Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Specimen Required: Whole blood Container Required: Blue top tube (sodium citrate) Volume of Specimen: 2.7 ml whole blood (blue top tube) Minimum Volume of Specimen: 2.7 ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: 24 hours daily and Stat Time Required for Processing: Routine same day, Stat 1 hour Reference Range: Negative DIC Profile General Use: Assess intravascular clotting Test Mnemonic: DIC Profile Includes: Prothrombin Time (PT), APTT, Fibrinogen, Platelet Count, and D-DQUAL Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: None (Note: anticoagulant therapy may interfere with test result interpretation) Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Specimen Required: Plasma and fresh whole blood. Container Required: 2 Blue top tubes (sodium citrate) and 1 lavender top tube (EDTA) Volume of Specimen: Two 2.7 ml of plasma (blue top tubes) and 5.0 ml whole blood (lavender top tube) Minimum Volume of Specimen: Two 2.7 ml (blue top tubes) and 5.0 ml of fresh whole blood (lavender top tube) Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: 24 hrs, daily and STAT Time Required Routinely for Processing: Routine same day; Stat 1 hour Reference Range: See report. Factor II Mutation see Prothrombin Gene Mutation Factor VIII Assay Synonyms: Factor 8 Assay, F8 General Use: Detecting specific coagulation factor assays. Test Mnemonic: VIII Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient must not be on anticoagulants Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Specimen Required: Plasma Container Required: Blue top tube (sodium citrate) Volume of Specimen: 2.7 ml Minimum Volume of Specimen: 2.7 ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Performed once a week Reference Range: See printed report Fibrinogen Level General Use: Quantitative fibrinogen level Test Mnemonic: FIBR Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Specimen Required: Plasma Container Required: Blue top tube (sodium citrate) Volume of Specimen: 2.7 ml (blue top tube) Minimum Volume of Specimen: 1.2 ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: 24 hours routine and Stat. Time Required Routinely for Processing: Routine 2 hours; Stat 30 minutes. Reference Range: See printed report. HCOAG see Hypercoagulable profile Hemorrhagic Screen see Coagulation Profile Hypercoagulable Profile Synonyms: HCOAG General Use: Assess hypercoagulable state Test Mnemonic: HCOAG Profile Includes: Protein C, ATIII, Factor VIII Assay, Fibrinogen, Lupus Anticoagulant, Protein S, Prothrombin Time, APTT, and APCR. Lab Performing Test: Hematology. Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient must not be on anticoagulants Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Specimen Required: Plasma Container Required: 3 Blue top tubes (sodium citrate) Volume of Specimen: 3 Full 2.7 ml blue top tubes Minimum Volume of Specimen: 2.7 ml X 3 Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Daily, not Stat; specimen collected and frozen 24 hours daily. Time Required Routinely for Processing: 2-5 days Reference Range: See printed report LUPA see Lupus Anticoagulant Lupus Anticoagulant Synonyms: LA, LUPA General Use: To evaluate patients for the presence of lupus anticoagulant Test Mnemonic: LUPA Lab Performing Test: Hematology send out Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient must not be on anticoagulants Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Specimen Required: Plasma Container Required: Blue top tube (sodium citrate) Volume of Specimen: 2 Full 2.7 ml blue top tubes. Minimum Volume of Specimen: 2.7 ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Specimen collected and frozen 24 hours daily. Time Required Routinely for Processing: Performed once a week Reference Range: See report. Mixing Studies Synonyms: C.A.C. Coagulation Mixing studies, Mixing Studies General Use: Detection of circulating antibodies Test Mnemonic: MXSTDY Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient must not be on anticoagulants Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Specimen Required: Plasma Container Required: 2 full blue top tubes (sodium citrate) Volume of Specimen: 2.7 mL Minimum Volume of Specimen: 2.7 ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Specimen collected and frozen 24 hours daily; test performed MonFri: 6am -10pm. Time Required Routinely for Processing: Weekdays-same day; weekendsspecimen frozen and test performed on Mondays. Additional Information Needed: Previous Prothrombin Time and APTT Reference Range: See printed report. PFA see Platelet Function Assay Platelet Function Assay General Use: To assess the ability of platelets to aggregate Test Mnemonic: PFA Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Specimen Required: Whole blood Container Required: Glass Blue top tube (sodium citrate) Volume of Specimen: 4.5 ml of whole blood (blue top tube) Minimum Volume of Specimen: 4.5 ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: 24 hours daily Time Required Routinely for Processing: 2 hours Reference Range: CEPI (Collagen/EPI): 65-181 seconds ADP (Collagen/ADP): 53-113 seconds Protein C General Use: Quantitative Protein C level Test Mnemonic: PC Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient must not be on anticoagulants Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Specimen Required: Plasma Container Required: Blue top tube (sodium citrate) Volume of Specimen: 2.7 ml (blue top tube) Minimum Volume of Specimen: 2.7 ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Test performed once a week. Reference Range: See printed report Protein S General Use: Quantitative Protein S level Test Mnemonic: PRS Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient must not be on anticoagulants Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Specimen Required: Plasma Container Required: Blue top tube (sodium citrate) Volume of Specimen: 2.7 ml (blue top tube) Minimum Volume of Specimen: 2.7 ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Test performed once a week. Reference Range: See printed report Prothrombin Time/INR Synonyms: PTBAT, Protime General Use: Monitoring oral anticoagulants Test Mnemonic: PTINR Profile Includes: PT and INR Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Use 21 or 22 gauge needle to obtain specimen; do not use butterfly needle. A discard tube must be drawn before a specimen for coagulation testing; then, a citrated blue top tube(s) should be drawn next. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10ml of blood collected must be discarded. Specimen Required: Plasma Container Required: Blue top tube (sodium citrate) Volume of Specimen: 2.7 ml (blue top tube) Minimum Volume of Specimen: 2.7 ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen, mislabeled or unlabeled specimen. Availability: 24 hours daily and Stat Time Required Routinely for Processing: Routine 2 hours; Stat 30 minutes Reference Range: INR of 2.0-3.0 for standard prophylaxis INR of 2.5-3.5 for high-risk prophylaxis PT/INR see Prothrombin Time/INR CYTOLOGY The Cytology Section is under the direction of Anica Antic, M.D., Director of Cytology. Services consist of examination of physiologically and artificially exfoliated or aspirated cells. The section is staffed by two part-time cytotechnologists. The Cytology Laboratory is open weekdays from 8:00 AM to 4:30 PM. After regular hours, and on weekends, cytology specimens are placed in specimen refrigerators. Please follow the appropriate protocol posted next to the Cytology door and on the refrigerator door. The most common sources of cytology specimens include gynecological smears and liquid-based preparations such as sputum, bronchial, esophageal, gastric, urinary tract and various body fluids (pleural and peritoneal) as well as fine needle aspirates from various organs. The principle emphasis is the evaluation of cell populations for the detection of malignant and pre-malignant changes. Labeling of specimens: All specimens must be labeled in the presence of the patient and submitted in a properly labeled container, to include the patient's name, date of birth, and specimen type/source. All prepared slides submitted must be identified by writing the patient's name, date of birth and specimen source on the frosted end of the slide with a #2 or #3 lead pencil. For all outpatient areas and the Emergency Department, each specimen, regardless of type, must be submitted with a standard cytology requisition. The following information is needed and must be entered on the Cytology requisition: 1. Patient's name, date of birth, hospital number, physician's name, hospital ward, office or clinic, and date of specimen collection. 2. Specimen type/source. 3. Clinical diagnosis and pertinent clinical history. 4. Medications: hormones, chemotherapeutic drugs, etc. 5. Sex of patient. For Surgery, Pequot Surgery, and inpatient units, cytology orders are entered in McKesson or Meditech. (See Order Entry procedures). Ascitic Fluid Cytology see Cytology, Body Fluids: Pleural, Ascitic and Pericardial Breast Cyst Fluid Cytology see Cytology, Spinal and Cyst Fluid: Renal, Ovarian, Breast, Etc. Bronchial Brushings, Cytology see Cytology, Brushings: Bronchial, Esophageal, Gastric, Small Bowel, Colonic, Etc. Bronchial Washings, Cytology see Cytology, Bronchial, Esophageal Washings and Tracheal Aspirations Cyst Fluid Cytology see Cytology, Spinal and Cyst Fluid: Renal, Ovarian, Breast, Etc. Cytology, Body Fluids: Pleural, Ascitic and Pericardial Synonyms: Pleural Fluid Cytology; Thoracentesis Cytology; Ascitic Fluid Cytology; Paracentesis Cytology; Pericardial Fluid Cytology; Pericardiocentesis Cytology Test Includes: Cytologic examination and tissue cell block (when possible) (Cytology) Lab Performing Test: Cytology Request Form: Cytology - include pertinent clinical information, e.g., previous carcinoma, drugs, radiation therapy or history of alcohol abuse. Under source include type of fluid. Special Instructions: Deliver to Cytology lab immediately Specimen Required: Fresh body fluid Container Required: Vacutainer bottles obtained in central supply. Container must be labeled in the presence of the patient and must include tha patient’s name, date of birth, and specimen source. Volume of Specimen: If 500 ml or less is obtained, send entire specimen to Cytology. If more, send an aliquot of at least 500 ml. Causes for Rejection: Improper labeling and improper container; i.e. plastic evacuation bags, syringes. Availability: Weekdays 8AM to 4:30PM, Time Required Routinely for Processing: 24-48 hours Additional Information: Specimen should be refrigerated if Cytology Lab is closed Reference Range: Negative Cytology, Bronchial, Esophageal Washings and Tracheal Aspirations Synonyms: Bronchial Washings Cytology; Esophageal Washings, Tracheal Aspiration Cytology General Use: To establish the presence of primary or metastatic neoplasm Lab Performing Test: Cytology Request form: Cytology - under source of specimen enter site of collection. Include pertinent clinical information, e.g., previous carcinoma. Special Instructions: Deliver to Cytology lab immediately Specimen Required: Obtained by physician Container Required: Available in central supply. Container must be labeled in the presence of the patient and must include tha patient’s name, date of birth, and specimen source. Volume of Specimen: Not less than 1-2 cc Causes for Rejection: Improper labeling Availability: Weekdays, 8AM to 4:30PM Time Required Routinely for Processing: 24-48 hours Additional Information: Specimen should be refrigerated if Cytology lab is closed Reference Range: Negative Cytology, Brushings: Bronchial, Esophageal, Gastric, Small Bowel, Colonic, Etc. Synonyms: Bronchial Brushings, Cytology General Use: To establish the presence of primary or metastatic neoplasm Lab Performing Test: Cytology Request Form: Cytology - under source of specimen specify the site brushed. Include pertinent clinical data, e.g., admitting diagnosis, history of carcinoma. Specimen Required: Brush lesion area, smear on slides (labeled with name, date of birth and specimen type) and fix immediately in 95% alcohol, or cytology spray fixative. Alternatively, immediately place the brush in Saccomanno’s fixative or equivalent. Agitate the brush, which may be left in the fixative. Container Required: Coplin jars and Saccomanno’s fixative are available in Cytology lab. Container must be labeled in the presence of the patient and must include tha patient’s name, date of birth, and specimen source. Causes for Rejection: Improper labeling, improper fixation Availability: Weekdays, 8AM-4:30PM Time Required Routinely for Processing: 24-48 hours Reference Range: Negative Cytology, Cervical – Vaginal Smears Synonyms: Papanicolaou Smear; Pap Smear ; Liquid-based cytology General Use: To establish the presence of primary or metastatic neoplasm, reactive processes or infectious disease; only offered for inpatients. Liquid-based specimens may also be tested by molecular methods for GC/Chlamydia DNA and HPV DNA. For HPV testing, specify whether to perform as a reflex for ASCUS/AGUS, or regardless of pap result. Lab Performing Test: All liquid based specimens will be sent to a reference lab for processing and interpretation. In hospital conventional smears will be screened and reviewed by Dr. Muscato, Dr. Green or Dr. Antic. Request Form: Cytology - under source of specimen indicate: endocervical, ectocervical or vaginal. Include pertinent clinical history, e.g., age, LMP, PMP, surgery, exogenous hormones, history of carcinoma, radiation, chemotherapy. Special Instructions: Slides frosted on one end should be labeled with the patient's name, date of birth and source of specimen. Vaginal smears: We recommend sampling the pool in the posterior vaginal vault. Cervical smears: A 360 degree scraping about cervical os using a wooden cervi-scraper is recommended, also a cytobrush inserted into the endocervix and rotated 1/2 to 1 full turn is recommended. Place slides immediately in 95% alcohol or spray with fixative. For liquid-based cytology (Cytyc ThinPrep or Roche SurePath), follow manufacturer recommendations. Specimen Required: "EXO and ENDO", "CX" and "ENDOCX" or "VAG" and "CX" Container Required: Pap kit organizers/slides, ThinPrep and SurePath supplies are available in Specimen Processing. Causes for Rejection: Improper labeling, of either slide or requisition. Availability: Weekdays, 8AM to 4:30PM Time Required Routinely for Processing: 24-72 hours, after receipt Reference Range: Negative Cytology, Nipple Discharge Synonyms: Nipple Discharge Cytology General Use: To establish the presence of primary or metastatic neoplasm Lab Performing Test: Cytology Request Form: Cytology - under source of specimen specify nipple discharge. Include slide, pertinent clinical data, e.g., history of carcinoma. Special Instructions: Label slides with name of patient, date of birth and source. Place in 95% alcohol or cytology spray fixative immediately after taking slides. Specimen Required: Nipple discharge Container Required: Cytology fixative available in Cytology Causes for Rejection: Improper labeling, improper fixation Availability: Weekdays, 8AM to 4:30PM Time Required Routinely for Processing: 24-48 hours Reference Range: Negative Cytology, Spinal and Cyst Fluid: Renal, Ovarian, Breast, Etc. Synonyms: Spinal Fluid Cytology; Cyst Fluid Cytology: Renal Cyst Fluid