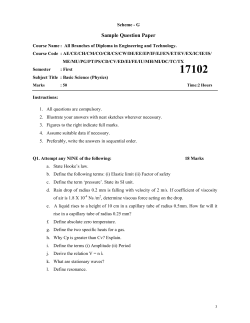
CTOP Retreat 2014 Esophageal Cancer Pathway May 23, 2014
CTOP Retreat 2014 Esophageal Cancer Pathway May 23, 2014 Introduction •Esophageal cancer is the 7th leading cause of cancer death. •Incidence of esophageal cancer has increased faster than any other solid tumor. •Despite advances in diagnosis, staging and treatment, the overall 5-year survival ranges from 15-30%. •Surgery for esophageal cancer has a routine complication rate of 50-75%. In these discouraging numbers lies an opportunity to have a meaningful and measurable impact on patient care. Mission: To provide a Dartmouth standard of care that surpasses current national standards Vision: Through the development of evidence-based clinical care pathways, we create a program to provide the highest quality of care for esophageal cancer patients Aims: 1. To assess current needs of patients and resources 2. To build a team of providers invested in a shared clinical pathway 3. To map the flow of patients through treatment of esophageal cancer 4. To optimize efficiency and evidence-based medicine 5. To track process and outcomes Aim 1: To assess current needs of patients and resources 1. List every contact with a DHMC service a patient with esophageal cancer may have 2. List all necessary studies (pathology, radiology, endoscopy) a patient may need, and the optimal order of events 3. Mailed questionnaire to patients. • “What did we do well?” • “Where could we improve?” 4. Reunion of past patients Aim 2: To build a team of providers invested in a shared clinical pathway 1. Secretarial lead 2. Nurse navigator 3. Physician lead 4. Surgery-anesthesia 5. Quality-Electronic Medical Record Aim 3: To map the flow of patients through treatment of esophageal cancer Palliative GI consult (stent/ablation) as needed Mandatory Palliative Care consult Mandatory medical oncology consult Stage IV Palliative thoracic surgery (J tube/G tube), as needed Initial Evaluation Specialty referral GI, Oncology Scheduler books coordinated appointment - Special Instructions: Tuesday pm dedicated new patient consultation, - 2 appts reserved Keep Tuesday pm appointments clear for esophageal patients until Friday NCCC- Thoracic Oncology PCP referral Thoracic surgery Radiation Oncology Connect to Thoracic Onc,Scheduler, NCCC 650-6344 If scheduler has clinical questions on who pt should see, refer to Nurse Navigator Alternate to NCCC: Thoracic Scheduler Alternate to Nurse Nav.: Physician Assistant GI Other Scheduler collects the following before initial appointment: □Physician notes □Endoscopy report □Pathology report □Pathology slides □EUS report □Imaging: CT/PET All stages On same day as surgical consult, joint appointment with: Consult with Dr. Erkmen to: Nurse Navigator contact prior to visit, with phone note asking about smoking status, weight loss, and transportation needs □Discuss stage and treatment plan □Receive patient education binder □Fill out questionnaire □Receive patient binder Staging information entered into eDH by Ellen Parker at Tumor Board Presentation at multidisciplinary tumor board Multidisciplinary staging designation Stage II/III Patient referred to DH Med Onc (dedicated Tuesday afternoon appt with Dr. Dragnev) Appointment for surgery booked Pre-operative Palliative Care consult Restaging Appointment Surveillance with Med Onc □Cardiac assessment, Patient would benefit from Shared Decision consult Stage I Proceed with surgery No Yes □Bloodwork □Chest xray □Abx □Heparin Yes Need for feeding tube Yes □Extra mayo stand for laparoscopy □Waterproof gown □Extra ioban for sleeves Review plan morning of surgery with Pain Service □Dietician □ Patient fills out □Signed consent □DPOA submitted □Advanced directives and care planning submitted □VNA selected □Rehab selected 3 weeks after last treatment, pelvic, abd, chest CT Restaging Appointment Check in appointment with Dr. Erkmen 3 weeks after completion of last treatment Screening for Shared Decision Making, screening questions entered into Nurse Navigator note Good sx candidate? On same day as surgical consult, joint appointment with: □MSW □Nurse navigator □Smoking cessation □Dietician Chemo/Radiation recovery period lasting 6-8 weeks Metastatic disease accommodate liver retractor and eschelon