‘‘If God Wanted Me Yesterday, I Wouldn’t Be Here Today’’:
JOURNAL OF PALLIATIVE MEDICINE
Volume 13, Number 5, 2010
ª Mary Ann Liebert, Inc.
DOI: 10.1089=jpm.2009.0343
‘‘If God Wanted Me Yesterday, I Wouldn’t Be Here Today’’:
Religious and Spiritual Themes in Patients’ Experiences
of Advanced Cancer
Sara R. Alcorn, B.A.,1–3,* Michael J. Balboni, M.Div., Th.M.,1,4,5,* Holly G. Prigerson, Ph.D.,1,4,6
Amy Reynolds, Ph.D.,7 Andrea C. Phelps, M.D.,1,4 Alexi A. Wright, M.D.,1,4,8 Susan D. Block, M.D.,1,4,6
John R. Peteet, M.D.,1,4,6 Lisa A. Kachnic, M.D.,9 and Tracy A. Balboni, M.D., M.P.H.1,3,4
Abstract
Background: This study sought to inductively derive core themes of religion and=or spirituality (R=S) active in
patients’ experiences of advanced cancer to inform the development of spiritual care interventions in the terminally ill cancer setting.
Methods: This is a multisite, cross-sectional, mixed-methods study of randomly-selected patients with advanced
cancer (n ¼ 68). Scripted interviews assessed the role of R=S and R=S concerns encountered in the advanced
cancer experience. Qualitative and quantitative data were analyzed. Theme extraction was performed with
interdisciplinary input (sociology of religion, medicine, theology), utilizing grounded theory. Spearman correlations determined the degree of association between R=S themes. Predictors of R=S concerns were assessed
using linear regression and analysis of variance.
Results: Most participants (n ¼ 53, 78%) stated that R=S had been important to the cancer experience. In descriptions of how R=S was related to the cancer experience, five primary R=S themes emerged: coping, practices,
beliefs, transformation, and community. Most interviews (75%) contained two or more R=S themes, with 45%
mentioning three or more R=S themes. Multiple significant subtheme interrelationships were noted between the
primary R=S themes. Most participants (85%) identified 1 or more R=S concerns, with types of R=S concerns
spanning the five R=S themes. Younger, more religious, and more spiritual patients identified R=S concerns more
frequently (b ¼ 0.11, p < 0.001; b ¼ 0.83, p ¼ 0.03; and b ¼ 0.89, p ¼ 0.04, respectively).
Conclusions: R=S plays a variety of important and inter-related roles for most advanced cancer patients.
Future research is needed to determine how spiritual care can incorporate these five themes and address R=S
concerns.
Introduction
R
eligion and=or spirituality (R=S) frequently play a
fundamental role in maintaining patient well-being in the
face of terminal illness.1–3 However, spiritual concerns often
arise in the setting of advanced illness,4,5 particularly among
ethnic minorities,5 a notable finding in light of the association
of spiritual distress with quality of life (QOL) decrements.3,6
Recognition of the implications of R=S for the well-being of
patients with advanced illness is reflected in the inclusion of
spiritual care in national and international palliative care
guidelines7,8—care in the medical context that (1) recognizes
and supports the role of R=S in illness and (2) attends to
spiritual needs.
Among patients with advanced cancer, spiritual care is
associated with improved patient QOL near death, greater
1
Center for Psycho-Oncology and Palliative Care Research, 3Department of Radiation Oncology, 4Department of Psycho-Oncology and
Palliative Care, 8Department of Medical Oncology, Dana-Farber Cancer Institute, Boston, Massachusetts.
2
Harvard Medical School, Boston, Massachusetts.
5
Department of Practical Theology, Boston University, Boston, Massachusetts.
6
Harvard Medical School Center for Palliative Care, Boston, Massachusetts.
7
Department of Sociology, Princeton University, Princeton, New Jersey.
9
Department of Radiation Oncology, Boston Medical Center, Boston, Massachusetts.
*These authors contributed equally to this work.
Accepted December 17, 2009.
581
582
hospice utilization, and less aggressive care at the end of life.9
Despite the recognition of the value of spiritual care, limited
data are available to guide its provision to terminally ill patients. An enhanced understanding of the elements of R=S
active at the end of life through both qualitative and quantitative methods has been identified as a key research area for
palliative care quality improvement by proceedings from a
recent national consensus conference.10 Such information is
necessary to guide spiritual care in the medical context and to
establish hypotheses upon which testable spiritual care
interventions can be developed.
The Religion and Spirituality in Cancer Care study is a
multisite, cross-sectional study of patients with advanced
cancer aiming to establish an empirical basis for spiritual care
by exploring how R=S functions in the terminal cancer experience and by characterizing the spiritual concerns of patients
with advanced cancer using mixed qualitative and quantitative methods.