Cytology; Ovarian Cyst Fluid Cytology; Breast Cyst Fluid Cytology General Use: To establish the presence of primary or metastatic neoplasm Lab Performing Test: Cytology Request Form: Cytology - under source of specimen specify specimen origin. Include pertinent clinical data, e.g., admitting diagnosis, history of carcinoma. Special Instructions: Deliver to Cytology lab immediately Specimen Required: Fresh fluid Container Required: If small amount of fluid, use sterile urine cups or urine tube. Container must be labeled in the presence of the patient and must include tha patient’s name, date of birth, and specimen source. Volume of Specimen: Not less than 1-2 ml Causes for Rejection: Improper labeling Availability: Weekdays, 8AM to 4:30PM Time Required Routinely for Processing: 24-48 hours Additional Information: Specimen should be refrigerated if Cytology lab is closed. Reference Range: Negative Cytology, Sputum Synonyms: Sputum Series Cytology; Sputum Cytology General Use: To establish the presence of primary or metastatic neoplasm Request Form: Cytology - under source of specimen enter sputum. Include admitting diagnosis and pertinent clinical history, e.g., history of carcinoma, exposure to carcinogen Specimen Required: Deep cough sputum, NOT SALIVA OR NASAL ASPIRATES Container Required: Sterile specimen container. Container must be labeled in the presence of the patient and must include tha patient’s name, date of birth, and specimen source. Causes for Rejection: Improper labeling, saliva or nasal aspirates Availability: Weekdays, 8AM to 4:30PM Time Required Routinely for Processing: 24-48 hours Additional Information: Specimen should be placed in refrigerator if Cytology lab is closed. Reference Range: Negative Cytology, Urine General Use: To establish the presence of primary or metastatic neoplasm Lab Performing Test: Cytology Request Form: Cytology - under source of specimen specify clean voided, catheterized or bladder washing Special Instructions: Urine specimen should be collected before patient has an IVP. Specimen should be delivered to lab immediately. If from office, alcohol may be added to the specimen. (50% ethanol, 1:1 by volume) Container Required: Plastic urine container. Container must be labeled in the presence of the patient and must include tha patient’s name, date of birth, and specimen source. Volume of Specimen: Not less than 10 cc, preferably 50 cc. Causes for Rejection: Improper labeling, 24-hour collection Availability: Weekdays, 8AM to 4:30PM Time Required Routinely for Processing: 24-48 hours Additional Information: Specimen should be refrigerated if Cytology lab is closed. Reference Range: Negative Cytology: Viral Study: Cytomegalic Virus on Urine Synonyms: Cytomegalic Inclusion Disease (CID); Cytomegalic Inclusion Bodies General Use: To establish the presence of Cytomegalovirus infection Lab Performing Test: Cytology Request Form: Cytology - under source of specimen enter urine and specify for Cytomegalic Inclusion Virus. Include pertinent clinical history, e.g., chemotherapy or immune-supression Special Instructions: Deliver to Cytology lab immediately Specimen Required: Fresh urine Container Required: Sterile urine container. Container must be labeled in the presence of the patient and must include tha patient’s name, date of birth, and specimen source. Volume of Specimen: Prefer 50 cc. Usually the greater the volume, the greater the number of cells for evaluation Causes for Rejection: Improper labeling Availability: Weekdays 8AM-4:30PM Time Required Routinely for Processing: 24-48 hours Additional Information: Specimen should be refrigerated if Cytology lab is closed. Reference Range: No viral inclusion bodies seen Cytomegalic Inclusion Bodies see Cytology: Viral Study: Cytomegalic Virus on Urine Cytomegalic Inclusion Disease (CID) see Cytology: Viral Study: Cytomegalic Virus on Urine Esophageal Washings, Tracheal Aspiration Cytology see Cytology, Bronchial, Esophageal Washings and Tracheal Aspirations Fine Needle Aspiration General Use: To establish the presence of primary or metastatic neoplasm or reactive process or infectious diseases Lab Performing Test: Cytology Laboratory Request Form: Cytology- under source of specimen indicate body site. Include pertinent clinical history, i.e., date of birth, surgery, history of carcinoma, radiation, chemotherapy, size of mass, etc. Patient Preparation: Physician's responsibility Special Instructions: Call X-Ray Department to schedule procedure. If procedure is performed in office, slide must be properly labeled (patient name, date of birth and specimen type), fixed with 95% alcohol or spray fixative and submitted with a completed requisition. Alternatively, the needle aspirate can be placed immediately in Saccomanno’s fixative or equivalent. Container Required: Coplin Jar with 95% alcohol, or cytology spray fixative, and Saccomanno’s fixative are available in Cytology. Container must be labeled in the presence of the patient and must include tha patient’s name, date of birth, and specimen source. Causes for Rejection: Improper labeling of specimen and incorrect specimen containers (no syringes with needles) Availability: Weekdays, 8AM to 4:30PM; Stat procedure available during weekday hours Time Required Routinely for Processing: 24-48 hours Additional Information: Cytology staff available for assistance. For questions please call ext. 5121 Reference Range: Negative Nipple Discharge Cytology, see Cytology, Nipple Discharge Ovarian Cyst Fluid Cytology see Cytology, Spinal and Cyst Fluid: Renal, Ovarian, Breast, Etc. Pap Smear see Cytology, Cervical - Vaginal Smears Papanicolaou Smear see Cytology, Cervical - Vaginal Smears Paracentesis Cytology see Cytology, Body Fluids: Pleural, Ascitic and Pericardial Pericardial Fluid Cytology see Cytology, Body Fluids: Pleural, Ascitic and Pericardial Pericardiocentesis Cytology see Cytology, Body Fluids: Pleural, Ascitic and Pericardial Pleural Fluid Cytology see Cytology, Body Fluids: Pleural, Ascitic and Pericardial Renal Cyst Fluid Cytology see Cytology, Spinal and Cyst Fluid: Renal, Ovarian, Breast, Etc. Spinal Fluid Cytology see Cytology, Spinal and Cyst Fluid: Renal, Ovarian, Breast, Etc. Sputum Cytology see Cytology, Sputum Sputum Series Cytology see Cytology, Sputum Thoracentesis Cytology see Cytology, Body Fluids: Pleural, Ascitic and Pericardial Tzanck Preparation Synonyms: Tzanck smear, smear for cutaneous herpes General Use: To establish the presence of Herpes Simplex Virus Lab Performing Test: Cytology Request Form: Cytology - under source of specimen indicate site. Include pertinent clinical information Specimen Required: Brush, scrape lesions, smear on appropriately labeled slides (patient name, date of birth and specimen type) and fix immediately in 95% Alcohol or cytology spray fixative Container Required: Available from Cytology lab Causes for Rejection: Improper labeling or fixation Availability: Weekdays 8AM-4:30PM Time Required Routinely for Processing: 24-48 hours, Stat on request Reference Range: Negative HEMATOLOGY The Hematology section of the Laboratory is directed by Victoria G. Reyes-D'Arcy/ Asim Ejaz, M.D., D.A.B. Pathologist, and Pedro Ugarelli, M.S., B.S., M.T., Hematology Manager. This section offers a wide range of services including coagulation, urinalysis, hematology, and body fluid analyses. For procedures not listed please consult with the Hematology Manager(Ext. 4137) or Pathologist. All specimens must be properly labeled with patient's full name, identification number, time and date of collection, and the test requested. Babesia Smear General Use: Rapid Screening for Babesia Test Mnemonic: BABSMR Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instruction: Specimen Required: Whole Blood Container Required: Lavender top tube (EDTA) Volume of Specimen: 4.0 ml of blood (lavender top tube) Minimum Volume of Specimen: 4.0 ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen Availability: Daily – not STAT Time Required Routinely for Processing: 2 hours Reference Range: Negative Body Fluid Analysis Synonyms: Body fluid cell count. General Use: Evaluation of cellularity and cell types contained in various body fluids for determining infection, malignancy, inflammatory reaction. Test Mnemonic: FCT Profile Includes: Body fluids (other than synovial fluid) includes WBC and RBC enumeration and review of cell morphology by a pathologist Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Responsibility of Physician Special Instructions: Anatomic origin of fluid required, i.e., chest, abdomen, etc.; deliver to the lab immediately upon collection Specimen Required: Thoracentesis or paracentesis fluids, miscellaneous body fluids. Container Required: Lavender top tube (EDTA) Volume of Specimen: 4.0 ml Minimum Volume of Specimen: 4.0 ml Causes for Rejection: Clotted specimen, insufficient specimen volume, mislabeled or unlabeled specimen. Availability: Cell Count - daily first and second shifts; Pathologist review of cell morphology Monday through Friday Time Required for Processing: Body fluid analysis - up to 4 hours (pathology review only on weekdays) Reference Range: See ranges on printed report. Body Fluid Specific Gravity Synonyms: Fluid specific gravity General Use: Determining if a fluid is an exudate or transudate in conjunction with other testing Test Mnemonic: FSPGR Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Responsibility of physician Special Instructions: Site of collection required, i.e., chest, knee, etc. Specimen Required: Body fluid Container Required: Urine container Volume of Specimen: 5.0 ml of fluid Minimum Volume of Specimen: 1.0 ml Causes for Rejection: Clotted specimen, inadequate specimen volume, mislabeled or unlabeled specimen Availability: 24/7 Time Required Routinely for Processing: up to 2 hours Reference Range: Physician interpretation. Bone Marrow General Use: Bone marrow aspirate/biopsy/clot section morphology, including cellularity, myeloid/erythroid ratio, and iron stores Test Mnemonic: Cannot be ordered in Meditech Profile Includes: H + E stain, Wright's stain, and iron stain Lab Performing Test: Hematology, Histology, and Pathology Request Form: Bone Marrow Request form (filled out in entirely by physician) Patient Preparation: Performed by physician Special Instructions: Call Hematology for bone marrow tray Specimen Required: Bone marrow biopsy and bone marrow aspirate Container Required: Lavender top tube (EDTA) for bone marrow aspirate; formalin for bone marrow biopsy Volume of Specimen: 1.0 ml of bone marrow aspirate (lavender top tube) Minimum Volume of Specimen: 1.0 ml Causes for Rejection: Mislabeled or unlabeled specimen. Availability: Mon. - Fri.; Not STAT, Not available on weekends or holidays. Bone Marrow samples must arrive in Hematology Lab before 2 PM . Time Required for Processing: Specimen prepared same day; Pathology report: 48-72 hours for biopsy Reference Range: Results interpreted by Pathology. CBC see Complete Blood Count Chronic Leukemia/Lymphoma Immunophenotyping Synonyms: Leukemia/Lymphoma Panel, CLLP General Use: Immunophenotypic markers for hematopoietic cells, leukemia, lymphoproliferative disorders. Test Mnemonic: CLLP Lab Performing Test: Specimen Processing, sent to Reference Lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Clinical history required Specimen Required: Whole blood Container Required: 1 Green top tube (sodium heparin) or 1 lavender (EDTA) Volume of Specimen: 8.0 ml of blood Minimum Volume of Specimen: 8.0 ml of blood Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen Availability: Daily, Mon.-Fri. Time Required Routinely for Processing: 1-2 days Reference Range: Interpretation made by pathologist Cerebrospinal Fluid Analysis Synonyms: CSF cell count; spinal fluid cell count. General Use: Evaluation of CSF for cellularity and cell typing in determining infection, intracranial bleed, malignancy, and other disease states. Test Mnemonic: CCT Profile Includes: WBC and RBC enumeration and WBC differential count Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Responsibility of physician Special Instructions: Specific tests to be performed on each collection tube must be indicated; deliver specimens to lab immediately upon collection. Specimen Required: CSF Container Required: Sterile CSF collection tube(s) Volume of Specimen: 2.0 ml Causes for Rejection: Clotted specimen, inadequate specimen volume, mislabeled or unlabeled specimen. Availability: 24 hours daily, always performed STAT Time Required for Processing: 2 hours. Reference Range: See printed report. Complete Blood Count Synonyms: CBC; Hemogram General Use: Evaluation of peripheral blood parameters Test Mnemonic: CBC Profile Includes: WBC, RBC, HGB, HCT, MCV, MCH, MCHC, PLCT and 6-part automated differential. Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood Container Required: EDTA Lavender top tube or Microtainer. Volume of Specimen: 4.0 ml of blood (lavender top tube) or 0.75 ml of blood (lavender Microtainer) Minimum Volume of Specimen: 4.0 ml (lavender top tube) or 0.5ml (Microtainer) Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: 24 hours daily, routine and STAT Time Required for Processing: Stat 30 minutes; routine same day. Reference Range: See accompanying ranges by age and gender in printed report Complete Blood Count with Manual Differential Synonyms: CBC and Manual Diff; Hemogram and Manual Diff. General Use: Evaluation of peripheral blood parameters Test Mnemonic: CBC Profile Includes: WBC, RBC, HGB, HCT, MCV, MCH, MCHC, PLCT and manual differential count and review of morphologic characteristics of blood cells Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood Container Required: EDTA Lavender top tube or Microtainer. Volume of Specimen: 4.0 ml of blood (lavender top tube) or 0.75 ml of blood (lavender Microtainer) Minimum Volume of Specimen: 4.0 ml (lavender top tube) or 0.5ml (Microtainer) Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: 24 hours daily, routine and STAT Time Required for Processing: Stat 30 minutes; routine same day. Reference Range: See accompanying ranges by age and gender in printed report CSFCT see Cerebrospinal Fluid Analysis. Ehrlichia Smear General Use: Rapid screening for Ehrlichia Test Mnemonic: EHRSMR Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instruction: Test will not be performed without a prior CBC. If the WBC is greater than 4.0 and/or platelet count is greater than 120,000/mL the test will not be performed. Specimen Required: Whole blood Container Required: Lavender top tube (EDTA) Volume of Specimen: 4.0 ml of blood (lavender top tube) Minimum Volume of Specimen: 4.0 ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Daily - not STAT Time Required Routinely for Processing: 4 hours Reference Range: Negative Eosinophil Smear Synonyms: Nasal smear for eosinophils; Sputum smear for eosinophils General Use: Investigation of allergic disorders Test Mnemonic: EOSM Lab Performing Test: Hematology send out Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Smear or swab of sputum, 2 slides of nasal secretion Causes for Rejection: Insufficient specimen, mislabeled or unlabeled specimen. Availability: Daily - Not STAT Time Required Routinely for Processing: Same day except for weekends Reference Range: None seen Erythrocyte Sedimentation Rate see Sedimentation Rate ESR see Sedimentation Rate FCEL see Body Fluid Analysis Fetal Hemoglobin Stain Synonyms: Kleihauer-Betke Fetal