progr am Shaping Future health 1 german arab meDiCal ConferenCe
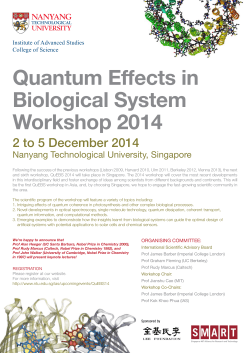
1st German Arab Medical Conference October 24th – 26th 2014 in Berlin progr a m Sh a ping F u t ur e He a lt h Cancer Diagnostics and Treatment multidimensional – interdisciplinar y – interprofessional Charité Comprehensive Cancer Center Suppor ted by: European Centre of Expertise for the Healthcare Industry Deutsch-Arabische Krebskonferenz www.dakk-berlin.de Die Anerkennung als ärztliche Fortbildungsmaßnahme und Bewertung mit Fortbildungspunkten durch die Ärztekammer Berlin (ÄKB) ist beantragt. Fortbildungspunkte können nach der erforderlichen Eintragung in der Teilnahmeliste zum 1. Deutsch-Arabischen Krebskongress beantragt werden. Berlin Medical Association (ÄKB) is requested to certify this conference as part of continuous medical education with CME credit points. You can apply for CME credit points after registration in the list of participants of 1st German Arab Medical Conference in Berlin 2014. 2 1st German-Arab Medical Conference in Berlin Shaping Future Health Cancer Diagnostics and Treatment Deutsch-Arabische Krebskonferenz multidimensional – interdisciplinary – interprofessional Principle Scientific Partner: Charité University Medicine Berlin Organization Partners: Berlin Partner for Business and Technology Chamber of Commerce and Industry of Berlin (IHK) Organizer: German Arab Friendship Association (DAFG) Organizational committee: El Hana GmbH Date: October 24th – 26th 2014 Venue: Chamber of Commerce and Industry of Berlin (IHK) Ludwig-Erhard-Haus Fasanenstraße 85, 10623 Berlin Charité Comprehensive Cancer Center 3 1st German-Arab Medical Conference in Berlin „Shaping future health“ Conference on Cancer Diagnostics and Treatment Berlin-2014 The 1st German Arab Medical Conference in Berlin „Shaping Future Health“ will take place from October 24th - 26th 2014. From 2014 Berlin is going to witness this international medical conference every year. The 1st German Arab Medical Conference in 2014 will focus on „Cancer Diagnostics and Treatment“. The conference is a scientific medical congress for German and Arab physicians from the Arab world, Germany and worldwide. Scientific contributions reflect cutting edge research in diagnostics and treatment. In addition to panels, workshops and poster sessions there will also be a session „Meet the Professor“, offering young physicians from the Arab world the chance to meet Berlin professors and medical specialists who are ready to accompany and guide their postgraduate training. „Berlin Partner for Business and Technology“, Berlin’s official marketing agency, is the principal partner in the conference organization. The scientific Organization committee includes Prof. Dr. Sehouli, Director of Clinic of Gynecology, Charité University Medicine, Berlin ; Prof. Dr. Ulrich Keilholz, acting Director of Charité Comprehensive Cancer Center and Prof. Dr. Abdulgabar Salama, acting Director of Charité Institute for Transfusion Medicine. Arab health ministries and medical institutes of renowned universities are the conference’s principal partners from the Arab world. The Chamber of Commerce and Industry of Berlin (IHK) is partner of the conference representing the commercial health sector. The 1st German Arab Medical Conference will be celebrated under the auspices of His Excellency Prof. Dr. med. Shobokshi, ambassador of the Kingdom of Saudi Arabia in Berlin. The Secretary of State in the Ministry of Economy, Technology and Research of Berlin, Henner Bunde and Dr. Layla Najim, Arab League Director of Health and Humanitarian Aid, will welcome the conference participants at the opening ceremony. Furthermore, „Shaping Future Health“ is the place to network, exchange 4 information and initiate cooperation among German and Arab physicians practicing in Berlin and their colleagues from the Arab world. For the opening ceremony and gala dinner, guests of honor are expected, the Arab diplomatic corps, delegates of Arab and German health policy and chamber of German physicians, as well as executives of Arab and German companies active in health business. Scientific Prospect With this unique congress we want to establish a sustainable platform for the induction and intensification of scientific and clinical projects between Germany and the Arab countries. Based on the existing collaboration in patient care between the Charité and a number of prominent Arab medical institutions, we want to expand these activities. At the German Arab Medical Conference in Berlin we will discuss all important issues concerning frequent diseases with emphasis on differences between German and Arab patients and the relevance of these differences for disease management. The 1st German Arab Medical Conference in Berlin 2014 will focus on cancer. Moreover, this congress will be held immediately after the annual Berlin Health Week, thus enabling conference visitors to get an overall view of Berlin as a health city with world reputation. The conference discussions will cover biomedical research, surgical and medical treatment options and patient counseling considering also the differences in socio-cultural background and health care systems. This multi-dimensional, interdisciplinary and interprofessional approach is absolutely necessary to significantly improve the outcome of our patients. The objective of this conference should be medical education and transfer of knowledge and the initiation of mutual comparative research projects. The envisioned comparative research projects will be highly relevant in order to help closing a huge science gap: There is broad knowledge concerning differences between pathogenesis, molecular disease factors and host contribution to disease between Caucasian and Asian populations, but very little research has been carried out on Arab and African populations. Such research projects are expected to be crucial to fulfill our expectations regarding personalized medicine. 