Topics to Review
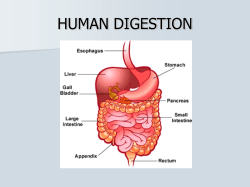
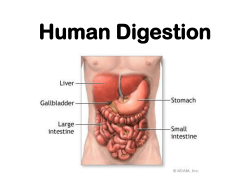
Topics to Review • Macromolecules (monomer to polymer structure) • Membrane transport proteins (carriers, pumps, channels) • Active Transport • Diffusion • Osmosis • Simple epithelium • Enzymes • Hydrolysis • Exocrine glands Digestive System • The digestive system allows your body to obtain substances required to sustain life that your body cannot make on its own including: – monosaccharides, amino acids, nucleic acids, fats, vitamins, electrolytes (ions) and water • The alimentary canal or gastrointestinal (GI) tract is a long muscular tube lined with epithelial tissue passing through the body which is closed off at each end by a sphincter of skeletal muscle • Opens to the outside world therefore the lumen and its contents are part of the external environment • Its primary function is to move water, nutrients and electrolytes from the external environment into the body’s internal environment The Digestive System • Accessory organs and exocrine glands (teeth, salivary glands, pancreas and the liver) aid in the process of digestion in the alimentary canal by physical manipulation of food or through the secretion of substances into the GI tract Anatomy of the Digestive System • Begins with the oral cavity (mouth and pharynx) where chewing and the secretion of saliva starts digestion • Food moves through the GI tract (esophagus to anus) – rings of smooth muscle act as sphincters to separate the tube into segments (esophagus → stomach → small intestine → large intestine) with different functions • Digestive secretions are added to the food by GI epithelium, liver and pancreas, turning it into a soupy mixture called chyme • The products of digestion pass out of the lumen into the ECF where they pass into blood or lymph for distribution throughout the body • Any material remaining in the lumen at the end of the GI tract is defecated through the anus Peritoneum • 2 connective tissue membranes in the abdominal cavity which protect the organs in the abdominal cavity from damage by friction/abrasion – Visceral peritoneum • covers external surface of digestive organs – Parietal peritoneum • lines the internal wall of the abdominal cavity • Between the 2 layers of the peritoneum is a peritoneal cavity which is filled with the peritoneal fluid secreted by the cells of each layer – the fluid functions to lubricate digestive organs, allowing them to slide across one another without creating friction which would lead to inflammation 4 Basic Processes of the Digestive System • Digestion – mechanical and chemical breakdown of food • Motility – movement of material along the GI tract • Secretion – release of substances (hydrolytic enzymes, mucus, acid, bicarbonate, water, ions) from salivary glands, GI epithelial cells, hepatocytes or pancreatic acinar cells into the GI tract lumen or ECF • Absorption – active or passive transfer of substances from the lumen of the GI tract to ECF • Processes are regulated by the nervous and endocrine systems as well as paracrine signals 4 Basic Processes of the Digestive System Wall of the Alimentary Canal 4 principle layers of the GI tract • Mucosa (superficial) – inner layer of epithelial, connective and muscular tissues that faces lumen • Submucosa – loose connective tissue with blood and lymph vessels and submucosal plexus of the Enteric Nervous System • Muscularis – 2 layers of smooth muscle (superficial circular and deeper longitudinal) responsible for motility which is innervated by the myenteric plexus of the Enteric Nervous System • Serosa (deep) – strong connective tissue membrane that maintains the structural integrity of the alimentary canal (visceral layer of the peritoneum) Layers of the Alimentary Canal Wall Mucosal Epithelium • Simple epithelium – absorptive cells use integral transporting proteins in the apical and basal membranes to absorb ions, water and nutrients out of the lumen into the body by facilitated diffusion, primary and secondary active transport processes – secretory cells (endocrine and exocrine) • exocytose digestive enzymes and mucus into lumen for digestion and protection against the autodigestion of the mucosa, respectively • exocytose hormones and/or paracrine molecules into the ECF for digestive regulation – sensory cells act as mechano- and chemoreceptors which detect the presence of food by the distension of the GI wall and by the presence of specific chemicals (proteins, salts, acids, fats…) Enteric Nervous System • A specialized division of the nervous system associated only with