Hgb Stain General Use: Qualitative evaluation of Hgb F, if present; to determine possible hemorrhage in the newborn; to assess the magnitude of fetal - maternal hemorrhage. Test Mnemonic: FHGBS Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood Container Required: Lavender top tube (EDTA) Volume of Specimen: 4.0 ml of blood (lavender top tube) Minimum Volume of Specimen: 4.0 ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen Availability: Daily, routine and stat until 10PM; Not done from 10PM to 7AM Time Required Routinely for Processing: Same day Reference Range: 0.000 (See Table II) FHCT see Hematocrit - Body Fluid Fluid Crystals General Use: Aid in the diagnosis of gout or pseudogout. Test Mnemonic: BFCRYS Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Responsibility of physician Special Instructions: Site of fluid extraction should be noted, ie., right knee, left elbow, etc. Specimen Required: Body fluid specimens. Specify body site. Container Required: Lavender top tube (EDTA) or green top tube (sodium heparin) Volume of Specimen: 2.0 ml (lavender top tube) Minimum Volume of Specimen: 2.0 ml Causes for Rejection: Insufficient specimen volume, mislabeled or unlabeled specimen Availability: Daily first and second shift; not stat Time Required Routinely for Processing: Up to 4 hours Reference Range: None seen Fluid Hematocrit Synonyms: Body fluid hematocrit General Use: Physician interpretation Test Mnemonic: FHCT Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Responsibility of physician Specimen Required: Body fluid Container Required: Lavender top tube (EDTA) Volume of Specimen: 1.0 ml (lavender top tube) Minimum Volume of Specimen: 1.0 ml Causes for Rejection: Clotted specimen, insufficient specimen volume, mislabeled or unlabeled specimen. Availability: 24/7 Time Required for Processing: 1- 2 hours Hemogram see Complete Blood Count Hematocrit - Peripheral Blood General Use: Evaluation of peripheral blood packed cell volume Test Mnemonic: HCT Request Form: Signed order by physician/Health Professional Affiliate(HPA) Lab Performing Test: Hematology Specimen Required: Whole blood Container Required: Lavender top tube (EDTA); lavender top Microtainer for infants. Volume of Specimen: 4.0 ml of blood (lavender top tube) or 0.75 ml blood (lavender top Microtainer) Minimum Volume of Specimen: 4.0 ml (lavender top tube) or 0.50 ml (lavender top Microtainer) Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: 24 hours, routine and STAT Time Required for Processing: Stat -30 minutes; routine-same day. Reference Range: See printed report for reference ranges by age and gender. Hemoglobin-Peripheral Blood General Use: Evaluation of peripheral blood hemoglobin level Test Mnemonic: HGB Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood (EDTA) Container Required: Lavender top tube (EDTA); lavender top Microtainer for infants Volume of Specimen: 5.0 ml of blood (lavender top tube) or 0.75 ml blood (lavender to Microtainer) Minimum Volume of Specimen: 2.0 ml (lavender top tube) or 0.50 ml blood (lavender top Microtainer) Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen Availability: 24 hours, routine and STAT. Time Required Routinely for Processing: Stat:30 minutes; Routine: same day. Reference Range: See printed report for reference ranges by age and gender. Hemogram see Complete Blood Count Iron Stain, Bone Marrow - see Bone Marrow Kleihauer-Betke Fetal Hgb Stain - see Fetal Hemoglobin Stain Malaria Smear General Use: Rapid Screening for Malaria Test Mnemonic: MALSMR Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instruction: Specimen Required: Whole blood Container Required: Lavender top tube (EDTA) Volume of Specimen: 4.0 ml of blood (lavender top tube) Minimum Volume of Specimen: 4.0 ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen Availability: Daily – not STAT Time Required Routinely for Processing: 4 hours Reference Range: Negative. Manual Differential see Differential White Blood Cell Count Nasal Smear for Eosinophils see Eosinophil Smear Platelet Count General Use: Enumeration of platelets Test Mnemonic: PLCT Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Use 21 or 22 gauge needle to obtain specimen; Do not use butterfly needle. If specimen is drawn from an in-dwelling catheter, line must be flushed with saline and the first 10 ml of blood collected must be discarded. Specimen Required: Whole blood. Container Required: Lavender top tube (EDTA). Volume of Specimen: 4.0 ml of whole blood (Lavender top tube). Minimum Volume of Specimen: 2.0 ml Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: 24 hours routine and STAT. Time Required Routinely for Processing: Routine same day; Stat: 30 minutes. Reference Range: See printed report for reference ranges by age and gender. Retic Count see Reticulocyte Count Reticulocyte Count Synonyms: Retic Count General Use: Enumeration of reticulocytes Test Mnemonic: RET Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA). Specimen Required: Whole blood. Container Required: EDTA Lavender top tube or Microtainer. Volume of Specimen: 4.0 ml of blood (lavender top tube) or 0.75 ml blood (lavender top Microtainer). Minimum Volume of Specimen: 2.0 ml (lavender top tube) or 0.50 ml (lavender top Microtainer) Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen. Availability: Routine and STAT. Time Required Routinely for Processing: Stat:30 minutes; Routine: 2hours. Reference Range: See printed report for reference ranges by age and gender. RTC see Reticulocyte Count Sedimentation Rate Synonyms: ESR, Sed Rate General Use: To assess non-specific activity of disease processes Test Mnemonic: ESR Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Draw an extra full lavender top tube if a CBC is not ordered as well Specimen Required: Whole blood Container Required: Black top Vacu-Tech tube (special collection tube) Volume of Specimen: 1.2 ml of blood Minimum Volume of Specimen: 1.2 ml of blood Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen Availability: 24/7 Time Required Routinely for Processing: Stat:1 hour; Routine: same day Reference Range: See printed report for reference ranges by age and gender. Sed Rate see Sedimentation Rate Sickle see Sickle Cell Preparation Sickle Cell see Sickle Cell Preparation Sickle Cell Preparation Synonyms: Sickle Cell; Sickle General Use: Detection of sickling hemoglobins Test Mnemonic: SICKL Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Test cannot be performed on infants Specimen Required: Whole blood Container Required: Lavender top tube (EDTA) Volume of Specimen: 4.0 ml of blood (lavender top tube) Minimum Volume of Specimen: 2.0 ml (lavender top tube) Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen Availability: Tuesday & Friday Reference Range: Negative Spinal Fluid Cell Count see Cerebrospinal Fluid Analysis Sputum for Eosinophils see Eosinophil Smear Synovial Fluid Analysis Synonyms: Synovial fluid cell count General Use: Evaluation of synovial fluid for inflammatory reaction, hemorrhage, or infection. Test Mnemonic: FCT Profile Includes: WBC and RBC enumeration and WBC differential count. Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA). Patient Preparation: Responsibility of physician. Special Instructions: Indicate site of fluid extraction, ie., left knee, right elbow, etc. Specimen Required: Synovial fluid. Container Required: EDTA Lavender top tube. Volume of Specimen: 4.0 ml of synovial fluid Minimum Volume of Specimen: 2.0 ml Causes for Rejection: Clotted specimen, insufficient specimen volume, mislabeled or unlabeled specimen Availability: 24 hours, routine and stat; differential may be left for review on the following morning Time Required Routinely for Processing: 2 hours Reference Range: See printed report for reference ranges by age and gender. WBC see White Blood Cell Count White Blood Cell Count Synonyms: WBC General Use: To determine the total leukocyte count of a peripheral blood specimen Test Mnemonic: WBC Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Whole blood Container Required: Lavender top tube (EDTA) or lavender top Microtainer for infants Volume of Specimen: 4.0 ml of blood (lavender top tube) or 0.75 ml (lavender top Microtainer) Minimum Volume of Specimen: 2.0 ml (lavender top tube) or 0.50 ml (lavender top Microtainer) Causes for Rejection: Clotted or hemolyzed specimen, incorrect specimen volume, mislabeled or unlabeled specimen Availability: 24 hours daily, routine and STAT Time Required Routinely for Processing: Stat: 30 minutes; routine: same day Reference Range: See printed report for reference ranges by age and gender HOME BLOOD DRAWING As a convenience to our homebound patients, we offer a home blood drawing service. We prefer at least one day’s notice prior to drawing blood. The attending physician may request home blood-drawing services by faxing a L&M HOME DRAWING REQUEST FORM. A blank L&M HOME DRAWING REQUEST FORM may be requested by calling the main laboratory (860-4445101 or 860-444-5102). MICROBIOLOGY The Microbiology section is directed by Elise Krejci, M.D. and Managed by Peter Speciale, MHS, PHD, M(ASCP)sm. The Microbiology Manager can be reached at 4420711 x4625. MICROBIOLOGY COVERAGE The following essential services in Microbiology are provided by laboratory personnel on a 24-hour basis, seven days a week. The regular microbiology staff will be on duty Monday through Sunday 7AM - 11 PM. At all other times, requests for service are to be directed to the main laboratory. The services available on a 24-hour basis include: 1. 2. 3. 4. 5. 6. 7. Plating of cultures (CSF as a STAT, others by special request). CSF gram stain (others by special request). Blood culture collection (service provided by the Laboratory at all times). FFN (Fetal Fibronectin) testing Rapid Beta Strep Screen FLU A/B H1N1 by PCR Chlamydia/GC PCR MICROBIOLOGY REQUISITIONING A. For Meditech, the test mnemonic is given. Microbiology procedures must be ordered in the category MIC B. The manual system (back up for Meditech) must be observed in all cases using the Universal Requisition: 1. 2. 3. 4. 5. Use a separate form for each specimen submitted. Indicate the date and time that the specimen is collected. Indicate the clinical diagnosis or impression relevant to the culture if pertinent. Indicate the specimen source. Patient name, date of birth, location, and physician requesting the test must be filled in accurately. 6. All specimen containers must be completely labeled with the patient full name, DOB, date and time of collection and specimen source. 7. All requisitions must be filled out in ink. Patient information should be stamped on the requisition if possible COLLECTION AND TRANSPORT OF MICROBIOLOGY SPECIMENS GENERAL GUIDELINES FOR PROPER SPECIMEN COLLECTION 1. Collect specimens before administering antimicrobial agents when possible. 2. Collect specimens with as little contamination from indigenous organisms as possible to ensure that the sample will be representative of the infected site. 3. Utilize appropriate collection devices. Use sterile equipment and aseptic technique to collect specimens in order to prevent the introduction of microorganisms during invasive procedures. 4. Clearly label the specimen container with the patient's full name and date of birth, date and time of collection, and the specimen source. 5. Collect an adequate amount of specimen. Inadequate amounts of specimen may yield false-negative results. 6. Identify the specimen source and/or specific site correctly so that the proper culture media will be selected during processing in the laboratory. 7. Collect specimens in sturdy, sterile, screw-cap, leakproof containers with lids that do not create an aerosol when opened. Be sure all lids are screwed on tightly! 8. Use appropriate transport systems for special test procedures (example: Genprobe transport tubes for GC and Chlamydia DNA Probe, viral swabs and viral transport media for viral cultures, anaerobic transport systems for anaerobic cultures etc.). Contact the microbiology laboratory before collecting specimens if there is any question 9. Specimens for testing for specific pathogens by molecular amplification methodology e.g. “amplified DNA” or “PCR” should not be opened again, once placed in their container. Any manipulation of the specimen must be performed in the lab biosafety cabinets, using sterile technique. This is to ensure that no other organism DNA, including human enters the specimen container. 10. All specimens must be accompanied by a Meditech requisition (or a Universal requisition as Meditech backup). A separate requisition must be submitted for each test requested. The requisition must include: a. b. c. d. e. f. g. h. the patient's full name date of birth the patient's location the ordering physician the source and/or specific site of the specimen the type of examination requested the diagnosis (if available) the date and time of collection GENERAL GUIDELINES FOR PROPER SPECIMEN TRANSPORT All specimens should be transported to the Microbiology Laboratory promptly (within 1 to 2 hours) to ensure the survival and isolation of fastidious organisms, and to prevent overgrowth by more hardy bacteria in order to provide a more accurate diagnosis of the infectious disease process. Certain specimens may have different time restrictions and these are noted in the specific listings. Routine cultures must be received in the Microbiology Laboratory by 10:00 PM to allow time for processing. ALTERNATIVES TO PROMPT DELIVERY 1. Refrigerate most specimens at 2 to 8 degrees C. The following are exceptions: a. If blood cultures are not delivered to the laboratory immediately upon collection they should remain at room temperature until delivery. b. Specimens that may harbor temperature-sensitive organisms such as Neisseria species should be left at room temperature. Do not refrigerate genital specimens! c. For anaerobic specimens, the use of an anaerobic transport system is mandatory. A regular culturette will not ensure the viability of fastidious anaerobes. Do not refrigerate anaerobic specimens! d. Stool specimens should be received within 2 hours of their collection; some pathogens may begin to die off after the first two hours. Specimens should be refrigerated if there will be a delay in transport to the laboratory. e. For swab cultures, a Culturette type collection/transport system should be used - be sure to crush the ampule of holding media if the system has one. Dry swabs are not acceptable for culture. REJECTION OF SPECIMENS Specimens will be rejected for the following reasons: 1. Mislabeled or unlabeled specimens and incomplete labeled specimens. 2. Specimens with insufficient quantity. 3. Specimens which have leaked from their container or are received with the container open. 4. Improper collection or transport devices. 5. Improperly stored specimens. 6. Specimens received after prolonged delay from time of collection. In general any specimen which is received greater than 24 hours after collection will be rejected. 7. Specimens other than stool which are received for culture in unsterile containers. 8. Sputum received as obvious saliva as determined by gross examination or gram stain. 9. Material received for anaerobic culture in a non-anaerobic collection tube. The culturette system will not ensure the viability of all anaerobes and is not acceptable for an anaerobic culture. Sputum, urine or cervical specimens received for anaerobic culture will be rejected since they are inappropriate sources for anaerobic culture. 