Methods
Study sample
Patients were enrolled between March 3, 2006 and April 14,
2008. Eligibility criteria included diagnosis of an advanced,
incurable cancer; active receipt of palliative radiation therapy
(RT); age 21 years or greater; and adequate stamina to undergo a 45-minute interview. We excluded patients who met
criteria for delirium or dementia by neurocognitive examination (Short Portable Mental Status Questionnaire11) and
those not speaking English or Spanish.
Study protocol
All research staff underwent a 1-day training session in the
study protocol and the scripted, interviewer-administered
questionnaire. Patients were recruited from four Boston,
Massachusetts, sites: Beth Israel Deaconess Medical Center,
Boston University Medical Center, Brigham and Women’s
Hospital, and Dana-Farber Cancer Institute. Patients were
randomly selected from RT schedules; all eligible patients
were approached for participation. To mitigate selection bias,
study staff informed all potential participants, ‘‘You do not
have to be religious or spiritual to answer these questions. We
want to hear from people with all types of points of view.’’
Participants provided written, informed consent according to
protocols approved by each site’s human subjects committee.
Definitions for R=S grounded the study’s design and were
provided to participants at the beginning of the interview,
with spirituality defined as ‘‘a search for or a connection to
what is divine or sacred’’ and religion defined as ‘‘a tradition
of spiritual beliefs and practices shared by a group of people.’’
Of 103 patients approached, 75 (73%) participated. Seven
patients had missing data, 5 due to being too sick=fatigued to
complete the interview (indicated by their lower average
performance status than other participants, 36.0 versus 68.8,
p ¼ 0.003), yielding a total of 68 patients (91% of 75).
ALCORN ET AL.
Religion/spirituality in the cancer experience. Patients
were asked, ‘‘Has religion or spirituality been important to
your experience with your illness?’’ Response options were
‘‘yes’’ or ‘‘no.’’ Those responding ‘‘yes’’ were asked, ‘‘How has
religion or spirituality been important to your experience with
your illness?’’ Responses were audio-recorded and transcribed verbatim.
Religious/spiritual concerns. R=S challenges and
struggles encountered in the advanced cancer experience were
assessed quantitatively and qualitatively. Patients were asked,
‘‘What spiritual issues have you had as you have been dealing
with your illness?’’ Response options were consistent with
prior studies of R=S concerns in the setting of advanced
illness5,13,14 and with the study’s R=S definitions, including:
‘‘seeking a closer connection with God or your faith’’;
‘‘doubting your belief in God or your faith’’; ‘‘finding meaning
in the experience of your cancer’’; ‘‘being angry with God’’;
‘‘wondering why God has allowed this to happen’’; ‘‘thinking
about forgiveness (being forgiven or being forgiven by
others)’’; and ‘‘thinking about what gives meaning to life.’’
Pargament’s validated negative religious coping items15 were
utilized as they assess R=S struggles previously shown to be
associated with QOL decrements3: feeling abandoned by God,
feeling abandoned by R=S communities, questioning God’s
love, questioning God’s power, thinking the devil caused the
cancer, and feeling punished by God. Response options were
‘‘not at all,’’ ’’somewhat,’’ ‘‘quite a bit,’’ and ‘‘a great deal,’’ with
the spiritual issue considered present when patients answered
‘‘somewhat’’ or greater. Patients were also asked in an openended manner, ‘‘What other spiritual issues have you experienced?’’ Responses were transcribed verbatim.
Other measured variables. Age, gender, race=ethnicity
(dichotomized to white versus non-white), and years of
education were patient-reported. Karnofsky performance
status was obtained by physician assessment.
Analytical methods
Qualitative methodology. The protocol followed a high
standard of qualitative research methodology16 including
triangulated analysis, employment of multidisciplinary perspectives (medicine, sociology, and theology), and the use of
reflexive narratives—all of which maximize the transferability
of interview data. Transcriptions were independently coded
line-by-line by two researchers (S.A. and M.B.) and were then
compiled into two preliminary coding schemes. Following
principles of grounded theory,17 a final set of themes and
subthemes inductively emerged through an iterative process
of constant comparison with input from S.A., M.B., A.R., and
T.B. Transcripts were then recoded by S.A. and M.B, each
working independently and using the derived themes and
subthemes. The interrater reliability score was high (k ¼ 0.85).
All spiritual concerns were categorized according to the R=S
themes derived through qualitative analysis by the study
investigators (M.B., S.A., T.B.).