5 We invite all researchers and physicians as well as providers from health care systems from all Arab countries as well as from Germany who are interested in networking and inactivities to optimize current standards. Young physicians and researchers from all over the world are also invited to present their projects during our poster sessions. The best three abstracts will be awarded with a poster price. Partners Charité University Medicine Berlin Partner for Business and Technology Chamber of Commerce and Industry of Berlin (IHK) Berlin Partner for Business and Technology invites her partners, media and journalists from the Arab world and Germany to participate and to cover the congress Participants There are at least 500 participants expected from the Arab world and Germany. Arab physicians from Germany, German physicians, Arab physicians from Arab countries and worldwide are not the only participants expected. The 1st German Arab Medical Conference will also be a forum for representatives of German hospitals with international partners and patients, as well as Arab and German companies involved in the health care sector. • Arab health politicians • German health politicians • Ambassadors • Health attachés of Arab embassies • Medical specialists • Physicians • Directors of clinics and hospitals • Head physicians • Administrative directors • Media representatives • Experts in Arab German medical cooperation • Representatives of Arab companies in the health sector • Representatives of German companies in the health sector 7 Guests of Honor For the opening ceremony and gala dinner, guests of honor are expected, the Arab diplomatic corps, delegates of Arab and German health policy and chamber of German physicians, as well as executives of Arab and German companies active in health business. Auspices The 1st German Arab Medical Conference will be celebrated under the auspices of HE the ambassador of Saudi Arabia to Germany, Prof. Dr. med. Shobokshi. The Secretary of State in the Ministry of Economy, Technology and Research of Berlin, Henner Bunde and Dr. Layla Najim, Arab League Director of Health and Humanitarian Aid will honor the conference with a welcoming address. Scientific Committee of the 1st German Arab Medical Conference in Berlin 2014 8 • Prof. Dr. med. Abdulgabar Salama Acting director of Institute for Transfusion Medicine, Charité University Medicine • Prof. Dr. Keilholz Acting director of Charité Comprehensive Cancer Center; vice director, medical department hematology and oncology, Charité University Medicine • Prof. Dr. med. Sehouli Director of Gynecological Department, Charité University Medicine Conference Program On Friday, October 24, 2014, the official opening plenary session will take place 9:00 – 11:00, followed by a full program of sessions and workshops, beginning at 11:00 a.m. at IHK Berlin, Ludwig-Erhard-Haus, Fasanenstraße 85, 10623 Berlin, to be continued Saturday morning, October 25. Saturday afternoon plenary and reporting sessions will follow. The meeting will conclude with a reception at the Saudi Arabian embassy. Welcoming addresses Message from Deputy Chief Executive of the Berlin Chamber of Industry and Commerce, Christian Wiesenhütter Message from the Secretary of State in the Ministry of Economy, Technology and Research of Berlin, Henner Bunde Message from the Doyen of Arab Ambassadors to Germany, Prof. Dr. med. Shobokshi Message from Dr. Layla Najim, Arab League Director of Health and Humanitarian Aid Message from German Arab Friendship Association, President Dr. Otto Wiesheu Message from the Permanent Secretary, German Ministry of Health, Ortwin Schulte Message from Professor Dr. Jalid Sehouli, Director of the Department of Gynecology. On behalf of the Scientific Committee Message from Professor Dr. Ulrich Keilholz, Acting director of Charité Comprehensive Cancer Center. On behalf of the Scientific Committee 9 Sessions • • • • • • • • • Molecular disease characteristics – is there Arab European diversity? Management of breast cancer Management of colorectal cancer Management of head and neck cancer Management of lung cancer Management of ovarian cancer and other gynecological malignancies Counseling aspects with emphasis on cultural diversity Discussion Session Poster Sessions Ceremonies and Social Program Official opening ceremony Friday, October 24, 9:30 am The official opening ceremony takes place at IHK Berlin, Ludwig-ErhardHaus, Fasanenstraße 85, 10623 Berlin, with welcome addresses of Arab and German high ranking representatives. Gala Dinner Saturday, October 25, 7:30 pm Saturday evening at 7:30 pm we celebrate the opening of the conference with a gala reception including musical performance, gala dinner, welcoming addresses and award presentations at the Hotel Maritim Pro Arte. Berlin Dialogue Sunday, October 26, 10:00 am Reception and résumé of the 1st German Arab Medical Conference in Berlin at the embassy of the Kingdom of Saudi Arabia. 10 Venues Organizer: IHK Berlin, Ludwig-Erhard-Haus, Fasanenstraße 85, 10623 Berlin DAFG e.V. Deutsch-Arabische Freundschaftsgesellschaft e.V. Friedrichstr. 185, Kontorhaus Mitte 10117 Berlin Phone: +49 (0)30. 20 64 88 88 Fax: +49 (0)30. 20 64 88 89 Web: www.dafg.eu Mail: [email protected] Hotel Maritim Pro Arte Friedrichstraße 151, 10117 Berlin Embassy of the Kingdom of Saudi Arabia Tiergartenstr. 33-34, 10785 Berlin Information, Organization: El Hana GmbH Unter den Linden 77 Im Hotel Adlon Kempinski, 10117 Berlin Phone: +49 (0)30. 20 64 58 55 Mail: [email protected] 11 1st German-Arab Medical Conference in Berlin Sessions and workshops 12 Session 1: Plenary Session Friday 24.10.2014 11:00 –13:00 Molecular disease characteristics – is there Arab European diversity? Chair: Prof. Dr. Ulrich Keilholz / Prof. Dr. Hamdi Abd El Azim 1. Colon cancer 11:00 – 11:15 11:15 – 11:30 Prof. Dr. Christine Sers 2. Breast cancer 11:30 – 11:45 11:45 – 12:00 Dr. Barbara Ingold Heppner 3. Head and neck cancer 12:00 – 12:15 12:15 – 12:30 PD Dr. Ingeborg Tinhofer-Keilholz 4. Lung cancer 12: 30 – 12:45 PD Dr. Frederick Klauschen 5. Ovarian cancer 12:45 – 13:00 Dr. Ioana Elena Braicu Prof. Nadia Mokhtar Prof. Nadia Mokhtar Prof. Dr. Alaa El Abouelnasr Session 2: Friday 24.10.2014 14:00 – 16:00 Management of breast cancer Chair: Prof. Dr. Jens-Uwe Blohmer, Prof. Dr. Mostafa Abouelnasr 1. Role of surgery for primary and local advanced breast cancer 14:00 – 14:15 14:15 – 14:30 14:30 – 14:45 Dr. Farkher Ismaeel Dr. Omar Youssef Prof. Hatem Aboul Kassem 2. Role of radiotherapy in curative treatment 14:45 – 15:00 PD Dr. Ulrike Höller 3. Neoadjuvant and systemic therapy of breast cancer: Option for all patients? 