10. Duplicate specimens will be rejected unless there is some indication on the requisition of anatomic or timing differences. Physician orders for cultures must be specific. The appropriate nursing station, clinic or physician will be notified by phone prior to the disposal of an unsatisfactory specimen and a repeat specimen will be requested. If the physician, for whatever reason, insists that the results of an improperly selected, collected, or transported specimen be reported, the Microbiology Laboratory will include in the report a statement explaining the potential compromised nature of the results. SPECIMEN COLLECTION A. Urine Cultures 1. Specimens for routine urine culture must be refrigerated after collection. They will be screened for fast growing aerobic pathogenic bacteria and Candida species. The following types of organisms are examples of those not isolated by routine urine culture: Neisseria gonorrhoeae, Leptospira and anaerobic bacteria. These must be requested separately - call Microbiology for specific instructions. 2. Suprapubic puncture or bladder washings are to be collected by the physician so as to avoid contamination with adjacent structures and surfaces. Cultures with any colonies will be identified. Antimicrobial susceptibility tests will be performed if appropriate. 3. Straight Catheterized urine specimens are to be collected by the physician or catheter care team so as to avoid contamination with adjacent structures and surfaces. Pure growth or cultures with 2 or less organisms will be identified and antimicrobial susceptibilities will be performed if appropriate. Cultures with 3 or more organisms will receive rough identification. 4. Mid-stream urine specimens/Foley catheter urine specimens a. Midstream specimens are to be collected by the patient after thorough cleansing of skin with soap and water or wipe provided. Only the middle portion of the voided specimen is to be collected. b. Criteria for organism identification. Organisms occurring in numbers less than 10,000 per ml will not be identified nor will susceptibility tests be performed unless specific instructions to the contrary are noted on the requisition. Organisms occurring in numbers greater than 10,000 per ml will be identified and susceptibility tests will be performed if the numbers of different types of organisms are not suggestive of contamination with mixed enteric and/or skin flora. If three or more different organisms are isolated from an individual specimen, the report will state that these organisms are suggestive of contamination with mixed enteric and/or skin flora and a repeat specimen will be requested. 5. Urine specimens submitted to the laboratory that are not identified by collection method will be worked up according to the mid-stream/foley catheter identification criteria. B. Respiratory Cultures The following collection sites are considered respiratory specimens: nose, nasopharyngeal swabs, throat, sputum, bronchial and tracheal aspirations and mouth. All specimens from these sites will be screened for fast-growing aerobic pathogenic organisms. The following organisms are examples of those not isolated by routine culture: Neisseria gonorrhoeae, Corynebacterium diptheriae, and Bordetella sp. For information on culture of non-routine organisms see the culture listing for the specific organism. 1. Throat specimens a. collection - throat swabs should be collected so as to avoid contamination by mouth and tongue. b. Beta Strep Screens for Group A strep will be screened for only that organism. c. Throat specimens for Neisseria gonorrhoeae will be screened only for that pathogen and must be specifically requested. 2. Nose or nasopharyngeal specimens a. Collection - to be collected so as to avoid contamination by adjacent structures. 3. Sputum specimens a. Collection - to be collected by instructing the patient to remove dentures, rinse mouth, gargle with water and cough deeply, expectorating into appropriate collection container. b. All specimens labeled "sputum" but actually consisting of saliva or upper respiratory secretions will be rejected. Rejection or acceptance will be based on one or both of the following criteria: 1. Gross examination for mucopurulent material. 2. Microscopic examination for mucopurulent material, presence/absence of squamous epithelial cells and presence/absence WBC’s. c. Specimens obtained by transtracheal aspiration, bronchoscopy, or sputum induction procedure will not be subjected to this screening procedure. Use of these collection techniques must be clearly stated on the requisition. Specimens from transtracheal aspiration can be screened for anaerobic pathogens if requested. C. Blood Cultures 1. Collection of specimens - Blood cultures are usually collected by the Laboratory; however, should the physician choose to collect the specimen he/she should contact the laboratory for proper equipment and procedures. The blood culture bottles must be labeled with the patient's name, date of birth, and the date and time of collection. The blood culture collection procedure can also be found in Meditech in the Laboratory section of patient care services. 2. All routine blood cultures are screened for aerobic and anaerobic pathogens by automated Bac-T-Alert methodology. All organisms isolated from blood cultures will be identified, susceptibility tests performed if appropriate. Organisms which are considered likely to be skin contaminants are coagulase negative Staph species , Bacillus sp, Diphtheroid sp, Propionibacterium and Alpha Strep. D. Miscellaneous Cultures 1. Specimens from normally sterile sites such as CSF, bone marrow, surgical specimens, joint fluids, etc., will be cultured for aerobic pathogenic organisms. If an anaerobic organism is suspected two swab specimens or adequate volume should be submitted for both aerobic and anaerobic culture and transported in the appropriate container. See the specific Anaerobic Culture listing for further details. 2. Bone marrow, eye swabs, joint fluids and spinal fluids will be routinely screened for fast-growing aerobic pathogenic organisms in addition to the fastidious species of Haemophilus and Neisseria . 3. Other body fluids and surgical specimens (including tissue) will be cultured for fast-growing aerobic pathogens. 4. Genital specimens are routinely cultured to isolate Neisseria gonorrhoeae (DO NOT REFRIGERATE) , Listeria and to determine the presence of Beta Hemolytic strep, and Staphylococcus aureus. If yeast is suspected a Candida culture should be ordered. If other pathogens are suspected, it should be noted on the order or specifically requested. 5. Specimens from wounds, abscesses, incisions, and pus will be screened for fast-growing aerobic organisms. If an anaerobe is suspected, a specimen must be properly submitted to the laboratory. See the specific Anaerobic Culture listing for further details. E. Stool Cultures 1. Ideally specimens for routine stool culture should not be older than 2 hours (see stool collection/transport guide). They must be properly collected in feces containers and covered. Homemade containers or containers lined with plastic, tissue paper, newspaper, etc. are unacceptable. Stool specimens should not be submitted in a diaper. 2. Rectal swabs for routine culture should not be older than 2 hours. (see stool collection/transport guide) The medium compartment on the swab must be broken. 3. Do not freeze stool specimens. 4. Stools will be routinely screened for Salmonella, Shigella, Campylobacter and E. coli 0157. If other pathogens are suspected, the appropriate test should be ordered so the proper media will be inoculated. 5. For routine culture no more than one specimen should be collected within a 24hour period. One specimen a day for three days may be submitted for optimum diagnosis. F. Anaerobic Culture Specimens 1. Anaerobic Specimens must be collected in a special anaerobic collection/transport tube. 2. Criteria for Rejection - culture sites unacceptable for anaerobic culture: a. b. c. d. e. f. g. Throat or nasopharyngeal swab Sputum or bronchoscopic specimens. Feces or rectal swabs. Mid-void or catheterized urine specimens. Vaginal or cervical swabs. Material from superficial wounds. Material from abdominal wounds obviously contaminated with feces (e.g. open fistula). 3. Handling problems a. Liquid and swab specimens must be transported in anaerobic transport media/container. b. All specimens should be received in the laboratory within 2 hours of collection. DO NOT REFRIGERATE! 4. Unacceptable Specimens a. Any specimens from inappropriate culture sites, improperly handled specimens, or those delayed in transport, are unacceptable for anaerobic culture. G. Viral Cultures Viral cultures are referred to a reference lab and must be placed in appropriate transport medium. IMPORTANT GENERAL REQUIREMENTS FOR VIRAL CULTURES Early Collection of Specimens - Material for virus isolation must be collected within a few days following onset of illness. By 7 days after onset it is generally too late to obtain satisfactory specimens for virologic diagnosis. Identification of Specimens - Clearly label each specimen with patient name, DOB, and date of collection and source. Indicate viral agent suspected and ordered test. Viral transport media is available in the microbiology laboratory. COLLECTIONS OF SPECIMENS FOR VIRAL ISOLATION When to Collect Specimens - Specimens should be collected as soon as possible after onset. How to Collect Specimens - The collection of the following specimens can best be accomplished by: Throat swab - Swab posterior wall of pharynx. Rectal swab - Insert swab 4-6 cm into rectum and rub against wall of mucosa until fecal material is seen to adhere to the swab. Vesicular lesion - Open mature vesicle, collect fluid on swab. Ulcerative lesions can be swabbed directly. Nasal swab - Insert dry swab into nasal passage and allow it to absorb secretions. Conjunctiva - Remove exudate before swabbing conjunctiva. Certain specimens require special handling: Spinal Fluid - Collect 3-5 ml in a sterile screw cap tube. Preferably, The 2nd or 3rd tube collected should be submitted for microbiological analyses. Urine - Collect 10-15 ml of urine in a sterile screw cap tube. (First morning specimens are preferred.) Note: specimens for isolation of cytomegalovirus (CMV) must be refrigerated and transported immediately to the laboratory on wet ice. Monday to Thurs. 7 AM – 10:00pm. Friday specimens must be rec’d by 12 noon..Specimens received Friday pm, Sat. Sun. and holidays will be processed on the next routine day. Autopsy specimens - Small tissue specimens roughly 2 cm square should be collected from areas of probable pathology with a separate sterile instrument for each specimen. Tissue specimens should be submitted in a sterile screw cap tube without preservatives. Tissue specimens that cannot be submitted directly should be frozen at -70 degrees C and submitted on dry ice. H. Parasitology Specimens Specimens for ova and parasites will be sent to a reference laboratory, Monday through Friday from 7:00 AM to 11:am. Any specimens received Friday after 11:00 AM or on weekends or holidays will be placed in a fixative and will be submitted on the next routine day. NOTE: If Cryptosporidium is suspected, Cryptosporidium antigen detection is the preferred test as an Ova and Parasite exam in most cases does not detect this parasite. Criteria for Collection of Stool Specimens: Stool Collection/Transport Guide Specimens should be collected in CLEAN, DRY wide-mouth containers with an appropriate lid forming a tight leak-proof fit. Specimens that are contaminated with urine or water are cause for rejection. Specimens should be transported to the laboratory as soon after collection as possible for optimal organism recovery. The following will serve as a guide when this is not possible. Approximately 5gm or 5ml of specimen per test (additional tests require additional volumes) is adequate unless otherwise specified. TEST: Stool Culture Whole stool/ Rectal swabs TRANSPORT TIME: 2 hours at room temp. Within 24 hours/4 C (refrigerated) INTERVAL: 24 hours Rotavirus 72 hours/4 C (pea sized portion) (Refrigerated) (swab unacceptable) Days 3 – 5 post onset of symptoms C. difficile toxin 24 hours minimum 24 hours/4 C O&P 15gm/15ml <30 minutes room temp 24hrs/4 C Cryptosporidium Antigen 24 hours/4C 24 – 48 hours *See below 2X recommended if 1st Negative and symptoms persist Cyclospora 24hours/ 4C same as O&P Giardia Antigen 24hrs/4 C Occult Blood within 72 hrs Pinworm Exam no time limit but must be collected on pinworm paddle device. 2X recommended if 1st Negative and symptoms persist each bowel movement Recommendation for O&P evaluation A Minimum of three specimens collected every day or every other day but not within the same day should be collected. Six specimens are recommended for the diagnosis of amebiasis. Specimens should be collected during a time frame of no more than ten days. If a series of six specimens is ordered, then they should be submitted within a 14-day period. Cause for rejection: Specimens will be rejected by the lab for determinations; if taken after a barium enema, taken after the administration of castor oil, taken after administration of laxatives, suppositories, or contaminated with urine. I. Additional Information: Special Susceptibility Testing: Requests for special antimicrobial susceptibility testing or for retaining a particular bacterial isolate for additional testing should be made as soon as possible after submission of the culture and before the final report is issued. Most organisms are not routinely held after finalization. (Exception: Blood Culture isolates are routinely retained for 30 days.) Tests other than those listed are often available through a reference laboratory. Please contact the Microbiology Department at ext. 5192 for information. AFB Blood Culture see Culture, Mycobacteria, Blood AFB Smear and Culture, MAV Culture, TB Culture see Culture, Mycobacteria Beta Strep Group A (Rapid Test) Synonyms: 10 Minute Beta Strep Screen General Use: Rule out Beta Strep Group A Test Mnemonic: BSSC Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Throat swab Container Required: Sterile culturette Volume of Specimen: 1 swab Causes for Rejection: Specimen not received in appropriate sterile container Availability: 24 hours daily Time Required Routinely for Processing: Negative & positive results will normally be reported 30 minutes after arrival in the lab Additional Information: Requisition must clearly state "For 10 minute Beta Strep Screen" NOTE: This test is considered presumptive when negative and a 24 hour Beta Strep Screen is recommended for confirmation Reference Range: Negative by Direct (Rapid) Beta Strep screen Beta Strep Screen (24 hour) see Culture, Throat, for Beta Strep Group A Blood Culture for MAV see Culture, Mycobacteria, Blood Blood Culture, Fungus see Culture, Blood Blood Culture, Routine see Culture, Blood C. Difficile Toxin Synonyms: Clostridium Difficile Toxin, Stool for C.diff General Use: To rule out C. difficile infection Test Mnemonic: CDIFF Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Stool Container Required: Sterile cup, stool cup Volume of Specimen: 1-2 ml Collection: Random, no more than one specimen should be submitted. Availability: Performed 24/7. Time Required Routinely for Processing: 1-2 hours