Acid Base Balancex
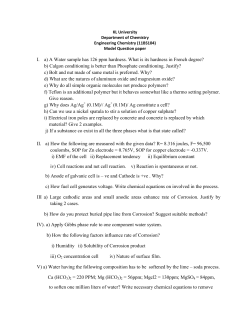
000022.jpg Regulation of acid-base balance: Objectives: Defense WHY?!! against the change in pH. Because H+ react highly with cellular proteins resulting in alteration in their function therefore avoiding acidemia and alkalemia by tightly regulation H+ which is essential for normal cellular function. Why we do Arterial Blood Gas Analysis? Oxygenation Represented by PaO2 Ventilation Represented by Pa Co2 Acid Base Status Represented by pH, HCO3 and base deficit. What information does ABG provide about the patient? FIRST: ABG provide an assessment of the following: 1)PaO2: Amount of o dissolved in the blood, it give initial information on efficiency of oxygenation. 2)PaCO2: Adequacy of ventilation is inversely proportional to Paco2 (when ventilation increase PaCO2 decrease and vice verse). 3) Acid base status (pH, HCO3, base deficit, anion gap). 4) Hb, Hct, oxygen saturation. 5) Electrolyte e.g. Na+, K+. SECOND: Calculation of Alveolar Gas Equation and A-a Gradient: PAO2 = FiO2×(Bp-pH2O)-PaCO2/R. = 21×(760-47)-40/0.8 = 100 mmHg. A-a Gradient is alvealo-arterial O2 gradient. A-a Gradient = PAO2 -PaO2 It is normally = Age/4+4. It’s Value: concise D.D of hypoxemia. e.g.: Decrease FiO2 Hypoventilation normal A-a Gradient Ventilation perfusion mismatch Rt to Lt shunting Diffusion abnormality increase A-a Gradient 1) Arterial/alveolar ratio(a/A) PaO2/PAO2 PAO2 is calculated by the alveolar air equation: PAO2 = FIO2 (PB – PH2O) – PaCO2/0.8 Normal value for the a/A ratio is 0.8, meaning that 80% of the alveolar oxygen is reaching the arterial system 2) PaO2/ FIO2 ratio Normal ratio is 550 (a person breathing FIO2 of 1.0 at sea level should have a PaO2 of 550 to 600 mmHg) 3) A-a gradient (on 100% oxygen) PAO2 - PaO2 Where PAO2 is calculated by the alveolar air equation previously presented Arterial/alveolar PCO2 Gradient (a-A PCO2) Arterial PCO2 - Alveolar PCO2 Where Alveolar PCO2 is measured by means of end–tidal PCO2 Normal gradient is an alveolar PCO2 2 mmHg less than arterial, Acute increase reflects increase in physiologic dead space Diagnosis of acid Base disorders Sample source and collection:•Arterial blood sample is common utilized clinically but venous blood may be useful in determining acid base status. (Except in CHF and shock). •Blood sample should be in heparin coated syringe. •The sample should be analyzed as soon as possible. •Air bubble should be eliminated. •The syringe should be capped and placed in ice. Problem associated with obtaining ABG: Arterial puncture may result in acute hyperventilation. To minimize that: we should use local anesthetic with small needle. When would you withdraw ABG sample after beginning or stopping O2 supplementation? In absence of significant lung disease we should wait from 5-7 minutes before withdraw ABG sample while patient with obstructive lung disease we should wait 25 min. Interpretation of ABG Normal blood gas values: Arterial blood Mixed venous Venous PH 7.37-7.47 7.30-7.40 7.30-7.40 PO2 80-100 35-40 30-50 PCO2 36-44 40-50 40-50 O2 saturation >95% 60%-80% 60%-85% HCO3 22-26 22-26 22-28 Base difference (deficit excess) -2 to 2 Measurement What is PH? PH is –ve log of H+ concentration. P=protenz (strength-power), H=H+ concentration. Henderson-Hasselbalch