15:00 – 15:15 Prof Dr. Jens-Uwe Blohmer 4. Familial breast and ovarian cancer 15:15 – 15:30 Dr. Dorothee Speiser Dr. Elke Rodekamp 5. Treatment of breast cancer during pregnancy 15:30 – 15:45 Dr. Wael Darwish 13 Session 3: Friday 24.10.2014 14:00 – 16:00 Management of colorectal cancer Chair: Prof. Dr. Martin E. Kreis, Prof. Dr. Reinhold Schäfer, Prof. Dr. Alaa El Haddad 1. Role of surgery for primary and metastatic disease 14:00 – 14:15 14:15 – 14:30 Prof. Dr. Johannes Pratschke Prof. Wael Gawad 2. Role of radiotherapy in rectal cancer 14:30 – 14:45 PD Dr. Harun Badakhshi 3. Medical treatment of primary and metastatic colorectal cancer 14:45 – 15:00 15:00 – 15:15 Prof. Dr. Hanno Riess 4. New developments of targeted therapies 15:15 – 15:30 15:30 – 15:45 Susen Burock Session 4: Prof. Hatem Aboul Kassem Dr. Wael Darwish Friday 24.10.2014 16:30 – 18:00 Management of head and neck cancer Chair: Prof. Dr. Ulrich Keilholz, Prof. Dr. Volker Budach, Prof. Dr. Abdulraheem Gari 1. Pathophysiology of head and neck cancer 16:30 – 16:45 PD Dr. Ingeborg Tinhofer-Keilholz 2. Modern radiotherapy for locally advanced head and neck cancer 16:45 – 17:00 17:00 – 17:15 Dr. Carmen Stromberger Prof. Nadia Mokhtar 3. 3. Role of medical treatment for management of advanced head and neck cancer and new developments of targeted therapies 17:15 – 17:30 Prof. Dr. Ulrich Keilholz 17:30 – 17:45 Dr. Wael Darwish 14 Session 5: Friday 24.10.2014 16:30 – 18:00 Management of lung cancer Chair: Prof. Dr. Norbert Suttorp, Prof. Dr. Hossam Kamel 1. Surgery vs. radiotherapy of primary disease 16:30 – 16:45 16:45 – 17:00 17:00 – 17:15 PD Dr. Jens-Carsten Rückert PD Dr. Harun Badakhshi Prof. Wael Abdel Gawad 2. Role of medical treatment for management of advanced lung cancer and new developments of targeted therapies 17:15 – 17:30 Caroline Anna Peuker Session 6: Saturday 25.10.2014 9:30 – 11:30 Management of ovarian cancer and other gynecological malignancies Chair: Prof. Dr. Jalid Sehouli, Prof. Dr. Omar Sharif 1. Diagnostics 9:30 – 9:45 Dr. Ioana Braicu 2. Pathology 9:45 – 10:00 Dr. Wolfgang Schmitt 3. New Aspects of Surgery in Ovarian Cancer 10:00 – 10:15 Dr. M. Z. Muallem 4. Current aspects of surgical and medical therapies in relapsed ovarian cancer 10:15 – 10:30 Prof. Dr. Jalid Sehouli 5. Current aspects of surgery in cervical and endometrial cancer 10:30 – 10:45 Dr. Jihad Dowaji 6. The application of Jasargil Clip in radical vaginal Trachelectomy make it easier 10:45 – 11:00 Dr. Shadi Younes 7. Role of robotic surgery in gynaecological cancers 11:00 – 11:15 PD Dr. Mandy Mangler 15 Session 7: Saturday 25.10.2014 12:30 – 14:00 Counseling aspects with emphasis on cultural diversity Chair: PD Dr. Jonas Felix Busch / PD Dr. Dirk Böhmer 1. Informing a patient on therapeutic options, shared decision making 12:30 – 12:45 PD Dr. Jonas Felix Busch 12:45 – 13:00 PD Dr. Dirk Böhmer 2. Patient expectations from doctors and other health care professionals 13:00 – 13:15 Prof. Dr. Jalid Sehouli 3. Counseling in palliative care, diversity in core values and expectations 13:15 – 13:30 PD Dr. Anne Letsch 4. Perspectives of Traditional European, Arabian and Asian Medicine in Integrative Oncology 13:30 – 13:45 Prof. Dr. Andreas Michalsen 5. Pain management in cancer and non-cancer pain“ 13:45 – 14:00 Prof. Dr. Michael Schäfer Discussion Session Saturday 25.10.2014 14:30 – 15:30 Dr. Layla Nijem (Arab League), Prof. Dr. Ulrich Keilholz Prof. Dr. Jalid Sehouli, Prof. Dr. Reinhold Schäfer, Prof. Wael Gawad 1. How to create an efficient German Arab research consortium 2. Meeting summary and future perspectives (½ hr) 16 Workshop: Saturday 25.10.2014 16:00 – 17:30 Allogeneic stem cell transplantation Chair: Prof. Dr. Renate Arnold 1. Indications and Results Prof. Dr. Renate Arnold / Dr. Mohammad Ahmed A Shinawi 2. Doner Selection Dr. Constanze Schönemann 3. Transplant Dr. Olga Abach 4. Supportive Care Prof. Dr. Renate Arnold / Dr. Mohammad Ahmed A Shinawi Poster Session Saturday 25.10.2014 16:00 • Prof. Dr. U. Keilholz • Prof. Dr. J. Sehouli • Prof. Dr. Mostafa Abouelnasr • Prof. Dr. Abdulraheem Gari Sunday 26.10.2014 10:00 – 12:00 In celebration of Berlin Dialogue: Embassy of the Kingdom of Saudi Arabia Future prospects of German Arab medical cooperation Prof. Dr. med. Shobokshi, Mrs. Layla Nijem (Arab League), Prof. Dr. Ulrich Keilholz, Prof. Dr. Jalid Sehouli Please notice: From Sunday, October, 26 2014 time changes to wintertime in Germany. During the night it changes from 03:00 o’clock to 02:00 o’clock. Subject to alterations | Änderungen vorbehalten! 17 1st German-Arab Medical Conference in Berlin Abstr acts 18 Antero-Posterior Perineal Approach-APPA - for Sphincter Preservation in Ultra Low Rectal Cancer. Oncologic and Functional Outcome. Wael M.S.Gawad, Osman Mansour, Mohammed Lotief, Mona Sakr National Cancer Institute,Cairo University Abstract Background: The perineal dissection through an antero-posterior perineal entry has been introduced to minimize the oncological drawbacks encountered with ultra-low rectal tumours resection (2-5 cm) from the anal verge as Circumferential Resection Margin (CRM) involvement, inadvertent introperative bowel perforation with subsequent increase in local recurrence rate and low overall survival. This approach confers better access to low seated rectal tumours enabling sphincter saving and bowel continuity with better life quality. Methods: Between 2008 and 2012, 35 consecutive patients with low rectal cancer tumours (3-5 cms) from anal verge,underwent ultra low rectal anterior resection with concomitant anteroposterior perineal entry compared to 45 patients with conventional low anterior resection.All patients received neoadjuvant cemoradiation with R0 resection. Patients’data was prospectively collected from our colorectal database. Rates of CRM involvement, bowel, perforation and wound infection were