Study measures
Participant religiousness and spirituality. Two items
from the previously-validated12 Fetzer Multidimensional
Measure of Religiousness=Spirituality for Use in Health Research assessed degree of patient religiousness and spirituality.
Statistics. Differences in sample characteristics according to importance of R=S to the cancer experience were analyzed with w2-test (dichotomous and categorical variables),
t-test (continuous variables), and Wilcoxon-Mann-Whitney
RELIGIOUS AND SPIRITUAL THEMES IN CANCER
test (ordinal variables). Exploratory analyses of subtheme
relationships were performed utilizing Spearman correlations. Potential predictors of spiritual concerns were examined by simple linear regression (continuous, ordinal, and
dichotomous variables) and analysis of variance (ANOVA;
categorical variables). Statistical analyses were performed
with SAS version 9.1 (SAS Institute Inc., Cary, NC). All reported p values are two-sided and are considered significant
when less than 0.05.
Results
Sample characteristics
Table 1 shows sample characteristics by patient-reported
importance of R=S to the cancer experience. Most patients
(81%) were at least slightly religious and spiritual, 12% were at
least slightly spiritual but not religious, and 7% were neither
religious nor spiritual. Most (78%; 53=68) indicated that R=S
had been important to their cancer experience, and most (85%)
had R=S concerns arise, with 75% reporting multiple concerns.
583
Religion and spirituality in the cancer experience:
primary themes
Five primary R=S themes were extracted from patients’
open-ended descriptions of the importance of R=S to their
cancer experience: coping through R=S, R=S practices,
R=S beliefs, R=S transformation, and R=S community
(Table 2).
The R=S coping theme was defined as patients’ expressions
of how R=S impacted their endurance of the cancer experience, a theme present in the majority of interviews (74%). The
most frequently cited way that R=S facilitated coping was by
extending longevity (10 of 39), exemplified by one participant
stating, ‘‘You’ve got to have faith and a positive outlook because it is going to help you last longer.’’ Additionally, R=S
was noted to provide promise of a potential cure (9=39),
strength (8=39), meaning (8=39), comfort (7=39), acceptance
(6=39), and emotional stability (5=39). One patient explained
with tears, ‘‘If it weren’t for my faith, I don’t know how
I would have kept my equilibrium through this process. It is
definitely though grace. . .Whenever I’m at the hardest places
Table 1. Sample Characteristics by Importance of Religion=Spirituality in Patients’ Experiences
of Advanced Cancer, n ¼ 68
Religion=spirituality important
to the cancer experience
Sample characteristics
Total—N (%)
Gender
Male, n (%)
Female, n (%)
Age, years—M (SD)
Karnofsky Performance Status—M (SD)
Race=ethnicityc
White, n (%)
Non-white, n (%)
Education, years—M (SD)
Religious tradition—N (%)
Catholic, n (%)
Not-Catholic Christian, n (%)
Jewish, n (%)
Otherd
To what extent do you consider yourself a religious person?
Very religious, n (%)
Moderately religious, n (%)
Slightly religious, n (%)
Not religious at all, n (%)
To what extent do you consider yourself a spiritual person?
Very spiritual, n (%)
Moderately spiritual, n (%)
Slightly spiritual, n (%)
Not spiritual at all, n (%)
Religious=spiritual concerns
No religious=spiritual concerns
1–3 religious=spiritual concerns
4 or more religious=spiritual concerns
a 2
68 (100)
36
32
60.2
68.8
(53)
(47)
(11.9)
(19.3)
57 (85)
10 (15)
15.3 (3.4)
No
53 (78)
15 (22)
26
27
60.1
68.4
(49)
(51)
(11.1)
(19.7)
42 (81)
10 (19)
15.3 (3.4)
10
5
60.3
70
p
(67)
(33)
(15.1)
(18.1)
0.23a
0.95b
0.78b
15 (100)
0 (0)
14.9 (3.5)
0.07a
0.69b
32
22
5
9
(47)
(32)
(7)
(13)
25
20
1
7
(47)
(38)
(2)
(13)
7
2
4
2
(47)
(13)
(27)
(13)
13
25
17
13
(19)
(37)
(25)
(19)
13
23
12
5
(25)
(43)
(23)
(9)
0
2
5
8
(0)
(13)
(33)
(53)
<0.001
25
24
14
5
(37)
(35)
(21)
(7)
25
19
9
0
(47)
(36)
(17)
(0)
0
5
5
5
(0)
(33)
(33)
(33)
<0.001e
10 (15)
23 (34)
35 (51)
w test.
t-test.
c
Missing data ¼ 1.
d
Other includes Muslim (1), Buddhist (2), no religious tradition (2), and ‘‘other’’ (4).
e
Wilcoxon-Mann-Whitney test.
