Document 353761
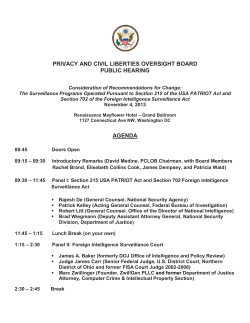
EVALUATION OF SURGICAL SITE INFECTION (SSI) SURVEILLANCE PROGRAMS IN THE ERIE-ST. CLAIR LHIN PHO IPAC Exchange, October 2014 E. Vitale MPH, B. Sc., MLT, CIC OBJECTIVES 1. Provide an overview of 5 participating facilities 2. Describe the purpose of the SSI surveillance Program Evaluation 3. Review the steps involved in program evaluation as applied to SSI surveillance, including the development of a logic model 4. Analyze key results and recommendations based on evaluation 5. Outline next steps OVERVIEW OF 5 FACILITIES Bluewater Health 13% surgical beds Ortho, general, obgyn 3.5 ICPs ChathamKent Health Alliance Leamington District Memorial Hospital 13% surgical beds Ortho, general, obgyn 3 ICPs 100% mixed med-surg beds Ortho, general. Ob-gyn, plastics 1 ICP Windsor Regional Hospital Met Campus 16% surgical beds Ortho, general, obgyn 3.5 ICPs Hotel Dieu Grace Hospital 23% surgical beds Ortho, general, cardiac, thoracic, neuro, plastics, trauma 3 ICPs PURPOSE OF THE EVALUATION PURPOSE OF THE EVALUATION 1. Gain knowledge about the SSI surveillance programs 2. Help improve or modify existing SSI surveillance programs 3. Determine effects of the SSI surveillance programs 4. Affect program participants (particularly members of the surgical program) by acting as a catalyst for change EVALUATION METHODS AND DESIGN EVALUATION METHODS AND DESIGN Literature review of best practices for SSI surveillance including programs in other jurisdictions or countries Development of an assessment / evaluation tool (see logic model) Detailed surveys with ICP leads, as well as surveying other surgical team members An analysis of the SSI surveillance programs data utilizing the assessment / evaluation tool Review infection rates / trends in each facility LOGIC MODEL Resources Activities Short term Outcomes / Outputs Intermediate Outcomes Long term Outcomes Goal Overall goal: to reduce the likelihood of surgical patients developing surgical site infections RESOURCES • Personnel: • Trained in epidemiology and surveillance • Clerical support • Computer and information technology support • Resources Appropriate training for personnel responsible for surveillance and/or data collection ACTIVITIES • Surveillance • Communication of surveillance results • Outcome monitoring Activities OUTPUTS 1. Regular report of procedure specific infection rates and surveillance data to key stakeholders 2. Regular individual reports of surveillance data to individual surgeons 3. Annual summary Short report from IPAC including total term number of surgicalOutcomes patient developing SSIs, clinical, Outputs epidemiologic and/ microbiologic features of patients who have developed SSIs (made available to HCWs caring for these patients) TRANSFER OF ACCOUNTABILITY • If no one, including the ICPs use the surveillance data to alter practice, one must conclude that their current system is ineffective • SSI surveillance programs cannot produce the intended outcome of reducing the likelihood of patient developing an SSI unless members of the surgical program take appropriate action INTERMEDIATE OUTCOMES • Enhanced dissemination of SSI rates and surveillance data • Increase awareness and understanding the impact of SSIs and the population at risk of developing SSIs • Increased ability to investigate cases, determine time Intermediate Outcomes and space clustering, and generate hypotheses about risk factors • Increase in active interventions to reduce SSIs LONGTERM OUTCOMES • Improved assessments of patients at risk of developing SSIs. • Increased ability to determine whether interventions to prevent infection were instituted effectively • Improved use of SSI rates to investigateLong deviations term Outcomes from baseline rates • Increased ability to monitor SSI rates when procedures change OVERALL GOAL • to reduce the likelihood of surgical patients developing surgical site infections (SSIs) DEVELOPING EVALUATION QUESTIONS AND INDICATORS • Evaluation questions were grouped into 4 categories based on what parts of the program were being evaluated: 1. 