compared. Continence was subjectively evaluated according to Kirwan scale. The sphincter preservation and Colo-Anal Anastomosis (CAA) in the anterioposterior approach was achieved through either hand sewing in 10 patients or double stapling technique in 25 patients with protective ileostomy in 15 patients. Results: The rates of CRM involvement, bowel perforation and wound infection in such approach versus conventional resection were 5% vs 10% (p = 0.04), 5% vs 21.1% (p = 0.521) and 11% vs 31% (p = 0.518) respectively. The mean distal clear margin was 1.5± 0.5 cms (range 0.5-1.7) versus 1±0.3 cms (0.3 - 1.2). Mean Operative time was lower with the perineal entry than with conventional surgery (220.3 & 300 minutes) respectively (p = 0.04). The post operative stay was 10±3 days (range 5-13) compared to 12±5 (range 6-15) in the conventional group. Continence to stool and flatus was achieved in 48 patients (88%) Kirwan scale I, while 7 patients (12%) had control to stools only. 19 Conclusion: This technique facilitates addressing ultra-low rectal tumours, with increased chances for sphincter preservation and bowel continuity concomitant with superior oncologic outcome compared to the conventional techniques suggesting its significance as a valid approach for low seated rectal tumours. Breast conservation of Tx breast cancer: is it feasible? By Hatem Aboul Kassem1, Emad El-Gemeie2 2 1 Department of Surgery, Department of Pathology, National Cancer Institute, Cairo University, Egypt Correspondence to: Hatem Aboul Kassem, Email: [email protected] Aim: Unfortunately, lumpectomy is still the most diagnostic tool for breast carcinoma in Egypt. Management of Tx breast carcinoma is still a controversial issue. Most of these patients are doomed to undergo mastectomy. The aim of this study is to analyze patients with Tx breast carcinoma after having their definitive treatment as regard residual disease in the lumpectomy cavity and factors affecting it. Methods: 60 patients with Tx breast carcinoma who had lumpectomy for a localized breast lump and were proved to be invasive breast cancer were subjected to this study. They were operated from January 2003 to December 2010. Pathologic and patient characteristics were all reviewed. Results: In this sample, the median age of the patients was 45 year, and the median tumor size was 3 cm. 52 patients (86.7%) had mastectomy and 8 patients (13.3%) had conservative breast therapy (CBT). Residual disease was present in 22 patients (36.7%). Margins less than 5 mm had residual tumors in 90.9% of cases. Tumors larger than 2.5 cm in diameter showed residual disease in 52.9% of cases. The other independent factors as age, sex, laterality and grade of tumor had no statistically significant effect on residual tumor. Conclusion: Mastectomy is not the only option for management of Tx breast cancer. Breast conserving therapy is still a valid option provided that a wide safety margin is excised with definitive negative margins. 20 Extending the indications of breast conserving surgery; the oncoplastic approach Omar Z. Youssef M.D, Professor of surgical oncology National Cancer Institute- Cairo University, Egypt Abstract: Background: Surgical management of patients with breast cancer includes either breast-conserving surgery (BCS) or mastectomy with or without reconstruction. Both options have similar rates of long-term survival, but BCS is associated with superior cosmetic and psychological outcomes. A more recent pathway is oncoplastic surgery (OPS) that allows for wider tumor resection with immediate reconstruction of the defect, avoiding mastectomy for a subset of patients, hence extending the indications of BCS for these patients. Patients and methods: This study includes 145 patients with breast cancer, who underwent oncoplastic resection of their tumors. Fifty patients underwent wide local excision and glandular reshaping (WLE+GR), 44 patients underwent therapeutic mammoplasty (TM) and 51 volume replacement procedures (VR) Results: Mean size of tumor in the first 2 groups was 3.1cm (Range 1.8 to 4.7 cm); while in the third group was 3.6cm (Range 2.8 to 8.6cm). The minimal margin width in the first 2 groups was 1.6cm (Range 0.8 to 4.8 m) and in the third group was 2.4 cm (Range 1.4 to 18 cm) Only one patient in VR group, had positive margins and underwent completion mastectomy. None of the patients had delay in their adjuvant treatment. Only one case had local recurrence in the first group after 19 months Conclusion: Although our study has a relatively short follow-up period, however, it confirmed the results of other studies that concluded that OPS is an oncological safe procedure and is a good third option for breast cancer surgery with good oncological and better cosmetic outcome. 21 Groin recurrence in patients with vulvar cancer with pathologically negative nodes on superficial inguinal node dissection H.A. Aboulkassem, A.H. Elaffandi and M.I. Elsherbiny National Cancer Institute, Cairo University, Egypt. Abstract: Objectives The objective of the study is to investigate the causes of the groin recurrence in patients with carcinoma of the vulva who had negative nodes in their superficial inguinal node dissection (SIND) specimens. Material and methods A prospective nonrandomized trial has been conducted in the period between 2005 and 2009 on 41 patients having squamous cell carcinoma of the vulva. The depth of invasion was more than 1 mm in all cases. Stage I included 13 patients and stage II included 26 patients. The number of patients who had unilateral sited lesions was 24 (4 had lesions within 1cm from the midline). The number of patients who had bilateral sited lesions was 17.They were then subjected to the standard treatment in the form of radical local excision with a safety margin 2 cm confirmed using intraoperative frozen section and SIND either in the form of unilateral inguinal dissection (20 patients) or bilateral inguinal dissection (21 patients). Among these patients 7 experienced groin recurrence that involved both side (1 patients) and one side (6 patient). Patients who suffered groin recurrence have been thoroughly investigated using CT pelvis and groin to exclude the presence of iliac nodes and to detect roughly the state of the vessels which was further evaluated using colored Doppler ultrasound. The recurrent cases have been subjected to deep inguinal nodal dissection (1 patient required ilioinguinal nodal dissection). No femoral vessel resection has been needed however femoral nerve resection has been done in 1 patient. Sartorius transposition has been done to protect the vessels after complete resection. Two patients required reconstruction of the skin defect using myocutanious flaps. In addition to the histopathological study of the resected nodes more slides were reviewed (5 sections from paraffin block of the previously resected superficial inguinal nodes) to exclude micrometastasis. 