Hyponatremia Approach to Core Topic UCI Internal Medicine Residency, 2012
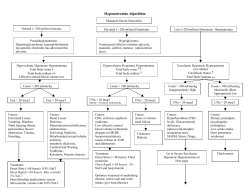
Approach to Hyponatremia Core Topic UCI Internal Medicine Residency, 2012 Clinical Scenario 74-year-old man p/w recent gastroenteritis characterized by n/v/d x 5 days, in addition to fatigue and headache. CT head (-) in ED. No focal neurologic deficits found. He looks dry on physical exam, with no evidence of fluid overload. BMP significant for Na+ of 118, baseline unknown. Serum osmolality is 266. Urine osmolality is 377. Urine sodium is 8. How would you approach this patient’s hyponatremia? How would your approach be different if this patient presented with new-onset seizures? Lecture Objectives Hyponatremia Clinical manifestations Diagnostic approach Clinical Scenario discussed Hyponatremia Defined Definition: Serum Na+ <135 meq/L Generally associated with decreased osmolality to <275 Most common electrolyte abnormality in the US Caused by retention of water Usually a drop in osmolality will suppress ADH to allow excretion of the excess water via dilute urine Most forms of hyponatremia are associated with elevated ADH (whether appropriate or inappropriate), which concentrates urine Signs & Symptoms More profound when the decrease in sodium is very large or occurs rapidly (i.e. over hours) Generally asymptomatic if Na+ level >125 Symptoms include: Headache Nausea, vomiting Muscle cramps Disorientation, depressed reflexes, lethargy, restlessness Seizure, coma, permanent brain damage, respiratory arrest, brainstem herniation & death Serious complications are more commonly seen in primary polydipsia, after surgery, and in menstruating women Approach to Hyponatremia 1st assess volume status Is the patient volume overloaded, depleted, or euvolemic? 2nd assess osmolality (hyper, iso, or hypo) Is the blood concentrated? For hypotonic hyponatremia, continue to 3rd step: 3rd assess urinary sodium excretion and FeNa % Is the urine concentrated? *Remember VOU – volume status, osmolality, and urine studies STEP 1 – (V) Volume Status 1st assess volume status (extracellular fluid volume) Hypotonic hyponatremia has 3 main etiologies: Hypovolemic – both H2O and Na decreased (H20 < Na) Consider obvious losses from diarrhea, vomiting, dehydration, malnutrition, etc Euvolemic – H20 increased and Na stable Consider siADH, thyroid disease, primary polydipsia Hypervolemic – H20 increased and Na increased (H2O > Na) Consider obvious CHF, cirrhosis, renal failure STEP 2 - (O) Osmolality 2nd assess osmolality hyper, iso, or hypo Hypotonic hyponatremia = warrants further workup, especially when there is no obvious fluid overload or depletion Serum Osmolality: lab value or calculation – in mosm/kg =(2 x Na+) + (glucose/18) + (BUN/2.8) + (ethanol)/4.6 Hypertonic - >295 hyperglycemia, mannitol, glycerol Isotonic - 280-295 pseudo-hyponatremia from elevated lipids or protein Hypotonic - <280 excess fluid intake, low solute intake, renal disease, siADH, hypothyroidism, adrenal insufficiency, CHF, cirrhosis, etc. STEP 3 – (U) Urine Studies For euvolemic hyponatremia, check urine osmolality Urine osmolality <100 - excess water intake Primary polydipsia, tap water enemas, post-TURP Urine osmolality >100 - impaired renal concentration siADH, hypothyroidism, cortisol deficiency Check urine sodium & calculate FeNa % A low urine sodium (<10) and low FeNa (<1%) implies the kidneys are appropriately reabsorbing sodium A high urine sodium (>20) and high FeNa (>1%) implies the kidneys are not functioning properly Hyponatremia Flow Sheet Hypotonic Hyponatremia Euvolemic – use patient history Hypovolemic Urine Na >20 Urine Na <10 FeNa >1% FeNa <1% Renal losses, mineralocorticoid deficiency, Addison’s disease Extrarenal losses (diarrhea, emesis, burns) Uosm >100 SiADH (urine osm usually much higher) Hypothyroidism Cortisol deficiency Hypervolemic Uosm <100 Uosm variable Primary polydipsia or low solute intake Reset osmostat (ie malnutrition, pregnancy) Urine Na <10 Urine Na >20 FeNa <1% FeNa >1% CHF Cirrhosis Nephrosis Renal failure Treatment of Hyponatremia Be CAUTIOUS with correction: 0.5 meq/L increase per every hour initially Do not increase Na more than 10 meq/L in 24 hrs or 18 meq/L in 48 hrs Treatment varies greatly by etiology of hyponatremia, and it is important to look-up via online or other resources. Clinical Scenario - Conclusion 74-year-old man p/w recent gastroenteritis characterized by n/v/d x 5 days, in addition to fatigue and headache. BMP significant for Na+ of 118, baseline unknown. Serum osmolality is 266. Urine osmolality is 377. How would you approach this patient’s hyponatremia? The steps: 1) Serum osmolality – 266, decreased (hypotonic) 2) Urine osmolality –377, increased (>100) 3) Volume status - hypovolemic 4) Urine Na, FeNa – urine Na 8, appropriately reabsorbing, likely volume depleted 2/2 N/V 5) Treatment: Mild symptoms, correct slowly w/ isotonic saline How would your approach be different if this patient presented with new-onset seizures? For symptomatic, severe hyponatremia, more rapid correction using 3% normal saline TAKE HOME POINTS Symptoms: Usually Na <125 or rapid decline N/V, headache, lethargy, AMS, seizures, coma WORK-UP in 3 important steps (V-O-U): 1) Assess volume status 2) Assess serum osmolality 3) Check urine sodium, osmolarity, & calculate FeNa Treatment varies by etiology, but cautious correction of sodium important to prevent demyelination as fluid leaves the brain
© Copyright 2026