the alimentary canal • Connected to the CNS via the Parasympathetic NS (stimulates digestion) and Sympathetic NS (inhibits digestion) – Composed of two major nerve plexuses (groups) which send both sensory and motor information throughout the alimentary canal to control digestion • Submucosal nerve plexus (submucosa layer) –associated with mechano- and chemoreceptors in the mucosa –controls the endo- and exocrine secretion of the mucosa • Myenteric nerve plexus (muscularis layer) –controls the contraction of smooth muscle Chemical Digestion • Chemical digestion occurs by the action of powerful enzymes that are either secreted into the lumen or are integral proteins of the mucosal epithelium hydrolyze complex macromolecules into molecules small enough to be absorbable • Occurs in the mouth, stomach and small intestine Motility Contraction of the muscularis causes motility in 2 ways • Peristalsis is characterized by progressive waves of contraction that move from one section to the next – moves food between 2 and 25 cm/sec – occurs over long distances in esophagus to move food from the pharynx to the stomach and within the stomach where it contributes to the mixing of food – occurs over short distances in the small intestine • Segmentation is characterized by short segments of the small and large intestines alternately contracting and relaxing which mixes contents and keeps them in contact with absorptive epithelium Secretion and Absorption • Exocrine (epithelial) cells of the salivary glands, pancreas and liver as well as the GI mucosal cells secrete as much as 7 liters of enzymes, mucus, electrolytes and water into the lumen daily • Occurs in all segments from the mouth to the rectum • The 7 liters of fluid secreted daily into the lumen of the GI tract must be absorbed to prevent dehydration – excessive vomiting or diarrhea can be dangerous • In addition, an average human ingests 2 liters of food and fluid daily that also needs to be absorbed • By the time the food and secretions reach the rectum ~98.9% will be absorbed and moved into the body leaving 100 mL of fluid to be defecated • Occurs in the small and large intestines 3 Stages of Digestion • The processes of digestion, secretion, motility and absorption take place throughout the entire length of the GI tract in 3 overlapping stages named by the location of food – Cephalic (head) phase • thinking about, smelling, or seeing food which has not entered the alimentary canal • food is in the mouth – Gastric phase • food is in the stomach – Intestinal phase • food is in the small intestine Cephalic phase • This phase prepares the digestive system before the ingestion of food which significantly decreases the time required for digestion and absorption • Anticipatory stimuli as well as the presence of food in the mouth activate Parasympathetic Nervous System (PNS) controlled reflexes coordinated by the medulla oblongata • Action potentials from the medulla are sent to the stomach, small and large intestines to increase the secretion of the mucosal cells as well as stimulate the contraction of the muscularis to move the previously consumed food distally towards the rectum • In addition, action potentials are sent to the salivary glands, and the pancreas to stimulate secretion of saliva and pancreatic juice, respectively Composition and Functions of Saliva • Water • Ions • Hydrolytic enzymes – salivary amylase • begins the chemical digestion of carbohydrates – lingual lipase • begins the chemical digestion of lipids • Mucin – protein that aids in the lubrication of a bolus • ball of chewed food and saliva that is swallowed • Lysozyme – antibacterial enzyme that reduces the risk of infections Swallowing (Deglutition) • The tongue forces the bolus into the pharynx causing the epiglottis to fold over the opening to the airways (glottis) and diverts the bolus into the esophagus • The tonically contracted upper esophageal sphincter which keeps the proximal esophagus closed, relaxes and opens momentarily while breathing is inhibited • Once the bolus enters the esophagus, a strong peristaltic wave pushes the bolus to the stomach • At distal end of the esophagus, the tonically contracted lower esophageal sphincter (cardiac sphincter) momentarily relaxes and opens momentarily to allow the bolus to enter the stomach – if the cardiac sphincter does not close properly, gastric juice containing acid can enter the esophagus causing painful irritatation (heart burn) Gastric Phase • As food enters the stomach, the gastric phase of digestion begins • The cephalic phase continues until the food has been