Complications of non-compaction of the left a prospective study
Clinical research European Heart Journal (2006) 27, 1855–1860 doi:10.1093/eurheartj/ehl112 Congenital heart disease Complications of non-compaction of the left ventricular myocardium in a paediatric population: a prospective study ´zek1, James J. Joyce5, Thomas Rau2, Barbara F. Finckh3, Florian Weiss4, Christian Lilje1,5*, Vit Ra Christian R. Habermann4, Janet C. Rice6, and Jochen Weil1 1 ¨ts-Klinikum Hamburg-Eppendorf, Martinistr. 52, D-20246 Hamburg, Germany; Departments of Kinderkardiologie, Universita ¨ts-Klinikum Hamburg-Eppendorf, Hamburg, Germany; Experimentelle & Klinische Pharmakologie & Toxikologie, Universita 3 ¨ts-Klinikum Hamburg-Eppendorf, Hamburg, Germany; 4 Diagnostische Radiologie, Clinical Pathology/Pediatrics, Universita ¨ts-Klinikum Hamburg-Eppendorf, Hamburg, Germany; 5 Section of Pediatric Cardiology, Tulane University Health Universita Sciences Center, New Orleans, LA, USA; and 6 Department of Biostatistics, Tulane University School of Public Health & Tropical Medicine, New Orleans, LA, USA 2 Received 28 September 2004; revised 5 April 2006; accepted 1 June 2006; online publish-ahead-of-print 3 July 2006 KEYWORDS Aims Non-compaction of the left ventricular myocardium (NCVM) is reportedly exceedingly rare and associated with a high morbidity and mortality. A different genetic background has been suggested for NCVM with [non-isolated NCVM (ni-NCVM)] and without [isolated NCVM (i-NCVM)] other congenital heart defects. We prospectively evaluated both the NCVM subgroups regarding frequency of occurrence and cardiovascular complications in a paediatric population. Results In a prospective, single-centre study, 66/5220 consecutive patients (1.26%) were diagnosed (25 i-NCVM, 41 ni-NCVM). The median age was 4 years (range 0–21), the median follow-up 12 months (range 0–51). The occurrence of congestive heart failure (CHF) at follow-up was 68.0%. CHF was as frequently seen in i-NCVM and ni-NCVM patients (77.5 vs. 62.1%, P ¼ 0.322). The occurrence of arrhythmias (20.0%) and thrombo-embolic events (13.9%) was not different between subgroups. The cardiomyopathy related mortality was 7.1%, with three and one deaths in the i-NCVM and ni-NCVM groups, respectively (P ¼ 0.126). Conclusion When prospectively evaluated, NCVM appears to have been previously under-diagnosed. Whereas arrhythmias and thrombo-embolic events were rare, CHF was frequently found. An equally aggressive anticongestive treatment regimen would seem indicated for both the NCVM subgroups. Introduction Non-compaction of the left ventricular myocardium (NCVM) is a distinct, not yet classified congenital cardiomyopathy.1 It is characterized by numerous, excessively prominent ventricular trabeculations and deep intertrabecular recesses.2 Recently, this entity has been increasingly recognized, but study-based data are limited. Supposedly, it is extremely rare and associated with a high morbidity and mortality.2–6 Although congestive heart failure (CHF) universally is a common finding, observations regarding other cardiovascular complications are less consistent. Early in gestational life, the myocardium is loosely compacted. Blood flow in this avascular sponge-like meshwork of interwoven myocardial fibres with intertrabecular recesses is provided from the ventricular cavity. Compaction of the ventricular myocardium occurs during * Corresponding author. Tel: þ49 40 42803 3718; fax: þ49 40 42803 6826. E-mail address: [email protected] gestational weeks 5–8, progressing from the epicardium towards the endocardium and from the base towards the apex. Simultaneously, the intertrabecular spaces are reduced to capillaries.2,7 NCVM is believed to represent an arrest in this gradual morphogenetic process.2,7,8 The ontogenetic determinants for this arrest are unknown. A heterogeneous genetic background is suspected. Mutations in the gene G4.5 on the Xq28 chromosomal region and in the gene Cypher/ZASP have been linked to infantile cardiomyopathies, including some familial forms of isolated NCVM (i-NCVM).9–13 Mutations in the gene a-dystrobrevin on the 18q12 chromosome and distal 5q35 deletion (CSX gene) were identified in familial NCVM associated with structural congenital heart defects (CHD), i.e. non-isolated NCVM (ni-NCVM).10,14,15 G4.5 mutations were not found in ni-NCVM.10 It only rarely caused i-NCVM in adults.16 Instead, autosomal-dominant adult forms of i-NCVM have been linked to chromosome 11p15 and lamin A/C gene mutations.16,17 In light of the above scarce and somewhat inconclusive data, and a suspected different genetic background for & The European Society of Cardiology 2006. All rights reserved. For Permissions, please e-mail: [email protected] Downloaded from by guest on October 21, 2014 Heart defects, congenital; Cardiomyopathy; Heart failure, congestive; Echocardiography; Non-compaction 1856 i-NCVM and ni-NCVM as outlined above, we sought to prospectively characterize both entities in a paediatric population regarding their frequency of occurrence and cardiovascular complications. C. Lilje et al. multicentre study on dilated cardiomyopathy and myocarditis (www.uni-essen.de/kinderklinik/downloads/protokoll.pdf). The procedures followed were in accordance with institutional guidelines. All patients/patient representatives gave informed consent. Statistical analysis Methods Study sample, design, and diagnostic criteria Results Patient characteristics Sixty-six out of 5220 patients (1.26%) met the criteria for NCVM and were included for further follow-up. The median age at diagnosis was 4 years (0–21). There were 32 female and 34 male patients (48.5 vs. 51.5%). The median follow-up was 12 months (0–51). i-NCVM was found in 25 patients, ni-NCVM in 41 patients. Age at diagnosis, gender ratio, and severity of NCVM were not different between the subgroups (Table 1). Diagnostic methods and morphology The degree of LV non-compaction was mostly moderate and not different between i-NCVM and ni-NCVM patients (Table 1). Autopsy findings, obtained in two neonatal cases, corresponded closely to echocardiographic findings. Mild subendocardial fibrosis was noted in one of them. The fibrotic changes predominately involved the LV apex as a thin layer of thickened endocardium, but was also found in focal areas of the LV-free wall. In both cases, the recesses were covered by endothelium that was in continuity with the ventricular endocardium. The myocyte fascicles were found to be loosely organized, the myocyte fibres abnormally thin and angulated, the number of filaments reduced. One specimen was remarkable for moderate mitochondrial proliferation. Right ventricular biopsies were performed in 14 i-NCVM patients. No proof of an infectious or Table 1 Patient characteristics at diagnosis Figure 1 Method of determining X-to-Y ratio according to Chin et al.,2 X represents the distance between the epicardial surface and the trough of the recesses and Y represents the distance between the epicardial surface and the peak of the trabeculations. X-to-Y ratios were measured at the level of the apex, papillary muscles, and mitral valve. Frequency of occurrence Age (years) median (range) Gender ratio (%) (female:male) NCVM grading Mild Moderate Severe i-NCVM (n ¼ 25) ni-NCVM (n ¼ 41) P-value 0.5% 0.8% 3 (0–21) 8 (0–20) 0.43 52:48 (13:12) 46:54 (19:22) 0.66 5 (20.0%) 17 (68.0%) 3 (12.0%) 8 (19.4%) 28 (68.3%) 5 (12.2%) 0.97 Downloaded from by guest on October 21, 2014 Between September 1999 and May 2002, we evaluated all consecutive patients who were sent for echocardiography. The study design was observational, single-centre, and prospective. The diagnosis of NCVM was made by transthoracic echocardiography in accordance with suggested criteria.2,4–6,18,19 Concurrence of two independent observers was required to confirm the diagnosis. Hypertrabeculation of the left ventricular (LV) with an apical X-to-Y ratio of 0.33 was a prerequisite, where X represents the distance between the epicardial surface and the trough of the recess and Y represents the distance between the epicardial surface and the peak of the trabeculations (Figure 1).2 To quantitate the magnitude of the myocardial non-compaction, X-to-Y ratios were measured at the level of the apex, papillary muscles, and mitral valve. NCVM was graded as mild (apical affection only with an X-to-Y ratio of 0.33–0.26), moderate (two level affection or an apical X-to-Y ratio of 0.25–0.20), or severe (three level involvement or an apical X-to-Y ratio of ,0.20). CHF was graded as mild, moderate/severe, or terminal (CHF-related death or transplant recipient) on the basis of a modified clinical score,20 the intensity of anticongestive therapy (no medication, 1–2 drugs, 3 drugs), and the LV shortening fraction by M-mode echocardiography (.27%, 20–27%, ,20%). Any structural CHD associated with the NCVM, including a muscular ventricular septal defect, qualified for the ni-NCVM group. Like in the previous reports, arrhythmias were considered significant, if they were ventricular and qualified for a Lown class III. Thrombo-embolic events were defined by either visualization of an intracardiac thrombus or typical neurological findings. Initial evaluation included a medical history, a physical examination, a 12-lead electrocardiogram (ECG), and a transthoracic echocardiogram. Follow-up visits were scheduled at 3, 6, 12 months, and 6 monthly thereafter. Follow-up included an interval history, a focused physical examination, a 12-lead ECG, and a transthoracic echocardiogram. Holter monitoring, additional imaging studies like transesophageal echocardiography, magnetic resonance imaging (MRI), scintigraphy, or cardiac catheterization, and therapeutic decisions were performed at the discretion of the primary cardiologist. Right ventricular biopsies were obtained in i-NCVM patients with LV dilatation as part of an unrelated ongoing German Descriptive statistics for continuous variables are presented as median (range). Patient characteristics at diagnosis were calculated by means of Mann–Whitney U test for continuous variables and x2 test for categorical variables. Cumulative event rates at 12 months follow-up were estimated by means of the Kaplan–Meier and the Log-Rang (Mantel-Cox) methods. Ages at occurrence of CHF were compared by means of the Kaplan–Meier method and Mann–Whitney U test. Reported P-values are two-sided. A P-value of ,0.05 was considered statistically significant. All follow-up data were analysed at 12 months after diagnosis using StatView 5.0 (SAS) and STATISTICA 6.0 (StatSoft). Non-compaction of the ventricular myocardium 1857 inflammatory process was found in any of them. MRI did not detect fatty deposits in the myocardium of the 13 patients who were imaged. Associated CHD Ventricular septal defects were the single most frequent lesions. They were found in 11 patients (26.8%) with 90.9% of the defects being muscular. 73.2% of associated CHD were found to be obstructive: 43.9% (18 patients) in the left heart, 29.3% (12 patients) in the right heart, and 7.3% (3 patients) on both sides. The left-sided obstructions comprised six patients with subaortic obstruction, six patients with valvar aortic stenosis including three with a bicuspid aortic valve, and six patients with coarctation of the aorta. The right-sided obstructions comprised one patient with Ebstein’s anomaly/pulmonary stenosis, four patients with valvar pulmonary stenosis, five patients with Tetralogy of Fallot, and two patients with pulmonary atresia/intact ventricular septum. Mortality CHF At diagnosis, CHF for the entire sample was found in 40.9% of patients. At 12 months follow-up, CHF had been detected in 68.0% of patients. The occurrence of CHF was not different between i-NCVM and ni-NCVM patients (77.5 and 62.1%, respectively; P ¼ 0.322) (Figure 2). CHF was at least severe in i-NCVM as in ni-NCVM patients at all times. The median age at diagnosis of CHF was 2.0 years (0.0–21.0) for i-NCVM patients vs. 8.5 years (0.0–18.0) for ni-NCVM patients (P ¼ 0.186). At 12 months follow-up, arrhythmias were found in four patients (20.0%) (Table 3); they were pre-existing in two patients. Their overall occurrence was not different in i-NCVM and ni-NCVM patients (Table 2). Thrombo-embolic events were detected in two patients (13.9%) (Table 3); they were pre-existing in one patient. Although no such events were observed in i-NCVM patients, their occurrence was likewise not different between the groups (Table 