INTRODUCTION to be older with multiple co-morbidities, more
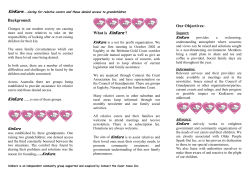
R.I.S.E for the prevention of pressure ulcers Reposition, Inspection, Skin care, Eat well (R.I.S.E.) – Information leaflet for carers for pressure ulcer prevention Georgina Gethin, Member of the EWMA Council PhD, RGN, PG Dip Wound Healing, FFNM RCSI, Dip Anatomy, Dip Applied Physiology, MSc (c) Clinical Research. Senior Lecturer, School of Nursing and Midwifery, National University of Ireland, Galway, Ireland Professor Caroline McIntosh, PhD, BSc (Hons), MSc, MChS. Head of podiatry, School of Health Sciences, National University of Ireland, Galway, Ireland Correspondence: georgina.gethin@ nuigalway.ie Acknowledgements We are grateful for the funding from the EXPLORE team at NUI Galway (Wound Management Association of Ireland [Western branch]) and the valuable feedback and contributions from many colleagues. Conflits of interest: None 52 INTRODUCTION Pressure ulcers are a significant health care issue that affect up to 18% of hospitalised patients and 3-10% in the home care setting. They also represent 4% of the caseload of community nurses1, 2. These ulcers are a major source of morbidity, and they cause pain, depression, and the reduced quality of life in the individual. In some cases, death may occur. In addition, they constitute a significant cost to the health service, the patients, and their families3. Pressure ulcers are defined as a localized injury to the skin and/or underlying tissue. They usually develop over a bony prominence as a result of pressure itself or in combination with shear and/ or friction4. Attempts to prevent pressure ulcers are varied and include approaches, such as risk assessment, pressure re-distributing devices, and local and regional health care initiatives, including education programmes for staff and patients and the introduction of clinical care pathways. Although all health care professionals have a role and responsibility in pressure ulcer prevention, the current situation of more people receiving health care in the home care setting means that informal carers are increasingly in the front line for prevention strategies. HOME CARE SETTING The shift in health care provisions from a hospitalbased system to the home care setting throughout Europe has been reported in the European Wound Management Association (EWMA) document entitled “Home Care Wound Care” (Probst et al. 2014) . The aim of this shift in care has been to promote community and health care delivery in the home care setting while simultaneously delivering better services, improving productivity, increasing patient safety, and improving the quality of care5. A key challenge is that there is an increasing trend for patients in the home care setting to be older with multiple co-morbidities, more disabilities, and more complex health needs6, 7. Such individuals rely not only on resources of the healthcare system but also on informal carers to help meet their needs. Informal carers may include spouses, children, neighbours, or friends. There is a large range of possible relationships. For example, a young informal carer could provide support to a parent or sibling, or younger parents could care for children. Informal carers often gain satisfaction from their caring role, as they are willing to take over the responsibility of caring for a family member at home8, 9. This underscores the need for the informal carer to receive appropriate support to be able to undertake practical health care tasks, such as the application of a wound dressing. Furthermore, the onus is on health care providers to ensure that appropriate information is available for informal carers and that they can access support for their decision-making role9. The aims of education for patients and carers are to optimize their input in the decision-making process, improve understanding, recall, and compliance, and reduce stress and anxiety. Effective education strategies for lay persons require an understanding of factors that influence them in decision making: knowledge, attitudes, skills, and understanding. These strategies should also consider literacy and language barriers and how people may access information. The latter elements of language and literacy should be a major consideration in designing information strategies, due to the multicultural societies we now live in and the low levels of literacy that are seen in some countries. Using data from Ireland as an example, the 2011 census figures showed that over half a million (514,068) Irish residents spoke a foreign language EWMA JOURNAL 2014 VOL 14 NO 2 Scientific Communication Samples of the leaflet were distributed by team members at the EWMA conference in Madrid in May 2014. PROJECT AIMS This project was established, due to (1) the important role of the informal carer in health care provisions and the promotion of health and wellbeing, (2) increases in the number of people who are receiving health care in the home care setting, and (3) challenges that are involved in increasing the awareness of pressure ulcers and their prevention. Funding was successfully obtained from EXPLORE at the National University of Ireland, Galway (NUI Galway). This scheme was intended to support initiatives in which students and staff collaborate as equal partners