2. 3. 4. Resources Relevance Process Effectiveness • Indicators were defined for each of the 16 evaluation questions Resources Relevance What resources are required to support current SSI surveillance programs? Do the ICPs in the region utilize the same standard definition for SSIs? Number of personnel with CIC* designation and responsible for SSI surveillance program Number of FTE required to produce current program outputs Number of ICPs using CDC standard case definitions for SSIs Process Effectiveness Who is the SSI surveillance data communicated to? Have active interventions or changes to patient care practices to reduce the risk of SSI been implemented as a result of the SSI surveillance data? Percent of members of surgical team receiving SSI surveillance data per facility Number of facilities reporting active interventions based on SSI data Number rating impact of SSI rates on active intervention as 3 or higher DATA COLLECTION PROCEDURES Group exercise with ICPs using NHSN educational material to review examples of types of SSIs and utilization of the CDC standard case definition Survey for ICPs on planning of program, types of procedures performed, data collected, surveillance actives, and communication of results Engagement survey for surgical program members Review of SSI rates of each facility data submitted by ICPs KEY RESULTS AND ANALYSIS RESPONDENTS • 5/5 lead ICPs • 43 / estimated 120 • ~36% KEY RESULTS • Standard surveillance definitions were used (CDC) • 4/5 facilities reported procedure specific rates • Data collected for each SSI case was almost identical • Surveillance processes varied (especially post discharge) • Limited transfer of accountability (?) or surveys too long (?) RATING THE IMPACT OF SSI RATES • on patient care practice changes as 3 or higher • 10/12 rated 3 or higher • on active interventions to decrease endemic or base line rates as 3 or higher • 9/12 rated 3 or higher • on the ability to assess the efficacy of infection prevention and control interventions as 3 or higher • 10/12 rated 3 or higher REVIEW OF SSI RATES • Unfortunately, accurate numerator (number of SSIs) and denominator data were not readily available for inclusion the in this evaluation. • Due to insufficient data available to perform a statistical analysis, it was not possible to evaluate whether or not a relationship exists between implementation of an SSI surveillance program, and a reduction in the likelihood of SSI. RECOMMENDATIONS Resources More formal training for ICPs Relevance Incorporate retrospective chart review Don’t compare current rates across facilities (too much variation in post discharge surveillance) RECOMMENDATIONS Process Investigate ways to increase effectiveness of transfer of accountability to various surgical teams Effectiveness Educate surgical team members Discuss SSI rates at relevant committees Annually review SSI data and rates LIMITATIONS • Small group – only 5 facilities being evaluated in the region • Self-selection bias • Response bias • Low Response Rate – estimated 36% • Drop out bias NEXT STEPS NEXT STEPS • Facility ICPs provided with summary report • Report recommendations considered per facility ICP / Surgical Program • Decision to establish regional bench mark for SSI identified via readmission for the following procedures • Primary total hip joint replacements • Primary total knee joint replacements • C-Sections • Hysterectomies QUESTIONS / COMMENTS REFERENCES • Centers for Disease Control and Prevention (2011). Introduction to program evaluation for public health programs: A self-study guide. U.S. Department of Health and Human Services Centers for Disease Control and Prevention. Office of the Director, Office of Strategy and Innovation, Atlanta, GA. Retrieved October 16 th, 2013 from: http://www.cdc.gov/EVAL/guide/CDCEvalManual.pdf • Society for Healthcare Epidemiologists of America (2004).Practical Handbook for Healthcare Epidemiologists 2 nd Edition. New Jersey, USA, SLACK Incorporated. • Zimlichman, E., Henderson, D., Tamir, O., Francz, C., Song, P., Yamin, C.K., Keohane, C., Denham, C.R., and Bates, D. W. (2013). Health Care-Associated Infections: A Meta-analysis of Costs and Financial Impact on the US Health Care System. JAMA Internal Medicine, 173(22):2039-46. • Shojania, K., Duncan, B., McDonnald K., and Wachter, R. (2001). Making Health Care Safer: A critical Analysis of Patient Safety Practices - Evidence Report/Technology Assessment. Agency for Healthcare Research and Quality; 2001:221-44. Retrieved March 12 th, 2014 from: http://www.ahrq.gov/research/findings/evidence-based-reports/ptsafetyuptp.html • Kirkland, K., Briggs, J., Trivette, S., Wilkinson, W., and Sexton, D. (1999). The impact of surgical-site infections in the 1990s: Attributable mortality, excess length of hospitalization, and extra costs. Infection Control and Hospital Epidemiology. 20(11): 725-730. Retrieved November 22 nd, 2014: http://www.ansell.com/sites/corporate/files/content/brands/The%20Impact%20of%20Surgical%20Site%20Infections%20in%20the%201990s_Kirkland_1999.pdf • Provincial Infectious Disease Advisory Committee (2011). Best Practices for Surveillance of Health Care-associated Infections in Patient and Resident Populations. Ontario Agency for Health Protection and Promotion, Public Health Ontario. Retrieved January 28 th, 2014 from: http://www.publichealthontario.ca/en/eRepository/Surveillance_3-3_ENGLISH_2011-10-28%20FINAL.pdf • Provincial Infectious Disease Advisory Committee (2011). Best Practices for Infection Prevention and Control Programs in Ontario. Ontario Agency for Health Protection and Promotion, Public Health Ontario. Retrieved January 28 th, 2014 from: http://www.publichealthontario.ca/en/eRepository/BP_IPAC_Ontario_HCSettings_2012.pdf • Lee, T., Montgomery, O., Marx, J., Olmsted, R., and Scheckler, W. (2007).Recommended practices for surveillance: Association for Professionals in Infection Control and Epidemiology (APIC), Inc. American Journal of Infection Control J Infect Control , Volume 35:427-40. Retrieved November 11 th, 2013 from: http://www.apic.org/Resource_/TinyMceFileManager/Practice_Guidance/AJIC-Surveillance-2007.pdf • Safer Healthcare Now! (2011). Prevent Surgical Site Infections – Getting Started Kit. Retrieved October 28 th, 2014 from: http://www.saferhealthcarenow.ca/EN/Interventions/SSI/Documents/SSI%20Getting%20Started%20Kit.pdf • Nichols, R. (2001). Preventing Surgical Site Infections: A Surgeon’s Perspective. Emerging Infectious Diseases; 7(2): 220-224. Retrieved November 11 th, 2013 from: http://wwwnc.cdc.gov/eid/article/7/2/70-0220_article.htm • Centers for Disease Control and Prevention (2006). Outline for Healthcare-Associated Infections Surveillance. Department of Health and Human Services. Retrieved November 5 th, 2013 from: http://www.cdc.gov/nhsn/pdfs/outlineforHAIsurveillance.pdf • Centers for Disease Control and Prevention (2012). Protocol for reporting Surgical Site Infections to the National Healthcare Safety Network (in use during 2011). Retrieved October 12 th, 2014 from: http://www.cdc.gov/hai/pdfs/NHSN/9pscSSI-SAMPLE.pdf • Horan, T., Andrus, M, and Dudeck, M. (2008). CDC/NHSN surveillance definition of health-care associated infection and criteria for specific types of infections in the acute care setting. American Journal of Infection Control. 36:309-32. Retrieved October 12 th, 2014 from: http://ac.els-cdn.com/S0196655308001673/1-s2.0S0196655308001673-main.pdf?