22 Results The median age at diagnosis and primary surgery was 59 years and the median depth of invasion was 4mm (more than 5 mm in recurrent cases). The size of the primary tumor ranged from 1.8 cm to 4.3 cm in the non recurrent cases while the range was 3 cm to 4.5 cm in recurrent cases. Six patients underwent unilateral groin dissection and one patient underwent bilateral groin dissection. The mean number of the lymph nodes removed per groin was 8 with an average size ranging from 0.4cm to 3.5cm. The median time to recurrence was 21 months. On examining the resected recurrent tissue, it has been found that in 1 patient recurrence has been identified in fibro adipose tissue. In the remaining 6 patients nodal tissue has been detected in the resected specimens. No micrometastasis has been detected in the reviewed slides. Conclusion We suggest that the groin relapse in patients with negative nodes on SIND is caused by metastatic disease in unresected inguinal nodes. All of the recurrent cases had stage II disease (size of the primary tumor > 3 cm while the depth was > 5 mm). SIND does not eliminate all the sites of the possible nodal metastasis in patients with the above mentioned measurements (stage II) Accelerated Balloon-Occluded Retrograde Transvenous Obliteration Of Gastric Varices Without Retaining The Occlusion Balloon Using A Terminal Gel Foam Plug in HCC Patients. Wael Darwish Abstract: Balloon-occluded retrograde transvenous obliteration in four consecutive cirrhotic HCV positive, Hepatocellular cancer (HCC) patients with gastric varices without indwelling balloon catheter occlusion, aiming to prevent gastric variceal bleeding. The four patients presented with HCC for treatment and the gastric varices was discovered on their initial or follow-up MRI or CT scans. 23 Methods: Alcohol was mixed with iodized oil and room air as much as possible to form a concoction that was injected in a retrograde fashion through the relatively small gastrorenal shunts, followed by a thick absorbable gelatin sponge plug under only 10-minute balloon occlusion (without keeping an indwelling balloon). CT & or endoscopy were performed within a month to monitor the gastric variceal occlusion/thrombosis and follow-up the esophageal varices. MELD score, Child-Pugh scores and the rest of renal and liver function labs were obtained as well as a complete blood picture were performed before and after the procedure periodically. Results: All four balloon-occluded retrograde transvenous obliterations were technically successful. No instilled sclerosant migration occurred after deflating and removing the balloon occlusion catheter. No procedural complications occurred. There was prompt prevention of the anticipated gastric variceal bleeding, at a mean clinical follow-up of nine months with complete thrombosis of the the gastric varices. Conclusion: Because complete obliteration of gastric varices was achieved in all patients without any complications, our technique is considered to be safe and effective for small gastric varices in cirrhotic HCC patients. First Author: Wael M. Darwish, MD, MSc. A. Lecturer of Radiology, Medical Director of VIR, National Cancer Institute, Cairo University. [email protected] +201000709702 Co-author: Ikram H. Mahmoud, MD, PhD Professor & Chairman of Radiology and Image guided Interventions, National Cancer institute, Cairo University. [email protected] +201001456261 24 Early Results of NCI, Cairo University in chemo-embolization of HCC in cirrhotic, HCV positive patients using Hepaspheres 30-60 & 50-100 microns with a restrict inclusion criteria and a unified maximum treatment dose. Wael Darwish Abstract: This study was started May, 2013 to examine the efficacy of trans-arterial chemo-embilization of hepatocellular carcinoma (HCC) in hepatitis C virus (HCV) positive cirrhotic patients using a superabsorbent polymer drug eluting embolic material. Methods & Early results : One hundred and seventy six patients with documented HCV positive results, cirrhosis and HCC, Child-Pugh score A, ECOG performance status 0-2 and having one to three lesions not amenable to ablation or resection. Hepaspheres 50-100 microns were used in one hundred and forty eight patients with a maximum dose of 50 mg Doxorubicin prepared on 50 mg hepaspheres per session. Hepaspheres 30- 60 microns were used in twenty eight patients with a maximum dose of 50 mg Doxorubicin prepared on 50 mg hepaspheres per session. All the lesions were embolized using various 5 F. catheters to select the Celiac axis, Superior mesenteric, right renal, inferior phrenic, intercostal, right internal mammary and left gastric arteries, then superselection of the feeding arteries as possible was done using Renegade Hi-flow microcatheter over 0.018 inch or 0.014 inch transcend microwire before the start of embolization. Arterio-venous shunting within or around the lesions were dealt with according to the presentation if found. All the needed labs were repeated after each embolization session by 21 days and a follow-up Dynamic MRI/DTI-ADC map was performed in the fourth week post-embolization. A period of 3-4 weeks was left between embolization sessions if more than 1 embolization session was needed. If a complete response was reached the MRI is then performed after 3 months from the last MRI examination, and if there is no new lesions or recurrence it’s then performed every 6 months. Response rates