2). Discussion We present the largest and the first prospective study on NCVM so far. It is one of the three investigations including ni-NCVM patients. Since the initial report of Chin et al.2 on 8 patients, just about a dozen studies involving at least that many patients have been published (Table 3).4–6,12,16,19,21–24 Six of them comprised exclusively adults.5,6,16,19,22,24 Unlike our study, two of them were focused on genetics and coronary function. Two investigations addressed both the i-NCVM and ni-NCVM,12,21 whereas only one compared these groups.21 Imaging and morphology Universally, echocardiography is considered the diagnostic modality of choice.2,5,8,10,12,18,19,21,25 Colour Doppler was particularly helpful in detecting intertrabecular perfusion from the ventricular cavity. Our two autopsy findings, as in the previous studies,5,26 confirmed the echocardiographic findings of NCVM. Subendocardial fibrosis, if present, is not a diagnostic criterion for NCVM but is probably an ominous prognostic finding indicating ischaemic necrosis. In terms of histology, a mild increase in mitochondrial size and density has been described previously.8,9 To avoid falsepositive diagnoses, we chose a X-to-Y cut-off value of 0.33, which is equivalent to the suggested non-compacted to compacted (N/C) ratio 2.5,12,18,19 However, diagnostic criteria may need refinement.25,27–29 We agree with several more recent investigators that with modern imaging technology, NCVM in children could reliably be diagnosed with an X-to-Y ratio well .0.33 (i.e. a N/C ratio , 2), Table 2 Cardiovascular complications at follow-up i-NCVM Mortalitya (n ¼ 25:41) CHFb (n ¼ 23:37) Arrhythmias (n ¼ 23:37) Thromb-embolic events (n ¼ 23:37) ni-NCVM P-value All NCVM 3 (12.0%) 1 (2.1%) 0.126 4 (6.1%) 17 (77.5%) 1 (5.0%) 24 (62.1%) 3 (34.5%) 0.322 0.369 41 (68.0%) 4 (20.0%) 0 (0.0%) 2 (26.1%) 0.160 2 (13.9%) P-values are given for NCVM subgroup comparison. Follow-up data were analysed at 12 months after diagnosis (median follow-up). Numbers in parenthesis (first column) indicate i-NCVM vs. ni-NCVM patients in whom information was available. a An additional death in the ni-NCVM group was unrelated to both NCVM and CHF. b CHF comprises patients who died from terminal CHF or became transplant recipients (three CHF). Figure 2 Kaplan–Meier estimate of cumulative freedom from CHF to follow-up time. The overall outcome was similarly poor for both subgroups (P ¼ 0.322). ni-NCVM patients experienced a more rapid decline early during follow-up; there were few late new onset CHF cases. i-NCVM patients presented with CHF more frequently; there was a slow but steady decline of freedom from CHF during follow-up. Data were analysed at 12 months (median follow-up time). CHF indicates congestive heart failure; i-NCVM, isolated NCVM; ni-NCVM, non-isolated NCVM; x, event time; o, censored observation time. Downloaded from by guest on October 21, 2014 Five patients died during 12 months follow-up. One death in the ni-NCVM group was unrelated to both the cardiomyopathy and CHF. The cardiomyopathy related mortality was 7.1%. Three patients (14.3%) died in the i-NCVM subgroup and one patient (2.7%) died in the ni-NCVM subgroup (P ¼ 0.126) (Table 2). All deaths in the i-NCVM patients occurred within the first 3 months following the diagnosis. Arrhythmias and thrombo-embolic events 67% 20% 4.0% 45 45:0 3.8a ? 3.0% 73% 65% ? 53% 41% 24% Frequency of occurrence 53% 47% 24% 91% 23% 0% 89% 2.8% 2.8% 35% 8% 0% 48% rare 7.4% 63% 63% 38% Three further studies did not in detail address cardiovascular complications.16,19,29 a Mean+ SD. b An additional death in the ni-NCVM group was unrelated to both NCVM and CHF. 62 62:0 ? 34 34:0 3.7a SD + 3.3 46% To quantify the degree of NCVM, different indices have been applied at different or non-specified wall segments and at different or non-specified points in time during the cardiac cycle.2,10,18,25 In our study, the X-to-Y ratio was applied at three levels with distinct threshold levels. We support Borreguero et al.31 and Petersen et al.25 that measurements should be taken in ventricular diastole rather than in systole to enhance diagnostic sensitivity and specificity. 