in projects. Therefore, this project aimed not only to promote the awareness of pressure ulcer prevention among informal carers but also to engage undergraduate nursing and podiatry students in wound care innovations and to foster a lifelong interest in the subject area. Further collaboration was gained from the Carers Association of Ireland and the Irish Practice 䊳 Nurses Association (IPNA). at home. Of these languages, Polish was by far the most common, followed by French, Lithuanian, and German10. Foreign languages are not the only consideration in the provision of information. The International Survey of Adult Literacy has shown that one in four Irish adults have literacy difficulties11. Another 30% of Irish adults were demonstrated to be at level 2, which signifies that they can only cope with very simple materials. Individuals with literacy difficulties struggle to understand discharge instructions, consent forms, handouts, and labels on prescriptions and over-the-counter medications. Many of them cannot understand important health-related letters or medical forms. Ulcers nt Pressure e v re P To Ho w Skin Care RISE Reposition • Inspect • Sk a ing for use you are car g the person dry but do When washin water and pat the skin e to ent make sur ll ntin mild soap and inco is person and dry we not rub! If the that area regularly in wash the skin in Care • Eat Well Repositon ? ssure Ulcer What iss a Pre e sore surre presssu ed a pre lled a ess ccall ime mettim some skin lcer ((so the skin ulce eu to the surre age to presssu damage A pre off dam om, rea o are otttom bot an a ip, b hip he h as tthe d sore)) iiss an or bed y area such od bon a r a good blo usually ove the skin needs The s. ssu ow pre re on heels or elb T o much To . Too lthy one hea in y g supply to sta e from sitting or lyin blood flow f r instanc fo skin, for can disrupt e, tim re g ssu lon . If pre fforr a position fo become red d; this is the skin to ome damage and cause skin can bec continues the re ulcer. r ssu called a pre What do pressure ulcers look like? RISE A pressure ulcer can look like redness of the skin that does not go away to an open sore that goes through to bone. Preventing Ulcer t a Pressure Who can ge at Those most . ffect anyone fforr aff r can affe y well, fo Pressure ulce who cannot move ver fforr long bed fo ple confined to risk are peo ple who are peo hairs. The le eelc mp wh exa y se in particularl time or tho are of s lth iod per h ill hea people wit elderly and at risk. This leaflet is intended as a guide only. If you are concerned about anything in this leaflet please discuss this with your healthcare professional. Shoulder Elbow Buttocks Shoulder Elbow Hip Ankle Heel Thigh (external) Shoulder top d at the Reposition • Inspect • Skinban Care • Eat Well the legs. To download this leaflet or for further information on pressure ulcers please visit : Sacrum Funded by: Heel Care Giver Tip Don’t forget to check places like the ears and tips of toes. These are common areas where pressure ulcers develop and are often forgotten. EWMA JOURNAL talk If concerned rning sign! red is a wa Remember ional. care profess to a health Further Information: • www.wmai.ie • www.carersassociation.ie • www.irishpracticenurses.ie Head Ischion r Tip Care Give Heel Thigh (internal) Ear v r Tip Care Give healthy p our bodies d food to kee to offer the We need goo ling. It is important nutrition. hea are high in and to help foods that uently and freq re ds mo flui person offered y dry it small meals the skin is ver Sometimes e meals. If larg enough n tha ting are easier son is not get per the sign lth may be a tact your hea con bt dou fluids. If in als. profession t elastic have a tigh not hav ulation in ks that do im ede circ n imp Choose soc as this can Toes Head a signs of or any ffo daily for wn skin at least pressu r points sho ssure Inspect the the that ticularly at ice redness otic not redness par f If you no a and overleaf. o off the are e r re u ssu in the picture ay, pre as your aw y keep io al such ssion ffess does not go profe to local health wi be able f rm your info se who will health nur lic pub or GP ir skin . eeling in the r ffee advise you have very poo u if an area is ple peo e Som tell you be able to efully. aref ca car and will not ays inspect alw so , hurting RISE Where on the body can you get Pressure Ulcers? Eat well Inspect Pressure Ulcers Reposition • Inspect • Skin Care • Eat Well Contact Details: for to move are caring person you ld involve y to help the more often. This cou Try lk rs or s a short wa nutes, every 2 hou hel f w min fe for a few ith help for bed b . Always r wit w or o r ng ir i ing d ndi nd cha sta ition in the pos as they are re ng u s ssu ss ngi pre or cha ily. heels free of d ver eas the y p ry e v kee age try to become dam sofft and can 2014 VOL 14 NO 2 Endorsed by: Information for Carers Project team Dr. Georgina Gethin, Professor Caroline McIntosh, Brid McGing, Fiona Mullins, Lauren Brennan, Sally Glynn, Orla Carey, Jacqui Hartigan, Ann Gardiner, and Moira GunningNoone. 