were calculated on intention to treat basis with complete response (CR) 22.4% reaching 27.8% for the targeted lesions. Over all 25 partial response (PR) was seen in 53.3%, stable disease in 15.1%, and progressive disease 9.1% of patients. Overall objective response (CR+PR) was seen in 75.7% of cases. Until August 2014 Mortality rates were 0% at 1 & 6 months and 2.1 % at 1 year (1 patient from the 47 patients who passed a year from the start of treatment) due to progressive liver cell failure/hematemesis. Conclusion: Drug eluting chemoembolization using hepaspheres is an effective modality of treatment for HCC in HCV positive patients that needs to be more evaluated on larger samples of patients and on longer periods of followup that will be continued in our study. First Author: Wael M. Darwish, MD, MSc. A. Lecturer of Radiology, Medical Director of VIR, National Cancer Institute, Cairo University. [email protected] +201000709702 Co-author: Ikram H. Mahmoud, MD, PhD Professor & Chairman of Radiology and Image guided Interventions, National Cancer institute, Cairo University. [email protected] +201001456261 Patterns of failure and Predictors of recurrence for urothelial bladder cancer after Radical Cystectomy: an Egyptian study performed at the National Cancer Institute, Cario University Hatem Aboul Kassem Abstract Background: Radical cystectomy remains the gold standard for local control of muscle invasive bladder cancer for decades. Despite this radical surgery, a significant proportion of patients develop disease recurrence. A detailed review of literature revealed a significant number of studies dealing with the patterns of failure/recurrence, and the predictive factors 26 associated with recurrence. The implications of such predictive factors on development of recurrence will help in modification of treatment strategies, in an aim to improve the prognosis of bladder cancer. Methods: This is a retrospective case-control study on patients with transitional cell carcinoma who underwent radical cystectomy at the National Cancer Institute in the three-year period between January 2007 to December 2009, and analyzed for the development of recurrence and potential risk factors. Results: Our study included 166 males (87.8%) and 23 females (12.16%). Their median age was 62 years (range: 31-85). One and five-year disease free survival rates were 77.2% and 53.6% respectively. Seventy one patients (37.56%) developed disease recurrence during the follow-up period. Of these recurrences; 17 patients (23.9%) were local and/or regional, while 45 (63.38%) developed distant metastasis, and eight (11.26%) developed both local/regional and distant recurrences. Site of recurrence was not documented in one patient. The most common site for distant metastasis was the skeletal system. On univariate analysis; lymph node metastasis (p<0.001), lymphovascular invasion (p<0.001), high grade (p=0.012) and extravesical extension (p=0.033) were positively associated with development of recurrence. On multivariate analysis, lymph node metastasis, lymphovascular invasion and high grade are associated with tumor recurrence and poor disease-free survival. Conclusions: Lymph node metastasis, lymphovascular invasion and high grade are independent factors affecting tumor recurrence and diseasefree survival. Other factors should be taken into account when assessing patient prognosis after radical cystectomy to improve accuracy and aid decision making. Keywords: Urothelial carcinoma - Radical cystectomy - Predictors of recurrence 27 Pelvic Exentration and Composite Sacral Resection In the Surgical Treatment of locally Recurrent Rectal Cancer. Wael Gawad, Medhat Khafagy, Mohamed Gameil, Moustafa Negm, Nadia Mokhtar, Mohamed Loutaef, Osman Mansour National Cancer Institute - Cairo University, Cairo, Egypt. Abstract Background The incidence of rectal cancer recurrence after surgery is 5-45%. Extended Pelvic resection such as pelvic exentration and abdominosacral composite resection which entails Enbloc resection of the tumour and adjacent involved organs provide the only true possible curative option for patients with locally recurrent rectal cancer. The Aim of this study is to evaluate the surgical and oncological outcome of such treatment. Methods: Between 2006 and 2012 a consecutive series of 40 patients with locally recurrent rectal cancer underwent abdominosacral resection (ASR) in 18 patients, total pelvic exentration with sacral resection in 10 patients and pelvic exentration in 12 patients. Patients with sacral resection were 28, the level of sacral division was at S 2/3 interface in 10 patients, S 3/4 in 15 patients and S 4/5 in 3 patients. Results: Forty patients, male to female ratio 1.7:1, mean age 45 years (range 25 – 65 Y) underwent extended pelvic resection in the form of pelvic exentration and Abdominosacral resection. Average blood transfusion was (0.4-6L), median hospital stay was 21 (range 7-52) days. The Morbidity, Readmission and Mortality rates were 55%, 15% and 5% respectively. The reported surgical complications were as such, wound gap in 10 patients, neurogenic bladder in 9 patients and enteric fistula in 9 patients. Mortality occurred in 2 patients due to enteric fistula and abdominal sepsis. A R0 and R1 sacral resection were achieved in 63% and 37% respectively. Thirty five patients underwent curative resection, they showed significantly improved survival with 5-year survival rate of 26.3% compared to 5 patients with palliative resection in a survival rate of 0%.Conclusion: Extended pelvic resection as pelvic exentration and sacral resection for locally recurrent rectal cancer are effective procedures with tolerable mortality rate and acceptable outcome. The associated morbidity remains high and deserves vigilant follow up. 28 Profile of Cancer Pathology in Egypt and the Role of Markers in Patients’ Management Nadia M. Mokhtar, MD, PhD Professor of Pathology National Cancer Institute, Cairo University Figure 1: A 12-year Cancer Pathology Registry, Mokhtar et al 2014, NCI, Cairo University Cancer Pathology Registry at the Department of Pathology of the National Cancer Institute (NCI), Cairo University