completely ingested and swallowed • The presence of food in the stomach detected by mechanoreceptors and chemoreceptors stimulates the secretion of gastric juice from the gastric mucosa into the lumen of the stomach to further hydrolyze ingested food • The presence of food in the stomach detected by mechanoreceptors and chemoreceptors also stimulates the contraction of the muscularis which mixes the food with gastric juice making a soupy mixture called chyme Gross Anatomy of the Stomach • The stomach is divided into the 3 regions: the fundus, the body and the antrum and is able to hold up to 2 liters of food and fluid when completely filled • When the stomach is empty, the mucosa folds into rugae – when filled, the expanded wall of the stomach causes these folds to disappear (flatten) The Stomach Wall • Tubular invaginations (depressions) of the surface epithelium called gastric glands extend down into the supporting connective tissue • Chief cells and parietal cells of gastric glands secrete substances into the lumen of the stomach which combine to make gastric juice Gastric Juice • Chief cells – secrete the inactive enzyme (zymogen) pepsinogen • Begins the chemical hydrolysis of proteins when pepsinogen is converted to pepsin (active) – secrete gastric lipase • continues the chemical hydrolysis of lipids • Parietal cells – secrete HCl (hydrochloric acid) to lower pH to 2.0 (optimal for chemical digestion in the stomach) • denatures swallowed proteins, kills bacteria and activates pepsin – secrete intrinsic factor which forms complexes with vitamin B12 and is essential for its absorption in the intestine • lack of intrinsic factor results in pernicious anemia which is a reduction of red blood cell synthesis due to a vitamin B12 deficiency Protection of the Stomach Mucosa • Mucous cells secrete a combination of mucus (superficial physical barrier) and bicarbonate (chemical buffer barrier under mucus) to protect the mucosa from autodigestion by HCl Hormonal Control of Gastric Function • The food that enters the stomach dilutes the HCl component of gastric juice which causes the pH to increase above 2 – in response, (G cells) of the gastric glands secrete the hormone gastrin • gastrin stimulates the parietal cells to secrete additional HCl to return the pH to 2 • During the intestinal phase (while food is slowly leaving the stomach), the intestinal hormones secretin and cholecystokinin (CCK) inhibit HCl secretion from parietal cells and inhibit the muscularis of the stomach thus limiting the rate of acidic chyme movement into the small intestine Gastric Motility • As food particles are reduced to a more uniform texture, each peristaltic wave forces a contracted pyloric sphincter open which allows only a small amount of chyme to move into the small intestine Small Intestine – 3 Segments • The 3 segments of the small intestine include: the duodenum (proximal 25 cm), the jejunum (middle 250 cm) and the ileum (distal 360 cm) • Here digestion is completed by intestinal enzymes aided by the secretions of the liver and pancreas – hepatic and pancreatic secretions (bile and pancreatic juice) enter the lumen of the small intestine at the duodenum through a duct which is guarded by the contracted sphincter of Oddi to keep these fluids from entering the small intestine except during the intestinal phase of digestion • The presence of food in the small intestine detected by mechanoreceptors stimulates a combination of segmental and peristaltic contractions which mixes the chyme with pancreatic juice and bile and moves it toward the large intestine Small Intestine Pancreas A triangular gland located behind the stomach which has both exocrine and endocrine functions • Acinar (epithelial) cells secrete pancreatic juice into a duct that empties through the sphincter of Oddi at the duodenum • Pancreatic islets (islets of Langerhans) secrete the hormones insulin and glucagon to control blood glucose levels Pancreatic Juice • Acinar cells exocytose pancreatic juice into the pancreatic duct which flows into the duodenum • Pancreatic juice contains: • pancreatic amylase hydrolyzes carbohydrates • pancreatic proteases hydrolyze proteins –secreted as zymogens • pancreatic lipase hydrolyzes lipids • pancreatic nucleases hydrolyze nucleic acids – bicarbonate (HCO3-) • a buffer secreted by duct cells that neutralizes the gastric acid, raising the pH to 8.0 (optimal for both pancreatic and intestinal enzymes) Pancreatic Zymogens • The pancreatic zymogens include: – trypsinogen – chymotrypsinogen – procarboxypeptidase • The zymogens are converted to their active