53 Scientific Communication STEPS OF THE PROJECT Step 1: Search and appraisal To look for leaflets and information that are specifically aimed at carers for pressure ulcer prevention, we searched international wound care organizations’ websites and researched health information. We found only six examples of information leaflets. However, these were all produced for patients and not for carers. No other forms of information, such as videos or interactive education portals, were found. The six leaflets were appraised by the team for readability, clarity of expression, language use, use of illustrations to convey messages, and general appeal. Of those identified, only one from the United States was sponsored by a commercial organization and of high quality. This leaflet was twelve pages long, A5 sized, and well-illustrated with colour images. The language was also clear and easily understood. However, the final four pages of the leaflet contained commercial advertising, along with product placements. One other leaflet contained excellent information but was of low readability. It was only available in text, used a font that was too small for the ease of reading, and had no illustrations. The remaining four leaflets were of even less quality, with technical language, small font sizes, and a lack of illustrations. Having failed to find any available leaflets, the process of designing content and presentation style commenced. A key driver of the project was the readability of the final product and the ease with which it could be translated into other languages. Step 2: R.I.S.E. The acronym, R.I.S.E., was devised to promote the basic principles of pressure ulcer prevention among carers. Reposition – regular repositioning can help prevent tissue damage. Inspect – daily inspection of the skin can identify areas that are at risk of ulceration. Skin care – washing and drying the skin can prevent tissue damage. Eat well – good nutrition and hydration are essential for health and wellbeing. We were mindful that this acronym could not be translated verbatim into other languages but recognized that it could be easily adapted by others. Although other acronyms have been suggested within the literature, none were targeted at carers. In addition, we wanted to keep the message simple and direct. Therefore, fewer letters would help in recall and understanding. 54 Step 3: Design and review Over six months, the leaflet went through numerous iterations, and a final design was chosen. Consultations with graphic designers, carers, and practice nurses took place, and further support, including project management and project promotion, was gained from the Explore team. Awareness and feedback on the project was also promoted at the Stop Pressure Ulcer Day at NUI Galway in November 2013. The readability was appraised and deemed to be appropriate to the reading ability of a 10-year-old person. This was important, as some carers may have low literacy levels when reading in their non-native language. FINAL LEAFLET The final leaflet was launched at the Explore event in May 2014. In addition, samples of the leaflet were distributed by team members at the EWMA conference in Madrid in May 2014. AVAILABILITY The leaflet is freely available and has been uploaded on the websites of the Wound Management Association of Ireland (www.wmai.ie), IPNA (www.irishpracticenurses. ie), and Carers Association (www.carersireland.com). Plans are under way to have this available on other sites. As the aim was to increase awareness and promote pressure ulcer prevention, we agree that the leaflet can be downloaded by any wound care organization, health care provider, or patient support network. Furthermore, it can be translated into other languages, as long as the original source 䡵 is acknowledged. References 1. Gallagher, P., Barry, P., Hartigan, I., McCluskey, P., O’Connor, K. & O’Connor, M. Prevalence of pressure ulcers in three university teaching hospitals in Ireland. J Tissue Viabil. 2008;17(4):103-9. 2. McDermott-Scales, L., Cowman, S. & Gethin, G. Prevalence of wounds in a community care setting in Ireland. J Wound Care. 2009;18(10):405-6, 408, 410 passim. 3. Gethin, G., Jordan O-Brien, J. & Moore, Z. Estimating the costs of pressure area management based on a survey of ulcer care in one Irish hospital. J Wound Care. 2005;14(4):162-5. 4. EPUAP (2009) Guide to pressure ulcer grading. EPUAP review 3 (on-line), www.epuap.org/newsletter/epuap-reviews/vol10-issue1-2009/. 5. Vowden, K., Vowden, P. & Posnett, J. The resource costs of wound care in Bradford and Airedale primary care trust in the UK. J Wound Care. 2009; 18(3):93-4, 96-8, 100 passim. 6. Probst, S., Seppanen, S., Gethin, G., Gerber, V., Hopkins, A. & Rimdeika, R. EWMA Document Homecare WoundCare. J Wound Care. 2014;23(5):1-44. 7. Barry, U. Elderly care in Ireland-Provisions and Providers. In UCD School of Social Justice Working Papers Series (U, B. ed. University College Dublin, Dublin) 2010:10:1-34. 8. Bee, P.E., Barnes, P. & Luker, K.A. A systematic review of informal caregivers’ needs in providing home-based end-of-life care to people with cancer. J Clin Nurs, 2009;18(10):1379-93. 9. McConigley, R., Halkett, G., Lobb, E. & Nowak, A. Caring for someone with high-grade glioma: a time of rapid change for caregivers. Palliat Med. 2010;24(5):473-9. 10. CSO (2011) This is Ireland. Vol. www.cso.ie Central Statistics office, Dublin. 11. OECD (2007) International Adult Literacy Survey: Results for Ireland. Vol. www.nala.ie Department of Education and Science, Dublin. EWMA JOURNAL 2014 VOL 14 NO 2
© Copyright 2026