is a periodical documentation data, regularly published by NCI. The recent issue of 2014 draws the relative frequency data of tumors and forms a detailed profile for a hospital-based registry allowing for a dynamic profile with time trend analysis. The material is presented with recent pathologic classifications, grading, and staging, including immunohistochemical and molecular test applications. Biopsy, specimens, frozen sections, FNAC procedures are applied when appropriate. The most frequent 4 systems presented in this registry are the breast, GIT, Urinary system, and lymphoid neoplasms (figure 1). Breast cancer forms a majority of 36% of female cancers with a T2 stage predominance and high lymph node involvement in more than 70% of cases. All cases are routinely tested for hormone receptors (ER and PR), Her-2/neu, and Ki-67 by automated immunohistochemistry. In situ hybridization (CISH) is applied in selected cases. Oncotype DX is applied to a few early breast cancer cases. Material is sent abroad for this test. Urinary system is the second most common due to high incidence of 29 schistosoma-associated bladder carcinoma (endemic bilharziasis). A close association was noted between the parasitic infestation of schistosoma hematobuim and the causation of bladder cancer with special clinicopathologic features, confined to the endemic area. However, lately during the last 2-3 decades a change was noticed and documented in subsequent Pathology Registries. A significant decline of the relative frequency of bladder cancer was decreased from 27% in old series to 12% in recent ones. Bilharzial association dropped from 82% to 55%. This is attributed to better control of bilharziasis by the Egyptian Ministry of Health in the rural population in Egypt. The change is also reflected on the histopathologic types. There was a significant decrease in squamous carcinoma, previously predominated and rise of transitional cell carcinomas from 16.0% to 60%, becoming at present the most common tumor type in bladder cancer. Such a pattern is approaching that of the Western World. The digestive and hepatobiliary systems form 20% of total malignancies. Colorectal cancer is the most common with predominance of T3 and high grade tumors. Routine molecular ras testing is done for metastatic cases prior to targeted therapy. Also GIST tumors are common in GIT with routine c-kit immunostaining for established diagnosis and prior to targeted therapy. Molecular testing for exon 9 is applied on resistant metastatic cases. Hepatocellular carcinoma shows a high rise in incidence in recent registries due to high HCV infestation and endemic pattern. Most tumors arise on top of liver cirrhosis and active interface hepatitis. Malignant lymphomas are the 4th most common tumors in the registry. Cases show a predominance of non-Hodgkin lymphoma forming 72%, while Hodgkin lymphoma forms 28%. There is a predominance of B-cell NHL of 84% and diffuse large B-cell lymphoma is the most frequent subtype of lymphoma, forming half of the cases. Small lymphocytic lymphoma forms only 6% and follicular lymphomas a low of 4%. Automated immunohistochemical stains are used routinely for accurate phenotyping and subtyping. Markers used are mainly CD20, CD3, CD43, LCA, CK, CD30, CD15, CD10, CD23, CD5, CD10, CD21, bcl-2, cyclinD1, kappa, lambda. Ki-67, MUM1, and bcl-6. Gene rearrangement tests are applied in difficult cases. Other less frequent systems are shown in Figure 1. Immunohistochemistry and molecular markers like EGFR, kras, and ALK are applied in some cases of lung cancer prior to targeted therapy. 30 Pre-operative Placement A Supra-renal (infra-atrial) IVC Filter in Cases of Renal/Adrenal Tumors with Tumoral Venous Thrombi Extending into the IVC to Prevent Accidental Intra-operative Pulmonary Embolism. Wael Darwish Abstract: A total of four patients, 3 males with Renal cell cancer (RCC) and 1 female angiomyolipoma received a supra-renal infra-atrial (Inferior Vena Cava) IVC filters, and two of them underwent pre-operative bland renal arterial embolization to prevent intra-operative tumoral pulmonary embolism , and reduce intra-operative blood loss respectively. Methods: A triphasic CT scan was performed prior the procedure, with a CT venography, the distance from the top of the thrombus to the right atrium (patent infra-atrial IVC was measured ) with a mean of 4.5 cm. A right Internal Jugular access was used to perform an IVC venogram through an eleven French sheath and a Universal Cook Celect Filter was placed through the same access. Radical nephrectomy and thrombectomy was performed within two days. Three weeks CT follow-up was performed. Results: Technical success was 100% (to place the filter). The three weeks followup showed no pulmonary or IVC residual thrombi, filter fracture, wall penetration or migration, however a filter tilt was noted in one case with hook projecting into the hepatic veins confluence. Conclusion: Placing a pre-operative infra-atrial (supra-renal) IVC filter is a technically safe procedure that should be adopted by Interventional radiologists to reduce radical nephrectomy/tumoral IVC thrombectomies. First Author: Wael M. Darwish, MD, MSc. A. Lecturer of Radiology, Medical Director of VIR, National Cancer Institute, Cairo University. [email protected]; +201000709702 31 Co-author: Ikram H. Mahmoud, MD, PhD Professor & Chairman of Radiology and Image guided Interventions, National Cancer institute, Cairo University. [email protected]; +201001456261 Targeted chemo infusion for local control of invasive breast cancer utilizing a retrograde subclavian artery resivoir post-redistribution of the breast bed arterial supply. Wael Darwish Lecturer of Interventional Radiology National Cancer Institute, Cairo University Abstract: Purpose: To describe the technique and evaluate effectiveness of a retrograde reservoir directed subclavian artery chemoinfusion with redistribution of the mammary vascular bed by obliterating the internal mammary artery (IMA). Materials and methods: A prospective study was performed in May 2008. Patients with locally advanced primary tumor (stage > = IIIb). Prior radiation therapy was the only