form by a series of biochemical reactions initially catalyzed by the duodenal brush-border enzyme enterokinase – enzymatically hydrolyzes trypsinogen to trypsin • trypsin then activates the other 2 zymogens –chymotrypsinogen to chymotrypsin –procarboxypeptidase to carboxypeptidase Activation of Pancreatic Zymogens Liver and Gallbladder • Hepatocytes of the liver secrete bile into the hepatic ducts leading to the gallbladder • composed of bile acids and phospholipids • a detergent which causes fat emulsification –increases the surface area of fat globules • increases of lipid hydrolysis by lipase • Gallbladder – a muscular sac that stores bile secreted from the liver when the sphincter of Oddi is closed Hormonal Control of Intestinal Phase • The presence of acidic chyme in the small intestine causes the secretion of the intestinal hormone secretin – stimulates the secretion of pancreatic bicarbonate • The presence of fatty acids and peptides in the chyme in the small intestine causes the secretion of the intestinal hormone CCK – stimulates the secretion of pancreatic enzymes – stimulates the contraction of the gallbladder to squeeze the bile into the bile duct – relaxes (opens) the sphincter of Oddi, allowing the entry of pancreatic juice and bile into duodenum • Both secretin and CCK inhibit HCl secretion from parietal cells and inhibit the muscularis of the stomach thus limiting the rate of acidic chyme movement into the small intestine pH < 8 fats and proteins CCK causes relaxation distension small Intestine stimulates contraction Sphincter of Oddi bile and pancreatic juice flows into duodenum stimulates enzyme secretion Gallbladder expel bile secretin inhibits peristalsis and HCl secretion stimulates HCO3secretion Stomach slow gastric emptying stimulates muscularis Small Intestine Pancreas increase pH in chemically the small intestine digest chyme segmentation and peristalsis Small Intestinal Mucosa Structural modifications of the mucosa increase the amount of surface area for digestion and absorption • When the small intestine is empty, the mucosa is folded into structures called plicae or circular folds – when filled, the expanded wall of the small intestine causes these folds to disappear (flatten) • Intestinal mucosa also projects into the lumen in small fingerlike structures called villi • Tubular invaginations (depressions) of the surface epithelium that extend down into the supporting connective tissue of the small intestine are called crypts Sectional View of Small Intestine • Individual epithelial cells of the small intestinal mucosa have a highly folded apical cell membrane – each fold is called a microvilli and increase the number of integral membrane proteins for digestion (enzymes) and absorption (transporters) that can be exposed to the lumen – aka the brush border for its bristle-like appearance Summary of Chemical Digestion in the GI Tract • Carbohydrates – salivary amylase (minor) in the mouth – pancreatic amylase (major) in the small intestine • Proteins – pepsin (minor) in the stomach – pancreatic proteases (major) in the small intestine • Lipids – lingual lipase (minor) in the mouth – gastric lipase (minor) in the stomach – pancreatic lipase (major) in the small intestine • bile significantly increases the rate of hydrolysis • Nucleic acids – pancreatic nucleases (deoxyribonucleases and ribonucleases) in the small intestine • Brush-border enzymes of the small intestine complete the final hydrolysis of carbohydrates, proteins and nucleotides prior to their absorption Absorption of Polar Substances • Absorption begins as the molecules cross the apical cell membrane of an absorptive cell of a villus and diffuse to the basal side of the cell • Absorption is completed as the molecules cross the basal cell membrane of an absorptive cell and is moved into a blood vessel (polar molecules) or a lymph lacteal (nonpolar molecules) in the submucosa of a villus • Most polar molecules (amino acids, nucleotides, monosaccharides) cross the apical cell membrane by secondary active transport, using the Na+ gradient generated by the Na+, K+-ATPase across the cell membrane • 95% of ingested and secreted (salivary, gastric, pancreatic, hepatic, and intestinal) water is absorbed in the small intestines by osmosis – molecules of water follow the absorption of solute molecules through aquaporins Absorption of Nonpolar Substances • Following the digestion of triglycerides, the fatty acids and monoglycerides assemble with cholesterol, lipid soluble vitamins and bile into a micelle • The nonpolar micelle diffuses across the apical cell