M, mean; SD, standard deviation.
b
Yes
5 (9)
19 (36)
29 (55)
5 (33)
4 (27)
6 (40)
0.008a
0.12e
584
ALCORN ET AL.
Table 2. Qualitatively Grounded Religious=Spiritual Themes in Patients’ Experiences
of Advanced Cancer, n ¼ 53a
Theme
n (%)
Representative quote
Coping through religion=spirituality
39 (74)
Religious=spiritual practices
31 (58)
Religious=spiritual beliefs
28 (53)
Religious=spiritual transformation
20 (38)
Religious=spiritual community
11 (21)
I don’t know if I will survive this cancer, but without God it is hard to stay sane
sometimes. For me, religion and spirituality keeps me going.
I pray a lot. It helps. You find yourself praying an awful lot. Not for myself, but for
those you leave behind. There will be a lot more praying.
It is God’s will, not my will. My job is to do what I can to stay healthy—eat right,
think positively, get to appointments on time, and also to do what I can to become
healthy again like make sure that I have the best doctors to take care of me. After
this, it is up to God.
Since I have an incurable disease that will shorten my life, it has made me focus on
issues of mortality and sharpened my curiosity on religion=spirituality and what
the various traditions have to say about that. I’ve spent a lot of time thinking
about those issues, and it has enriched my psychological, intellectual, and
spiritual experience of this time.
Well, I depend a lot upon my faith community for support. It’s proven incredibly
helpful for me.
a
53 of 68 indicated religion=spirituality was important to their cancer experience.
in life, God just sends his Holy Spirit, and it just takes over,
just like He said it would.’’
The R=S practices theme was defined as patients’ descriptions of R=S practices important to their cancer experience,
raised by 58% of patients. The most frequently noted practice
was prayer (27=31). Patients reported praying for themselves
(21=27), praying more frequently (5=27), receiving prayer
from others (4=27), praying with others (3=27), and praying
for others (4=31). The most cited reason for prayer was to ask
for strength (4=27), illustrated by a patient sharing, ‘‘I just say
to God, ‘Okay. You’re going to give me something to deal
with, just give me the strength to deal with it.’ ’’ Other perceived benefits derived from engaging in R=S practices included healing (3=27), guidance (1=27), and perseverance
(1=27). Additional R=S practices subthemes mentioned were
religious service attendance (6=31), reading sacred writings
(1=31), and meditation (1=31).
The R=S beliefs theme was defined as patients’ references to
R=S beliefs important to their experience of cancer. The majority (53%) raised this theme. A common subtheme was the
view that R=S plays a significant role in life independent of
cancer (13=28), illustrated by comments such as ‘‘religion has
always played an important part of my life.’’ Also frequently
mentioned was a belief in God’s will (12=28), exemplified by
the statement, ‘‘[based] on my religious beliefs I think I was
given a certain number of days on this earth from day one,
and I don’t think that changes any with my diagnosis . . . It
tells me that if God wanted me yesterday, I wouldn’t be here
today, and if He wants me to survive [cancer] 20 years without a cure, then that’s His will also.’’ Additional R=S beliefs
subthemes included belief in an afterlife (7=28) and beliefs
being spiritual but not religious (5=28).
The religious=spiritual transformation theme was defined
as patients’ expressions of transformation in R=S beliefs or
participation resulting from the cancer experience, raised by
38% of patients. Several patients mentioned that their cancer
engendered a new or deeper reflection on faith and mortality
(10=20), reflected in statements such as ‘‘it’s a transformative
experience to have an illness such as this, and when you have
that you have to reevaluate all you’ve done in life, who you
are, and who you’re going to be.’’ Patients also endorsed
spiritual transformation through an enhanced personal faith
(8=20), an increase in faith-based activities (8=20), a heightened sense of companionship with God or a higher power
(7=20), and greater appreciation for life and health (3=20).
The religious=spiritual community theme, defined by patients referring to an R=S community (e.g., clergy or other
spiritual supporters) as important to their cancer experience,
was raised by 21% of patients. For example, one patient
shared, ‘‘A lot of people have offered to put me on their church
prayer list. . .and I think if a friend or person believes in it, then
it is giving a gift to you as a cancer patient. . . .’’
Relationships between religious=spiritual themes
In describing R=S in the cancer experience, most responses
(75%) contained two or more primary themes, with 45%
raising three or more themes. The exploratory analysis of the
relationships between R=S subthemes is shown in Table 3 and
reveals multiple significant correlations between subthemes.
