Are Emergency Physicians Too Aggressive With Empirically Treating Gonorrhea and
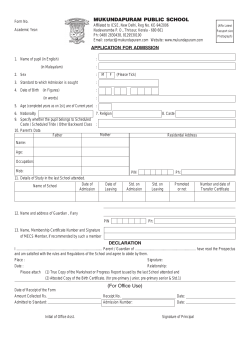
Are Emergency Physicians Too Aggressive With Empirically Treating Gonorrhea and Chlamydia In The Face of Rising Resistance? FOEM Oral Abstract Competition ACOEP 2014 Fall Conference Xandus Chen, DO Co-Authors Xandus Chen, DO Christopher Komurek, DO Michael Samodio, DO Kelly King, DO Scott Plasner, DO Aria Health, Philadelphia Background Neisseria Gonorrhea (NG) and Chlamydia Trachomatis (CT) are the highest reported sexually transmitted diseases (STD) in this country and across the globe Philadelphia is ranked #4 as of 2011 CDC recommends a low threshold to treat higher risk patients Background Significant part of the patient population seen at ARIA-Frankford ED are higher risk patients EM physicians commonly empirically treat patients with STD complaints for NG/CT before the PCR result are available Results take 2-3 days Concern that NG/CT will develop resistance Background NG resistant to prior 1st line agents PCN and fluoroquinolones Increased antibiotic dosing Dual therapy recommended Evidence that CT has capability to express resistant phenotypes Objective/Hypothesis Objective: Establish the percentage of patients with actual infection from those who were empirically treated for NG/CT Hypothesis: Despite working with a higher risk population in our ED, overtreatment of patients without NG/CT infections occur at a higher rate than expected Methods Design: Retrospective study Setting: ARIA –Frankford ED is an urban community ED in Philadelphia Patient Selection: 100 patients randomly selected Medically evaluated at ARIA-Frankford ED Received empiric treatment for NG/CT Had endocervical or urethral sample collected for NG/CT PCR testing Main Outcome Measures Percentage of infected patients among those who received empiric treatment Frequency of STD-concerning symptoms and history Dysuria Discharge Partner concerns Prior STD testing Prior STD history Results 21/100 patients had positive NG/CT cultures 11 patients had NG, 6 patients had CT, 4 had both When comparing patients infected with NG/CT to all patients, higher percentage complained of STDconcerning symptoms and history Dysuria (52% vs 28%) Genital discharge (81% vs 60%) Partner concerns (24% vs 16%) Prior testing (52% vs 33%) Prior STD history (43% vs 16%) Comparison of Empirically Treated Patients A11 Treated Males Infected Treated 21% Females Infected Treated 39% Infected 7% Dysuria 28% 52% 39% 53% 11% 50% Discharge 60% 81% 61% 82% 33% 75% Partner 16% 24% 25% 29% 5% 0% Prior Testing 33% 52% 32% 59% 19% 25% Prior STD 16% 43% 23% 53% 6% 0% Concerns Results 17/44 male (39%) were infected When comparing male patients infected with NG/CT to all male patients, higher percentage complained of: Dysuria (53% vs 39%), Penile discharge (82% vs 61%) Partner concerns (29% vs 25%) Prior STD testing (59% vs 32%) Prior STD history (53% vs 23%) Comparison of Empirically Treated Patients A11 Treated Males Infected Treated 21% Females Infected Treated 39% Infected 7% Dysuria 28% 52% 39% 53% 11% 50% Discharge 60% 81% 61% 82% 33% 75% Partner 16% 24% 25% 29% 5% 0% Prior Testing 33% 52% 32% 59% 19% 25% Prior STD 16% 43% 23% 53% 6% 0% Concerns Results 4/56 females (7%) were infected When comparing infected females to all females, higher percentage complained of: Dysuria (50% vs 11%) Discharge (75% vs 33%) Prior STD testing (25% vs 19%) Lower percentage of infected females complained of: Partner concerns (0% vs 5%) Prior STD history (0% vs 6%) Comparison of Empirically Treated Patients A11 Treated Males Infected Treated 21% Females Infected Treated 39% Infected 7% Dysuria 28% 52% 39% 53% 11% 50% Discharge 60% 81% 61% 82% 33% 