68% 20% 14% 50a 42a SD + 7 42a ? 17 17:0 2.5a SD + 2.3 59% 3.0 ? 22 22:0 3.9a ? 23% 5.7 (0–15) 27 27:0 6 (up to 17) 7.4% 8.9a ? 8 8:0 ? (up to 5) 38% Age (years) Median (range) n i-NCVML: ni-NCVM Follow-up (years) Median (range) Mortality þheart transplants Heart failure Arrhythmias Thrombo-embolic events Ichida et al.4 3.5 ? 12 5:7 2.6a ? 0% 0.3 (0–17) 36 31:15 3.2 (0.5–12) 24% 4.0 (0–21) 66 25:41 1.0 (0–4.3) 7.1%b ? Sto ¨llberger et al.22 Oechslin et al.5 Wald et al.23 Pignatelli et al.12 Lilje et al. Ritter et al.6 Grading Chin et al.2 Oezk utlu et al.21 likely as high as 0.5.12,25,29 Today, even fetal detection is possible.26 Although NCVM of the right ventricle has been reported in clinical and in autopsy series,6,12,26,29,30 sufficiently precise criteria for a reliable in vivo diagnosis are lacking. The prospectively evaluated frequency of occurrence of NCVM in our study—even if considering i-NCVM patients only—was startlingly higher than one would expect from the early previous reports. Like for other studies, a referral bias has to be accounted for in the setting of a large tertiary care centre. Our institution serves an area of about 3.4 million people. Roughly, 35% of the population is 21 years of age. The low frequency of occurrence referred to previously (0.014–0.045%) unanimously originates from only two studies.6,18 Both studies exclusively addressed adult i-NCVM patients. However, not all NCVM patients survive through adulthood. In adults, echocardiographic windows usually do not permit a similar fine resolution of myocardial structure as in paediatric patients. Even though imaging technology has significantly improved as has the awareness of echocardiographers for the disease, most investigators agree that NCVM is still underdiagnosed.8,18,27,32 It is missed in up to 90% pf patients.4,29 More recent data support a considerably higher frequency of occurrence of i-NCVM,8,12,22,23,32 whereas no previous data have been available for ni-NCVM. Associated CHD Only recently it has been increasingly recognized in paediatric series that NCVM can also accompany diverse forms of structural CHD.8,29 Ventricular septal defects and outflow obstructive lesions were the most frequent associated entities. Both associations have been observed previously.12,22,27,31 It is easily conceivable that the deep intertrabecular recesses present both in the right ventricle and in a non-compacted LV interfere with the formation of an intact ventricular septum leading to muscular septal defects. However, it is not known whether the prominent trabeculations hinder fetal blood flow leading to hyperplasia and outflow obstruction. Or whether the outflow obstruction (in ni-NCVM) accounts for the occurrence of at least some degree of noncompacted hypertrabeculation, which may be functionally different from the hypertrabeculation in i-NCVM. Mortality As in the previous reports,2,4–6,12,23 the mortality in our population was concerning. The difference between the subgroups, though not statistically significant, was remarkable in a setting of small numbers and a high-survival rate. For Downloaded from by guest on October 21, 2014 Table 3 Major clinical studies on NCVM ? C. Lilje et al. Murphy et al.24 1858 Non-compaction of the ventricular myocardium 1859 the i-NCVM patients, our findings were comparable to data provided by Ichida et al.4 Mortality in Oezkutlu’s et al.21 was found to be lower, but it was even higher in the studies by Chin et al.2 and Pignatelli et al.12 as well as in the earlier adult populations.5,6 Paediatric non-survivors are not accounted for in adult series (Table 3). Most previous studies have a longer, but retrospective, follow-up period. No previous data are available on the mortality in ni-NCVM. find evidence of fatty myocardial degeneration in any of the patients studied by MRI. Interestingly, late potentials and prolonged QT dispersion have been found in NCVM by electrophysiological studies.33 In terms of thrombo-embolic events, the non-laminar intertrabecular flow and early CHF certainly constitute the risk factors. CHF The prevalence of NCVM in a non-selected or even general