Additional information: Test detects toxigenic Cdiff and the epidemic strain 027 . Reference Range: Negative Candida Antigen General Use: To determine diagnosis & prognosis of Candida infection Test Mnemonic: CANAG Lab Performing Test: Sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: 10 cc clotted blood Container Required: red top tube Volume of Specimen: 2 ml serum Availability: Specimens will be processed Mon-Fri 7:00AM-3:30PM Time Required Routinely for Processing: 72 hours Reference Range: Negative Chlamydia PCR General Use: Identification of Chlamydia trachomatis by PCR. NOTE: Culture is the method of choice in cases of suspected sexual abuse, ascending pelvic infections, throat or rectal infections or when determining test of cure. Test Mnemonic: CTPCR Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Vaginal / endocervical or urine Container Required: xpert CT/NG vaginal/endocervical specimen collection kit, for urine use a sterile cup or yellow cap urinalysis tube Volume of Specimen: 1 swab in special transport vial, Urine –Min. 1 ml Causes for Rejection: Specimen not received in appropriate transport media. Inappropriate specimen. Specimen CANNOT be shared with any other tests. Availability: Testing performed 7 days/week ( first shift ONLY) Time Required Routinely for Processing: 2-3 hours Reference Range: Negative Clostridium Difficile Toxin, Stool for C.Diff see C. Difficile Toxin Cryptococcal Antigen, Blood General Use: Aid in the diagnosis and prognosis of cryptococcal infections Test Mnemonic: CRYBLD Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: 10 cc of clotted blood Volume of Specimen: 2 ml serum Availability: 7:00AM-3:00PM Mon-Fri; not Stat Time Required Routinely for Processing: 24 hrs Reference Range: Negative Cryptococcal Antigen, CSF General Use: Aid in the diagnosis and prognosis of cryptococcal infections Test Mnemonic: CRYCSF Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Spinal fluid Container Required: Sterile tube Minimum Volume of Specimen: 2mL Causes for Rejection: Blood in CSF or inadequate volume Availability: 7:00AM-3:00PM Mon-Fri; as a Stat only 3:00PM-11:00PM when indicated by diagnosis (if positive, titer will be done next routine day) Time Required Routinely for Processing: 24 hrs Reference Range: Negative Cryptococcus Stain see India Ink Prep Cryptosporidum Antigen General Use: Determine presence or absence of Cryptosporidium as cause of infection. Test Mnemonic: CRYPT Lab Performing Test: Sent to reference Lab. Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Stool Container Required: Plastic urine or stool container Minimum Volume of Specimen: 5 ml Causes for Rejection: Insufficient quantity, contamination with urine, mineral oil. etc.; less than 24 hours between duplicate specimens. Availability: Specimens will be processed Mon-thurs. 7:00AM-3:30PM Specimens received after noon on Friday, Sat. Sun., or holidays will be processed on the next routine day. Time Required Routinely for Processing: results available within 72 hrs. Reference Range: Negative Culture, Anaerobic General Use: To identify infection due to anaerobic organisms Test Mnemonic: ANER Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Indicate type of specimen & site; see general information for unacceptable specimens Specimen Required: Swab of wound, drainage, etc., biopsy material, pus. Specimen for anaerobic culture should be accompanied by a specimen for aerobic culture from the same site. Container Required: Anaerobic transport tube (available from Microbiology Laboratory) Volume of Specimen: Small piece of tissue from biopsy site, 1 swab, 1-10 ml of fluid, etc. Causes for Rejection: Specimen not received in appropriate transport tube or vial. Refrigerated specimens (refrigeration inhibits viability of anaerobic organisms). Specimens from sites which have anaerobic bacteria as normal flora will routinely be rejected, e.g., throat, rectal swabs, cervical-vaginal mucosal swabs, sputums. etc. Availability: Cultures will be processed daily 7:00AM - 10:00PM Time Required Routinely for Processing: Cultures showing no bacterial growth will be reported after 5 days. Complete reports of cultures with anaerobic bacteria may take as long as 10 days to 2 weeks after receipt of culture depending upon the nature of the organisms isolated. Reference Range: No growth of anaerobes from normally sterile sites. Culture, Candida Synonym: Yeast Culture, Monilia culture General Use: To support or rule out Candida (yeast) infection Test Mnemonic: CANDC Test Includes: Screening for Candida species Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Swab of wound, drainage, genital area, etc Container Required: Sterile culturette Volume of Specimen: 1 swab Causes for Rejection: Received in improper container Availability: Specimens will be processed daily 7:00AM-10:00PM Time Required Routinely for Processing: Cultures will be held 3 days before going out as negative; additional time may be needed for identification if growth of yeast occurs Reference Range: No growth Culture, Anal/Rectal for GC General Use: Support diagnosis of Neisseria gonorrhea as cause of infection Test Mnemonic: ANALGC Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Deliver to lab immediately; do not refrigerate. Specimen Required: Anal swab/Rectal swab Container Required: Sterile culturette Volume of Specimen: 1 swab Causes for Rejection: Refrigeration Availability: Specimens will be processed daily 7:00AM-10:00PM Time Required Routinely for Processing: Cultures with no growth will be reported after 48 hours. Reference Range: No Growth of Neisseria gonorrhoeae Culture, Blood – Bacterial Synonyms: Blood Culture, Routine; Blood Culture Fungal General Use: Isolate and identify causative agent of infection. If a fungal isolate is suspected, the microbiology lab MUST be notified. Test Mnemonic: BLC Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: After selecting a vein, the arm should be wiped thoroughly with 70% alcohol and allowed to dry. It is then wiped with an iodophore swab (or 2% tincture of iodine) and allowed to dry for 1 minute. The venipuncture site must not be palpated after the above steps. 10 ml of venous blood is then drawn into two blood culture bottles which have been properly labeled, exercising extreme caution not to inject air into the anaerobic bottle. Special Instructions: Should be drawn prior to administration of antibiotics and before expected temperature rise. Specimen Required: Blood Container Required: 2 special blood collection bottles (aerobic and anaerobic) Volume of Specimen: 10 ml (5ml in each bottle) - 20 ml (10 ml in each bottle) Minimum Volume of Specimen: 2 ml (1 ml in each bottle) Causes for Rejection: Insufficient volume Availability: Specimens will be processed daily 7:00AM-11:00PM and drawn as a Stat 24 hours daily Time Required Routinely for Processing: Routine Blood Cultures are held for 5 days if negative; Fungal Blood Cultures are held 21 days if negative. Reference Range: No Growth Culture, Body Fluid General Use: Determine causative agent of infection Test Mnemonic: FLDC Test Includes: A gram stain if sufficient quantity of fluid is received and not collected by swab. Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Sterile preparation of the aspiration site Special Instructions: Indicate type of body fluid Specimen Required: Sterile aspirated body fluid Container Required: Sterile tube or culturette - do not submit in vacutainer tubes . Volume of Specimen: 2.0 ml; 1 swab Causes for Rejection: Specimen not received in appropriate sterile container Availability: Specimens will be processed daily 7:00AM-11:00PM Time Required Routinely for Processing: Preliminary reports available at 24 hours; cultures with no growth will be reported after 5 days. Reference Range: No growth Culture, Bone General Use: To determine presence of infection Test Mnemonic: BONC Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Bone Container Required: Sterile cup Volume of Specimen: As much as can be obtained Availability: Specimens will be processed daily 7:00AM-11:00PM Time Required Routinely for Processing: Specimens will be held for 5 days before reporting as negative Reference Range: No growth Culture, Bone Marrow General Use: To support or rule out infection Test Mnemonic: BMC Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: As required for Bone Marrow Aspiration Special Instructions: Media may be obtained in Microbiology Lab Specimen Required: Bone Marrow Container Required: Planted on proper media at bedside (Thio Broth) Volume of Specimen: 1 ml Availability: Specimens will be processed daily 7:00AM-3:30PM Time Required Routinely for Processing: Specimens will be held for 5 days before reporting as negative Reference Range: No growth Culture, Bone Marrow for AFB see Culture, Mycobacteria, Bone Marrow Culture, Bronchial Washing General Use: Determine causative agent of infection Test Mnemonic: BRWC Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Bronchial washings, bronchial brushings, bronchial lavage Container Required: Sterile cup or sterile bronchscopy tube (be sure to keep from leaking) Minimum Volume of Specimen: 2 ml Causes for Rejection: Specimen not received in appropriate sterile container. Availability: Specimens will be processed daily 7:00AM-10:00PM Time Required Routinely for Processing: Preliminary reports available at 24 hours; Cultures with no growth will be reported after 48 hours; reports on specimens from which pathogens are isolated require a minimum of 48 hours for completion. Reference Range: No growth or growth consistent with normal respiratory flora Culture, Catheter Tip General Use: To determine causative agent of infection Test Mnemonic: CTC Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Catheter tip (must specify type of catheter tip) Container Required: Sterile tube Volume of Specimen: 1-5 cm catheter tip Availability: Specimens will be processed daily 7:00AM-10:00PM Time Required Routinely for Processing: Preliminary reports available at 24 hours; cultures with no growth will be reported after 3 days Reference Range: No growth Culture, CMV General Use: To support or rule out CMV infection Synonyms: Culture, Cytomegalovirus Test Mnemonic: CMVC Test Includes: CMV early antigen screen & CMV cell culture Lab Performing Test: Sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Urine must be received in early AM on ice; must be transported to reference lab (on ice) same day as collected. Blood must be put on ice after collection. Specimen Required: Urine, heparinized blood; contact Micro for specific requirements Container Required: Sterile cup; green top tube; call Micro for other requirements Volume of Specimen: 2 ml urine; 10 cc blood; call Micro for other requirements Causes for Rejection: Specimen not received on ice; specimen received after courier pick up Availability: Specimens will be processed Mon-thurs. 7:00AM-3:30PM Specimens received after noon on Friday, Sat. Sun., or holidays will be processed on the next routine day. Time Required Routinely for Processing: Early antigen available in 72 hours; culture held 8 weeks if negative Reference Range: Negative Culture, CSF for AFB see Culture, Mycobacteria, CSF Culture, CSF & Gram Stain General Use: Determine causative agent of infection. Test Mnemonic: CSFC Test Includes: CSF culture as well as a gram stain on all specimens submitted Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Sterile preparation of the aspiration site Specimen Required: Spinal fluid, shunt fluid Container Required: Sterile tube Volume of Specimen: 2-5 ml Minimum Volume of Specimen: 1 ml Causes for Rejection: Specimen not received in appropriate sterile container. Availability: Specimens will be processed daily 7:00AM-11:00PM and planted as a STAT culture 11:00PM-7:00AM (culture will be planted and gram stain will be made and stained.) Time Required Routinely for Processing: Preliminary reports available at 24 hours; Cultures with no growth will be reported after 72 hours; reports of cultures from which pathogens are isolated may require additional time for completion. Reference Range: No growth Culture, Cytomegalovirus see Culture, CMV Culture, Ear General Use: To determine causative agent of infection Test Mnemonic: EARC Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Ear swab Container Required: Sterile culturette Volume of Specimen: 1 swab Availability: Specimens will be processed daily 7:00AM-10:00PM Time Required Routinely for Processing: Preliminary reports available at 24 hours; Cultures with no growth will be reported after 72 hours Reference Range: No growth Culture, Eye General Use: Determine causative agent of infection Test Mnemonic: EYEC Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Eye swabbing, conjunctiva Special Instructions: DO NOT REFRIGERATE Container Required: Sterile culturette Volume of Specimen: 1 swab Availability: Specimens will be processed daily 7:00AM-10:00PM Time Required Routinely for Processing: Preliminary reports available at 24 hours; Cultures with no growth will be reported after 72 hours Reference Range: No growth Culture, Fungus General Use: To support or rule out fungal infection Test Mnemonic: FUNG Test Includes: Isolation and identification of yeasts and pathogenic fungi Lab Performing Test: Sent to Reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Same as for routine culture of specific site Specimen Required: Swab of wound, drainage, biopsy material, fluid, pus, etc. Container Required: Sterile culturette; sterile cup or tube Volume of Specimen: 1 swab, 2-3 ml fluid Causes for Rejection: Insufficient specimen volume, received in improper container Availability: Specimens will be processed Mon-thurs. 7:00AM-3:30PM Specimens received after noon on Friday, Sat. Sun., or holidays will be processed on the next routine day. Time Required Routinely for Processing: Cultures will be held 15 days before going out as negative; growth of fungus may take additional time for identification. Note: some fungus species may take as long as one month to grow; if dermatophytes are suspected the lab should be notified Reference Range: No growth Culture, Fungus, Bone Marrow General Use: To support or rule out fungal infection Test Mnemonic: FUNG Lab Performing Test: Sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: As required for bone marrow aspiration Special Instructions: Media may be obtained in Microbiology Lab Specimen Required: Bone marrow Container Required: Planted on proper media at bedside (SAB agar slants) Volume of Specimen: 2 ml Availability: Specimens will be processed Mon-thurs. 7:00AM-3:30PM Specimens received after noon on Friday, Sat. Sun., or holidays will be processed on the next routine day. Time Required Routinely for Processing: Specimens will be held 15 days before going out as negative; growth of fungus may take additional time for identification Reference Range: No growth Culture, Fungus, Skin Synonyms: Skin scrapings for fungus General Use: To support or rule out fungal infection Test Mnemonic: FUNG Lab Performing Test: Sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Wash area with alcohol swab. Allow to dry and scrape with blade or edge of glass slide Specimen Required: Skin scrapings, exudates, nail clippings, whole nail, debris under nail Container Required: Sterile petri dish Volume of Specimen: As much as possible Causes for Rejection: Insufficient specimen volume Availability: Specimens will be processed Mon-thurs. 