Illustrating theme interrelationships, one patient shared, ‘‘I’m
praying a lot more. I’m receiving cards, which are mass cards,
from family, friends—it’s just incredible. . .So, that has helped
me to be more faithful and have more faith.’’ This quote
demonstrates connections between R=S practice (prayer), R=S
community (spiritual family and friends), and R=S transformation (increased faith) in this patient’s cancer experience.
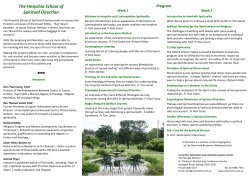
Figure 1 illustrates the exploratory analyses of subtheme
inter-relationships between the five primary R=S themes.
Religious/spiritual concerns in the experience
of advanced cancer
The frequency of quantitatively-assessed spiritual concerns
is shown in Table 4A, categorized by primary R=S themes.
Most participants (85%) identified 1 or more R=S challenges
and struggles. The majority reported concerns related to
seeking greater connection with God or faith and seeking
greater meaning in life or in the cancer experience. Notably,
one or more of the six spiritual struggles defined by Pargament’s’ negative religious coping items (e.g., feeling aban-
585
2
3
4
5
6
b
c
—
—
—
—
—
—
7
—
—
—
—
—
—
—
8
—
—
—
—
—
—
—
—
—
—
—
—
—
—
10 11
—
—
—
—
—
—
—
12
0.35c — 0.45b —
— —
—
—
0.48b
—
—
—
—
—
—
—
—
9
—
—
0.29c
—
—
—
—
0.35b
—
—
—
—
13
—
0.35b
—
—
—
—
—
—
0.57b
—
0.43b
—
—
15
0.33c
—
—
—
—
—
—
14
0.48b
—
—
—
—
0.35c
—
16
—
—
—
—
—
—
0.49b
—
0.33c
—
0.33c
—
—
0.39b
—
17
—
0.35b
—
—
0.40b
—
—
0.49b
—
0.28c
—
—
—
—
—
—
Nonsignficant relationships in this exploratory analysis are indicated by a ‘—’. For all significant relationships, Spearman correlations are shown.
p < 0.01.
p < 0.05.
a
1 R=S provides strength
— — — —
—
2 R=S provides emotional stability
— — —
—
3 R=S provides meaning to cancer
— —
0.51b
c
4 R=S improves survival
0.30 —
5 R=S provides hope for cure
—
6 R=S facilitates acceptance
7 R=S provides comfort
Religious=spiritual practices
8 General prayer
9 Prayer by self
10 Prayer with others
11 Others praying for patient
12 Increased prayer
13 Prayer for healing
14 Prayer for strength
15 Prayer for perseverance
16 Prayer for guidance
17 Prayer for others
18 Religious services
19 Religious writings
20 Meditation
Religious=spiritual beliefs
21 Belief in God=higher power’s will
22 Belief in an afterlife
23 R=S as personal worldview
24 Beliefs spiritual, not religious
Religious=spiritual transformation
25 Increased faith
26 Increased appreciation for life=health
27 Increased faith-based activities
28 Increased reflection on faith=mortality
29 Increased companionship with
God=higher power
30 Experience of forgiveness
31 Religious=spiritual community
Coping through religion=spirituality
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
0.57b
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
18 19
—
—
—
—
—
—
—
—
—
—
—
—
—
0.43c
—
—
—
—
—
20
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
0.40b
—
—
0.52b
—
21
—
—
—
—
—
—
—
—
—
—
—
—
—
— —
— —
—
—
—
—
—
—
—
—
—
—
—
—
—
—
0.43b
—
—
—
—
—
—
—
23 24
—
—
—
—
—
—
—
—
—
—
—
—
0.39b
—
—
—
—
—
—
—
—
—
—
—
—
—
0.34c
22
—
—
—
—
—
—
—
0.28c
—
0.35b
—
—
—
—
0.30c
—
—
—
—
0.41b
—
—
—
—
25
27
28
29
30
0.46b
—
0.30c
—
0.71b —
—
—
—
—
—
—
—
0.29c
—
—
—
—
—
0.46b
0.34c
0.30c
—
—
—
—
—
—
—
—
—
—
—
0.36b
—
—
—
—
—
—
—
—
0.36b
—
—
—
—
—
0.39b
—
—
—
—
—
—
—
—
—
0.46b
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
0.29c
—
0.34c
0.34c
—
—
0.28c
—
—
—
0.37c
—
—
—
—
0.28c
0.40b
0.35b
—
—
—
0.28c
0.46b
—
—
—
—
—
—
—
—
—
—
—
0.43b
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
26
Table 3. Exploratory Analysis of Correlations between Religious=Spiritual Subthemes in Patients’ Experiences of Advanced Cancera, n ¼ 53
31
—
0.43b
—
0.43b
—
0.35c
—
—
—
—
0.30c
—
0.28c
0.56b
—
0.48b
—
—
—
—
0.35c
0.27c
—
—
—
—
—
—
—
—
586
ALCORN ET AL.