75% Partner 16% 24% 25% 29% 5% 0% Prior Testing 33% 52% 32% 59% 19% 25% Prior STD 16% 43% 23% 53% 6% 0% Concerns Discussion 79% of patients did not have NG/CT NG was 50% more prevalent than CT infections Males had higher incidence of infection (39%) Females had lower incidence of infection (7%) Discussion Patients who were positive for NG/CT more commonly complained of STD-concerning symptoms and history Complaints were nonspecific Discharge was the most common complaint of infected patients (82%) 48% of males WITHOUT infection also complained of discharge 5 patients were positive for CT/NG several times within 3-5 month span Discussion Disadvantage of overtreatment Increasing resistance Higher cost of medical care Longer time spent in ED Risk of allergic reaction Increased risk of C. Difficile infection Anxiety and social stigma of STD infection Discussion Disadvantage of postponing treatment until positive PCR results Patients lost to follow up Continued transmission disease Consequences of no treatment: PID Epididymitis Infertility (men and women) Vertical transmission Disseminated gonorrhea Limitations Sample size Physician variable collection techniques Numbers of patients with specific complaints were dependant on Patients providing information Medical documentation Prior ARIA hospital visits Conclusion Significant overtreatment in ED for NG/CT (79%) Low threshold to treat males Collect cultures for repeat infections STD-concerning symptoms and history are nonspecific Still recommend judicious empiric treatment for NG/CT References 1. CDC. (2014, January). CDC Fact Sheet: Reported STDs in the United States. Retrieved from http://www.cdc.gov/std/ 2. Feyler, Nan (June 18, 2012). Philadelphia Department of Public Health, Health Notification, Gonorrhea Treatment Verification. Retrieved from https://hip.phila.gov/xv/Portals/0/HIP/Health_Alerts/2012/PDPH HAN_Notification_2_GonorrheaTreatmentVerification_061812.pdf 3. CDC. (February 15, 2013). CDC Grand Rounds: The Growing Threat of Multidrug-Resistant Gonorrhea. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6206a3.htm 4. Ohnishi, M., Golparian, D., Shimuta, K., Saika, T., Hoshina, S., Iwasaku, K., Nakayama. S., Kitawaki, J. (2011). Is Neisseria Gonorrhoeae Initiating a Future Era of Untreatable Gonorrhea?: Detailed Characterization of the First Strain with High-Level Resistance to Ceftriaxone. Antimicrobial Agents and Chemotherapy, 55(7), 3538-45. 5. Sandoz, K. M., Rockey, D. D., (2010). Antibiotic Resistance in Chlamydiae. Future Microbiology. 5(9), 1427–1442. References 6. Somani, J., Bhullar, V. B., Workowski, K. A., Farshy, C. E., Black, C. M. (2000). Multiple Drug–Resistant Chlamydia trachomatis Associated with Clinical Treatment Failure. 7. The Journal of Infectious Diseases, 181(4), 1421–7. 8. Tyndall, M. W., Kidula, N., Sande, J., Ombette, J., Temmerman, M. (1999). Predicting Neisseria gonorrhoeae and Chlamydia trachomatis infection using risk scores, physical examination, microscopy, and leukocyte esterase urine dipsticks among asymptomatic women attending a family planning clinic in Kenya. Sex Transm Dis. 26(8), 47682. 9. Pettifor, A., Walsh, J., Wilkins, V., Raghunathan, P. (2000). How Effective Is Syndromic Management of STDs? A Review of Current Studies. Sexually Transmitted Diseases, 27(7), 371–385. 10. Andric, B., Drowos, J., Trepka, M. J., Suciu, G., Alonso, A., Hennekens, C. H. (2013). High Frequencies of Negative Pretreatment Results Following Presumptive Antibiotic Treatment for Chlamydia and Gonorrhea. Southern Medical Journal. 106(5), 321-326. 11. Ng, L. K., Martin, I. E., (2005). The Laboratory Diagnosis of Neisseria Gonorrhoeae. Can J Infect Dis Med Microbiol. 16(1), 15–25. Thank you Questions?
© Copyright 2026