7:00AM-3:30PM Specimens received after noon on Friday, Sat. Sun., or holidays will be processed on the next routine day. Time Required Routinely for Processing: 21 days. Growth of fungus may take additional time. Reference Range: No growth Culture, Genital Sites General Use: Determine causative agent of infection Test Mnemonic: GENC Test Includes: Screening for Beta Strep Group B, Listeria, Neisseria gonorrhoeae and predominating amounts of Gardnerella vaginalis and candida species unless otherwise indicated. Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: DO NOT REFRIGERATE Specimen Required: Swab of genital area, prostatic fluid, placental swab, etc. Container Required: Sterile culturette or sterile tube Volume of Specimen: 1 swab or 2 ml fluid Causes for Rejection: Specimen not received in appropriate sterile container; refrigerated specimens. Availability: Specimens will be processed daily 7:00AM-10:00PM Time Required Routinely for Processing: Preliminary reports available at 24 hours; cultures with no growth will be reported after 72 hours; reports of cultures from which pathogens are isolated may require additional time for completion. Reference Range: No growth or normal genital flora depending on site Culture, Legionella Synonyms: Legionella Culture General Use: To establish Legionella species as cause of infection Test Mnemonic: LEGC Lab Performing Test: Sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Sputum, bronchial washings Container Required: Sterile cup Volume of Specimen: 2 ml Availability: Specimens will be processed Mon-Thur. 7:00AM-3:00PM. Specimens received after 10:00am on Friday or Saturday, Sunday or holidays will be processed on the next routine day. Time Required Routinely for Processing: 2 weeks Reference Range: Negative Culture, Mycobacteria Synonyms: AFB Smear and Culture, MAV Culture, TB Culture General Use: Determine presence or absence of Mycobacteria Test Mnemonic: AFB Test Includes: DNA probe identification of mycobacteria when present Lab Performing Test: Microbiology to perform concentrated smear ony as stat. All others sent to reference lab. Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Indicate type of specimen on requisition. If gastric aspirate is to be collected, the Microbiology Department must be notified before collection. Specimen Required: Sputum, fasting gastric aspirate, induced sputum, Bronchial washing, wound, body fluid, stool, etc. Container Required: Sterile cup Volume of Specimen: 5 - 10 ml Minimum Volume of Specimen: 5 ml Causes for Rejection: Specimen consisting entirely of saliva, insufficient specimen volume Availability: Specimens processed daily 7:00AM-10:00PM.. Concentrated AFB smears will be performed inhouse if clinically indicated (Inpatient). Otherwise sent to reference lab. Time Required Routinely for Processing: Cultures are held 6 weeks for Negative. Reference Range: No Growth of Mycobacteria Culture, Mycobacteria, Blood Synonyms: Blood Culture for AFB; Blood Culture for MAV; AFB Blood Culture; MAV Blood Culture General Use: To support the diagnosis of AFB Test Mnemonic: BLAFB Test Includes: DNA probe identification of Mycobacteria when present Lab Performing Test: Microbiology (initial incubation). If positive sent to reference lab. Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Bottles for drawing specimens may be obtained in Microbiology Specimen Required: Blood Container Required: MB/Bact Blood culture Bottle Volume of Specimen: 5 ml Collection: Timed; usually drawn x2 Causes for Rejection: Insufficient volume; improper container Availability: 7:00AM-11:00PM. for routine processing; will be drawn 24 hours daily by request. Time Required Routinely for Processing: 6 weeks Reference Range: No growth of Mycobacteria Culture, Mycobacteria, Bone Marrow Synonyms: Culture, Bone Marrow for AFB General Use: Determine presence or absence of Mycobacteria Test Mnemonic: AFB Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: As required for bone marrow aspiration Special Instructions: Media may be obtained in Microbiology Lab Specimen Required: Bone Marrow Container Required: Planted on proper media at bedside (LJ slant) Volume of Specimen: 2 ml Availability: Specimen will be processed daily 7:00AM-3:30PM Time Required Routinely for Processing: 6 weeks Reference Range: No Growth of Mycobacteria Culture, Mycobacteria, CSF Synonyms: Culture, CSF for AFB General Use: Determine presence or absence of Mycobacteria Test Mnemonic: AFB Lab Performing Test: To reference lab. Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Usual sterile preparation Special Instructions: Indicate "CSF" as source Specimen Required: Cerebrospinal fluid Container Required: Sterile tube Volume of Specimen: 1-10 ml Minimum Volume of Specimen: 1 ml Causes for Rejection: Insufficient specimen volume Availability: Not Stat, specimens processed daily 7:00AM-11:00PM Time Required Routinely for Processing: 6 weeks . Direct smear available in 24 hours Reference Range: No Growth of Mycobacteria Culture, Mycoplasma Pnemoniae General Use: To determine causative agent of infection Test Mnemonic: MYCUL Test Includes: Culture for Mycoplasma pneumoniae Lab Performing Test: Sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Must be kept refrigerated until receipt and frozen if > 24 hour delay in transport Specimen Required: Respiratory – throat, sputum. Container Required: Special holding media available in Microbiology Volume of Specimen: 1 swab Causes for Rejection: Received in inappropriate container; not refrigerated Availability: Specimens will be processed Mon-thurs. 7:00AM-3:30PM Specimens received after noon on Friday or Sat. Sun., or holidays will be processed on the next routine day. Time Required Routinely for Processing: 8 weeks Reference Range: Negative Culture, Mycoplasma/Ureaplasma General Use: To determine causative agent of infection Test Mnemonic: MYURC Test Includes: Culture for Mycoplasma hominis & Ureaplasma urealyticum Lab Performing Test: Sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Must be kept refrigerated until receipt and frozen if >24 hour delay in transport. Specimen Required: urogenital, respiratory, sterile body fluids, tissue, wounds Container Required: Special holding media available in Microbiology Volume of Specimen: 1 swab Availability: Specimens will be processed Mon-thurs. 7:00AM-3:30PM Specimens received after noon on Friday or Sat. Sun., or holidays will be processed on the next routine day. Time Required Routinely for Processing: 6 weeks Reference Range: Negative Culture, Nose General Use: Determine causative agent of infection Test Mnemonic: NOSC Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Nose swab Container Required: Sterile culturette Volume of Specimen: 1 swab Causes for Rejection: Specimen not received in appropriate sterile culturette. Availability: Specimens will be processed daily 7:00AM-10:00PM Time Required Routinely for Processing: Preliminary reports available at 24 hours; Cultures with no growth will be reported after 48 hrs. Reference Range: Alpha strep, Diphtheroids, Neisseria sp. Staphylococcus epidermidis are all normal flora Culture, Pertussis Synonyms: Whooping Cough General Use: Used to support the diagnosis of Bordetella pertussis (Whooping Cough) Test Mnemonic: PERTC Test Includes: Culture for B.pertussis Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Nasopharyngeal swab from Pertussis collection kit; transport to lab immediately. Container Required: Pertussis kit suplied by lab Volume of Specimen: 1 swab from kit Availability: Specimens will be processed daily 7:00AM to 10:00PM. Time Required Routinely for Processing: If received Mon-Fri by noon, culture held 5 days. Reference Range: Negative Culture, Skin General Use: To determine causative agent of infection Test Mnemonic: SKIN Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Usual sterile preparation Specimen Required: Swab of skin; indicate whether deep specimen or superficial Container Required: Sterile culturette Volume of Specimen: 1 swab Causes for Rejection: Specimen not received in appropriate sterile container Availability: Specimens will be processed daily 7:00AM-10:00PM Time Required Routinely for Processing: Preliminary reports available at 24 hours; Cultures with no growth will be reported after 48 hours. Reference Range: No growth Culture, Sputum and Gram Stain General Use: Determine causative agent of infection Test Mnemonic: SPUC Test Includes: Sputum culture as well as a gram stain on all specimens submitted Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: The patient should be instructed to remove dentures, rinse mouth and gargle with water. The patient should then be instructed to cough deeply and expectorate sputum into proper container. Specimen Required: Sputum, first morning specimen preferred Container Required: Sterile cup Minimum Volume of Specimen: 2 ml Causes for Rejection: Specimen not received in appropriate sterile container or received in tissue paper; contamination with mouthwash. If specimen is macroscopically/ microscopically consistent with saliva it will be rejected and a new specimen will be requested. Availability: Specimens will be processed daily 7:00AM-10:00PM Time Required Routinely for Processing: Preliminary reports available at 24 hours; cultures with no growth will be finaled after 48 hours. Reference Range: Normal upper respiratory flora Culture, Stool Synonyms: Stool for Enteric Pathogens General Use: Screen for bacterial pathogens in the stool Test Mnemonic: STLC Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Rectal swab or fresh random stool; ideally stool should be received within 2 hours of passage Container Required: Sterile culturette or stool cup Volume of Specimen: 10 ml Minimum Volume of Specimen: 1 ml Causes for Rejection: Rectal swabs in which the medium compartment is not broken; improper container, insufficient specimen volume, specimen contaminated with urine and/or water, specimen containing interfering substances, e.g. castor oil, bismuth, metamucil, barium; specimens greater than 24 hrs old Availability: Specimens will be processed daily 7:00AM-10:00PM Time Required Routinely for Processing: 48 hrs if negative. Additional Information: A routine stool culture includes screening for Salmonella, Shigella, Campylobacter & E coli 0157 only. If other enteric pathogens such as Yersinia or Vibrio species are suspected, testing must be specifically requested. Reference Range: No growth of enteric pathogens Culture, Throat (Comprehensive) General Use: Determine causative agent of infection Test Mnemonic: THRC Test Includes: Screening for respiratory pathogens Group A Strep, Haemophilus influenzae and Streptococcus Pneumoniae. Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Avoid contamination with tongue or sides of mouth Specimen Required: Throat swab Container Required: Sterile culturette Volume of Specimen: 1 swab Causes for Rejection: Specimen not received in appropriate sterile container Availability: Specimens will be processed daily 7:00AM to 10:00PM. Time Required Routinely for Processing: up to 48 hours for a negative result. Reference Range: Normal upper respiratory flora Culture, Throat Beta Strep Group A Synonyms: Beta Strep Screen General Use: Rule out Beta Strep Grp. A Test Mnemonic: BSSC Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Throat swab Container Required: Sterile culturette Volume of Specimen: 1 swab Causes for Rejection: Specimen not received in appropriate sterile container Availability: Specimens will be processed daily 7:00AM to 10:00PM. Time Required Routinely for Processing: up to 48 hours for a negative result. A 10 MINUTE RAPID RESULT IS AVAILABLE 24 HOURS DAILY, and must be clearly stated on the requisition as “10 minute Beta Strep”. Reference Range: No Beta strep isolated or negative by rapid screen Culture, Throat, for C. Diphtheria General Use: Rule out C. diphtheria as causative agent of infection Test Mnemonic: MISC Lab Performing Test: CT State Laboratory Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Contact Microbiology and Infection control prior to collection. The preferred diagnostic test is to send acute and convalescent serum for diphtheria antibody titers to the State Lab. Secondary testing may include histological and microbiological testing of the pseudomembrane. Culture, Throat, for Neisseria Gonorrhoeae Synonyms: G.C. Culture, Throat General Use: Rule out Neisseria gonorrhoeae as causative agent of infection Test Mnemonic: THRC Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Transport specimen immediately; hand carry to laboratory; do not refrigerate. Additional description field must indicate "for Neisseria Gonorrhoeae"; DNA Probe testing is NOT approved for use on throat cultures Specimen Required: Throat swab Container Required: Sterile culturette Volume of Specimen: 1 swab Causes for Rejection: Specimen not received in appropriate sterile container; refrigeration of specimen Availability: Specimens will be processed daily 7:00AM to 10:00PM Time Required Routinely for Processing: 48 hours for negative Reference Range: No Neisseria gonorrhoeae isolated Culture, Tissue General Use: To determine cause of infection Test Mnemonic: TISC Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Hip capsule, knee capsule, lymph node, other body tissues Container Required: Sterile cup, tube or petri dish hand delivered to the lab, must be kept upright to keep from leaking Volume of Specimen: Amount of tissue available depending on source Causes for Rejection: Specimen leaking into bag (since blood may leak back into petri dish cultures may be contaminated) Availability: Specimens will be processed daily 7:00AM-10:00PM Time Required Routinely for Processing: Preliminary results available after 24 hours. Negative cultures are held for 5 days Reference Range: No growth Culture, Urine, Catheterized General Use: To determine causative agent of urinary tract infection. Test Mnemonic: URNC Test Includes: Colony count Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: As per Nursing Procedure Manual for catheterization. Special Instructions: Specimen must be refrigerated if not immediately taken to laboratory to be processed. Additional description field must indicate type of catheter collection method ie; “Straight Catheter” or “Foley Catheter”. Specimen Required: Catheterized Urine Specimen Container Required: Sterile tube or sterile urine container Minimum Volume of Specimen: 2 ml Causes for Rejection: Specimen not received in appropriate sterile container, refrigerated specimen older than 24 hours. Non-refrigerated specimen older than 2 hours. Availability: Specimens will be processed daily 7:00AM-10:00PM Time Required Routinely for Processing: Preliminary reports available at 24 hours; cultures with no growth will be reported after 24 hours. Cultures with significant growth will require a minimum 48 hours for completion. Reference Range: No Growth Culture, Urine Midvoid Specimen General Use: To determine causative agent of urinary tract infection Test Mnemonic: URNC Test Includes: Colony count Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Thoroughly instruct patient for proper collection of midvoid urine specimen to avoid contamination with skin flora. Refer to Nursing Procedures for further instructions. Special Instructions: Specimen must be refrigerated if not immediately taken to