FIG. 1. Exploratory diagram of religious=spriritual subtheme interrelationships in patients’ experiences of advanced cancer.
*The area of each theme’s circle corresponds to the proportional theme frequency. {Proportion of subthemes that are significantly correlated to one another of the total potentially related subthemes (N).
doned by God) were endorsed by 43% of patients. The qualitatively-assessed spiritual concerns are shown in Table 4B,
categorized according to primary R=S themes. Predictors of
greater R=S concerns included younger age (b ¼ 0.11,
p < 0.001), increasing religiousness (b ¼ 0.83, p ¼ 0.03), and
increasing spirituality (b ¼ 0.89, p ¼ 0.04). Gender, race, education, performance status, religious affiliation, and importance of R=S to the cancer experience were not associated with
frequency of spiritual concerns.
Discussion
This study demonstrates that religion and=or spirituality
are important to most patients’ experiences of advanced
cancer, and that the elements of R=S active in the cancer experience can be categorized into five primary R=S themes:
beliefs, community, transformation, coping, and practices.
The frequency by which patients spontaneously reported
these themes suggests that multiple themes play a meaningful role for the majority of patients with advanced cancer.
Moreover, frequent significant correlations between subcategories of the primary themes in exploratory analyses suggest there may be dynamic, complex relationships
between the domains. Additionally, most patients with advanced cancer experience one or more R=S concerns. This
study provides an inductively derived understanding of the
R=S themes active in the cancer experience, their interconnections, and the related R=S concerns that may inform the
content of spiritual care.
The five R=S themes are consistent with other studies examining how R=S operates among cancer populations. Gall
and Cornblat18 conducted a study of 39 breast cancer survivors and identified similar R=S themes. Prior studies have
similarly demonstrated correlations between R=S domains,
including interrelationships between meaning, beliefs,
and faith19 and between religious coping and R=S beliefs,
practices, and transformation.14, 20 Other studies have noted
similar frequencies of spiritual needs.4,5 The particular R=S
concerns we identified are supported by prior reports that
have characterized needs and struggle surrounding meaning,5,21,22 connection with God=higher power,13 forgiveness,13
death and the afterlife,5,22 peace of mind,4,5 and R=S practices.21,23 Finally, a study of incurable cancer patients noted
similar rates of patients experiencing one or more of the following spiritual struggles: feeling punished, feeling abandoned by God, feeling abandoned by R=S communities,
questioning God’s love, believing the devil caused the cancer,
or questioning God’s power.24
Other qualitative studies grounding spiritual care21, 25 have
focused on practitioners’ approach to and practices of spiritual care. Daaleman et al.25 identified three key practitioner
qualities in spiritual care provision termed: being present,
opening eyes, and cocreating. Hanson et al.21 assessed spiritual care activities of various caregivers and identified four
domains of spiritual care practices: relationship, understanding, coping, and practices. Our study complements
these studies by inductively grounding the content of spiritual
care based on patients’ testimonies and their associated R=S
concerns.
Our findings suggest that comprehensive spiritual care
might include attention to each of the five R=S themes, in light
of frequent endorsement of multiple themes, their interrelationships, and the frequency of R=S concerns. Spiritual
care interventions focused on a single characteristic of R=S
may insufficiently account for the inter-dependence of the R=S
themes. Moreover, spiritual care interventions that emphasize
practitioner attitudes or techniques (e.g., empathic listening)
may be inadequate if they do not also account for the substantive R=S content active in the cancer experience. Future
spiritual care models must balance supportive caregiver
attitudes with substantive engagement of patients’ spiritual
resources, struggles, and practices.26
RELIGIOUS AND SPIRITUAL THEMES IN CANCER
587
Table 4A. Quantitatively Assessed
Religious=Spiritual Concerns in Patients
with Advanced Cancer, n ¼ 68
n (%)
Religious=Spiritual Beliefs
Doubting one’s belief in God or one’s faith
Questioning God’s lovea
Questioning God’s powera
Believing the devil caused the cancera
Religious=spiritual community
Feeling abandoned by ones religious=
spiritual communitya
Religious=spiritual transformation
Seeking a closer connection with God
or one’s faith
Seeking what gives meaning to life
Seeking forgiveness (of oneself or others)
Feeling angry at God
Feeling abandoned by Goda
Feeling punished by Goda
Religious=spiritual coping
Seeking meaning in the experience
of cancer
13
14
14
6
(19)
(21)
(21)
(9)
6 (9)
36 (53)
37
32
17
19
15
(54)
(47)
(25)
(28)
(22)
34 (50)
Table 4B. Other Spiritual Concerns Reported
by Patients with Advanced Cancer in Response
to an Open-Ended Assessment, n ¼ 68b
n
Religious=spiritual transformation
Thinking about death
Seeking to live life more fully
Seeking peace
Religious=spiritual coping
Struggle with cancer causing loss of control
Religious=spiritual practices
Seeking greater spiritual practice (e.g., yoga, prayer)
practices and transformation, along with cancer patients’
common perceived need to be better connected to R=S
communities,23 suggest that future models of spiritual care
in the medical context should include a central role for patients’ R=S communities.