In-room time documented Pneumoboots placed Two bovie pads placed Foley with temp probe Left lateral decubitus Pillow between legs Time out to include glucagon, communication with ICU Prep and drape Chest surgery start time documented Chest surgery stop time documented 3 to put through 12mm port □28f chest tube □3-0 vicryl to close ports □Carter port closing device □Glucagon 2mg to anesthesia □Linear 75 green load stapler □Jejunostomy tube prepared and □Camera port anteriorly □Harmonic port □Azygous port □Counter traction port □Anterior traction of lunch □Harmonic and thoracoscopic flushed in alcohol, then flushed with sterile saline solution Call ICU fellow to secure bed Bronch □Epidural □Double lumen (left sided, check placement) □A-line and Central line □Subcutaneous heparin □Preop antibiotics: 1.5g cefuroxine and 500mg Placement of 18F NGT debakey pleura No Evidence of residual disease PET, EUS No Follow-up with Med Onc No □Liberal clipping of lymphatic and vascular attachments Yes Palliative Care consult □Turn start time documented □Turn to supine □Reposition to bottom of bed □Place legs in stirrups □Left arm tucked, right arm out □Roll under neck for extension □Replace EKG pads prep □End turn time documented □Resection of level 4,7,8,9 lymph nodes for permanent □Dissect thoracic duct between aorta, azygous and esophagus □Clip off thoracic duct □28F straight chest tube placed □Lung reinflated under thoracoscopic □45 vascular stapler around azygous view □Penrose to encircle esophagus □Ports closed 2-0 vicryl x2 and 4-0 □Dissection above azygous keeping monocryl pleura intact □Chest tube placed to suction □Cut and leave Penrose at proximal □Bovie, suction, camera, harmonic esophagus marked cords and saved □Dissection to hiatus □Dermaflex Follow-up with Med Onc □Document neck start time □Left neck incision along □Drape □Start abdomen surgery □Posterior dissection □Ensure suction to check posteriorly to vertebral body tube and pneumoboots on □Staple drape to blue towels □Cut hole for neck □Secure bovine x2 □Secure suction, camera, insufflation, □Take hepato-gastric ligament □Take left gastric artery with 45 vascular stapler □Dissect lesser curvature to pylorus keeping vasculature intact harmonic □Midline laparotomy □Place Alexis hand port □Insufflate through hand port □Place 12mm left lateral port for camera and switch □Place 12mm left lateral port for harmonic □Place 12mm right liver port □Find gastroepiploic □Take short gastric arteries to hiatus with harmonic □Take omentum distal to gastroepiploic, palpating pulse □Extend dissection to pylorus, gastroduodenal posterior to pylorus Send esophagus to pathology with proximal margin looking for malignancy and Barrett’s sternocleidomastoid documented □Feel for NGT □Pull NGT back to intra thoracic esophagus □Identify crow’s foot □Mark esophagus with purple pen □Dissection to pull Penrose up □Dissect vascular bundle off lesser curve □Push esophagus □Remove liver retractor 45- □Divide esophagus with linear 75 green loads □Kocher maneuver □Test pylorus to hiatus □Circumferentially dissect esophagus to vascular staple across lesser curve vascular bundle hiatus stomach to shape conduit □Encircle esophagus at hiatus □Enlarge hiatus □Suture chest tube to proximal □Double check NGT □Eschelon-60 green loads across from abdomen, pull from neck □Take lymph nodes and esophagus with alis □Place jejunostomy tube □Witzel jejunostomy tube and tack distally □Test jejunostomy tube from specimen stomach stump with 0-silk sutures □Give glucagon □Pull NGT back to prevent it Switch to single lumen tube with anesthesia attending Right lung deflated □Hold gastric conduit Intra-operative legs Thoracic Surgery (Dr. Erkmen) □Axesis wound protector □Three 12mm ports, bladed which □Fan liver retractor □Eschelon stapler □Extra purple marker for marking □0-silk suture on SH cut to 15cm x cessation Pre-op Preparedness : Anesthesia Consult : □Pain Management □Pre-op assessment □Intra-operative □ICU care questionnaire Scheduler calls patient to check in 10 weeks after initial evaluation appointment No □Bertchold bed □CO2 filled □Pick list □Bean bag match □Harmonic □Penrose □45 Vascular stapler □Endoscopic clip applier □Two bovie pads and bovies □Stapler for draping supine □Two extra half sheets for stirrup □MSW □Nurse navigator □Smoking including EKG, option for echo Yes Preop Checklist On same day as surgical consult, joint appointment with: Appointment with Thoracic Surgery (Dr. Erkmen) Pre-operative Shared Decision Making consult Yes Chemo and Radiation lasting 8-12 weeks Patient referred to DH Rad Onc (dedicated Tuesday afternoon appt with Dr. Zaki) with dietary by Thoracic/NCCC scheduler Opt out Intra-operative Patient seen at DHMC for chemotherapy/ radiation therapy Stage I Stage II/III Pt to receive concurrent chemotherapy and radiation therapy at DH or local hospital No □MSW □Nurse navigator □Smoking cessation □Direct scheduling from being stapled during division of the esophagus flagyl, clinda for alternative Post Op Day 3 Neruo: epidural, PCA CV: telemetry, watch for afib Respiratory: chest PT and deep breathing, chest tube to water seal if no leak Neck JP ensure holding bulb suction GI: NPO/NGT to low wall suction, flush every 30 cc to ensure patency J tube to gravity, flush with 30 cc every 8 hours, GI prophylaxis GU: Keep ins and outs even, pt should start to self-diurese, heplock IV, balance electrolytes based on labs Heme: sq heparin bid, CBC ID: no antibiotics Tubes/Lines/Drains: obtain PICC line, d/c triple lumen catheter, d/c aline, Neck JP, chest tube, NGT, J tube Activity: ambulating, PT consult Disposition: transfer to floor Post Op Day 2 Neruo: epidural, PCA CV: telemetry, keep SBP > 100, avoid pure alpha agents for pressors Respiratory: chest PT and deep breathing, chest tube to water seal if no leak Neck JP ensure holding bulb suction GI: NPO/NGT to low wall suction, flush every 30 cc to ensure patency J tube to gravity, flush with 30 cc every 8 hours, GI prophylaxis obtain albumin/prealbumin, start TPN for prealbumin < 20 GU: Keep ins and outs even, decrease all IVF to sum of 75 cc/hour, balance electrolytes based on lab Heme: sq heparin bid, CBC ID: ensure d/c of perioperative antibiotics Tubes/Lines/Drains: Keep triple lumen, keep a-line, Neck JP, chest tube, NGT, J tube Activity: ambulating, PT consult Disposition: ISCU, but can transfer to floor if doing well Post Op Day 4 Neruo: epidural, PCA CV: telemetry, watch for afib Respiratory: chest PT and deep breathing, chest tube to water seal, check for leak of chyle or bile, Neck JP ensure holding bulb suction GI: If + flatus, D/C NGT, J tube feeding, 20 cc/hour to increase by 20 cc every 8 hours as tolerated to a maximum 100 cc/hour GU: pt should be negative for the day, balance electrolytes based on labs Heme: sq heparin bid, CBC ID: no antibiotics Tubes/Lines/Drains: PICC line, Neck JP, chest tube, J tube Activity: ambulating, PT consult Disposition: floor alert CRC of possible discharge on POD #8-14 Post Op Day 5,6 Neruo: epidural, d/c PCA, liquid roxicette via j tube CV: telemetry, watch for afib Respiratory: chest PT and deep breathing, chest tube to water seal, looking for chyle and bile, Neck JP ensure holding bulb suction GI: tube feeds to 100 cc/hour x 20 hours, GU: achieve baseline weight and even fluid balance for hospitalization, may need diuresis, balance electrolytes based on labs Heme: sq heparin bid, CBC ID: no antibiotics Tubes/Lines/Drains: PICC line, Neck JP, chest tube, J tube Activity: ambulating, PT consult Disposition: floor, alert CRC of possible discharge on POD #8-14, prepare for rehab or home with VNA, prepare for tube feeding Post Op Day 8 Neruo: liquid roxicette via j tube, make sure patient has liquid roxicette (bottle, not just Rx) for home CV: d/c telemetry, Respiratory: D/c chest tube and jp if no evidence of leak after drinking clears GI: advance to clear liquid diet, make sure nutrition educates patient on diet, albumin/prealbumin shortly before discharge, resume home meds crushed and given P.O., j tube teaching, tube feeds to 100 cc/hour x 20 hours GU: achieve baseline weight and even fluid balance for hospitalization, may need diuresis, balance electrolytes based on Heme: sq heparin bid, ID: no antibiotics Tubes/Lines/Drains: PICC line,, J tube Activity: ambulating, PT consult Disposition: floor, alert CRC of possible discharge on POD #8-14, prepare for rehab or home with VNA, prepare for tube feeding Post Op Day 7 Neruo: d/c epidural, liquid roxicette via j tube CV: telemetry, watch for afib Respiratory: chest PT and deep breathing, chest tube to water seal. Neck JP ensure holding bulb suction GI: obtain swallow study to rule out anastomotic leak and evaluate gastric emptying, can start sips of clears if swallow study is favorable, d/c TPN if tolerating tube feeding, tube feeds to 100 cc/hour x 20 hours GU: achieve baseline weight and even fluid balance for hospitalization, may need diuresis, balance electrolytes based on labs Heme: hold sq heparin in expectation of epidural removal, CBC ID: no antibiotics Tubes/Lines/Drains: PICC line, Neck JP, chest tube, J tube Activity: ambulating, PT consult Disposition: floor, alert CRC of possible discharge on POD #8-14, prepare for rehab or home with VNA, prepare for tube feeding Rehab Discharge Neruo: liquid roxicette via j tube, make sure patient has liquid roxicette (bottle, not just Rx) for home GI: clear liquid diet, tube feeds to 100 cc/hour x 20 hours Tubes/Lines/Drains: d/c PICC line, J tube Disposition: home/rehab with follow up in 2 weeks with a CXR in Dr. Erkmen’s clinic Recovery in Rehab on tube feeds Discharge Plan □Diet □F/U appt with Dr. Erkmen in Pain management questions 2 weeks □ Copy of discharge to PA, NP, Nurse Navigator, Linda Mason, and Nutrition Services □ Copy of discharge to PCP Post Discharge Weeks 2-12: Office visits every 2-3 weeks for weight checks, wound checks, chest xrays, gradually advance diet Post Discharge Week 12: Remove feeding tube, discuss return to work (depending on occupation) Follow up with Esophageal Cancer Clinic as needed and attend Esophageal Reunion Meetings every 6 months. Fill out questionnaire Yes and referring physicians Home No Recovery at Home on tube feeds Call PA and/or NP 650-8537 Post-operative Post-operative Overnight in ICU Post Op Day 1 Neruo: epidural, can start PCA if awake CV: Continue telemetry, keep SBP > 100, avoid pure alpha agents for pressors Respiratory: Extubated, chest PT and deep breathing, chest tube to -20 Neck JP ensure holding bulb suction CXR to monitor conduit and lungs GI: NPO/NGT to low wall suction, flush every 30 cc to ensure patency J tube to gravity, flush with 30 cc every 8 hours, GI prophylaxis GU: Keep ins and outs even, avoid fluid overload, maintenance IVF, balance electrolytes based on labs Heme: sq heparin bid ID: Complete antibiotics for prophylaxis Tubes/Lines/Drains: Keep triple lumen, keep a-line, Neck JP, chest tube, NGT, J tube Activity: up in chair Disposition: can transfer to ISCU if doing well Aim 4: To optimize efficiency and evidencebased medicine • Identify optimal, evidence-based practices • Identify opportunities to – Educate patients – Educate providers – Reorganize current resources Aim 5: To track process and outcomes • Retrospective chart review of pathway patients • Compare to previous consecutive esophagectomy patients Pathway vs. Controls • No demographic differences Immeasurable Benefits • Patient connection with providers • Providers working as a team with equal voice • Identify deficiencies Limitations • Few patients • Maintenance of pathway • Resources Future Directions • Pathway integrated with database • Pathway manager? Thank You Questions? To personalize the experience of each patient treated for esophageal cancer at DHMC-NCCC • Patient Binder • Patient Video • Shared Decision-making Shared Decision-Making Learning about esophageal cancer Obtaining high quality information about available options, the pros and cons Decision based on what is important to you. Learning about esophageal cancer •The esophagus is a muscular tube connecting the mouth and the back of the throat (pharynx) to the stomach. •Normal cells of the esophagus grow and divide to replace old or damaged cells •Sometimes this process goes wrong. New cells form when the body does not need them or damaged cells do not die as they should. The buildup of extra cells forms a mass of tissue called a tumor •Esophageal cancer begins in the inner layer of the esophagus. Over time, the cancer may 1. invade more deeply into the esophagus 2. Spread to nearby lymph nodes* 3. Spread to other parts of the body *Lymph nodes normally act as filters. They filter out infection and cancer. Often, esophageal cancer will spread to lymph nodes before spreading to other parts of the body Thank You
© Copyright 2026