population cannot be determined from this study. A referral bias has to be accounted for in the setting of a large tertiary care centre. Screening for gene mutations was not part of this observational study protocol. The degree to which heart failure in the ni-NCVM group was due to the associated CHD other than the NCVM could not be quantified. Holter monitoring, transesophageal echocardiography, MRI, scintigraphy, and angiography for the detection of arrhythmias and thrombo-emboli were done on clinical indication only. Medication was initiated and modified according to the judgment of the primary cardiologist. Only two autopsies were available. ni-NCVM patients generally had more frequent follow-up appointments than i-NCVM patients. Incomplete follow-up data tend to over-represent symptomatic patients. The follow-up period was relatively short. Conclusion In paediatric patients, both i-NCVM and ni-NCVM appear to have been previously under-diagnosed. As the diagnosis is easily missed, familiarity with the characteristic imaging features is mandatory. Two-dimensional echocardiography including the LV apex assisted by colour Doppler is diagnostic. Arrhythmias and thrombo-embolic events in either group were not nearly as frequent as observed in some previous retrospective (and mostly adult) studies. In contrast, CHF was an overall very common finding. Eventual cumulative freedom from CHF was unusual and not different between the NCVM subgroups. The mortality was concerning in either subgroup. An equally aggressive anticongestive treatment regimen would seem indicated for both NCVM populations. However, i-NCVM and ni-NCVM may carry a different cardiovascular risk, and the risk may be different at different ages. Long-term prospective follow-up studies, possibly including tissue velocity imaging, strain rate analysis, and screening for gene mutations, could help to further characterize this risk. Arrhythmias and thrombo-embolic events Arrhythmias and thrombo-embolic events were observed remarkably infrequently in our series compared to some previous reports. They were generally more common in adult series.5,6,22,24 Also, retrospective studies tend to be biased towards pathologic findings. The early data of Chin et al.2 were based on a small sample size. Our findings are consistent with more recent reports on paediatric patients.3,4,12,21,33 However, previous reports mostly analysed i-NCVM patients only. Besides, we did not routinely screen our patients with Holter monitoring, transesophageal echocardiography, MRI, or angiography unless clinical suspicion was raised. Why NCVM appears to be arrhythmogenic is not known. The suggested conjectural analogy to arrhythmogenic right ventricular dysplasia is appealing.2 However, we did not Acknowledgements The authors thank Bradley K. Taylor, Ph.D. and James L. Reynolds, M.D. for valuable comments and for proofreading of the manuscript. Conflict of interest: none declared. References 1. Richardson P, McKenna W, Bristow M, Maisch B, Mautner B, O’Connell J, Olsen E, Thiene G, Goodwin J, Gyarfas I, Martin I, Nordet P. Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the definition and classification of cardiomyopathies. Circulation 1996;93:841–842. 2. Chin T, Perloff J, Williams R, Jue K, Mohrmann R. Isolated noncompaction of left ventricular myocardium: a study of eight cases. Circulation 1990;82:507–513. Downloaded from by guest on October 21, 2014 CHF is a common finding in most previous observations, especially in paediatric studies (Table 3).2–6,12,22–24 It was by far the most prominent complication in our study. The cumulative freedom from CHF by follow-up time was similarly poor for both subgroups. Though not statistically different, there was a tendency for i-NCVM patients to develop CHF at younger ages than for ni-NCVM patients. ni-NCVM patients were more likely to be evaluated early with a lesser chance of a delayed diagnosis and anticongestive therapy. Besides, there was possibly a more aggressive treatment bias towards ni-NCVM patients and/or a higher recovery rate (e.g. after corrective surgery) in the latter group. Patients with asymptomatic or mild CHF likely