Equation Relationship between pH & [H+] pH = pK’a + log ([HCO3] / 0.03 x pCO2) pH [H+] (nanomoles/l) 6.8 6.9 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 7.8 158 125 100 79 63 50 40 31 25 20 15 or more simply: The Henderson equation: [H+] = 24 x ( pCO2 / [HCO3] ) What is base deficit? The base deficit is the amount of acid or base needed to titrate a serum PH back to normal (7.40) at 37 degree while the Paco2 is held constant at 40 mmHg, thus eliminating the respiratory component therefore the base deficit represent only the metabolic component of acid base disorders. Its +ve value indicate metabolic alkalosis, While –ve value indicate metabolic acidosis. ABG analyzer derives the base deficit from nomogram based on: 1) pH 2) HCO3 3) Hb concentration STEPS for interpretation of ABG STEP 1: Determine if numbers fit: H+ = 24 PCO2 HCO3 H+ = (7.8-PH)×100. The Rt side of the equation should be within 10% of the Lt Side. If not so another ABG or chemistry panel for HCO3 should be done. STEP 2: STEP 3: Determine if: Acidemia (PH<7.37) OR Alkalemia(PH >7.44) is present. Identify primary disturbance: PH Increase Decrease Alkalosis Acidosis Look at PCO2 Increased Metabolic Alkalosis Decrease Increased Respiratory Alkalosis Respiratory acidosis Decreased Metabolic acidosis STEP 4: Look at the direction of the change of HCO3/PCO2: •If it is in the same direction it is either simple or mixed change. •But if it is in the opposite direction so it is mixed change. STEP 5: Calculate rate of change of Hco3 and co2 (Expected compensation) Disturbance Response Expected change Metabolic acidosis ↓Paco2 1.2×(24-HCO3 measured) Metabolic alkalosis ↑Paco2 0.7×(HCO3-24) Acute respiratory acidosis ↑Hco3 0.1×(PaCO2-40) Chronic respiratory acidosis ↑ Hco3 0.4×(PaCO2-40) Acute respiratory alkalosis ↓ Hco3 0.2×(40-PaCO2) Chronic respiratory alkalosis ↓ Hco3 0.4×(40-PaCO2) N.B.: There is no over correction or compensation in acid base balance → if the compensatory response is more or less than expected → it is mixed acid base disorder N.B.: • In respiratory disturbance arterial pH change 0.08 for every 10 mmHg change in PCO2. • In metabolic disturbance arterial pH change 0.1 for every 6 meq /l change in HCO3. Determine the Anion Gap The Anion Gap [(Na+) + (K+)] – [(Cl-) + (HCO3-)] The normal anion gap is 12meq ± 4. Causes ofHyperchloremic Acidosis ↑ GIT loss of HCO3 as in: diarrhea, high output fistula (pancreatic, biliary or small intestinal). ↑ renal HCO3 loss as in: RTA(I, II), CAIs, hypoaldosteronism. TPN. Large amount of HCO3 free fluid. ↑ CL containing acids. Wide Anion Gap Acidosis Keto Acidosis Uremia Lactic Acidosis Salicylism Toxins : Methanol,Paraldehyde,Ethylene glycol All anions and cations ANIONS CATIONS Proteins 15 Calcium 5 Organic acids 5 Magnesium 1.5 Phosphates 2 Potassium 4.5 Bicarbonate 24 Sodium 140 Sulfates 1 Chloride 104 TOTAL 151 TOTAL 151 Non anion gap metabolic acidosis: Metabolic acidosis associated with normal AG is typically characterized by hyperchloremia. Plasma CL- ↑ to take the place of HCO3 ions lost. Calculation of AG in urine: Urine AG = ( Na+ + K+) – CLIn a patient with a hyperchloraemic metabolic acidosis: •A negative UAG suggests GIT loss of bicarbonate (eg diarrhoea) •A positive UAG suggests impaired renal distal acidification (ie renal tubular acidosis). STEP 6: If there is metabolic acidosis calculate the anion gap Anion Gap = Na+ - (Cl- + HCO3-) = 12meq ± 4. • Corrected anion gap = observed anion gap + 2.5 (normal albumin - measured albumin). • If the anion gap ↑ proceed to step 7. STEP 7: If the anion gap metabolic acidosis is present we should evaluate for additional metabolic disorder because the elevation of anion gap above normal ∆ AG = (AG-12) should be buffered by HCO3. Adding ∆AG to current HCO3 will yield the corrected Hco3 which should be normal value 24 meq/l unless there is another disorder present. Corrected HCO3 = current HCO3 (measured) +∆A.G (Normal value 24 meq/l) •If corrected HCO3 >24 → metabolic alkalosis is also present •If corrected HCO3 <24 → a non gap metabolic acidosis is also present •If corrected HCO3 = 24 → it is pure gap metabolic acidosis. Delta ratio = (Increase in anion gap / Decrease in bicarbonate) Delta Ratio Assessment Guideline < 0.4 Hyperchloraemic normal anion gap acidosis 0.4 - 0.8 Consider combined high AG & normal AG acidosis BUT note that the ratio is often <1 in acidosis associated with renal failure 1 to 2 Usual for uncomplicated high-AG acidosis Lactic acidosis: average value 1.6 DKA more likely to have a ratio closer to 1 due to urine ketone loss (esp if patient not dehydrated) >2 Suggests a pre-existing elevated HCO3 level: consider a concurrent metabolic alkalosis or a pre-existing compensated respiratory acidosis. STEP 8: In case of metabolic alkalosis: measure urinary Cl- concentration Final step: Be sure that the interpretation of blood gas is consistent and correlated with the clinical picture of the patient. Case 1 A 75-year-old man presents to the ED after a witnessed out of hospital VF cardiac arrest. Arrived after 10 minutes, CPR had not been attempted. The paramedics had successfully restored spontaneous circulation after 6 shocks. On arrival the man is comatose with a GCS of 3 and his lungs are being ventilated with 50% oxygen via ET tube. He has a ST with rate of 120 min-1 and a blood pressure of 150/95 mmHg. ABG Analysis reveals: FiO2 pH PaCO2 PaO2 HCO3 BE 0.5 7.10 6.0 kPa (45 mmHg) 7.5 kPa(56 mmHg) 14 mmol l-1 - 10 mmol l-1 Case 2 A 65-year-old man with severe COPD has just collapsed in the respiratory high-care unit. On initial assessment he is found to be apnoeic but has an easily palpable carotid pulse at 90 min-1. A nurse is ventilating his lungs with a BVM and supplementary O2 (with reservoir) ABG Analysis reveals: FiO2 pH PaCO2 PaO2 HCO3 BE 0.85 (estimated) 7.20 20.0 kPa (151 mmHg) 19.5 kPa (147 mmHg) 36 mmol l-1 + 12 mmol l-1 Case 3 A 75-year-old lady is admitted to the ED following a VF cardiac arrest, which was witnessed by the paramedics. A spontaneous circulation was restored after 4 shocks, but the patient remained comatose and apnoeic. The paramedics intubated her trachea, and on arrival in hospital her lungs are being ventilated with an automatic ventilator using a tidal volume of 900 ml and a rate of 18 breaths min-1. ABG Analysis reveals: FiO2 pH PaCO2 PaO2 HCO3- BE 1.0 7.60 2.65 kPa (20 mmHg) 25.4 kPa (192 mmHg) 20 mmol l-1 - 4 mmol l-1 Case 4 An 18-year-old male insulin dependent diabetic is admitted to the ED. He has been vomiting for 48 hours and because he was unable to eat, he