This study’s limitations include the fact that it is based on a
circumscribed definition of R=S in order to clearly distinguish
R=S from related, but distinct psychosocial parameters (e.g.,
social support); hence some aspects of R=S may have been excluded. Second, though patients were randomly sampled and
the response rate was high, the study population was from a
single U.S. region, largely Judeo-Christian, and Caucasian.
Additionally, since qualitative interviews are limited by what
participants spontaneously share, theme frequencies may underestimate the true frequency of theme endorsement and
subsequent quantitative assessment of subtheme interrelationships may underestimate the frequency of significant relationships between subthemes. Given these limitations of qualitative
data and the cross-sectional nature of our study, these analyses
were exploratory and hypothesis-generating only.
By comprehensively assessing the functioning of R=S in the
advanced cancer experience and the attendant spiritual concerns, this study aids in providing an inductively derived
framework for the content of spiritual care. Given the implications of R=S for patient’s end-of-life care9,24 and wellbeing1,9 and the frequent lack of engagement of patient R=S in
end-of-life care,27 laying an inductively derived foundation
for spiritual care holds promise for improving the care of
patients with cancer at the end of life.
Acknowledgments
2
2
1
This research was supported in part by an American
Society of Clinical Oncology Young Investigator Award to
Dr. Tracy Balboni.
2
Author Disclosure Statement
7
Pargament’s negative religious coping items.15
b
Qualitative answers already represented under the quantitative
spiritual concerns categories excluded.
No competing financial interests exist.
a
Our study findings can also inform the content of spiritual
care interventions for further research. For example, the high
frequency of prayer and its interrelationship with the other
four themes suggests that prayer may have a key role in
spiritual care interventions. Other examples include patients’
frequent endorsement of particular beliefs (e.g., beliefs being
spiritual but not religious), the relationship of those beliefs to
other themes (e.g., the connection of belief in God’s will
to acceptance of the cancer diagnosis), and tensions related to
those beliefs (e.g., questioning God’s love or power). Additionally, engaging cancer patients’ R=S may commonly
involve attending to their unique belief systems, which may
require the involvement of individuals with particular training and experience relevant to patients’ R=S beliefs. A final
example is the endorsement of the R=S community theme,
notable in light of data indicating that terminally ill patients
with cancer frequently become less engaged with R=S communities as a result of physical limitations.27 The frequent
relationships between the R=S community theme with R=S
References
1. Brady MJ, Peterman AH, Fitchett G, Mo M, Cella D: A case
for including spirituality in quality of life measurement in
oncology. Psychooncology 1999;8:417–428.
2. Steinhauser KE, Christakis NA, Clipp EC, McNeilly M,
McIntyre L, Tulsky JA: Factors considered important at the
end of life by patients, family, physicians, and other care
providers. JAMA 2000;284:2476–2482.
3. Tarakeshwar N, Vanderwerker LC, Paulk E, Pearce MJ, Kasl
SV, Prigerson HG: Religious coping is associated with the
quality of life of patients with advanced cancer. J Palliat Med
2006;9:646–657.
4. Astrow AB, Wexler A, Texeira K, He MK, Sulmasy DP: Is
failure to meet spiritual needs associated with cancer patients’ perceptions of quality of care and their satisfaction
with care? J Clin Oncol 2007;25:5753–5757.
5. Moadel A, Morgan C, Fatone A, Grennan J, Carter J, Laruffa
G, Skummy A, Dutcher J: Seeking meaning and hope: Selfreported spiritual and existential needs among an ethnicallydiverse cancer patient population. Psychooncology 1999;8:
378–385.
6. Sherman AC, Simonton S, Latif U, Spohn R, Tricot G: Religious struggle and religious comfort in response to illness:
588
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
ALCORN ET AL.
Health outcomes among stem cell transplant patients.
J Behav Med 2005;28:359–367.