laboratory to be processed. Additional description field should indicate, "clean voided" Specimen Required: Clean void urine specimen Container Required: Sterile tube or sterile urine container Minimum Volume of Specimen: 2 ml Causes for Rejection: Specimen not received in appropriate sterile container; refrigerated specimen older than 24 hours; non-refrigerated specimen older than 2 hours Availability: Specimens will be processed daily 7:00AM-11:00PM Time Required Routinely for Processing: Preliminary reports available at 24 hours; cultures with no growth will be finaled after a full 24 hours. Cultures with growth require a minimum of 48 hours to completion Reference Range: No growth Culture, Urine, Suprapubic Puncture General Use: To determine causative agent of urinary tract infection. Test Mnemonic: URNC Test Includes: Colony count Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Specimen to be obtained by suprapubic puncture so as to avoid any contamination with normal skin flora. Special Instructions: Specimen should be immediately taken to laboratory to be processed. Additional description field must indicate "suprapubic puncture" Specimen Required: Urine obtained by suprapubic puncture Container Required: Sterile tube or sterile urine container Minimum Volume of Specimen: 2 ml Causes for Rejection: Specimen not received in appropriate sterile container; refrigerated specimen older than 24 hours; non-refrigerated specimen older than 2 hours Availability: Specimens will be processed daily 7:00AM-10:00PM Time Required Routinely for Processing: : Preliminary reports available at 24 hours; cultures with no growth will be finaled after a full 24 hours. Cultures with growth require a minimum of 48 hours to completion Reference Range: No growth Culture, Wound, Miscellaneous Sites General Use: Determine causative agent of infection. Test Mnemonic: WDC Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Usual sterile preparation Special Instructions: Indicate type of specimen & site Specimen Required: Swab of wound, drainage, etc.; biopsy material; pus Container Required: Sterile tube, sterile culturette Volume of Specimen: 2.0 ml, 1 swab Causes for Rejection: Specimen not received in appropriate sterile container Availability: Specimens will be processed daily 7:00AM-10:00PM Time Required Routinely for Processing: Preliminary reports available at 24 hours; cultures with no growth will be reported after 72 hours; reports on specimens from which pathogens are isolated require a minimum of 48 hours for completion. Reference Range: No growth Cyclospora Stain General Use: To rule out infection due to Cyclospora Test Mnemonic: CYCLO Lab Performing Test: to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Stool Container Required: Plastic urine or stool container Minimum Volume of Specimen: 5 ml Causes for Rejection: Insufficient quantity; contamination with urine, mineral oil, etc.; less than 24 hours between duplicate specimens Availability: Specimens will be processed Mon-thurs. 7:00AM-3:30PM Specimens received after noon on Friday, Sat. Sun., or holidays will be processed on the next routine day. Time Required Routinely for Processing: Mon - Friday by 11:00AM will be completed that same day. Reference Range: Negative PCR for Neisseria Gonorrhoeae Synonyms: GC PCR General Use: Identification of Neisseria gonorrhoeae by DNA Probe. NOTE: Culture is the method of choice in cases of suspected sexual abuse, ascending pelvic infections, throat or rectal infections or when determining test of cure. Test Mnemonic: GCPCR Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Genital swab Container Required: xpert CT/GC media (available in Microbiology) Volume of Specimen: 1 swab in special transport vial Causes for Rejection: Specimen not received in appropriate transport media; sources not appropriate for this test. Availability: Testing performed 7 days/week ( first shift ONLY) Time Required Routinely for Processing: 2-3 hours Reference Range: Negative Enterovirus PCR (CSF) General Use: To screen for Enterovirus CSF Test Mnemonic: ENVCSF Test Includes: Screening for ENTEROVIRUS ONLY Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: NASAL swab Container Required: Cepheid Copan Red top swab Volume of Specimen: 1 swab Causes for Rejection: inappropriate swab Availability: 24/7 Time Required Routinely for Processing: 2-3 hours Additional Information: Presumptive positive cultures will be called as soon as possible Reference Range: Negative Fetal Fibronectin Test Synonyms: FFN General Use: To predict the risk for preterm delivery Test Mnemonic: FFN Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: As for a sterile speculum examination Special Instructions: Specimens for FFN should be collected prior to a digital cervical exam and before collection of any culture specimens Specimen Required: Swab of the posterior fornix of the vagina Container Required: Special FFN swab and holding media ONLY Volume of Specimen: 1 FFN swab (available in Microbiology) Collection: by physician Causes for Rejection: Inappropriate container; delay in transport to lab Availability: 24 hours daily Time Required Routinely for Processing: 2 hours Limitations: Vaginal bleeding may contribute to difficulty in interpreting the FFN result Additional Information: Specimens must be delivered to Microbiology immediately after collection. If there will be any delay in transport, the specimen should be refrigerated. Transport from outside the hospital should be on an ice pack. Fungal Wet Prep see KOH Prep GBS Screen see Group B Strep Screen G.C. Culture, Throat see Culture, Throat, for Neisseria Gonorrhoeae GC DNA Probe see DNA Probe for Neisseria Gonorrhoeae Giardia Antigen General Use: Determine presence or absence of Giardia lamblia as cause of infection. Test Mnemonic: GLAG Lab Performing Test: To reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Stool Container Required: Sterile cup, stool container Volume of Specimen: 5-10 ml Minimum Volume of Specimen: 5 ml Causes for Rejection: Received older than 24 hrs, received in container lined with tissue or newspaper Availability: Specimens will be processed Mon-thurs. 7:00AM-3:30PM Specimens received after noon on Friday, Sat. Sun., or holidays will be processed on the next routine day. Time Required Routinely for Processing: 72 hours Reference Range: Negative Gram Stain General Use: To determine presence or absence of bacteria, yeast, neutrophils and epithelial cells. Test Mnemonic: GRAM Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Same as for routine culture of specific site. Specimen Required: Same specimen as for routine culture of the specific site. Container Required: Sterile tube, sterile culturette Minimum Volume of Specimen: 1 ml, or one swab Causes for Rejection: Specimen not received in appropriate sterile container. Stool specimens are not appropriate for gram staining. See stool for Ploys. Availability: Specimens will be processed daily 7:00AM-10:00PM. Time Required Routinely for Processing: 24 hours Group B Strep Screen (Culture/PCR) Synonyms: GBS Screen General Use: For GBS screening in pregnant women Test Mnemonic: GBS Test Includes: Screening for Beta Strep Group B ONLY Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Collect one or two swabs of vaginal introitus AND anorectum Specimen Required: Vaginal-rectal swabs are the preferred specimen Container Required: sterile culturette Volume of Specimen: 1 or 2 swabs Causes for Rejection: Inappropriate container, improper specimen Availability: Specimens will be processed daily 7:00AM-10:00PM Time Required Routinely for Processing: Cultures are held a total of 72 hours before being reported as negative Additional Information: It is recommended that both vaginal and rectal cultures be taken; the combination can increase sensitivity 5 - 27% over vaginal culture alone. Cervical cultures are not acceptable for GBS screening Reference Range: Negative for Group B Strep India Ink Prep Synonyms: Cryptococcus Stain General Use: Determine the presumptive presence of Cryptococcus sp. Test Mnemonic: INKP Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Same as for routine culture of specific site Specimen Required: Appropriate specimen is the same as for culture of a given site. Most commonly done on CSF Container Required: Sterile tube Minimum Volume of Specimen: 1 ml Causes for Rejection: Insufficient specimen volume Availability: 7:00AM to 10:00PM daily Time Required Routinely for Processing: 2 hours Stat; next routine working day if received after 10:00PM Additional information: Cryptococcal Antigen detection test is a more sensitive and specific test and is recommended instead of the India Ink prep on CSF specimens. Reference Range: Negative Influenza PCR Synonym: Flu Test General Use: To establish Influenza A/B as cause of infection Test Mnemonic: FLUPCR Test Includes: Screening for Influenza A+B , H1N1 Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Only swabs and transport media approved for test can be accepted - obtained from the Microbiology Lab. Specimen Required: Nasopharyngeal washes/aspirates or swabs recommended; throat swabs will be accepted but are not preferable. Volume of Specimen: 1 swab Causes for Rejection: Improper specimen or container. Received greater than 24 hours after collection Availability: 24/7 Reference Range: Negative for Influenza A/B antigen KOH Prep Synonyms: Fungal Wet Prep General Use: Determine presence of fungal elements Test Mnemonic: KOHP Lab Performing Test: To reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Same as for routine culture of specific site Specimen Required: Appropriate specimen for KOH preparation is the same as for fungus culture Container Required: Sterile tube Volume of Specimen: 2 ml sputum or fluid: skin scrapings Causes for Rejection: Insufficient specimen volume, dry swab Availability: Performed daily 7:00AM-9:00PM Time Required Routinely for Processing: Specimens will be processed Monthurs. 7:00AM-3:30PM Specimens received after noon on Friday, Sat. Sun., or holidays will be processed on the next routine day. Reference Range: No yeast or fungal elements Legionella Culture see Culture, Legionella Legionella DFA General Use: To support diagnosis of Legionella infection Test Mnemonic: LDFA Lab Performing Test: Sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Sputum, bronchial washings Container Required: Sterile cup Volume of Specimen: 2 ml Causes for Rejection: Specimen consistent with saliva Availability: Specimens will be processed Mon-Thurs. 7:00AM-2:00PM. Specimens received on Fridays after 12 noon or on Sat, Sun or holidays will be processed on the next routine day. Time Required Routinely for Processing: 48 – 72 hours. Reference Range: Negative Legionella Urine Antigen General Use: To support diagnosis of Legionella infection Test Mnemonic: LEGUR Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Clean void urine (keep refrigerated) Container Required: Sterile cup or tube Volume of Specimen: 10-20 ml Minimum Volume of Specimen: 10 ml Availability: Specimens will be processed Mon-Fri 7:00AM-3:30PM Time Required Routinely for Processing: Specimens received by 11:00AM will be complete the same day Reference Range: Negative MAV Blood Culture see Culture, Mycobacteria, Blood Maximum Bactericidal Dilution (MBD) Synonyms: Schlicter Test; Serum Cidal Test; MBD General Use: To determine the greatest dilution of the serum or body fluid which will kill the patient's infecting organism Test Mnemonic: MBD Lab Performing Test: Sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: If a maximum bactericidal dilution test is desired, the physician must request the laboratory to save the patient's isolate (if the isolate has not been saved, the test cannot be performed.) Specimen Required: 10 cc of clotted blood and the saved isolate Container Required: Red top tube; sterile tube for body fluid Volume of Specimen: 10 cc of clotted blood or 2 ml of body fluid in a sterile tube Minimum Volume of Specimen: 2 ml serum Causes for Rejection: Insufficient amount of serum or fluid; specimen not received in appropriate sterile container: specimen older than 4 hours: no request to save organism Availability: Specimens will be processed daily 7:00 a.m. to 3:30 p.m.; blood will be drawn any time required Time Required Routinely for Processing: At least 72 hours MBC see Minimum Bactericidal Concentration MBD see Maximum Bactericidal Dilution (MBD) MIC see Minimum Inhibitory Concentration (Send Out Test) Minimum Bactericidal Concentration Synonyms: MBC General Use: To determine Minimum lethal concentration of antimicrobial agent Test Mnemonic: MBCSO Lab Performing Test: Sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: The patient's infecting organism must be save at the request of the physician (if the isolate has not been saved, the test cannot be performed) Specimen Required: Isolation plate of organism to be tested (prepared by the Microbiology Laboratory) Container Required: Agar plate or tube Volume of Specimen: NA Causes for Rejection: Organism discarded prior to request by physician to save the organism for MBC Availability: Send out Mon – Thur. 2PM. Friday specimens must be submitted by 10:00 AM. Time Required Routinely for Processing: At least 72 hours Minimum Inhibitory Concentration (Special request Send Out Test) Synonyms: MIC General Use: To determine susceptibility of a given organism to an antimicrobial agent Test Mnemonic: MICSO Lab Performing Test: Sent to reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: The patient's infecting organism must be saved at the request of the physician Specimen Required: Isolation plate of organism to be tested (prepared by the Microbiology Laboratory) Container Required: Agar plate or tube Volume of Specimen: NA Causes for Rejection: Organism discarded prior to request by physician to save the organism for MIC Availability: Send out Mon – Thurs. 