_tid=7533c6fa-a9f7-11e3-b778-00000aacb35d&acdnat=1394636784_9a9aa7ac0f35b9ba273ffb1efb39009a • Mu, Y., Edwards, J., Horan, T., Berrios-Torres, S., and Fridkin, S. (2011). Improving Risk-Adjusted Measures of Surgical Site Infection for the National Healthcare Safety Network. Infection Control and Hospital Epidemiology; 32(10) :970-986. Retrieved November 12 th, 2014 from: http://www.cdc.gov/nhsn/PDFs/pscManual/SSI_ModelPaper.pdf • Edwards, J., Peterson, K., Mu, Y., Banerjee, S., Allen-Bridson, K., Morrell, G., Dudeck, M., Pollock, D., Horan, T. (2009). National Healthcare Safety Network (NHSN) report: data summary for 2006 through 2008. American Journal of Infection Control;37:783-805. Retrieved October 28 th, 2013 from: http://www.cdc.gov/nhsn/PDFs/dataStat/2009NHSNReport.PDF • Victorian Nosocomial Infection Surveillance System (2013). VICNISS Surveillance Module: Surgical Site Infection (SSI) Protocol. Quality, Safety and Patient Experience Branch, Victorian Government, Department of Health, Melbourne, Victoria. Retrieved October 6 th, 2013 from: http://www.vicniss.org.au/Resources/HCWType1&2Manual/VICNISS_Surveillance_Type1&2_ModuleSSI_1Protocol.pdf • Victorian Nosocomial Infection Surveillance System (2013). VICNISS hospital acquired infection surveillance Annual Report 2009–10. Quality, Safety and Patient Experience Branch, Victorian Government, Department of Health, Melbourne, Victoria. Retrieved October 6 th, 2013 from:http://www.vicniss.org.au/Resources/VICNISSAnnualReport2009-10.pdf • Center for Healthcare Related Infection Surveillance and Prevention (2008). Surgical Site Infection Signal - Section 4. Queensland Health. Retrieved November 12 th, 2014 from: http://www.health.qld.gov.au/chrisp/signal_infection/signal-manual.pdf • European Centre for Disease Prevention and Control (2013). Long-term surveillance strategy 2014–2020. Stockholm: ECDC; 2013. Retrieved November 1 st, 2013 from: http://www.ecdc.europa.eu/en/publications/publications/long-term-surveillance-strategy-2014-2020.pdf • European Centers for Disease Prevention and Control (2012).Surveillance of surgical site infections in European hospitals –HAISSI protocol. Version 1.02, Stockholm: ECDC. Retrieved from: http://www.ecdc.europa.eu/en/publications/publications/120215_ted_ssi_protocol.pdf • European Centers for Disease Prevention and Control (2012). Surveillance of surgical site infections in European hospitals – HAISSI protocol. Version 1.02, Stockholm: ECDC. Retrieved from: http://www.ecdc.europa.eu/en/publications/publications/120215_ted_ssi_protocol.pdf • Harrington, P., Wloch,C., Elgohari, S. and andLamagni, T. (2013). Protocol for the Surveillance of Surgical Site Infection. Public Health England -Surgical Site Infection Surveillance Service. Retrieved November 12 th, 2014 from: http://www.hpa.org.uk/webc/hpawebfile/hpaweb_c/1194947388966 • Center for Health Protection (2009). Recommendations on Prevention of Surgical Site Infection. Scientific Committee on Infection Control, and Infection Control Branch, Centre for Health Protection, Department of Health. Retrieved October 6 th, 2013 from:http://www.chp.gov.hk/files/pdf/recommendations_on_prevention_of_surgical_site_infection_r.pdf • National Collaborating Centre for Women’s and Children’s Health (2008). Surgical site infection prevention and treatment of surgical site infection - Clinical Guideline. Royal College of Obstetricians and Gynaecologists. Retrieved February 13 th, 2014 from: http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0010039/ • Provincial Infection Control Network (PICNet) (2008).Surgical Site Infection Surveillance Working Group’s Strategic Plan and Options Paper Report. Retrieved October 12 th, 2014 from: http://www.picnet.ca/download.php?filepath=%2Fpublications%2F21%2Fattachment.pdf&filetitle=SSI_Working_group_options_paper&extension=pdf • Centers for Disease Control and Prevention (2013). Surgical, Site, Infections (SSI) Case Studies. Retrieved December 8 th, 2013 from: http://www.youtube.com/watch?v=b6bdbjiZgiI • Altman, D. G. (1991). Practical statistics for medical research. London: Chapman & Hall/CRC. • Brenner, E. (2008). Explaining 95% Confidence Intervals. Retrieved March 28 th, 2014 from: https://mail.google.com/mail/?hl=en&shva=1#inbox/1453ed442a14e899
© Copyright 2026