presented late in either groups. An at least equally high incidence of CHF in i-NCVM patients as in ni-patients was also observed by Oezkutlu et al.,21 the only other study separately analysing both groups. Several mechanisms may lead to CHF in NCVM. Noncompacted myocardium is more dependent on aerobic oxidation and more sensitive to oxygen deprivation and toxic effects of catecholamines than compacted myocardium.7 Its myosin ATPase activity is lower resulting in a lower contraction velocity.7 Abnormal LV wall motion appearances have been detected by tissue velocity echocardiography with strain rate imaging.28 They were even suggested to be pathognomonic for NCVM. Besides, coronary flow may be affected by lacuno-vascular shunts7,19,33 and a dysfunctional microcirculation. Segmental subendocardial perfusion deficits, possibly leading to subendocardial fibrosis, are detectable by MRI34,35 and have been reported as an unfavourable early prognostic finding.36 On the other hand, inflammatory processes were unlikely to be the cause of CHF in our i-NCVM patients. Finally, as pointed out earlier, emerging evidence suggests a different genetic background for i-NCVM and ni-NCVM.8–17,27 These subgroups may thus carry a potentially different risk for the development of CHF. Study limitations 1860 18. Jenni R, Oechslin E, Schneider J, Attenhofer C, Kaufmann P. Echocardiographic and pathoanatomical characteristics of isolated left ventricular non-compaction: a step towards classification as a distinct cardiomyopathy. Heart 2001;86:666–667. 19. Jenni R, Wyss C, Oechslin E, Kaufmann P. Isolated ventricular noncompaction is associated with coronary microcirculatory dysfunction. J Am Coll Cardiol 2002;39:450–454. 20. Ross R. Grading the severity of congestive heart failure in infants. Pediatr Cardiol 1992;13:72–75. 21. Oezkutlu S, Ayabakan C, Celiker A, Elshershari H. Noncompaction of ventricular myocardium: a study of 12 patients. J Am Soc Echocardiogr 2002;15:1523–1528. 22. Sto ¨llberger C, Finsterer J, Blazek G. Left ventricular hypertrabeculation/ noncompaction and association with additional cardiac abnormalities and neuromuscular disorders. Am J Cardiol 2002;90:899–902. 23. Wald R, Veldtman G, Golding F, Kirsh J, McCrindle B, Benson L. Determinants of outcome in isolated ventricular noncompaction in childhood. Am J Cardiol 2004;94:1581–1584. 24. Murphy R, Thaman R, Blanes J, Ward D, Sevdalis E, Papra E, Kiotsekolglou A, Tome M, Pellerin D, McKenna W, Elliot P. Natural history and familial characteristics of isolated left ventricular noncompaction. Eur Heart J 2005;26:187–192. 25. Petersen S, Selvanayagam J, Wiesmann F, Robson M, Francis J, Anderson R, Watkins H, Neubauer S. Left ventricular non-compaction: insights from cardiovascular magnetic resonance imaging. J Am Coll Cardiol 2005;46:101–105. 26. Moura C, Hillion Y, Daikha-Dahmane F, Eydoux P, Fallet C, Oury JF, Azancot A. Isolated non-compaction of the myocardium diagnosed in the fetus: two sporadic and two familial cases. Cardiol Young 2002;12:278–283. 27. Sto ¨llberger C, Finsterer J. Left ventricular hypertrabeculation/ noncompaction. J Am Soc Echocardiogr 2004;17:91–100. 28. Williams R, Masani N, Buchalter M, Fraser A. Abnormal myocardial strain rate in noncompaction of the left ventricle. J Am Soc Echocardiogr 2003;16:293–296. 29. Burke A, Mont E, Kutys R, Virmani R. Left ventricular noncompaction: a pathological study. Human Pathol 2005;36:403–411. 30. Hook S, Ratliff N, Rosenkranz E, Sterba R. Isolated noncompaction of the ventricular myocardium. Pediatr Cardiol 1996;17:43–45. 31. Borreguero L, Corti R, de Soria R, Osende J, Fuster V, Badimon J. Images in cardiovascular medicine. Diagnosis of isolated noncompaction of the myocardium by magnetic resonance imaging. Circulation 2002; 105:e177–e178. 32. McCrohon J, Richmond D, Pennell D, Mohiaddin R. Isolated noncompaction of the myocardium: a rarity or missed diagnosis? Circulation 2002;106:e22–e23. 33. Junga G, Kneifel S, von Smekal A, Steinert H, Bauersfeld U. Myocardial ischemia in children with isolated ventricular non-compaction. Eur Heart J 1999;20:910–916. 