2PM. Friday specimens must be submitted by 10:00 AM. Time Required Routinely for Processing: At least 72 hours MRSA Screen PCR General Use: To screen for MRSA Colonization Test Mnemonic: MRSAN Test Includes: Screening for MRSA ONLY Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: NASAL swab Container Required: Cepheid Copan Red top swab Volume of Specimen: 1 swab Causes for Rejection: inappropriate swab Availability: 24/7 Time Required Routinely for Processing: 2-3 hours Additional Information: Presumptive positive cultures will be called as soon as possible Reference Range: Negative MRSA/SA Screen PCR (soft tissue) General Use: To screen for MRSA Test Mnemonic: STAPHC Test Includes: Screening for MRSA and Staph aureus Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: tissue swab Container Required: Cepheid Copan Red top swab Volume of Specimen: 1 swab Causes for Rejection: inappropriate swab Availability: 24/7 Time Required Routinely for Processing: 2-3 hours Additional Information: Presumptive positive cultures will be called as soon as possible Reference Range: Negative O& P, Stool for Amoeba, Worm Identification see Ova and Parasites Occult Blood, Guaiac Method Synonyms: Stool for Blood; Stool for Guaiac General Use: Routine screening procedure for occult blood in stool, etc. Test Mnemonic: OBLD Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Patient should not receive vitamin C (ascorbic acid) for 3 days prior to occult blood testing; patient should also refrain from eating red meat the day prior to testing. Specimen Required: Stool, vomitus, gastric asp Container Required: Sterile cup; stool cup Minimum Volume of Specimen: 5 ml Causes for Rejection: Specimen received on swab or wooden applicator Availability: Testing routinely done Mon - Fri afternoon unless requested verbally as STAT Time Required Routinely for Processing: 1 hr Reference Range: Negative or trace Pinworm Exam Synonyms: Scotch tape prep; Pinworm Prep General Use: To detect cases of enterobiasis. One negative result does not rule out the possibility of parasitic infection Test Mnemonic: PINW Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Adhesive slide paddle obtained from the microbiology lab; if scotch tape is used, it must be TRANSPARENT tape placed on a Clear glass slide for transport. Volume of Specimen: 1 slide Container Required: Adhesive pinworm paddle (available in Microbiology) Availability: 7:00AM – 11:00AM Mon-Fri Time Required Routinely for Processing: If specimen is received by 11 am it will be complete the same day Causes for Rejection: specimens received on opaque tape; specimens not obtained/transported properly. Reference Range: No pinworm (Enterobius vermicularis) eggs seen Pinworm Prep see Pinworm Exam Pneumocystis DFA Synonyms: Sputum for PCP General Use: Used to support the diagnosis of Pneumocystis pneumonia Test Mnemonic: PCPT Lab Performing Test: reference laboratory Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Sputum must be collected by respiratory therapist to obtain induced specimen Specimen Required: induced Sputum; Bronchoalveolar lavage; Bronchial washings. Routinely expectorated sputum is NOT acceptable Container Required: Sterile Cup Volume of Specimen: 2-3 ml Minimum Volume of Specimen: Causes for Rejection: Routinely expectorated Sputum Availability: Mon-Fri send out at 2PM. Time Required Routinely for Processing: up to 6 days Reference Range: Negative Respiratory Syncytial Virus Synonyms: RSV Exam General Use: Used to support the diagnosis of RSV Test Mnemonic: RSV Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Nasopharyngeal secretions into a mucus extractor Container Required: Mucus extractor Volume of Specimen: 0.5 - 1 ml Availability: 24/7 Reference Range: Negative Rotavirus Exam General Use: To support the diagnosis of Rotavirus infection Test Mnemonic: ROTA Lab Performing Test: To reference lab Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Stool Container Required: Sterile cup; stool cup Volume of Specimen: 2 ml Availability: Specimens will be processed Mon-thurs. 7:00AM-3:30PM Specimens received after noon on Friday, Sat. Sun., or holidays will be processed on the next routine day. Time Required Routinely for Processing: 24 hrs to 72 hrs Reference Range: Negative RSV Exam see Respiratory Syncytial Virus Schlicter Test see Maximum Bactericidal Dilution (MBD) Scotch tape prep see Pinworm Exam Semen Analysis General Use: Infertility screening Test Mnemonic: SEMEN Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Patient Preparation: Follow physician's instructions Specimen Required: Semen Container Required: Clean dry glass or plastic container Volume of Specimen: Full amount that is collected Minimum Volume of Specimen: 1 ml Causes for Rejection: Refrigerated specimen. Specimen received greater than one hour after collection; insufficient quantity, improper container. Availability: ONLY BY APPOINTMENT Time Required Routinely for Processing: Same Day Contraindications: If specimen is post vasectomy do not order a complete semen analysis, order a "sperm post vasectomy" Reference Range: See report form for individual parameters Serum Cidal Test see Maximum Bactericidal Dilution (MBD) Skin scrapings for fungus see Culture, Fungus, Skin Sperm Post Vasectomy General Use: As follow up to vasectomy Test Mnemonic: SPVAS Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Semen Container Required: Sterile urine cup; clean glass or plastic container Volume of Specimen: Full amount that is collected Causes for Rejection: Refrigerated specimen; specimen received >1 hour after collection, improper container Availability: Mon - Friday 7:00AM-2:00PM. Specimens must be received by 2:00pm. No Sat, Sun or holiday testing Time Required Routinely for Processing: Same day Reference Range: No spermatozoa seen Sputum for PCP see Pneumocystis DFA Staph aureus/MRSA Nasal Screen PCR General Use: To screen for SA/ MRSA Colonization Test Mnemonic: STAPHC Test Includes: Screening for MRSA AND Staph aureus Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: NASAL swab Container Required: Cepheid Copan Red top swab Volume of Specimen: 1 swab Causes for Rejection: inappropriate swab Availability: 24/7 Time Required Routinely for Processing: 2-3 hours Additional Information: Presumptive positive cultures will be called as soon as possible Reference Range: Negative Stool for Blood see Occult Blood, Guaiac Method Stool for Enteric Pathogens see Culture, Stool Stool for Guaiac see Occult Blood, Guaiac Method Trichomonas Rapid Test Synonyms: Wet prep for Trichomonas General Use: To detect Trichomonas Test Mnemonic: TRICA Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Must be received immediately in 1cc of sterile saline Specimen Required: Vaginal or urethral swabs Container Required: Sterile rayon swab from kit Volume of Specimen: Causes for Rejection: Inappropriate swab Availability: 7:00AM-11:00PM daily Time Required Routinely for Processing: Same day Reference Range: Negative Urine for G.C. see Culture, Urine for Neisseria Gonorrhoeae VRE PCR General Use: To screen for VRE colonization Test Mnemonic: VANA Test Includes: Screening for VRE ONLY Lab Performing Test: Microbiology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Required: Rectal swab Container Required: Sterile culturette Volume of Specimen: 1 swab Causes for Rejection: No Stool Availability: Specimens will be processed daily 7:00AM-10:00 PM Time Required Routinely for Processing: 2-3 hours Additional Information: Presumptive positive cultures will be called as soon as possible Reference Range: Negative Wet prep for Trichomonas see Trichomonas Prep Whooping Cough see Culture, Pertussis URINALYSIS The Urinalysis section of the Laboratory is directed by Victoria G. Reyes-D'Arcy/ Asim Ejaz, M.D., D.A.B. Pathologist, and Pedro Ugarelli, M.S., B.S., M.T., Hematology Manager. For procedures not listed please consult with the Hematology Manager (Ext. 4137) or Pathologist. All specimens must be properly labeled with patient's full name, identification number, time and date of collection, and the test requested. Clinitest General Use: To detect the presence of reducing substances other than glucose Test Mnemonic: URED Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Special Instructions: Test automatically performed on children less than one year old when a routine urinalysis is performed Specimen Requirements: Fresh urine. Deliver within 1-2 hours of collection or maintain specimen refrigerated at 2-8° C. Container Required: Urine collection cup or plastic urinalysis tube Volume of Specimen: 1 ml Minimum Volume of Specimen: 1 ml Causes for Rejection: Incorrect specimen volume, mislabeled or unlabeled specimen Availability: Routine 24 hours Time Required Routinely for Processing: Same day Reference Range: Negative Eosinophils in Urine Synonyms: Urine Eosinophils General Use: Interpretation by Physician Test Mnemonic: UEOS Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Requirements: Fresh urine. Deliver within 1-2 hours of collection or maintain specimen refrigerated at 2-8° C. Container Required: Plastic urinalysis tube or urine collection cup Volume of Specimen: 8 ml Minimum Volume of Specimen: 6 ml Causes for Rejection: Incorrect specimen volume, mislabeled or unlabeled specimen Availability: Daily, not stat Time Required for Processing: Same day Reference Range: Negative EOUR see Eosinophils in Urine Hemosiderin, Urine Synonyms: Urine Iron General Use: Evaluation of hemolytic diseases Test Mnemonic: UHSDRN Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Requirements: Fresh urine. Deliver within 1-2 hours of collection or maintain specimen refrigerated at 2-8° C. Container Required: Plastic urinalysis tube or urine collection cup. Volume of Specimen: 8 ml Minimum Volume of Specimen: 6 ml Causes for Rejection: Incorrect specimen volume, mislabeled or unlabeled specimen Availability: Weekdays only, not stat Time Required Routinely for Processing: Same day Reference Range: Negative Routine Urine see Urinalysis - Routine Urinalysis – Routine Synonyms: Routine Urine; Routine Urinalysis General Use: Detection of abnormal urinary chemical, inorganic, or cellular elements Test Mnemonic: URIN Profile Includes: Color, clarity, specific gravity, pH, leukocyte esterase, nitrites, glucose, ketones, bilirubin, urobilinogen, protein, blood and microscopic cellular review. Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Requirements: Fresh urine. Deliver within 1-2 hours of collection or maintain specimen refrigerated at 2-8° C. Container Required: Plastic urinalysis tube. Volume of Specimen: 6 ml. Minimum Volume of Specimen: 3 ml Causes for Rejection: Incorrect specimen volume, mislabeled or unlabeled specimen. Availability: 24/7 Time Required Routinely for Processing: Stat:30 min; Routine:same day. Reference Range: See reference ranges for individual tests. Urine Bilirubin General Use: To determine the presence of bilirubin in urine Lab Performing Test: Hematology Request Form: When this is needed, order Urine test. Patient Preparation: None Specimen Requirements: Fresh urine. Deliver within 1-2 hours of collection or maintain specimen refrigerated at 2-8° C. Container Required: Plastic urine tube Volume of Specimen: 6 ml Minimum Volume of Specimen: 3 ml Causes for Rejection: Incorrect specimen volume, mislabeled or unlabeled specimen Availability: 24/7 Time Required Routinely for Processing: Stat:30 minutes; Routine: same day. Reference Range: Negative Urine Blood General Use: To determine the presence of hemoglobin in urine Lab Performing Test: Hematology Request Form: When this is needed, order Urine test. Specimen Requirements: Fresh urine. Deliver within 1-2 hours of collection or maintain specimen refrigerated at 2-8° C. Container Required: Plastic urine tube Volume of Specimen: 6 ml Minimum Volume of Specimen: 3 ml Causes for Rejection: Incorrect specimen volume, mislabeled or unlabeled specimen Availability: 24/7 Time Required Routinely for Processing: Stat:30 minutes; Routine: same day Reference Range: Negative Urine Glucose General Use: To determine the presence of glucose in urine Lab Performing Test: Hematology Request Form: When this is needed, order Urine test. Patient Preparation: None Specimen Requirements: Fresh urine. Deliver within 1-2 hours of collection or maintain specimen refrigerated at 2-8° C. Container Required: Plastic urine tube Volume of Specimen: 6 ml Minimum Volume of Specimen: 3 ml Causes for Rejection: Incorrect specimen volume, mislabeled or unlabeled specimen Availability: 24/7 Time Required Routinely for Processing: Stat: 30 minutes; Routine: same day Reference Range: Negative Urine Iron see Hemosiderin, Urine Urine Ketones General Use: To determine the presence of ketones in urine Lab Performing Test: Hematology Request Form: Signed order by physician/Health Professional Affiliate(HPA) Specimen Requirements: Fresh urine. Deliver within 1-2 hours of collection or maintain specimen refrigerated at 2-8° C. Container Required: Plastic urine tube Volume of Specimen: 6 ml Minimum Volume of Specimen: 3 ml Causes for Rejection: Incorrect specimen volume, mislabeled or unlabeled specimen Availability: 24/7 Time Required Routinely for Processing: Stat:30 minutes; Routine:same day Reference Range: Negative Urine Leukocyte Esterase General Use: To screen for the presence of leukocytes in urine Lab Performing Test: Hematology Request Form: When this is needed, order Urine test. Specimen Requirements: Fresh urine. Deliver within 1-2 hours of collection or maintain specimen refrigerated at 2-8° C. Container Required: Plastic urinalysis tube Volume of Specimen: 6 ml Minimum Volume of Specimen: 3 ml Causes for Rejection: Incorrect specimen volume, mislabeled specimen Availability: 24/7 Time Required Routinely for Processing: Stat:30 minutes; Routine:same day Reference Range: Negative Urine Nitrites General Use: To screen for the presence of nitrite-forming bacteria in a random urine specimen Lab Performing Test: Hematology Request Form: When this is needed, order Urine test. Patient Preparation: None Specimen Requirements: Fresh urine. Deliver within 1-2 hours of collection or maintain specimen refrigerated at 2-8° C. Container Required: Plastic urinalysis tube Volume of Specimen: 6 ml Minimum Volume of Specimen: 3 ml Causes for Rejection: Incorrect specimen volume, mislabeled or unlabeled specimen Availability: 24/7 Time Required Routinely for Processing: Stat:30 minutes; Routine: same day Reference Range: Negative Urine pH General Use: To determine the acidity or alkalinity of a random urine specimen; interpretation by physician Lab Performing Test: Hematology Request Form: When this is needed, order Urine test. Specimen Requirements: Fresh urine. Deliver within 1-2 hours of collection or maintain specimen refrigerated at 2-8° C. Container Required: Plastic urinalysis tube Volume of Specimen: 6 ml Minimum Volume of Specimen: 3 ml Causes for Rejection: Incorrect specimen volume, mislabeled or unlabeled specimen Availability: 24/7 Time Required Routinely for Processing: Stat: 30 minutes; Routine - same day Reference Range: 6-7.4 Urine Protein Synonyms: Random urine protein General Use: To determine the protein present in a random urine specimen Lab Performing Test: Hematology Request Form: When this is needed, order Urine test. Specimen Requirements: Fresh urine. Deliver within 1-2 hours of collection or maintain specimen refrigerated at 2-8° C. Container Required: Plastic urinalysis tube Volume of Specimen: 6 ml Minimum Volume of Specimen: 3 ml Causes for Rejection: Incorrect specimen volume, mislabeled or unlabeled specimen Availability: 24/7 Time Required Routinely for Processing: Stat:30 minutes; Routine: same day Reference Range: Negative Urine Specific Gravity General Use: To determine the specific gravity of a random urine specimen; interpretation by physician Lab Performing Test: Hematology Request Form: When this is needed, order Urine test. Specimen Requirements: Fresh urine. Deliver within 1-2 hours of collection or maintain specimen refrigerated at 2-8° C. Container Required: Plastic urinalysis tube Volume of Specimen: 6 ml Causes for Rejection: Incorrect specimen volume, mislabeled or unlabeled specimen. Availability: 24/7 Time Required for Processing: Stat:30 minutes; Routine: same day. Reference Range: 1.003 - 1.035 Urine Urobilinogen General Use: Liver function and hemolytic disease screening Lab Performing Test: Hematology Request Form: When this is needed, order Urine test. Specimen Requirements: Fresh urine. Deliver within 1-2 hours of collection or maintain specimen refrigerated at 2-8° C. Container Required: Plastic urinalysis tube Volume of Specimen: 6 ml Minimum Volume of Specimen: 3 ml Causes for Rejection: Incorrect specimen volume, mislabeled or unlabeled specimen Availability: 24/7 Time Required for Processing: Stat:30 minutes; Routine: same day Reference Range: <2.0 Ehrlich units/dL urine
© Copyright 2026