World Health Organization Palliative Care: Symptom
Management and End of Life Care IMoAaAIWHO, 2004.
http:==ftp.who.int=htm=IMAI=Modules=IMAI_palliative.pdf
(Last accessed May 15, 2009).
NCP Clinical Practice Guidelines for Quality Palliative Care
SENCP, 2009. http:==ww.nationalconsensusproject.org=
guideline.pdf (Last accessed May 15, 2009).
Balboni TA, Paulk MA, Balboni MJ, et al. Provision of spiritual care to advanced cancer patients: Associations with
medical care and quality of life near death. J Clin Oncol
2010;28:445–452.
Puchalski C, Ferrell B, Virani R, Otis-Green S, Baird P, Bull J,
Chochinov H, Handzo G, Nelson-Becker H, Prince-Paul M,
Pugliese K, Sulmasy D: Improving the quality of spiritual
care as a dimension of palliative care: The report of the
Consensus Conference. J Palliat Med 2009;12:885–904.
Pfeiffer E: A short portable mental status questionnaire for
the assessment of organic brain deficit in elderly patients.
J Am Geriatr Soc 1975;23:433–441.
Fetzer Insitute: Multidimensional Measurement of Religiousness=Spirituality for Use in Health Research: A Report
of the Fetzer Institute=National Institute on Aging Working
Group. www.fetzer.org=PDF=Total_Fetzer_Book.pdf. (Last
accessed May 6, 2009).
The George H. Gallup International Institute: Spiritual beliefs and the dying process, a report of a national survey.
Princeton: Conducted for the Nathan Cummings Foundation and the Fetzer Institute, 1997.
Pargament KI: The Psychology of Religion and Coping: Theory,
Research, Practice. New York: Guilford Press, 1997.
Pargament KI, Koenig HG, Perez LM: The many methods of
religious coping: Development and initial validation of the
RCOPE. J Clin Psychol 2000;56:519–543.
Malterud K: Qualitative research: Standards, challenges, and
guidelines. Lancet 2001;358:483–488.
Corbin JM, Strauss AL: Basics of Qualitative Research: Techniques and Procedures for Developing Grounded Theory, 3rd Ed.
Los Angeles: SAGE Publications, 2008.
Gall TL, Cornblat MW: Breast cancer survivors give voice: A
qualitative analysis of spiritual factors in long-term adjustment. Psychooncology 2002;11:524–535.
19. McClain-Jacobson C, Rosenfeld B, Kosinski A, Pessin H,
Cimino JE, Breitbart W: Belief in an afterlife, spiritual wellbeing and end-of-life despair in patients with advanced
cancer. Gen Hosp Psychiatry 2004;26:484–486.
20. Taylor EJ, Outlaw FH, Bernardo TR, Roy A: Spiritual conflicts associated with praying about cancer. Psychooncology
1999;8:386–394.
21. Hanson LC, Dobbs D, Usher BM, Williams S, Rawlings J,
Daaleman TP: Providers and types of spiritual care during
serious illness. J Palliat Med 2008;11:907–914.
22. Grant E, Murray SA, Kendall M, Boyd K, Tilley S, Ryan D:
Spiritual issues and needs: Perspectives from patients with
advanced cancer and nonmalignant disease. A qualitative
study. Palliat Support Care 2004;2:371–378.
23. Hampton DM, Hollis DE, Lloyd DA, Taylor J, McMillan SC:
Spiritual needs of persons with advanced cancer. Am J Hosp
Palliat Care 2007;24:42–48.
24. Phelps AC, Maciejewski PK, Nilsson M, Balboni TA, Wright
AA, Paulk ME, Trice E, Schrag D, Peteet JR, Block SD,
Prigerson HG: Religious coping and use of intensive lifeprolonging care near death in patients with advanced cancer. JAMA 2009;301:1140–1147.
25. Daaleman TP, Usher BM, Williams SW, Rawlings J, Hanson
LC: An exploratory study of spiritual care at the end of life.
Ann Fam Med 2008;6:406–411.
26. Puchalski CM, Lunsford B, Harris MH, Miller RT: Interdisciplinary spiritual care for seriously ill and dying patients: A collaborative model. Cancer J 2006;12:398–416.
27. Balboni TA, Vanderwerker LC, Block SD, Paulk ME, Lathan
CS, Peteet JR, Prigerson HG: Religiousness and spiritual
support among advanced cancer patients and associations
with end-of-life treatment preferences and quality of life.
J Clin Oncol 2007;25:555–560.
Address correspondence to:
Tracy A. Baloni, M.D., M.P.H.
Psycho-Oncology and Palliative Care
Dana-Farber Cancer Institute
44 Binney Street
Boston, MA 01225
E-mail: [email protected]
© Copyright 2026