membrane of the absorptive cell into the Golgi apparatus • Once inside Golgi apparatus, the lipids are “packaged” with proteins (required for transport around the body) forming a chylomicron • The chylomicrons are packed into vesicles that are exocytosed out of the basal membrane • Chylomicrons, which are too large to enter a blood vessel, enter lymph lacteals which are large enough to accommodate the entry of chylomicrons Distribution of Absorbed Substances • The polar molecules are absorbed into the blood vessels flow directly to the liver via the hepatic portal vein – connects the blood supply of the gastrointestinal system and liver – The liver uptake (transport) some of the nutrients into the hepatocytes (liver cells) to store a portion of the absorbed nutrients, the remainder is distributed to all other cells of the body • Chylomicrons move through lymphatic vessels until these vessels merge with the heart where they enter the circulatory system to be distributed to all cells of the body Absorptive and Postabsorptive States • The absorptive state is the period of time when the alimentary canal is absorbing nutrients into the body increasing their levels (most importantly glucose) • The postabsorptive state is the period of time between absorptive states (when the alimentary canal is NOT absorbing nutrients into the body) – nutrient levels decrease during this time as they are constantly used • 2 antagonistic hormones from 2 different cell types of the pancreatic islets of Langerhans are secreted during the absorptive or the postabsorptive state in order to control the levels of circulating glucose (blood sugar) – Alpha () cells secrete glucagon – Beta () cells secrete insulin Pancreatic Islet Insulin • A peptide hormone that is synthesized first in beta cells as proinsulin (inactive) – proinsulin is then converted to active insulin in the Golgi apparatus • Secreted into circulation during the absorptive state in response to an increase in the blood glucose level • Insulin causes a decrease in the blood glucose level returning it to the set point – stimulates the uptake of glucose out of the blood into skeletal muscle cells – stimulates the uptake of glucose out of the blood into adipose cells and its subsequent conversion to glycerol which is stored in adipose as triglycerides – stimulates the enzymatic conversion of glucose into glycogen (glycogenesis) Glucagon • A peptide hormone that is secreted into circulation during the postabsorptive state in response to a decrease in the blood glucose level • Glucagon causes an increase in the blood glucose level returning it to the set point – stimulates lipolysis of triglycerides in adipose cells and the release of fatty acids into circulation – stimulates the enzymatic hydrolysis of glycogen (glycogenolysis) in the liver – stimulates gluconeogenesis in the liver • The glucose that is synthesized by the liver is transported out of the liver into the blood increasing the blood glucose level Insulin vs. Glucagon • Insulin decreases blood glucose levels – hypersecretion causes hypoglycemia • low blood sugar – hyposecretion causes hyperglycemia • high blood sugar • can lead to diabetes mellitus • Glucagon increases blood glucose levels – hypersecretion causes hyperglycemia – hyposecretion causes hypoglycemia Diabetes Mellitus • A metabolic condition caused by inability of insulin to function properly • The 5 symptoms of diabetes mellitus are: – Hyperglycemia – Glycosuria • glucose found in urine – Polyuria • large urine output – Polydipsia • large thirst –due to dehydration caused by polyuria – Polyphagia • large hunger and food consumption Diabetes Mellitus • Type I – insulin dependent diabetes mellitus (IDDM) or juvenile onset diabetes • caused by the loss of insulin synthesis by beta cells and require insulin injections to control blood sugar • Type II – non-insulin dependent diabetes mellitus (NIDDM) or adult onset diabetes • mainly caused by a defect/reduction in the insulin receptor on target cells • these individuals produce insulin, therefore insulin injections are ineffective • exhibit insulin insensitivity • The types can be differentially diagnosed in part by a glucose tolerance test Large Intestine • Any food in the small intestine that could not be chemically digested is moved into the large intestine where most of the remaining water and ions are absorbed and the remaining material removed by defecation • Subdivided into 3 anatomical segments – the colon • ascending colon • transverse colon • descending colon • sigmoid colon – rectum – anal canal Large Intestine
© Copyright 2026