exclusion. The ipsilateral brachial artery was accessed and the axillary artery was cannulated in a retrograde fashion. The IMA was embolized utilizing N-butyl cyanoacrylate and lipiodol to redistribute the arterial supply to the breast to make it solely from the subclavian branches. A 5-French (tapered to 3.3-French) catheter was placed with its tip distal to the takeoff of the IMA and vertebral artery and connected to a port-a-catheter reservoir placed in a forearm subcutaneous pocket. Chemotherapeutic agents were administered weekly via the reservoir starting intraoperatively. Administered agents included 30 milligrams Adriamycin (intraoperatively), 750 milligrams of 5-Flurouracil and 10 milligrams of Cisplatimum. This was repeated for 3-6 months. Tumor response was by CT tumor volumetry and graded by Response Evaluation Criteria in Solid Tumors [RECIST: complete response (CR), partial response (PR), and Stable disease (SD) represented 100%, >50%, and <50% tumor reduction respectively]. 32 Results: 5 patients were enrolled. 1 patient had hand gangrene at 2 weeks, and a foot gangrene at 8 weeks. The remaining 4 patients had a RECIST PR (50% tumor reduction) achieved at 1.1 - 4.3 months (mean 2.3 months). Conclusion: Locoregional subclavian artery weekly chemo infusion with arterial bed redistribution by occluding the IMA is effective. Targeted irinotecan eluting hepaspheres arterial embolization of hepatic metastatic colorectal cancer. Wael Darwish Lecturer of Interventional Radiology National Cancer Institute, Cairo University Abstract: Purpose: To evaluate effectiveness of arterial embolization of hepatic colorectal metastatic liver disease using Irinotecan eluting hephaspheres. Materials and methods: A prospective study is being performed from February 2012 in NCI, Cairo University, Egypt. Patients who underwent surgical resection of the primary colorectal cancer, having or later developed liver metastatic disease. The patients could have started systemic chemotherapy or with concomitant chemotherapy at the time of arterial embolization. CT &/or MRI was performed on the liver as well as the operative bed to define the extent of the metastatic liver disease and evaluate the operative bed. A right common femoral artery access was done, followed by imaging of the superior mesenteric artery, Celiac axis, hepatic artery, left gastric and phrenic, right renal arteries if was indicated by a 5 French catheter. further selection of the hepatic artery branches was performed using a 2.8 French microcatheter that was used for injecting the prepared Irinotecan (100 mg/2 ml) eluting (50 mg) 30-60 microns hepaspheres. Stopping the injection was considered after stopping of the arteriolar flow on angiography. This was repeated four weeks if there is residual on the Dynamic liver MRI (Magnetic Resonance Imaging) +/- DTI (Diffusion Tensor Imaging) in the early fourth week. Tumor response was by MRI tumor volumetry, Diffusion facilitation, and decrease or disappearance of lesion contrast enhancement. 33 Results: twelve patients were enrolled till now. 6 patients had disappearance of vascular enhancement, and diffusion facilitation with later reduction in the tumor volume after an average of 2.1 sessions and are under follow up after 3 months, then every 6 months by Dynamic MRI/DTI. Two patients had partial response of more than 30% reduction of all the above mentioned criteria. Two patients had stable disease. Two patients had progressive disease with stopping of treatment due to high bilirubin due to peripheral bile ducts obstruction even after bilobar biliary drainage. The other one after refusing further treatment after 13 months of followup following the first two sessions. Conclusion: Catheter directed (targeted) Irinotecan hepasphere arterial embolization of colorectal liver metastases is of value, yet larger volumes of patients are needed for further evaluation of the modality. The Incidence and Distribution Of Cancer In the Arab world and Egypt. Wael Gawad The Arab world includes 22 countries with a total population of nearly 362 million. The Urban / Rural population split is about 55.8/45.2 %. The Arab world has the following common epidemiological features which contribute to the profile of cancer problem; (1) High incidence of infections and Malnutrition. (2) Young population age. (3) Increasing industrialization and urbanization accompanied by lack of protective measures. (4) High Solar exposure. (5) Inadequate public awareness leading to late case presentation. Cancer Registration is a vital tool for sizing the cancer problem, hence determing the strategic planning for treatment, control and prevention. 34 The Cancer profile among Arab countries is characterized by a high frequency of Breast, Prostate, Bladder, Colo-Rectal, Lung , Liver, Oesophagus and Cervix . Relatively high frequency rates of lung Cancers were reported from Baharain, Tunisia, Libya, Moraco and Algeria. In Egypt ,the mean age of Cancer Patients is 48 years, nearly two decades younger than western patients. According to the National Cancer Registry, there is a slight male predominance in cancer ratio 1.05 : 1. The leading cancers among Egyptian Patients according to the National cancer Registry are: Breast, Urinary Bladder, NHL, Liver, Lung, Leukaemia, Colorectal, Brain, CNS, prostate & ovary. Unser Dank geht an die Sponsoren der Veranstaltung: Roche Deutschland Holding GmbH 6.000 €, Europäische Branchenkompetenzzentrum für die Gesundheitswirtschaft 4.000€, Novartis Oncology 4.000 €, W.O.M. WORLD OF MEDICINE GmbH 2.000 € 35 www.dakk-berlin.de Venues IHK Berlin, Ludwig-Erhard-Haus, Fasanenstraße 85 10623 Berlin Hotel Maritim Pro Arte Friedrichstraße 151 10117 Berlin Embassy of the Kingdom of Saudi Arabia Tiergartenstr. 33-34 10785 Berlin Organizer: DAFG e.V. Deutsch-Arabische Freundschaftsgesellschaft e.V. Friedrichstr. 185, Kontorhaus Mitte 10117 Berlin Phone: +49 (0)30. 20 64 88 88 Fax: +49 (0)30. 20 64 88 89 Web: www.dafg.eu Mail: [email protected] Information, Organization: El Hana GmbH Unter den Linden 77 Im Hotel Adlon Kempinski, 10117 Berlin Phone: +49 (0)30. 20 64 58 55 Mail: [email protected]
© Copyright 2026