omitted his insulin. He has a ST at a rate of 130 min-1 and his blood pressure is 90/65 mmHg. He is breathing spontaneously with deep breaths at a rate of 35 min-1 and is receiving oxygen 4 l min-1 via a Hudson mask. His GCS is 12 (E3, M5, V4). ABG Analysis reveals: FiO2 pH PaCO2 PaO2 HCO3- BE 0.4 6.79 1.48 kPa (11.3 mmHg) 17.0 kPa (129.2 mmHg) 4.7 mmol l-1 - 29.2 mmol l-1 Case 5 His vital signs are: Heart rate 120 min-1 – sinus tachycardia – warm peripheries Blood pressure 70/40 mmHg Respiratory rate 35 breaths min-1 SpO2 on oxygen 92% Urine output 50 ml in the last 6 hours GCS 13 (E3, M6, V4) ABG Analysis reveals: FiO2 pH PaCO2 PaO2 HCO3- BE 0.4 (approx) 7.12 4.75 kPa (36 mmHg) 8.2 kPa (62 mmHg) 12 mmol l-1 - 15 mmol l-1 Case 6 Which patient is more hypoxemic, and why? Patient A: pH 7.48, PaCO2 34 mm Hg, PaO2 85 mm Hg, SaO2 95%, Hemoglobin 7 gm% Patient B: pH 7.32, PaCO2 74 mm Hg, PaO2 55 mm Hg, SaO2 85%, Hemoglobin 15 gm% Patient A: Arterial oxygen content = .95 x 7 x 1.34 = 8.9 ml O2/dl Patient B: Arterial oxygen content = .85 x 15 x 1.34 = 17.1 ml O2/dl Patient A, with the higher PaO2 but the lower hemoglobin content, is more hypoxemic. Case 7 The PO2 in a cup of water open to the atmosphere is always higher than the arterial PO2 in a healthy person (breathing room air) who is holding the cup. True or False Case 8 A patient is admitted to the ICU with the following lab values: BLOOD GASES pH: 7.40 PCO2: 38 HCO3: 24 PO2: 72 ELECTROLYTES, BUN & CREATININE Na: 149 K: 3.8 Cl: 100 CO2: 24 BUN: 110 Creatinine: 8.7 What is(are) the acid-base disorder(s)? Step 1: Anion gap AG = Na+ - (Cl- + CO2)= 149 - (100 + 24) = 25 This high an AG indicates an anion gap metabolic acidosis Step 2: Delta anion gap calculated AG 25 mEq/L normal AG = 12 mEq/L 25 - 12 = 13 mEq/L; this is the excess or delta anion gap Step 3: Delta serum CO2 = normal CO2 - measured CO2 =27 (average normal venous CO2) - 24 = 3 mEq/L Step 4: Bicarbonate Gap = delta AG - delta CO2 = 13 - 3 = 10 mEq/L The patient was both uremic (causing metabolic acidosis) and had been vomiting (metabolic alkalosis). Case 9 In the clinical setting, which of the following statements concerning blood gas physiology is(are) true? a) End-tidal PCO2 should always be higher than arterial PCO2. b) In a steady state situation, alveolar PO2 should always be higher than arterial PO2. c) The %oxyhemoglobin + %carboxyhemoglobin + %methemoglobin should never exceed 100%. d) The ratio of dead space to tidal volume should never exceed 1.0. e) The average airway pressure does not exceed barometric pressure in a spontaneously-breathing patient. a) is false; End-tidal PCO2 should always be equal or lower than PaCO2. b) is true. c) is true. d) is true. e) is true; the average airway pressure is always equal to barometric pressure in a spontaneously-breathing patient. Case 10 55 yrs old pt. who drink fifth of wesky per day has 2 wks history of diarrhea , Anion gap is 17, HCO3 = 10, PH = 7.30, PO2 =0.90 mmHg, PCO2 = 30 mmHg. What is(are) the acid-base disorder(s)? Case 11 25 yrs pt. come to ER with fever, abd. pain , vomiting, with the history of migrane PH = 7.33, PCO2 = 10mmHg, PO2 = 80 mmHg, HCO3 = 5, Sodium = 140 mmol, K = 3 mmol, CL = 108 mmol. What is(are) the acid-base disorder(s)? Any Question? Thank You
© Copyright 2026