34. Hamamichi Y, Ichida F, Hashimoto I, Uese K, Miyawaki T, Tsukano S, Ono Y, Echigo S, Kamiya T. Isolated noncompaction of the ventricular myocardium: ultrafast computed tomography and magnetic resonance imaging. Int J Cardiovasc Imaging 2001;17:305–314. 35. Borges A, Kivelitz D, Baumann G. Isolated left ventricular noncompaction: cardiomyopathy with homogeneous transmural and heterogeneous segmental perfusion. Heart 2003;89:e21. 36. Soler R, Rodriguez E, Monserrat L, Alvarez N. MRI of subendocardial perfusion deficits in isolated left ventricular noncompaction. J Comp Assist Tomogr 2002;26:373–375. Downloaded from by guest on October 21, 2014 3. Grillo R, Pipitone S, Mongiovi M, Cipolla T, Giudice G, Gagliano S, Sperandeo V. [Isolated non-compaction of left ventricle in childhood: clinical experience with 5 cases]. [Italian]. Italian Heart J 2002;8(Suppl.):858–863. 4. Ichida F, Hamamichi Y, Miyawaki T, Ono Y, Kamiya T, Akagi T, Hamada H, Hirose O, Isobe T, Yamada K, Kurotobi S, Mito H, Miyake T, Murakami Y, Nishi T, Shinohara M, Seguchi M, Tashiro S, Tomimatsu H. Clinical features of isolated noncompaction of the ventricular myocardium: long-term clinical course, hemodynamic properties, and genetic background. J Am Coll Cardiol 1999;34:233–240. 5. Oechslin E, Attenhofer C, Jost C, Rojas J, Kaufmann P, Jenni R. Long-term follow-up of 34 adults with isolated left ventricular noncompaction: a distinct cardiomyopathy with poor prognosis. J Am Coll Cardiol 2000;36:493–500. 6. Ritter M, Oechslin E, Sutsch G, Attenhofer C, Schneider J, Jenni R. Isolated noncompaction of the myocardium in adults. Mayo Clinic Proc 1997;72:26–31. 7. Ostadal B. Comparative aspects of the cardiac blood supply. Advances Organ Biol 1999;7:91–110. 8. Freedom R, Yoo S-J, Perrin D, Taylor G, Petersen S, Anderson R. The morphological spectrum of ventricular noncompaction. Cardiol Young 2005;15:345–364. 9. Bleyl S, Mumford B, Brown-Harrison MC, Pagotto L, Carey J, Pysher T, Ward K, Chin T. Xq28-linked noncompaction of the left ventricular myocardium: prenatal diagnosis and pathologic analysis of affected individuals. Am J Med Genet 1997;72:257–265. 10. Ichida F, Tsubata S, Bowles K, Haneda N, Uese K, Miyawaki T, Dreyer W, Messina J, Li H, Bowles N, Towbin J. Novel gene mutations in patients with left ventricular noncompaction or Barth syndrome. Circulation 2001;103:1256–1263. 11. Chen R, Tsuji T, Ichida F, Bowles KR, Yu X, Watanabe S, Hirono K, Tsubata S, Hamamichi Y, Ohta J, Imai Y, Bowles NE, Miyawaki T, Towbin JA. Mutation analysis of the G4.5 gene in patients with isolated left ventricular noncompaction. Mol Genet Metab 2002;77:319–325. 12. Pignatelli R, McMahon C, Dreyer W, Denfield SW, Price J, Belmont JW, Craigen WJ, Wu J, El Said H, Bezold LI, Clunie S, Fernbach S, Bowles NE, Towbin JA. Clinical characterization of left ventricular noncompaction in children: A relatively common form of cardiomyopathy. Circulation 2003;108:2672–2678. 13. Vatta M, Mohapatra B, Jimenez S, Sanchez X, Faulkner G, Perles Z, Singara G, Lin J-H, Vu T, Zhou Q, Bowles K, Di Lenarda A, Schimmenti L, Fox M, Chrisco M, Murphey R, McKenna W, Elliot P, Bowles N, Chen J, Valle G, Towbin J. Mutations in Cypher/ZASP in patients with dilated cardiomyopathy and left ventricular noncompaction. J Am Coll Cardiol 2003;42:2014–2027. 14. Sadoulet-Puccio H, Feener C, Schaid DJ, Thibodeau SN, Michels VV, Kunkel LM. The genomic organization of human dystrobrevin. Neurogenetics 1997;1:37–42. 15. Pauli R, Scheib-Wixted S, Cripe L, Izumo S, Sekhon G. Ventricular noncompaction and distal chromosome 5q deletion. Am J Med Genet 1999;85:419–423. 16. Sasse-Klaassen S, Gerull B, Oechslin E, Jenni R, Thierfelder L. Isolated noncompaction of the left ventricular myocardium in the adult is an autosomal dominant disorder in the majority of patients. Am J Med Genet 2003;119A:162–167. 17. Hermida-Prieto M, Monserrat L, Castro-Beiras A, Laredo R, Soler R, Peteiro J, Rodriguez E, Bouzas B, Alvarez N, Muniz J, Crespo-Leiro M. Familial dilated cardiomyopathy and isolated left ventricular noncompaction associated with lamin A/C gene mutations. Am J Cardiol 2004;94:50–54. C. Lilje et al.
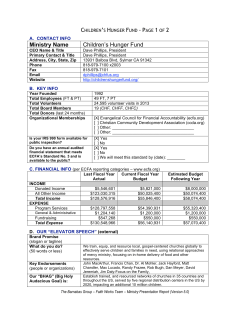
© Copyright 2026